Abstract
Purpose
Selective serotonin reuptake inhibitors (SSRIs) are the preferred treatments for depression. The most common adverse drug reactions are symptoms involving the digestive system, leading to low compliance in patients with depression. Therefore, it is important to assess the safety of SSRIs with respect to the digestive system. Several meta-analyses have compared the risks of digestive side effects of SSRIs and other antidepressants. We aimed to compare the risks of various SSRIs (fluoxetine, escitalopram, citalopram, paroxetine, and sertraline) for adverse reactions of the digestive system.
Methods
Systematic searches returned 30 randomized controlled trials (n = 5004) of five antidepressants and placebos.
Results
Fluoxetine had the lowest probability of digestive side effects, ranking fifth at 0.548. Sertraline had the highest probability of digestive side effects, with a probability of 0.611. For gastrointestinal tolerability, escitalopram was better than paroxetine (odds ratio [OR] =0.62, 95% confidence interval [CI] 0.43–0.87) and sertraline (OR=0.56, 95% CI 0.32–0.99).
Conclusion
Fluoxetine exhibited distinct advantages compared to other SSRIs, while sertraline had the greatest likelihood of digestive system side effects. These findings will help doctors understand the relative advantages of various antidepressants.
Keywords: depression, selective serotonin reuptake inhibitors, digestive system side effects, network meta-analysis
Introduction
Depression is the most common psychiatric disorder, and SSRIs are first-line drugs for its treatment.1,2 Among SSRIs, fluoxetine, escitalopram, citalopram, paroxetine, and sertraline are the most prescribed drugs.3 SSRIs act by inhibiting the 5-hydroxytryptamine (5-HT) transporter (5-HTT) on the axonal terminals of serotonergic neurons in the raphe nuclei, which terminates serotonin signaling through rapid presynaptic reuptake.4 Under the action of SSRIs, 5-HT reuptake is inhibited; therefore, the levels of 5-HT in the neurosynaptic junction are increased, leading to the relief of depression symptoms.5 SSRIs are usually taken orally,6 but orally administered drugs often cause gastrointestinal side effects, which may lead to poor patient compliance. Some adverse drug reactions can occur during SSRI treatment, the most common of which are symptoms concerning the digestive system and abdomen, such as nausea and diarrhea, possibly owing to the increase in the usability of 5-HT in the gastrointestinal system. Digestive side effects appear early in the treatment process, which is extremely common during the critical first few weeks of treatment and poses a risk of patient noncompliance.7,8
Some studies have shown that fluoxetine can cause diarrhea and nausea.9,10 However, studies have also shown that fluoxetine can be used to treat constipation.11 Nausea occurred in 42.5% of the escitalopram-treated patients.12 Acute treatment with citalopram also temporarily reduced gastric basal tone and gastric regulation, leading to nausea.13,14 In addition to causing nausea, paroxetine causes constipation by delaying upper gastrointestinal transit.15,16 However, sertraline was related to a significantly lower frequency of constipation and a higher frequency of nausea and diarrhea.13,17 Diarrhea and nausea were the most common adverse associated with vilazodone and venlafaxine.18–20 Although several meta-analyses have compared the risk of digestive side effects between SSRIs and other antidepressants,21–23 there has been no comparative analysis of the risk of digestive side effects of various SSRIs.
Therefore, this study aimed to conduct a network meta-analysis to comparatively analyze the most widely used SSRIs antidepressants (fluoxetine, escitalopram, citalopram, paroxetine, and sertraline) with respect to their incidence of digestive side effects among patients with depression to rank the incidence of SSRI-induced digestive side effects and provide clear evidence for clinicians making the best choices for patients with depression.
Methods
Inclusion Criteria
Participants
We included patients aged more than 18 years, of either sex, and with a preliminary diagnosis of depression according to international diagnostic criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III, (DSM)-IV, International Classification of Diseases (ICD)-10, and Chinese Classification and the Diagnosis Criteria of Mental Disorders (CCMD)-3.
We excluded patients with secondary affective disorders, postpartum depression, postmenopausal depression, atypical depression, dysthymia, and studies involving older patients. We also excluded participants diagnosed with other psychiatric disorders or concomitant medical disorders.
Interventions
The following antidepressants were included: fluoxetine, escitalopram, citalopram, paroxetine, and sertraline. We only included studies in which patients were randomly assigned drugs within the permitted dose range.
Outcomes
The main outcome of this review was the digestive side effects caused by SSRIs in patients with depression. Side effects were assessed by encouraging patients to express both negative and positive effects of the drug. In this study, the digestive side effects included dyspepsia, stomach discomfort, burning sensation, nausea, vomiting, abdominal pain, diarrhea and constipation. We excluded studies in which patients were diagnosed with peptic ulcers, gastropathy, or other relevant comorbidities, as these factors would interfere with the results.
Types of Studies
We included double-blind, randomized controlled trials (RCT) comparing one SSRI with another or placebo as monotherapy in the acute-phase treatment of depression. Although there is no direct relationship between understanding the digestive side effects of placebo and clinical practice, many trials compare SSRIs to placebo, and including them in the network provides important indirect evidence for a more precise evaluation of clinically relevant drugs. Studies on relapses, switching to other drugs, or combination therapy were excluded.
Length of Trial
We considered the number of participants with adverse events in each treatment group at 8 weeks. If the information at 8 weeks was not available, we used the data from 6 to 12 weeks (the time point closest to 8 weeks was preferred).
Comparability of Dosages
We included only study groups in which patients were randomized to drugs within the approved dose. Both fixed-dose and flexible-dose designs were permitted.
Search Strategy
The entire EMBASE, PubMed, CNKI, ProQuest, ScienceDirect, Cochrane Central, Web of Science, Clinicalkey databases were searched from 1980 to January 1, 2020, to identify studies on the acceptability of five drugs for depression treatment. We used the search terms “depression” or “RCT” combined with a list of all included antidepressants without language restrictions.
The article screening process included: (1) conducting preliminary screening based on subjects and abstracts to select RCTs and reviews that may be related to the subject; (2) using the references of articles screened out by preliminary screening to identify articles missed in the computer database search. Two researchers independently searched for and screened the articles. Any differences were resolved through discussions with a third member of the review team.
Data Extraction
The following basic information was extracted from the included studies: first author, publication year and country, diagnostic criteria, primary outcomes, length of RCT, intervention drug, control drug, and sample size of the intervention and control groups.
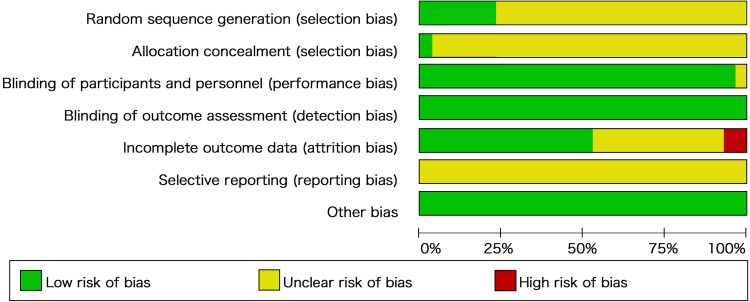
Quality Assessment
We assessed the risk of bias in the included studies using the tool described in the Cochrane Collaboration Handbook as a reference guide. Graphic representations of potential biases within and between studies were generated using RevMan V.5.3. Two researchers independently assessed the risk of bias in the included studies. Any disagreements were resolved through discussions with a third member of the review panel.
