Abstract
Objectives
We aimed to systematically map the extent, range and nature of research activity on value-based healthcare (VBHC), and to identify research gaps.
Design
A scoping review with an additional cited reference search was conducted, guided by the Joanna Briggs Institute methodology.
Data sources
The search was undertaken in PubMed, Embase and Web of Science.
Eligibility criteria
Eligible articles mentioned VBHC or value with reference to the work of Porter or provided a definition of VBHC or value.
Data extraction and synthesis
Data were independently extracted using a data extraction form. Two independent reviewers double extracted data from 10% of the articles. Data of the remaining articles (90%) were extracted by one reviewer and checked by a second. The strategic agenda of Porter and Lee was used to categorise the included articles.
Results
The searches yielded a total of 27,931 articles, of which 1,242 were analysed. Most articles were published in North America. Most articles described an application of VBHC by measuring outcomes and costs (agenda item 2). The other agenda items were far less frequently described or implemented. Most of these articles were conceptual, meaning that nothing was actually changed or implemented.
Conclusion
The number of publications increased steadily after the introduction of VBHC in 2006. Almost one-fifth of the articles could not be categorised in one of the items of the strategic agenda, which may lead to the conclusion that the current strategic agenda could be extended. In addition, a practical roadmap or guideline to implement VBHC is still lacking. Future research could fill this gap by specifically studying the effectiveness of VBHC in day-to-day clinical practice.
Keywords: Health policy, Quality in health care, HEALTH SERVICES ADMINISTRATION & MANAGEMENT
Strengths and limitations of this study.
The search method of this scoping review was comprehensive: it includes a large set of articles from a long period of time (2006 to present) with all peer-reviewed study designs.
With this scoping review, a database was created that can contribute to more in-depth systematic reviews to further explore what is known within each of the agenda items.
Practical VBHC improvement initiatives might be under-represented in this study because grey literature and non-peer-reviewed articles were not included.
The included articles have not been assessed for quality because of the scoping nature of this review.
Introduction
In 2006, value-based healthcare (VBHC) was introduced in the USA as a way to reform healthcare.1 Rising costs, mounting quality issues and an increasing healthcare demand prompted the development of the VBHC concept by Porter and Teisberg.1 According to them, improving value for the patient should be the overarching goal in healthcare. In healthcare, there are different approaches of defining and measuring value. In VBHC, value is defined as the health outcomes achieved per dollar spent.1 To improve patient value, healthcare delivery should be organised around medical conditions over the full cycle of care. Universal measurement of value (outcomes and costs) is an important element in monitoring improvement.2
Strategic agenda for value transformation
In 2013, a strategic agenda was published, consisting of six agenda items for implementing a high-value healthcare delivery system (box 1).3 The agenda items were intended to support healthcare providers in the transition from a focus on volume, that is, being organised around functionally organised departments and specialties, to a focus on value, that is, being organised around what matters to patients with a specific medical condition.
Box 1. The six agenda items of the strategic agenda3.
Organise into integrated practice units (IPUs) around the patient’s medical condition.
Measure outcomes and costs for every patient.
Move to bundled payments for care cycles.
Integrate care delivery across separate facilities.
Expand excellent services across geography.
Build an enabling information technology platform.
Implementation of VBHC
The implementation of VBHC requires a major transition at both the level of healthcare providers as well as at the level of (national) healthcare systems. Healthcare providers, such as hospitals, are typically (vertically) organised around functional departments and specialties. Transitioning towards an organisation that is based on medical condition (horizontal) (agenda item 1) requires a fundamental reorganisation of hospitals and their collaborating care chain partners (agenda item 4). Measuring outcomes over the full cycle of care for a certain medical condition (agenda item 2) also requires further major change. When VBHC was introduced in 2006, healthcare quality systems were aimed at monitoring providers’ compliance to (international) quality guidelines and norms. At the time, quality indicators were primarily focused on process optimisation and safety. Health outcomes were hardly available and not measured at the level of medical conditions. Moreover, costs should be measured over the full cycle of care taking the true costs of care delivery into account. This requires a different approach for most healthcare providers (agenda item 2). The reimbursement of healthcare providers should move to payment for value, which requires major changes for healthcare providers, and for health insurance companies and healthcare industry, such as pharmaceutical companies (agenda item 3). The expansion of excellent care across geography (agenda item 5) is challenging, because it arises from the progress on the other agenda items. Finally, building an enabling information technology (IT) platform (agenda item 6) is essential for the value transition. The availability of high-quality data and IT infrastructure is named one of the main cornerstones to move forward with VBHC.4
The maturity of VBHC
VBHC has become a popular vision for healthcare organisations. Since the introduction of VBHC in the USA, the concept has spread around the world, and an increasing number of healthcare providers are adopting VBHC principles in order to continuously improve care. The article ‘What is value in health care?’5 has since been cited over 4500 times.6 However, few details have been published on how to practically implement VBHC. The strategic agenda proposed the major themes that need to be addressed in healthcare, but how to actually implement these items is hardly described. VBHC has been introduced as a strong vision for healthcare, but a practical guideline or scientific proof for the success of the proposed strategic agenda is lacking. As a result, various aspects of VBHC are only superficially understood and interpreted in different ways.7 Scientific output on VBHC is important since the healthcare sector, perhaps more than in economics or management, uses an evidence-based paradigm. Healthcare professionals are used to consider the scientific evidence before implementing an organisational reform such as VBHC.
