Abstract
Objectives:
Older displaced persons often receive limited attention from aid organizations and policy-makers and service providers in countries of resettlement. The objective of this study is to identify the relationship between experiencing traumatic events and stressors prior to resettlement, current resettlement stressors, social support, and mental health of older Bhutanese with a refugee life experience.
Method:
Study participants were 190 older Bhutanese with a refugee life experience living in a metropolitan area in New England (US) and Ontario (Canada). We used structural equation modeling to determine the association between traumatic and stressful events in Bhutan and Nepal, current resettlement stressors, and symptoms of anxiety and depression, as measured by the GAD-7 and PHQ-9. We assessed the role of social support as an effect modifier in the relationship between these variables.
Results:
Surviving torture was associated with anxiety (p=.006), and experiencing threats to physical wellbeing in Nepal was associated with both anxiety (p=.003) and depression (p=.002). The relationship between physical threats in Nepal and current mental health were partially mediated by resettlement stressors. Social support moderated the relationship between trauma, stress, and mental health.
Conclusion:
Both past traumas and current resettlement stressors contribute to the current psychosocial functioning of older Bhutanese with a refugee life experience. Based on our findings, social support is critical in promoting mental health in this population.
Keywords: aging, refugees, trauma, resettlement stress, Bhutanese, mental health, social support
Introduction
In 2020, the number of civilians worldwide forcibly displaced from their homes due to persecution, conflict, violence, or human rights violations reached 82.4 million, with over 26 million of these identified as refugees (UNHCR, 2021). A refugee is defined as “someone who is unable or unwilling to return to their country of origin owning to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group, or political opinion” (UNHCR, 2010). It is well known that, compared to the general population, refugees have elevated risk of mental health disorders, with individual, family, and community level factors contributing to adverse outcomes (Fazel, Wheeler & Danesh, 2005; Fazel, Reed, Panter-Brick & Stein, 2012). Unfortunately, most of this existing research has focused on children and younger adults, with minimal information on the psychosocial well being of older refugees (Virgincar, Doherty & Siriwardhana, 2016).
Older refugees include older individuals currently displaced or newly relocated in a third country of resettlement as well as those aging in place in destination countries. The health and wellbeing of this population has historically received limited attention from aid organizations as well as governments and service providers in countries of resettlement (UNHCR, 2016; Ajrouch, Barr & Daiute, 2020; Lood, Haggblom-Kronlof, & Dahlin-Ivanoff, 2015). This is problematic as older refugees may have more physical and mental health concerns than younger refugees (Strong, Varady, Chadha, et al, 2015; Bazzi & Chemali, 2016). In addition, research indicates health disparities between older persons with a refugee life experience compared to others in the same age group in host countries (Torr & Walsh, 2018; Lin, Kobayashi, Tong, et al., 2020; King, Lulle, Sampaio et al., 2017; Sand & Gruber, 2018). As countries in Europe and North America in particular see an increase in the size of their population from foreign-born people aged 50 and over, there is new interest in identifying the needs of this group and improving policies and practices to promote their health (WHO Regional Office for Europe (WHO), 2018; Ciobanu, Fokkema & Nedelcu, 2017).
Mental health of older refugees
A life course approach that integrates knowledge from gerontology, refugee studies, and psychiatric epidemiology is needed to more fully understand the mental health of older individuals who have been forcibly displaced (Ben-Schlomo & Kuh, 2002; Ciobanu, Fokkema & Nedelcu, 2017; Rousseau & Frounfelker, 2019; Spallek, Zeeb & Rosum, 2011; Gilman & Marden, 2014). Processes of migration and ageing are conceptualized as “entwined trajectories” that heighten vulnerability to adverse mental health outcomes (King, Lulle, Sampaio et al., 2017). For instance, there are experiences common among the majority of older adults regardless of migration status, including concerns over maintaining functional capability, quality of life, and access to care, that may negatively impact mental health (WHO, 2018). In addition, compared to majority populations, older refugees are disproportionately burdened by historical traumas experienced during flight from country of origin and displacement as well as post-resettlement socioeconomic stressors, both predictors of current mental health among war-affected populations (Miller & Rasmussen, 2017).
The field of life course epidemiology is particularly interested in examining the temporal order of exposures to risk factors for disease and evaluating the pathways in which exposures impact health (Ben-Schlomo & Kuh, 2002). Such pathways include the accumulation of adverse exposures over time, in which researchers posit that as the number, duration, or severity of exposures increase, so does the likelihood of a negative impact on health (Kuh, Ben-Schlomo, Lynch et al., 2003). A second life course model is that of a chains of risk, in which exposures are causally linked together as “chain reactions,” with earlier lifetime adversities leading to exposures later during the lifespan, ultimately resulting in adverse health outcomes (Kuh et al., 2003). Chains of risk models frequently involve the examination of mediating and modifying factors on the pathway to health outcomes, and also investigate whether earlier life exposures increase the risk of and susceptibility to subsequent adverse events but also have an independent effect on disease (Kuh et al., 2003). Within the context of the refugee experience, a life course approach to the mental health of older refugees then entails focusing on dimensions of time relative to milestones in the refugee life experience (Spallek, Zeeb, & Rosum, 2011; Ajrouch, Barr & Daiute, 2020). Trauma exposures in countries of origin and life in displacement can be conceptualized as primary stressors that can independently have a negative impact on the mental health of refugees, but also influence current well-being via mediating mechanisms of secondary stressors experienced in resettlement (Miller & Rasmussen, 2017; Rousseau & Frounfelker, 2019).
Although a life course epidemiology theoretical framework has great promise as a way to disentangle the relationship between pre and post-resettlement traumas and stressors and current mental health, to date there has been limited application of the use of analytic approaches to evaluate risk pathways in quantitative studies of refugee mental health more broadly and older refugee psychological well-being more specifically. The vast majority of studies investigate the independent contribution of pre and post-resettlement traumas and stressors on refugee mental health, but do not assess chains of risk via mediating pathways (for exceptions see O’Donnell, Stuart & O’Donnell, 2020; Riley, Varner, Ventevogel et al., 2017; Steel, Silove, Bird, et al., 1999). This is a major shortcoming, as unpacking the differential relationships and pathways of pre- and post-resettlement exposures on mental health outcomes has implications for identifying appropriate interventions to improve the psychosocial functioning of refugees of all ages and older refugees more specifically, given their sometimes decades of exposure to traumas and stressors related to their experience as refugees.
Older Bhutanese with a refugee life experience
In the mid-1980s, Bhutan perceived ethnic-Nepali Bhutanese and other minority groups living in the country as a threat to the national identity (Rizal, 2004). The ‘One Nation, One People’ policy initiated by the Bhutanese government mandated wearing of the national dress, required use of the official language, Dzongkha, and prohibited the teaching of the Nepali language. Government actions such as the 1980 marriage laws and 1985 Citizenship Act stripped Bhutanese citizenship from ethnic-Nepali Bhutanese, and deprived them of rights including land ownership and access to education (Rizal, 2004). Pressure to leave the country intensified, with Bhutanese authorities threatening violence and carrying out rape, murder, and torture of ethnic-Nepali (Giri, 2005; Hutt, 1996). This persecution culminated in the forced displacement of over 100,000 ethnic-Nepali from Bhutan into Nepal in the early 1990’s (Hutt, 1996).
The United Nations High Commissioner for Refugees (UNHCR) assumed the responsibility of providing emergency relief to Bhutanese refugees in Nepal starting in 1991, and established refugee camps at five different locations (Hutt, 2005). There was limited opportunity for integration into the local population in Nepal for a variety of political reasons, including an influx of refugees entering the country in the early 1990’s (Banki, 2008). Bhutanese refugees were themselves very active in campaigning for repatriation and returning to Bhutan, but, even after over a dozen rounds of bilateral talks between the governments of Nepal and Bhutan, were unsuccessful (Hutt, 2005; Rizal, 2004). As a result, Bhutanese refugees lived in camps in Nepal for 15–20 years before third-country resettlement commenced in 2008 (Reiffers, Dahal, Koirala, et al., 2013). Since that time, over 90,000 Bhutanese have relocated to North America; the vast majority is in the United States, with roughly 6,000 in Canada (Embassy of the United States, 2016; International Organization for Migration, 2014). For the purposes of this paper, we use the terminology Bhutanese “with a refugee life experience” to describe study participants as opposed to calling them “refugees,” as many ethnic-Nepali Bhutanese have obtained citizenship in countries of resettlement, and therefore no longer fit the legal definition of a refugee established by the United Nations.
