Abstract
Background
Hypertension, also referred to as the silent killer, is known to be one of the most common chronic diseases in the world today. This study aimed to identify the prevalence and risk factors of prehypertension and hypertension among Algerian population.
Methods
This is a descriptive cross-sectional epidemiological study involving individuals aged 18 to 69 years old who were identified in the database of the national survey on non-communicable diseases (NCDs) risk factors conducted in Algeria between 2016 and 2017 using the World Health Organization’s (WHO) STEPwise approach.
Differences in prevalence between normotensives, prehypertensives and hypertensives were assessed using the chi-square test. We also looked at the role of numerous socio-demographic, economic, geographical, and behavioural factors in blood pressure status using a logistic regression model.
Results
The prevalence of prehypertension and hypertension was 36.2% (95% confidence interval: 35.2–37.5%) and 31.6% (95% CI: 30.5–32.7%) respectively. Prehypertension was shown to be substantially higher in males than in women, while hypertension was found to be higher in females compared to men. In addition, both sexes had a rise in the prevalence of blood pressure as they grew older.
A according to multivariate logistic regression analysis, the main common risk factors for prehypertension and hypertension were ageing, obesity, and abdominal obesity. Moreover hypercholesterolemia, and marital status (separated/divorced) were correlated to hypertension.
Conclusion
Prehypertension and hypertension are high and epidemic in Algeria. Therefore, the urgent quantification and monitoring of their risk factors becomes a necessity to plan appropriate preventive measures, in order to fight against NCDs in general.
Keywords: Hypertension, Prehypertension, Risk factors, Non-communicable diseases, - World Health Organization (WHO) - STEPS, Algeria
Background
High blood pressure (HBP) is one of the five major chronic non-communicable diseases (NCDs) on which the World Health Organization (WHO) has recently published a report calling for effective action. It is a vascular disorder that was initially considered rare- but is now a serious global health problem due to its high morbidity, mortality and management costs. HBP is the most common cardiovascular disease affecting 20% of the world’s adult population and resulting in nine million deaths per year [1]. As a result of population growth and ageing, approximately 972 million people were affected in 2000 [2]. Projections based on these data suggest that by 2025, this number is expected to increase by about 60% to 1.56 billion people worldwide [3].
Many persons with HBP are usually diagnosed accidently or after serious organ damage due to its asymptomatic nature [4]. The level of awareness, treatment and control of the disease remains low in developing countries including Algeria, and as a result, most people affected by HBP are unaware of their status [5].
In a detailed study done on the risks of HBP, the National Committee on Prevention, Detection, Evaluation and Treatment of Hypertension (JNC-7) published its seventh report where they defined prehypertension as the blood pressure (BP) category of 120 ± 139 mmHg systolic blood pressure (SBP), and/or 80 ± 89 mmHg diastolic blood pressure (DBP) [6].
People with prehypertension, according to the same report, have a higher risk of developing hypertension as well as a higher risk of cardiovascular morbidity and mortality [6–8].
The highest worldwide prevalence of hypertension was reported among adults from Africa (with 30% of people affected) followed by Asia and Hispanic origins, compared to Caucasians, while the lowest proportion was recorded in America [9–11].
Algeria, like many other developing countries, is witnessing an increased rate in NCDs, owing primarily to the country’s rapid epidemiological transition over the last three decades [12], as well as the emergence of numerous environmental risk factors as a result of uncontrolled globalization, unrestrained urbanization, and rapid lifestyle change [13].
According to the WHO, NCDs in Algeria accounted for nearly 63% of all deaths in 2010 [14]. In 1993, the epidemiological health survey placed hypertension as the leading cause of consultation (17.2%). The prevalence of hypertension among most Algerian population is around 30–40% [13, 15–17].
Similarly, according to the results of an Algerian STEPwise survey of 4156 people on the measurement of NCD risk factors conducted in 2003,by the Ministry of Health in collaboration with WHO, the proportion of hypertension reached a rate of 26 ± 2.6% [16]. The TAHINA (Epidemiological Transition And Health Impact in North Africa) study conducted in 2005 among 4818 households also revealed a level of 24.9% [13]. The results of the Africa/Middle East Cardiovascular Epidemiological research for the Algerian subgroup released in 2018with a relatively high estimated rate of 39.5% [18]. In addition, the multi-center Epidemiological Trial of Hypertension carried out in North Africa in 2013 (“ETHNA”), showed a relatively high prevalence of various cardiometabolic risk factors in the Maghreb countries (41.8% in Algeria) with a proportion of hypertension of about 45% (including 29% of new cases) [19].
In sum, the findings of these various national and international studies point to a concerning health situation in terms of the risk of increased morbidity from hypertension and its impact on Algeria’s socio-economic sector.
Although the exact cause of HBP is unknown, several risk factors have been associated with this disease. There are two types: non-modifiable and modifiable variables. Age, gender, race, family history, genetic makeup, and others are non-modifiable risk factors. On the other hand, Obesity, excessive salt intake, physical inactivity, a high-fat diet, smoking, and alcohol consumption, are modifiable risk factors [20].
Overall, genetic and environmental lifestyle determinants play a significant influence in the development of cardiovascular diseases (CVDs) in general and hypertension in particular [13].
At the end, these determinants weigh heavily on patients’ health care costs, especially as chronic diseases require long and expensive management. All these considerations lead us to think about the early diagnosis and the control of BP which has become a requirement for reducing the risk of common health problems, especially CVD.
Thus, it seems that studies on the epidemiology, etiology, and prevalence of prehypertension/hypertension, as well as associated risk factors, are still rare or even less studied in Algeria.
In this paper, we used the descriptive data of the STEPSwise reports in order to assess and explore the prevalence of prehypertension and hypertension in the Algerian population and in biological, demographic and anthropometric risk factor subgroups.
Additionally, we explored these data to identify and analyse the risk factors associated with this disease, aiming to follow the pattern of its course and risk factors and to provide information that can be used as a basis for the design of health policies and programme that would promote a healthy lifestyle and appropriate planning to target preventive public health interventions in Algeria.
Methods
Study design and data source
In a detailed study done on the risks of HBP, a secondary analysis was carried out from a descriptive cross-sectional study database of the national survey on the measurement of the burden of NCD risk factors according to the STEPwise Algeria approach, conducted in 2016–2017, by the Ministry of Health, Population and Hospital Reform - General Directorate of Prevention and Health Promotion, in collaboration with the National Institute of Public Health with the support of WHO HQ-Geneva and the WHO- Algeria representation office.
The STEPS is a standardized tool, developed and recommended by WHO for the surveillance of NCD risk factors, morbidity and mortality. They consist of three sequential levels: 1) collecting socio-demographic and behavioral information by pairs of investigators (doctor and health worker) using a standardized questionnaire. This data included: age, sex, locality (rural and urban), education level, marital status and occupation; 2) taking physical measurements of BP, height, weight and waist circumference (WC); 3) performing biochemical tests on blood samples such as fasting blood glucose, blood lipids … [21, 22].
The use of the same standardized questionnaires and protocols allows all countries to use the information produced by this system, not only to monitor trends in their own country but also to make space-time comparisons of indicators (through time and between countries) [21].
The main goal of the STEPwise Algeria survey was to estimate the frequency of these factors on a representative sample of 7450 adult, aged 18 to 69 years old, drawn at random from households throughout the country.
The risk factors studied (STEPS core modules) were tobacco and alcohol use, low fruit and vegetable consumption, physical inactivity, overweight and obesity, HBP, hyperglycemia and dyslipidemia. Optional modules on oral health, mental health, trauma, violence and anti-tobacco policy were also included.
The survey database was obtained from the STEPwise official website [23]. The sampling procedures were described in the survey report [22, 24].
Definitions and measurements
Definition of hypertension
According to the Algerian STEPS survey, HBP is defined as SBP greater than or equal to 140 mmHg and / or DBP greater than or equal to 90 mmHg [25] or patients currently taking antihypertensive medication. An automated BP measuring device (OMRON® digital device) was used to obtain BP readings. Three readings were taken at 3–5-minutes intervals after the participant had rested for 15 minutes. As recommended by the WHO, the average of the last two readings was calculated and used as the final BP measurement [24].
In this study BP was classified according to the JNC7 guidelines [6]. The detection of hypertension was based on self-report of any previous diagnosis of hypertension by a health professional. Participants who were on antihypertensive medication for two weeks were defined as self-reported as well.
Secondly, all individuals who were not diagnosed by health personnel and had an SBP more than or equal to 140 mmHg and/or a DBP greater than or equal to 90 mmHg were considered newly detected hypertensive cases. At the same time, prehypertension was defined as participants not taking antihypertensive drugs and having an SBP of 120 ± 139 mmHg and/or a DBP of 80 ± 89 mmHg. Similarly, normotension was defined as participants with SBP less than 120 mmHg and DBP less than 80 mmHg not taking antihypertensive medication.
