Abstract
Purpose
The German population-based longitudinal COVID-19 andPsychological Health study monitors changes in health-related quality of life (HRQoL) and mental health of children and adolescents during the COVID-19 pandemic and identifies vulnerable groups.
Methods
A nationwide, population-based survey was conducted in May 2020 to June 2020 (Wave 1), December 2020 to January 2021 (Wave 2), and September 2021 to October 2021 (Wave 3). In total, n = 2,097 children and adolescents aged 7–17 years were investigated using measures to assess HRQoL (KIDSCREEN-10), mental health problems (SDQ), anxiety (SCARED), depressive symptoms(PHQ-2), and psychosomatic complaints(HBSC-SCL).
Results
The prevalence of low HRQoL increased from 15% prepandemic to 40% and 48% in Waves 1 and 2 and improved slightly to 35% in Wave 3 (all differences significant). Similarly, overall mental health problems increased from 18% prepandemic to 29% in Wave 1 and 31% in Wave 2 to 28% in Wave 3 (all differences significant, except Wave 3 vs. 2), anxiety increased from 15% prepandemic to 24% and 30% in Waves 1 and 2 and was still 27% in Wave 3. Depressive symptoms increased from 10% prepandemic to 11% and 15% in Waves 1 and 2 and were 11% in Wave 3. A group with low parental education, restricted living conditions, migration background, and parental mental health problems was at significantly increased risk of HRQoL and mental health impairments.
Discussion
The prevalence of low HRQoL, mental health problems, and anxiety has been elevated throughout the pandemic. Thus, mental health promotion, prevention, and intervention strategies need to be implemented to support adolescents–particularly those at risk.
Keywords: SARS-COV-2, Longitudinal study, Mental health, Health-related quality of life, Adolescents, Depression, Anxiety
Implications and Contribution.
As one of the first longitudinal population-based studies during the COVID-19 pandemic, the COPSY study reports a decline in mental health and health-related quality of life in the first year of the pandemic, followed by a slight improvement in autumn 2021, although the deterioration remains high compared to prepandemic data.
More than two years have passed since the COVID-19 pandemic started, fundamentally affecting young people worldwide. Fortunately, most children and adolescents display only mild acute symptoms of COVID-19 [1,2]. Yet, it is still unclear to what extent long COVID, a blanket term used for persistent symptoms following a COVID-19 infection characterized by fatigue, breathlessness, concentration problems, and depression, affects the youth. Prevalence rates reported in reviews are highly variable, but reach values up to 66% [3,4]. In addition to the physical impact of COVID-19, the pandemic poses many challenges to mental health.
Many studies report that for the majority of children and adolescents it was most challenging that social contacts were restricted [[5], [6], [7]], homeschooling was strenuous [[8], [9], [10], [11]], and the youth felt burdened by restrictions of their leisure activities [8]. Furthermore, studies show that physical activity decreased, while screen time [12], eating, and weight increased [[13], [14], [15]]. Experts also warn and empirical evidence demonstrates that maltreatment and violence against children and adolescents increased during the pandemic [16,17].
Reviews of cross-sectional studies [[18], [19], [20]] and a growing body of longitudinal studies indicate that health-related quality of life (HRQoL) of children and adolescents significantly decreased during the pandemic [7,21,22] and that mental health problems increased [21,[23], [24], [25], [26], [27], [28], [29], [30], [31]]. Reviews describe an average doubling of symptoms of anxiety (21%) and depression (25%) [20] and high prevalences of depression (29%), anxiety (26%), sleep disorders (44%), and post-traumatic stress symptoms (48%) [18]. However, some studies report mixed results [[32], [33], [34]] or no difference between prepandemic and pandemic data [35,36]. Longitudinal studies covering both the prepandemic period and long periods during the pandemic are needed to substantiate and differentiate our growing knowledge about the effects of the pandemic on the mental health of children and adolescents [37,38].
The German CO VID-19 and Psy chological Health (COPSY) study is one of the first population-based longitudinal studies to monitor HRQoL and mental health in children and adolescents during the COVID-19 pandemic, covering three waves of data collection so far and having the advantage of prepandemic population-based data being available for comparison (Behaviour and Well-being of Children and Adolescents in Germany [BELLA] study [39] and Health Behaviour in School-aged Children [HBSC] study [40]). The aim of this study is to examine the course of mental health and HRQoL in children and adolescents during the pandemic. We also aim to identify groups vulnerable to deteriorating mental health and HRQoL. The following research questions are to be answered:
-
(1)
How did child and adolescent HRQoL and mental health change during Waves 1 to 3 of the COPSY study and compared with prepandemic data? We expected an increase in the prevalence of low HRQoL and mental health problems from prepandemic data to Wave 1 due to lockdown measures and restrictions, a slight increase between Wave 1 and Wave 2 due to ongoing restrictions, and improvements from Wave 2 to Wave 3 due to low infection rates, vaccination, and a loosening of restrictions in summer/autumn 2021.
-
(2)
Are (theoretically and empirically derived) risk factors associated with lower HRQoL and mental health during the pandemic? We expected a certain constellation of socioeconomic and psychosocial factors to be associated with lower HRQoL and mental health in children and adolescents across the different phases of the pandemic.
