Abstract
Background: COVID-19 pandemic has brought new and fundamental challenges to the healthcare system. Physiotherapists, like other rehabilitation professionals, have been involved in this crisis. One way to protect both the clients and physiotherapists from getting infected and provide physiotherapy services effectively is tele-physiotherapy (TPT). This study investigated the physiotherapists’ perception of TPT and the barriers to its practical application during the COVID-19 outbreak.
Methods: This cross-sectional, descriptive study was adopted in December 2020, using a newly designed checklist. The checklist had four sections, consisting of physiotherapists’ knowledge and awareness, satisfaction, attitude, and also barriers to the use of TPT during the COVID-19 outbreak. The checklist was uploaded to social physiotherapy networks across Iran, and the descriptive data were analyzed statistically.
Results: In this study, 192 physiotherapists participated as follows. Before the COVID-19 outbreak, 48.96% of the participants used TPT, while this rate grew to 64.06% during the outbreak. The majority of the participants (65.1%) believed that the use of TPT would improve the relationship among the physiotherapists and their patients. They also had the lowest level of knowledge (27.08%) about one item in the checklist, i.e., "how to consult with TPT". Based on the participants' views, lack of proper familiarity with the use of this method (87.5%), a lack of high-speed internet access (86.45 %), and a lack of awareness of this method and its benefits (84.37%) had the highest frequencies compared to other barriers.
Conclusion: The results indicate that during the COVID-19 pandemic in Iran, a significant increase in the use of TPT has developed. The overall physiotherapists’ attitude towards TPT was positive, but it was necessary to minimize or eliminate the barriers to applying this effective method. Major recommendations from the participants were: continue to seek physiotherapists’ and patients’ perspectives, introduce proper educational programs for new students enrolled in professional associations and universities, and support the infrastructures, such as telecommunication and financial assistance from insurance companies.
Keywords: Tele-Physiotherapy, Tele-Rehabilitation, COVID-19, Physiotherapy, Rehabilitation
Introduction
↑What is “already known” in this topic:
With the spread of COVID-19, the need for tele-physiotherapy is increasingly felt. There are obstacles to achieving optimal use of this technology.
→What this article adds:
During the COVID-19 outbreak, more physiotherapists used tele-physiotherapy. Physiotherapists and patients have a favorable view of this technology. Still, there are obstacles in this way, such as lack of insurance coverage, lack of proper internet coverage, lack of public acceptance, and lack of clear guidelines.
Late in December 2019, the World Health Organization (WHO) was informed of cases of pneumonia with unknown etiology in China, which quickly spread from a single city to the entire country (1). After a while, it was reported that a highly contagious strain of the coronavirus was spreading (2). It did not take long before the disease spread to the world. Subsequently, the WHO declared this situation a pandemic (3). Scientists believed quarantine and contact tracing of symptomatic individuals alone might not be the best solution. Therefore, strong monitoring measures, such as social distancing necessary in order to stop the transmission of the virus at an early stage (4). The objectives of the social distancing were to decrease or interrupt transmission of the disease in the populations and consequently to reduce its spread, to delay and reduce the epidemic peak, and to relieve the unexpected burden on the healthcare system (5).
In physiotherapy practice, close contact and hands-on treatments are the inevitable parts of providing the services. This makes the physiotherapists susceptible to numerous infectious diseases (6). In response to the COVID-19 pandemic, physiotherapists must consider alternative methods of service provision, such as TPT for both the hospitalized and post-discharge patients with COVID-19, people who have been quarantined at home (7), and all other non-COVID patients who need physiotherapy services. For these reasons, TPT is a potential and practical alternative for delivering PT services (8). TPT as a part of tele-rehabilitation and telehealth is now a component of physiotherapy, with the advantage of providing therapy to patients wherever it is most convenient through web-based communication (9). Although some physiotherapy aspects, such as electrotherapy and manual techniques, cannot be performed remotely, others, such as therapeutic exercises, consultation, and follow up can be performed in this context. A wide range of patients and clients such as musculoskeletal patients, cardiovascular patients, neurologic patients, the elderly, diabetics, etc., can be the audience of this service.
The COVID-19 outbreak has become a turning point for TPT that has tried for decades to attract public acceptance. Citing its numerous benefits, the WHO has stated that tele-healthcare, as well as TPT, should be one of the main areas of the strategic plans to reform the healthcare systems in the 21st century (10). The use of TPT will not be limited to the COVID -19 crisis, and it will continue to be used after this outbreak, especially in rural and remote areas.