Definitions of risk factors
The risk factors associated with prehypertension and hypertension were selected and extracted from the STEPS database. They divided into three categories:
Socio-demographic variables such as gender, age, education level, professional status, socio-economic level expressed in monthly salary, locality (rural or urban), geographical area,
Behavioral variables such as tobacco consumption, eating habits, and physical inactivity. The frequency of alcohol consumption was not included among the risk factors because of the low response rate of respondents in the database, especially women;
Clinical variables such as general and abdominal obesity (AO), diabetes, hypercholesterolemia, heart attacks, and heart rate (HR). In addition, for analysis convenience and results interpretation, education level, marital status, geographical region, occupation, smoking status, fruit and vegetable consumption, physical activity, body mass index (BMI) and AO were reclassified and recalculated into original data.
The education level was classified into five groups: no formal education, primary, middle, secondary and university.
The marital status was restructured into three categories: married, divorced/separated and widowed.
The 48 departments surveyed were divided into five geographical regions according to the government division of 1995, Central, East, West, Southern East and Southern West regions [26].
The wealth index was estimated using the respondent’s disclosed monthly income. The categories were created using the national guaranteed minimum wage as a starting point. This allowed us to divide the people into four groups, ranging from the least wealthy to the richest.
The weight and height of survey participants were measured using standardized techniques to estimate BMI. It was calculated as weight in kilograms divided by height in square meters (kg/m2).
The BMI was classified as underweight (<18.5 kg/m2), normal (18.5- < 25 kg/m2), overweight (25 to <30 kg/m2), and obese (30 kg/m2) [27].
A men WC greater than 94 and a women WC greater than 80 cm was defined as AO [28].
Physical activity behavior was assessed in three different domains: work, transport and leisure. The activities were divided into two categories: vigorous and moderate. “Vigorous-intensity activities” were those that required a significant physical effort and caused large increases in breathing or HR. “Moderate intensity activities” were those that required only moderate physical effort and caused slight increases in breathing or HR. On this basis, an adult should perform at least 150 minutes of moderate intensity work, 75 minutes of vigorous intensity work, or 60 minutes of mixed vigorous and moderate intensity work per week. Participants were classified as physically inactive if their reported physical activity did not meet the WHO standard [29].
Fruit and vegetable consumption was divided into two categories following the diet quality indicator: less than five servings per day and five or more servings per day [30].
Cigarette smoking status was self-reported, with daily smokers, ex-daily smokers, and non-smokers being the three categories.
The following questions were used to define hyperglycemia, hypercholesterolemia, and heart attacks: “Have you ever been told by a doctor or other health worker that you have high blood sugar or diabetes? “Have you ever been told by a doctor or other health worker that you have high cholesterol?“ and “Have you ever had a heart attack or chest pain from heart disease (angina) or a stroke (cerebrovascular accident or incident)? On this basis, a dummy variable categorized as “yes” or “no” was generated, with the value “yes” depending on the respondent’s answer.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Science (SPSS) version 25 (IBM Statistics, USA). Descriptive statistics were used to examine the study characteristics of the population as well as the prevalence of prehypertension and hypertension.
The continuous variables were presented as median (IQR) and compared by the Kruskal-Wallis test after having assessed the normality of the distribution using the Kolmogorov-Smirnov statistical test (p < 0.05).
The categorical variables were expressed as percentages and compared using the Chi-square (χ2) test.
Bivariate logistic regression analysis was performed to identify significant risk factors for prehypertension in association to normotensive status and hypertension in relation with normal BP plus prehypertension. In addition, multivariate logistic regression modelling was performed for all variables of interest showing a significant association with p-value <0.05. These variables included age, gender, locality, geographical region, marital status, education level, occupation, behavioral variables such as fruit and vegetable consumption, smoking, physical activity, and metabolic risk parameters such as BMI, AO, hyperglycemia, and hypercholesterolemia which are considered as recommended risk factors for assessment in the STEPS manual [24].
Adjusted odds ratios (AORs) with their 95% confidence intervals (CIs) and p-values were generated to determine the predictors of prehypertension and hypertension.
The final multivariate binary logistic regression model was found to be consistent with the results of the Hosmer-Lemeshow fit test.
Results
Description of study population
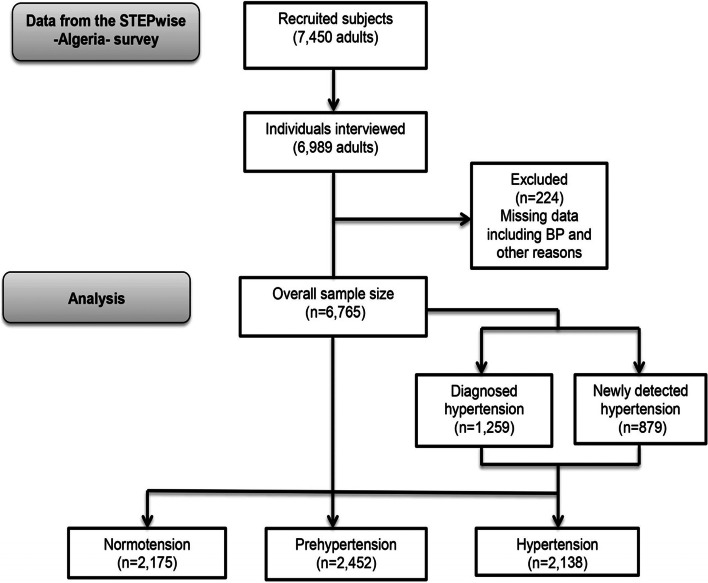
The study was carried out with 7450 adults, of whom only 6989 were interviewed; i.e., a response rate of 93.8% (3082 males and 3907 females, aged 18–69 years). Out of the 6989 participants, 224 were excluded from our study due to missing or outlier data, including BP data (Fig. 1).
Fig. 1.
The disposition of overall sample size analyzed
Thus, as shown in Table 1, a total of 6765 participants (2968 men and 3797 women) were included in the statistical analysis. With 39.3%, the age group (30–44) is the greatest in the sample, followed by the age group (45–59) with an estimated percentage of 27.7%, the younger group (18–29) with 21.4%, and the older group with 11.6%. Approximately 67.5% of these participants live in urban areas with a predominance of demographic density especially in the northern geographical region of the country compared to those in the south. In terms of marital status of participants in our sample, 69.2% were married, 24.3% single, 3% separated and/or divorced and 3.5% widowed. As for the level of education, 32.5% of participants had a primary school level or have never attended school, while the other three levels (middle, secondary and university) had an almost equal distribution around 22.5%. Homemaker (29.2%) was the most common occupation, followed by the unemployed (24.1%), government employees (17.2%), the self-employed (11.7%), private sector employees (10.4%), and retirees (7.3%). Regarding to the wealth index, 67.9% of respondents earned two times the minimum wage or less (lowest and second lowest), 23.2% earned between two and four times the minimum wage (middle and second highest) and 8.8% earned more than four times the minimum wage (highest).
Table 1.
Participant characteristics, overall
| Predictor variables | Effective (n = 6765) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 2968 | 43.9 |
| Female | 3797 | 56.1 |
| Age group (years) | ||
| 18–29 | 1446 | 21.4 |
| 30–44 | 2659 | 39.3 |
| 45–59 | 1872 | 27.7 |
| 60–69 | 788 | 11.6 |
| Marital status | ||
| Never married | 1642 | 24.3 |
| Current married/Cohabitating | 4676 | 69.2 |
| Separated/Divorced | 202 | 3.0 |
| Widowed | 239 | 3.5 |
| Level of education | ||
| No formal school | 1140 | 16.9 |
| Primary school | 1053 | 15.6 |
| Moyen school | 1600 | 23.7 |
| Secondary school | 1566 | 23.2 |
| University | 1390 | 20.6 |
| Locality | ||
| Urban | 4562 | 67.4 |
| Rural | 2203 | 32.6 |
| Geographical region | ||
| North-Centre | 2448 | 36.2 |
| North -West | 1470 | 21.7 |
| North -East | 2104 | 31.1 |
| South -West | 215 | 3.2 |
| South -East | 528 | 7.8 |
| Occupation | ||
| Unemployed (able and not able to work) /Student/No paid | 1630 | 24.1 |
| Government employee | 1162 | 17.2 |
| Non-government employee | 703 | 10.4 |
| Self-employed | 788 | 11.7 |
| Homemaker | 1974 | 29.2 |
| Retired | 495 | 7.3 |
| Wealth index (Family monthly income quintile) | ||
| Lowest (less than or equal to SMIG) | 1172 | 28.4 |
| Second lowest (More than to SMIG, less than or equal to 2x SMIG | 1628 | 39.5 |
| Midle (More than to 2x SMIG, less than or equal to 3x SMIG | 692 | 16.8 |
| Second highest (More than to 3xSMIG, less than or equal to 4x SMIG) | 265 | 6.4 |
| Highest (More than to4xSMIG) | 364 | 8.8 |
| Smoking | ||
| Never smoked | 5203 | 76.9 |
| Past smoked | 754 | 11.9 |
| Current Daily smoked | 808 | 11.1 |
| Physical activity | ||
| Low (< 150 Min/week) | 1315 | 19.4 |
| High (More 150 Min/week) | 5450 | 80.6 |
| Fruits and vegetables consumption | ||
| < 5 fruit/veg/day | 5592 | 85.1 |
| More 5 fruit/veg/day | 978 | 14.9 |
| BMI (Kg/m2) | ||
| < 18,5 (Underwieght) | 219 | 3.3 |
| 18,5–24,9 (Normal weight) | 2400 | 36.6 |
| 25–29,9 (Overweight) | 2303 | 35.0 |
| ≥ 30 (Obese) | 1631 | 24.9 |
| Abdominal obesity | ||
| No (Low) | 2106 | 32.2 |
| Yes (High) | 4429 | 67.8 |
| Blood glucose (Hyperglycemia) | ||
| Yes | 600 | 17.5 |
| No | 2825 | 82.5 |
| Cholesterol (Hypercholesterolemia) | ||
| Yes | 665 | 29.6 |
| No | 1578 | 70.4 |
| Heart attacks | ||
| Yes | 410 | 6.1 |
| No | 6344 | 93.9 |
Furthermore, 24.9% of the Algerian population were obese, 35.01% were overweight, 36.6% were normal, and 3.3% were underweight, according to BMI. AO was found to be present in 67.8% of the population. Tobacco use was distributed between 76.9% of non-smokers versus11.9 and 11.1% of ex-daily and daily smokers respectively. Findings revealed that 85.1% of individuals consumed less than five servings of fruit and vegetables per day. In addition, 80.6% of respondents exercised for 150 minutes or more per week. In addition, 17.5% had diabetes, 29.6% had high cholesterol, and only 6.1% percent experienced a heart attack.
