Abstract
Background: Capitation payment is the best-known strategy for paying providers in primary health care. Since health care needs and personal characteristics play an essential role in health care utilization and resource spending, there is a growing tendency on risk adjustment models among health researchers. The objective of this systematic review was to examine the weights used for risk adjustment in primary health care capitation payment.
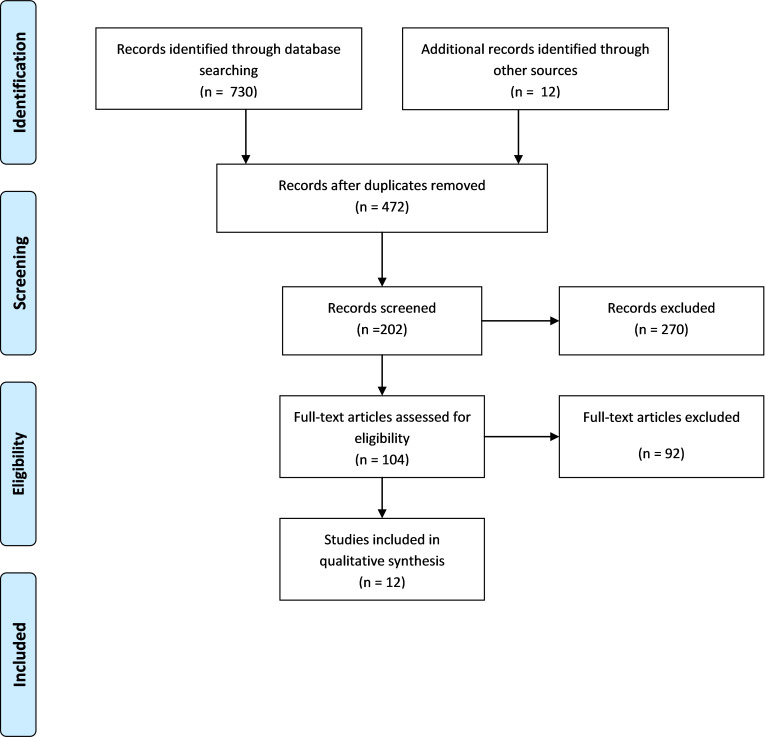
Methods: We systematically searched Scopus, ProQuest, Web of Science, and PubMed in March 2018. Two authors independently apprised the included articles and they also evaluated, identified, and categorized different factors on capitation payments mentioned in the included studies.
Results: A total of 742 studies were identified and 12 were included in the systematic review after the screening process. Risk factors for capitation adjustment included age, gender, and income with the weighted average being 1.76 and 1.03, respectively. Moreover, the weighted average disease incidence adjusted clinical groups (ACGs), diagnostic cost groups (DCGs), principal in patient diagnostic cost groups (PIP-DCGs), and hierarchical coexisting conditions (HCCs) were reported as 1.31, 24.7-.99, 10.4-.65, and 11.7-1.01, respectively.
Conclusion: In low-income countries, the most effective factors used in capitation adjustment are age and sex. Moreover, the most applied factor in high-income countries is adjusted clinical groups, and income factors can have a better impact on the reduction of costs in low-income countries. Each country can select its most efficient factors based on the weight of the factor, income level, and geographical condition.
Keywords: Risk Adjustment, Capitation, Risk Factor, Systematic Review, Health Care
Introduction
↑What is “already known” in this topic:
Primary health care is a global strategy for ensuring basic health care for all people and risk adjusted capitation payment is the best strategy for PHC payment. Risk factors for capitation adjustment include age, gender, income, adjusted clinical groups, diagnostic cost groups, principal in patient diagnostic cost groups, and hierarchical coexisting conditions.
→What this article adds:
This was the first systematic review on weight of risk factors for adjusting capitation in primary health care. The results of this study can be used by expert health economists, health policymakers, and health managers to select the best factor in capitation adjustment and prevent wasting resources.
Primary health care (PHC) has been promulgated for over 2 decades as a global strategy for ensuring basic health care for all people. The PHC is characterized by equity, accessibility, availability of resources, social participation, interpectoral community act ion, and cultural sensitivity (1). Primary health care focuses on reducing costs, improving health and providing quality services through accessing appropriate services and reducing inequalities in people's health (2).
There is no single optimal method for paying the providers. All methods (capitation, salary, fee-for-service, and mixed systems have both advantages and drawbacks, and the desirability of a specific approach depends on the economic, social, and institutional context of a particular setting. Capitation payments is the best strategy for reducing incentives for risk selection and reducing costs in between other payment systems (3,4).
The simple design model of the capitation system is to allocate a fixed value to all individuals regardless of the difference in their individual and social characteristics. At the same time, there is a significant difference in the healthcare needs of different demographic groups and their health expenses (5,6).
A capitation can be defined as the amount of health service funds to be assigned to a person with certain characteristics for the service and time in question, subject to overall budget constraints. The health care needs of citizens vary considerably, depending on personal factors such as age, morbidity, and social factors. Generally, the risk adjustment (RA) logic is based on the principle that fixed capitation should be adjusted in a way that could reflect the costs and health needs of the stakeholders. Considerable effort has therefore been expended on a process known as RA (7).
