Abstract
Background: Two-dimensional (2D) radiographic parameters have been used to estimate the amount of heart and lung irradiated for minimizing heart and lung complications in breast cancer patients. The aim of this study was to investigate the correlation between traditionally used 2D radiographic and dose-volume parameters during adjuvant radiotherapy of breast cancer.
Methods: In this cross-sectional study, we analyzed 121 female patients treated with breast-conserving surgery (BCS) or modified radical mastectomy (MRM) and 3D conformal radiotherapy (3DCRT) using two-field radiotherapy (2FRT) or three-field radiotherapy (3FRT) technique. All patients underwent computed tomography (CT)-planning. Two-D parameters, including central lung distance (CLD), maximum lung depth (MLD), maximum heart length (MHL), maximum heart distance (MHD), and chest wall separation (CWS), were measured using digitally reconstructed radiographs (DRR) and CT images. DVHs for lung, heart, and target were created. The Pearson correlation test was used to evaluate the correlation between 2D radiographic and dose-volume parameters.
Results: There was a correlation between CLD and ipsilateral lung V5-20Gy and Dmean and between MLD and ipsilateral lung V5-20Gy. In 2FRT, only moderate correlation between CLD and ipsilateral lung V20Gy (r = 0.453, P = 0.003) and between MLD and ipsilateral lung V20Gy (r = 0.593, P <0.001) were observed. Poor correlation of MHL and heart V25Gy (r = 0.409, P = 0.007) was seen only in 3FRT. There was a correlation between MHD and heart dose-volume data, with a strong correlation between MHD and heart V5-25Gy and Dmean (r = 0.875-0.934, P<0.001) in the 2FRT group. No correlation between CWS and breast Dmax was found.
Conclusion: There was a correlation between 2D parameters (i.e., CLD, MLD, and MHD) and the heart and lung dose-volume parameters during adjuvant breast radiotherapy. Although CLD was correlated to ipsilateral lung V5-20Gy and Dmean, the correlation between CLD and ipsilateral lung V20Gy was greater than other dose-volume parameters. MHD provided a close estimation of heart dose-volume parameters.
Keywords: 2D Radiographic Parameters, 3D Dose-Volume Parameters, CLD, Breast Cancer, Adjuvant Radiotherapy
Introduction
↑What is “already known” in this topic:
In adjuvant breast radiotherapy, two-dimensional (2D) radiographic parameters of lung and heart irradiated have been used to estimate the amount of heart and lung irradiated for minimizing heart and lung complications in breast cancer patients.
→What this article adds:
There is a correlation between traditionally used 2D parameters and the heart and lung dose-volume parameters during adjuvant radiotherapy of breast cancer. CLD was correlated to ipsilateral lung V5-20Gy and Dmean.
Breast cancer is the most common type of cancer and the second leading cause of cancer-related death among women worldwide (1). Although there are several treatment options for breast cancer, surgery, chemotherapy, and radiotherapy are considered as the main treatment options (2). Adjuvant loco-regional radiotherapy has been established as an important component of the current standard multimodality approach after surgery for breast cancer because it reduces local and regional recurrences and death following breast-conserving surgery (BCS), as well as after mastectomy in high-risk patients (3,4). In radiotherapy for breast cancer, it is essential to minimize radiotherapy-induced side effects because most breast cancer patients are cured. As such, it is crucial to consider the long-term hazards of breast radiotherapy. Hence, it is important to spare the heart and lung, as major organs at risk (OARs), in breast cancer patients undergoing adjuvant radiotherapy. In cases of left-sided breast cancer, incidental irradiation to the heart has resulted in an increased risk of cardiac events (5-7). Furthermore, breast cancer radiotherapy inevitably involves irradiation of the lung tissue, leading to radiotherapy-induced lung injuries such as radiation pneumonitis and lung fibrosis (6,8). The aforementioned radiation complications are technique- and dose-volume dependent (9-11).
Until now, a number of radiotherapy techniques have been applied to treat breast cancer (12). Over the past 50 years, conventional two-dimensional (2D) planning in adjuvant radiotherapy for breast cancer has been used, with good target coverage. However, in current clinical practice, 3D computed tomography (CT) based conformal planning techniques are fast replacing 2D planning in breast cancer radiotherapy (13). Three-D conformal plans lead to an improved evaluation of target volume coverage and OARs doses, thereby providing a great opportunity to predict the risk of radiation toxicities (13).
For the conventional plans, certain 2D radiographic parameters have been traditionally applied as a proxy to estimate the irradiated lung and heart volume during radiotherapy for breast cancer, and hence, predict the risk of radiation-induced toxicity (14-16). Several simple 2D parameters such as central lung distance (CLD), chest wall separation (CWS), and maximum heart distance (MHD) have been defined to estimate the radiation dose delivered to the lung and heart (17). Several studies have reported that the CLD is the best predictor of ipsilateral irradiated lung volume during two-field tangential breast radiotherapy (14,15). However, the relationship between lung volume irradiated and the CLD, as a predictor of radiation pneumonitis risk, is reduced in cases of additional lymphatic field irradiation (15,18). In the era of CT-based conformal treatment planning, it is possible to directly measure the volume of lung irradiated using dose-volume histograms (DVH) that are generated by treatment planning software (TPS). Nowadays, a number of TPS with advanced dose calculation algorithms are available that can readily generate DVH. Dose-volume parameters can be applied to optimize treatment plans, thereby reducing radiation doses to OARs. In addition, such information can be useful in identifying certain parameters for the prediction of the risk of radiation-induced side effects. For example, it has been reported that there is a positive relationship between the mean V20Gy (the volume of lung receiving ≥ 20Gy) of the ipsilateral lung and radiation pneumonitis risk (19).