Ethnic-Nepali Bhutanese were exposed to a wide range of traumas and stressors in Bhutan and Nepal. Particularly noteworthy is the incarceration and torture of ethnic-Nepali by government authorities in Bhutan as a way to pressure individuals, families, and entire communities to leave the country (Van Ommeren, de Jong, Sharma et al., 2001). In the early 2000’s researchers examined the mental health of torture survivors living in refugee camps in Nepal. Compared to Bhutanese who were not tortured, those who were had higher prevalence of psychiatric disorders (including anxiety disorders and depression), psychiatric disability, and physical health problems (Van Ommeren, de Jong, Sharma et al., 2001; Thapa, Van Ommeren, Sharma, et al., 2003; Mills, Singh, Roach & Chong, 2008). Once in Nepal, Bhutanese refugees suffered physical hardships that significantly impacted their wellbeing. During the first several months in Nepal in the early 1990’s, exposure to infectious diseases led to widespread illness and death (Marfin, Moore, Collins et al., 1994). Over a decade later, UNHCR reported overall poor quality of health programs and services in established camps, including concerns over a lack of qualified health care personnel, poor management of infectious diseases, insufficient nutrition programs, and lack of coordination of services for survivors of interpersonal violence (UNHCR Evaluation and Policy Analysis Unit, 2005).
The mental health of Bhutanese has received increased attention since onset of resettlement compared to other refugee populations given the disproportionally high rate of suicide among this group, double that of the general population in the United States (Centers for Disease Control and Prevention, 2013). There is a small but growing body of literature focusing on risk and protective factors for mental health among resettled Bhutanese, with some research focusing on older Bhutanese with a refugee life experience (Im & Neff, 2020, Frounfelker et al., 2020; Lewis, 2020). Qualitative work has identified the importance of both pre-resettlement trauma and post-resettlement stressors in understanding mental health of this subgroup (Frounfelker et al., 2020; Im & Neff, 2020) as well as the role of social support and social capital may play in buffering the relationship between these factors and psychological distress (Lewis, 2020; Frounfelker et al., 2020).
Current study
The overall objective of this study is to quantitatively identify the relationship between traumatic and stressful events prior to resettlement in Bhutan and Nepal, current resettlement stressors in the United States and Canada, and mental health of older Bhutanese with a refugee life experience. An examination of these pathways of influence can serve to identify present-day factors that can be targeted for intervention to ameliorate mental health problems. We strived to answer the following research questions: 1) What is the association between past traumatic and stressful experiences and current symptoms of depression and anxiety?; 2) Is the relationship between past events and symptoms of depression and anxiety mediated by current post-resettlement socioeconomic stressors?; and 3) Is the relationship between past events, resettlement stressors and outcomes moderated by social support?
We hypothesized that surviving torture in Bhutan and threats to physical wellbeing in refugee camps in Nepal would be directly associated with current symptoms of depression and anxiety. Additionally, we hypothesized that the relationship between these past experiences and symptoms of depression and anxiety would be partially mediated by post-resettlement stressors related to physical health and economic hardships. Finally, we hypothesized that social support would be an effect modifier in the relationship between these variables.
Method
Participants
Study participants were Bhutanese with a refugee life experience living in a metropolitan area in New England (US) and a metropolitan area in Ontario (Canada) and part of a larger mixed methods community-based participatory research study on the psychosocial wellbeing of older Bhutanese. Participants were interviewed between 2017 and 2019. Eligibility criteria included being age 50 and older and first-generation ethnic-Nepali Bhutanese born outside the US or Canada. Age 50 was chosen as the lower cut-off for eligibility based on consultation with Bhutanese community members and alignment with cultural definitions of older age. Exclusion criteria included being an immediate relative (parent) of a study team member, in acute mental distress, having cognitive deficits, or physical health problems that would impair the ability to participate. A total of 190 Bhutanese participated in the study. Researchers obtained ethics approval from the Institutional Review Boards of Harvard T.H. Chan School of Public Health and McGill University Faculty of Medicine and Health Sciences.
Procedures
Data were collected in partnership between Harvard T.H. Chan School of Public Health, McGill University, and Bhutanese community-based advocacy organizations. In both the US and Canada, Bhutanese community leaders and Bhutanese research assistants (RAs) identified Bhutanese aged 50 and over known to the community organization residing in the area. RAs approached eligible individuals for study participation, and used maximum variation sampling to recruit older Bhutanese based on age and sex. In the US community, a total of 12 individuals declined participation or were ineligible, and 150 individuals enrolled in the study. In the Canadian community, a total of 10 individuals were ineligible and 40 individuals enrolled in the study; none declined to participate.
Verbal informed consent was obtained from individuals prior to the start of the interview, and included informing participants that they could decline to answer any study question. Interviews were conducted in Nepali in private in the homes of study participants, and lasted roughly one hour. Because of limited literacy in the population, questionnaires were administered orally and visual aids were used to assist participants in responding to assessments with Likert-scale response options. If participants experienced distress they could discontinue the interview or reschedule for a later time. No participants discontinued participation. All study participants were compensated for their time with a $25 gift certificate.
Measures
All study measures were selected and adapted in consultation with Bhutanese members of the larger research team with a refugee life experience. When necessary, measures were forward- and back-translated from English to Nepali using a standardized protocol that followed best practices (Van Ommeren, Sharma, Thapa, et al., 1999).
Trauma Experiences.
The Comprehensive Trauma Inventory for refugees (Hollifield, Eckert, Warner, et al., 2005) was shortened and adapted for the Bhutanese refugee context and assessed participant exposure to traumatic experiences in Bhutan and Nepal. Two trauma exposures were included in this study: surviving torture by government authorities in Bhutan and experiencing threats to physical wellbeing in refugee camps in Nepal (being physically assaulted and/or surviving a serious illness or injury).
Resettlement Hardships.
We used an adapted Post-War Adversities Index (Layne, Stuvland, Saltzman et al., 1999) to assess hardships faced by participants in the previous three months in the United States and Canada. Two hardships were measured dichotomously (yes/no) and included in the study. Economic hardship was assessed with the questions “Has your housing been very inadequate (overcrowded, unsanitary, etc.) or unfit for people to live in?” and “Have you (your family) lacked money for basic things you need (e.g., food, housing, clothing, or medical care)?” Participants with a positive response to either of these questions were coded “yes” for economic hardship. The question related to physical health was “Has someone you lived with had a serious physical disability or other chronic health problem (e.g., diabetes, heart problems)?”
Social Support.
Social support was assessed with the Medical Outcomes Social Support Survey (Sherbourne & Stewart, 1991). The survey is an 8-item validated assessment of the frequency of having concrete and emotional support in daily life. Scores range from 8 to 32, with higher scores indicating higher levels of social support. Psychometric properties of the scale in this sample indicate adequate internal validity reliability (α =.89). Item response theory graded response models were used to create latent social support theta values for each participant (Yang & Kao, 2014). Theta values in the sample ranged from −2.03 to 1.36. For the purposes of moderation analysis, scores were dichotomized into high or low levels of social support, with low including those participants with scores in the lowest third (below the theta value of −.47, n=62)
Anxiety and Depression.
Anxiety and depression were assessed with the Generalized Anxiety Disorder-7 (GAD-7) scale and Patient Health Questionnaire-9 (PHQ-9) scale. The GAD-7 is a 7-item validated anxiety assessment of the frequency of anxiety symptoms in the past two weeks (Spitzer, Kroenke, Williams et al, 2006; Lowe, Decker, Muller, et al., 2008). Scores range from 0 to 21, with higher scores indicating more severe symptoms. The PHQ-9 is a 9-item depression assessment of the frequency of depression symptoms in the past two weeks. Scores range from 0 to 27, with higher scores indicating more severe symptoms. Authors used an adapted Nepali-language version of the PHQ-9 validated in Nepal (Kohrt, Luitel, Acharya et al., 2016). Cronbach’s alphas indicate adequate internal consistency reliability for both anxiety and depression (α =.82 and .75, respectively). Item response theory graded response models were used to create latent depression and anxiety theta values for each participant and used as outcome variables. Theta values for anxiety ranged from −1.74 to 3.08, with a mean of −.0003 (SD=.91). Theta values for depression ranged from −1.95 to 2.88, with a mean of −.002 (SD=.88).
Demographics.