Methods
Study design and sample
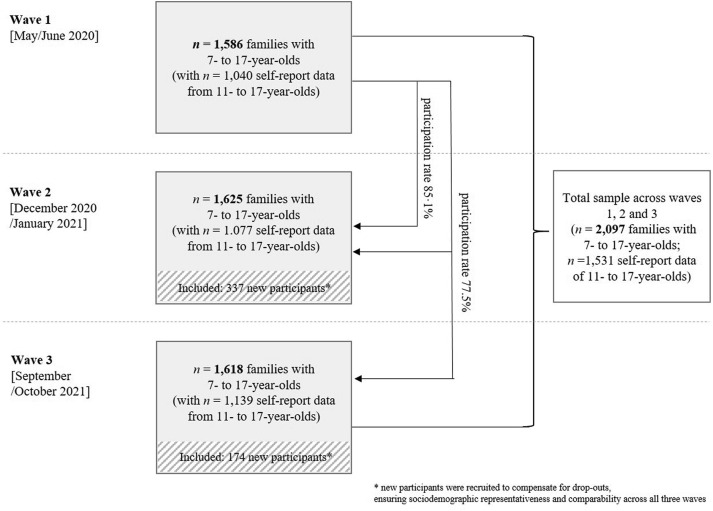
The COPSY study is a population-based longitudinal study on child and adolescent mental health during the COVID-19 pandemic in Germany. The survey was conducted in three waves. Wave 1 (May 2020 to June 2020) took place when Germany was under a partial lockdown, with schools and leisure facilities mostly closed. Wave 2 (December 2020 to January 2021) was conducted while the second wave of the pandemic was ongoing and the country was under a nationwide lockdown. Wave 3 (September 2021 to October 2021) was undertaken after a summer with low infection rates and which led to countrywide restrictions being loosened. To ensure that the sample reflected the sociodemographic characteristics of the German population, families were recruited from an online panel using quota sampling. Participating families were reinvited at each follow-up of the COPSY study and new families were recruited to compensate for dropouts, ensuring sociodemographic representativeness and comparability across all three waves. Parent-reported data were collected from children and adolescents aged 7–17 years, and additionally self-reported data were gathered from children and adolescents aged 11–17 years. Finally, n = 2,097 families participated in at least one measuring point of the COPSY study, including n = 1,531 self-reports for 11–17 year olds and n = 2,097 parent-reports for 7–17 year olds. For an overview of the COPSY sample, see Figure 1 .
Figure 1.
Numbers of participating families and children in Wave 1, Wave 2, and Wave 3 of the COPSY study.
In Wave 1, n = 1,040 self-reports and n = 1,586 parent-reports provided data; in Wave 2, n = 1,077 self-reports and n = 1,625 parent-reports provided data with a retention rate from Wave 1 to Wave 2 of 85%. The design and findings of the first two waves have been described elsewhere [3,31]. In Wave 3, n = 1,139 self-reports and n = 1,618 parent-reports provided data (see Figure 1).
In total, n = 806 families participated in all three waves of the study with a longitudinal participation rate of 77.5%. Parents participating in all three waves were on average 2.3 years older (d = 0.31) and were more likely to have a lower level of education (20.5% vs. 15.2%; V = 0.07) compared with those who only participated in one or two waves. No other significant differences in sociodemographic or mental health-related variables were found. The data sets from all three waves of the COPSY study were each weighted to correspond to the sociodemographic characteristics of the German population (according to the 2018 Microcensus). The COPSY study was approved by the Local Psychological Ethics Committee (LPEK-0151) and the Commissioner for Data Protection of the University of Hamburg.
Prepandemic German population-based data were used for comparison [39] from the longitudinal BELLA study, conducted between 2014 and 2017 providing data of n = 1,020 participants (aged 11–17 years) on mental health and HRQoL; the German HBSC study [40] conducted between 2017 and 2018 provides data on psychosomatic complaints of n = 1,073 participants (aged 11, 13, and 15 years).
Measures
Sociodemographics
The survey included questions on age, gender, education, living space, and migration background.
COVID-19 burden
The survey contained a question as to whether there had been a COVID-19 infection in the family, whether the adolescent had been infected, whether a family member had died of COVID-19, and two self-developed questions asked about the perceived burden of the pandemic [5].
Quality of life and mental health in children and adolescents
Internationally established and validated questionnaires were administered. HRQoL was assessed using the self-reported KIDSCREEN-10 Index [[41], [42]]. Children and adolescents were classified as having low, normal, or high HRQoL using reference data from the national BELLA study (normal HRQoL was defined as MBELLA+/-1SDBELLA). The Strengths and Difficulties Questionnaire (SDQ) [43] provides a total difficulties score across 20 items and four subscale scores on emotional problems, conduct problems, hyperactivity, and peer problems. Higher scores indicate more severe problems. Cutoffs served to differentiate between participants with versus without mental health problems (noticeable/abnormal and borderline vs. normal) [44]. Anxiety was assessed using the general anxiety subscale of the Screen for Child Anxiety Related Disorders [45]. A sum score of the nine items was calculated, with higher scores indicating more severe anxiety. Groups of participants with versus without anxiety were created using the established cutoff [45]. Depressive symptoms were measured using the Patient Health Questionnaire [46,47] with its two items. A higher sum score indicates more severe depressive symptoms. A validated cutoff was applied to categorize participants with and those without noticeable depressive symptoms [46]. Furthermore, the self-reported HBSC symptom checklist [48] was administered to measure the frequencies of psychosomatic complaints during the past week. Participants were divided into groups of subjects who experienced each psychosomatic symptom at least once per week versus those who experienced it less frequently. The KIDSCREEN-10 Index, the SDQ, and the Screen for Child Anxiety Related Disorders were also applied in the BELLA study, and the HBSC-SCL was administered in the HBSC study, thus allowing comparisons with the COPSY data.