It is worthwhile to mention that 2D radiographic parameters (i.e., CLD, CWS, MHD, and so on) were empirically used prior to the advent of CT-based planning. Many patients were treated using the 2D conventional radiotherapy technique about 10-20 years ago and are now being followed up for possible side effects. It is essential to find the correlation treatment parameters from 2D to 3D treatment for the analysis of the outcome. Hence, the purpose of this study is to investigate the correlation between traditionally used 2D radiographic parameters and dose-volume parameters to assess the extent of lung and heart irradiation during adjuvant radiotherapy of breast cancer.
Methods
Patient selection
This cross-sectional study was conducted on 121 women with breast cancer treated with BCS or modified radical mastectomy (MRM) and adjuvant radiotherapy between January 2012 and December 2017 at the Department of Radiation Oncology, Hafte-Tir-Hospital, Iran University of Medical Sciences, Tehran, Iran. Prior to radiotherapy, all patients provided written informed consent. After the radiotherapy procedure, no informed consent was received owing to the study design.
The inclusion criteria were age ≥ 18; a histopathological diagnosis of breast cancer after BCS or having a T3 and N1-3 tumors after MRM who received adjuvant radiotherapy using 3D-CT planning techniques to the breast or chest wall with supraclavicular (three-field radiotherapy (3FRT)) or without supraclavicular irradiation (2FRT). Our exclusion criteria were patients with inadequate dosimetric data, unconventional treatment technique or dose/ fractionation, previous irradiation, and bilateral breast irradiation.
Radiotherapy treatment
All patients underwent CT-planning using a Toshiba Aquilion 16 Slice CT Scanner (Toshiba America Medical Systems, Tustin, CA) in the supine position with an inclined breast board. Patients were scanned with a slice thickness of 3 mm from mid-neck to mid-abdomen. CT images were imported into the ISOgray TPS. Clinical target volume (CTV), planning target volume (PTV), and OARs (e.g., heart and lung) were contoured according to the protocol of Radiation Therapy Oncology Group (RTOG) (20).
The two opposing tangential fields were used for the treatment of the entire breast/chest wall (2FRT), with or without an anterior supraclavicular field (3FRT), as shown in Figure 1. Herein, we used the half beam block in the posterior aspect of the field to provide a non-divergent beam edge, thereby reducing the dose to the lung and heart. The prescribed dose for all patients was 50 Gy in 25 fractions with 6 MV photons. Siemens linear accelerator machine (Siemens AG, Erlangen, Germany) was used for delivering 3D conformal radiotherapy (3DCRT). For tangential fields, the source to axis distance (SAD) technique was used and the dose was calculated at the isocenter point. For supraclavicular fields, a single field was used with the source to skin distance (SSD) technique, and the gantry was rotated up to 8 degrees to reduce the spinal cord doses. The dose for the supraclavicular field was prescribed at a depth of 3.5 cm from the skin surface. Plans were normalized to cover PTV by a 95% iso-dose line.
Fig. 1.

Sagittal and coronal CT slices for two representative patients. Dose distribution in 2-field radiotherapy (a and b) and 3-field radiotherapy (c and d).
Two-dimensional radiographic parameters
The CT data were reconstructed using TPS to form digitally reconstructed radiographs (DRR). DRRs and CT images were used to assess 2D radiographic parameters (Fig. 2), i.e., CLD, maximum lung distances (MLD), MHD, maximum heart length (MHL), and CWS.
Fig. 2.
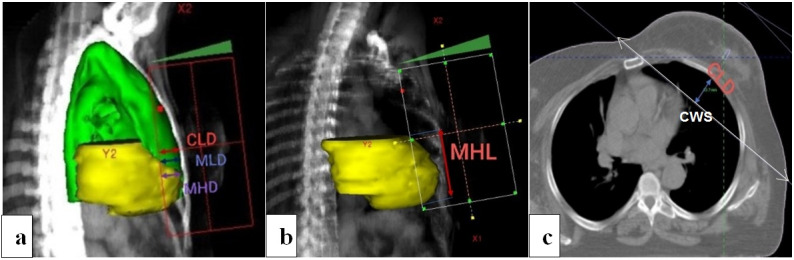
Two-dimensional parameters measured on digitally reconstructed radiographs and CT images: CLD (central lung depth); MLD (maximum lung distance); MHD (maximum heart distance); MHL (maximum heart length); and CWS (chest wall separation)
The CLD was measured from the field border to the edge of the lung contour at the central axis on the tangential simulation DRR, as shown in Figure 2. The MLD was defined as the maximum depth of the lung irradiated. For patients with left-sided breast cancer, we also measured MHD and MHL. The MHD was defined as the maximum width of the heart in the tangent fields. The MHL was measured as the maximum length of the heart in the tangential fields. The CWS was measured as the non-divergent posterior field edge from the sternum to the lateral exterior aspect of the chest wall in patients with BCS.
Dose-volume parameters
DVHs for lung, heart and target volumes were created. Three-D dosimetric endpoints were as follows: the mean dose (Dmean) of the lung and heart; the volume of the lung receiving 5Gy (V5Gy), V10Gy, and V20Gy; V5Gy, V10Gy, V20Gy, and V25Gy of the heart; and maximum breast dose (Dmax).
Statistical analysis
Statistical analysis was performed using SPSS 20.0 software (SPSS Inc., Illinois, Chicago, USA). The Pearson correlation test was used to evaluate the correlation between 2D radiographic and dose-volume parameters. The correlation was considered statistically significantatP ≤ 0.01. A good correlation between datasets was considered as a Pearson correlation coefficient (r) ≥ 0.7; moderate when 0.5 ≤ r < 0.7; and poor when r < 0.5.
