ABSTRACT
Background
The diagnosis of autism spectrum disorder (ASD) in Down syndrome (DS) is underestimated because it is necessary to understand which aspects of the behavioral phenotype are related to DS and which are related to ASD.
Objective
To conduct a systematic review of the literature on early identification and diagnosis of ASD in patients with DS.
Data source
The VHL, MEDLINE, Cochrane, CINAHL, Scopus, Web of Science and Embase databases were searched and data were evaluated using PRISMA.
Data synthesis
Out of 1,729 articles evaluated, 15 were selected. Although well studied, identification of ASD in DS can be difficult because of the need to understand which aspects of the behavioral phenotype are related to Down syndrome and which to autism. In this review, the prevalence of ASD was found to range from 12% to 41%. Early identification of autism risk in individuals with Down syndrome is still poorly studied, even though there are screening instruments for infants. Several instruments for diagnosing autism in individuals with Down syndrome were found, but a developmental approach is fundamental for making a clear diagnosis
Conclusions
Screening procedures are important for detecting early signs of autism risk in the first year of life. Careful evaluation methods are needed to establish the diagnosis, which include choosing appropriate tools for evaluation of development and cognition, and analysis of qualitative aspects of social interaction, among others. It has been indicated in the literature that early detection and timely accurate diagnosis, in association with an intervention, may benefit development, quality of life and social inclusion.
Keywords: Autism Spectrum Disorder, Down Syndrome, Diagnosis
RESUMO
Antecedentes:
O diagnóstico de autismo na síndrome de Down é subestimado, sendo necessário entender quais aspectos do fenótipo comportamental estão relacionados à síndrome de Down e quais são do autismo.
Objetivo
Revisão Sistemática da Literatura sobre identificação precoce e diagnóstico do Transtorno do Espectro Autista em pacientes com síndrome de Down. Fonte de dados: Busca nas bases BVS, MEDLINE, Cochrane, CINAHL, Scopus, Web of Science e Embase e avaliação pelo PRISMA.
Síntese dos dados
De 1.729 artigos avaliados, foram selecionados 15. Apesar de ser bastante estudada, a identificação do transtorno do espectro do autismo na síndrome de Down pode ser difícil devido a compreensão de quais aspectos do fenótipo comportamental estão relacionados à síndrome de Down e quais são do autismo. Nessa revisão foi encontrada variação na prevalência de 12% a 41%. A identificação precoce de risco de autismo na síndrome de Down é pouco estudada mesmo existindo instrumentos de triagem para lactentes. Sobre o diagnóstico do autismo na síndrome de Down foram encontrados diversos instrumentos, mas é necessária abordagem desenvolvimental para um diagnóstico apurado.
Conclusões
É destacada a importância de procedimentos de triagem de sinais precoces de risco de autismo ainda no primeiro ano de vida. São para estabelecimento do diagnóstico a escolha de instrumentos para a avaliação do desenvolvimento e cognição, análise dos aspectos qualitativos da interação social, dentre outros. A detecção precoce e o diagnóstico preciso no tempo correto e uma intervenção poderão beneficiar o desenvolvimento, a qualidade de vida e inclusão social.
Palavras-chave: Transtorno do Espectro Autista, Síndrome de Down, Diagnóstico
INTRODUCTION
Down Syndrome (DS) is a common chromosomal anomaly and affects around 1 in 1000 individuals 1 2 . Recent research has indicated that the prevalence of autism spectrum disorder (ASD) is higher among individuals with DS 1 .
ASD consists of a heterogeneous group of neurodevelopmental disorders that are characterized by disorders of social relations and communication, repetitive behaviors and restricted interests 3 . According to data from the CDC, this disorder affects approximately 1 in 54 individuals 4 . Another study showed that the ASD rate was 1 in 100 children born in the United States 5 . Data on the prevalence of ASD in DS vary, since studies have indicated that ASD affects between 2% and 10% of the population with DS, a rate that is higher than in the general population 2 6 .
The diagnosis of ASD in Down syndrome is underestimated, because it is necessary to understand which aspects of the behavioral phenotype are related to DS and which are related to ASD 7 .