Despite its clinical importance, due to the novelty of the scenario, there are many limitations to the implementation of TPT (9). The needs assessment is one of the crucial aspects of a sustainable TPT protocol. An efficient TPT system may be developed if it is accepted by the consumers and used as an alternative method. Attitude plays a vital role in our lives, thoughts, and behavior both individually and collectively. Our views on various issues determine our actions and responses and justify our motivation or reluctance to show resort to certain behaviors. Thus, an individual’s attitude toward TPT is not an exception. This article aims to clarify the Iranian PTs’ perception of TPT and explore the barriers to its application during the COVID-19 outbreak.
Methods
Study Design and Data Collection
This cross-sectional study was conducted in December 2020, using a new checklist developed by the authors. The checklist’s questions were uploaded on one of the online systems (www.digisurvey.net), and the address was published on Iranian PT social networks. The survey was designed in the form of open and closed questions based on a review of previous articles and the related text-based materials by scientific committee members (11).
The checklist consisted of four main sections. The first section had sixteen questions about PT’s satisfaction and their views on using TPT. The second section consisted of twelve questions about the physiotherapists’ level of knowledge of TPT and an open-ended question on whether community PTs were familiar with this method. The PTs’ level of knowledge about TPT was scored using a five-point Likert scale, ranging from very low to very high. The third section had sixteen questions on PTs’ attitudes toward TPT. The last one was a checklist of items covering the barriers facing the application of TPT.
The checklist’s validity was assessed by the opinion of eight experts and professors with a content validity index of (0.87), and a validity ratio index of (0.83). Its reliability was confirmed by using a test-retest method - 10 days apart (r= 0.87).
Statistical Analysis
After the checklist collection, the data were analyzed using Statistical Package for Social Sciences (SPSS), version 18.0 (SPSS Inc. Chicago, Illinois, USA), and the descriptive statistics of the frequency and percentage were derived.
Results
The demographic data of participants are summarized in Table 1.
Table 1. Participants’ demographics .
| Demographic variable | NO. (%) |
| Gender | Male 96 (50), female 96 (50) |
| Age (years) | 37.38±10.15 |
| Work experience (years) | 13.97±9.45 |
| Participants' employment status | Private clinic: 107 (55.72) Hospital-outpatient: 24 (12.5) Hospital-inpatient: 24 (12.5) Home visit: 37 (19.27) |
| Educational degree | Bachelor of Science: 103 (53.64) Master of Science: 45 (23.44) DPT: 22 (11.45) PhD: 22 (11.45) |
As Figure 1 shows, the respondents were distributed across the provinces. It was Tehran physiotherapists who accounted for 20.83% of respondents, with the rest distributed across the provinces.
Fig. 1.
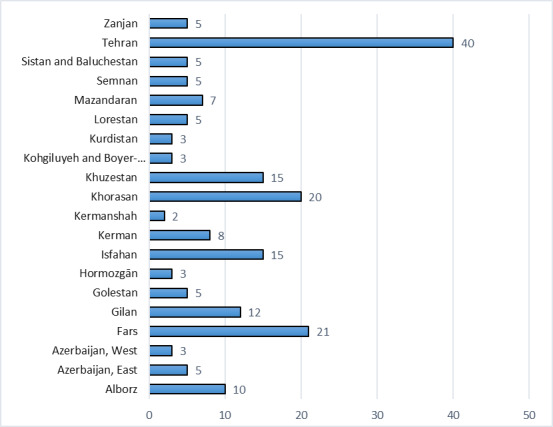
Distribution of Respondents by Province
Before the COVID pandemic, 48.96% of participants (N=94) used TPT. This rate reached 64.06% (N=123) during the outbreak. Participants who used TPT stated that they had an average of five sessions with approximately 15 minutes of treatment per week per patient. Figure 2 represents the distribution of TPT services during the COVID-19 pandemic. According to physiotherapists’ statements, TPT usage during the COVID-19 outbreak is categorized as tele-consultation (52.85%), tele-follow-up (21.14%), and regular TPT sessions (26.01%).
Fig. 2.