RA methods are extensively used to decrease costs for the primary health care system. Most RA plans depend on patients’ demographics and diagnoses. Many diagnosis-based RA systems have been effective in reducing the cost of health care in different countries (8).
Risk adjustment models are a novel way to create a new model for health and medical systems now and in the future. These methods are necessary to anticipate the predicted needs for individuals’ health hazards. The main focus of RA capitation models is on diagnostic information. Based on the conducted studies, in addition to risk-based diagnostic systems, these models have reduced the cost of health care in the United States and other countries (6,9). Pay capitation is used to represent expected costs, which can significantly reduce the costs and increase the income obtained from health programs through proper settings. Nevertheless, these payments are made with a strong incentive to create low-cost programs. Family health networks (FHNs) and family health institutions (FHOs) represent 2 successful models in the per capita model, which have used the gender adjustment model, eventually leading to improved health and lower costs (10). RA can play an important role in accessing an appropriate financial level and ensuring resource allocation meets the health needs of the population (11,12).
Some of the most efficient techniques (eg, behavioral characteristics, patients’ socioeconomic status, and factors related to the environment, and disease incidence) to control risk-adjusted capitation can anticipate the application of primary care up to 50% (13,14). According to the literature, explanatory capacities in risk-adjusting models have been restricted by demographic factors (15,16). Over the last 2 decades, various types of risk-adjusting factors have been exploited to improve the predictability of the relevant models.
This systematic review aimed to examine the different RA factor weights of capitation in different countries.
Methods
The preferred items for systematic reviews PRISMA checklist (SI 1) were followed to report the review process. A protocol for this review was registered in the PROSPERO (CRD42017073190) (17).
Appendix 1 presents PRISMA checklist.
Search Strategy and Database
TheScopus, ProQuest, Web of Science, and PubMed databases were searched with the formulation of the following searching terms: "risk factor," "risk adjustment," "adjustment capitation," "per capita adjustment," "capitation fee adjustment," "capitation adjustment," and "adjustment per capita" up until March 2018. Manual searches in the reference lists were also conducted in Google Scholar. All the identified articles were entered in the Endnote software and the duplicates were removed. Title and abstract screening of the retrieved literature was performed by 2 authors (AKh and AM), and any disagreement was resolved by discussion and a third author (ShN).
Appendix 2 presents the search strategy used for this systematic review.
Eligibility Criteria
The survey studies were regarded as eligible for inclusion based on language (English) and content (article of certain methods of RA capitation); the excluded articles were those dealing exclusively with therapies of different diseases/illnesses (not related to RA capitation) and also duplicates. We screened the titles and abstracts of the identified papers and excluded those that were obviously unrelated to our review.
Data Extraction
Two authors cooperated in data extraction of included studies and entered them in to the data extraction sheet designed by the authors. The extracted data included author names, year of publication, country, region, risk factors, and weight of risk factors for adjusting capitation. In addition, the website of the OECD was used to classify countries in terms of economic status.
Quality Appraisal of the Studies
The quality appraisal of the remaining articles was assessed by 2 authors through the Strengthening the Reporting of Observational Studies in Epidemiology tool and any discrepancies between them were resolved through discussion (17).
Data Analysis
We identified different factors on capitation payments mentioned in studies and categorized the factors into 2 groups: "demographic and socioeconomic factors" (age, sex, and income) and "disease incidence factor":
- Adjusted Clinical Groups (ACGs): The combination of diseases of a person is regarded by the ACG system for a predetermined period (usually one year), which is extended to visits and providers. Every category of the ACG is recognized as a calculation for a group of patients with similar morbidity constellations, which demonstrates the demand for care in each category. Researchers in the United States have extensively assessed the reliability and validity of the ACG system (18).
- Diagnostic Cost Groups (DCGs): In the case of the DCG factor, the patient is classified in a separate group according to his or her health factors and morbidities. Based on the information on the number of insured participants in one group and the average treatment costs, the average capitation costs for each group were calculated (15).
- Principal in Patient Diagnostic Cost Groups (PIP-DCGs): The principal inpatient (PIP) diagnostic cost group (DCG) is a measure interpreted by clinical situations in the last year to account for risk of patients in the Medicare health maintenance organization population. This measure is applied by the Center for Medicare and Medicaid Services based in the United States (19).
- Hierarchical Coexisting Conditions (HCCs): Diagnoses obtained from all hospital encounters and physicians are used by the HCC model, describing the medical problems of enrollees with diagnostic groups (HCCs), which are not equally complete. The total anticipated cost of an enrollee is the estimation of all incremental predicted expenses, accompanied by the assigned HCCs of patients (20,21).
Finally, we extracted the weight of each of the various factors playing a role in capitation adjustment in studies and estimated the main or range of each factor.
Results
A total of 742 articles were gathered from the databases. After removing 270 duplicates, the remaining 472 articles were assessed based on title, abstract, and full text. Finally, 12 studies (8,20-30) met the inclusion criteria (Fig. 1). The characteristics of the included studies are presented in Table 1 and also the details of quality appraisal of studies are shown in the Appendix 3.
Fig. 1.