Information on gender (male/female) and age (continuous variable) was collected for all participants and included in analysis as potential confounders in the relationship between prior trauma experiences, resettlement stressors, and current mental health. Other sociodemographic information was included for descriptive purposes. This includes categorical variables of marital status (single, divorced/separated, widowed, married), religion (Hindu, Buddhist, Christian, Kirat, Manav Dharma), highest education (none, preschool, primary school, high school, and some college), employment and income (employed, unemployed but other income, no income), self-perceived health (poor, fair, good, very good, excellent), and health insurance (yes/no). Years resettled in the US or Canada was measured as a continuous variable.
Data Analysis
We used univariate statistics to describe the sample and participant responses on all scales and indexes. Descriptive data and item-level correlations for all measures can be found in the appendix. We performed univariate and bivariate tests of normality for the two outcome variables (depression and anxiety theta scores). Both were normally distributed (depression x2=5.79, p=.06; anxiety x2=1.28, p=.53) in univariate analysis and the bivariate test for normality failed to reject the null hypothesis (x2=6.82, df=4, p=.15). Only 1 participant had missing data on an outcome variable and was removed from analysis. We used maximum likelihood estimation for all analyses.
We used univariate statistics to identify the prevalence of exposure to traumatic events in Bhutan and Nepal and current resettlement stressors. We next tested our hypothesis that trauma exposures would be directly associated with symptoms of anxiety and depression. We conducted a path analysis controlling for gender and age, with anxiety and depression theta scores as observed, exogenous variables. Post-resettlement stressors in the United States and Canada were included as observed, mediating variables. We determined the direct, indirect, and total effects of trauma exposures in Bhutan and Nepal on mental health scores using bootstrapping (N=200) to obtain standard errors and confidence intervals (Hayes, 2009).
Finally, we tested our hypothesis that social support would moderate the relationship between trauma exposures in Bhutan and Nepal, resettlement stressors in the United States and Canada, and the outcomes. First, we estimated a model that constrained all parameters across high and low social support groups. Then, we estimated a model freeing the direct paths between model variables. We used a likelihood ratio test to compare the fit of both models, with the fully constrained model nested within the model with freely estimated paths. A number of model fit indices were used to measure how well proposed models fit the study data, including the chi-square statistic, RMSEA, the standardized root mean square residual (SRMR) and the comparative fit index (CFI). Criteria for model fit included: x2 p>.05, RMSEA <.08, SRMR<.08, CFI >.90 (Kline, 2016; Hu & Bentler, 1999). Stata 16 was used for all analysis (StataCorp, 2019).
Results
Roughly half of the sample was women (46.8%), with an average age of 64.87 (SD=9.61, range=50–87). Average length of time in the United States was 5.2 years (SD=2.5), and 7.4 years (SD=1.6) in Canada. The vast majority of participants had no formal education (83.7%) and were currently unemployed (94.7%). Although few participants had jobs, over three quarters (76.3%) had some income in the form of government benefits (such as Social Security Disability Insurance). No participant self-rated their physical health as excellent or very good, with the majority reporting fair health (63.7%) (see Table 1).
Table 1.
Sociodemographic characteristics of older Bhutanese with a refugee life experience in the United States (US) and Canada (N=190)
|
Total sample
N=190 N (%) |
US
N=150 N (%) |
Canada
N=40 N (%) |
||||
|
| ||||||
| Sex | ||||||
| Female | 89(46.8) | 76(50.7) | 13(32.5) | |||
| Male | 101(53.2) | 74(49.3) | 27(67.5) | |||
| Martial status | ||||||
| Single | 0(0) | 0(0) | 0(0) | |||
| Divorced/separated | 7(3.7) | 7(4.7) | 0(0) | |||
| Widowed | 34(17.9) | 23(15.3) | 11(27.5) | |||
| Married | 148(77.9) | 120(80) | 29(72.5) | |||
| Religion | ||||||
| Hindu | 94 (49.8) | 84(56) | 10(25) | |||
| Buddhist | 27(14.2) | 21(14) | 6(15) | |||
| Christian | 65(34.2) | 42(28) | 23(57.5) | |||
| Kirat | 3(1.6) | 2(1.3) | 1(2.5) | |||
| Manav Dharma | 1(5) | 1(0.7) | 0(0) | |||
| Highest Education | ||||||
| None | 159(83.7) | 130(86.7) | 29(72.5) | |||
| Preschool | 1(0.53) | 1(0.7) | 0(0) | |||
| Primary school (1–5) | 16(10) | 11(7.3) | 8(20) | |||
| High school | 2(1.1) | 2(1.3) | 0(0) | |||
| Some college | 3(1.6) | 2(0.7) | 1(2.5) | |||
| Employment & Income | ||||||
| Employed | 10(5.3) | 8(5.3) | 2(5) | |||
| Other income - government benefits | 145(76.3) | 107(71.3) | 38(95) | |||
| No income | 35(18.4) | 35(23.3) | 0(0) | |||
| Self-perceived health rating | ||||||
| Excellent | 0(0) | 0(0) | 0(0) | |||
| Very Good | 0(0) | 0(0) | 0(0) | |||
| Good | 11(5.8) | 10(6.7) | 1(2.5) | |||
| Fair | 121(63.7) | 86(57.3) | 35(87.5) | |||
| Poor | 58(30.5) | 54(36) | 4(10) | |||
| Health insurance | ||||||
| No | 8(4.2) | 8(5.3) | 0(0) | |||
| Yes | 182(95.8) | 142(94.7) | 40(100) | |||
|
| ||||||
| Mean | SD | Mean | SD | Mean | SD | |
|
| ||||||
| Age | 64.87 | 9.61 | 65.3 | 9.8 | 63.0 | 8.6 |
| Years in US/Canada | 5.62 | 2.48 | 5.2 | 2.5 | 7.4 | 1.6 |
A total of 19 participants (10.00%) survived torture in Bhutan and a quarter (n=46, 24.21%) survived physical assault or a serious illness/injury while in the refugee camps in Nepal. Specific to resettlement stressors in the United States and Canada, 25 (13.16%) participants reported economic insecurity, while 43 (22.63%) reported stress related to physical health.
Past traumas, resettlement stress, and mental health
There were significant total effects in the relationship between both traumas and current mental health. Surviving torture in Bhutan was associated with anxiety (β =.61, SE=.22, p=.006). Experiencing threats to physical wellbeing in Nepal was associated with both outcomes (depression: β =.49, SE=.16, p=.002; anxiety: β =.45, SE=.15, p=.003). There were significant direct paths between both torture in Bhutan and threats to physical wellbeing in Nepal and anxiety. In addition, there was a significant direct path between physical harm in Nepal and depression. Specific to resettlement stressors experienced in the United States and Canada, health stressors were associated with both anxiety and depression; economic stressors were associated with only anxiety. There was no mediation between torture in Bhutan and mental health. In regards to surviving threats to physical wellbeing in Nepal, mediating mechanisms of both economic and health stressors in the United States and Canada accounted for 46% of the relationship with symptoms of depression (p=.02) and 33% of the association with anxiety (p=.02). See Figure 1 for all significant pathways.
Figure 1.