Prevalence of hypertension, prehypertension and abnormal BP
The socio-demographic, behavioral and health characteristics of participants classified by BP category are presented in Table 2.
Table 2.
Prevalence of prehypertension and hypertension by predictor variables
| Predictor variables | Number of individuals | Normal BP | Prehypertension | Hypertension | Statistic | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| (N) | (%) | (N) | (%) | (N) | (%) | χ2 / Kruskal-Wallis | df | P value | ||
| 2175 | 32.2% | 2452 | 36.2% | 2138 | 31.6% | |||||
| CI 95% (31.0–33.3) | CI 95% (35.2–37.5) | CI 95% (30.5–32.7) | ||||||||
| Gender | ||||||||||
| Male | 2968 | 847 | 28.5 | 1282 | 43.2 | 839 | 28.3 | 110.53 a | 2 | <0.001 |
| Female | 3797 | 1328 | 35 | 1170 | 30.8 | 1299 | 34.2 | |||
| Age group (years) | ||||||||||
| 18–29 | 1446 | 788 | 54.5 | 512 | 35.4 | 146 | 10.1 | 1281.52 a | 6 | <0.001 |
| 30–44 | 2659 | 951 | 35.8 | 1120 | 42.1 | 588 | 22.1 | |||
| 45–59 | 1872 | 361 | 19.3 | 647 | 34.6 | 864 | 46.2 | |||
| 60–69 | 788 | 75 | 9.5 | 173 | 22 | 540 | 68.5 | |||
| Marital status | ||||||||||
| Never married | 1642 | 779 | 47.4 | 628 | 38.2 | 235 | 14.3 | 446.765 a | 6 | <0.001 |
| Current married/Cohabitating | 4676 | 1307 | 28 | 1694 | 36.2 | 1675 | 35.8 | |||
| Separated/Divorced | 202 | 57 | 28.2 | 69 | 34.2 | 76 | 37.6 | |||
| Widowed | 239 | 28 | 11.7 | 60 | 25.1 | 151 | 63.2 | |||
| Level of education | ||||||||||
| No formal school | 1140 | 184 | 16.1 | 368 | 32.3 | 588 | 51.6 | 423.42 a | 8 | <0.001 |
| Primary school | 1053 | 240 | 22.8 | 407 | 38.7 | 406 | 38.6 | |||
| Moyen school | 1600 | 556 | 34.8 | 604 | 37.8 | 440 | 27.5 | |||
| Secondary school | 1566 | 598 | 38.2 | 585 | 37.4 | 383 | 24.5 | |||
| University | 1390 | 589 | 42.4 | 485 | 34.9 | 316 | 22.7 | |||
| Locality | ||||||||||
| Urban | 4562 | 1512 | 33.1 | 1573 | 34.5 | 1477 | 32.4 | 18.97 a | 2 | <0.001 |
| Rural | 2203 | 663 | 30.1 | 879 | 39.9 | 661 | 30 | |||
| Geographical region | ||||||||||
| North-Centre | 2448 | 824 | 33.7 | 851 | 34.8 | 773 | 31.6 | 13.24 a | 8 | NS |
| North -West | 1470 | 473 | 32.2 | 526 | 35.8 | 471 | 32 | |||
| North -East | 2104 | 624 | 29.7 | 799 | 38 | 681 | 32.4 | |||
| South -West | 215 | 74 | 34.4 | 76 | 35.3 | 65 | 30.2 | |||
| South- East | 528 | 180 | 34.1 | 200 | 37.9 | 148 | 28 | |||
| Occupation | ||||||||||
| Unemployed (able and not able to work) /Student/No paid | 1630 | 662 | 40.6 | 573 | 35.2 | 395 | 24.2 | 403.71 a | 10 | <0.001 |
| Government employee | 1162 | 430 | 37 | 438 | 37.7 | 294 | 25.3 | |||
| Non-government employee | 703 | 233 | 33.1 | 302 | 43 | 168 | 23.9 | |||
| Self-employed | 788 | 220 | 27.9 | 373 | 47.3 | 195 | 24.7 | |||
| Homemaker | 1974 | 564 | 28.6 | 615 | 31.2 | 795 | 40.3 | |||
| Retired | 495 | 59 | 11.9 | 147 | 29.7 | 289 | 58.4 | |||
| Wealth index (Family monthly income quintile) | ||||||||||
| Lowest (less than or equal to SMIG) | 1172 | 344 | 29.4 | 415 | 35.4 | 413 | 35.2 | 8.29 a | 8 | NS |
| Second lowest (More than to SMIG, less than or equal to 2x SMIG | 1628 | 524 | 32.2 | 586 | 36 | 518 | 31.8 | |||
| Midle (More than to 2x SMIG, less than or equal to 3x SMIG | 692 | 230 | 33.2 | 249 | 36 | 213 | 30.8 | |||
| Second highest (More than to 3xSMIG,less than or equal to 4x SMIG) | 265 | 93 | 35.1 | 93 | 35.1 | 79 | 29.8 | |||
| Highest (More than to4xSMIG) | 364 | 115 | 31.6 | 125 | 34.3 | 124 | 34.1 | |||
| Smoking | ||||||||||
| Never smoked | 5203 | 1741 | 33.5 | 1797 | 34.5 | 1665 | 32 | 98.57 a | 4 | <0.001 |
| Past smoked | 754 | 161 | 21.4 | 291 | 38.6 | 302 | 40.1 | |||
| Current Daily smoked | 808 | 273 | 33.8 | 364 | 45 | 171 | 21.2 | |||
| Physical activity | ||||||||||
| Low (< 150 Min/week) | 1315 | 406 | 30.9 | 457 | 34.8 | 452 | 34.4 | 5.79 a | 2 | NS |
| High (More 150 Min/week) | 5450 | 1769 | 32.5 | 1995 | 36.6 | 1686 | 30.9 | |||
| Fruit and vegetables consumption | ||||||||||
| < 5 fruit/veg/day | 5592 | 1790 | 32 | 2023 | 36.2 | 1779 | 31.8 | 0.86 a | 2 | NS |
| More 5 fruit/veg/day | 978 | 325 | 33.2 | 355 | 36.3 | 298 | 30.5 | |||
| BMI (Kg/m2) | ||||||||||
| < 18,5 (Underwieght) | 219 | 135 | 61.6 | 55 | 25.1 | 29 | 13.1 | 432.65 a | 6 | <0.001 |
| 18,5–24,9 (Normal weight) | 2400 | 966 | 40.3 | 930 | 38.8 | 504 | 21 | |||
| 25–29,9 (Overweight) | 2303 | 627 | 27.2 | 888 | 38.6 | 788 | 34.2 | |||
| ≥ 30 (Obese) | 1631 | 358 | 21.9 | 514 | 31.5 | 759 | 46.5 | |||
| Abdominal obesity | ||||||||||
| No (Low) | 2106 | 891 | 42.3 | 841 | 39.9 | 374 | 17.8 | 309.26 a | 2 | <0.001 |
| Yes (High) | 4429 | 1191 | 26.9 | 1536 | 34.7 | 1702 | 38.4 | |||
| Blood glucose (Hyperglycemia) | ||||||||||
| Yes | 600 | 76 | 12.7 | 134 | 22.3 | 390 | 65 | 196.46 a | 2 | <0.001 |
| No | 2825 | 905 | 32 | 938 | 33.2 | 982 | 34.8 | |||
| Cholesterol (Hypercholesterolemia) | ||||||||||
| Yes | 665 | 102 | 15.3 | 139 | 20.9 | 424 | 63.8 | 116.91 a | 2 | <0.001 |
| No | 1578 | 462 | 29.3 | 500 | 31.7 | 616 | 39 | |||
| Heart attacks | ||||||||||
| Yes | 410 | 107 | 26.1 | 91 | 22.2 | 212 | 51.7 | 84.82 a | 2 | <0.001 |
| No | 6344 | 2063 | 32.5 | 2360 | 37.2 | 1921 | 30.3 | |||
| Blood pressure | ||||||||||
| SBP (mmHg) M (P25 ~ P75) | 112 (107.5 ~ 116) | 127.5 (123 ~ 132.5) | 144.5 (134.5 ~ 155.5) | 4619.46b | <0.001 | |||||
| DBP (mmHg) M (P25 ~ P75) | 69 (63.5 ~ 74) | 77 (71.5 ~ 82) | 82.5 (75 ~ 90) | 1912.45 b | <0.001 | |||||
| Heart Rate | ||||||||||
| HR (bpm) M (P25 ~ P75) | 76 (69 ~ 83.5) | 77 (70 ~ 84.5) | 78.5 (71 ~ 86) | 47.23 b | <0.001 | |||||
Continuous variables were presented as median (IQR) and compared using the Kruskal-Wallis test
Categorical variables were expressed as effectives /percentages and analyzed by the χ2 test
Variables are shown as M (P25 ~ P75) or percentage
aχ2 test
bKruskal-Wallis test
df Degrees of freedom
The prevalence of normotension, prehypertension and hypertension in Algeria was 32.2% (95% CI: 31.0–33.3%), 36.2% (95% CI: 35.2–37.5%), 31.6% (95% CI: 30.5–32.7%), respectively. The prevalence of hypertension was derived from the sum of 18.6% (1259 cases reported to have been previously diagnosed by a doctor or health worker) and 13.0% (879 newly detected cases). The bivariate analysis shows a highly significant difference (P < 0.001) between the prevalence of the prehypertension/hypertension groups according to the categories of a) sex mainly due to the high prevalence of prehypertension in men (43.2%) and hypertension in women (34.2%), b) locality which is related to the significantly high proportion of prehypertension in individuals living to rural areas of 39. 9%, c) occupation (due to the high rates of prehypertension among retirees and homemakers as well as the high rate of prehypertension among the self-employed), and d) smoking status owing to the high percentages of prehypertension (45%) and hypertension (40%) among smokers and ex-smokers respectively.