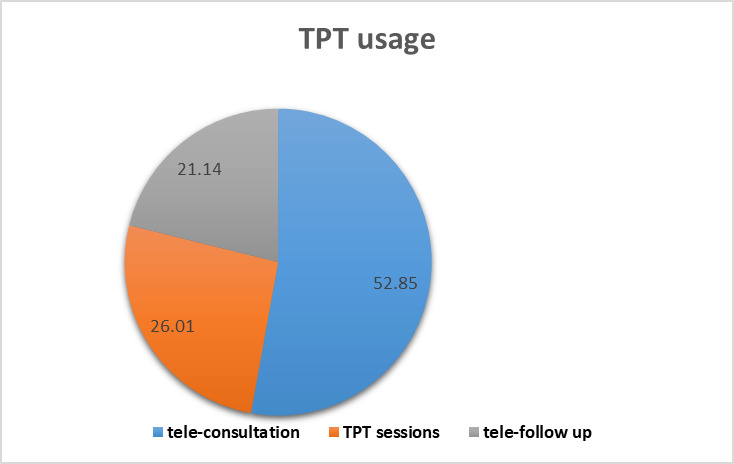
Distribution of TPT usage among physiotherapists ( number of participants: 123)
The data of the participants' satisfaction regarding the quality of the use of TPT during the outbreak of COVID-19 are summarized in Table 2.
Table 2. Physiotherapists' satisfaction level on the use of TPT during the COVID-19 outbreak (N=123) .
| Survey Item | Very low satisfaction, N* (%) |
Low satisfaction, N* (%) |
Relative satisfaction, N* (%) |
High satisfaction, N* (%) |
Very high satisfaction N* (%) |
| The convenience of using apps for TPT | 31 (25.20) | 10 (8.13) | 39 (31.70) | 20 (16.26) | 23 (18.70) |
| Satisfaction with the sound and image quality of the application used | 17 (13.82) | 14 (11.38) | 67 (54.47) | 22 (17.88) | 3 (2.43) |
| The level of cooperation between patients and PT regarding the recommendations made | 14 (11.38) | 61 (49.59) | 19 (15.44) | 19 (15.45) | 10 (8.13) |
| Effectiveness of TPT | 9 (7.31) | 30 (24.39) | 61 (49.60) | 18 (14.63) | 5 (4.06) |
| The feasibility of the proposed treatment methods | 16 (13.01) | 15 (12.19) | 64 (52.03) | 20 (16.26) | 8 (6.50) |
| The extent to which medical goals are achieved | 14 (11.38) | 31 (25.20) | 66 (53.66) | 9 (7.31) | 3 (2.44) |
| Overall satisfaction from TPT | 18 (14.63) | 29 (23.58) | 60 (48.78) | 12 (9.75) | 4 (3.25) |
| Overall average | 13.82 | 22.07 | 43.67 | 13.93 | 6.5 |
*N = Number
The results of the study on the satisfaction of physiotherapists with the use of TPT during the pandemic showed that on average: 13.82 % of users had very low satisfaction, 22.07 % low satisfaction, 43.67 relative satisfaction, 13.93 % high satisfaction, and 6.5 % very high satisfaction. The highest satisfaction level of physiotherapists was with the “convenience of using apps on TPT” (Table 2). Table 3 summarizes the used applications and platforms during the COVID outbreak.
Table 3. Physiotherapists’ views on the use of TPT during the COVID-19 outbreak (N = 123) .
| Opinion | Strongly disagree N* (%) |
Disagree N* (%) |
Neutral Neither agree Nor disagree N* (%) |
Agree N* (%) |
Strongly agree N* (%) |
| It facilitates the treatment of patients. | 11 (8.94) | 16 (13.01) | 36 (29.27) | 50 (40.65) | 10 (8.13) |
| It Increases communication between physiotherapist and patient. | 4 (3.25) | 17 (13.82) | 22 (17.89) | 63 (51.22) | 17 (13.82) |
| It can reduce the number of visits to physiotherapy clinics. | 5 (4.06) | 26 (21.14) | 28 (22.76) | 57 (46.34) | 7 (5.70) |
| It allows the physiotherapist to provide services more quickly. | 5 (4.06) | 34(27.64) | 36 (29.27) | 44 (35.77) | 4 (3.25) |
| It is compatible with all aspects of my work. | 7 (5.69) | 59 (47.97) | 28 (22.76) | 23 (18.70) | 6 (4.87) |
| It is fully functional and compatible with the current situation. | 7 (5.69) | 20 (16.26) | 41 (33.33) | 47 (38.21) | 8 (6.50) |
| It requires a lot of knowledge. | 2 (1.63) | 27 (21.95) | 32 (26.02) | 47 (38.21) | 15 (12.20) |
| It increases the workload. | 3 (2.44) | 35 (28.46) | 30 (24.39) | 51 (41.46) | 4 (3.25) |
| It creates new responsibilities. | 0 (0) | 9 (7.31) | 16 (13.01) | 83 (67.48) | 15 (12.20) |
| It poses a threat to privacy and confidentiality. | 10 (8.13%) | 47 (38.21) | 43 (34.96) | 22 (17.89) | 1 (1) |
*N = Number
Based on the data shown in Figure 3, PTs used and recommended WhatsApp more often than other web-based applications.