Several standardized scales have been used to evaluate the ASD criteria 8 9 . Some researchers have recommended a developmental approach to the diagnosis of ASD among cognitively impaired children, i.e. the social or communication function needs to be qualitatively different and more impaired than the general cognitive function, for an additional ASD diagnosis to be made. Researchers taking this approach have generally reported lower ASD prevalence. Epidemiological studies using a developmental approach to estimate the prevalence of autism among children with Down syndrome are scarce 8 10 .
The discussion about which criteria and instruments should be used to diagnose ASD in DS has been the subject of some studies, because the tools generally used have been validated considering individuals who do not have specific syndromes but who do have different levels of development. Furthermore, these tools do not exclude individuals with functional disorders, such as are present in DS 2 .
In such cases, professionals should consider whether individuals’ communicative social functioning corresponds to their basal level of development. In the absence of a developmental perspective, delays that are symptoms of a social disorder, e.g. ASD, can be misinterpreted 1 2 .
Another aspect of ASD is that, when early signs of risk of this disorder are identified and the intervention occurs in the first year of life, the chances of successful therapies are greater 11 - 13 . Intervention at earlier ages is favored because this is the time of greatest potential for neural plasticity. Studies on detection and intervention mechanisms are increasingly necessary 14 15 . Identification of early signs of autism risk (before one year of age) occurs at a developmental point at which the diagnosis is more difficult to make. Intervention at this point will aim to modify the trajectory and change the prognosis 16 .
Identification of early signs of autism risk has been widely studied, since no biomarker for the diagnosis of autism currently exists. The diagnosis is still made late, at around three years of age, even though symptoms are present in the first years of life 17 . In cases of DS, the diagnosis tends to be made even later 18 .
With increasing numbers of studies on the early signs of autism risk, screening tools such as M-CHAT R have been created and tested at younger ages. In Brazil, law 13.438 recommends that formal evaluation of child development should be conducted on all infants using the Caderneta da Criança (Children's Booklet), which contains data that can guide ASD screening. Nonetheless, even with the increase in research, diagnostic tools for children, such as CARS, ADI-R and ADOS, are mainly concentrated around the age of two years. There are also tools that evaluate children in the first year, but few before the first year of life 17 .
Identification of early signs of autism risk may lead to interventions at the most appropriate time and with better results 17 . Children with DS often present considerable delay in receiving the diagnosis of ASD, and this may result in inadequate strategies 13 11 . Attending to the need for earlier interventions, tools have been used to detect signs of autism in the first months of the child's life 17 .
These interventions can prevent or minimize autism symptoms, such as premature appearance of stereotypes, isolation and communication delay. These are the symptoms that can subsequently lead to a diagnosis of ASD, particularly among children with DS 19 .
In this regard, understanding how to identify early signs of autism risk among infants and make the diagnosis of autism in the population of people with DS is important, given the propositions that are necessary in these contexts. Faced with this issue, we conducted a systematic review on ASD in DS.
METHODS
This was a systematic review of the literature based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses)20. A search was conducted in the BVS, MEDLINE, Cochrane, CINAHL, Scopus, Web of Science and Embase databases to identify the main studies that evaluated autism spectrum disorder in Down syndrome.
Search strategy
To search for articles, specific descriptors linked to Boolean operators (AND and OR) were used with the aid of parentheses - ( ) - to delimit intercalations within the same logic and quotation marks (") to identify compound words. Therefore, the descriptors were applied as follows: "Autistic Disorder" OR "Trastorno do Espectro do Autismo" OR "Transtorno do Espectro Autista" OR autismo OR "Autismo Infantil" OR "Síndrome de Kanner" OR autism OR "Autism, Early Infantile" OR "Disorder, Autistic" OR "Disorders, Autistic" OR "Early Infantile Autism" OR "Infantile Autism" OR "Infantile Autism, Early" OR "Kanner Syndrome" OR "Kanners Syndrome" OR "Autism, Infantile" OR "Kanner's Syndrome") AND (tw: "Down Syndrome" OR "Síndrome de Down" OR "Síndrome de Down" OR "Down Syndrome, Partial Trisomy 21" OR "Down's Syndrome" OR "Partial Trisomy 21 Down Syndrome" OR "Downs Syndrome" OR "Syndrome, Down" OR "Syndrome, Down's”. This search was conducted in June and July 2019.
