Abstract
Reports of penile sarcoidosis are rare in the literature. We describe the case of a male who presented with several months of distal penile swelling and progressive inability to retract the foreskin. Firm, non-tender subcutaneous nodules were palpated near the base of the penis. The patient ultimately underwent penile skin resection, partial scrotal resection, and split thickness skin graft to the penis after failing multiple conservative treatments. Pathology revealed non-caseating granulomatous lesions which in addition to CT chest findings of bilateral hilar adenopathy suggested a diagnosis of penile sarcoidosis.
Keywords: Penile disorders, Lymphedema, Sarcoidosis
1. Introduction
Sarcoidosis is a heterogeneous non-caseating granulomatous disease which is often challenging to diagnose. Whereas its most characteristic manifestation is pulmonary disease, extrapulmonary involvement can affect virtually any organ system. Subcutaneous sarcoidosis is one such presentation consisting of nontender nodules in the deep dermis,.1 Presently, reports of penile sarcoidosis in the literature are limited to several case reports spanning the past five decades,.2, 3, 4, 5 Here we report the case of a male in his late forties who presented with several months of distal penile swelling caused by subcutaneous sarcoidosis.
2. Case presentation
The patient is a male in his late forties who initially presented to the emergency department with a chief complaint of three weeks of penile swelling with progressive inability to retract the foreskin. Additional symptoms included mild numbness of the glans penis and ambiguous diffuse abdominal tenderness. Pertinent negatives were a lack of fever, dysuria, or hematuria. All standard labs were within normal limits. CT of the pelvis and abdomen was notable only for foreskin swelling, with no evidence of infection.
The patient was seen in our practice four weeks later for unresolved penile swelling. By this time, he had had an MRI which was unrevealing, and had undergone conservative treatments with sitz baths, antibiotics, antifungals, and steroids with no improvement. On physical examination an indurated area on the proximal penile shaft was noted, with several palpable nodules (Fig. 1). Suspecting that these lesions might be causing distal lymphedema, surgical options were discussed with the patient and weighed against conservative options such as wrapping. The patient elected to undergo surgery and was scheduled for combined surgical intervention with urology and plastic surgery in the form of total penile skin resection, partial scrotal resection, scrotoplasty, and split thickness skin graft to the penis.
Fig. 1.
Pre-operative photograph of patient's penis and scrotum, demonstrating edema and a buried appearance.
In the interim, the patient had two visits to an out-of-state emergency department due to bilateral leg swelling, and shortness of breath. On exam he was found to have an ecchymotic rash on the right arm with palpable, non-mobile subcutaneous masses. His workup was notable for a significantly elevated D-dimer of 1276. Deep vein thrombosis and pulmonary embolism were ruled out in the emergency department. On CT angiogram of the chest “significant hilar and subcarinal lymphadenopathy” was noted without any focal pulmonary lesions.
The surgical procedure was eventually performed by making a circular incision around the prepubic area and dissecting down to the pubic bone. All prepubic tissue, penile skin, and some scrotal skin was resected (Fig. 2). Four one-centimeter mobile nodules were identified and dissected near the base of the penis and sent for intraoperative frozen pathology revealing “severe granulomatous disease, negative for malignancy.” Rotational flaps from the suprapubic and inguinal tissue were developed and used to cover the surgical defect over the pubic bone and the spermatic cords, and a 15-Blake drain was left in place. Finally, a Y-Z technique scrotoplasty was used to recreate the median raphe before the operation was turned over to the plastic surgery team to perform a skin graft to the penis.
Fig. 2.
Intra-operative photograph of patient's penis status post total penile skin resection.