Flowchart of screened, excluded, and included studies
Table 1. Summary of the Final Studies .
| No | Study | Location | By Region | By Income | Year of the study | Risk Factors for the Capitation Adjustment |
| 1 | Sibley et al, 2012 | Ontario, Canada | NORTH AMERICA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2012 | AGE & SEX - ACG – INCOME |
| 2 | Hindle et al, 2004 | Croatia | EUROPE AND CENTRAL ASIA | UPPER-MIDDLE-INCOME ECONOMIES | 2004 | AGE & SEX |
| 3 | Hindle et al, 2006 | Mongolia | EAST ASIA AND PACIFIC | LOWER-MIDDLE-INCOME ECONOMIES | 2007 | AGE & SEX – INCOME |
| 4 | Shmueli et al, 2014 | Israeli | MIDDLE EAST AND NORTH AFRICA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2014 | AGE – ACG |
| 5 | Wender et al, 2003 | Taiwan | EAST ASIA AND PACIFIC | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2003 | AGE & SEX – PIP DCG – TPIP DCG |
| 6 | Chang et al, 2002 | Taiwan | EAST ASIA AND PACIFIC | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2002 | AGE & SEX – DCG |
| 7 | Behrend et al. 2007 | Germany | EUROPE AND CENTRAL ASIA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2007 | AGE & SEX - HCC - HOSP - RRW |
| 8 | Vargas et al, 2006 | Chile | LATIN AMERICA AND THE CARIBBEAN | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2006 | AGE & SEX – DCG |
| 9 | Yuen et al, 2003 | Umbria, Italy | EUROPE AND CENTRAL ASIA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2003 | AGE & SEX - ACG – PIP DCG |
| 10 | Donato et al, 2006 | Australia | EAST ASIA AND PACIFIC | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2006 | AGE & SEX - HCC |
| 11 | Kuhlthau et al, 2005 | The United States | NORTH AMERICA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2005 | AGE & SEX – ACG - DCG – HCC |
| 12 | Pietz et al, 2004 | The United States | NORTH AMERICA | HIGH-INCOME ECONOMIES ($12,236 OR MORE) | 2004 | AGE & SEX – ACG – DCG |
Study Characteristics
All the observational studies included in this systematic review were retrospective. Ten out of the 12 studies were conducted between 2002 to 2014 and were done in high-income countries (8,20-30) and 2 other studies were performed in 2004 and 2007, respectively, (8,20-30) and reported in middle income countries. Age and gender were included in all the studies on the RA capitation.
According to above studies, the influencing factors includeddemographic and socioeconomic factors (age, gender, and income) and disease incidence (adjusted clinical groups, etc).
Risk Adjustment (RA) Factors
Demographic and socioeconomic factors: The demographic characteristics (age and gender) were an effective and applicable variable in all the studies (with the exception of Israel, which only used the age factor) and income was used as an effective factor in capitation adjustment in only 2 studies (Canada and Mongolia). Out of the 12 country studies the mean weight of the age and gender factors was estimated 1.76, SD (1.10). The highest (3.8) and lowest (0.925) weights were, respectively, related to Taiwan (27) and Chile. The mean weight of income was estimated to be 1.04 SD (0.15); the highest and lowest weights of the factors were observed in Mongolia (1.14) and Canada (0.93), respectively. The mean weight of the ACG was estimated to be 1.32, SD (0.59) in the evaluated countries that used the mentioned factor in capitation adjustment. In this regard, the highest and lowest weights of the factor were observed in Israel (2.375) and Italy (1). The ACG factor was used by 5 countries (Canada, Israel, Italy, America (New Jersey), and the United States).The weight range of the DCG factor was 0.99-24.7 in the mentioned countries and was observed in Chile and Taiwan (27), respectively.
To pay for managed care plans of Medicare in 2000, the PIPDCG was executed by the US Health Care Financing Administration (HCFA) after collecting experiences related to the enhancement of RA models based on diagnosis, which are obtained during a decade (31). The main logic of using the PIPDCG model is the application of inpatient diagnoses in the past year as a proxy of the health status of individuals. In addition, these diagnoses can allow the distinction of the enlisted with various health-related costs in the following year. The diagnoses were divided into 172 diagnostic groups, which were clinically homogenous (32)
and used the PIPDCG factor, where the weight range of the factor was 0.65-10.4. In this respect, the lowest and highest weights of the factors were observed in Italy (0.65) and Taiwan (10.4).
In our study, the mean weight of the factor was 3.524 in the mentioned 3 countries that used the HCC factor in capitation adjustment. In this regard, the highest (7.6) and lowest (1.013) weights of the factor were observed in Germany and the United States (New Jersey), respectively.
All the factors indicated in the 12 studies were divided into 2 subcategories: (1) demographics and socioeconomics and (2) disease incidences (Table 2). Moreover, the weight of various risk factors and their mean were extracted accurately in the mentioned studies and calculated.