Statistical Analysis
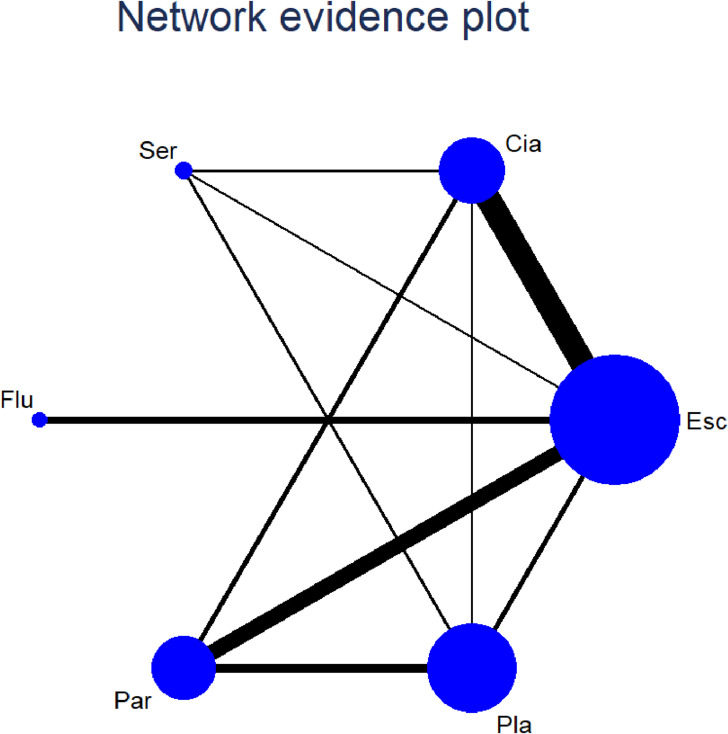
We plotted a network diagram to present the available evidence graphically. The width of the lines was proportional to the number of trials that compared each pair of treatments. The size of each circle is proportional to the number of randomly assigned participants. We used R software for the network meta-analysis. The model calculations based on Bayesian theory adopt Markov chain Monte Carlo, with n. adapt = 10000 and n. iter = 50000. Convergence was checked by running multiple chains and monitoring their mixing using the Brooks-Gelman-Rubin diagnostic. We also used the model to draw forest plots and ordination maps and to perform tests for consistency and heterogeneity. We used a random-effects meta-analysis model to synthesize data for each pairwise comparison in the dataset to obtain ORs with 95% confidence intervals. Consistency in network meta-analysis refers to the similarity between the direct and indirect comparison results. The node-splitting method was used to evaluate the consistency assumption. We calculated the p-value, which measures consistency, by calculating the probability of observing the outcomes from the data sample, assuming that the null hypothesis is true. The smaller the p-value, the greater the inconsistency. p<0.05 indicated that the direct and indirect evidence in the network are significantly inconsistent. Heterogeneity was evaluated using Cochran’s Q-statistic and quantified using the I2 statistic. Cochran’s I2 value above 50% indicated very high heterogeneity. Publication bias was assessed using comparison-adjusted funnel plots. The horizontal axis of the graph represents the difference between the effect of one paired comparison in a study and the comprehensive effect of multiple similar comparisons, whereas the vertical axis usually represents the standard error of the effect size. If there were no small-sample effects, the funnel plots adjusted for comparison were symmetrical about the zero line.
Results
Study Selection
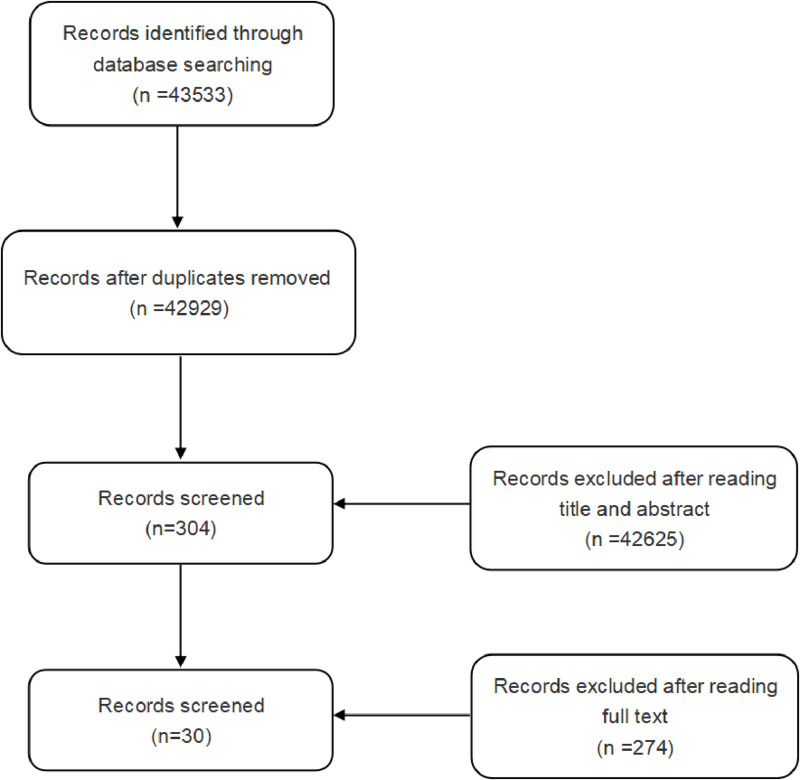
We searched the databases according to the search strategy and initially obtained 43533 potentially eligible trials. After screening titles and abstracts, 42625 studies were excluded. Among the remaining 304 full-text studies, 274 were excluded because of a lack of valuable results. In total, 30 articles were eventually included in this study to evaluate the digestive system safety of SSRIs.24–53 A flowchart of the study selection process is shown in Figure 1.
Figure 1.
Flow diagram of search.
Study Characteristics and Risk of Bias Within Studies
A total of 30 studies were included in this review (Table 1 shows basic information in the literature). A total of 5004 patients with depression were randomly assigned to receive one of five effective drugs or a placebo. Of these, 1782 received escitalopram, 854 received citalopram, 189 received fluoxetine, 651 received paroxetine, 218 received sertraline, and 56.7% of the patients were from China. The mean study sample size was 167 patients. The risk of bias plots and summaries are shown in Figure 2. Figure 3 shows all available evidence for the meta-analysis of the digestive side effects of SSRIs.
Table 1.