No filters such as article language, target audience or publication deadline were added. No such limitation were imposed because the objective was to include the largest number of articles relating to the prevalence of ASD in DS.
Recruitment and selection bias
To select potentially eligible articles, after exporting the studies selected from the databases, the Rayyan software was used. This is specific software for systematic reviews, in the form of a web and mobile app http://jped.elsevier.es/pt-asthma-control-in-quality-life-articulo-S2255553619300734 21 . After importing the search results, the following steps were conducted: a) identification ‐ recruitment of studies; b) selection ‐ exclusion of duplicates and exclusion through reading of titles and abstracts; c) eligibility ‐ exclusion through full reading of the studies; and d) inclusion ‐ eligible studies, according to pre-established inclusion criteria.
The whole process was carried out by two independent researchers and was assessed by a third reviewer by reading the titles and abstracts. It should be noted that two inclusion or exclusion criteria were followed: a) articles selected by both researchers were included; and b) articles selected by only one researcher were analyzed by the third reviewer and, if these fitted the criteria, they were included. A further search was performed through reading the reference lists of the studies included in the eligibility phase (full reading of the articles).
Inclusion criteria
The criteria for inclusion of articles were the following: a) eligible cross-sectional epidemiological studies describing the prevalence of autism in the population with Down syndrome; b) eligible studies that presented the specificities of the diagnosis of autism in Down syndrome, with a detailed approach to diagnostic methods; c) eligible studies that showed the identification of signs of autism risk in the population of infants with Down syndrome; and d) no restrictions regarding age, gender, class of healthcare professional or the date of use of the service. Studies in English and Spanish were included.
Studies that did not demonstrate the criteria for the diagnosis of autism and those conducted prior to 2000 were excluded.
Data extraction
The data from each article were distributed in a table. The following information was included: country, year of publication, study design and data collection tools.
The quality of the evidence was evaluated in accordance with the criteria proposed by the EPHPP (Effective Public Health Practice Project - Quality Assessment Toll for Quantitative Studies - Annex 3) 22 These criteria evaluate the selection bias, study design, potential confounding factors, blinding of the investigator and participant, method of data collection, loss of follow-up, integrity of the intervention and appropriate analysis of the research question. Based on these criteria, studies were then classified as having weak, moderate or strong quality of evidence.
RESULTS
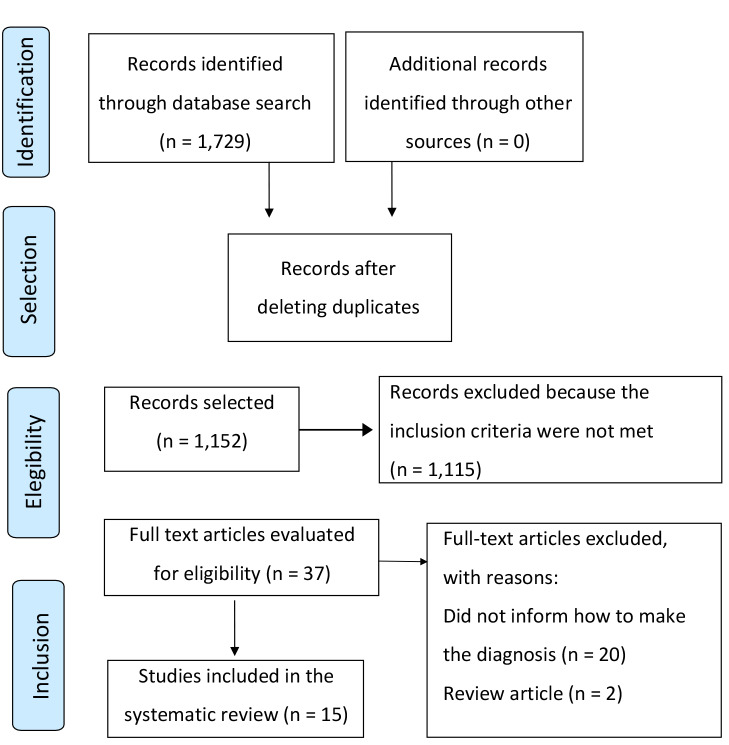
The search based on the proposed content resulted in retrieval of 1,729 articles. Out of these, 577 duplicates were excluded, and 1,149 articles were selected for reading the titles and abstracts. Through this first analysis, 37 articles were selected for full reading. Out of these, 15 articles met the inclusion criteria for review. Figure 1 shows the selection flowchart for the studies. Table 1 shows the general characteristics of the articles included in this review.