Table 2. Weight of Risk Factors for Adjusting Capitation .
| NO | Study | Demographics & Socioeconomics | Disease Incidence | ||||
| Age & Sex | Income | ACG | DCG | PIP DCG | HCC | ||
| 1 | Sibley and Glazier (2012) - Ontario, Canada | 1.27 | .9302 | 1.17 | - | - | - |
| 2 | Hindle and Kalanj (2004) – Croatia | 1.76 | - | - | - | - | - |
| 3 | Hindle and Khulan (2007) - Mongolia | 1.15 | 1.14 | - | - | - | - |
| 4 | Shmueli (2014) - Israeli | 1.364 | - | 2.375 | - | - | - |
| 5 | Lin.et al. - (2003) – Taiwan | 3.7 | - | - | - | 10.4 | |
| 6 | Chang et al. - (2002) - Taiwan | 3.8 | - | - | 24.7 | - | - |
| 7 | Behrend et al. - (2007) – Germany | 3.1 | - | - | - | - | 11.7 |
| 8 | Vargas and Wasem - (2006) – Chile | .925 | - | .99 | |||
| 9 | Yuen et al. - (2003) - Umbria, Italy | 1.00 | - | 1.00 | - | .65 | - |
| 10 | Donato and Richardson - Australia |
1.001 | - | - | 1.96 | ||
| 11 | Kuhlthau et al. - (2005) – The United States: Georgia New Jersey Wisconsin | 1.017 | - | 1.017 | 1.017 | - | 1.013 |
| 12 | Pietz et al. - (2004) - The United States | 1.05 | - | 1.03 | 1.46 | - | |
| TOTAL | The mean weight or range of the studies | Max: 3.8 Min:.925 |
Max: 1.14 Min:.9302 |
Max: 2.375 Min: 1 |
Max: 24.7 Min:.99 |
Max: 10.4 Min:.65 |
Max: 11.7 Min: 1.013 |
| Mean (SD) = 1.76 (1.10) |
Mean (SD) = 1.04 (0.15) |
Mean (SD) = 1.32 (0.59) |
Range= (24.7-0.99) | Range= (10.4-0.65) | Range = (11.7-1.01) | ||
Discussion
According to the applied strategy, the 12 articles from Canda, Croatia, Mongolia, Israel, Germany, Chile, Italy, and Australia (one article each), and United States and Taiwan (2 articles each) (8,22-32) were used in the final stage, which were separately evaluated based on various factors involved in capitation adjustment.
The demographic characteristics(age and gender) had the most use in RA capitation. Also, all countries in any geographical region and with any level of income use age and gender as effective variables for capitation adjustment. In addition, the mentioned factors are among the most frequently used factors in capitation adjustment (8,22-23).
Similar to age and gender, the ACG factor is significantly important in studies and is recognized as the most applicable factor after the age and gender variables. Moreover, all the 5 mentioned countries that applied the ACG factor had an income level of above $12.236. Furthermore, 3 of the 5 mentioned countries were from North America (8,24,25,31,32).
The DCG factor was evaluated in 3 out of 12 countries, including Taiwan, Chile, and the US. All the mentioned countries, which evaluated the DCG factor, had a high level of income (above $12.236). With respect to the geographical region, 1 of the 3 mentioned countries are in North America, one is in East Asia and Pacific and one is in Latin America (8,27,29,31).
The income factor was used as a method in capitation adjustment in only 2 (Canada and Mongolia) out of the 12 countries. In the 2 mentioned countries, which used the income factor, Canada had a higher level of income and is located in North America, whereas Mongolia had an income rate below medium ($1.006-3.955) and is located in East Asia and Pacific.
Moreover, the mentioned countries (Canada and Mongolia) were both among the high-income countries of the world ($12.236) (8,22,23,26). Regarding the geographical region, generally, the mean weight was higher in the Asian countries as compared to the European countries.
Conclusion
Age and gender are the most effective factors in capitation adjustment in low-income countries. Following the mentioned factors, the most applied factor in high-income countries is ACG. On the other hand, the factor with the lowest use in capitation adjustment in Germany was HCC, which had the greatest effectiveness in the country. The income factor can have a better impact on reducing costs in low-income countries, where there is a low weight of the factor. DCG is a proposed variable for high-income countries. However, the best factors which can be effective at any time or place regardless of income level, geographical location, and development level are age and gender, which have a favorable mean weight compared to other factors. On the other hand, the income factor is the best factor in capitation adjustment in terms of the mean weight of the factor. Generally, the best weight of the factor for capitation adjustment of various countries cannot be certainly determined. However, each country can select its most efficient factor based on the weight of the factor, level of income, and geographical condition of the country.
Acknowledgment
This study was supported by Tabriz University of Medical Sciences.The authors are thankful to the Department of Health Economics, Tabriz Health Services Management Research Center, Health Management and Safety Promotion Research Institute, Tabriz University of Medical Sciences.
Conflict of Interests
The authors declare that they have no competing interests.
Appendix
Appendix 1. PRISMA checklist .