Characteristic of Included Studies
| Study | Year | Length of RCT | Age | Diagnostic criteria | Recruitment | Intervention | Sample Size | Response |
|---|---|---|---|---|---|---|---|---|
| Yevtushenko VY24 | 2007 | 6 | 25--45 | DSM-IV | Russia | Esc/Cia | 108/108 | 2/8 |
| Wade A25 | 2002 | 8 | 18--65 | DSM-IV | NA | Esc/Pla | 191/189 | 17/7 |
| Moore N26 | 2005 | 8 | 18--65 | DSM IV | France | Esc/Cia | 142/152 | 6/11 |
| Valle-Cabrera R27 | 2018 | 10 | 18--65 | DSM-IV | Cuban | Ser/Pla | 39/38 | 27/12 |
| Mao PX28 | 2008 | 8 | 18--65 | DSM-IV | China | Esc/Flu | 123/117 | 15/16 |
| Dunbar GC29 | 1993 | 6 | 18--65 | DSM-III | US | Par/Pla | 167/169 | 93/35 |
| Wang YJ39 | 2016 | 6 | 20--65 | CCMD-3 | China | Esc/Cia | 48/48 | 3/3 |
| Zhu YH41 | 2015 | 8 | 19--64 | ICD-10 | China | Par/Esc | 23/23 | 4/1 |
| Liu R42 | 2013 | 6 | 18--60 | CCMD-3 | China | Esc/Cia | 40/40 | 3/6 |
| Xu Y43 | 2011 | 6 | 18--60 | CCMD-3 | China | Esc/Cia | 35/35 | 9/7 |
| Wang XF44 | 2010 | 6 | 18--55 | CCMD-3 | China | Esc/Flu | 36/34 | 5/5 |
| Zhang XX45 | 2010 | 6 | 18--62 | CCMD-3 | China | Esc/Ser | 35/35 | 9/9 |
| Hu MR46 | 2010 | 6 | 18--60 | CCMD-3 | China | Esc/Cia | 25/23 | 3/5 |
| Xun GL47 | 2009 | 6 | 18--65 | CCMD-3 | China | Esc/Cia | 115/117 | 26/26 |
| Liu XB48 | 2009 | 6 | 18--65 | CCMD-3 | China | Esc/Par | 37/36 | 10/16 |
| Xu FL52 | 2009 | 6 | 18--60 | CCMD-3 | China | Esc/Flu | 39/38 | 12/8 |
| Yang R49 | 2008 | 6 | 24--61 | CCMD-3 | China | Par/Cia | 27/29 | 4/1 |
| Hsu JW30 | 2011 | 6 | 20--65 | DSM-IV | China | Ser/Cia | 26/25 | 7/5 |
| Ou JJ31 | 2011 | 6 | 18--65 | DSM-IV | China | Esc/Cia | 115/117 | 22/25 |
| Woo YS32 | 2017 | 6 | 18--65 | DSM-IV | Korean | Par/Esc | 150/148 | 44/40 |
| Detke MJ33 | 2004 | 8 | ≥18 | DSM-IV | USA | Par/Pla | 86/93 | 16/6 |
| Perahia DG34 | 2006 | 8 | ≥18 | DSM-IV | NA | Par/Pla | 97/99 | 10/6 |
| Jin XS50 | 2015 | 12 | ≥18 | CCMD-3 | China | Par/Esc | 34/37 | 8/12 |
| Croft H35 | 1999 | 8 | ≥18 | DSM-IV | US | Ser/Pla | 118/119 | 68/25 |
| Rickels K36 | 1989 | 6 | ≥18 | DSM-III | NA | Par/Pla | 55/56 | 29/8 |
| Goldstein DJ37 | 2004 | 8 | ≥18 | DSM-IV | US | Par/Pla | 87/89 | 26/5 |
| Lepola UM38 | 2003 | 8 | 18--65 | DSM-IV | Denmark | Esc/Cia/Pla | 155/160/154 | 37/35/19 |
| Zhou ZX40 | 2018 | 12 | ≥18 | CCMD-3 | China | Par/Esc | 28/28 | 8/3 |
| Cen LP53 | 2009 | 6 | 18--62 | CCMD-3 | China | Par/Esc | 28/28 | 9/7 |
| Nierenberg AA51 | 2007 | 8 | ≥18 | DSM-IV | NA | Esc/Pla | 274/137 | 88/32 |
Abbreviations: CCMD, Chinese Classification and the Diagnose Criterion of Mental Disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; RCT, random controlled trial; Esc, escitalopram; Cia, citalopram; Flu, fluoxetine; Par, paroxetine; Pla, placebo; Ser, sertraline; US, the United States; NA, not available.
Figure 2.
Risk of bias.
Figure 3.
Network of evidence.
Notes: Width of the lines was proportional to the number of trials comparing every pair of treatments. Size of every circle was proportional to the number of randomly assigned participants.
Abbreviations: Cia, citalopram; Esc, escitalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
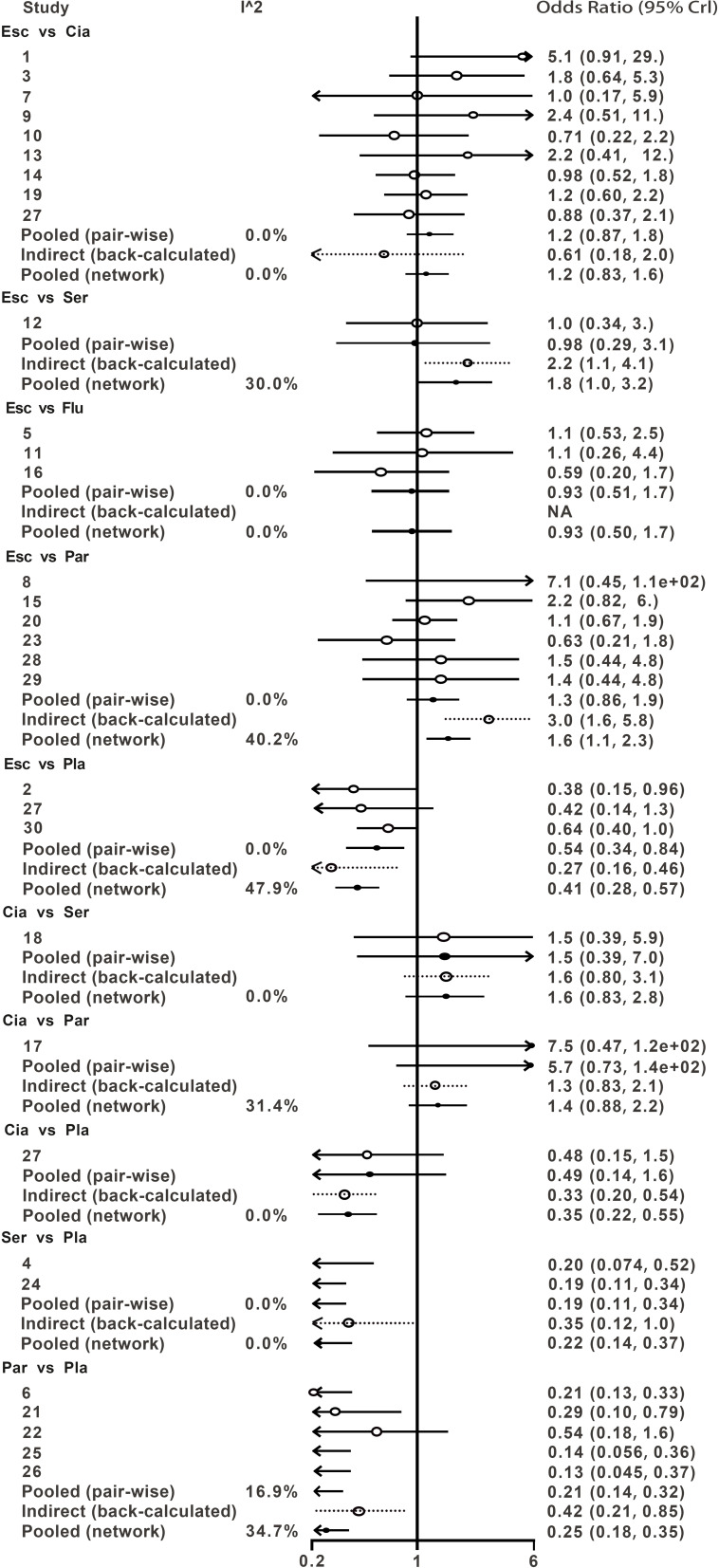
Network Meta-Analysis
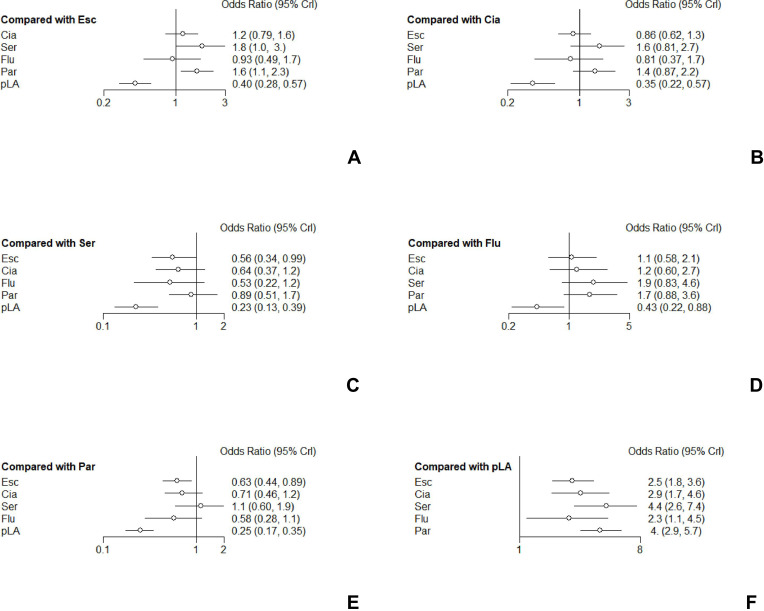
As shown in Table 2, the incidence of digestive side effects was significantly higher for the five drugs than for the placebo. Escitalopram (OR 2.5, 95% CI 1.8–3.5); citalopram (OR 2.9, 95% CI 1.9–4.5); sertraline (OR 4.4, 95% CI 2.6–7.3); fluoxetine (OR 2.3, 95% CI 1.1–4.6); paroxetine (OR 4.0, 95% CI 2.9–5.7). Escitalopram had a significantly lower incidence of digestive side effects than paroxetine (OR=0.62, 95% CI 0.43-0.87). Escitalopram also had a significantly lower incidence of digestive side effects than sertraline (OR=0.56, 95% CI 0.32-0.99). The other comparisons were not statistically significant. A forest plot of the network results is shown in Figure 4.