Figure 1. Flow of studies included in the review - PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses).
Table 1. General characteristics of the studies included in the systematic review*.
| Author, year | Location | Study design | Origin and sample size | Age range | Study outcome | Quality of evidence |
|---|---|---|---|---|---|---|
| Ortiz et al. 22 , 2017 | Catalonia, Spain | Retrospective cohort | Down's Medical Centre (12) | 0 to 5 years | Identification of early signs of ASD in DS | Weak |
| Starr et al. 23 , 2005 | Manchester, Liverpool and Leeds, England | Cohort | Down Syndrome Association, UK (13) | 7 to 31 years | Diagnosis of ASD in DS | Weak |
| Carter et al. 24 , 2006 | USA | Cohort | Not informed (127) | 2 to 24 years | Diagnosis of ASD in DS | Weak |
| Hepburn et al. 6 , 2007 | Denver, USA | Cohort | Mile High Down Syndrome Association (20) | 2 to 3 years | Diagnosis of ASD in DS | Weak |
| Dressler et al. 18 , 2011 | Pisa, Livorno, Bologna and Pistoia, Italy | Cohort | IRCCS Stella Maris Foundation, University of Pisa (24) | 6 to 34 years | Diagnosis of ASD in DS | Weak |
| Ji et al. 25 , 2011 | USA | Cohort | Kennedy Krieger Institute Down Syndrome Clinic (293) | 2 to 13 years | Diagnosis of ASD in DS | Weak |
| Magyar et al. 26 , 2012 | USA | Cohort | Participants in a prevalence study (71) | 4 to 14 years | Diagnosis of ASD in DS | Weak |
| Pandolfi et al. 7 , 2017 | USA | Cohort | Participants in a prevalence study (71) | 3 to 15 years | Diagnosis of ASD in DS | Weak |
| Godfrey et al. 27 , 2019 | USA | Cohort | Parents’ association (18) | Born between 1996 and 2003 | Diagnosis of ASD in DS | Weak |
| Oxelgren et al. 28 , 2019 | Uppsala, Sweden | Cohort | Uppsala University Children's Hospital (60) | 5 to 17 years | Diagnosis of ASD in DS | Weak |
| Capone et al. 29 , 2005 | Baltimore, USA | Cohort | Kennedy Krieger Institute (131) | 2 to 21 years | Diagnosis of ASD in DS | Weak |
| DiGuiseppi et al. 8 , 2010 | Colorado, USA | Cross-sectional | General population and the Mile High Down Syndrome Association (123) | 2 to 11 years | Diagnosis of ASD in DS | Weak |
| Moss et al.30, 2013 | Birmingham and London, UK | Cross-sectional | Down Syndrome Association, UK (108) | 4 to 62 years | Diagnosis of ASD in DS | Weak |
| Warner et al. 31 , 2014 | England and Wales | Cohort | Down Syndrome Association, UK (160) | 4 to 40 years | Diagnosis of ASD in DS | Weak |
Out of the studies included in the systematic review, 13 were cohort studies 7 18 23 - 28 30 32 , among which one was retrospective 23 , and two were cross-sectional 29 33 These studies were published between 2005 and 2019. The ages of the subjects ranged from two to 40 years and the sample sizes ranged from 12 to 293 people. Seven studies were conducted in European countries and eight in the United States. Regarding outcomes, only one study identified early signs of autism risk 22 In addition, nine diagnosed autism 6 7 18 24 - 29 and five, the diagnosis and prevalence of ASD in DS 8 28 30-32 The quality of the evidence was evaluated in accordance with the criteria proposed by the EPHPP and the articles were classified as having weak quality of evidence.