Also, a significantly high association was recorded between hypertension and the last two age groups (45–59); (60–69), the marital status (widowed (63.2%) and separated (37.6%)), the education levels (uneducated, primary with a prevalence of 51.6 and 38.5% respectively), the BMI (overweight and obesity respectively with rates of 34.2% and 46.53), the AO (38.4%), diabetes (65%), hypercholesterolemia (63.8%), heart attacks (51.7%), as well as SBP, DBP and HR (P < 0.001).
However, no significant relationship was found between individuals with hypertension compared to participants with normotension and prehypertension in the categories of geographical region, wealth index, physical activity, and fruit and vegetable consumption.
Risk factors for raised BP (prehypertension and hypertension)
Multivariate logistic regression analysis was performed to determine the factors associated with prehypertension and hypertension (Table 3).
Table 3.
Risk factors for raised BP (prehypertension and hypertension)
| Predictor variables | Normal BP /Prehypertension | Hypertension/ Normal BP + Prehypertension | ||||
|---|---|---|---|---|---|---|
| COR (95%CI) | AOR (95%CI) | P value | COR (95%CI) | AOR (95%CI) | P value | |
| Gender | ||||||
| Male | 1 | 1 | 1 | 1 | ||
| Female | 0.582 (0.518, 0.654) | 0.382 (0.279, 0.523) | <0.001 | 1.320 (1.189, 1465) | 0.838 (0.529, 1.327) | NS |
| Age group (years) | ||||||
| 18–29 | 1 | 1 | 1 | 1 | ||
| 30–44 | 1.813 (1.574, 2.087) | 1.673 (1.265, 2.215) | <0.001 | 2.528 (2.082, 3.069) | 1.965 (1.084, 3.562) | <0.05 |
| 45–59 | 2.758 (2.327, 3.270) | 2.286 (1.638, 3.191) | <0.001 | 7.632 (6.288, 9.263) | 4.558 (2.477, 8.388) | <0.001 |
| 60–69 | 3.550 (2.649, 4.758) | 2.879 (1.703, 4.868) | <0.001 | 19.388 (15.439, 24.347) | 12.274 (6.041, 24.936) | <0.001 |
| Marital status | ||||||
| Never married | 1 | 1 | 1 | 1 | ||
| Current married/Cohabitating | 1.608 (1.415, 1.826) | 0.959 (0.732, 1.255) | NS | 3.342 (2.875, 3.885) | 1.296 (0.814, 2.063) | NS |
| Separated/Divorced | 1.502 (1.041, 2.166) | 1.154 (0.653, 2.041) | NS | 3.611 (2.632, 4.955) | 2.872 (1.229, 6.712) | <0.05 |
| Widowed | 2.658 (1.677, 4.214) | 0.928 (0.490, 1.756) | NS | 10.274 (7.634, 13.825) | 1.732 (0.806, 3.720) | NS |
| Level of education | ||||||
| No formal school | 2.429 (1.961, 3.008) | 1.298 (0.882, 1.909) | NS | 3.620 (3.051, 4.295) | 0.838 (0.503, 1.396) | NS |
| Primary school | 2.059 (1.687, 2.515) | 1.079 (0.757, 1.538) | NS | 2.133 (1.788, 2.544) | 1.009 (0.613, 1.662) | NS |
| Moyen school | 1.319 (1.117, 1.558) | 0.890 (0.664, 1.193) | NS | 1.289 (1.091, 1.523) | 0.810 (0.523, 1.254) | NS |
| Secondary school | 1.188 (1.007, 1.402) | 0.860 (0.651, 1.137) | NS | 1.100 (0.928, 1.305) | 0.762 (0.503, 1.154) | NS |
| University | 1 | 1 | 1 | 1 | ||
| Locality | ||||||
| Urban | 1 | 1 | 1 | 1 | ||
| Rural | 1.274 (1.127, 1.441) | 1.129 (0.914, 1.396) | NS | 0.895 (0.802, 1.000) | 1.072 (0.779, 1.477) | NS |
| Geographical region | ||||||
| North-Centre | 1 | 1 | 1 | 1 | ||
| North -West | 1.077 (0.920, 1.260) | 0.899 (0.689, 1.173) | NS | 1.022 (0.889, 1.174) | – | NS |
| North -East | 1.240 (1.076, 1.429) | 1.144 (0.914, 1.432) | NS | 1.037 (0.915, 1.175) | – | NS |
| South -West | 0.994 (0.712, 1.389) | 0.813 (0.421, 1.572) | NS | 0.939 (0.693, 1.272) | – | NS |
| South -East | 1.076 (0.861, 1.345) | 1.254 (0.838, 1.877) | NS | 0.844 (0.685, 1.039) | – | NS |
| Occupation | ||||||
| Unemployed (able and not able to work) /Student/No paid | 1 | 1 | 1 | 1 | ||
| Government employee | 1.177 (0.989, 1.400) | 0.539 (0.390, 0.744) | <0.001 | 1.059 (0.890, 1.260) | 0.651 (0.386, 1.099) | NS |
| Non-government employee | 1.497 (1.221, 1.837) | 0.653 (0.438, 0.973) | <0.05 | 0.982 (0.798, 1.208) | 0.716 (0.369, 1.390) | NS |
| Self employed | 1.959 (1.603, 2.394) | 1.035 (0.686, 1.562) | NS | 1.028 (0.844, 1.253) | 0.844 (0.435, 1.636) | NS |
| Home marker | 1.260 (1.074, 1.478) | 1.073 (0.801, 1.437) | NS | 2.108 (1.824, 2.436) | 1.286 (0.832, 1.986) | NS |
| Retired | 2.879 (2.086, 3.972) | 0.784 (0.464, 1.324) | NS | 4386 (3.550, 5420) | 0.894 (0.494, 1.619) | NS |
| Wealth index (Family monthly income quintile) | ||||||
| Lowest (less than or equal to SMIG) | 1 | – | 1 | 1 | ||
| Second lowest (More than to SMIG, less than or equal to 2x SMIG | 0.927 (0.770, 1.116) | – | NS | 0.858 (0.732, 1.005) | 0.826 (0.581, 1.175) | NS |
| Midle (More than to 2x SMIG, less than or equal to 3x SMIG | 0.897 (0.714, 1.129) | – | NS | 0.817 (0.668, 0.999) | 0.743 (0.489, 1.127) | NS |
| Second highest (More than to 3xSMIG, less than or equal to 4x SMIG) | 0.829 (0.601, 1.143) | – | NS | 0.781 (0.585, 1.042) | 0.796 (0.461, 1.375) | NS |
| Highest (More than to4xSMIG) | 0.901 (0.674, 1.205) | – | NS | 0.950 (0.741, 1.216) | 0.981 (0.593, 1.622) | NS |
| Smoking | ||||||
| Never smoked | 1 | 1 | 1 | 1 | ||
| Current Daily smoked | 1.292 (1.090, 1.531) | 0.907 (0.625, 1.316) | NS | 0.570 (0.477, 0.682) | 0.821 (0.454, 1.486) | NS |
| Past smoked | 1.751 (1.429, 2.146) | 1.185 (0.816, 1.719) | NS | 1.420 (1.214, 1.661) | 1.225 (0.782, 1.918) | NS |
| Physical activity | ||||||
| Low (< 150 Min/week) | 0.998 (0.861, 1.158) | – | NS | 1.169 (1.029, 1.328) | 1.001 (0.707, 1.416) | NS |
| High (More 150 Min/week) | 1 | – | 1 | 1 | ||
| Fruits and vegetables consumption | ||||||
| < 5 fruit/veg/day | 1.035 (0.879, 1.218) | – | NS | 1.065 (0.919, 1.234) | – | NS |
| More 5 fruit/veg/day | 1 | – | 1 | – | ||
| BMI (Kg/m2) | ||||||
| 18,5–24,9 (Normal weight) | 1 | 1 | 1 | 1 | ||
| < 18,5 (Underwieght) | 0.423 (0.305, 0.586) | 0.306 (0.146, 0.641) | <0.01 | 0.574 (0.384, 0.859) | 0.812 (0.228, 2.889) | NS |
| 25–29,9 (Overweight) | 1.471 (1.284, 1.686) | 1.210 (0.947, 1.545) | NS | 1.957 (1.717, 2.230) | 1.039 (0.722, 1.494) | NS |
| ≥ 30 (Obese) | 1.491 (1.268, 1.754) | 1.362 (1.026, 1.807) | <0.05 | 3.274 (2.852, 3.760) | 1.687 (1.143, 2.489) | <0.01 |
| Abdominal obesity | ||||||
| No (Low) | 1 | 1 | 1 | 1 | ||
| Yes (High) | 1.366 (1.211, 1.542) | 1.363 (1.046, 1.776) | <0.05 | 2.890 (2.545, 3.282) | 1.686 (1.119, 2.541) | <0.05 |
| Blood glucose (Hyperglycemia) | ||||||
| Yes | 1.701 (1.265, 2.287) | 1.351 (0.977, 1.870) | NS | 3.485 (2.897, 4.193) | 1.341 (0.954, 1.884) | NS |
| No | 1 | 1 | 1 | 1 | ||
| Cholesterol (Hypercholesterolemia) | ||||||
| Yes | 1.259 (0.947, 1.675) | – | NS | 2.748 (2.277, 3.315) | 2.029 (1.500, 2.746) | <0.001 |
| No | 1 | – | 1 | 1 | ||