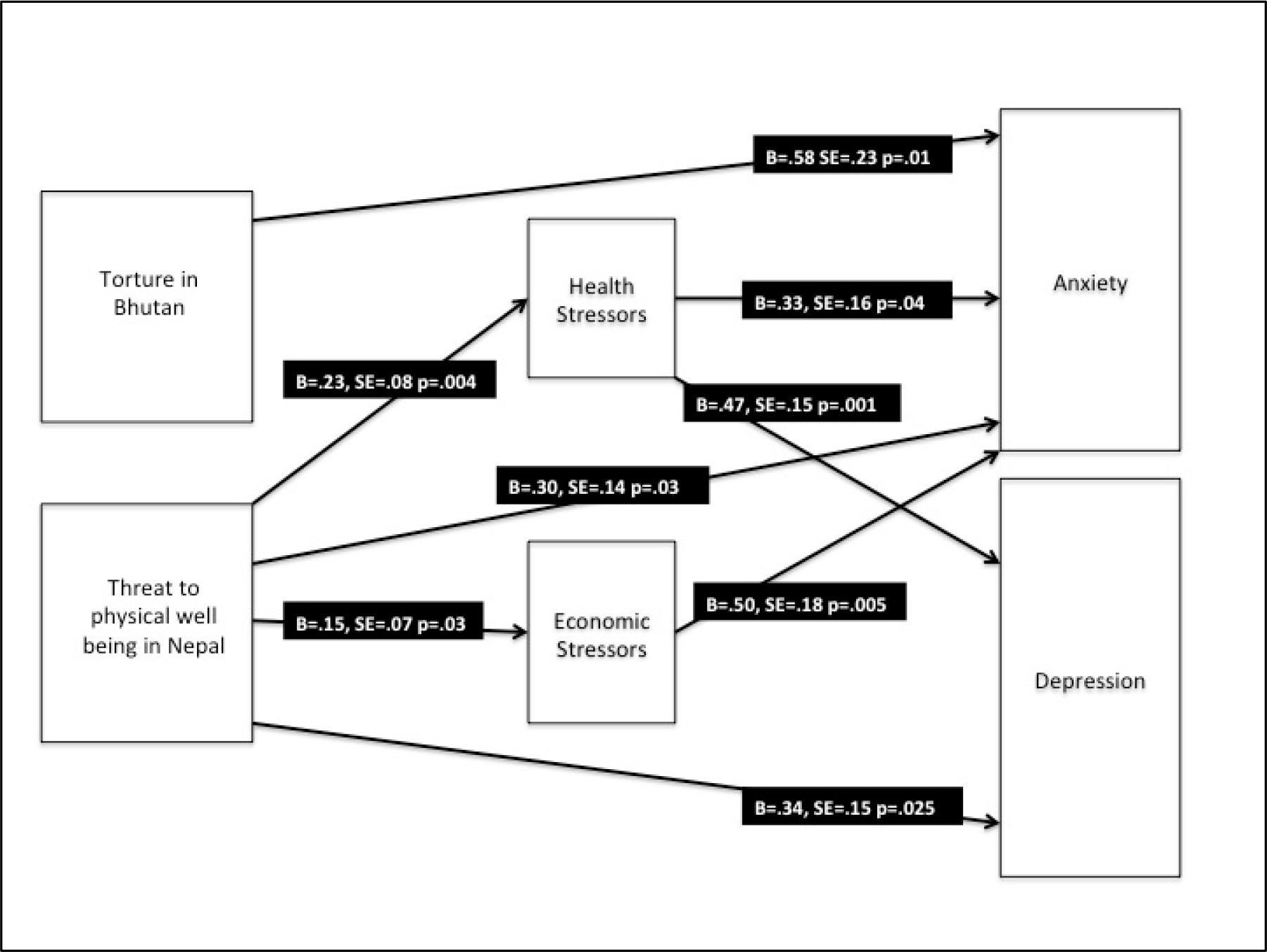
Trauma, resettlement stress, and mental health SEM model in older Bhutanese with a refugee life experience (N=189). Results present standardized regression coefficients and bootstrapped standard errors. Model controls for age and gender as exogenous variables. Model fit statistics: x2=3.62 (4) p=.46; RMSEA=.000; CFI=1.00; SRMR=.022
Moderating role of social support
We compared a fully constrained model with one that allowed pathways to differ between groups based on level of social support. A likelihood ratio test indicated that freeing pathways improved the model (x2=33.38 (16), p=.007) and had acceptable fit statistics (x2=26.92 (18), p=.08; RMSEA=.073; CFI=.94; SRMR=.063). Among the low social support group, there were significant total effects in the relationship between surviving torture in Bhutan and both anxiety (β =.68, SE=.29, p=.02) and depression (β =1.27; SE=.44, p=.004). Likewise, there were significant total effects between experiencing threats to physical wellbeing in Nepal and both outcomes (depression: β =.75, SE=.26, p=.004; anxiety: β =.56, SE=.27, p=.039).
In the lower social support group, there were significant direct paths between both traumas and depression, and as well as torture in Bhutan and anxiety. Specific to resettlement experiences in the United States and Canada, health stressors were associated with depression, and economic stressors with anxiety. Mediating mechanisms accounted for 32% of the relationship between surviving physical threats in Nepal and depression and was statistically significant (p=.048); mediation accounted for 43% of the relationship with anxiety but was not significant (p=.051). See Figure 2 for all significant pathways in the low social support group.
Figure 2.
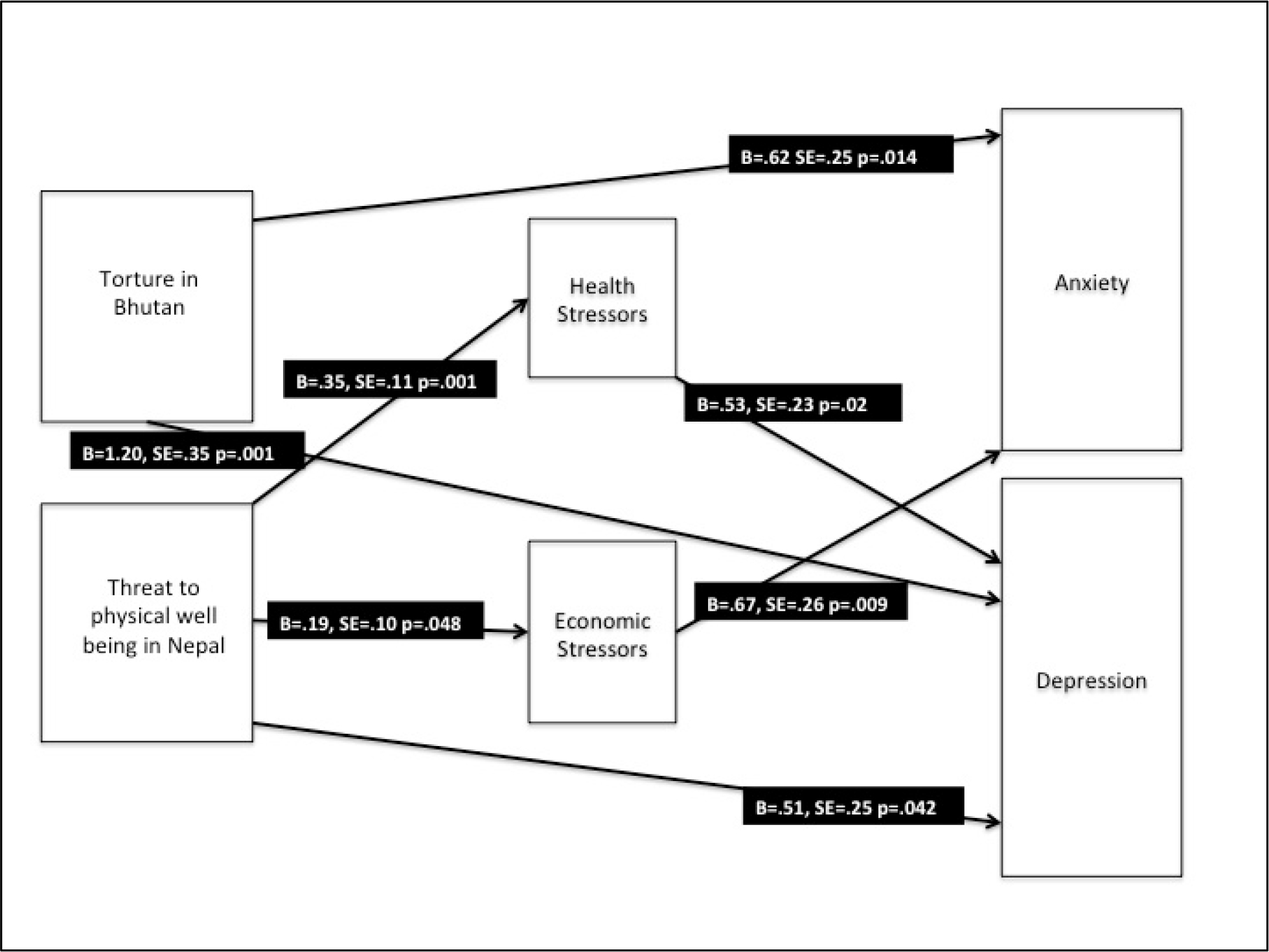
Trauma, resettlement stress, and mental health SEM model among older Bhutanese with low social support (N=62). Results present standardized regression coefficients and bootstrapped standard errors. Model controls for age and gender as exogenous variables.
Among the high social support group, there were significant total effects only between surviving torture in Bhutan and anxiety (β =.67, SE=.32, p=.04). By themselves, neither direct nor indirect pathways between these variables were statistically significant. In addition, neither health nor economic stressors in resettlement were associated with either outcome.