Results
Table 1 summarizes patient characteristics. A total of 121 female patients treated with BCS or MRM and adjuvant radiotherapy were eligible for analysis. As shown in Table 1, the mean age of patients was 49 years (range, 29-75 years). A dose of 50 Gy (2Gy/fraction) was delivered to the breast after BCS (n = 62), or to the chest wall after MRM (n = 59). Two-third (66.1%) of patients were treated with 3FRT (n = 80), whereas one third (33.9%) received 2FRT (n = 41).
Table 1. Patient characteristics (n = 121) .
| Characteristics | Mean (range) | No. (%) |
| Age | 49 (29-75) | |
| Treatment site | ||
| Left | 59 (48.8) | |
| Right | 62 (51.2) | |
| Treatment technique | ||
| Two-field | 41 (33.9) | |
| Three-field | 80 (66.1) | |
| Surgery type | ||
| BCS | 62 (51.2) | |
| MRM | 59 (48.8) |
BCS: Breast-conserving surgery; MRM: Modified
Radical mastectomy
The average (± standard deviation (SD)) 2D and dose-volume (i.e., 3D) parameters, regardless of treatment technique, treatment site, and type of surgery, is outlined in Table 2. The correlation between 2D and 3D parameters, regardless of treatment technique, treatment site, and type of surgery, is summarized in Table 3. Overall, there was a moderate correlation between CLD and ipsilateral lung V5-20Gy (r = 0.504-0.651, P < 0.001), between MLD and ipsilateral lung V5-20Gy and Dmean (r = 0.492-0.637, P < 0.001), and also between MHD and heart V5-25Gy and Dmean (r = 0.626-0.690, P < 0.001). Poor correlation was found between CLD and ipsilateral mean lung dose (r = 0.374, P < 0.001), and also between MHL and heart V5-25Gy and Dmean (r = 0.298-0.402, P = 0.001-0.019). There was no correlation between CWS and maximum dose of breast (r = 0.103, P = 0.427).
Table 2. Mean ± standard deviation (SD) values of conventional 2D and dose-volume parameters .
| Variable | Mean ± SD |
| 2D parameters | |
| CLD (cm) | 3.0 ± 0.6 |
| MLD (cm) | 3.2 ± 0.6 |
| MHL (cm) | 7.6 ± 0.2 |
| MHD (cm) | 2.4 ± 0.7 |
| CWS (cm) | 22.3 ± 3.1 |
| Dose-volume parameters for ipsilateral lung | |
| V5Gy (%) | 39.8 ± 8.6 |
| V10Gy (%) | 28.5 ± 6.9 |
| V20Gy (%) | 22.4 ± 5.9 |
| Dmean (Gy) | 23.8 ± 6.1 |
| Dose-volume parameters for heart | |
| V5Gy (%) | 19.1 ± 7.0 |
| V10Gy (%) | 13.8 ± 5.8 |
| V20Gy (%) | 11.1 ± 5.7 |
| V25Gy (%) | 9.5 ± 5.2 |
| Dmean (Gy) | 12.7 ± 4.9 |
| Maximum dose of breast (%) | 108.5 ± 2.7 |
2D: Two-dimensional; CLD: Central lung depth; MLD:
Maximum lung depth; MHL: Maximum heart length; MHD:
Maximum heart distance; CWS: Chest wall separation; Vx:
Volume of lung or heart receiving xGy; Dmean: Mean dose
Table 3. Pearson correlation factors between conventional 2D and dose-volume parameters .
| Variable | PCF (P-value) |
| CLD vs. DVH (ipsilateral lung) | |
| V5Gy (%) | 0.504 (< 0.001) |
| V10Gy (%) | 0.593 (< 0.001) |
| V20Gy (%) | 0.651 (< 0.001) |
| Dmean (Gy) | 0.374 (< 0.001) |
| MLD vs. DVH (ipsilateral lung) | |
| V5Gy (%) | 0.492 (< 0.001) |
| V10Gy (%) | 0.556 (< 0.001) |
| V20Gy (%) | 0.637 (< 0.001) |
| Dmean (Gy) | 0.610 (< 0.001) |
| MHL vs. DVH (heart) | |
| V5Gy (%) | 0.298 (0.019) |
| V10Gy (%) | 0.301 (0.018) |
| V20Gy (%) | 0.313 (0.013) |
| V25Gy (%) | 0.402 (0.001) |
| Dmean (Gy) | 0.361 (0.004) |
| MHD vs. DVH (heart) | |
| V5Gy (%) | 0.669 (< 0.001) |
| V10Gy (%) | 0.656 (< 0.001) |
| V20Gy (%) | 0.626 (< 0.001) |
| V25Gy (%) | 0.690 (< 0.001) |
| Dmean (Gy) | 0.668 (< 0.001) |
| CWS vs. DMax breast | 0.103 (0.427) |
CLD: Central lung depth; DVH: Dose-volume histogram; MLD:
Maximum lung depth; MHL: Maximum heart length; MHD:
Maximum heart distance; Vx: Volume of lung or heart receiving xGy;
Dmean: Mean dose; CWS: Chest wall separation; Dmax: Maximum dose
PCF: Pearson correlation factor
PCF significant if P ≤ 0.01; PCF ≥ 0.7: Good correlation;
PCF ≥ 0.5 and < 0.7: Moderate correlation.
PCF < 0.5: Poor correlation.