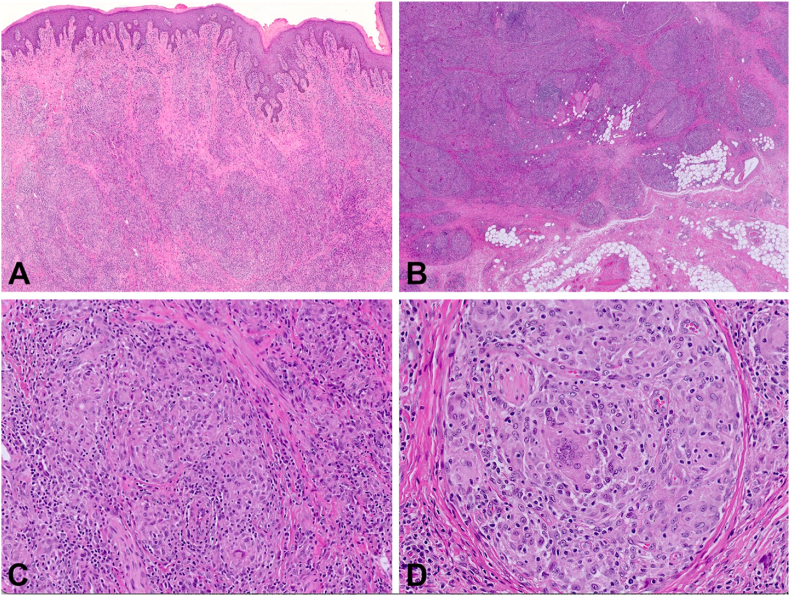
The removed nodules were further studied by the pathology team. Gross examination revealed skin excisions (largest 10.4 x 6.7 × 3.5 cm) with full-thickness induration. The process was diffuse with no discrete mass formation. The cut surfaces were diffusely tan and firm. Minimal uninvolved tissue was identified. The histologic examination revealed marked noncaseating granulomatous inflammation and fibrosis (Fig. 3A–D). Grocott methenamine silver (GMS) and Acid-Fast Bacillus (AFB) and stains failed to reveal infectious organisms. The pathologic results in combination with the CT chest findings of adenopathy and an elevated D-dimer, were most consistent with a diagnosis of sarcoidosis with penile subcutaneous lesions.
Fig. 3.
Microscopic Features revealed diffuse inflammatory process proliferating as sheets and nodules separated by fibrosis involving the dermis (A) and extending into the subcutaneous adipose tissue (B). The inflammatory process was composed noncaseating granulomas with epithelioid histiocytes, multinucleated giant cells, lymphocytes and plasma cells (C–D).
On follow-up with the surgical teams 6 weeks post operation the patient was healing well and penile swelling was reduced.
3. Discussion
Extrapulmonary manifestations of sarcoidosis can be difficult to recognize even for experienced clinicians. Recognizing sarcoidosis as a cause of penile pathology is even more challenging due to its rarity and scarcity of published information. One report described sarcoidosis involving the male urethra in a patient who presented with dysuria, hematuria, and ulcerative skin lesions,.2 Another case report described scrotal and penile swelling secondary to sarcoid granulomas in the inguinal lymph nodes with a possible epidydimal lesion,.3 Finally, two reports have been published on patients presenting with cutaneous sarcoid lesions of the penis,.4,5
The patient presented in this case had an initial complaint of distal swelling of the foreskin refractory to conservative management. Diagnosis was made more difficult by a lack of significant radiologic findings. The granulomatous lesions were discovered on physical exam, highlighting the importance of a thorough physical exam during any diagnostic workup. Identification of the lesions as noncaseating granulomas, and ruling out of infectious causes by the pathologist led to the conclusion that the patient's symptoms were most consistent with sarcoidosis. This diagnosis was supported by the presence of bilateral hilar lymphadenopathy on CT chest, as well as the presence of nodular lesions on his arm. Furthermore, the patient's symptoms of lymphedema in the lower limbs also supports the diagnosis of sarcoidosis.
4. Conclusion
Here, we have presented the case of a male with progressive lymphedema of the penile shaft and foreskin caused by proximal non-caseating subcutaneous granulomatous lesions. Given the multitude of imaging, pathology, and physical exam findings, the cause of the patient's symptoms was determined to be sarcoidosis. While only sparsely documented in the literature, sarcoidosis can affect the penis with subcutaneous lesions and associated lymphedema caused by proximal disruption of lymphatic vessels and nodes. Therefore, sarcoidosis should be on the differential when evaluating a patient with new penile edema or skin lesions.
Declaration of competing interest
The authors have no conflicts of interest to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Wanat K.A., Rosenbach M. Cutaneous sarcoidosis. Clin Chest Med. 2015;36(4):685–702. doi: 10.1016/j.ccm.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Mahmood N., Afzal N., Joyce A. Sarcoidosis of the penis. Br J Urol. 1997;80(1):155. doi: 10.1046/j.1464-410x.1997.00280.x. [DOI] [PubMed] [Google Scholar]
- 3.Vahid B., Weibel S., Nguyen C. Scrotal swelling and sarcoidosis. Am J Med. 2006;119(11):e3. doi: 10.1016/j.amjmed.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Rubinstein I., Baum G.L., Hiss Y. Sarcoidosis of the penis: report of a case. J Urol. 1986;135(5):1016–1017. doi: 10.1016/s0022-5347(17)45964-7. [DOI] [PubMed] [Google Scholar]
- 5.Wei H., Friedman K.A., Rudikoff D. Multiple indurated papules on penis and scrotum. J Cutan Med Surg. 2000;4(4):202–204. doi: 10.1177/120347540000400406. [DOI] [PubMed] [Google Scholar]