Discussion
Our hypotheses were partially supported. As anticipated, traumatic experiences of torture in Bhutan and other threats to physical well-being in Nepal were associated with depression and anxiety. Our second hypothesis was partially supported, with post-resettlement stressors in the United States and Canada mediating the relationships between surviving physical threats in Nepal and the outcomes. However, there was no statistically significant mediation between the experience of torture in Bhutan and mental health. Our third hypothesis was supported, with social support modifying the relationship between traumas in Bhutan and Nepal, stressors in the United States and Canada, and the outcome.
To date, few studies have focused on quantitatively identifying predictors of mental health among older refugee populations (Virgincar, Doherty & Siriwardhana, 2016). Our study findings are aligned with this small body of research. For instance, studies of older Cambodian and Kurdish refugees in the United States and Somali refugees resettled in Finland have established relationships between exposure to premigration trauma, present resettlement socioeconomic stressors and mental health and general life satisfaction among older refugees (Marshall, Schell & Elliott, et al., 2005; Molsa, Punamaki, Saarni, et al. 2014; Molsa, Kuittinen, Tiilikainen et al., 2017; Cummings, Sull, Davis et al., 2011). Our study adds to this body of research by identifying mediating pathways and chains of risk between past traumas, current stressors, and mental health. Our finding on the relationship between pre-resettlement trauma in Nepal and current economic hardship is particularly noteworthy, as few studies have examined the direct association of pre-resettlement experiences on financial hardships among resettled refugees (Uba & Chung, 1991; O’Donnell et al., 2020).
Specific to resettled Bhutanese, our findings are unique in assessing the long-term mental health consequences of traumas experienced earlier in the refugee life experience. To date, quantitative research on Bhutanese mental health in resettlement has focused primarily on understanding how contemporary resettlement stressors are associated with mental health and suicidal ideation (Lumley, Katsikitis & Statham,2018; Poudel-Tandukar, Jacelon, Bertone-Johnson, et al., 2020; Gautam, Rydberg, Ho, et al., 2021; Aoe et al., 2016), with a few studies looking at the association between the cumulative number of lifetime traumatic events and current psychological distress (see for example Vonnahme, Lankau, Ao, et al., 2015; Adhikari, Daniulaityte & Bhatta, 2021). This is certainly critical information; however, we illustrate the importance of specific past traumas in Bhutan and Nepal in understanding current mental health, both independently and via mediating pathways with post-resettlement stressors. Of particular importance is our focus on the experience of torture in Bhutan and current functioning. Our study is one of the first to document persistence in disparities between the mental health of tortured and non-tortured Bhutanese almost 3 decades after these events occurred.
Other research on older refugees has assessed the moderating role of social support (Lin, Kobayashi, Tong, et al., 2020) on current psychosocial functioning. Specific to resettled Bhutanese, there are established relationships between social support (concrete and emotional) and older refugee mental health. In one study, higher levels of social capital were associated with higher levels of social integration among older resettled Bhutanese in the United States (Lewis, 2020). In other quantitative and qualitative research among resettled Bhutanese of all ages, social support from family and friends plays an important role in protecting against negative mental health (Aoe, Shetty, Sivilli et al., 2016, Chase & Sapkota, 2017, Frounfelker et al, 2020). Our work supports the important role of social support in older Bhutanese wellbeing and more specifically identifies how social support mitigates the impact of pre-resettlement traumas and post-resettlement stressors on current mental health.
Limitations
There are several limitations to this study. First, although we assessed exposure to traumatic events in Bhutan and Nepal that occurred prior to resettlement, this is a cross-sectional study and we cannot make causal inferences. Additionally, participants come from resettled Bhutanese communities in the Northeast United States and Canada, and may not be representative of older Bhutanese living elsewhere in North America or other countries of resettlement. Also of note is that many study participants had pre-existing social relationships with RAs who conducted interviews. This may lead to participants providing responses that were socially desirable. For instance, participants may have been motivated to underreport prior and current psychosocial traumas and stressors and minimize their current psychosocial distress. If this is the case, our results may underestimate the association between prior resettlement traumas, current resettlement stressors, and mental health. Related to this issue, both study RAs were male. This is relevant as female participants may have been hesitant to share their experiences of torture with male interviewers based on gender dynamics in the Bhutanese community. Finally, the majority of study participants are illiterate, and assessments were administered orally by RAs. This may compromise the validity of study data. Unfortunately, the relatively small sample size also prohibits us from more in depth investigation into the relationship between some study variables. For instance, the social support scale does not differentiate between the kinds of social support being offered, and who is providing social support; this is an important avenue for research moving forward.
Implications
Despite these limitations, study findings have implications for health policies and services for older individuals with a refugee life experience. Certainly, our findings reinforce policy recommendations from the World Health Organization that assert creating supportive social environments and promoting opportunities for social connection within refugee communities is important for older refugees as a way to help them engage in meaningful relationships that promote their health (WHO, 2018). Such policy recommendations may seem obvious, but are in reality difficult to implement in countries of resettlement. For instance, specific to Bhutanese, older individuals were able to informally gathered under trees or “chautara” daily and spent hours talking and playing games and cards (bagchal) with each other in refugee camps in Nepal. These opportunities for casual gatherings are typically nonexistent in resettlement in North America and, compounded by language barriers and lack of transportation, lead to isolation and loneliness. There are some initiatives to address this issue, including the development of adult day care facilities, run by ethnic-Nepali community organizations, that provide yoga sessions, social gatherings, and other cultural activities for older residents (see for example Heinonen, 2019). However, government funding is limited in scope. For instance, while the United States Office for Refugee Resettlement has historically had monies designated for services for older adults, there are restrictions based on age (60 and over) and length of time in the United States (up to 5 years) (Office of Refugee Resettlement, 2021a, accessed on-line 7/6/21). Likewise, the government’s Ethnic Community Self-Help program financially supports refugee ethnic community-based organizations, but monies must be used to assist refugees who have arrived in the country within the last 5 years (Office of Refugee Resettlement, 2021b, accessed on-line 7/6/21). These policies and funding restrictions related to age and time in resettlement do not reflect the longer-term health needs of refugee populations and cultural definitions of older age (i.e., less than 60 years of age) that exist not just among older Bhutanese, but other aging populations with a refugee life experience more broadly.
Health care providers can also develop services to address the needs of older individuals with a refugee life experience, which, based on our findings, include addressing the long-term impact of past traumas as well as current resettlement stressors on mental health. In particular, there is great potential to adapt existing evidence-based interventions (EBI) such as cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) for older individuals with a refugee life experience. For instance, the intervention Calmer Life is a person-centered CBT evidence-based program that addresses late-life anxiety and worry, and includes the option for participants to incorporate religion/spirituality in all of the program workshops (Stanley, Wilson, Shrestha, et al., 2018). Another community-based program anchored in evidence-based components is Healthy IDEAS (Identifying Depression, Empowering Activities for Seniors) (Quijano, Stanley, Petersen, et al., 2007). This program consists of four parts: Screening and Assessment, Education, Referral and Linkage to health and mental health professionals, and Behavioral Activation, and is effective in reducing the severity of depression and pain among older adults as well as increasing participants’ understanding about how and where to get help for their symptoms (Quijano et al., 2007).
Such interventions need to undergo modification and adaptation to address the needs of older individuals with a refugee life experience more broadly and be culturally aligned with individual refugee populations (Naeem, Latif, Muktar, et al., 2021; Ramaiya, Fiorillo, Regmi et al., 2017). Adaptions include prioritizing linguistic communication, cultural safety (such as awareness of relevant cultural issues and adjustments in therapeutic techniques) and utilization of an interdisciplinary team to deliver care (Naeem et al., 2021; Nies, Febles, Fanning, Tavernier, 2018). It is important that non-specialists, such as community health workers, who speak the language of those engaged in services and are already trusted members of the community can deliver interventions. These individuals naturally have in depth cultural understanding of the population with whom they are working and can integrate informal care providers such as religious leaders or traditional healers into services and care plans. Mental health programs must also prioritize addressing limited awareness of mental health services and stigma regarding mental health (Atwell, Correa-Velez & Gifford, 2007; Oglak & Hussein, 2016; Karl, Ramos & Kuhn, 2017). Case management, referral and linkage should be elevated and augmented in these interventions as it can help bridge the connection between clients and social, health and mental health services and minimize external factors that contribute to depressive symptoms (Quijano et al., 2007; Gitlin, Harris, McCoy, et al., 2013). More specifically, these may include connections to services for refugees related to employment, housing, citizenship, language skills, and other basic needs. Effective integration and/or adaptation of these factors into existing interventions would again include case managers who speak the same language and come from the same culture.