Table 4 outlines the average (±SD) 2D and 3D parameters in patients treated with BCS and MRM and 2FRT and 3FRT. Table 5 summarizes the correlation between 2D and 3D parameters in patients with BCS and MRM and 2FRT and 3FRT. In the BCS group, there was a moderate correlation between CLD and ipsilateral lung V5-20Gy, between MLD and ipsilateral lung V5-20Gy and Dmean, and also between MHD and heart V5-25Gy and Dmean. In both BCS and MRM groups, no correlation was found between MHL and heart V5-25Gy and Dmean. In the MRM group, a moderate correlation was found between CLD and ipsilateral lung V5-20Gy, and between MLD and ipsilateral lung V5-20Gy and Dmean. As displayed in Table 5, no correlation was found between CLD and ipsilateral lung Dmean in the BCS group, whereas a poor correlation was observed in the MRM group. There was a good correlation between MHD and heart V5-25Gy and Dmean (r = 0.769-0.812, P < 0.001) in patients treated with MRM, as shown in Table 5. In 2FRT, there was a poor correlation between CLD and ipsilateral lung V20Gy (r = 0.453, P = 0.003), and between MLD and ipsilateral lung V10-20Gy and Dmean. In both 2FRT and 3FRT, no correlation was found between MHL and heart V5-25Gy and Dmean, except between MHL and heart V25Gy in 3FRT (r = 0.409, P = 0.007). In 2FRT, there was a good correlation between MHD and heart V5-25Gy and Dmean (r = 0.875-0.934, P < 0.001), as shown in Table 5. In 3FRT, a moderate correlation was found between CLD and ipsilateral lung V5-20Gy and Dmean, between MLD and ipsilateral lung V5-20Gy and Dmean, and between MHL and heart V5-25Gy and Dmean. In both 2FRT and 3FRT, there was no correlation between CWS and maximum dose of the breast.
Table 4. Mean ± SD values of conventional 2D and dose-volume parameters by type of surgery and treatment technique .
| Variable | BCS | MRM | 2FRT | 3FRT |
| 2D parameters | ||||
| CLD (cm) | 2.8 ± 0.7 | 3.3 ± 0.5 | 2.9 ± 0.6 | 3.1 ± 0.6 |
| MLD (cm) | 3.0 ± 0.6 | 3.3 ± 0.5 | 3.1 ± 0.5 | 3.2 ± 0.6 |
| MHL (cm) | 7.3 ± 1.8 | 8.0 ± 1.4 | 7.8 ± 1.6 | 7.6 ± 1.7 |
| MHD (cm) | 2.4 ± 0.9 | 2.5 ± 0.5 | 2.3 ± 0.6 | 2.5 ± 0.8 |
| CWS (cm) | - | - | 23.1 ± 2.5 | 21.9 ± 3.3 |
| Dose-volume parameters for ipsilateral lung | ||||
| V5Gy (%) | 39.2 ± 8.6 | 40.5 ± 8.6 | 32.0 ± 5.5 | 43.8 ± 7.0 |
| V10Gy (%) | 27.3 ± 6.9 | 29.9 ± 6.7 | 23.7 ± 4.1 | 31.0 ± 6.7 |
| V20Gy (%) | 21.1 ± 6.0 | 23.8 ± 5.6 | 18.7 ± 3.7 | 24.3 ± 6.0 |
| Dmean (Gy) | 23.0 ± 6.4 | 24.6 ± 5.7 | 20.8 ± 5.8 | 25.3 ± 5.7 |
| Dose-volume parameters for heart | ||||
| V5Gy (%) | 18.0 ± 7.1 | 20.1 ± 6.7 | 18.7 ± 7.0 | 19.3 ± 7.0 |
| V10Gy (%) | 12.5 ± 6.0 | 15.2 ± 5.4 | 13.3 ± 5.8 | 14.1 ± 5.9 |
| V20Gy (%) | 10.1 ± 6.5 | 12.0 ± 4.7 | 10.3 ± 5.4 | 11.5 ± 5.9 |
| V25Gy (%) | 8.3 ± 5.5 | 10.8 ± 4.6 | 9.0 ± 5.3 | 9.8 ± 5.1 |
| Dmean (Gy) | 11.7 ± 5.0 | 13.7 ± 4.6 | 12.3 ± 4.9 | 12.9 ± 4.9 |
| Maximum dose of breast (%) | - | - | 108.5 ± 2.9 | 108.5 ± 2.6 |
2D: Two-dimensional; CLD: Central lung depth; MLD: Maximum lung depth; MHL: Maximum heart length; MHD: Maximum heart distance; CWS: Chest wall separation; Vx: Volume of lung or heart receiving xGy; Dmean: Mean dose; BCS: Breast-conserving surgery; MRM: Modified radical mastectomy; 2FRT: Two-field radiotherapy; 3FRT: Three-field radiotherapy
Table 5. Pearson correlation factors between conventional 2D and dose-volume parameters by type of surgery and treatment technique .