In order to support organisations in the implementation of VBHC, it is important to understand how the VBHC concept and strategic agenda have been used in different contexts and have evolved over time. Therefore, the aim of this scoping review was to systematically map the extent, range and nature of research activity on VBHC over the last 15 years, and to identify potential research gaps. As this is a scoping review, the quality of the included articles was not assessed.
Methods
This scoping review was guided by the Joanna Briggs Institute (JBI) methodology for conducting scoping reviews,8 to answer the main research question: ‘What are the extent, range and nature of research activities on VBHC over the last fifteen years, and what are the research gaps?’
Patient and public involvement
Patients and the public were not involved in this study’s design, conduct or dissemination plans.
Eligibility criteria
The first eligibility criterion was that the article had to discuss or refer to VBHC. This criterion was met if the article (1) mentioned VBHC or value with reference to the work of Porter,1 3 5 9–11 or (2) provided a definition of VBHC or value in line with Porter’s definition. The purpose of this criterion was to be inclusive towards all interpretations of VBHC. If VBHC or value was only mentioned as a suggestion for further research, the article was not included.
The second criterion was that the context of the article had to be healthcare related. No restrictions were made with regard to the type of participants, type of study design or the outcomes measured. Only peer-reviewed articles were included.
Information sources and search strategy
The three-step search strategy from the JBI was used.8 First, an initial limited search was performed in PubMed. The title, abstract and index terms of the retrieved articles were analysed to provide keywords for the final search. Second, the final search was carried out using the identified keywords from step 1. This search was undertaken in PubMed, Embase and Web of Science (online supplemental file 1). Third, the reference lists of all the retrieved articles were examined for additional articles. Additionally, a cited reference search for the article ‘What is value in health care?’ was conducted.5 In perspective with Porter’s other references on VBHC, this is his most cited article.
bmjopen-2022-064983supp001.pdf (44.4KB, pdf)
Only articles published in English were included. The search was limited to publications between 1 January 2006 and 7 June 2021 (the day of the search) because of the introduction of VBHC in 2006.1
Selection process
All search results were uploaded to EndNote. Duplicates were removed before screening. Titles, abstracts and full texts were independently assessed for eligibility by pairs of reviewers (JRGV, KD, GS, PvdN, MMG). Reviewers did not screen the articles they had written themselves. Discrepancies between reviewers were resolved in consensus meetings. If necessary, a third reviewer made the final decision. For the selection process, the application Rayyan was used.12
Data extraction
Data were independently extracted using a data extraction form in Research Electronic Data Capture which was specifically developed and pilot tested for this review.13 14 Extraction questions were aimed at the article’s main characteristics, references to VBHC, design, measured outcomes and the implemented elements of the strategic agenda. For each article, the reviewers (JRGV, KD, GS, PvdN, MMG) indicated which items of the strategic agenda were reported, and had the possibility to write down potential new agenda items.
Data from 10% of the articles (at random) were double extracted by two independent reviewers. Discrepancies in the extracted data were discussed and resolved by a set of reviewers. Thereafter, data extraction of the remaining 90% was performed by one reviewer (JRGV, KD, GS, MMG) and checked by a second.
Analysis and presentation of results
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart was used to summarise the review decision process.15 The extracted data were summarised quantitatively. The categorical data were expressed as frequencies. The statistical analysis was performed with use of Mathematica software (Wolfram Research, Mathematica V.12.1.1, Champaign, Illinois, 2021).
Results
Selection
The search yielded a total of 27,931 records, of which 2,218 records were found by the cited reference search (figure 1). After duplicate removal, 12,909 potentially relevant articles remained. Title and abstract screening resulted in 8,078 articles to be excluded. Ten articles were excluded because no full text was available. The remaining 4,821 articles were assessed for eligibility in a full text screening, of which 74 were excluded because they were not peer reviewed and 3,501 were excluded because they did not discuss or refer to VBHC. In total, 1,246 articles were included in this review. Four of these articles were not included in the analysis because they were written by Porter and described elements of the VBHC theory (source reports). Finally, 1,242 articles were analysed.2 10 11 16 The full data set with included articles and collected outcomes can be found in online supplemental file 2.
Figure 1.