Study findings also have implications for adaptations of mental health evidence-based interventions for ethnic-Nepali populations more specifically, when understood within the context and framework of Nepali ethnopsychology. Nepali components of the self include the physical body (jiu or saarir), heart-mind (man), and brain-mind (dimaag) (Kohrt, Maharjan, Timsina & Griffith, 2012). The association found in our study between threats to physical health and well-being in Nepal, current physical health stressors, and mental health can be perhaps understood by cultural explanatory models of the relationship between bodily pains and suffering and worries in the heart-mind (man). Addressing problems in the heart-mind (man), associated with traumatic and intrusive memories, worries, and anxiety, may be particularly salient to ethnic-Nepali older individuals and lead to a reduction in suffering related to the physical body (jiu or saarir). Thus, framing CBT interventions as a way to address the connection between heart-mind problems and problems in the physical body may be especially relevant. The differentiation between the heart-mind (man) and brain-mind (dimaag) in Nepali ethnopsychology is also important - the brain-mind (dimaag) monitors cognition and social regulation, and brain-mind problems are highly stigmatized and associated with severe mental illness and psychosis (Kohrt et al., 2012). Specific to an intervention such as CBT, work related to thoughts and appraisals of experiences that tie to symptoms of depression, anxiety, and posttraumatic stress disorder should not just reference brain-mind processes, but also focus on psychoeducation and reduction of stigma related to these issues (Kohrt et al., 2012).
The success of such interventions and their adaptation will hinge on sustainable collaborations between community health agencies and ethnic community-based organizations. It is challenging to find bilingual service providers with advanced training in mental health among many ethnic groups with a refugee life experience. As such, service providers frequently need to pair clinicians with bilingual community members, interpreters, and cultural brokers from refugee communities to deliver care. This requires partnering with ethnic organizations to recruit and train people with a refugee life experience as community health workers. These partnerships can only take place in an environment in which federal, state/provincial, and local health policies incentivize and fund collaborations that promote culturally sensitive mental health care services.
Conclusion
The current psychosocial wellbeing of refugee populations needs to be understood within the context of traumas and stressors experienced prior to third-country resettlement, along with current socioeconomic difficulties they face after life in a refugee camp (Miller and Rasmussen, 2017). The wellbeing of older refugees is, and should be, of growing interest given the size of this subgroup now residing in countries of resettlement. It should also be of growing interest as a human rights issue, in that no segment of the refugee population should be left behind when we consider the future health, both physical and mental, of displaced populations, regardless of age.
Acknowledgments:
The authors would like to thank all staff that assisted in data collection and provided critical contextual knowledge on the lives of Bhutanese with a refugee life experience, in particular Narad Adhikari, Durga Giri, and Brian Khadka. We would also like to thank the generosity of study participants for sharing their life stories. Haami yas anusandhan ma udaar bhayera hamilaii aafna jiwanka kathaharu sunaunubhayeka sahabhagiharulaii pani dhanyabaad din chahanchhaun.
Footnotes
Disclosure of Interest: The authors report no conflict of interest. Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number P30AG024409, the Canadian Institutes of Health Research under a Postdoctoral Training Fellowship Award, and a Fellowship Award from the Research Institute of the McGill University Health Centre. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Canadian Institutes of Health Research, or McGill University.
Contributor Information
Rochelle L. Frounfelker, Division of Social and Transcultural Psychiatry, Department of Psychiatry, McGill University, 4955 Edouard Montpetit Blvd, Apt 12, Montreal, Quebec, Canada.
Tej Mishra, Research Program on Children and Adversity, Boston College School of Social Work, Chestnut Hill, MA, United States.
Alexa Carroll, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, QC.
Robert T. Brennan, Research Program on Children and Adversity, Boston College School of Social Work, Chestnut Hill, MA, United States, Women’s Study Research Center, Brandeis University, Waltham, MA, United States.
Bhuwan Gautam, Bhutanese Society of Western Massachusetts, Inc., Springfield, MA, United States.
Eman Abdullahi Alas Ali, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, QC.
Theresa S. Betancourt, Research Program on Children and Adversity, Boston College School of Social Work, Chestnut Hill, MA, United States.
Data Availability Statement:
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
- Adhikari SB, Daniulaityte R, & Bhatta DN (2021). Demographic and Psychosocial Factors Associated with Suicidal Ideation among Resettled Bhutanese Refugees. Journal of Immigrant and Minority Health, 23(3), 511–518.DOI: 10.1007/s10903-021-01149-z. [DOI] [PubMed] [Google Scholar]
- Ajrouch KJ, Barr R, Daiute C, Huizink AC & Jose PE (2020). A lifespan developmental science perspective on trauma experiences in refugee situations. Advances in Life Course Research, 45, DOI: 10.1016/j.alcr.2020.100342. [DOI] [PubMed] [Google Scholar]
- Anonymous. (2020).
- Aoe T, Shetty S, Sivilli T, Blanton C, Ellis H…..& Cardozo BL (2016). Suicidal ideation and mental health of Bhutanese refugees in the United States. Journal of Immigrant and Minority Health, 18(4), 828–835. DOI: 10.1007/s10903-015-0325-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atwell R, Correa-Velez I, & Gifford S (2007). Ageing out of place: health and well-being needs and access to home and aged care services for recently arrived older refugees in Melbourne, Australia. International Journal of Migration, Health and Social Care, 3(1), 4–14. DOI: 10.1108/17479894200700002. [DOI] [Google Scholar]
- Banki S (2008). Resettlement of the Bhutanese from Nepal: The durable solution discourse. In Adelman H (ed.) Protracted Displacement in Asia: No Place to Call Home. Routledge. Pgs. 29–58. [Google Scholar]
- Bazzi L, & Chemali Z (2016). A Conceptual Framework of Displaced Elderly Syrian Refugees in Lebanon: Challenges and Opportunities. Global journal of health science, 8(11), 54–61. DOI: 10.5539/gjhs.v8n11p54 [DOI] [Google Scholar]
- Ben-Schlomo Y & Kuh D (2002). A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31, 285–293. DOI: 10.1093/ije/31.2.285 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC. (2013). Suicide and suicidal ideation among Bhutanese refugees--United States, 2009–2012. MMWR. Morbidity and mortality weekly report, 62(26), 533. [PMC free article] [PubMed] [Google Scholar]
- Chase L, & Sapkota RP (2017). “In our community, a friend is a psychologist”: An ethnographic study of informal care in two Bhutanese refuge communities. Transcultural Psychiatry, 54(3), 400–422. DOI: 10.1177/1363461517703023 [DOI] [PubMed] [Google Scholar]
- Ciobanu RO, Fokkema T & Nedelcu M (2017). Ageing as a migrant: vulnerabilities, agency and policy implications. Journal of Ethnic and Migration Studies, 43(2), 164–181. DOI: 10.1080/1369183X.2016.1238903. [DOI] [Google Scholar]
- Cummings S, Sull L, Davis C, & Worley N (2011). Correlates of depression among older Kurdish refugees. Social Work, 56(2), 159–168. DOI: 10.1093/sw/56.2.159 [DOI] [PubMed] [Google Scholar]
- Embassy of the United States. (2016). U.S. Ambassador bids farewell to 90,000th refugee to resettle to the United States. Available on-line at: https://nepal.usembassy.gov/pr-2016-09-21.html