Table 2.
Results of SSRIs for the Incidence of Induced-Digestive System Side-Effects from Network Meta-Analysis
| Esc | |||||
| 0.86 (0.61, 1.19) | Cia | ||||
| 0.56 (0.32, 0.99) | 0.66 (0.36, 1.21) | Ser | |||
| 1.07 (0.58, 2.04) | 1.24 (0.63, 2.61) | 1.9 (0.82, 4.47) | Flu | ||
| 0.62 (0.43, 0.87) | 0.72 (0.45, 1.14) | 1.1 (0.61, 1.97) | 0.58 (0.28, 1.15) | Par | |
| 2.47 (1.75, 3.51) | 2.87 (1.85, 4.5) | 4.39 (2.64, 7.31) | 2.31 (1.12, 4.61) | 3.97 (2.85, 5.68) | Pla |
Note: Bold values indicate P<0.05, data presented as OR (95% CI).
Abbreviations: Esc, escitalopram; Cia, citalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
Figure 4.
Forest plots of network meta-analysis of all trials for acceptability. (A) Forest plots for the outcomes compared with Escitalopram. (B) Forest plots for the outcomes compared with Citalopram. (C) Forest plots for the outcomes compared with Sertraline. (D) Forest plots for the outcomes compared with Fluoxetine. (E) Forest plots for the outcomes compared with Paroxetine. (F) Forest plots for the outcomes compared with Placebo.
Abbreviations: Cia, citalopram; CrI, confidence intervals; Esc, escitalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
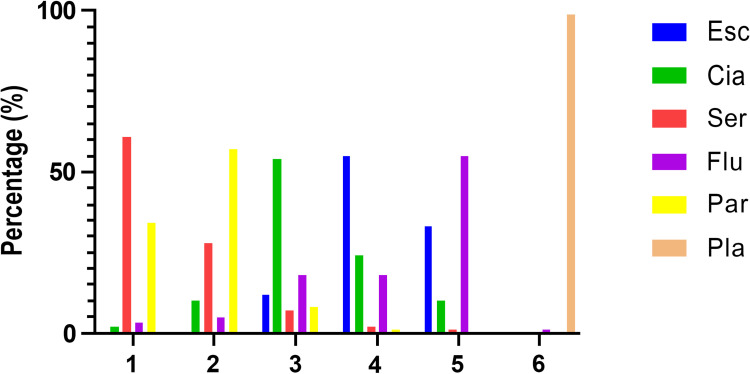
We ranked the probabilities of digestive side effects caused by the five drugs, in Table 3 and Figure 5. The drugs were ranked according to the number of digestive side effects from highest to lowest; the smaller the number, the higher the drug’s safety. The probability of digestive side effects with fluoxetine was the lowest (0.547), ranking fifth. Escitalopram had a probability of 0.548, ranking fourth. Sertraline and paroxetine are most likely to cause digestive side effects. Sertraline ranked first, with a probability of 0.611, and paroxetine ranked second, with a probability of 0.566.
Table 3.
Rank Probability of Caused Digestive System Side Effects Among SSRIs
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Esc | 0.0005 | 0.00375 | 0.1189 | 0.54815 | 0.32915 | 0 |
| Cia | 0.0209 | 0.0962 | 0.54315 | 0.24135 | 0.0984 | 0 |
| Ser | 0.61095 | 0.282 | 0.07395 | 0.0219 | 0.0112 | 0 |
| Flu | 0.02965 | 0.05195 | 0.18205 | 0.17665 | 0.54715 | 0.01255 |
| Par | 0.33845 | 0.5661 | 0.08195 | 0.0119 | 0.0016 | 0 |
| Pla | 0 | 0 | 0 | 0.0005 | 0.0125 | 0.98745 |
Abbreviations: Esc, escitalopram; Cia, citalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo; Rank probability, preferred direction=1.
Figure 5.
Rank probability of caused digestive system side effects among SSRIs.