Fig. 3.
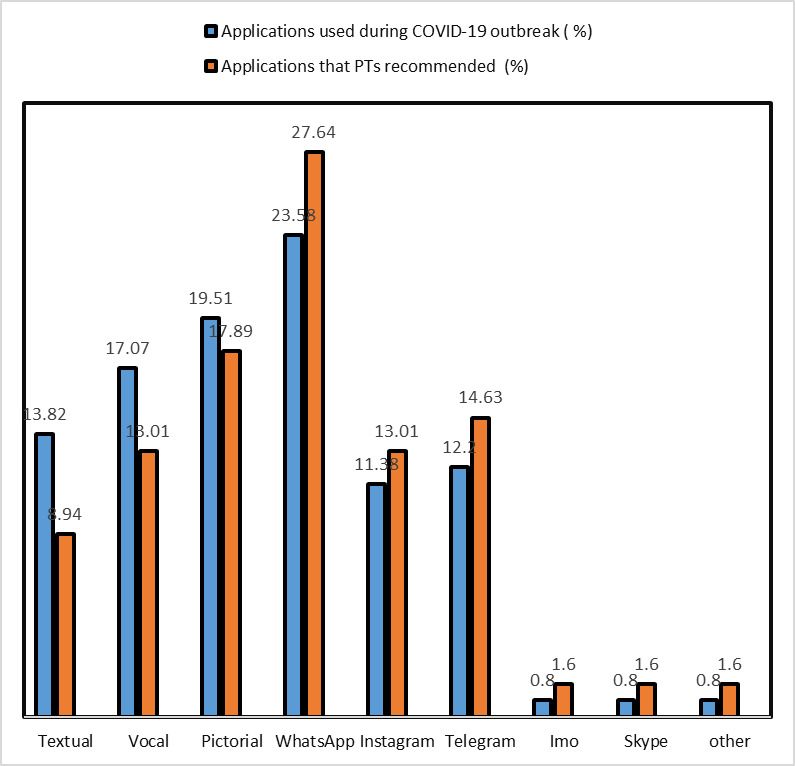
The applications and platforms used during the pandemic situation and recommendation rate (number of participants: 123)
The data in Table 3 indicate that 50.4% of PTs thought they needed more knowledge, 79.7% argued the use of TPT would create additional responsibilities for them, and 65.1% believed that using TPT would improve their relationship with the patients.
As shown in Table 4, the results of the PTs’ knowledge analysis suggest that on average: 14.88 % of the users had very poor knowledge, 26.95 % poor knowledge, 38.93 relative knowledge, 15.88 % high knowledge, and 3.34 % very high knowledge of TPT. They also had the lowest level of knowledge (27.08) on “how to consult patients with TPT” and the highest level of knowledge about the TPT standards (30.21 %).
Table 4. Current PTs’ Knowledge of TPT (N=192) .