- Fazel M, Wheeler J, & Danesh J (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet, 365(9467), 1309–1314. DOI: 10.1016/S0140-6736(05)61027-6 [DOI] [PubMed] [Google Scholar]
- Fazel M, Reed RV, Panter-Brick C & Stein A (2012). Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. The Lancet, 379, 266–282. DOI: 10.1016/S0140-6736(11)60051-2. [DOI] [PubMed] [Google Scholar]
- Frounfelker RL, Mishra T, Dhesi S, Gautaum B, Adhikari N & Betancourt TS (2020). “We are all under the same roof”: Coping and meaning-making among older Bhutanese with a refugee life experience. Social Science and Medicine, 264, 1–9. 10.1016/j.socscimed.2020.113311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautam R, Mawn BE, & Beehler S (2018). Bhutanese older adult refugees recently resettled in the United States: A better life with little sorrows. Journal of Transcultural Nursing, 29(2), 165–171. DOI: 10.1177/1043659617696975. [DOI] [PubMed] [Google Scholar]
- Gautam R, Rydberg J, Ho I, Siwakoti B, Chadbourne W, & Mawn BE (2021). Psychological distress among Bhutanese refugees living in the northeast region of the United States. Journal of Refugee Studies. DOI: 10.1093/jrs/feab025 [DOI] [Google Scholar]
- Gilman SE & Marden JR (2013). Role of the social environmental over the life course in the aetiology of psychiatric disorders. In Koenen KC, Rudenstine S, Susser E, & Galea S (Eds.). A Life Course Approach to Mental Disorders. Oxford University Press. Pgs 215–226. [Google Scholar]
- Giri B (2005). Mourning the 15th anniversary of crisis: The plight of Bhutanese refugee women and children. Journal of Asian and African Studies, 40(5), 345–369. DOI: 10.1177.0021909605057742. [Google Scholar]
- Gitlin LN, Harris LF, McCoy MC, Chernett NL, Pizzi LT, Jutkowitz E, Hess E & Hauck WW (2013). A home-based intervention to reduce depressive symptoms and improve quality of life in older African Americans: A randomized trial. Annals of internal medicine, 159(4), 243–252. DOI: 10.7326/0003-4819-159-4-20130820000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication monographs, 76(4), 408–420. DOI: 10.1080/03637750903310360 [DOI] [Google Scholar]
- Heinonen S (2019). Namaste Adult Day Care provides healthcare for aging southeast Asian population. The Reminder. Available on-line at: https://www.thereminder.com/localnews/west-springfield/namaste-adult-day-care-provides-healthcare-for-agi/
- Hollifield M, Eckert V, Warner TD, Jenkins J, Krakow B, Ruiz J, & Westermeyer J (2005). Development of an inventory for measuring war-related events in refugees. Comprehensive psychiatry, 46(1), 67–80. DOI: 10.1016/j.comppsych.2004.07.003 [DOI] [PubMed] [Google Scholar]
- Hu L & Bentler PM. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. DOI: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hutt M (1996). Ethnic nationalism, refugees and Bhutan. Journal of Refugee Studies, 9(4),397–420. DOI: 10.1093/jrs/9.4.397 [DOI] [Google Scholar]
- Hutt M (2005). The Bhutanese refugees : Between verification, repatriation and royal realpolitik. Peace and Democracy in South Asia, 1(1), 44–56. [Google Scholar]
- Im H, & Neff J (2020). Spiral Loss of Culture: Cultural Trauma and Bereavement of Bhutanese Refugee Elders. Journal of Immigrant & Refugee Studies, 1–15. DOI: 10.1080/15562948.2020.1736362 [DOI] [Google Scholar]
- International Organization for Migration. (2014). Bhutanese refugee number 90,000 resettled from Nepal to Canada. Available on-line at: https://www.iom.int/news/bhutanese-refugee-number-90000-resettled-nepal-canada
- Karl U, Ramos AC & Kuh B (2017). Older migrants in Luxembourg – care preferences for old age between family and professional services. Journal of Ethnic and Migration Studies, 32(2), 270–286. DOI: 10.1080/1369183X.2016.1238909. [DOI] [Google Scholar]
- King R Lulle A, Sampaio D & Vullnetari J (2017). Unpacking the ageing-migration nexus and challenging the vulnerability trope. Journal of Ethnic and Migration Studies, 43(2), 182–198. DOI: 10.1080/1369183X.2016.1238904 [DOI] [Google Scholar]
- Kline RB. (2016). Principles and Practice of Structural Equation Modeling (4th ed.) New York: Guilford Press. [Google Scholar]
- Kuh D, Ben-Schlomo Y, Lynch J, Hallqvist J & Power C (2003). Life course epidemiology. Journal of Epidemiology and Community Health, 57 (10), 778–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Luitel NP, Acharya P, & Jordans MJ (2016). Detection of depression in low resource settings: validation of the Patient Health Questionnaire (PHQ-9) and cultural concepts of distress in Nepal. BMC psychiatry, 16(1). DOI: 10.1186/s12888-016-0768-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Maharjan SM, Timsina D & Griffith JL (2012). Applying Nepaliethnopsychology to psychotherapy for the treatment of mental illness and prevention of suicide among Bhutanese refugees. Annals of Anthropological Practice, 36, 88–112. DOI: 10.1111/j.2153-9588.2012.010194.x [DOI] [Google Scholar]
- Layne CM.; Stuvland R; Saltzman W; Djapo N; Pynoos RS. (1999). Post War Adversities Index. Unpublished manuscript. [Google Scholar]
- Lewis JL (2020). Social Capital Matters for Older Bhutanese Refugees’ Integration. Journal of Immigrant and Minority Health, 22, 1295–1303. DOI: 10.1007/s10903-020-01057-8. [DOI] [PubMed] [Google Scholar]
- Lin S, Kobayashi K, Tong H, Davison KM, Arora SRA & Fuller-Thomson E (2020). Close relations matter: The associations between depression and refugee status in the Canadian Longitudinal Study on Aging (CLSA). Journal of Immigrant and Minority Health, 22, 946–956. DOI: 10.1007/s10903-020-00980-0. [DOI] [PubMed] [Google Scholar]
- Lood Q, Häggblom-Kronlöf G, & Dahlin-Ivanoff S (2015). Health promotion programme design and efficacy in relation to ageing persons with culturally and linguistically diverse backgrounds: a systematic literature review and meta-analysis. BMC health services research, 15:560. DOI 10.1186/s12913-015-1222-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, & Herzberg PY (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical care 46(3), 266–274. Available on-line at: https://www.jstor.org/stable/40221654 [DOI] [PubMed] [Google Scholar]
- Lumley M, Katsikitis M, & Statham D (2018). Depression, anxiety, and acculturative stress among resettled Bhutanese refugees in Australia. Journal of Cross-Cultural Psychology, 49(8), 1269–1282. DOI: 10.1177/0022022118786458 [DOI] [Google Scholar]
- Marfin AA, Moore J, Collins C, Biellik R, Kattel U, Toole MJ & Moore PS (1994). Infectious disease surveillance during emergency relief to Bhutanese refugees in Nepal. Journal of the American Medical Association, 272, 377–381. DOI: 10.1001/jama.1994.03520050057030 [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Elliott MN, Berthold SM, & Chun CA (2005). Mental health of Cambodian refugees 2 decades after resettlement in the United States. Jama, 294(5), 571–579. DOI: 10.1001/jama.294.5.571 [DOI] [PubMed] [Google Scholar]
- Miller KE, & Rasmussen A (2017). The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiology and psychiatric sciences, 26(2), 129–138. DOI: 10.1017/S2045796016000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills E, Singh S, Roach B & Chong S (2008). Prevalence of mental disorders and torture among Bhutanese refugees in Nepal: a systematic review and its policy implications. Medicine, Conflict and Survival, 24(1), 5–15. DOI: 10.1080/13623690701775171. [DOI] [PubMed] [Google Scholar]
- Mölsä M, Punamäki RL, Saarni SI, Tiilikainen M, Kuittinen S, & Honkasalo ML (2014). Mental and somatic health and pre-and post-migration factors among older Somali refugees in Finland. Transcultural psychiatry, 51(4), 499–525. DOI: 10.1177/1363461514526630 [DOI] [PubMed] [Google Scholar]
- Molsa M, Kuittinen S, Tiilikainen M, Konkasalo M-L, Punamaki R-L (2017). Mental health among older refugees: the role of trauma, discrimination, and religiousness. Aging and Mental Health, 21(8), 829–837. DOI: 10.1080/13607863.2016.1165183 [DOI] [PubMed] [Google Scholar]