Abbreviations: Cia, citalopram; Esc, escitalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
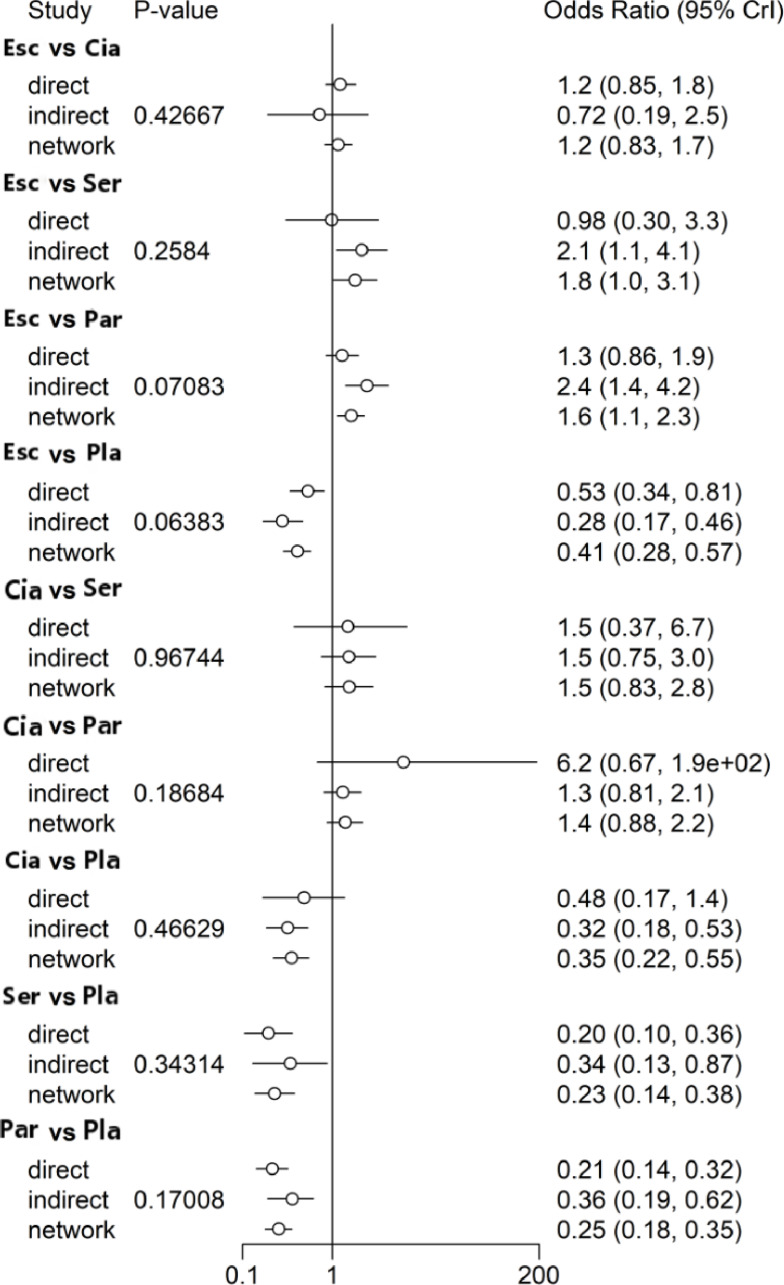
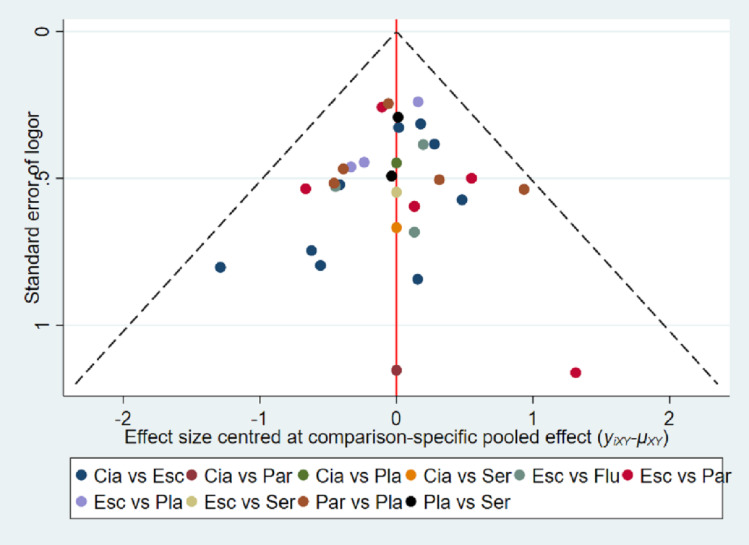
Heterogeneity, Consistency, and Publication Bias
Heterogeneity was assessed using the I2 test, with an I2 >50% indicating the presence of heterogeneity (Figure 6); there was no significant heterogeneity among the included studies. The consistency of direct and indirect evidence was assessed using the node-splitting method. A forest plot is shown in Figure 7. No significant differences were observed in this study. We used a comparison-adjusted funnel plot to assess publication bias and small-sample effects. The horizontal axis of the graph represents the difference between the effect of one paired comparison in a study and the combined effect of many similar comparisons, whereas the vertical axis usually represents the standard error of the effect size. If there is no small-sample effect or publication bias, the funnel plot adjusted by comparison will be symmetrical around the zero line. A funnel plot is shown in Figure 8. It can be seen from the figure that the funnel chart is roughly symmetrical. There was no significant publication bias, and a small-sample effect was found.
Figure 6.
The heterogeneity of the included studies.
Abbreviations: Cia, citalopram; Esc, escitalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
Figure 7.
Summarized results of direct and indirect comparisons between different SSRI.
Abbreviations: Cia, citalopram; Esc, escitalopram; Flu, fluoxetine; Ser, sertraline; Par, paroxetine; Pla, placebo.
Figure 8.
Comparison-adjusted funnel plots.
Notes: The red line suggests the null hypothesis that the study-specific effect sizes do not differ from the respective comparison-specific pooled effect estimates. Different colors represent different comparisons.
Discussion
This study found that fluoxetine had a lower risk of digestive side effects than other SSRIs. Patients treated with sertraline are at a high risk of digestive side effects such as nausea and diarrhea. These results may help inform patients, doctors, and policymakers about the relative advantages of different SSRIs for depression.
Fluoxetine is a classical antidepressant that inhibits brain-derived neurotrophic factor (BDNF) precursor protein (proBDNF)/pan neurotrophin receptor 75 (p75NTR) signaling in monocytes/macrophages in the intestine.54 ProBDNF is an intermediate in the synthesis of mature BDNF, which is involved in the development of depression.54,55 Studies have shown that direct intracerebral injection of pro-BDNF can induce depression-like behavior in rodents. Notably, depressive symptoms were relieved by injecting antibodies against pro-BDNF into the brain or periphery.56 ProBDNF combines with p75NTR to regulate the inflammatory response, affects the function of smooth muscle and nerves, and leads to gastrointestinal dysfunction, such as constipation.54 A study showed that upregulation of proBDNF/p75NTR in peripheral blood mononuclear cells of patients with depression was positively correlated with gastrointestinal diseases.54
The most obvious digestive side effects of sertraline are nausea and diarrhea.27,35 Sertraline is the most potent antidepressant against dopamine transporter (DAT). DAT regulates the concentration of dopamine (DA) in the synaptic cleft by rapidly clearing the neurotransmitters released from the extracellular space. Evidence suggests that DAT exists in the endocrine cells of the gut that produce DA.57 DA promotes diarrhea by triggering inflammatory responses via DA receptors on immune cells in the colon. In vitro studies have demonstrated that sertraline is 2 to 10 times stronger than other antidepressants in inhibiting serotonin reuptake. Sertraline inhibits the 5-HTT.58 5-HTT absorbs 5-HT through the dissipation of the Na+ gradient established by the electrogenic pump Na/K ATPase.59 Sertraline inhibits various Na+ channels.60 A study showed that sertraline has a concentration-dependent inhibitory effect on intracellular Na+ channels in mice.61 Sertraline may inhibit 5-HTT by inhibiting Na+ channels, increasing the extracellular 5-HT levels. Elevated 5-HT levels and decreased 5-HTT levels in the gut are considered the basis of gastrointestinal disturbances such as diarrhea and inflammation. For example, the deletion of 5-HTT in mice results in increased fecal water content (suggesting a diarrheal phenotype).62 In addition, 5-HT can induce nausea by stimulating 5-HT3 receptors on vagal afferent nerves. Activation of the 5-HT3 receptor induces rapid excitatory postsynaptic potentials and rapid depolarization of serotonergic neurons, leading to an increase in the intracellular Ca2+ concentration that causes the release of different emetic neurotransmitters.63 This results in a high risk of digestive side effects of sertraline.
In this study, we also found that citalopram was more likely to cause digestive side effects than escitalopram. Escitalopram significantly increased serum levels of the anti-inflammatory cytokine interleukin-10 (IL-10).64 IL-10 is one of the most important anti-inflammatory cytokines affecting intestinal mucosal immune response.65 Administration of IL-10 can prevent the worsening of inflammation and, therefore, disease development.65 However, citalopram did not affect changes in serum levels of IL-10, and the anti-inflammatory effect of citalopram was inferior to that of escitalopram.64 Citalopram showed weaker blocks of the norepinephrine transporter than paroxetine in vitro.66 High norepinephrine levels may lead to gastric motility disorders.67 This might explain why paroxetine is more likely to cause gastrointestinal side effects than citalopram.