Data analysis–changes in HRQoL and mental health
First, the reported burden of the pandemic on children and adolescents was compared across the three COPSY waves. Second, the proportion of youth displaying impaired HRQoL, mental health problems, anxiety, depressive symptoms, and psychosomatic complaints was compared across all measurement points. Age- and gender-adjusted proportions were calculated using logistic regression models for each outcome. Data from the BELLA and HBSC studies were used to compare HRQoL and mental health outcomes with prepandemic reference data. Chi-square tests and effect sizes (Phi coefficient φ resp. Cramer's V, with .10 indicating a small, .30 a medium, and .50 a strong effect) were calculated for comparisons across the waves and for group comparisons. Gender differences were expressed as risk ratios (RRs) for girls. The chi-square tests as well as the φ and V statistics for comparisons across the COPSY waves do not take into account that the majority of measurements represent repeated measures of the same respondents. This led to lower statistical power in order to detect differences across the COPSY waves.
Furthermore, the individual stability and variability of HRQoL classification over the course of the pandemic (trajectories) were analyzed by examining how respondents with low, medium, or high HRQoL in Wave 1 were classified in Waves 2 and 3.
Prior to analyzing the data, a power analysis was conducted using G-Power (Version 3.1). The minimum sample size based on a statistical significance of p (α) < .05 and a power of p (1-ß) = 0.8 for a medium effect (w = 0.3) between waves according to age groups (7–10 years, 11–13 years, 14–17 years) and female versus male was n = 88.
Data analysis–risk factors for lower HRQoL and mental health
To answer the second research question, it was examined whether a group of children are at higher risk of being impaired by the pandemic. Based on previous empirical evidence [5], a number of five risk factors (i.e., parental education, migration background, living space, parental mental health problems, and parental pandemic burden) were identified to define a risk group of vulnerable children and adolescents. Children were assigned to the risk group if their parents had a low level of education and either a migration background or lived in close quarters (<20 m2 living space/person). Furthermore, children were assigned to the risk group if their parents had mental health problems or were extremely burdened by the pandemic. In total, n = 365 (17.2%) children and adolescents were assigned to the risk group. Children who did not meet the inclusion criteria of risk factors were defined as not risk group. Using logistic regression analyses, this risk group was examined for HRQoL impairments and mental health problems in each of the three waves using age and gender as covariates. In an additional logistic regression analysis, it was tested whether the schooling situation and the number of social contacts outside the family were associated with low HRQoL. These analyses were controlled for age and gender. Effects were described in terms of odds ratios (ORs). All analyses were performed using SPSS Version 26.
Results
Sociodemographics
Overall, n = 2,097 families with children and adolescents aged 7–17 years old (mean = 13.21; standard deviation = 3.30; 50.3% female) participated in the COPSY study (parent proxy reports). Of those, n = 1,531 children and adolescents aged 11–17 years old (mean = 14.82; standard deviation = 2.23; 53.9% female) completed the self-report survey. Sociodemographic characteristics are summarized in Table 1 .
Table 1.
Sociodemographic characteristics of the COPSY sample
| Children and adolescents aged 7–17 years (parent reports) (n = 2,097) |
Children and adolescents aged 11–17 years (self-reports) (n = 1,531) |
|||
|---|---|---|---|---|
| n (%) | M (SD) | n (%) | M (SD) | |
| Age | 13.21 (3.30) | 14.82 (2.23) | ||
| 7–10 years | 566 (27.0) | - | ||
| 11–13 years | 470 (22.4) | 470 (30.7) | ||
| 14–17 yearsa | 1,061 (50.6) | 1,061 (69.3) | ||
| Gender | ||||
| Male | 1,030 (49.1) | 495 (46.0) | ||
| Female | 1,055 (50.3) | 580 (53.9) | ||
| Other | 10 (0.5) | 2 (0.2) | ||
| Age of the parent | 44.41 (7.44) | 45.93 (7.19) | ||
| Migration background | ||||
| No | 1,741 (83.0) | 1,274 (83.2) | ||
| Yes | 356 (17.0) | 257 (16.8) | ||
| Parental education | ||||
| Low | 371 (17.7) | 271 (17.7) | ||
| Medium | 1,216 (58.0) | 868 (56.7) | ||
| High | 493 (23.5) | 379 (24.8) | ||
| No information | 17 (0.8) | 13 (0.8) | ||
| Single parent | ||||
| No | 1,678 (80.0) | 1,211 (79.1) | ||
| Yes | 419 (20.0) | 320 (20.9) | ||
| Occupational status | ||||
| Full-time employed | 1,069 (51.0) | 808 (52.8) | ||
| Part-time employed | 616 (29.4) | 433 (28.3) | ||
| Self-employed | 81 (3.9) | 60 (3.9) | ||
| Other employment | 40 (1.9) | 28 (1.8) | ||
| Stay-at-home parent | 142 (6.8) | 92 (6.0) | ||
| Retiree/pensioner | 52 (2.5) | 44 (2.9) | ||
| On parental leave | 31 (1.5) | 18 (1.2) | ||
| Unemployed | 66 (3.1) | 48 (3.1) | ||
| COVID-19 infection | ||||
| A family member has been infected | 361 (17.2) | 259 (16.3) | ||
| The child has been infected | 78 (3.7) | 53 (3.5) | ||
| A relative has died of COVID-19 | 140 (6.7) | 106 (6.9) | ||
Note. Unweighted data.
COPSY = COVID-19 and Psychological Health; M = mean; SD = standard deviation.
n = 148 adolescents had already turned 18 when they participated in the survey but were included in the age group of 14- to 17-year-olds.
Changes in HRQoL during the pandemic
70.3% of children and adolescents aged 11–17 years reported being burdened by the pandemic at Wave 1, 82.8% at Wave 2 (p < .001; φ = 0.15), and 82.0% at Wave 3 (p = .522; φ = 0.014).