| Knowledge | Level of knowledge | ||||
| Very poor N* (%) |
Poor N* (%) |
Satisfactory N* (%) |
Good N* (%) |
Excellent N* (%) |
|
| Use of computer applications in PT | 22 (11.46) | 38 (19.79) | 74 (38.54) | 54 (28.12) | 4 (2.08) |
| Use of TPT | 38 (19.79) | 46 (23.96) | 88 (45.83) | 16 (8.33) | 4 (2.08) |
| Application of TPT in Teaching and Communication with Patients | 15 (7.81) | 48 (25) | 81 (42.19) | 32 (16.66) | 16 (8.33) |
| Consult patients with TPT | 16 (8.33) | 36 (18.75) | 82 (42.71) | 48 (25) | 10 (5.21) |
| Use video chat software | 34 (17.71) | 48 (25) | 56 (29.16) | 46 (23.96) | 8 (4.17) |
| Provide physiotherapy and care services using TPT | 32 (16.67) | 51 (26.56) | 86 (44.79) | 18 (9.37) | 5 (2.60) |
| TPT Methods (Stored and Posted Offline or Online) | 26 (13.54) | 58 (30.21) | 76 (39.58) | 26 (13.54) | 6 (3.12) |
| Different methods of TPT services | 42 (21.87) | 64 (33.33) | 66 (34.37) | 16 (8.33) | 4 (2.08) |
| benefits of TPT | 28 (14.58) | 42 (21.87) | 84 (43.75) | 32 (16.67) | 6 (3.12) |
| Knowledge about the organization responsible for the implementation of TPT | 48 (25) | 64 (33.33) | 66 (34.37) | 12 (6.25) | 2 (1.04) |
| Creation and implementation of TPT technology | 42 (21.87) | 64 (33.33) | 66 (34.37) | 16 (8.33) | 4 (2.08) |
| TPT standards | 0 (0) | 62 (32.29) | 72 (37.50) | 50 (26.04) | 8 (4.17) |
| Overall average | 14.88 | 26.95 | 38.93 | 15.88 | 3.34 |
Figure 4 shows the highest percentages of PTs’ positive attitudes were related to the useful combination of TPT with face-to-face healthcare services (92.70%), and the need for accurate documentation and training guidelines on the use of TPT network systems (90.62%).
Fig. 4.
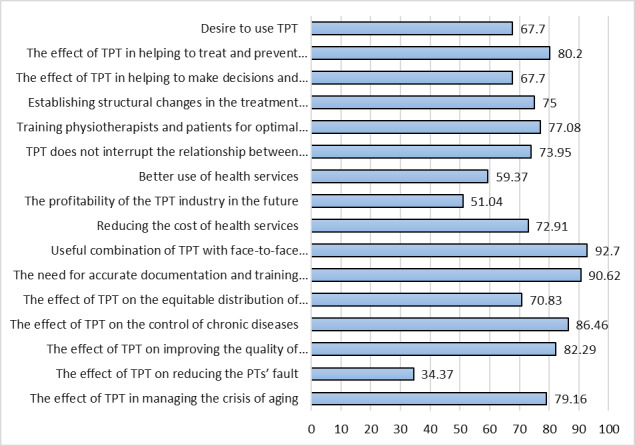
PTs’ positive attitude toward using TPT (N = 192)
As shown in Figure 5, lack of proper training to use this technology (87.5%); lack of high-speed internet access and high bandwidth (86.45 %); lack of awareness and familiarity with this technology and its benefits (84.37%) had the highest frequency compared to other barriers and are the most critical barriers to the use of TPT technology from the perspective of physiotherapists.
Fig. 5.
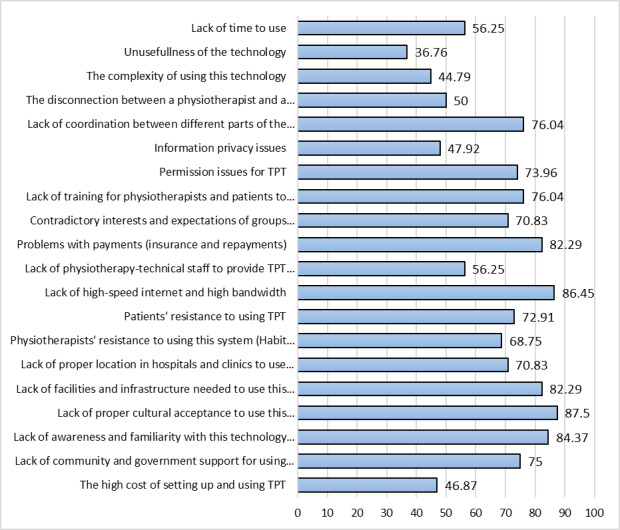
Obstacles to the use of TPT technology from the perspective of physiotherapists (N=192)
Discussion
It should be noted that due to the need for social distancing, more burden has been placed on the PT society than on other rehabilitation professionals. Nevertheless, since the community's response was not commensurate with the quarterly closure of offices and due to reductions in hospital admissions, a comprehensive analysis of the limitations of the maximum use of TPT should be conducted (12,13).