Inclusion criteria were strictly limited in this study to ensure transferability between comparisons. Consistency was the primary method for determining the accuracy and reliability of the network meta-analysis. In network meta-analysis, consistency refers to the similarity between the results of direct and indirect comparisons. This study did not found that the results of direct and indirect comparisons were inconsistent. In general, this network meta-analysis has good consistency and reliable results.
Our study had some limitations. The first major limitation is that more than 50% of the included studies were from China, and the number of included trials was relatively small. Second, fluvoxamine was not included in this study because we did not find any articles on the digestive side effects of fluvoxamine compared with other SSRI drugs during the literature search. Third, in accordance with our protocol, we excluded participants with depression and anxiety. This exclusion is intended to maintain network transmissibility. However, it might have limited the universality of the results of this study, as such patients account for a significant proportion of patients in real clinical settings. Finally, we did not perform a specific classification of digestive side effects such as nausea and vomiting. Although specific digestive symptoms were mentioned in the included RCTs, the number of subjects with specific digestive symptoms included in the studies meeting the inclusion criteria was too small to constitute a network meta-analysis of specific digestive symptoms; studies with a small number of subjects can cause publication bias and generate a relatively large side effect. Therefore, we suggest that more subjects be included in future studies, and the incidence of specific digestive side effects caused by SSRIs should be ranked to provide better clinical treatment suggestions and guidance for patients with depression.
Conclusion
In summary, regarding digestive system safety, fluoxetine exhibited the least probability of inducing digestive side effects when used in patients with depression, whereas sertraline exhibited the highest probability of inducing digestive side effects among patients with depression. Therefore, clinicians must choose the best drug according to the specific situation of the patient. Our findings may provide a useful perspective for making these decisions. Future studies should include more studies and include participants with depression accompanied by anxiety to confirm these conclusions.
Acknowledgments
This study was supported by grant 2017E0267 from the Technology Support Project of Xinjiang, grants 2018D01C228 and 2018D01C239 from the Natural Science Foundation of Xinjiang Uyghur Autonomous Region, grant 2017Q007 from the Tianshan Youth Project–Outstanding Youth Science and Technology Talents of Xinjiang, grant 7152074 from the Beijing Natural Science Foundation, grant 2017KY720 from the Projects of Medical and Health Technology Program in Zhejiang Province, and the Opening Project of Zhejiang Provincial Top Key Discipline of Pharmaceutical Sciences.
Abbreviations
SSRIs, Selective serotonin reuptake inhibitors; OR, odds ratio; CI, confidence interval; 5-HT, 5-hydroxytryptamine; 5-HTT, 5-hydroxytryptamine transporter; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; CCMD, Chinese Classification and the Diagnosis Criteria of Mental Disorders; RCT, randomized controlled trials; BDNF, brain-derived neurotrophic factor; proBDNF, brain-derived neurotrophic factor precursor protein; p75NTR, pan neurotrophin receptor 75; DAT, dopamine transporter; DA, dopamine; IL-10, interleukin-10.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Vadodaria KC, Ji Y, Skime M., et al. Serotonin-induced hyperactivity in SSRI-resistant major depressive disorder patient-derived neurons. Mol Psychiatry. 2019;24(6):795–807. doi: 10.1038/s41380-019-0363-y [DOI] [PubMed] [Google Scholar]
- 2.Fischer Fumeaux CJ, Morisod Harari M, Weisskopf E, et al. Risk-benefit balance assessment of SSRI antidepressant use during pregnancy and lactation based on best available evidence - an update. Expert Opin Drug Saf. 2019;18(10):949–963. doi: 10.1080/14740338.2019.1658740 [DOI] [PubMed] [Google Scholar]
- 3.Furukawa TA, Cipriani A, Cowen PJ, Leucht S, Egger M, Salanti G. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601–609. doi: 10.1016/S2215-0366(19)30217-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plenge P, Abramyan AM, Sørensen G, et al. The mechanism of a high-affinity allosteric inhibitor of the serotonin transporter. Nat Commun. 2020;11(1):1491. doi: 10.1038/s41467-020-15292-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yaman B, Bal R. Pindolol potentiates the antidepressant effect of venlafaxine by inhibiting 5-HT1A receptor in DRN neurons of mice. Int J Neurosci. 2022;132(1):23–30. doi: 10.1080/00207454.2020.1797723 [DOI] [PubMed] [Google Scholar]
- 6.Cussotto S, Strain CR, Fouhy F, et al. Differential effects of psychotropic drugs on microbiome composition and gastrointestinal function. Psychopharmacology. 2019;236(5):1671–1685. doi: 10.1007/s00213-018-5006-5 [DOI] [PubMed] [Google Scholar]
- 7.Golden RN. Making advances where it matters: improving outcomes in mood and anxiety disorders. CNS Spectr. 2004;9(6 Suppl 4):14–22. doi: 10.1017/S1092852900025463 [DOI] [PubMed] [Google Scholar]
- 8.Kostev K, Rex J, Eith T, Heilmaier C. Which adverse effects influence the dropout rate in selective serotonin reuptake inhibitor (SSRI) treatment? Results for 50,824 patients. German Med Sci. 2014;12:Doc15. doi: 10.3205/000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou C, Ding X, Flaherty JH, Dong B. Clinical efficacy and safety of fluoxetine in generalized anxiety disorder in Chinese patients. Neuropsychiatr Dis Treat. 2013;9:1661–1670. doi: 10.2147/NDT.S38899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11(11):Cd012436. doi: 10.1002/14651858.CD012436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talley NJ. How effective is fluoxetine for the treatment of pain and constipation-predominant irritable bowel syndrome? Nat Clin Pract Gastroenterol Hepatol. 2006;3(4):196–197. doi: 10.1038/ncpgasthep0444 [DOI] [PubMed] [Google Scholar]
- 12.Yrondi A, Fiori LM, Frey BN, et al. Association between side effects and blood microrna expression levels and their targeted pathways in patients with major depressive disorder treated by a selective serotonin reuptake inhibitor, escitalopram: a CAN-BIND-1 report. int j neuropsychopharmacol. 2020;23(2):88–95. doi: 10.1093/ijnp/pyz066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janssen P, Van Oudenhove L, Casteels C, Vos R, Verbeke K, Tack J. The effects of acute citalopram dosing on gastric motor function and nutrient tolerance in healthy volunteers. Aliment Pharmacol Ther. 2011;33(3):395–402. doi: 10.1111/j.1365-2036.2010.04522.x [DOI] [PubMed] [Google Scholar]