- Naeem F, Latif M, Mukhtar F, Kim YR, Li W, Butt MG, Kumar N, & Ng R (2021) Transcultural adaptation of cognitive behavioral therapy (CBT) in Asia. Asia-Pacific Psychiatry, 13(1), 12442. DOI: 10.1111/appy.12442 [DOI] [PubMed] [Google Scholar]
- Nies MA, Febles C, Fanning K & Tavernier SS (2018). A conceptual model for home based primary care of older refugees. Journal of Immigrant and Minority Health, 20, 485–491. DOI: 10.1007/s10903-017-0610-8. [DOI] [PubMed] [Google Scholar]
- O’Donnell AW, Stuart J, & O’Donnell K (2020). The long-term financial and psychological resettlement outcomes of pre-migration trauma and post-resettlement difficulties in resettled refugees. Social Science and Medicine, 262, DOI: 10.1016/j.socscimed.2020.113246. [DOI] [PubMed] [Google Scholar]
- Office of Refugee Resettlement. (2021a). Services to older refugees. Accessed on-line at:https://www.acf.hhs.gov/orr/programs/older-refugees
- Office of Refugee Resettlement. (2021b). Ethnic community self-help. Accessed on-line at:https://www.acf.hhs.gov/orr/programs/refugees/ethnic-community-self-help
- Oglak S, & Hussein S (2016). Active Ageing: Social and Cultural Integration of Older Turkish Alevi Refugees in London. Journal of Muslim Minority Affairs, 36(1), 74–87. DOI: 10.1080/13602004.2016.1147152 [DOI] [Google Scholar]
- Poudel-Tandukar K, Jacelon CS, Bertone-Johnson ER, Gautam B, Palmer PH, & Hollon SD (2020). Coping strategies and stress among resettled Bhutanese adults in Massachusetts. American Journal of Orthopsychiatry, 90(4), 502–509. DOI: 10.1037/ort0000453 [DOI] [PubMed] [Google Scholar]
- Quijano LM, Stanley MA, Petersen NJ, Casado BL, Steinberg EH, Cully JA, &Wilson, N. L. (2007). Healthy IDEAS: A depression intervention delivered bycommunity-based case managers serving older adults. Journal of Applied Gerontology, 26(2), 139–156. DOI: 10.1177/0733464807299354 [DOI] [Google Scholar]
- Ramaiya MK, Fiorillo D, Regmi U, Robins CJ, & Kohrt BA (2017). A cultural adaptation of dialectical behavior therapy in Nepal. Cognitive and behavioral practice, 24(4), 428–444. DOI: 10.1016/j.cbpra.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiffers R, Dahal RP, Koirala S, Gerritzen R, Upadhaya N, Luitel NP, ... & Jordans MJ (2013). Psychosocial support for Bhutanese refugees in Nepal. Intervention, 11(2),169–179. DOI: 10.1097/WTF.0b013e32835e368c [DOI] [Google Scholar]
- Riley A, Varner A, Ventevogel P, & Taimur Hasan MM (2017). Daily stressors, trauma exposure, and mental health among stateless Rohingya refugees in Bangladesh. Transcultural Psychiatry, 54(3), 304–331. DOI: 10.1177/1363461517705571 [DOI] [PubMed] [Google Scholar]
- Rizal D (2004). The unknown refugee crisis: Expulsion of the ethnic Lhotsampa from Bhutan. Asian Ethnicity, 5(2), 151–177. DOI: 10.1080/1463136042000221861 [DOI] [Google Scholar]
- Rousseau C, & Frounfelker RL (2019). Mental health needs and services for migrants: an overview for primary care providers. Journal of Travel Medicine, 26(2). DOI: 10.1093/jtm/tay150 [DOI] [PubMed] [Google Scholar]
- Sand G & Gruber S (2018). Differences in subjective well-being between older migrants and natives in Europe. Journal of Immigrant and Minority Health, 20, 83–90. DOI: 10.1007/s10903-016-0537-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS social support survey. Social science & medicine, 32(6), 705–714. DOI: 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Stanley MA, Wilson NL, Shrestha S, Amspoker AB, Wagener P, Bavineau J, Turner M, Fletcher TL, Freshour J, Kraus-Schuman C and Kunik ME, 2018. Community based outreach and treatment for underserved older adults with clinically significant worry: A randomized controlled trial. The American Journal of Geriatric Psychiatry, 26(11), pp.1147–1162 [DOI] [PubMed] [Google Scholar]
- Spallek J, Zeeb H, & Razum O (2011). What do we have to know from migrants’ past exposures to understand their health status? a life course approach. Emerging themes in epidemiology, 8(1), 1–8. DOI: 10.1186/1742-7622-8-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine, 166(10), 1092–1097. DOI: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software: Release 16 [computer program] (2019). College Station, TX:StataCorp LLC: StataCorp. [Google Scholar]
- Steel Z, Silove D, Bird K, McGorry P & Mohan P (1999). Pathways from war trauma to posttraumatic stress symptoms among Tamily asylum seekers, refugees, and immigrants. Journal of Traumatic Stress, 12(3), 421–435. DOI: 10.1023/A:1024710902543 [DOI] [PubMed] [Google Scholar]
- Strong J, Varady C, Chahda N, Doocy S, & Burnham G (2015). Health status and health needs of older refugees from Syria in Lebanon. Conflict and Health, 9, 12. DOI: 10.1186/s13031-014-0029-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapa SB, Van Ommeren M, Sharma B, de Jong JTVM & Hauff E (2003). Psychiatric disability among tortured Bhutanese refugees in Nepal. The American Journal of Psychiatry, 160, 2032–2037. DOI: 10.1176/appi.ajp.160.11.2032 [DOI] [PubMed] [Google Scholar]
- Torr BM & Walsh ET (2018). Does the refugee experience overshadow the effect of SES? An examination of self-reported health among older Vietnamese refugees. Race and Social Problems, 10, 259–271. DOI: 10.1007/s12552-018-9240-6. [DOI] [Google Scholar]
- Uba L & Chung RC (1991). The relationship between trauma and financial and physical well-being among Cambodians in the United States. The Journal of General Psychology, 118(3), 215–225. DOI: 10.1080/00221309/1991.9917782 [DOI] [PubMed] [Google Scholar]
- United Nations High Commissioner for Refugees. (2010). Convention and Protocol Relating to the Status of Refugees. Geneva: UNHCR. Available online at: https://www.unhcr.org/protection/basic/3b66c2aa10/convention-protocol-relating-status-refugees.html [PubMed] [Google Scholar]
- United Nations High Commissioner for Refugees. (2016). UNHCR Age, Gender and Diversity:Accountability Report 2015. Available on-line at: http://www.unhcr.org/en-us/older-people.html
- United Nations High Comissioner for Refugees. (2021). Global trends: Forced displacement in 2020. UNHCR: Denmark. Available on-line at: https://www.unhcr.org/60b638e37/unhcr-global-trends-2020 [Google Scholar]
- United Nations High Commissioner for Refugees Evaluation and Policy Analysis Unit. (2005). Refugee health in Nepal: Joint UNHCR-WHO evaluation of health and health programmes in Bhutanese refugee camps in Nepal. Geneva, Switzerland. Available on-line at: https://www.alnap.org/help-library/refugee-health-in-nepal-joint-unhcr-who-evaluation-of-health-and-health-programmes-in [Google Scholar]
- Van Ommeren M, Sharma B, Thapa S, Makaju R, Prasain D, Bhattarai R, & de Jong J (1999). Preparing instruments for transcultural research: use of the translation monitoring form with Nepali-speaking Bhutanese refugees. Transcultural psychiatry, 36(3), 285–301. DOI: 10.1177/136346159903600304 [DOI] [Google Scholar]
- Van Ommeren M, de Jong JTVM, Sharma B, Komproe I, Thapa SB & Cardena E (2001). Psychiatric disorders among tortured Bhutanese refugees in Nepal. Archives of General Psychiatry, 58(5), 475–482. DOI: 10.1001/archpsyc.58.5.475 [DOI] [PubMed] [Google Scholar]
- Virgincar A, Doherty S, & Siriwardhana C (2016). The impact of forced migration on the mental health of the elderly: A scoping review. International Psychogeriatrics, 28(6),889–896. DOI: 10.1017/S1041610216000193. [DOI] [PubMed] [Google Scholar]
- Vonnahme LA, Lankau EW, Ao T, Shetty S, & Cardozo BL (2015). Factors associated with symptoms of depression among Bhutanese refugees in the United States. Journal of immigrant and minority health, 17(6), 1705–1714. DOI: 10.1007/s10903-014-0120-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2018). Health of older refugees and migrants: Technical guidance.Copenhagen: WHO Regional Office for Europe. Available on-line at: http://www.euro.who.int/en/publications/abstracts/health-of-older-refugees-and-migrants-2018 [Google Scholar]
- Yang FM & Kao ST (2014). Item response theory for measurement validity. Shanghai Archives of Psychiatry, 26(3), 171–177. DOI: 10.3969/j.issn.1002-0829.2014.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.