This study aimed to investigate the attitude and perceived challenges by PTs to implement TPT during the COVID-19 outbreak. More than 60% of the participants used the technology during the pandemic, which was about a third more than before the crisis. Also, physiotherapists acknowledged that they had little knowledge of the use of this technology. Moreover, they had the lowest knowledge on providing consults to their patients through TPT but had the highest level of knowledge on the TPT standards. The positive attitude of physiotherapists towards the use of TPT despite infrastructural barriers in the study is consistent with what was also conducted by Albahrouh and Buabbas in Kuwait (14).
According to researchers’ knowledge, Although PTs have positive views toward TPT, some negative PTs views towards TPT might be due to the fact that a large part of routine PT treatments in Iran is the use of electrotherapy agents and manual therapies that this TPT technology did not cover. Educational programs about the use of TPT in universities and colleges and through the Iranian physiotherapy association can help reduce the negative attitude and familiarize PTs with the practical and diverse aspects of TPT.
Based on the participants’ statements, the most significant obstacles were:
Lack of proper cultural acceptance to use this technology
Lack of high-speed internet access and high bandwidth
Lack of awareness and familiarity with this technology and its benefits
The lack of proper cultural acceptance for the use of TPT as a challenging factor to implement this technology in Iran has also been documented in studies conducted in other developing countries (15). To address this limitation, promoting awareness through mass media, such as newspapers, radio and TV programs, and the healthcare system is essential.
Lack of access to high-speed internet, which was reported by some PTs during this study, poses a great challenge to the effective use of TPT in Iran. This issue was also an obstacle in previous studies that examined the implantation of telemedicine in Iran (11). In previous studies and systematic reviews, the infrastructure constraints (such as poor internet connectivity, lack of user-friendly software, and network failure) were cited as the reasons for the lack of access and application of this technology globally (16,17). The obstacles were consistent with the previous report by Odele and Sarah Ibraheem from Nigeria (8). Still, that study was reported in different time zones and geographic areas, and at that time, the benefits of using the technology in critical situations were not well elaborated. In another study which was conducted by Aloyuni et al. in 2020, they found technical issues and costs related to implementing TPT settings as the main obstacles (18). A solution to overcome this barrier is the provision of necessary infrastructures by relevant organizations.
To increase the familiarity of both therapists and patients with TPT, it is recommended that part of the assessment, rehabilitation, or follow-up process be done with TPT so that over time patients and therapists would be more receptive to this technology. The lack of insurance coverage is another challenge in using TPT, which must be addressed by health policymakers and public and private insurance companies.
Our findings are also similar to those of Ullah et al., who found the majority of physiotherapists considered TPT as an essential service delivery method. Still, most of them did not use the technology (19). Therefore, the researchers concluded that establishing local standards and removing the obstacles, providing training courses, policy-making, and promoting the patients’ perception are the necessary aspects of the new technology. Educating Iranian physiotherapists on the use of tele-rehabilitation, including TPT and related courses, is essential.
This study was the first to be conducted about TPT during COVID-19 in Iran to provide preliminary information for healthcare decision-makers. This study had some limitations: 1) the quality of the TPT session is not considered. we just focused on the number of sessions. 2) it was an online survey, and maybe some physiotherapists don’t have any access to the internet. 3) the study was based on physiotherapist reports, and maybe they overestimated their abilities.
Conclusion
Based on the findings of this study, the Iranian government should intelligently work toward promoting TPT by drawing responsible health policies that address the identified challenges facing the implementation of TPT. The COVID-19 outbreak is not the last of its kind, and if we take advantage of the opportunities to set up and improve upon TPT, we can turn the idea from a crisis into a valuable opportunity for both the Iranian patients and the healthcare community. TPT can cause patients to use specialty services in specific aspects of physiotherapy and also provide physiotherapy services in rural and remote areas. Educating Iranian physiotherapists on the use of tele-rehabilitation (including TPT and related courses) and eliminating barriers is essential.