- 14.Kocabay G, Yildiz M, Eksi Duran N, Ozkan M. Sinus arrest due to sertraline. Clin Cardiol. 2010;33(6):E114–115. doi: 10.1002/clc.20647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afzal A, Ajmal K, Shakir S, Khan BT, Ara I. Paroxetine: an update of response on intestinal motility. J Pak Med Assoc. 2016;66(3):240–242. [PubMed] [Google Scholar]
- 16.Coates MD, Johnson AC, Greenwood-Van Meerveld B, Mawe GM. Effects of serotonin transporter inhibition on gastrointestinal motility and colonic sensitivity in the mouse. Neurogastroenterol Motility. 2006;18(6):464–471. doi: 10.1111/j.1365-2982.2006.00792.x [DOI] [PubMed] [Google Scholar]
- 17.Cohn CK, Shrivastava R, Mendels J, et al. Double-blind, multicenter comparison of sertraline and amitriptyline in elderly depressed patients. J Clin Psychiatry. 1990;51:28–33. [PubMed] [Google Scholar]
- 18.Mathews M, Gommoll C, Chen D, Nunez R, Khan A. Efficacy and safety of vilazodone 20 and 40 mg in major depressive disorder: a randomized, double-blind, placebo-controlled trial. Int Clin Psychopharmacol. 2015;30(2):67–74. doi: 10.1097/YIC.0000000000000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gartlehner G, Hansen RA, Morgan LC, et al. AHRQ Comparative Effectiveness Reviews. Second-Generation Antidepressants in the Pharmacologic Treatment of Adult Depression: An Update of the 2007 Comparative Effectiveness Review. Rockville (MD): Agency for Healthcare Research and Quality (US); 2011. [PubMed] [Google Scholar]
- 20.Kadam RL, Sontakke SD, Tiple P, Motghare VM, Bajait CS, Kalikar MV. Comparative evaluation of efficacy and tolerability of vilazodone, escitalopram, and amitriptyline in patients of major depressive disorder: a randomized, parallel, open-label clinical study. Indian J Pharmacol. 2020;52(2):79–85. doi: 10.4103/ijp.IJP_441_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oliva V, Lippi M, Paci R, et al. Gastrointestinal side effects associated with antidepressant treatments in patients with major depressive disorder: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110266. doi: 10.1016/j.pnpbp.2021.110266 [DOI] [PubMed] [Google Scholar]
- 22.Solmi M, Fornaro M, Ostinelli EG, et al. Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects. World Psychiatry. 2020;19(2):214–232. doi: 10.1002/wps.20765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo S, Yang Y, Pei XJ, Liu FY. Comparative risk of Selective Serotonin Reuptake Inhibitors (SSRIs)-induced nausea among Chinese senile depression patients: a network meta-analysis of randomized-controlled trials. Medicine. 2020;99(7):e19133. doi: 10.1097/MD.0000000000019133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yevtushenko VY, Belous AI, Yevtushenko YG, Gusinin SE, Buzik OJ, Agibalova TV. Efficacy and tolerability of escitalopram versus citalopram in major depressive disorder: a 6-week, multicenter, prospective, randomized, double-blind, active-controlled study in adult outpatients. Clin Ther. 2007;29(11):2319–2332. doi: 10.1016/j.clinthera.2007.11.014 [DOI] [PubMed] [Google Scholar]
- 25.Wade A, Michael Lemming O, Bang Hedegaard K. Escitalopram 10 mg/day is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol. 2002;17(3):95–102. doi: 10.1097/00004850-200205000-00001 [DOI] [PubMed] [Google Scholar]
- 26.Moore N, Verdoux H, Fantino B. Prospective, multicentre, randomized, double-blind study of the efficacy of escitalopram versus citalopram in outpatient treatment of major depressive disorder. Int Clin Psychopharmacol. 2005;20(3):131–137. doi: 10.1097/00004850-200505000-00002 [DOI] [PubMed] [Google Scholar]
- 27.Valle-Cabrera R, Mendoza-Rodríguez Y, Robaina-García M, et al. Efficacy of sertraline in patients with major depressive disorder naive to selective serotonin reuptake inhibitors: a 10-week randomized, Multicenter, Placebo-Controlled, Double-Blind, Academic Clinical Trial. J Clin Psychopharmacol. 2018;38(5):454–459. doi: 10.1097/JCP.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 28.Mao PX, Tang YL, Jiang F, et al. Escitalopram in major depressive disorder: a multicenter, randomized, double-blind, fixed-dose, parallel trial in a Chinese population. Depress Anxiety. 2008;25(1):46–54. doi: 10.1002/da.20222 [DOI] [PubMed] [Google Scholar]
- 29.Dunbar GC, Claghorn JL, Kiev A, Rickels K, Smith WT. A comparison of paroxetine and placebo in depressed outpatients. Acta Psychiatr Scand. 1993;87(5):302–305. doi: 10.1111/j.1600-0447.1993.tb03376.x [DOI] [PubMed] [Google Scholar]
- 30.Hsu JW, Su TP, Huang CY, Chen YS, Chou YH. Faster onset of antidepressant effects of citalopram compared with sertraline in drug-naïve first-episode major depressive disorder in a Chinese population: a 6-week double-blind, randomized comparative study. J Clin Psychopharmacol. 2011;31(5):577–581. doi: 10.1097/JCP.0b013e31822c091a [DOI] [PubMed] [Google Scholar]
- 31.Ou JJ, Xun GL, Wu RR, et al. Efficacy and safety of escitalopram versus citalopram in major depressive disorder: a 6-week, multicenter, randomized, double-blind, flexible-dose study. Psychopharmacology. 2011;213(2–3):639–646. doi: 10.1007/s00213-010-1822-y [DOI] [PubMed] [Google Scholar]
- 32.Woo YS, McIntyre RS, Kim JB, et al. Paroxetine versus venlafaxine and escitalopram in Korean patients with major depressive disorder: a randomized, rater-blinded, six-week study. Clin Psychopharmacol Neurosci. 2017;15(4):391–401. doi: 10.9758/cpn.2017.15.4.391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Detke MJ, Wiltse CG, Mallinckrodt CH, McNamara RK, Demitrack MA, Bitter I. Duloxetine in the acute and long-term treatment of major depressive disorder: a placebo- and paroxetine-controlled trial. Eur neuropsychopharmacol. 2004;14(6):457–470. doi: 10.1016/j.euroneuro.2004.01.002 [DOI] [PubMed] [Google Scholar]
- 34.Perahia DG, Wang F, Mallinckrodt CH, Walker DJ, Detke MJ. Duloxetine in the treatment of major depressive disorder: a placebo- and paroxetine-controlled trial. Eur psychiatr. 2006;21(6):367–378. doi: 10.1016/j.eurpsy.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 35.Croft H, Settle E Jr, Houser T, Batey SR, Donahue RM, Ascher JA. A placebo-controlled comparison of the antidepressant efficacy and effects on sexual functioning of sustained-release bupropion and sertraline. Clin Ther. 1999;21(4):643–658. doi: 10.1016/S0149-2918(00)88317-4 [DOI] [PubMed] [Google Scholar]
- 36.Rickels K, Amsterdam J, Clary C, Fox I, Schweizer E, Weise C. A placebo-controlled, double-blind, clinical trial of paroxetine in depressed outpatients. Acta Psychiatr Scand Suppl. 1989;350:117–123. doi: 10.1111/j.1600-0447.1989.tb07188.x [DOI] [PubMed] [Google Scholar]
- 37.Goldstein DJ, Lu Y, Detke MJ, Wiltse C, Mallinckrodt C, Demitrack MA. Duloxetine in the treatment of depression: a double-blind placebo-controlled comparison with paroxetine. J Clin Psychopharmacol. 2004;24(4):389–399. doi: 10.1097/01.jcp.0000132448.65972.d9 [DOI] [PubMed] [Google Scholar]