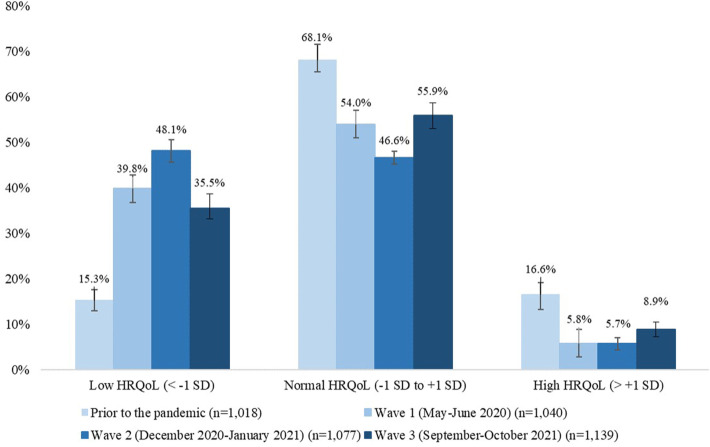
Before the pandemic, only 15.3% of children and adolescents reported low HRQoL. This increased to 39.8% at Wave 1 (p < .001; φ = 0.27), followed by a further increase to 48.1% at Wave 2 (p < .001; φ = 0.08), and then a decrease at Wave 3 to 35.5% (p < .001; φ = .13). Thus, the prevalence of low HRQoL at Wave 3 is still more than twice as high as the prepandemic rate (see Figure 2 ). An analysis stratified by gender revealed that girls had a 1.2 to 2 fold higher risk of low HRQoL compared to boys (RR ranged between 1.2 and 2). Half of the youth (54.0%) reported medium HRQoL at the beginning of the pandemic, with the majority of them remaining there across all waves (65.7%–72.1%). Of those who reported high HRQoL at the start of the pandemic, only a third (29%) maintained their high HRQoL over the course of the study. The majority of those who initially reported low HRQoL (57%–76%) continued to report low HRQoL during the latter Waves 2 and 3. All reported percentages were adjusted for age and gender.
Figure 2.
Percentages of children and adolescents with low, normal, and high health-related quality of life measured prior to the COVID-19 pandemic (BELLA study), in Wave 1, Wave 2, and Wave 3 of the COPSY study.
Changes in mental health during the pandemic
Prior to the pandemic, less than one fifth (17.6%) of all children and adolescents aged 7–17 years had overall mental health problems. This number rose to 28.8% in Wave 1 and 30.6% in Wave 2. In Wave 3, there was a slight but nonsignificant decrease in mental health problems to 28.0%, which is still substantially higher than before the pandemic.
While emotional problems, hyperactivity, conduct problems, and peer problems increased from prepandemic to pandemic data of Wave 1, conduct and peer problems continued to increase at Wave 2. Hyperactivity decreased at Wave 2, followed by an additional small decrease at Wave 3. All subscales at Wave 3 were higher compared to prepandemic data. Children and adolescents had continuously increasing emotional problems over the course of the pandemic (see Table 2 ).
Table 2.
Mental health problems and anxiety and depressive symptoms in children and adolescents prior to the COVID-19 pandemic (BELLA study), and in Waves 1, 2, and 3 of the COPSY study
| BELLA Prepandemic (n = 1,552) |
COPSY Wave 1 (n = 1,586) |
COPSY Wave 2 (n = 1,625) |
COPSY Wave 3 (n = 1,618) |
BELLA versus COPSY Wave 1 |
BELLA versus COPSY Wave 2 |
COPSY Wave 1 versus Wave 2 |
COPSY Wave 2 versus Wave 3 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | p-value | Effect size (φ) | p-value | Effect size (φ) | p-value | Effect size (φ) | p-value | Effect size (φ) | |
| Mental health problems (total) | ||||||||||||
| Normal | 82.4 | 71.2 | 69.4 | 72.0 | ||||||||
| Borderline/abnormal | 17.6 | 28.8 | 30.6 | 28.0 | < .001 | 0.13 | < .001 | 0.15 | .264 | .104 | ||
| Emotional problems | ||||||||||||
| Normal | 83.6 | 80.0 | 76.8 | 74.6 | ||||||||
| Borderline/abnormal | 16.4 | 20.0 | 23.2 | 25.4 | .009 | 0.05 | < .001 | 0.09 | .028 | 0.04 | .144 | |
| Conduct problems | ||||||||||||
| Normal | 86.9 | 81.7 | 81.3 | 82.2 | ||||||||
| Borderline/abnormal | 13.1 | 18.3 | 18.7 | 17.8 | <.001 | 0.07 | < .001 | 0.08 | .770 | .507 | ||
| Hyperactivity | ||||||||||||
| Normal | 87.2 | 78.1 | 80.3 | 80.9 | ||||||||
| Borderline/abnormal | 12.8 | 21.9 | 19.7 | 19.1 | < .001 | 0.12 | < .001 | 0.09 | .125 | .666 | ||
| Peer problems | ||||||||||||
| Normal | 88.6 | 78.7 | 73.8 | 76.2 | ||||||||
| Borderline/abnormal | 11.4 | 21.3 | 26.2 | 23.8 | < .001 | 0.13 | < .001 | 0.19 | .001 | 0.06 | .115 | |
| Anxiety symptoms | (n = 1,018) | (n = 1,040) | (n = 1,077) | (n = 1,139) | ||||||||
| No | 85.1 | 76.4 | 69.9 | 73.8 | ||||||||
| Yes | 14.9 | 23.6 | 30.1 | 26.2 | < .001 | 0.12 | < .001 | 0.18 | .002 | 0.07 | .086 | |
| Depressive symptoms | (n = 1,018) | (n = 1,040) | (n = 1,077) | (n = 1,139) | ||||||||
| No | 90.0 | 88.9 | 85.1 | 88.6 | ||||||||
| Yes | 10.0 | 11.1 | 14.9 | 11.4 | .320 | < .001 | 0.08 | .012 | 0.05 | .007 | 0.06 | |
Note. Weighted data, percentages adjusted for age and gender. Normal versus borderline/abnormal: Groups were compared based on the German cutoffs of the SDQ. p-values indicating significant differences (p ≤ .050) and effect sizes (Phi coefficient φ) indicating small effects (φ ≥ 0.10) are printed in bold type. Effect sizes are only reported for significant differences.