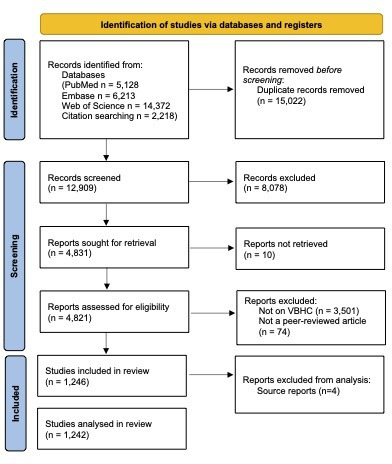
Flow chart with review decision process. VBHC, value-based healthcare.
bmjopen-2022-064983supp002.xlsx (497.8KB, xlsx)
Review findings
General
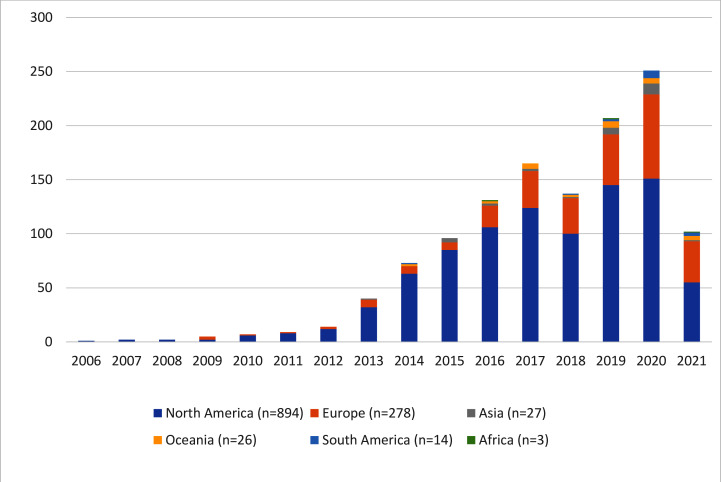
From 2006 to 2011, fewer than 10 articles were published per year (figure 2). The number of articles increased yearly, with the exception of 2018. North American centres published 72% (n=894) of the articles and published all the included articles up to the year 2009. In Europe, the first articles on VBHC were published in 2009. South America, Oceania, Asia and Africa together published 5% of the included articles (n=70). The location of the articles was based on the affiliation of the first author.
Figure 2.
Bar chart with number of publications over the years. The search was conducted in June 2021.
Most articles were original articles (n=627, 50%), followed by narrative reviews, perspectives, opinion papers and short report (n=506, 41%). Six per cent of the articles were systematic or scoping literature reviews (n=69). Case studies accounted for 3% of the included articles (n=36) and methodologies for less than 1% (n=4) (table 1).
Table 1.
Characteristics of included articles
| Characteristics | n (%) |
| Type of article | |
| Original article | 627 (50) |
| Short report/brief communications/perspective/commentary/opinion paper/narrative review | 506 (41) |
| Literature review (scoping or systematic) | 69 (6) |
| Case study | 36 (3) |
| Methodology | 4 (<1) |
| Study design | |
| Observational design | 561 (89) |
| Experimental design | 42 (7) |
| Both designs | 4 (1) |
| Unknown | 5 (1) |
| Not applicable | 15 (2) |
| Research method | |
| Quantitative method | 474 (76) |
| Qualitative method | 72 (11) |
| Both methods | 67 (11) |
| Unknown | 8 (1) |
| Not applicable | 6 (1) |
| Data collection | |
| Retrospective | 337 (60) |
| Cross-sectional | 113 (20) |
| Prospective | 86 (15) |
| Mix of retrospective and prospective | 14 (3) |
| Unknown | 5 (1) |
| Not applicable | 6 (1) |
| Type of organisation* | |
| Hospital | 687 (55) |
| Public/preventive care organisation | 27 (2) |
| University | 12 (1) |
| General practitioner | 11 (1) |
| Pharmaceutical organisation | 8 (1) |
| Health insurer | 3 (<1) |
| Other† | 56 (5) |
| Unknown | 77 (6) |
| Not applicable | 378 (30) |
*Total is more than 100% because multiple answers could be selected.
†For example: ambulatory care organisations, databases, dental care organisations, companies, focus clinics, government, home care facilities, non-governmental organisations (NGOs), primary healthcare, rehabilitation facilities.
Most of the original articles had an observational study design (n=561, 89%); 7% of the articles had an experimental design (n=42). In 76% of the original articles quantitative research methods were used (n=474). A small part of the articles used a qualitative method (n=72, 11%). Of the 561 observational articles, the majority collected the data retrospectively (n=337, 60%).
The effect measures or endpoints in the original articles were clinical outcomes (n=359, 57%), costs (n=291, 46%), patient-reported outcome measures (PROMs) (n=125, 20%), patient-reported experience measures (PREMs) (n=31, 5%), no outcomes (n=73, 12%) or were indicated not applicable (NA) (n=47, 8%). Four articles measured all the above effect measures (clinical outcomes, costs, PROMs and PREMs). Twenty-four per cent of the articles that measured PROMs measured generic PROMs (n=30), 33% measured condition-specific PROMs (n=41) and 31% measured both (n=39). In 12% of the articles that measured PROMs (n=15), it was unknown which PROMs were used.
When comparing the two continents that published the most articles (North America and Europe), a difference in measured endpoints was noted. In North America, the emphasis was on measuring clinical outcomes and costs (respectively n=274, 62% and n=243, 55%). While in Europe, the emphasis was on measuring clinical outcomes and PROMs (respectively n=67, 47% and n=46, 32%). Costs were measured less frequently as endpoint in Europe (n=35, 24%).