| Variable | BCS PCF (P-value) |
MRM PCF (P-value) |
2FRT PCF (P-value) |
3FRT PCF (P-value) |
| CLD vs. DVH (ipsilateral lung) | ||||
| V5Gy (%) | 0.501 (< 0.001) | 0.530 (< 0.001) | 0.151 (0.346) | 0.688 (< 0.001) |
| V10Gy (%) | 0.578 (< 0.001) | 0.572 (< 0.001) | 0.316 (0.044) | 0.698 (< 0.001) |
| V20Gy (%) | 0.637 (< 0.001) | 0.617 (< 0.001) | 0.453 (0.003) | 0.732 (< 0.001) |
| Dmean (Gy) | 0.314 (0.013) | 0.414 (0.001) | 0.105 (0.514) | 0.559 (< 0.001) |
| MLD vs. DVH (ipsilateral lung) | ||||
| V5Gy (%) | 0.478 (< 0.001) | 0.518 (< 0.001) | 0.330 (0.035) | 0.650 (< 0.001) |
| V10Gy (%) | 0.515 (< 0.001) | 0.569 (< 0.001) | 0.463 (0.002) | 0.628 (< 0.001) |
| V20Gy (%) | 0.610 (< 0.001) | 0.628 (< 0.001) | 0.593 (< 0.001) | 0.692 (< 0.001) |
| Dmean (Gy) | 0.623 (< 0.001) | 0.572 (< 0.001) | 0.425 (0.006) | 0.704 (< 0.001) |
| MHL vs. DVH (heart) | ||||
| V5Gy (%) | 0.319 (0.080) | 0.215 (0.246) | 0.264 (0.262) | 0.317 (0.041) |
| V10Gy (%) | 0.274 (0.136) | 0.248 (0.179) | 0.264 (0.261) | 0.324 (0.037) |
| V20Gy (%) | 0.280 (0.126) | 0.298 (0.103) | 0.378 (0.101) | 0.297 (0.056) |
| V25Gy (%) | 0.389 (0.031) | 0.336 (0.065) | 0.407 (0.075) | 0.409 (0.007) |
| Dmean (Gy) | 0.353 (0.052) | 0.303 (0.097) | 0.333 (0.152) | 0.381 (0.013) |
| MHD vs. DVH (heart) | ||||
| V5Gy (%) | 0.641 (< 0.001) | 0.790 (< 0.001) | 0.901 (< 0.001) | 0.588 (< 0.001) |
| V10Gy (%) | 0.636 (< 0.001) | 0.769 (< 0.001) | 0.875 (< 0.001) | 0.577 (< 0.001) |
| V20Gy (%) | 0.566 (0.001) | 0.796 (< 0.001) | 0.923 (< 0.001) | 0.521 (< 0.001) |
| V25Gy (%) | 0.665 (< 0.001) | 0.811 (< 0.001) | 0.934 (< 0.001) | 0.600 (< 0.001) |
| Dmean (Gy) | 0.632 (< 0.001) | 0.812 (< 0.001) | 0.910 (< 0.001) | 0.581 (< 0.001) |
| CWS vs. DMax breast | - | - | 0.098 (0.672) | 0.108 (0.502) |
CLD: Central lung depth; DVH: Dose-volume histogram; MLD: Maximum lung depth; MHL: Maximum heart length; MHD: Maximum heart distance; Vx: Volume of lung or heart receiving xGy; Dmean: Mean dose; Dmax: Maximum dose; CWS: Chest wall separation; BCS: Breast conserving surgery; MRM: Modified radical mastectomy; 2FRT: Two-field radiotherapy; 3FRT: Three-field radiotherapy PCF: Pearson correlation factor;PCF significant if P ≤ 0.01; PCF ≥ 0.7: Good correlation; PCF ≥ 0.5 and < 0.7: Moderate correlation; PCF < 0.5: Poor correlation.
Table 6 summarizes the average (± SD) 2D and 3D parameters in left- and right-sided breast cancer. The correlation between 2D and 3D parameters in left- and right-sided breast cancer is outlined in Table 7. In left-sided breast cancer, there was no correlation between CLD and ipsilateral lung Dmean (r = 0.082, P = 0.537). A moderate correlation was found between CLD and ipsilateral lung V10-20Gy in left-sided breast cancer and also between MLD and ipsilateral lung V20Gy and Dmean, as shown in Table 7. In right-sided breast cancer, a moderate correlation was found between CLD and ipsilateral lung V5-20Gy and Dmean, and also between MLD and ipsilateral lung V5-20Gy and Dmean. There was no correlation between CWS and maximum dose of breast either left-sided or right-sided breast cancer.
Table 6. Mean ± SD values of conventional 2D and dose-volume parameters by type of treatment site .
| Variable | Left | Right |
| 2D parameters | ||
| CLD (cm) | 3.2 ± 0.7 | 2.9 ± 0.5 |
| MLD (cm) | 3.2 ± 0.6 | 3.1 ± 0.5 |
| CWS (cm) | 22.5 ± 2.6 | 22.2 ± 3.5 |
| Dose-volume parameters for ipsilateral lung | ||
| V5Gy (%) | 40.4 ± 9.4 | 39.2 ± 7.7 |
| V10Gy (%) | 29.5 ± 7.7 | 27.5 ± 5.9 |
| V20Gy (%) | 23.3 ± 6.7 | 21.6 ± 5.0 |
| Dmean (Gy) | 23.9 ± 6.3 | 23.6 ± 5.9 |
| Maximum dose of breast (%) | 108.9 ± 2.9 | 108.2 ± 2.6 |
2D: Two-dimensional; CLD: Central lung depth; MLD: Maximum lung depth; CWS: Chest wall separation; Vx: Volume of lung or heart receiving xGy; Dmean: Mean dose
Table 7. Pearson correlation factors between conventional 2D and dose-volume parameters by table-type of the treatment site .
| Variable | Left PCF (P-value) |
Right PCF (P-value) |
| CLD vs. DVH (ipsilateral lung) | ||
| V5Gy (%) | 0.413 (0.001) | 0.557 (< 0.001) |
| V10Gy (%) | 0.528 (< 0.001) | 0.614 (< 0.001) |
| V20Gy (%) | 0.588 (< 0.001) | 0.675 (< 0.001) |
| Dmean (Gy) | 0.082 (0.537) | 0.596 (< 0.001) |
| MLD vs. DVH (ipsilateral lung) | ||
| V5Gy (%) | 0.372 (0.004) | 0.563 (< 0.001) |
| V10Gy (%) | 0.463 (< 0.001) | 0.607 (< 0.001) |
| V20Gy (%) | 0.594 (< 0.001) | 0.660 (< 0.001) |
| Dmean (Gy) | 0.534 (< 0.001) | 0.666 (< 0.001) |
| CWS vs. DMax breast | 0.149 (0.423) | 0.057 (0.761) |
CLD: Central lung depth; DVH: Dose-volume histogram; MLD: Maximum lung depth; Vx: Volume of lung or heart receiving xGy; Dmean: Mean dose; CWS: Chest wall separation; Dmax: Maximum dose; PCF: Pearson correlation factor; PCF significant if P ≤ 0.01; PCF ≥ 0.7: Good correlation; PCF ≥ 0.5 and < 0.7: Moderate correlation. PCF < 0.5: Poor correlation.