| Section/topic | # | Checklist item | Reported on page # | Explanation |
| TITLE | ||||
| Title | 1 |
Identify the report as a systematic review, meta-analysis, or both. The report is identified as a systematic review in Abstract and Methods section. |
1 | It is reported in title |
| ABSTRACT | ||||
| Structured summary | 2 |
Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. This summary is given in the abstract. |
1 | It is reported in abstract |
| INTRODUCTION | ||||
| Rationale | 3 |
Describe the rationale for the review in the context of what is already known. The rationale is clearly stated in the Introduction section. |
2 | Over the last two decades, various types of risk-adjusting factors have been exploited to improve the predictability of the relevant models. Occasionally, the RA is regarded as a positive technique used to make more development in health systems. Despite the difficulties faced during the RA enhancement, it is still necessary to perform this method. The need for improvement of dominant risk-adjustment systems (RASs) has been confirmed after reviewing the studies the last 15 years |
| Objectives | N/A | - | ||
| Methods | ||||
| Protocol and registration | 5 |
Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. The review protocol is given in Appendix S2 Supporting Information - see section A ‘Developing the Search Strategy’ |
4 |
https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=73190 Ali Khezri, S.N., Determine the weight or coefficients risk factors for the capitation adjustment in different countries. PROSPERO 2017 CRD42017073190 Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017073190. Refer to: supplement information 1 (SI 1) |
| Eligibility criteria | 6 |
Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. The eligibility criteria are given in Appendix S2 Supporting Information - see section A ‘Developing the Search Strategy’ |
Page 6 figure 1 |
Refer to the result: figure 1 The literature search identified 742 citations, of which 270 were duplicates. We researched 60 full- texts through screening the titles and abstracts. Twelve studies met the inclusion criteria (Fig. 1). The characteristics of the included studies are presented in Fig. 1. |
| Methods | ||||
| Information sources | 7 |
Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. The information sources are given in Appendix S2 Supporting Information - see Section A ‘Developing the Search Strategy’ and Section B ‘Final Search Strategies’. |
11-13 And 4 |
last searched in March 2017 Final Search Strategies: Refer to: supplement information 1 (SI 1) |
| Search | 8 |
Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. This is given in Appendix S2 Supporting Information - Section B ‘Final Search Strategies’. |
SI (1) The systematic review search strategies Page 4 |
supplement information 1 (SI 1) for the PubMed: ((((((((capitation adjustment[Title/Abstract]) OR capitation adjustment[MeSH Terms])) OR (("per capita adjustment"[Title/Abstract]) OR "per capita adjustment"[MeSH Terms])) OR (("capitation fee adjustment"[Title/Abstract]) OR "capitation fee adjustment “Mesh Terms]))) OR ((((("adjustment per capita"[Title/Abstract]) OR "adjustment per capita"[MeSH Terms])) OR ((adjustment capitation[Title/Abstract]) OR adjustment capitation[MeSH Terms])) OR (("adjustment capitation fee"[Title/Abstract]) OR "adjustment capitation fee"[MeSH Terms])))) AND ((((risk adjustment[Title/Abstract]) OR risk adjustment[MeSH Terms]) OR risk factor[Title/Abstract]) OR risk factor[MeSH Terms]) |
| Study selection | 9 |
State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). The study selection for eligibility and screening is given in the main manuscript under Methods. |
4-5 | The survey studies were regarded as eligible for inclusion based on language (English) and content (article of certain methods of RA capitation); the excluded articles were those dealing exclusively with therapies of different diseases/illnesses (not related to RA capitation) and also duplicates. We screened the titles and abstracts of the identified papers and excluded those that were obviously unrelated to our review. |
| Data collection process | 10 |
Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. This is stated in the Methods section, Paragraph 1. |
4-5 | It is reported the data collection process |
| Data items | 11 |
List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. This is stated in the Methods section, Paragraph 1. |
5 | In publishing this manuscript, no funding was received from public finance, commercial or nonprofit organizations. |
| Risk of bias in individual studies | 12 | N/A | - | N/A |
| Summary measures | 13 |
State the principal summary measures (e.g., risk ratio, difference in means). We estimated trends in causes of vision impairment, including analysis of uncertainties, by age, sex, and geographical region and fractions of blindness and visual impairment due to glaucoma. This is detailed in the Methods section, second paragraph. |
5 | We identified Different factors that influenced capitation payments in the included studies. We categorized the factors in two group "demographic &Socioeconomics factor" (Age & Sex and income) and "disease incidence factor" (Adjusted clinical groups (ACGs), Diagnostic cost groups (DCGs), Principal in patient diagnostic cost groups (PIP-DCGs), Hierarchical coexisting conditions (HCCs)) (Table 1).We evaluated the weight of each of the various factors playing a role in capitation adjustment in studies and report the main and range of each factors. If a factor mentioned in minimum two studies, we considered that factor likely as a risk-adjustment factor to affect the capitation payment |
| Synthesis of results | 14 | N/A | - | |
| Risk of bias across studies | 15 |
Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). These are described under ‘limitations of the study’ in the final paragraph of the Discussion section. |