BELLA = Behaviour and Well-being of Children and Adolescents; COPSY = COVID-19 and Psychological Health; SDQ = Strengths and Difficulties Questionnaire
Children and adolescents aged 11–17 years reported more symptoms of anxiety during the first wave (23.6%) than before the pandemic (14.9%). Anxiety further increased in Wave 2 (30.1%), while in Wave 3 anxiety levels decreased slightly to 26.2%, but were still higher compared with prepandemic times (see Table 2). All reported percentages were adjusted for age and gender.
Depressive symptoms in adolescents aged 11–17 years slightly and nonsignificantly increased from prepandemic data to Wave 1 (10.0%–11.1%), the increase reached significance in Wave 2 (14.9%), followed by a significant decrease in Wave 3 (11.4%). The p-values and effect sizes are reported in Table 2, most reported changes were negligible to small.
Similarly to the gender difference in HRQoL, girls were more likely to report anxiety (RR ranged between 1.4 and 2.1) and more likely to report depressive symptoms (RR ranged between 1.4 and 1.9).
Changes in psychosomatic complaints
Psychosomatic complaints in adolescents aged 11–17 years increased during the pandemic as reported for Waves 1 and 2 elsewhere [5]. In Wave 3, the prevalence further increased for stomachaches (39.2%; p = .169; φ = 0.03) and headaches (48.7%; p = .005; φ = 0.06), and remained high for irritability (57.0%), sleeping problems (46.0%), and feeling low (41.2%). In Wave 3, all psychosomatic complaints were more prevalent compared to prepandemic and Wave 1 data (see Figure A1). Girls were at a higher risk of psychosomatic complaints, in particular with regard to having headaches (RR between 1.2 and 1.9) and feeling low (RR between 1.3 and 1.9).
Children and adolescents at risk for impaired HRQoL and mental health
At all three waves, children and adolescents of the risk group (for definition, see section Data analysis–risk factors for lower HRQoL and mental health) had a higher risk of experiencing low HRQoL (ORs ranged from 2.1 to 2.7), mental health problems (ORs ranged from 2.7 to 3.0), anxiety symptoms (ORs ranged from 1.7 to 2.2), and depressive symptoms compared with their peers (ORs ranged from 2.3 to 4.1). The prevalence of being burdened by the pandemic, having low HRQoL, and overall mental health problems was higher for the risk group across all 3 waves (see Figure A2). Regarding age- and gender-specific differences, adolescents aged 14–17 years had a lower risk of mental health problems at Waves 2 and 3 compared with 7- to 10-year-olds (ORs ranged from 0.3 to 0.6). Furthermore, 14- to 17-year-olds had a lower risk of anxiety at Waves 1 and 2 compared with 11- to 13-year-olds (ORs ranged from 0.5 to 0.6, see Table 3 ).
Table 3.
Associations between belonging to a risk group and low HRQoL, mental health problems, anxiety and depressive symptoms measured using odds ratios for 11- to 17-year-olds across Waves 1, 2, and 3 of the COPSY study
| Low HRQoL (KIDSCREEN-10) | Wave 1 |
Wave 2 |
Wave 3 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Risk groupa | 2.079 (1.465; 2.950) | 2.653 (1.894; 3.717) | 2.364 (1.722; 3.245) |
| Female | 1.418 (0.878; 2.290) | 1.003 (0.648; 1.551) | 1.008 (0.668; 1.519) |
| 14–17 years | 0.917 (0.610; 1.378) | 1.211 (0.842; 1.742) | 0.921 (0.643; 1.319) |
| Female 14–17 years | 0.954 (0.542; 1.679) | 1.152 (0.680; 1.950) | 1.448 (0.870; 2.413) |
| Nagelkerke's Pseudo-R2 | 0.033 | 0.048 | 0.042 |
| Hosmer–Lemeshow test of fit |
p = .776 |
p = .983 |
p = .571 |
| Mental health problems (SDQ) |
Wave 1 |
Wave 2 |
Wave 3 |
| OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Risk groupa | 2.731 (2.012; 3.707) | 2.764 (2.080; 3.674) | 3.049 (2.278; 4.081) |
| Female | 0.594 (0.375; 0.940) | 0.640 (0.406; 1.007) | 0.817 (0.493; 1.354) |
| 11–13 years | 0.716 (0.463; 1.106) | 0.771 (0.508; 1.170) | 1.335 (0.852; 2.091) |
| 14–17 years | 0.318 (0.207; 0.488) | 0.412 (0.274; 0.618) | 0.621 (0.401; 0.962) |
| Female 11–13 years | 1.476 (0.770; 2.828) | 1.016 (0.532; 1.939) | 0.748 (0.377; 1.485) |
| Female 14–17 years | 1.365 (0.706; 2.639) | 1.653 (0.906; 3.018) | 1.235 (0.643; 2.373) |
| Nagelkerke's Pseudo-R2 | 0.095 | 0.071 | 0.071 |
| Hosmer–Lemeshow test of fit |
p = .854 |
p = .857 |
p = .428 |
| Generalized anxiety (SCARED) |
Wave 1 |
Wave 2 |
Wave 3 |
| OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Risk groupa | 2.183 (1.506; 3.163) | 1.687 (1.206; 2.361) | 1.297 (0.923; 1.823) |
| Female | 1.088 (0.639; 1.853) | 0.593 (0.367; 0.957) | 1.558 (1.021; 2.380) |
| 14–17 years | 0.545 (0.339; 0.878) | 0.509 (0.342; 0.759) | 0.769 (0.518; 1.141) |
| Female 14–17 years | 2.113 (1.112; 4.015) | 4.424 (2.472; 7.917) | 1.084 (0.633; 1.858) |
| Nagelkerke's Pseudo-R2 | 0.058 | 0.065 | 0.024 |
| Hosmer–Lemeshow test of fit |
p = .858 |
p = .994 |
p = .706 |
| Depressive symptoms (PHQ-2) |
Wave 1 |
Wave 2 |
Wave 3 |
| OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Risk groupa | 3.684 (2.385; 5.690) | 4.070 (2.796; 5.925) | 2.333 (1.534; 3.547) |
| Female | 1.489 (0.720; 3.080) | 0.506 (0.250; 1.026) | 0.971 (0.494; 1.907) |
| 14–17 years | 0.773 (0.393; 1.519) | 0.878 (0.519; 1.485) | 1.015 (0.565; 1.824) |
| Female 14–17 years | 1.095 (0.457; 2.627) | 3.251 (1.436; 7.358) | 1.899 (0.844; 4.273) |
| Nagelkerke's Pseudo-R2 | 0.074 | 0.104 | 0.044 |
| Hosmer–Lemeshow test of fit | p = .957 | p = .870 | p = .729 |
CI = confidence interval; HRQoL = health-related quality of life; OR = odds ratio; SDQ = Strengths and Difficulties Questionnaire; SCARED = Screen for Child Anxiety Related Disorders; PHQ-2 = Patient Health Questionnaire.