Most original articles reported on patients (n=463, 74%), some on healthcare professionals (n=116, 19%) (table 2).
Table 2.
Population of original articles
| Study population (n=627) | n (%) |
| Type of population* | |
| Patients | 463 (74) |
| Healthcare professionals | 116 (19) |
| Other | 52 (8) |
| Not applicable | 52 (8) |
| Median size of patient population | 565 (min: 3, max: 18.474.860) |
| Median size of healthcare professional population | 40 (min: 3, max: 185.075) |
*Total is more than 100% because multiple answers could be selected.
Medical context
More than 50% of the articles reported on hospital care (table 1). The most often studied medical specialty was orthopaedic surgery (n=182, 15%) (table 3).
Table 3.
Medical specialties studied in the included articles
| Medical specialty* | n (%) |
| Orthopaedic surgery | 182 (15) |
| Internal medicine† | 178 (14) |
| Surgery† | 111 (9) |
| Radiology† | 61 (5) |
| Paediatrics† | 50 (4) |
| Anaesthesiology | 38 (3) |
| Urology | 32 (3) |
| Plastic surgery | 31 (2) |
| Thoracic surgery | 31 (2) |
| Otolaryngology | 29 (2) |
| Obstetrics and gynaecology | 26 (2) |
| Neurological surgery | 22 (2) |
| Colon and rectal surgery | 20 (2) |
| Neurology | 20 (2) |
| Physical medicine and rehabilitation | 20 (2) |
| Neurological surgery and orthopaedic surgery | 18 (1) |
| Psychiatry | 16 (1) |
| Ophthalmology | 12 (1) |
| Emergency medicine | 10 (1) |
| Dermatology | 9 (1) |
| Family medicine | 4 (<1) |
| Allergy and immunology | 2 (<1) |
| Pathology | 2 (<1) |
| NA | 248 (20) |
| Multiple | 18 (1) |
| Other† | 52 (4) |
*List of specialties according to the American Board of Medical Specialties.25
†Subspecialties are displayed in online supplemental file 3.
NA, not applicable.
bmjopen-2022-064983supp003.pdf (71KB, pdf)
Value-based healthcare
All included articles were rated for their extent to which VBHC played a role in the article. From highest to lowest VBHC rating, the categories were: (1) describing or implementing multiple agenda items and/or using the whole VBHC theory (n=171, 14%); (2) describing or implementing one of the agenda items (n=395, 32%); (3) discussing or using value in the article with Porter’s definition, but not discussing or implementing any agenda items (n=373, 30%); (4) mentioning VBHC only as a motivation or context in the article (n=290, 23%) (table 4). Furthermore, the type of article was registered. Most articles were either conceptual or with an application. Conceptual articles are solely descriptive, whereas articles with an application researched a topic in daily practice. Only 11% of the included articles were development studies, meaning that an innovation or initiative was developed but not implemented.
Table 4.
Overview of each article’s relation to VBHC
| Extent to which VBHC played a role in the article (as rated by extractors) | n (%) |
| 1. Describe or implement multiple agenda items (highest rating). | 171 (14) |
| 2. Describe or implement a specific part of VBHC or the strategic agenda. | 395 (32) |
| 3. Discuss how to improve value or measure value, with value defined. | 373 (30) |
| 4. VBHC is context or motivation for the study (lowest rating) | 290 (23) |
| Other* | 13 (1) |
| Type of article‡ | n (%) |
| Conceptual article | 528 (43) |
| Article with a development | 138 (11) |
| Article with an application† | 579 (47) |
*For example: discussed VBHC as one of the possible approaches or description of a new interpretation of VBHC.
†For example: research into an implementation or retrospective research into two different patient groups.
‡Total ws more than 100% because multiple answers could be selected.
VBHC, value-based healthcare.
Most of the articles (n=953, 77%) referred to Porter’s article ‘What is value in health care’5 (online supplemental file 4). Articles that contained multiple sections (n=735) mostly referred to a paper of Porter in the introduction section (n=564, 77%), or the discussion section (n=233, 32%) (online supplemental file 4).
bmjopen-2022-064983supp004.pdf (77KB, pdf)
Implementation in general
In 288 articles (23%), the effect of an implementation was measured. The definition of an implementation article was that the article described a new process or technique implemented in daily work and presented the results. Two hundred and seven of these articles (79%) reported that the implementation was a success. Implementation initiatives were considered successful if the authors indicated in the discussion and/or conclusion section that the implementation had led to improvement. Forty-five articles (16%) had no statements regarding the effectiveness of implementation and 16 articles (5%) reported that the implementation was not a success.
Items of the strategic agenda
The most frequently found agenda item was measuring outcomes and/or costs (n=941, 76%). All other agenda items were found in less than 10% of the articles (table 5). Five articles discussed or implemented all the agenda items.
Table 5.