N/A | N/A |
| Additional analyses | 16 |
Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. These were not performed. |
N/A | N/A |
| Results | ||||
| Study selection | 17 |
Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. This is given as Figure 1 using a PRISMA flowchart. |
Figure 1
PAGE 6 |
The literature search identified 742 citations, of which 270 were duplicates. We researched 60 full-texts through screening the titles and abstracts. Twelve studies [8, 28-38] met the inclusion criteria (Fig. 1). The characteristics of the included studies are presented in Fig. 1. |
| Study characteristics | 18 |
For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. The citations are available in Appendix S3 Table B of Supporting Information |
Appendix Table 2 Page 6 |
According to the above studies, the influencing factors included demographic and socioeconomic factors (age, gender and income) and disease incidence (adjusted clinical groups, etc.). The characteristics of the included studies are summarized in Table 2. |
| Risk of bias within studies | 19 |
Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). We were unable to comment on this beyond the decision to exclude studies that carried a significant risk of bias as detailed in Point 12 of the checklist. |
N/A | |
| Results of individual studies | 20 |
For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. In terms of prevalence of vision impairment and blindness, the graphs in Figure H of Appendix S3 of Supporting Information demonstrate the confidence intervals around the prevalence for studies included in the analysis. |
Table 3 page 8 |
As mentioned above, All the factors indicated in the 12 studies were divided into two subcategories of demographic and socio-economics as well as disease incidence (Table 3). Moreover, the weight of various risk factors and mean of them were extracted accurately in the mentioned studies and calculated. TABLE 3 |
| Synthesis of results | 21 |
Present results of each meta-analysis done, including confidence intervals and measures of consistency. These results are reported with 95% Uncertainty Intervals in the results section and Tables. |
N/A |
N/A |
| Results | ||||
| Risk of bias across studies | 22 |
Present results of any assessment of risk of bias across studies (see Item 15). The statistical model investigated the risk of bias across studies and an account of this can be found in Appendix S3 of Supporting Information |
N/A | N/A |
| Additional analysis | 23 |
Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). Not applicable. |
N/A | N/A |
| Discussion | ||||
| Summary of evidence | 24 |
Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). This is summarised in the discussions section. |
9-10 | According to the applied strategy, the 12 articles from the countries of Canada, Croatia, Mongolia, Israel, Germany, Chile, Italy and Australia (one article each) America and Taiwan (two articles each) were used in the final stage, which were separately evaluated based on various factors involved in capitation adjustment |
| Limitations | 25 |
Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). The limitations are discussed in the discussion section. |
9-10 | |
| Conclusions | 26 |
Provide a general interpretation of the results in the context of other evidence, and implications for future research. Please see the discussion and conclusions section. |
9-10 | the best factors which can be effective at any time or place regardless of level of income, geographical location and level of development are the age and gender variables, which have a favorable mean weight compared to other factors. On the other hand, the income factor is the best factor in capitation adjustment in terms of the mean weight of the factor. Generally, the best weight of the factor for capitation adjustment of various countries cannot be certainly determined. However, each country can select its most efficient factor based on the weight of the factor, level of income and geographical condition of the country. |
| Funding | ||||
| Funding | 27 |
Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. These are given in the title page of the manuscript |
10 | In publishing this manuscript, no funding was received from public finance, commercial or non-profit organizations. |
Appendix
Appendix 2. The systematic review search strategies .
| PUBMED SEARCH** | |
|
Step 1 |
((((((((capitation adjustment[Title/Abstract]) OR capitation adjustment[MeSH Terms])) OR (("per capita adjustment"[Title/Abstract]) OR "per capita adjustment"[MeSH Terms])) OR (("capitation fee adjustment"[Title/Abstract]) OR "capitation fee adjustment “Mesh Terms]))) OR ((((("adjustment per capita"[Title/Abstract]) OR "adjustment per capita"[MeSH Terms])) OR ((adjustment capitation[Title/Abstract]) OR adjustment capitation[MeSH Terms])) OR (("adjustment capitation fee"[Title/Abstract]) OR "adjustment capitation fee"[MeSH Terms])))) AND ((((risk adjustment[Title/Abstract]) OR risk adjustment[MeSH Terms]) OR risk factor[Title/Abstract]) OR risk factor[MeSH Terms]) |
| SCOPUS SEARCH** | |
| Step 2 | TITLE-ABS(risk adjustment) OR TITLE-ABS(risk factor)AND TITLE-ABS(capitation adjustment ) OR TITLE-ABS("per capita adjustment") OR TITLE-ABS("capitation fee adjustment") OR TITLE-ABS(adjustment capitation ) OR TITLE-ABS("adjustment per capita") OR TITLE-ABS( "adjustment capitation fee") |
| *WEB OF SCIENCE SEARCH* | |
| Step 3 | (TOPIC: (((((capitation adjustment OR "capitation fee adjustment") OR "per capita adjustment") OR adjustment capitation) OR "adjustment per capita") OR "adjustment capitation fee") AND TOPIC: (“risk adjustment” OR “risk factor”)) [185 results] |
| *PROQUEST* | |
| Step 4 | all(capitation adjustment OR "per capita adjustment" OR "capitation fee adjustment" OR adjustment capitation OR "adjustment per capita" OR "adjustment capitation fee") AND all(risk adjustment OR risk factor |
Appendix
Appendix 3. STROBE checklist .