After adjustment, the analysis revealed that getting older was linked to a linear rise in the probability of having prehypertension. When compared to the younger age group (18–29), this risk was more than one and a half times higher in the (30–44) age group (AOR = 1.673; [1.265–2.215]; P < 0.001), more than two times higher in the (45–59) age group (AOR = 2.286; [1.638–3.191]; P < 0.001) and about three times higher in the age group (60–69 years) (AOR = 2.879; [1.703–4.868]; P < 0.001). Obese individuals who were also abdominally obese had a higher risk of developing prehypertension. When compared to healthy individuals, they respectively have more than one risk in the obese BMI category (AOR = 1.362; [1.026–1.807]; P < 0.05) with AO (AOR = 1.363; [1.046–1.776]; P < 0.05).
Gender (female) (P < 0.001), government employee and non-government employee (P < 0.001; P < 0.05), and underweight subjects (P < 0.01), on the other hand, appeared to have a protective effect.
Prehypertension was not significantly correlated with marital status, education level, locality, geographical region, wealth index, smoking, fruit and vegetable consumption, physical activity, diabetes, and hypercholesterolemia.
Hypertension, on the other hand, was found to have a highly significant relationship with increasing age. When compared to the (18–29 years) group, the risk was almost two times higher in the (30–44 years) age group (AOR = 1.965; [1.084–3.562]; P < 0.05), more than four and a half times higher in the (45–59 years) age group (AOR = 4.558; [2.477–8.388]; P < 0.001) and about twelve and a half times higher in the (60–69 years) group (AOR = 12.274; [6.041–24.936]; P < 0.001). Obese people (AOR = 1.687; [1.143–2.489]; P < 0.01) with AO (AOR = 1.686; [1.119–2.541]; P < 0.05) had a higher risk of hypertension than healthy people.
Furthermore, marital status, and hypercholesterolemia were all factors contributing to getting hypertension. Separated/Divorced had a risk of hypertension of 2.872; [1.229–6.712]; P < 0.05), and patients with hypercholesterolemia had a risk of 2.029; [1.500–2.746]; P < 0.001). Gender, education level, locality, geographical region, occupation, wealth index, smoking status, fruit and vegetable consumption, physical activity, and diabetes, on the other hand, were not shown to be significantly associated with hypertension.
Discussion
Algeria has been the focus of extensive national and international research on evaluating the burden of NCD risk factors in the context of the epidemiological transition study and its impact on health systems in North Africa. In a 2014 WHO report on Algeria, NCDs were associated to 77% of death causes, with CVD accounting for the majority (41%) [31].
Prehypertension and hypertension are the most frequent cardiovascular disorders worldwide, and they are increasingly regarded as one of the most serious public health issues, particularly in developing nations [32].
This study was conducted on a representative sample of 6765 adults using data from the Algerian STEPwise survey 2016–2017 to assess and determine the prevalence of prehypertension and hypertension as well as the risk factors in Algeria.
The results showed that prevalence of prehypertension was high in the Algerian population, with a rate of 36.2%, affecting more males than females (43.2% vs 30.8%). As a result, preventive measures should be adopted with patients who have been diagnosed as prehypertensive, such as monitoring their blood pressure more closely, because a considerable proportion of them are at risk of developing hypertension [6].
Being an under-studied disease in Maghreb countries, prehypertension had a prevalence of 36.2%, which is identical to that found in a cross-sectional survey conducted in Algiers recently which estimated the rate of prehypertension at 36.7% (49.5% in men, against 31.4% in women) [33].
The findings of that study also corresponded to the rate of the adult population in north-east China (36.0%) [34] and the adult population of Brazil (36.1%) [35]. However, it was lower than the rate of Bangladesh’s population aged 25 to 45 years (41.8%) [36], and still slightly higher than the adult population of southern Iran (33.7%) [37] and Taiwanese adults (34%) [38].
Furthermore, the results indicated that the overall prevalence of hypertension in our study was 31.6%, of which 13.0% were newly detected at the time of the study evaluation; i.e., a rate of 41.1% of Algerian participants living with undiagnosed hypertension. The latter may have a higher risk of complications, which would then be too late to avoid.
In comparison to national and regional studies, this proportion of hypertension is consistent with that found in most Algerian populations, which ranges from 30 to 40% [13, 15–17]. It is higher than in some previous studies. The STEPSwise survey in Algeria in 2003 found a BP rate of 26 ± 2.6% [16]. A level of 24.9% was also found in a TAHINA research conducted in 2005 [13]. However, it was still significantly lower than the North African multicenter study conducted in 2013 with a very high hypertension’s proportion of about 45.4% [19], as well as the “Africa / Middle East Cardiovascular Epidemiological” study conducted in 2018 with an estimated hypertension rate of 39.5% for the subgroup “Algeria” [18].
In addition, the prevalence of hypertension in this study was comparable to the overall prevalence in sub-Saharan Africa, which was estimated at 30% [39], as well as Tunisia’s prevalence of 30.6% [40], and higher than the global adult population’s prevalence of 26.4%, Sudan’s prevalence of 27.6% [41], Palestine’s prevalence of 27.6% [42], and Canada’s prevalence of 27% [43].
On the other hand, it was judged to be significantly lower than in Morocco (39.8% [44]), Oman (41.5% [45]), and European countries (38% in Sweden, 42% in England, 47% in Spain, 55% in Germany) [43].
Furthermore, the prevalence of prehypertension in both sexes decreased in the older age groups from 30–44 years, according to our results. However, in both sexes, the prevalence of hypertension rose with age, which is in line with the findings of other research [34, 35].
Risk factors
Algeria has seen an epidemiological transition as a result of ageing combined with changes in lifestyle, particularly dietary and behavioral patterns. These had a significant impact on risk factors as well as on the incidence of cardiovascular morbidities, diabetes and obesity [12].
Although the bivariate analysis showed a significant correlation between the prevalence of the prehypertension/hypertension groups according to the categories of gender, age, marital status, education level, locality, occupation, BMI (overweight and obesity), AO, smoking status, diabetes, and hypercholesterolemia, the multivariate analysis using logistic regression retained only some determinants with a significant influence on the prevalence of prehypertension and hypertension.