Reported agenda items
| Agenda item* | n (%) |
| 1. Organise into integrated practice units (IPUs) around the patient’s medical condition. | 71 (6) |
| 2. Measure outcomes and costs for every patient. | 941 (76) |
| 3. Move to bundled payments for care cycles. | 84 (7) |
| 4. Integrate care delivery across separate facilities. | 22 (2) |
| 5. Expand excellent services across geography. | 13 (1) |
| 6. Build an enabling information technology platform. | 83 (7) |
| No item selected | 228 (18) |
*Total is more than 100% because multiple answers could be selected.
For 228 articles, no agenda item could be selected. The six most mentioned ‘new’ agenda items were ‘other type of contracting’ (n=29), ‘quality improvement’ (n=23), ‘VBHC culture’ (n=11), ‘education’ (n=10), ‘shared decision making’ (n=8) and ‘care delivery value chain’ (n=5). Table 6 shows the number of agenda items selected per article. For most articles only one agenda item was selected (n=868, 70%). All the agenda items are discussed separately in the next sections.
Table 6.
Number of agenda items selected per article
| Number of selected agenda items | n (%) |
| 0 | 228 (18) |
| 1 | 868 (70) |
| 2 | 115 (9) |
| 3 | 19 (2) |
| 4 | 6 (<1) |
| 5 | 1 (<1) |
| 6 | 5 (<1) |
Agenda item 1: organising into integrated practice units
Although 71 articles discussed an integrated practice unit (IPU), only three of them reported on the actual implementation of an IPU (4%). In most articles, the IPU was focused on one medical condition (n=32, 45%) and involved a multidisciplinary team (n=43, 61%) (table 7).
Table 7.
In-depth information regarding the strategic agenda items
| Agenda item 1: organising into integrated practice units (IPUs) (n=71) | n (%) |
| Phase of IPU* | |
| Design | 15 (21) |
| Implementation | 3 (4) |
| Evaluation of implementation | 25 (35) |
| Other | 7 (10) |
| Not applicable | 23 (32) |
| Scale in organisation | |
| In the whole organisation | 3 (4) |
| Around one disease | 32 (45) |
| Other | 7 (10) |
| Not applicable | 26 (37) |
| Unknown | 3 (4) |
| Team | |
| Yes, the team is multidisciplinary | 43 (61) |
| No, the team has one discipline/specialty | 1 (1) |
| Not applicable | 19 (27) |
| Unknown | 8 (11) |
| Agenda item 2: measuring outcomes/costs (n=941) | n (%) |
| Outcome set developed | |
| Yes | 63 (7) |
| PROM developed | |
| Yes | 13 (1) |
| Types of costs measured | |
| Direct costing† | 274 (29) |
| Indirect costing‡ | 2 (<1) |
| Direct and indirect costing | 40 (4) |
| Other | 14 (1) |
| None/not applicable | 596 (63) |
| Unknown | 15 (2) |
| Entire chain | |
| Yes | 66 (20) |
| Agenda item 3: moving to bundled payments (n=84) | n (%) |
| Type of contracting* | |
| Pay-for-performance bonuses | 26 (31) |
| Bundled payments | 66 (79) |
| Population-based payments | 7 (8) |
| Other | 17 (20) |
| Agenda item 6: building an information platform (n=83) | n (%) |
| User of platform* | |
| Healthcare professionals | 47 (57) |
| Patients | 25 (30) |
| Management | 9 (11) |
| Administrative department | 7 (8) |
| Financial department | 4 (5) |
| Other | 7 (8) |
| Not applicable | 24 (29) |
| Unknown | 5 (6) |
| Real time | |
| Yes | 8 (10) |
| Telemedicine/telehealth/e-health* | |
| Telemedicine§ | 13 (16) |
| e-Health§ | 10 (12) |
| Telehealth§ | 8 (10) |
| Other | 15 (18) |
| None | 37 (45) |
| Unknown | 2 (2) |
*Total is more than 100% because multiple answers could be selected.
†The definition of direct costing used: ‘the costs associated with medical resource utilization, which include the consumption of in-patient, out-patient, and pharmaceutical services within the health care delivery system’.26
‡The definition of indirect costing used: ‘the expenses incurred from the cessation or reduction of work productivity as a result of the morbidity and mortality associated with a given disease’.26
§Telemedicine: the provision of medical care with the use of communication technologies to connect healthcare providers and patients who are in different locations.17 Telehealth: broader scope and includes patient education, public health and in-service training for healthcare professionals.17 e-Health: applications in which internet technology is used to offer information, products and/or services in healthcare.17
PROM, patient-reported outcome measure.
Most of the articles that discussed an IPU were conceptual (n=41, 58%). Thirty-four per cent (n=24) of the articles that discussed an IPU implemented some sort of a (medical) intervention or did a comparative study. Two articles (n=2, 3%) described the development of an IPU. Four articles combined these three phases.