Discussion
In the present study, the correlation between heart and lung dose-volume data and conventionally used 2D parameters (i.e., CLD, MLD, MHL, and MHD) in adjuvant radiotherapy for breast cancer was investigated. In summary, our results revealed that there is a moderate correlation between CLD and ipsilateral lung V5-20Gy and between MLD and ipsilateral lung V5-20Gy. In 2FRT, there is a poor correlation between CLD and ipsilateral lung V5-10Gy, whereas a moderate correlation between CLD and ipsilateral lung V20Gy and between MLD and ipsilateral lung V20Gy were observed, as shown in Table 5. Poor correlation of MHL and heart V25Gy was seen only in 3FRT. From our data, it can be seen that there is a correlation between MHD and heart dose-volume data, as observable in Tables 3 and 5. No correlation between CWS and the maximum dose of the breast was found.
Previous studies have demonstrated a correlation of a simple 2D parameter such as CLD with lung 3D dose-volume data (16,17,21). Teh et al. found a strong correlation between CLD and ipsilateral lung V10-40Gy in patients treated with 2FRT (n = 51), whereas no statistically significant correlation between CLD and ipsilateral lung V10-40Gy was observed in patients treated with 3FRT (n = 38) (16). In another similar study, Onal et al. have also reported that although there is a correlation between ipsilateral lung volume irradiated and the CLD during two-field tangential breast radiotherapy, this correlation is reduced once supraclavicular fields are added for nodal irradiation (21). By contrast, with 3FRT, the results of our study show that there is a moderate correlation between CLD and ipsilateral lung V5-10Gy, as well as a good correlation of CLD and ipsilateral lung V20Gy, as observable in Table 5. The characteristics of the patient population in the present study were similar to previous studies. Similar to our study, patients in previous studies had different types of surgery (BCS or mastectomy) for left- or right-sided breast cancer (16,17,21). Possible causes for these discrepancies can be associated with patient-specific anatomy, variation in the shape of the anterior chest wall, variation in the patient’s position, and patient motion related to breathing. Also, we used the traditional matching technique (TMT), whereas the mono-isocentric technique (MIT) was used in previous studies (16,17,21). Thus, the difference between the two radiotherapy planning techniques (i.e., TMT and MIT) might affect the heart and lung doses. The observation of a higher lung dose with supraclavicular field to treat the regional lymph nodes is not surprising, as shown in Table 4. It has been reported that the addition of a supraclavicular field can increase actual irradiated lung volume and ipsilateral lung V20Gy up to 183 ± 80.2 cm3 and 16.5 ± 6.2 %, respectively (22). Also, a significant correlation between CLD and ipsilateral lung V20Gy was found in breast cancer patients (n = 74) who received regional irradiation (22). It is worthwhile to mention that CLD of the supraclavicular field was defined as the longitudinal distance from the matching line with tangents to the lung apex at the central axis (22), whereas we measured the CLD from the field border to the edge of the lung contour at the central axis on the tangential simulation DRR.
CLD, as a surrogate measure of lung volume irradiated, has been traditionally used for predicting the risk of radiation pneumonitis as a consequence of breast radiotherapy. As stated by the European Organization for Research and Treatment of Cancer (EORTC) and the European Society of Mastology (EUSOMA) guidelines, CLD should be less than 3 cm to limit the incidence of radiation pneumonitis following adjuvant radiotherapy for breast cancer (23). With a CLD less than 3 cm, no cases of radiation pneumonitis were reported among 1624 breast cancer patients treated with radiotherapy (24). Also, with a CLD range of 1-3 cm and CLD greater than 4 cm, the risk of symptomatic radiation pneumonitis was calculated to be less than 2% and up to 10%, respectively (25). As shown in Table 2, the mean CLD was 3.0 cm in our study. Therefore, it can be expected that the incidence of radiation pneumonitis should be very low. In recent years, due to the increasing availability of 3D CT-based planning, it may be better to use dose-volume parameters to assess the risk of radiation pneumonitis. It has been reported that lung V20Gy and Dmean are reliable dosimetric parameters for predicting radiation pneumonitis (26). In an old study, a correlation between ipsilateral lung V20Gy and risk of radiation pneumonitis was found in breast cancer patients treated with different radiotherapy techniques. Using the two-field tangential technique, the incidence of pneumonitis was less than 1% with the mean lung V20Gy value of 7% (19). With the addition of regional irradiation, the mean lung V20Gy increased to 20%-30%, resulting in a 7.5% to 11.5% increase in the incidence of pneumonitis (19). A 1.1% incidence of pneumonitis with the mean ipsilateral lung V20Gy values of 14% was also reported using 2FRT (16). However, adding a supraclavicular field resulted in an ipsilateral lung V20Gy increase of 22% (16). From Table 4, it can be seen that the mean ipsilateral lung V20Gy (18.7% with 2FRT and 24.3% with 3FRT) was similar to that of the previous studies.