It revealed a highly significant relationship between the chance of acquiring prehypertension and hypertension as one gets older. These results are in line with previous publications from African and global populations [19, 46–48]. The scientists speculate that this is related to changes in blood vessel physiology as people get older. The elasticity of the artery walls would be lost, resulting in a rise in blood pressure [49, 50]. According to previous studies [51], this could be linked to hormonal changes in both sexes at different ages. As a result, frequent monitoring is essential for detecting hypertension early in the menopausal transition.
Furthermore, the results of our study show that obesity is associated with a high prevalence of prehypertension and hypertension. Data from the literature in North Africa [19, 52] and around the world [46, 53] significantly corroborated this conclusion.
This link was frequently discovered among women [35, 46], and as a result, it has become a major public health issue, particularly in developing nations. As a result, WHO classified it as a “global pandemic” Weight gain as a result of improved living standards and decreased physical activity results in increased blood flow to various vital parts of the body like organs and tissues in response to their increased metabolic demands. As a result, the artery walls will be subjected to increased pressure [49]. However, data from Tanzania and Uganda revealed that the population with a high BMI and central obesity had a low proportion of hypertension [54].
Furthermore, our results showed that there was a correlation between the prevalence of AO and the risk of developing prehypertension and hypertension. This matches respectively the findings of Mammeri et al. [12] and Midha et al. [55]. It appears to be linked to the mechanisms of sympathetic nervous system hyperactivity and renin-angiotensin system activation, according to some authors. By causing peripheral vasoconstriction, these mechanisms can cause hypertension. Dyslipidemia and metabolic dysregulation caused by dietary changes are also risk factors [56, 57]. Consumption of saturated animal fats and processed carbohydrates has increased in recent years, but consumption of fruits and vegetables has dropped [19].
Hypertension in Algeria’s population was found to be positively correlated with marital status (separated/divorced), as in many previous studies. The authors [19, 58] have extensively reported on these findings. It is noted that separated or widowed people compared to married people are more susceptible to have diseases such as anxiety and depression, which explains the risk of developing HBP. Hypercholesterolemia was also a factor in the development of hypertension in our study. This result supports the findings of a number of researche [19, 40, 59]. The direct reasons for this affinity are attributed to urbanization and the nutritional transition associated to the risk of metabolic syndrome [60].
On the other hand, no association was found between the proportion of prehypertension and hypertension with respect to gender, and there was even a protective effect of female versus male gender in prehypertensive status. This result is in line with those mentioned by: Temmar et al. [17] and Ong et al. [61], who found no difference in hypertension prevalence between the sexes. This could be owing to both sexes having the same economic level. In contrast, Pereira et al. [62] discovered a higher average prevalence of BP in males than in women, particularly in developed countries. The gender differences could be explained by the molecular mechanisms underlying vascular, nervous system and kidney functions, that led to hypertension [63], while some studies from sub-Saharan Africa [61, 64, 65] found that the frequency of hypertension is clearly more prevalent for women than for men, with the hormonal profile and postmenopausal status of women accounting for this difference [66].
Furthermore, our study did not show a significant association between geographical region, locality and hypertension. Several studies [67, 68] have noted that people living in urban areas had a higher risk of hypertension. This could be interpreted as a change of lifestyle in these urban areas, including dietary habits, like access to fast food, high-fat, and energy-dense frozen food, and the availability of transport, all of which contributed to physical inactivity. Other studies [19, 34], established the link with the rural area. This is most likely due to the lack of screening as a result of the limited health infrastructure and the low level of education in these areas.
Similarly, we found no evidence of a link between hypertension and education, income, or occupation. These socio-demographic and economic determinants were frequently considered as contributing factors to the development of hypertension [69–71]. According to several studies, illiterate or less educated people, as well as a lack of resources, might had an impact on their general knowledge of how to prevent hypertension which led to unhealthy lifestyles.
In terms to diabetes, the present study found no association with hypertension, contrary to what was pointed out in several research that demonstrated a strong link between the levels of insulin secreted and BP [17, 53].
Although smoking, low fruit and vegetable consumption and physical inactivity play an important role in the development of cardiovascular events including prehypertension and hypertension [72, 73], our results contradicted this while some authors [74] reported the same outcome. The difference could be explained by a number of factors, on top of which is Algeria’s population low proportion of smokers and ex-smokers.
Second, the Mediterranean diet, which is described by several authors as balanced and helpful in improving blood glucose and cholesterol levels in metabolic syndrome, and in preventing diabetes [75].
Third, there has been an upsurge in physical activity among North Africans in recent years [19, 76].
Finally, this study provided important data on some cardiovascular risk factors linked to Algeria’s high rate of prehypertension and hypertension. On the one hand, it would be useful to spread within Algeria’s population awareness on the risks of CVD in order to detect HBP early and effectively treat people with prehypertension to prevent chronic hypertension. The introduction of healthy habits, therefore, should be encouraged [19].
Study limitations
This study has some limitations. First, the cross-sectional epidemiological study design used in the Algerian STEPwise survey, although used for its speed, efficiency and suitability for chronic diseases, it may not establish the causal relationship between risk factors for prehypertension and hypertension, or may it allow for the generalization of results to the whole population.
Second, the hypertension real prevalence may be inaccurate, either because of under- or over-reporting resulting from self-reporting of hypertension, or because of slight over- or underestimation due to the three measurements of systolic and diastolic BP which were taken only once on one day, or because participants could have recall bias, leading to redundancy in the information provided. Similarly, the study did not include people over 69 years old, which may also distort the overall prevalence of HBP in the population.
Third, the variables analysed in this study can only explain part of the disease determinants.
At the end, the link of genetic factors to the high prevalence of prehypertension and hypertension was not studied.
Conclusions
The present study found a high prevalence of prehypertension and hypertension in the adult Algerian population by analysing data from the STEPwise Survey (2016–2017). The lack of awareness of prehypertension among many participants is a concerning issue. Those at higher risk of hypertension need special attention to control the future burden of NCDs.
Therefore, prehypertension, hypertension and the majority of their risk factors are frequently preventable or effectively managed through health education about the importance of early detection and preventive interventions. Ways of raising doing this can be in the form of lifestyle awareness targeting diet, physical activity, and smoking cessation, among other things.
Finally, these results are important for establishing a national programme and policies related to the initiation of prevention and public health control in order to reduce the prevalence of NCD in general and to prevent the increase of health care expenditures in the future.
Acknowledgments
We would like to acknowledge the participants and the supporting staff in this study for their immense support. Special thanks go to the Ministry of Health, Population and Hospital Reform - Directorate General for Prevention and Health Promotion, to the National Institute of Public Health as well as to the WHO-Geneva headquarters and to the WHO-Algeria representative office for the assistance provided in carrying out the national survey on the measurement of the burden of risk factors for NCDs according to STEPwise. We also thank the administration of the official STEPwise website for providing us with the survey database.
Abbreviations
- AO
Abdominal Obesity
- AOR
Adjusted Odds Ratio
- BMI
Body Mass Index
- BP
Blood Pressure
- CI
Confidence Interval
- CVDs
Cardiovascular Disease
- DBP
Diastolic Blood Pressure
- HBP
High Blood Pressure
- HR.
Heart Rate
- JNC-7
The Seventh report of the National Committee on Prevention, Detection, Evaluation and Treatment of Hypertension
- NCDs
Non Communicable Diseases
- SBP
Systolic Blood Pressure
- SMIG
The national guaranteed minimum wage
- SPSS
Statistical Package for Social Science
- TAHINA
The Epidemiological Transition And Health Impact in North Africa
- WC
Waist Circumference
- WHO
World Health Organization
Authors’ contributions
All authors contributed to the data interpretation and manuscript writing. AM, AA and DB designed the research and contributed to the data interpretation; AM and AS performed the extraction and selection of data from the survey database obtained from the STEPwise official website; AM, AS and HH participated in the statistical analisis; AM, AA, DB interpreted the results; AM, HH and AS wrote the article and had primary responsibility for the final content. All authors have read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The survey database was obtained from the STEPwise official website. Those datasets used and/or analysed during the current study are available from the first author Abdellatif Moussouni (abdellatif.moussouni@gmail.com) on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with relevant guidelines and regulations to Helsinki Declaration. Our study’s objectives and procedures were based on data from the STEPwise survey, for which ethical approval was approved a priori by the ethics committee at the Thematic Agency of Research in Health Sciences (ATRSS), from the Algerian Ministry of Health, Population and Hospital Reform - General Directorate of Prevention and Health Promotion according to the Executive Decree No. 92–276 of 06 July 1992 on the Algerian Code of Medical Ethics. Written informed consent was obtained from the participants.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Global overview of hypertension. A “silent killer” responsible for a global public health crisis. 2013. [Google Scholar]
- 2.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380(9841):611–619. doi: 10.1016/s0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 3.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)70151-3. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva: World Health Organization; 2002. [Google Scholar]
- 5.Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. Plos One. 2014;9(8):e104300. doi: 10.1371/journal.pone.0104300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41:1178–1179. doi: 10.1161/01.HYP.0000075790.33892.AE. [DOI] [PubMed] [Google Scholar]
- 7.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 8.Huang Y, Wang S, Cai X, Mai W, Hu Y, Tang H, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177. doi: 10.1186/1741-7015-11-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agyemang C, Kunst A, Bhopal R, Zaninotto P, Unwin N, Nazroo J, et al. A cross-national comparative study of blood pressure and hypertension between English and Dutch South-Asian- and African-origin populations: the role of national context. Am J Hypertens. 2010;23(6):639–648. doi: 10.1038/ajh.2010.39. [DOI] [PubMed] [Google Scholar]
- 10.Lane D, Lip GY. Blood pressure in different ethnic groups. Am J Cardiol. 2001;88(10):1218–1219. doi: 10.1016/s0002-9149(01)01963-4. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization . STEPS country reports. 2015. [Google Scholar]
- 12.Mammeri A, Tebaibia A. Cardiometabolic risk in Algeria: past and present. Intern Emerg Med. 2020;15(4):531–535. doi: 10.1007/s11739-019-02207-z. [DOI] [PubMed] [Google Scholar]
- 13.National Institute of Public Health . National health survey (Epidemiological transition and health impact in North Africa) TAHINA Project; 2005. [Google Scholar]
- 14.World Health Organization. World health statistics 2012. Geneva: WHO; 2012. https://apps.who.int/iris/handle/10665/44844. Accessed 19 Feb 2021.