Agenda item 2: measuring outcomes and costs
Of 941 articles reporting on outcomes and costs, most articles compared outcomes between treatments or interventions (n=155, 16%). A quarter of the articles did not compare outcomes (n=238, 25%). Of the 554 original articles in this category, 30% (n=168) reported solely on outcomes (clinical, PROMs or PREMs), 16% (n=87) reported solely on costs and 36% (n=201) reported on both outcomes and costs. Eighteen per cent (n=98) reported on other type of endpoints.
Different types of costs were measured. Direct costs were reported in 274 articles (29%); 40 articles reported direct and indirect costs (4%). Sixty-six articles measured the costs along the entire chain (20%). No distinction was made between whether the entire care chain was located inside or outside the hospital. Sixty-three articles (7%) developed a standard outcome set and 13 articles (1%) a PROM (table 7).
Half of the articles that discussed outcomes and costs reported an application (n=486, 52%), a third of the articles were conceptual (n=308, 33%) and 10% reported on a development (n=95, 10%). Fifty-two articles reported on a combination of the three categories (n=52, 5%).
Agenda item 3: moving to bundled payments
There were 84 articles that discussed a form of bundled payments (table 7). Most of the articles were conceptual (n=55, 65%), followed by articles with an application (n=26, 31%) and articles with a development (n=2, 2%). One article described a combination of the three categories.
Besides bundled payments, ‘other forms of contracting’ were frequently discussed. For example, pay-for-performance bonuses were discussed in 48 of all included articles (4%) and population-based payments in eight articles (1%).
Agenda item 4: integrating across separate facilities
Of the 22 articles in this category, 11 reported on a collaboration between healthcare providers or hospitals (50%). One article described the collaboration between a healthcare provider and an insurance company (5%). Another article discussed the collaboration between a healthcare provider and a university (5%). For the other nine articles, the question was NA (41%).
Fifty per cent of the articles were conceptual (n=11, 50%), followed by articles with an application (n=8, 36%) and articles with a development (n=2, 9%). One article was a combination of the three categories (n=1, 5%).
Agenda item 5: expanding across geography
Thirteen articles reported on a spread of best practices across geography. Six of these articles reported on a spread within the country (national) (n=6, 46%). Seven articles reported on a spread across geography (n=7, 54%), but it remained unknown in which way. There were no articles that reported on a spread of best practices between countries (international).
Most of the articles were conceptual (n=7, 54%), followed by articles with an application (n=4, 31%) and one article reported on a development (n=1, 8%). One article was a combination of the three categories (n=1, 8%).
Agenda item 6: building an information platform
A total of 83 articles reported on information platforms. A majority of the platform users were healthcare providers (n=47, 57%), followed by patients (n=25, 30%). Ten per cent of the articles reported the use of real-time outcome information (n=8, 10%) (table 7). Thirteen articles reported on telemedicine (16%), 10 on e-health (12%) and 8 on telehealth (10%). Telemedicine was defined as the provision of medical care with the use of communication technologies to connect healthcare providers and patients who are in different locations.17 e-Health is the application in which internet technology is used to offer information, products and/or services in healthcare.17 Telehealth includes patient education, public health and in-service training for healthcare professionals.17
Most of the articles were conceptual (n=50, 60%), followed by articles with an application (n=23, 28%) and articles with a development (n=5, 6%). Five articles were a combination of the three categories (n=5, 6%).
Discussion
Main findings
This review showed that the extent, range and nature of VBHC research are large and still increasing; over the last 15 years more than 1200 articles reported on VBHC. They described (the implementation of) the strategic agenda items within various specialties. The number of published articles increased each year, especially since 2013, with the exception of 2018. Most articles were published in the USA/North America, followed by Europe.
The majority of articles described the measurement of outcomes and costs. Other agenda items were far less frequently described or implemented. Most of the articles were conceptual, meaning that nothing was actually changed or implemented. When looking at the role that VBHC played in the articles, almost half of the articles discussed or implemented one or more agenda items; only five articles described or implemented all agenda items. Most articles were published from surgical specialties. Four main observations on these results are highlighted in the following paragraphs.
First, research on VBHC focused primarily on the agenda item ‘measuring outcomes and costs’. Furthermore, this agenda item had a relatively high ratio (52%) of application articles, meaning that outcomes and costs were actually measured. All other agenda items were reported on in a more conceptual way, without actually implementing or applying anything. The predominant focus on outcomes and costs might be explained by the formulation of the value definition, in which outcomes and costs are both specifically mentioned. Furthermore, it seems relatively difficult to implement other agenda items such as bundled payments of IPUs without measuring outcomes and costs (value). The importance of measuring outcomes and costs has also been recognised in other quality of care concepts such as the Donabedian model.18 Another explanation for the popularity of measuring outcomes and costs could be the clarity of this agenda item; this item is the least susceptible to interpretation differences. Additionally, Porter stated that measuring outcomes is the most import step and he dedicated a practical article on standard outcome sets,5 which further facilitates the focus on measuring outcomes and costs. The types of outcomes and costs that were measured differed between continents. North America more often measured costs than Europe. Moreover, in the USA, VBHC was often used in the context of healthcare funding laws that place emphasis on curbing cost growth such as the Affordable Care Act (ACA). One of the goals of ACA was to expand healthcare coverage and to make healthcare affordable to more citizens.19 This focus on costs and payment methods might explain the higher number of articles measuring costs in North America.