| Item No | Recommendation | Author/Year | ||||||||||||
| Sibley et al, 2012 | Hindle et al, 2004 | Hindle et al, 2006 | Shmueli et al, 2014 |
Wender et al, 2003 |
Chang et al, 2002 | Behrend et al. 2007 | Vargas et al, 2006 | Yuen et al, 2003 | Donato et al, 2006 | Kuhlthau et al, 2005 | Pietz et al, 2004 | |||
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | + | + | + | + | + | + | + | + | + | + | + | + |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Background | 2 | Explain the scientific background and rationale for the investigation being reported | + | + | + | + | + | + | + | + | + | + | + | + |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | + | + | + | + | + | + | + | + | + | + | + | + |
| Study design | 4 | Present key elements of study design early in the paper | + | + | + | + | + | + | + | + | + | + | + | + |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | + | + | + | + | + | + | + | + | + | + | + | + |
| Participants | 6 |
(a) Cohort study—Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up Case-control study—Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants |
+ | + | + | + | + | + | + | + | + | + | + | + |
|
(b) Cohort study—For matched studies, give matching criteria and number of exposed and unexposed Case-control study—For matched studies, give matching criteria and the number of controls per case |
+ | + | + | + | + | + | + | + | + | + | + | + | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | + | + | + | + | + | + | + | + | + | + | + | + |
| Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | + | + | + | + | + | + | + | + | + | + | + | + |
| Bias | 9 | Describe any efforts to address potential sources of bias | + | + | N/A | + | + | + | + | N/A | + | N/A | + | + |
| Study size | 10 | Explain how the study size was arrived at | + | + | + | + | + | + | + | + | + | + | + | + |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | + | + | + | + | + | + | + | + | + | + | + | + |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | + | + | + | + | + | + | + | + | + | + | + | + |
| (b) Describe any methods used to examine subgroups and interactions | + | + | + | + | + | + | + | + | + | + | + | + | ||
| (c) Explain how missing data were addressed | + | + | + | + | + | + | + | + | + | + | + | + | ||
|
(d) Cohort study—If applicable, explain how loss to follow-up was addressed Case-control study—If applicable, explain how matching of cases and controls was addressed Cross-sectional study—If applicable, describe analytical methods taking account of sampling strategy |
+ | + | + | + | + | + | + | + | + | + | + | + | ||
| (e) Describe any sensitivity analyses | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed | + | + | N/A | + | + | + | + | + | + | N/A | N/A | + |
| (b) Give reasons for non-participation at each stage | + | + | N/A | + | + | + | + | + | + | N/A | N/A | + | ||
| (c) Consider use of a flow diagram | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | + | + | + | + | + | + | + | + | + | + | + | + |
| (b) Indicate number of participants with missing data for each variable of interest | + | + | + | + | + | + | + | + | + | + | + | + | ||
| (c) Cohort study—Summarise follow-up time (eg, average and total amount) | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Outcome data | 15* | Cohort study—Report numbers of outcome events or summary measures over time | + | + | + | + | + | + | + | + | + | + | + | + |
| Case-control study—Report numbers in each exposure category, or summary measures of exposure | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Cross-sectional study—Report numbers of outcome events or summary measures | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included | + | + | + | + | + | + | + | + | + | + | + | + |
| (b) Report category boundaries when continuous variables were categorized | + | + | + | + | + | + | + | + | + | + | + | + | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses | + | + | + | + | + | + | + | + | + | + | + | + |
| Key results | 18 | Summarise key results with reference to study objectives | + | + | + | + | + | + | + | + | + | + | + | + |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | + | + | + | + | + | + | + | + | + | + | + | + |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | + | N/A | N/A | N/A | + | + | + | + | + | + | + | + |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results | N/A | + | N/A | + | + | N/A | + | N/A | + | N/A | N/A | N/A |
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | + | N/A | N/A | + | N/A | N/A | N/A | + | + | N/A | + | N/A |
Cite this article as: Khezri A, Mahboub-ahari A, Tabrizi JS, Nosratnejad S. Weight of Risk Factors for Adjusting Capitation in Primary Health Care: A Systematic Review. Med J Islam Repub Iran. 2022 (2 Feb);36:2. https://doi.org/10.47176/mjiri.36.2
References
- 1.McElmurry BJ. Primary health care. Ann Rev Nurs Res. 1999;17(1):241–268. [PubMed] [Google Scholar]
- 2.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rice N, Smith PC. Capitation and risk adjustment in health care financing: an international progress report. Milbank Q. 2001;79(1):81–113. doi: 10.1111/1468-0009.00197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gosden T, Forland F, Kristiansen I, Sutton M, Leese B, Giuffrida A, et al. Capitation, salary, fee‐for‐service and mixed systems of payment: effects on the behaviour of primary care physicians. Cochrane Libr 2000;3. [DOI] [PMC free article] [PubMed]
- 5.Barnum H, Kutzin J, Saxenian H. Incentives and provider payment methods. Int J Health Plann Manage, 1995;10(1):23–45. doi: 10.1002/hpm.4740100104. [DOI] [PubMed] [Google Scholar]
- 6. Iezzoni LI. Risk adjustment for measuring health care outcomes. Health Admin Press Chicago 2003;3.
- 7. Rice N, Smith P. Approaches to capitation and risk adjustment in health care: an international survey. 1999: University of York The Centre for Health Economics.