Note. Risk groups were predefined as children/adolescents with low parental education and/or migration status and/or confined living conditions and/or previous parental mental illness. Numbers in bold indicate statistically significant results. The reference group for all analyses except SDQ was boys aged 11–13 years not belonging to the risk group. For the SDQ analyses, the reference group was boys aged 7–10 years not belonging to the risk group.
The potential role of homeschooling and reduced social contacts for impaired HRQoL
In all three waves, reduction of social contacts outside the family was associated with a higher risk of low HRQoL (ORs ranged from 2.3 to 5.6). Schooling mainly at home was associated with ORs between 1.2 and 3.2 for low HRQoL. The ORs for schooling only sometimes/irregularly at school ranged from 0.8 to 1.5.
Discussion
The results of the German population-based longitudinal COPSY study indicate a significant increase in low HRQoL and mental health problems at the start of the pandemic compared with prepandemic levels. HRQoL impairments and mental health problems continuously increased in Waves 1 (spring 2020) and 2 (winter 2020/21), followed by a slight improvement in Wave 3 (autumn 2021). However, the level of mental health deterioration remains high and almost double that before the pandemic. The slight improvements in adolescent HRQoL and mental health in Wave 3 could be explained by the low infection rates, vaccination, and the loosening of restrictions in Germany in autumn 2021.
The initial drastic decrease in HRQoL at the start of the pandemic has been replicated by two further German studies, which also used the KIDSCREEN-10 prior to and during the pandemic [6,7]. Regarding mental health problems, internalizing problems (such as emotional problems) remained high at Wave 3, while externalizing problems (such as hyperactivity) significantly decreased. This may have been the result of children and adolescents having had more freedom to move around in autumn 2021 compared with during the lockdowns. These results are largely in line with studies from the United States [30], the United Kingdom [31], and Japan [28] that also used the SDQ. Minor differences in prevalence rates between the studies may be due to differing data collection times and country restrictions. We found that reduced social contacts and school-closing or irregular schooling were associated with lower HRQoL. The increase in social contacts and schooling from Wave 2 to 3 thus could also explain the decrease in low HRQoL from Wave 2 to 3.
As previously reported [5,21], the COPSY study surprisingly did not find a significant rise in depression levels from prepandemic to Wave 1 data, but a significant peak of depressive symptoms at Wave 2, while depressive symptoms decreased again at Wave 3. Depression levels across all waves (10%–15%) are interestingly below the ones reported in two meta-analyses by Racine et al. (25%) [20] and Ma et al. (29%) [18]. This may be because those meta-analyses primarily summarize Asian studies with high infection rates and stricter lockdown measures.
In terms of gender differences, we found that a higher proportion of girls reported low HRQoL, anxiety, depressive symptoms, and psychosomatic complaints both before and during the pandemic. Further in-depth analyses on gender-specific risks and coping strategies are needed.
In addition, the findings of the COPSY study suggest that a group of socially disadvantaged children and adolescents as well as children of parents with mental health problems are at a particularly high risk of experiencing low HRQoL, mental health problems, and depressive symptoms during the pandemic. This is in line with previous COPSY results [5,21] as well as other studies of risk factors [29,33]. Information about these risk factors could help to screen for mentally burdened children and adolescents and develop targeted, low-threshold prevention and intervention programs to reduce social inequalities in mental health. Further in-depth analyses using multivariate and multilevel statistical models and including additional risk and resource factors will be carried out and published in a separate article.
The strengths of the COPSY study include its longitudinal design, the large population-based sample and the coverage of a long time span across the pandemic; the availability of nationally representative, prepandemic data sets for comparison; and the administration of well-established instruments. The limitations of the study include the fact that the sample was drawn by matching data from the 2018 German Microcensus, meaning the findings may not be generalizable to other countries; the survey was conducted using an online panel with incentives, which may have influenced participation; due to pandemic restrictions highly burdened families or children with mental disorders might have been less likely to participate in the survey; due to the online administration, only families with Internet access could participate. Lastly, the study does not allow any causal conclusions to be drawn about what exactly accounts for the main findings.