Second, the current strategic agenda seemed to be incomplete. In 18% of the included articles, none of the current agenda items were discussed. Based on the issues that were addressed in these articles, we proposed four new agenda items: ‘quality improvement’, ‘VBHC culture’, ‘shared decision making’ and ‘education’. These four agenda items matched the new agenda items that were recently suggested.20 It is important to note that some of the new agenda items, such as shared decision making, were discussed in many of the included articles. However, in our methods, a new agenda item was only suggested by the reviewers when none of the current agenda items were checked in the data extraction form. Thus, the number of articles with new agenda items was under-reported.
Third, there was a scarcity of articles on implementation of agenda items. Only a quarter of the included articles described an implementation. The majority of these articles focused on one agenda item. Few articles described implementation of multiple agenda items. The lack of implementation articles was in line with other research in hospital settings; Reitblat et al concluded that the implementation and investigation of the strategic agenda in urology was limited21 and another scoping review specifically focusing on VBHC implementation in hospital settings showed the same scarcity.22 One reason for the lack of implementation articles might be the absence of a practical implementation guide for VBHC. The need for a roadmap that addresses the required steps for organisational changes has been acknowledged before.10 Currently, this roadmap with practical steps is still missing and the available VBHC theory is interpreted in various ways.23 This could lead to an inadequate implementation, as an ill-defined management intervention is often implemented in different ways.24 Furthermore, it was argued that a low level of understanding might result in a dilution of the concept.7 Therefore, it seems especially important to describe and observe different implementation initiatives around the world to ultimately create a guideline for each healthcare context.
Finally, it was striking that many of the included articles were focused on surgical specialties. A possible explanation is that these specialties have a longer history of quality registries (including outcome measures) and generally perform intervention-driven studies. Intervention-driven studies often compare health outcomes between interventions or patient groups. As a result, surgical articles focused more on health outcomes and linked this to the VBHC concept and the definition of value; outcomes compared with costs. Another reason could be that VBHC principles are easier to implement in surgery as there is a more direct relation between intervention and outcomes.
Strengths and limitations
Some limitations need to be considered when interpreting the results of this study. First, the search strategy did not specifically include search terms for each agenda item, which could have resulted in selection bias. Second, using the article ‘What is value in health care?’5 for the cited reference search might have resulted in the over-representation of articles focusing on measuring value, outcomes or costs. However, the representation of ‘What is value in health care’ and other references to Porter found in our study is similar to the representation found in PubMed. Third, the focus of this study was on scientific peer-reviewed articles. As a result, VBHC implementation initiatives published in ‘gray literature’ or published as non-peer-reviewed articles have not been included in this study. This might have led to an under-representation of the actual number of VBHC implementations in practice. Finally, inherent to the design of a scoping review, the included articles were not assessed for their research quality.
A major strength of this review is its broad scope. The present study provides a comprehensive overview including items such as medical specialties, countries and all strategic agenda items (including potential new ones) (online supplemental file 2). In addition, the study’s exclusion criteria deliberately generated a broad picture of the current state of research on VBHC. This has resulted in a complete picture of the current state of research on VBHC. The broad scope of this study was especially important in light of the different interpretations of the VBHC concept. Finally, to date, hardly any reviews on VBHC have been published, and existing reviews focusing on, for example, articles with an implementation of VBHC.22
Implications for clinical practice and/or research
With the exception of measuring outcomes and costs, few articles have implemented and researched the implementation of strategic agenda items. There is a need for studies that evaluate the implementation of the different strategic agenda items within different medical specialties. Insight in practical implementation is needed in order to work towards a roadmap for step-by-step implementation of VBHC. It is important to collect evidence from daily practice to serve the evidence-based paradigm of the healthcare sector. To contribute to more evidence, our database (online supplemental file 2) can be used for in-depth systematic reviews to further explore what is known within each of the agenda items.
Conclusion
This study showed that the number of publications steadily increased after the introduction of VBHC in 2006. The largest output came from North America, followed by Europe. There was a predominant focus on measuring outcomes and costs. In addition, almost one-fifth of the articles could not be categorised in one of the items of the strategic agenda, which may lead to the conclusion that the current strategic agenda could be extended. Topics such as ‘quality improvement’, ‘VBHC culture’, ‘shared decision making’ and ‘education’ were proposed as potential new agenda items. Furthermore, there was a scarcity of articles with a practical implementation, leading to the conclusion that a practical roadmap or guideline to implement VBHC is still lacking. And last, many of the included articles were focused on surgical specialties. Future research could fill the gap by specifically researching the evidence on VBHC’s effectiveness in day-to-day clinical practice.
Supplementary Material
Acknowledgments
First, we would like to thank Nienke van der Werf, information specialist at the Antonius Academy, for her help in setting up the search strategy for the three databases. In addition, we would like to thank Oscar van Staveren of the Antonius Academy for his help in finding the articles we wanted to screen full text.