Traditional 2D radiographic parameters can also be associated with 3D dose-volume data of the heart. CT-based treatment planning provides accurate dose-volume information. Nonetheless, 2D parameters can be useful in radiotherapy centers without 3D resources. In the current study, we have demonstrated that heart 2D parameters, especially MHD, can be used to estimate the volume of the heart receiving high doses when using tangential fields and these results are in line with previous studies (17,18). Herein, we observed a good correlation between MHD and heart V5-20Gy and Dmean using tangential beams (r = 0.875-0.934, P < 0.001), as shown in Table 5. In a previous study, a strong correlation between MHD and heart Dmean was observed (27). Also, it has been reported that patients with MHD more than 3 cm show a higher risk of cardiac events; however, these results were not statistically significant (28). In the current study, there was only a poor correlation between MHL and heart V25Gy; therefore, this 2D parameter is not recommended as a surrogate measure of heart volume irradiated.
In a previous study, it has been observed that in a patient population with CWS in the range of 16-35 cm, there is a direct correlation between the size of the breast and the maximum dose of the breast. Hence, the authors suggested that the use of advanced techniques such as field-in-field and intensity-modulated radiotherapy (IMRT) can be useful for patients with large CWS (17). Herein, we observed no correlation between CWS and the maximum dose of the breast. Compared to the previous study (17), in our study, the average ± SD CWS was 22.3 ± 3.1 cm (median, 22.8 cm; range, 11.1-27.8 cm), so breast size was smaller and more uniform.
Our study has certain limitations. A small cohort of patients was included in this study. In a study to investigate the relationship between the two parameters, it is necessary to have a large sample size to make the results more reliable. Moreover, we did not report the incidence of radiation pneumonitis and cardiac events to better elucidate the relationship between 2D and 3D parameters and radiation-induced lung and heart injuries.
Conclusion
In conclusion, this study demonstrated that there is a correlation between traditionally used 2D parameters (i.e., CLD, MLD, and MHD) and the heart and lung dose-volume parameters during adjuvant radiotherapy of breast cancer. Although CLD was correlated to ipsilateral lung V5-20Gy and Dmean, the correlation between CLD and ipsilateral lung V20Gy was greater than other dose-volume parameters. Also, the correlation between CLD and volume of lung irradiated for 3FRT was stronger; as compared to 2FRT.MHD provided a close estimation of heart dose-volume parameters, especially in the two-field tangential technique where there was a strong correlation between MHD and heart V5-25Gy and Dmean.Investigating the correlation between 2D and 3D treatment parameters provides an opportunity to compare the outcomes in older studies.
Acknowledgment
We are thankful to the staff of the Department of Radiation Oncology, Hafte-Tir-Hospital (Tehran, Iran).
Ethical statement
The study was approved by the ethics committee of Iran University of Medical Sciences, Tehran, Iran. Ethics No. is IR.IUMS.FMD.REC.1396.9411188003. Informed consent was obtained from all individual participants prior to their inclusion in the study.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Fadavi P, Mehrabian A, Salmanian S, Mahdavi SR, Yousefi Diba AA, Javadinia SA. The Relationship between Lung and Heart Two-Dimensional Parameters and Three-Dimensional Dose-Volume Data in Adjuvant Radiotherapy for Breast Cancer. Med J Islam Repub Iran. 2022 (2 Mar);36:16. https://doi.org/10.47176/mjiri.36.16
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Moo TA, Sanford R, Dang C, Morrow M. Overview of Breast Cancer Therapy. PET Clin. 2018;13(3):339–54. doi: 10.1016/j.cpet.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials. Lancet 2011;378(9804):1707-16. [DOI] [PMC free article] [PubMed]
- 4.McGale P, Taylor C, Correa C, Cutter D, Duane F, Ewertz M, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–35. doi: 10.1016/S0140-6736(14)60488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darby SC, Ewertz M, McGale P, ennet AM, Blom-Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–98. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 6.Taylor C, Correa C, Duane FK, Aznar MC, Anderson SJ, Bergh J, et al. Estimating the Risks of Breast Cancer Radiotherapy: Evidence From Modern Radiation Doses to the Lungs and Heart and From Previous Randomized Trials. J Clin Oncol. 2017;35(15):1641–9. doi: 10.1200/JCO.2016.72.0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boero IJ, Paravati AJ, Triplett DP, Hwang L, Matsuno RK, Gillespie EF, et al. Modern Radiation Therapy and Cardiac Outcomes in Breast Cancer. Int J Radiat Oncol Biol Phys. 2016;94(4):700–8. doi: 10.1016/j.ijrobp.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 8.Aznar MC, Duane FK, Darby SC, Wang Z, Taylor CW. Exposure of the lungs in breast cancer radiotherapy: A systematic review of lung doses published 2010-2015. Radiother Oncol. 2018;126(1):148–54. doi: 10.1016/j.radonc.2017.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piroth MD, Baumann R, Budach W, Dunst J, Feyer P, Fietkau R, et al. Heart toxicity from breast cancer radiotherapy: Current findings, assessment, and prevention. Strahlenther Onkol. 