Acknowledgment
The authors wish to extend their gratitude to the management, faculty members, and staff of Shahid Beheshti University of Medical Sciences for their support and for the financial assistance provided that made the conduction of this study a reality.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Arzani P, Khalkhali Zavieh M, Khademi Kalantari Kh, Azadi F, Naim P. Tele-Physiotherapy in Iran: Perceived Challenges by Physiotherapists to Its Implementation in COVID19 Outbreak. Med J Islam Repub Iran. 2022 (5 Mar);36:17. https://doi.org/10.47176/mjiri.36.17
References
- 1.Khan S, Siddique R, Ali A, Xue M, Nabi G. Novel coronavirus, poor quarantine, and the risk of pandemic. J Hosp Infect. 2020;104(4):449–50. doi: 10.1016/j.jhin.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner NW, Ke R. The novel coronavirus, 2019-nCoV, is highly contagious and more infectious than initially estimated. arXiv preprint arXiv:200203268. 2020.
- 3. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis 2020;91(1):157. [DOI] [PMC free article] [PubMed]
- 4.Thunström L, Newbold SC, Finnoff D, Ashworth M, Shogren JF. The benefits and costs of using social distancing to flatten the curve for COVID-19. J Benefit Cost Anal. 2020;11(2):179–95. [Google Scholar]
- 5. Gourinchas PO. Flattening the pandemic and recession curves. Mitigating the COVID Economic Crisis: Act Fast and Do Whatever. CEPR 2020;31:57-62.
- 6.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arzani P, Zavieh MK, Khademi-Kalantari K, Baghban AA. Pulmonary rehabilitation and exercise therapy in a patient with COVID-19: A Case report. Med J Islam Repub Iran. 2020;34:106. doi: 10.34171/mjiri.34.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odole AC, Odunaiya NA, Ojo OD, Afolabi K. Tele-physiotherapy in Nigeria: perceived challenges by physiotherapists to its implementation. Int J Telemed Clin Pract. 2015;1(2):186–96. [Google Scholar]
- 9.Arzani P, Khalkhali Zavieh M, Khademi-Kalantari K, Akbarzadeh Baghban A. Opportunities and barriers for telerehabilitation during Coronavirus outbreak. Med J Islam Repub Iran. 2021;35(1):773–6. doi: 10.47176/mjiri.35.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Organization WH. Rehabilitation in health systems: guide for action. 2019.
- 11.Rezaei P, Maserrat E, Torab-Miandoab A. Specialist physicians’ perspectives about telemedicine and barriers to using it in Tabriz teaching hospitals Iran. South Med. J 2018;20(6):562–72. [Google Scholar]
- 12.Aderonmu JA. Emerging challenges in meeting physiotherapy needs during COVID-19 through telerehabilitation. Bull Fac Phys Ther. 2020;25(1):1–4. [Google Scholar]
- 13.Maggio MG, Maresca G, De Luca R, Stagnitti MC, Porcari B, Ferrera MC, et al. The growing use of virtual reality in cognitive rehabilitation: fact, fake or vision? A scoping review. J Natl Med AsSoc. 2019;111(4):457–63. doi: 10.1016/j.jnma.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Albahrouh SI, Buabbas AJ. Physiotherapists’ perception of and willingness to use telerehabilitation in Kuwait during the COVID-19 pandemic. BMC Med Inform Decis Mak. 2021;21(1):1–12. doi: 10.1186/s12911-021-01478-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leochico CFD, Espiritu AI, Ignacio SD, Mojica JAP. Challenges to the emergence of telerehabilitation in a developing country: a systematic review. Front Neurol. 2020;11:1007. doi: 10.3389/fneur.2020.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cottrell MA, Hill AJ, O'Leary SP, Raymer ME, Russell TG. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: a qualitative study. Musculoskelet Sci Pract. 2017;32:7–16. doi: 10.1016/j.msksp.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aloyuni S, Alharbi R, Kashoo F, Alqahtani M, Alanazi A, Alzhrani M, et al., editors. Knowledge, attitude, and barriers to telerehabilitation-based physical therapy practice in Saudi Arabia. Healthcare. 2020: Multidisciplinary Digital Publishing Institute. [DOI] [PMC free article] [PubMed]
- 19.Ullah S, Maghazil AM, Qureshi AZ, Tantawy S, Moukais IS, Aldajani AA. Knowledge and attitudes of rehabilitation professional toward telerehabilitation in Saudi Arabia: A cross-sectional survey. Telemed J E Health. 2021;27(5):587–91. doi: 10.1089/tmj.2020.0016. [DOI] [PubMed] [Google Scholar]