Footnotes
Author contributions: JRGV, KD, MMG, MBVRvdV, DB, WJWB, FvM and PvdN designed the review. JRGV and KD conducted the literature search. JRGV, KD, GS, MMG and PvdN screened the articles for inclusion and extracted data from the included articles. JRGV, KD and MMG analysed and interpreted the data. JRGV, KD, GS, MMG and PvdN drafted the manuscript. All authors critically reviewed the manuscript. All authors approved the final version of the manuscript. PvdN is the guarantor for this work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics Approval: Ethics approval for this scoping review is not necessary under Dutch law (AVG) according to the Medical Research Involving Human Subjects Act (WMO) because no human participants were involved.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Porter ME, Teisberg EO. Redefining health care: creating value-based competition on results: Harvard business review press, 2006. [Google Scholar]
- 2.Porter ME. Value-Based health care delivery. Ann Surg 2008;248:503–9. 10.1097/SLA.0b013e31818a43af [DOI] [PubMed] [Google Scholar]
- 3.Porter ME, Lee TH. The strategy that will fix health care. Harvard Business Review 2013;91:50-+.23898735 [Google Scholar]
- 4.Cossio-Gil Y, Omara M, Watson C, et al. The roadmap for implementing value-based healthcare in European university Hospitals-Consensus report and recommendations. Value Health 2022;25:1148-1156. 10.1016/j.jval.2021.11.1355 [DOI] [PubMed] [Google Scholar]
- 5.Porter ME. What is value in health care? N Engl J Med 2010;363:2477–81. 10.1056/NEJMp1011024 [DOI] [PubMed] [Google Scholar]
- 6.Google Scholar - Citations "What is value in health care?" - M. E. Porter. [Google Scholar]
- 7.Fredriksson JJ, Ebbevi D, Savage C. Pseudo-understanding: an analysis of the dilution of value in healthcare. BMJ Qual Saf 2015;24:451–7. 10.1136/bmjqs-2014-003803 [DOI] [PubMed] [Google Scholar]
- 8.Peters M, Godfrey C, McInerney P. Chapter 11: Scoping Reviews, in JBI Manual for Evidence Synthesis. JBI, 2020. [Google Scholar]
- 9.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev 2011;89:46–52. [PubMed] [Google Scholar]
- 10.Porter ME. A strategy for health care reform--toward a value-based system. N Engl J Med 2009;361:109–12. 10.1056/NEJMp0904131 [DOI] [PubMed] [Google Scholar]
- 11.Porter ME, Larsson S, Lee TH. Standardizing patient outcomes measurement. N Engl J Med 2016;374:504–6. 10.1056/NEJMp1511701 [DOI] [PubMed] [Google Scholar]
- 12.. Available: http://rayyan.qcri.org
- 13.Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372:n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Porter ME, Teisberg EO. How physicians can change the future of health care. JAMA 2007;297:1103–11. 10.1001/jama.297.10.1103 [DOI] [PubMed] [Google Scholar]
- 17.Fatehi F, Wootton R, Telemedicine WR. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J Telemed Telecare 2012;18:460–4. 10.1258/jtt.2012.gth108 [DOI] [PubMed] [Google Scholar]
- 18.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q 1966;44):::166–206. Suppl. 10.2307/3348969 [DOI] [PubMed] [Google Scholar]
- 19.Bundled payments for care improvement initiative (BPCI) fact sheet. Available: https://www.cms.gov/newsroom/fact-sheets/bundled-payments-care-improvement-initiative-bpci-fact-sheet
- 20.van der Nat PB. The new strategic agenda for value transformation. Health Serv Manage Res 2022;35:189–93. 10.1177/09514848211011739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reitblat C, Bain PA, Porter ME, et al. Value-Based healthcare in urology: a collaborative review. Eur Urol 2021;79:571–85. 10.1016/j.eururo.2020.12.008 [DOI] [PubMed] [Google Scholar]
- 22.van Staalduinen DJ, van den Bekerom P, Groeneveld S, et al. The implementation of value-based healthcare: a scoping review. BMC Health Serv Res 2022;22:1–8. 10.1186/s12913-022-07489-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinmann G, van de Bovenkamp H, de Bont A, et al. Redefining value: a discourse analysis on value-based health care. BMC Health Serv Res 2020;20:862. 10.1186/s12913-020-05614-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colldén C, Hellström A. Value-Based healthcare translated: a complementary view of implementation. BMC Health Serv Res 2018;18:1–11. 10.1186/s12913-018-3488-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Specialty and subspecialty certificates. Available: https://www.abms.org/member-boards/specialty-subspecialty-certificates/
- 26.Boccuzzi SJ. Indirect health care costs. In: Cardiovascular health care economics. Springer, 2003: 63–79. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064983supp001.pdf (44.4KB, pdf)
bmjopen-2022-064983supp002.xlsx (497.8KB, xlsx)
bmjopen-2022-064983supp003.pdf (71KB, pdf)
bmjopen-2022-064983supp004.pdf (77KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.