2019;195(1):1–12. doi: 10.1007/s00066-018-1378-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gokula K, Earnest A, Wong LC. Meta-analysis of incidence of early lung toxicity in 3-dimensional conformal irradiation of breast carcinomas. Radiat Oncol. 2013;8:268. doi: 10.1186/1748-717X-8-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Käsmann L, Dietrich A, Staab-Weijnitz CA, Manapov F, Behr J, Rimner A, et al. Radiation-induced lung toxicity – cellular and molecular mechanisms of pathogenesis, management, and literature review. Radiat Oncol. 2020;15:214. doi: 10.1186/s13014-020-01654-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schubert LK, Gondi V, Sengbusch E, Westerly DC, Soisson ET, Paliwal BR, et al. Dosimetric comparison of left-sided whole breast irradiation with 3DCRT, forward-planned IMRT, inverse-planned IMRT, helical tomotherapy, and topotherapy. Radiother Oncol. 2011;100(2):241–6. doi: 10.1016/j.radonc.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Aras S, İkizceli T, Aktan M. Dosimetric Comparison of Three-Dimensional Conformal Radiotherapy (3D-CRT) and Intensity Modulated Radiotherapy Techniques (IMRT) with Radiotherapy Dose Simulations for Left-Sided Mastectomy Patients. Eur J Breast Health. 2019;15(2):85–9. doi: 10.5152/ejbh.2019.4619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neal AJ, Yarnold JR. Estimating the volume of lung irradiated during tangential breast irradiation using the central lung distance. Br J Radiol. 1995;68(813):1004–8. doi: 10.1259/0007-1285-68-813-1004. [DOI] [PubMed] [Google Scholar]
- 15.Das IJ, Cheng EC, Freedman G, Fowble B. Lung and heart dose volume analyses with CT simulator in radiation treatment of breast cancer. Int J Radiat Oncol Biol Phys. 1998;42(1):11–9. doi: 10.1016/s0360-3016(98)00200-4. [DOI] [PubMed] [Google Scholar]
- 16.Teh AY, Park EJ, Shen L, Chung HT. Three-dimensional volumetric analysis of irradiated lung with adjuvant breast irradiation. Int J Radiat Oncol Biol Phys. 2009;75(5):1309–15. doi: 10.1016/j.ijrobp.2008.12.077. [DOI] [PubMed] [Google Scholar]
- 17.Das IJ, Andrews JZ, Cao M, Johnstone PA. Correlation of 2D parameters to lung and heart dose-volume in radiation treatment of breast cancer. Acta Oncol. 2013;52(1):178–83. doi: 10.3109/0284186X.2012.673737. [DOI] [PubMed] [Google Scholar]
- 18.Kong FM, Klein EE, Bradley JD, Mansur DB, Taylor ME, Perez CA, et al. The impact of central lung distance, maximal heart distance, and radiation technique on the volumetric dose of the lung and heart for intact breast radiation. Int J Radiat Oncol Biol Phys. 2002;54(3):963–71. doi: 10.1016/s0360-3016(02)03741-0. [DOI] [PubMed] [Google Scholar]
- 19.Lind PA, Wennberg B, Gagliardi G, Fornander T. Pulmonary complications following different radiotherapy techniques for breast cancer, and the association to irradiated lung volume and dose. Breast Cancer Res Treat. 2001;68(3):199–210. doi: 10.1023/a:1012292019599. [DOI] [PubMed] [Google Scholar]
- 20.Gee HE, Moses L, Stuart K, Nahar N, Tiver K, Wang T, et al. Contouring consensus guidelines in breast cancer radiotherapy: Comparison and systematic review of patterns of failure. J Med Imaging Radiat Oncol. 2019;63:102–15. doi: 10.1111/1754-9485.12804. [DOI] [PubMed] [Google Scholar]
- 21.Onal C, Oymak E, Kotek A, Efe E, Arslan G. Correlation of conventional and conformal plan parameters for predicting radiation pneumonitis in patients treated with breast cancer. J Breast Cancer. 2012;15(3):320–8. doi: 10.4048/jbc.2012.15.3.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chie EK, Shin KH, Kim DY, Kim TH, Kang HS, Lee ES, et al. Radiation Pneumonitis after Adjuvant Radiotherapy for Breast Cancer: A Volumetric Analysis Using CT Simulator. J Breast Cancer. 2009;12(2):73–8. [Google Scholar]
- 23.Bartelink H, Garavaglia G, Johansson KA, Mijnheer BJ, Van den Bogaert W, van Tienhoven G, et al. Quality assurance in conservative treatment of early breast cancer. Report on a consensus meeting of the EORTC Radiotherapy and Breast Cancer Cooperative Groups and the EUSOMA (European Society of Mastology) Radiother Oncol. 1991;22(4):323–6. doi: 10.1016/0167-8140(91)90172-d. [DOI] [PubMed] [Google Scholar]
- 24.Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991;21(2):355–60. doi: 10.1016/0360-3016(91)90782-y. [DOI] [PubMed] [Google Scholar]
- 25.Lichter AS, Fraass BA, Yanke B. Treatment Techniques in the Conservative Management of Breast Cancer. Semin Radiat Oncol. 1992;2(2):94–106. doi: 10.1053/SRAO00200094. [DOI] [PubMed] [Google Scholar]
- 26.Seppenwoolde Y, Lebesque JV, De Jaeger K, Belderbos JS, Boersma LJ, Schilstra C, et al. Comparing different NTCP models that predict the incidence of radiation pneumonitis. Int J Radiat Oncol Biol Phys. 2003;55(3):724–35. doi: 10.1016/s0360-3016(02)03986-x. [DOI] [PubMed] [Google Scholar]
- 27.Taylor CW, Nisbet A, McGale P, Darby SC. Cardiac exposures in breast cancer radiotherapy: 1950s-1990s. Int J Radiat Oncol Biol Phys. 2007;69(5):1484–95. doi: 10.1016/j.ijrobp.2007.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Borger JH, Hooning MJ, Boersma LJ, Snijders-Keilholz A, Aleman BM, Lintzen E, et al. Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: the role of irradiated heart volume. Int J Radiat Oncol Biol Phys. 2007;69(4):1131–8. doi: 10.1016/j.ijrobp.2007.04.042. [DOI] [PubMed] [Google Scholar]