- 15.Benkhedda B, Chibane A, Temmar M, Aicheur T, Bendaoud N, Azou M, et al. Prevalence of hypertension in Algeria: national survey SAHA Abstract XIV; European conference on arterial hypertension Paris June. 2004. [Google Scholar]
- 16.MSPRH - Department of Prevention. Measurement of risk factors for non-communicable diseases in two pilot wilayas in Algeria 2003 (WHO STEPwise approach) Final report - Algeria 2005.
- 17.Temmar M, Labat C, Benkhedda S, Charifi M, Thomas F, Bouafia MT, et al. Prevalence and determinants of hypertension in the Algerian Sahara. J Hypertens. 2007;25:2218–2226. doi: 10.1097/HJH.0b013e3282dc7549. [DOI] [PubMed] [Google Scholar]
- 18.Brouri M, Ouadahi N, Nibouche D, Benabbas Y, El hassar M, Bouraoui S, et al. A subgroup analysis of the “Africa / Middle East Cardiovascular Epidemiological” study. Ann Cardiol Angeiol. 2018;67(2):61–66. doi: 10.1016/j.ancard.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Nejjari C, Arharbi M, Chentir MT, Boujnah R, Kemmou O, Megdiche H, et al. Epidemiological Trial of Hypertension in North Africa (ETHNA): an international multicentre study in Algeria, Morocco and Tunisia. J Hypertens. 2013;31(1):49–62. doi: 10.1097/HJH.0b013e32835a6611. [DOI] [PubMed] [Google Scholar]
- 20.Mayega RW, Makumbi F, Rutebemberwa E, Peterson S, Ostenson CG, Tomson G. Modifiable socio-behavioral factors associated with overweight and hypertension among persons aged 35 to 60 years in eastern Uganda. Plos One. 2012;7:7632. doi: 10.1371/journal.pone.0047632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riley L, Guthold R, Cowan M, Savin S, Bhatti L, Armstrong T, et al. The World Health Organization STEPwise Approach to Non communicable disease risk-factor surveillance: methods, challenges, and opportunities. Am J Public Health. 2016;106(1):74–78. doi: 10.2105/AJPH.2015.302962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.STEPwise Algeria 2016-2017 survey: Better knowledge of the health profiles of Algerians for the risk factors of non-communicable diseases. Regional Office for Africa. Available from: https://www.afro.who.int/fr/media-centre/events/enquete-stepwise-algerie-2016-2017-meilleure-connaissance-du-profil-de-sante. Accessed 11 Feb 2021.
- 23.NCD Microdata Repository. https://extranet.who.int/ncdsmicrodata/index.php/home. Accessed 14 Feb 2021.
- 24.World Health Organization . WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. Geneva: WHO; 2005. [Google Scholar]
- 25.World Health Organization . Clinical guidelines for the management of hypertension. 2005. [Google Scholar]
- 26.Brahamia B. Health economics, evolution and trend of health systems. Edition Bahaeddine Constantine. 2010. p. 363. [Google Scholar]
- 27.World Health Organization. Global database on body mass index. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed 8 Feb 2021.
- 28.World Health Organization . Waist circumference and waist–hip ratio: report of a WHO expert consultation. 2011. [Google Scholar]
- 29.World Health Organization . Global strategy on diet, physical activity and health. World Health Organization; 2018. [Google Scholar]
- 30.Garriguet D. Diet quality in Canada. Health Rep. 2009;20(3):41–52. [PubMed] [Google Scholar]
- 31.World Health Organization-Non-Communicable diseases-Country profiles 2014. https://www.who.int/nmh/publications/ncd-profiles-2014/en/ Accessed 28 Mar 2021.
- 32.Fuentes R, Ilmaniemi N, Laurikainen E, Tuomilehto J, Nissinen A. Hypertension in developing economies: a review of population-based studies carried out from 1980 to 1998. J Hypertens. 2000;18:521–529. doi: 10.1097/00004872-200018050-00003. [DOI] [PubMed] [Google Scholar]
- 33.Mammeri A, Guermaz R, Brouri M, Tebaibia A. Prevalence of Prehypertension and its Relationship to Risk Factors for Cardiovascular Diseases in Algeria: Analysis from a Cross-Sectional Survey. Adv Card Res. 2020;3(2):282–287. doi: 10.32474/ACR.2020.03.000160. [DOI] [Google Scholar]
- 34.Yang G, Ma Y, Wang S, Su Y, Rao W, Fu Y, et al. Prevalence and correlates of prehypertension and hypertension among adults in Northeastern China: a Cross-Sectional Study. Int J Environ Res Public Health. 2016;13(1):82. doi: 10.3390/ijerph13010082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silva DA, Petroski EL, Peres MA. Prehypertension and hypertension among adults in a metropolitan area in Southern Brazil: population-based study. Rev Saude Publica. 2012;46(6):988–998. doi: 10.1590/S0034-89102012000600008. [DOI] [PubMed] [Google Scholar]
- 36.Islam SMS, Mainuddin AKM, Islam MS, Karim MA, Mou SZ, Arefin S, et al. Prevalence of risk factors for hypertension: a cross-sectional study in an urban area of Bangladesh. Global Cardiol Sci Pract. 2015;4(43). 10.5339/gcsp.2015.43. [DOI] [PMC free article] [PubMed]
- 37.Rahmanian K, Shojaie M. The prevalence of pre-hypertension and its association to established cardiovascular risk factors in South of Iran. BMC Res Notes. 2012;5:386. doi: 10.1186/1756-0500-5-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsai PS, Ke TL, Huang CJ, Tsai JC, Chen PL, Wang SY, et al. Prevalence and determinants of prehypertension status in the Taiwanese general population. J Hypertens. 2005;23:1355–1360. doi: 10.1097/01.hjh.0000173517.68234.c3. [DOI] [PubMed] [Google Scholar]
- 39.Ataklte F, Erqou S, Kaptoge S, Taye B, et al. Burden of undiagnosed hypertension in sub-saharan Africa: a systematic review and meta-analysis. Hypertension. 2015;65(2):291–298. doi: 10.1161/HYPERTENSIONAHA.114.04394. [DOI] [PubMed] [Google Scholar]
- 40.Ben Romdhane H, Ben Ali S, Skhiri H, Traissac P, Bougatef S, Maire B, et al. Hypertension among Tunisian adults: results of the TAHINA project. Hypertens Res. 2012;35(3):341–347. doi: 10.1038/hr.2011.198. [DOI] [PubMed] [Google Scholar]
- 41.Awadalla H, Elmak NE, El-Sayed EF, Almobarak AO, Elmadhoun WM, Osman M, Noor SK, Ahmed MH. Hypertension in Sudanese individuals and associated risk factors: the critical intersection between salt and sugar intake. Cardiovasc Diagn Ther. 2018;8(4):432–438. doi: 10.21037/cdt.2018.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khdour MR, Hallak HO, Shaeen M, Jarab AS, Al-Shahed QN. Prevalence awareness, treatment and control of hypertension in the Palestinian population. J Hum Hypertens. 2013;27(10):623–628. doi: 10.1038/jhh.2013.26. [DOI] [PubMed] [Google Scholar]
- 43.Cifkova R, Fodor G, Wohlfahrt P. Changes in hypertension prevalence, awareness, treatment, and control in high-, middle-, and low-Income countries: an update. Curr Hypertens Rep. 2016;18:62. doi: 10.1007/s11906-016-0669-y. [DOI] [PubMed] [Google Scholar]
- 44.El Achhab Y, Nazek L, Maalej M, Alami M, Nejjari C. Prevalence, control and risk factors related to hypertension among Moroccan adults: a multicentre study. East Mediterr Health J. 2019;25(7):447–456. doi: 10.26719/emhj.18.057. [DOI] [PubMed] [Google Scholar]
- 45.Abd El-Aty MA, Meky FA, Morsi MM, Al-Lawati JA, El Sayed MK. Hypertension in the adult Omani population: predictors for unawareness and uncontrolled hypertension. J Egypt Public Health Assoc. 2015;90(3):125–132. doi: 10.1097/01.EPX.0000470547.32952.cf. [DOI] [PubMed] [Google Scholar]