- 8. Pietz K, Ashton CM, McDonell M. Predicting healthcare costs in a population of veterans affairs beneficiaries using diagnosis-based risk adjustment and self-reported health status. Med Care. 2004:1027-1035. [DOI] [PubMed]
- 9. Rosen AK, Loveland S, Anderson JJ, Rothendler JA, Hankin CS, Rakovski CC, et al. Evaluating diagnosis-based case-mix measures: how well do they apply to the VA population? Med Care. 2001:692-704. [DOI] [PubMed]
- 10.Wranik DW, Durier-Copp M. Physician remuneration methods for family physicians in Canada: expected outcomes and lessons learned. Health Care Anal. 2010;18(1):35–59. doi: 10.1007/s10728-008-0105-9. [DOI] [PubMed] [Google Scholar]
- 11.Glazier RH, Klein-Geltink J, Kopp A, Sibley LM. Capitation and enhanced fee-for-service models for primary care reform: a population-based evaluation. CMAJ. 2009;180(11):E72–E81. doi: 10.1503/cmaj.081316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reid RJ, MacWilliam L, Verhulst L, Roos N, Atkinson M. Performance of the ACG case-mix system in two Canadian provinces. Med Care. 2001:86-99. [DOI] [PubMed]
- 13. Manitoba Centre for Health Policy and Evaluation, Reid RJ. Do Some Physician Groups See Sicker Patients Than Others?: Implications for Primary Care Policy in Manitoba. Manitoba Centre for Health Policy and Evaluation, Department of Community Health Sciences, Faculty of Medicine, University of Manitoba 2001;2001 Jul.
- 14.Zielinski A, Kronogård M, Lenhoff H, Halling A. Validation of ACG Case-mix for equitable resource allocation in Swedish primary health care. BMC Public Health. 2009;9(1):347. doi: 10.1186/1471-2458-9-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellis RP, Pope GC, Iezzoni LI, Ayanian JZ, Bates DW, Burstin H. et al. Diagnosis-based risk adjustment for Medicare capitation payments. Health Care Financ Rev. 1996;17(3):101. [PMC free article] [PubMed] [Google Scholar]
- 16. Ettner SL, Frank RG, McGuire TG, Newhouse JP, Notman EH. Risk adjustment of mental health and substance abuse payments. Inquiry. 1998:223-239. [PubMed]
- 17.Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reid RJ, Roos NP, MacWilliam L, Frohlich N, Black C. Assessing population health care need using a claims‐based ACG morbidity measure: a validation analysis in the Province of Manitoba. Health Serv Res. 2002;37(5):1345–1364. doi: 10.1111/1475-6773.01029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosen AK, Loveland S, Anderson JJ. Applying diagnostic cost groups to examine the disease burden of VA facilities: comparing the six" Evaluating VA Costs" study sites with other VA sites and Medicare. Med Care. 2003:II91-II102. [DOI] [PubMed]
- 20.Hindle D, Kalanj K. New general practitioner payment formula in Croatia: is it consistent with worldwide trends? Croat Med J. 2004;45(5):604–610. [PubMed] [Google Scholar]
- 21. Hindle D, Khulan B. New payment model for rural health services in Mongolia. Rural Remote Health 2006;6(1). [PubMed]
- 22.Shmueli A. On the calculation of the Israeli risk adjustment rates. Eur J Health Econ. 2015;16(3):271–277. doi: 10.1007/s10198-014-0572-x. [DOI] [PubMed] [Google Scholar]
- 23. Sibley LM, Glazier RH. Evaluation of the equity of age–sex adjusted primary care capitation payments in Ontario, Can Health Policy 2012;104(2):186-192. [DOI] [PubMed]
- 24.Behrend C, Buchner F, Happich M, Holle R, Reitmeir P, Wasem J. Risk-adjusted capitation payments: how well do principal inpatient diagnosis-based models work in the German situation? Results from a large data set. Eur J Health Econ. 2007;8(1):31–39. doi: 10.1007/s10198-006-0004-7. [DOI] [PubMed] [Google Scholar]
- 25.Chang RE, Lin W, Hsieh CJ, Chiang TL. Healthcare utilization patterns and risk adjustment under Taiwan's National Health Insurance system. J Formos Med Assoc. 2002;101(1):52–59. [PubMed] [Google Scholar]
- 26. 26 Lin W, Chang RE, Hsieh CJ, Yaung CL, Chiang TL. Development of a risk-adjusted capitation model based on principal inpatient diagnoses in Taiwan. J Formos Med Assoc. 2003. 102(9):637-643. [PubMed]
- 27.Vargas V, Wasem J. Risk adjustment and primary health care in Chile. Croat Med J. 2006;47(3):459–468. [PMC free article] [PubMed] [Google Scholar]
- 28.Donato R, Richardson J. Diagnosis-based risk adjustment and Australian health system policy. Aust Health Rev. 2006;30(1):83–99. [PubMed] [Google Scholar]
- 29. Kuhlthau K, Ferris TG, Davis RB, Perrin JM, Iezzoni LI. Pharmacy-and diagnosis-based risk adjustment for children with Medicaid. Med Care. 2005:1155-1159. [DOI] [PubMed]
- 30.Yuen EJ, Louis DZ, Di Loreto P, Gonnella JS. Modeling risk-adjusted capitation rates for Umbria, Italy. Eur J Health Econ. 2003;4(4):304–312. doi: 10.1007/s10198-003-0193-2. [DOI] [PubMed] [Google Scholar]
- 31.Grimaldi PL. Medicare's risk-adjusted capitation method. J Health Care Fin. 2002;28(3):105–119. [PubMed] [Google Scholar]
- 32.Pope GC, Ellis RP, Ash AS, Liu CF, Ayanian JZ, Bates DW. et al. Principal inpatient diagnostic cost group model for Medicare risk adjustment. Health Econ Rev. 2000;21(3):93. [PMC free article] [PubMed] [Google Scholar]