- 38.Lepola UM, Loft H, Reines EH. Escitalopram (10–20 mg/day) is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol. 2003;18(4):211–217. doi: 10.1097/00004850-200307000-00003 [DOI] [PubMed] [Google Scholar]
- 39.Wang Y. Comparison of the effects of escitalopram and citalopram in the treatment of depression. Strait Pharma J. 2016;28(12):119–120. [Google Scholar]
- 40.Zhou Z. Clinical efficacy and adverse reactions of escitalopram and paroxetine in the treatment of single depression. Contemp Med. 2018;24(22):152–153. [Google Scholar]
- 41.Zhu Y. Analysis of the therapeutic effect of escitalopram oxalate and paroxetine hydrochloride on 46 patients with depression. Contemp Med. 2015;21(05):150–151. [Google Scholar]
- 42.Liu R, Yu Z. Wu X. The efficacy and side effects of escitalopram in the treatment of depression. Jilin med j. 2013;34(24):4871–4872. [Google Scholar]
- 43.Xu Y, Pan X, Pan X, Hao C, Deng Y. A controlled study of escitalopram and citalopram in the treatment of depression. J Clin psychiatry. 2011;21(01):42. [Google Scholar]
- 44.Wang X, Han D, Wang L. Escitalopram vs. Fluoxetine in the Treatment of Depression: A Control Study. Eval Anal Drug-Use Hospital China. 2010;10(07):620–622. [Google Scholar]
- 45.Zhang X, Xu X. Comparison of the treatment of Escitalopram and Sertraline for depression. Med j Chinese People’s Health. 2010;22(17):2205–2206+2209. [Google Scholar]
- 46.Hu M, Li Y, Lu X, Xu G, Chen J. Escitalopram vs citalopram for depression: a randomized, double-blind, double-dummy, multicenter parallel controlled study. Central South Pharmacy. 2010;8(01):67–69. [Google Scholar]
- 47.Xun G, Li Y, Zhao J, et al. Escitalopram vs citalopram in treatment of depression: a randomized, double-blind, double-dummy, multicenter parallel controlled study. Chin J New Drugs Clin Rem. 2009;28(04):263–267. [Google Scholar]
- 48.Liu X, Zhang Y, Tan Q, Chen Y, Wang Z, Nie D. A controlled study in the treatment of depression with escitalopram and paroxetine. J Clin psychiatr. 2009;19(03):177–178. [Google Scholar]
- 49.Yang R. A comparative study of citalopram and paroxetine in the treatment of depression. Shanxi Med j. 2008;37(06):563. [Google Scholar]
- 50.Jin X, Xu X, Xu D, Yy C. Clinical efficacy and safety of escitalopram oxalate versus paroxetine in the treatment of unipolar depression. Chin J Clin Pharmacol. 2015;31(10):812–814. [Google Scholar]
- 51.Nierenberg AA, Greist JH, Mallinckrodt CH, et al. Duloxetine versus escitalopram and placebo in the treatment of patients with major depressive disorder: onset of antidepressant action, a non-inferiority study. Curr Med Res Opin. 2007;23(2):401–416. doi: 10.1185/030079906X167453 [DOI] [PubMed] [Google Scholar]
- 52.Xu F, Xu L. Escitalopram vs. Fluoxetine for Depression: A Control Study. China Pharm. 2009;20(14):1084–1086. [Google Scholar]
- 53.Cen L, Zou J, Tong J. Comparative study on escitalopram and paroxetine in the treatment of depression. Shanghai arch psychiatr. 2009;21(01):41–42. [Google Scholar]
- 54.Yu YQ, Zhang YL, Wang Z, et al. Involvement of proBDNF in Monocytes/Macrophages with gastrointestinal disorders in depressive mice. Neurotox Res. 2020;38(4):887–899. doi: 10.1007/s12640-020-00235-8 [DOI] [PubMed] [Google Scholar]
- 55.Liu Y, Zou GJ, Tu BX, et al. Corticosterone induced the increase of proBDNF in primary hippocampal neurons via endoplasmic reticulum stress. Neurotox Res. 2020;38(2):370–384. doi: 10.1007/s12640-020-00201-4 [DOI] [PubMed] [Google Scholar]
- 56.Lin LY, Kelliny S, Liu LC, Al-Hawwas M, Zhou XF, Bobrovskaya L. Peripheral ProBDNF delivered by an AAV vector to the muscle triggers depression-like behaviours in mice. Neurotox Res. 2020;38(3):626–639. doi: 10.1007/s12640-020-00256-3 [DOI] [PubMed] [Google Scholar]
- 57.Walker JK, Gainetdinov RR, Mangel AW, Caron MG, Shetzline MA. Mice lacking the dopamine transporter display altered regulation of distal colonic motility. Am J Physiol Gastrointest Liver Physiol. 2000;279(2):G311–318. doi: 10.1152/ajpgi.2000.279.2.G311 [DOI] [PubMed] [Google Scholar]
- 58.Matsushima Y, Terada K, Kamei C, Sugimoto Y. Sertraline inhibits nerve growth factor-induced neurite outgrowth in PC12 cells via a mechanism involving the sigma-1 receptor. Eur J Pharmacol. 2019;853:129–135. doi: 10.1016/j.ejphar.2019.03.032 [DOI] [PubMed] [Google Scholar]
- 59.Baudry A, Pietri M, Launay JM, Kellermann O, Schneider B. Multifaceted regulations of the serotonin transporter: impact on antidepressant response. Front Neurosci. 2019;13:91. doi: 10.3389/fnins.2019.00091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Frizzo ME. Can a selective serotonin reuptake inhibitor act as a glutamatergic modulator? Curr Ther Res Clin Exp. 2017;87:9–12. doi: 10.1016/j.curtheres.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee HA, Kim KS, Hyun SA, Park SG, Kim SJ. Wide spectrum of inhibitory effects of sertraline on cardiac ion channels. Korean j Physiol Pharmacol. 2012;16(5):327–332. doi: 10.4196/kjpp.2012.16.5.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singhal M, Manzella C, Soni V, et al. Role of SHP2 protein tyrosine phosphatase in SERT inhibition by enteropathogenic E. coli (EPEC). Am J Physiol Gastrointest Liver Physiol. 2017;312(5):G443–g449. doi: 10.1152/ajpgi.00011.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhong W, Shahbaz O, Teskey G, et al. Mechanisms of nausea and vomiting: current knowledge and recent advances in intracellular emetic signaling systems. Int J Mol Sci. 2021;22(11):5797. doi: 10.3390/ijms22115797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dong C, Zhang JC, Yao W, et al. Effects of escitalopram, R-citalopram, and reboxetine on serum levels of tumor necrosis factor-α, interleukin-10, and depression-like behavior in mice after lipopolysaccharide administration. Pharmacol Biochem Behav. 2016;144:7–12. doi: 10.1016/j.pbb.2016.02.005 [DOI] [PubMed] [Google Scholar]
- 65.Zurita-Turk M, Mendes Souza B, Prósperi de Castro C, et al. Attenuation of intestinal inflammation in IL-10 deficient mice by a plasmid carrying Lactococcus lactis strain. BMC Biotechnol. 2020;20(1):38. doi: 10.1186/s12896-020-00631-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.David DJ, Bourin M, Jego G, Przybylski C, Jolliet P, Gardier AM. Effects of acute treatment with paroxetine, citalopram and venlafaxine in vivo on noradrenaline and serotonin outflow: a microdialysis study in Swiss mice. Br J Pharmacol. 2003;140(6):1128–1136. doi: 10.1038/sj.bjp.0705538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Song J, Wang T, Zhang X, Li B, Zhu C, Zhang S. Upregulation of gastric norepinephrine with beta-adrenoceptors and gastric dysmotility in a rat model of functional dyspepsia. Physiol Res. 2020;69(1):135–143. doi: 10.33549/physiolres.934169 [DOI] [PMC free article] [PubMed] [Google Scholar]