- 46.Hu L, Huang X, You C, Li J, Hong K, Li P, et al. Prevalence and Risk Factors of Prehypertension and Hypertension in Southern China. Plos One. 2017;12(1):e0170238. doi: 10.1371/journal.pone.0170238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yameogo NV, Kagambega LJ, Millogo RC, Kologo KJ, Yameogo AA, Mandi GD, et al. Factors associated with poor blood pressure control in hypertensive black Africans: cross-sectional study of 456 hypertensive patients from Burkina Faso. Annales de cardiologie et d’angeiologie. 2013;62(1):38–42. doi: 10.1016/j.ancard.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Boukli Hacène L, Meguenni K. Cardiovascular risk factors in the urban community of Tlemcen (Algeria) Cah Sante. 2007;17(3):153–158. [Google Scholar]
- 49.Hall JE, Guyton AC. Guyton and Hall textbook of medical physiology. 12. Philadelphia: Saunders Elsevier; 2011. [Google Scholar]
- 50.Franklin SS, Gustin W, 4th, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 51.Staessen JA, Celis H, Fagard R. The epidemiology of the association between hypertension and menopause. J Hum Hypertens. 1998;12(9):587–592. doi: 10.1038/sj.jhh.1000670. [DOI] [PubMed] [Google Scholar]
- 52.Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci. 2014;16(1):126–130. doi: 10.1111/nhs.12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahman M, Zaman M, Islam JY, Chowdhury J, Ahsan HN, Rahman R, et al. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. J Hum Hypertens. 2018;32:334–348. doi: 10.1038/s41371-017-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kavishe B, Biraro S, Baisley K, Vanobberghen F, Kapiga S, Munderi P, et al. High prevalence of hypertension and of risk factors for noncommunicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Med. 2015;13:126. doi: 10.1186/s12916-015-0357-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Midha T, Krishna V, Nath B, Kumari R, Rao YK, Pandey U, et al. Cut-off of body mass index and waist circumference to predict hypertension in Indian adults. World J Clin Cases. 2014;2(17):272–278. doi: 10.12998/wjcc.v2.i7.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rahmouni K, Correia MLG, Haynes WG, Mark AL. Obesity-associated hypertension: New insights into mechanisms. Hypertension. 2005;45(1):9–14. doi: 10.1161/01.HYP.0000151325.83008.b4. [DOI] [PubMed] [Google Scholar]
- 57.Bouhenni H, Daoudi H, Djemai H, Noirez P, Rouabah A, Vitiello D, et al. Relationships between metabolic profile, hypertension and uric acid with cardiometabolic risk in adolescents with abdominal obesity: impact of geodemographic factors on the prevalence of abdominal obesity. Int J Adolesc Med Health. 2017;32(2) /j/ijamh.2020.32.issue-2/ijamh-2017-0107/ijamh-2017-0107.xml. 10.1515/ijamh-2017-0107. [DOI] [PubMed]
- 58.Seow LSE, Subramaniam M, Abdin E, Vaingankar JA, Chong SA. Hypertension and its associated risks among Singapore elderly residential population. J Clin Gerontol Geriatr. 2015;6(4):125–132. doi: 10.1016/j.jcgg.2015.05.002. [DOI] [Google Scholar]
- 59.Pessinaba S, Mbaye A, Yabeta GA, Kane A, Ndao CT, Ndiaye MB, et al. Prevalence and determinants of hypertension and associated cardiovascular risk factors: data from a population-based, cross-sectional survey in Saint Louis. Senegal Cardiovasc J Afr. 2013;24(5):180–183. doi: 10.5830/CVJA-2013-030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li R, Li WC, Lun ZJ, Zhang HP, Sun Z, Kanu JS, Qiu S, Cheng Y, Liu YW. Prevalence of metabolic syndrome in mainland china: a meta-analysis of published studies. BMC Public Health. 2016;16:296. doi: 10.1186/s12889-016-2870-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of Hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 62.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27(5):963–975. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 63.Zimmerman MA, Sullivan JC. Hypertension: what’s sex got to do with its physiology? Physiology (Bethesda) 2013;28(4):234–244. doi: 10.1152/physiol.00013.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Opie LH, Seedat YK. Hypertension in sub-Saharan African populations. Circulation. 2005;112(23):3562–3568. doi: 10.1161/CIRCULATIONAHA.105.539569. [DOI] [PubMed] [Google Scholar]
- 65.Bachir Cherif A, Bouamra A, Taleb A, Nedjar R, Bouraghda A, Hamida F, et al. Differences in prevalence, treatment and control rates of hypertension between male and female in the area of Blida (Algeria) Ann Cardiol Angeiol (Paris) 2017;66:123–129. doi: 10.1016/j.ancard.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 66.The ESHRE Capri Workshop Group Hormones and cardiovascular health in women. Hum Reprod Update. 2006;12(5):483–497. doi: 10.1093/humupd/dml028. [DOI] [PubMed] [Google Scholar]
- 67.Boukli HL, Khelil MA, Chabane Sari D, Meguenni K, Meziane TA. Prevalence of cardiovascular risk factors in urban and rural communities in the Wilaya of Tlemcen (Algeria): a comparative study. Rev Epidemiol Sante Publique. 2017;65(4):277–284. doi: 10.1016/j.respe.2017.01.121. [DOI] [PubMed] [Google Scholar]
- 68.Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low- and middle-income countries: A systematic review and meta-analysis. Medicine (Baltimore) 2015;94(50):e1959. doi: 10.1097/MD.0000000000001959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ganguli MC, Grimm RH, Jr, Svendsen KH, Flack JM, Grandits GA, Elmer PJ. Higher education and income are related to a better Na:K ratio in blacks: baseline results of the Treatment of Mild Hypertension Study (TOMHS) data. Am J Hypertens. 1997;10(9 Pt 1):979–984. doi: 10.1016/s0895-7061(97)00162-3. [DOI] [PubMed] [Google Scholar]
- 70.Tobe SW, Kiss A, Szalai JP, Perkins N, Tsigoulis M, Baker B. Impact of job and marital strain on ambulatory blood pressure results from the double exposure study. Am J Hypertens. 2005;18:1046–1051. doi: 10.1016/j.amjhyper.2005.03.734. [DOI] [PubMed] [Google Scholar]
- 71.Rumball-Smith J, Nandi A, Kaufman JS. Working and hypertension: gaps in employment not associated with increased risk in 13 European countries, a retrospective cohort study. BMC Public Health. 2014;14:536. doi: 10.1186/1471-2458-14-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.D'Elia L, De Palma D, Rossi G, Strazzullo V, Russo O, Iacone R, et al. Not smoking is associated with lower risk of hypertension: results of the Olivetti Heart Study. Eur J Pub Health. 2014;24(2):226–230. doi: 10.1093/eurpub/ckt041. [DOI] [PubMed] [Google Scholar]
- 73.Cleroux J, Feldman RD, Petrella RJ. Lifestyle modifications to prevent and control hypertension. 4. Recommendations on physical exercise training. Canadian Hypertension Society, Canadian Coalition for High Blood Pressure Prevention and Control, Laboratory Centre for Disease Control at Health Canada, Heart and Stroke Foundation of Canada. CMAJ. 1999;160(Suppl 9):S21–S28. [PMC free article] [PubMed] [Google Scholar]
- 74.Vaidya A, Pokharel PK, Karki P, Nagesh S. Exploring the iceberg of hypertension: a community-based study in an eastern Nepal town. Kathmandu Univ Med J. 2007;5(3):349–359. [PubMed] [Google Scholar]
- 75.O’Connor LE, Hu EA, Steffen LM, Selvin E, Rebholz CM. Adherence to a Mediterranean-style eating pattern and risk of diabetes in a U.S. prospective cohort study. Nutr. Diabetes. 2020;10(1):8. 10.1038/s41387-020-0113-x. [DOI] [PMC free article] [PubMed]
- 76.Eman S, Chaza A, Hala G, Carla M. Physical inactivity, gender and culture in Arab countries: a systematic assessment of the literature. BMC Public Health. 2018;18:639. doi: 10.1186/s12889-018-5472-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The survey database was obtained from the STEPwise official website. Those datasets used and/or analysed during the current study are available from the first author Abdellatif Moussouni (abdellatif.moussouni@gmail.com) on reasonable request.