Overall, the third wave of the COPSY study demonstrates lingering impaired HRQoL and mental health for a substantial proportion of children, particularly the at-risk groups, with only slight improvements in mental health in autumn 2021. Further waves of the COPSY study are underway to further examine mental health trajectories through multivariate statistical panel model analysis and in-depth subgroup analysis. Research is needed that investigates the pandemic-related causes of low HRQoL and monitors mental health trajectories in more detail. In particular, we call for research that is comparable, using the same measures, comparable time intervals, designs and methods, and capturing infection rates, and policy responses to the pandemic for cross- and within-country comparisons. This is crucial as it will lead to an understanding of national and regional differences in child and adolescent mental health trajectories during the pandemic, and clarify the effect of different policy responses to the COVID-19 pandemic on these key variables [49].
It is also imperative that awareness for children and adolescents in need of mental support be increased in policy, educational, and health care settings. Facing challenges like the pandemic, policymakers need to pave the way for better screening for at-risk children and adolescents, and support them through prevention and intervention programs that might mitigate the effects the pandemic appears to have on them.
Acknowledgments
The authors would like to thank all the children, adolescents, and their parents who participated in this study for their time and involvement. The corresponding author affirms that she has listed everyone who contributed significantly to the work in the Acknowledgments.
Footnotes
Conflicts of interest: There is no conflict of interest, real and perceived, for all named authors.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2022.06.022.
Funding Sources
The COPSY study was funded by the Kroschke Child Foundation and the Fritz and Hildegard Berg Foundation. The funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Supplementary Data
References
- 1.Howard-Jones A.R., Burgner D.P., Crawford N.W., et al. COVID-19 in children. II: Pathogenesis, disease spectrum and management. J Paediatrics Child Health. 2021;18:2470. doi: 10.1111/jpc.15811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castagnoli R., Votto M., Licari A., et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: A systematic review. JAMA Pediatr. 2020;174:882–889. doi: 10.1001/jamapediatrics.2020.1467. [DOI] [PubMed] [Google Scholar]
- 3.Zimmermann P., Pittet L.F., Curtis N. How common is long COVID in children and adolescents? Pediatr Infect Dis J. 2021;40:e482–e487. doi: 10.1097/INF.0000000000003328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michelen M., Manoharan L., Elkheir N., et al. Characterising long COVID: A living systematic review. BMJ Glob Health. 2021;6:e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ravens-Sieberer U., Kaman A., Erhart M., et al. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. Eur Child Adolesc Psychiatry. 2021;12:1–4. doi: 10.1007/s00787-021-01889-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christner N., Essler S., Hazzam A., Paulus M. Children’s psychological well-being and problem behavior during the COVID-19 pandemic: An online study during the lockdown period in Germany. PLOS ONE. 2021;16:e0253473. doi: 10.1371/journal.pone.0253473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vogel M., Meigen C., Sobek C., et al. Well-being and COVID-19-related worries of German children and adolescents: A longitudinal study from pre-COVID to the end of lockdown in spring 2020. JCPP Adv. 2021;1:e12004. doi: 10.1111/jcv2.12004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poulain T., Meigen C., Sobek C., et al. Loss of childcare and classroom teaching during the covid-19-related lockdown in spring 2020: A longitudinal study on consequences on leisure behavior and schoolwork at home. Plos one. 2021;16:e0247949. doi: 10.1371/journal.pone.0247949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zinn S., Bayer M. Time spent on school-related activities at home during the pandemic: A longitudinal analysis of social group inequality among secondary school students. Front Psychol. 2021:3493. doi: 10.3389/fpsyg.2021.705107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Larsen L., Helland M.S., Holt T. The impact of school closure and social isolation on children in vulnerable families during COVID-19: A focus on children’s reactions. Eur child Adolesc Psychiatry. 2021;26:1–11. doi: 10.1007/s00787-021-01758-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spitzer M. Mediennutzung in Zeiten von Corona. Nervenheilkunde. 2020;39:698–703. [Google Scholar]
- 13.Jarnig G., Jaunig J., van Poppel M.N. Association of COVID-19 mitigation measures with changes in cardiorespiratory fitness and body mass index among children aged 7 to 10 years in Austria. JAMA Netw Open. 2021;4:e2121675. doi: 10.1001/jamanetworkopen.2021.21675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lange S.J., Kompaniyets L., Freedman D.S., et al. Longitudinal Trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 Years—United States, 2018–2020. Morbidity Mortality Weekly Rep. 2021;70:1278. doi: 10.15585/mmwr.mm7037a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pietrobelli A., Pecoraro L., Ferruzzi A., et al. Effects of COVID-19 lockdown on Lifestyle Behaviors in children with Obesity living in Verona, Italy: A longitudinal study. Obesity (Silver Spring) 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cappa C., Jijon I. COVID-19 and violence against children: A review of early studies. Child Abuse Neglect. 2021;116:105053. doi: 10.1016/j.chiabu.2021.105053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kourti A., Stavridou A., Panagouli E., et al. Domestic violence during the CoViD-19 pandemic: A systematic review. Trauma Violence Abuse. 2021;17 doi: 10.1177/15248380211038690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma L., Mazidi M., Li K., et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imran N., Aamer I., Sharif M.I., et al. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci. 2020;36:1106–1116. doi: 10.12669/pjms.36.5.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Racine N., McArthur B.A., Cooke J.E., et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ravens-Sieberer U., Kaman A., Erhart M., et al. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry. 2021;31:879–889. doi: 10.1007/s00787-021-01726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ravens-Sieberer U., Kaman A., Otto C., et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117:828–829. doi: 10.3238/arztebl.2020.0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hawes M.T., Szenczy A.K., Olino T.M., et al. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Res. 2021;298:113778. doi: 10.1016/j.psychres.2021.113778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hussong A.M., Midgette A.J., Thomas T.E., et al. Coping and mental health in early adolescence during COVID-19. Res Child Adolesc Psychopathol. 2021;49:1113–1123. doi: 10.1007/s10802-021-00821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paschke K., Arnaud N., Austermann M.I., Thomasius R. Risk factors for prospective increase in psychological stress during COVID-19 lockdown in a representative sample of adolescents and their parents. BJPsych open. 2021;7 doi: 10.1192/bjo.2021.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bignardi G., Dalmaijer E.S., Anwyl-Irvine A.L., et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child. 2020;106:791–797. doi: 10.1136/archdischild-2020-320372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conti E., Sgandurra G., De Nicola G., et al. Behavioural and emotional changes during covid-19 lockdown in an Italian paediatric population with neurologic and psychiatric disorders. Brain Sci. 2020;10:918. doi: 10.3390/brainsci10120918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takahashi F., Honda H. Prevalence of clinical-level emotional/behavioral problems in schoolchildren during the coronavirus disease 2019 pandemic in Japan: A prospective cohort study. JCPP Adv. 2021;1:e12007. doi: 10.1111/jcv2.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hafstad G.S., Sætren S.S., Wentzel-Larsen T., Augusti E.-M. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak–A prospective population-based study of teenagers in Norway. Lancet Reg Health-Europe. 2021;5:100093. doi: 10.1016/j.lanepe.2021.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosen M.L., Rodman A.M., Kasparek S.W., et al. Promoting youth mental health during the COVID-19 pandemic: A longitudinal study. PloS one. 2021;16:e0255294. doi: 10.1371/journal.pone.0255294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waite P., Pearcey S., Shum A., et al. How did the mental health symptoms of children and adolescents change over early lockdown during the COVID-19 pandemic in the UK. JCPP Adv. 2021;1:e12009. doi: 10.1111/jcv2.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Achterberg M., Dobbelaar S., Boer O.D., Crone E.A. Perceived stress as mediator for longitudinal effects of the COVID-19 lockdown on wellbeing of parents and children. Sci Rep. 2021;11 doi: 10.1038/s41598-021-81720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu Y., Qian Y. COVID-19 and adolescent mental health in the United Kingdom. J Adolesc Health. 2021;69:26–32. doi: 10.1016/j.jadohealth.2021.04.005. [DOI] [PubMed] [Google Scholar]
- 34.Berry A., Burke T., Carr A. The impact of the first wave of the COVID-19 pandemic on parents of children with Externalising difficulties in Ireland: A longitudinal cohort study. Int J Clin Pract. 2021;75 doi: 10.1111/ijcp.14941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vira E.G., Skoog T. Swedish middle school students’ psychosocial well-being during the COVID-19 pandemic: A longitudinal study. SSM-Population Health. 2021;16:100942. doi: 10.1016/j.ssmph.2021.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koenig J., Kohls E., Moessner M., et al. The impact of COVID-19 related lockdown measures on self-reported psychopathology and health-related quality of life in German adolescents. Eur child Adolesc Psychiatry. 2021;10:1–10. doi: 10.1007/s00787-021-01843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wade M., Prime H., Browne D.T. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020;290:113143. doi: 10.1016/j.psychres.2020.113143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shek D.T. COVID-19 pandemic and Developmental outcomes in adolescents and young Adults: In Search of the Missing Links. J Adolesc Health. 2021;69:683–684. doi: 10.1016/j.jadohealth.2021.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Otto C., Reiss F., Voss C., et al. Mental health and well-being from childhood to adulthood: Design, methods and results of the 11-year follow-up of the BELLA study. Eur Child Adolesc Psychiatry. 2021:1–19. doi: 10.1007/s00787-020-01630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moor I., Winter K., Bilz L., et al. The 2017/18 health Behaviour in school-aged children (HBSC) study - Methodology of the World health Organization’s child and adolescent health study. J Health Monit. 2020;5:88–102. doi: 10.25646/6904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krause K.R., Chung S., Adewuya A.O., et al. International consensus on a standard set of outcome measures for child and youth anxiety, depression, obsessive-compulsive disorder, and post-traumatic stress disorder. Lancet Psychiatry. 2021;8:76–86. doi: 10.1016/S2215-0366(20)30356-4. [DOI] [PubMed] [Google Scholar]
- 42.Ravens-Sieberer U, The European KIDSCREEN Group . Lengerich: Pabst Science Publisher; 2006. The KIDSCREEN Questionnaires - quality of life questionnaires for children and adolescents – Handbook. [Google Scholar]
- 43.Goodman R. The strengths and difficulties questionnaire: A research note. J Child Psychol Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 44.Woerner W., Becker A., Rothenberger A. Normative data and scale properties of the German parent SDQ. Eur Child Adolesc Psychiatry. 2004;13:ii3–ii10. doi: 10.1007/s00787-004-2002-6. [DOI] [PubMed] [Google Scholar]
- 45.Birmaher B., Brent D.A., Chiappetta L., et al. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Kroenke K., Spitzer R.L., Williams J.B. The Patient health questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 47.Löwe B., Spitzer R., Zipfel S., Herzog W. Gesundheitsfragebogen für Patienten (PHQ-D). Manual-Komplettversion und Kurzform. Autorisierte deutsche Version des “Prime MD Patient Health Questionnaire (PHQ) Pfizer, Heidelberg. 2002;2:90–93. [Google Scholar]
- 48.Haugland S., Wold B. Subjective health complaints in adolescence--reliability and validity of survey methods. J Adolescence. 2001;24:611–624. doi: 10.1006/jado.2000.0393. [DOI] [PubMed] [Google Scholar]
- 49.Felfe C., Saurer J., Schneider P., et al. The youth mental health crisis during the COVID-19 pandemic: The role of school closures. Res Square. 2022 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.