Among these fifteen studies included, the use of screening assessment tools and autism diagnosis varied. In the study by Ortiz et al. 22 which was the only one that aimed to identify early signs of autism risk (Table 2), we opted to use a tool based on other standardized ones, although there are mechanisms for this purpose that have already been validated. In the fourteen studies (Table 3) that presented the diagnosis of ASD as an outcome, only Capone et al. 29 did not show any use of tools validated for evaluation. Also, in relation to the diagnosis, the reference criterion varied. Six studies 24 - 28 30 33 used the DSM-IV as the reference and four 6 - 8 18 used the DSM-IV TR. One 24 additionally used the ICD-10 and another 26 additionally used the DSM-IIIR. Two studies 28 32 used the DSM-V. Three studies 28 29 31 did not report the diagnostic criterion.
Table 2. Methodological characteristics of the studies, for identifying early signs of autism risk.
| Author, year | Study design | Inclusion criteria | Sample size | Age range (years) | Autism assessment tools | Information source | Proportions of men/women |
|---|---|---|---|---|---|---|---|
| Ortiz et al. 22 , 2017 | Retrospective cohort | Individuals with DS and with SD and autism | Down's Medical Centre (12) | 0 to 5 | Modified Checklist for Autism in Toddlers (M-CHAT) and Autism Diagnostic Interview-Revised (ADI-R) | Analysis of home videos | 2:1 |
Table 3. Methodological characteristics of studies on the diagnosis and prevalence of autism in DS.
| Author, year | Inclusion criteria | Sample size | Age range (years) | Autism assessment tools | Information sources | Reference criterion for diagnosis | Diagnostic benchmark prevalence | Proportions of men/women |
|---|---|---|---|---|---|---|---|---|
| Starr et al. 23 , 2005 | Individuals with DS and severe intellectual disability | 13 | 7 to 31 | Autism Diagnostic Interview-Revised (ADI-R) and Adapted Pre-Linguistic Autism Diagnostic Observation Schedule (A-PL-ADOS) | Parents | DSM-IV and CID-10 | - | 1.16:1 |
| Carter et al. 24 , 2006 | Individuals with DS | 127 | 2 to 24 | Autism Behavior Checklist and Aberrant Behavior Checklist | Parents | DSM‐IV | - | 2.33:1 |
| Hepburn et al. 6 , 2007 | Children with SD | 20 | 2 to 3 | Autism Diagnostic Interview-Revised and Autism Diagnostic Observation Schedule-Generic | Parents | DSM-IV TR | - | 2.45:1 |
| Dressler et al. 18 , 2011 | Individuals with DS and/or autism living with their family | 24 | 6 to 34 | Childhood Autism Rating Scale (CARS) | Parents | DSM-IV TR | - | 0.84:1 |
| Ji et al. 25 , 2011 | Individuals with DS | 293 | 2 to 13 | Autism Behavior Checklist | Not informed | DSM-IIIR and DSM-IV | - | 3.16:1 |
| Magyar et al. 28 , 2012 | Individuals with DS | 71 | 4 to 14 | Archival Social Communication Questionnaire (SCQ), Autism Diagnostic Interview-Revised (ADI-R) and Autism Diagnostic Observation Schedule | Not informed | DSM-IV | - | 1.29:1 |
| Pandolfi et al. 7 , 2017 | Individuals with DS | 71 | 3 to 15 | Pervasive Developmental Disorder in Mental Retardation Scale (PDD- MRS), Social Communication Questionnaire - Lifetime Version (SCQ-L) and Autism Diagnostic Interview-Revised (ADI-R) | Parents | DSM-IV- TR | - | 1.15:1 |
| Godfrey et al. 28 , 2019 | Individuals with DS born between January 1, 1996, and December 21, 2003, and who had a caregiver who spoke English or Spanish fluently | 33 | born between 1996 and 2003 | Autism Diagnostic Observation Schedule (ADOS) and Autism Diagnostic Interview-Revised (ADI-R) | Parents | DSM-V | - | 2.01:00 |
| Oxelgren et al. 29 , 2019 | Individuals with DS | 60 | 5 to 17 | Autism Diagnostic Interview-Revised (ADI-R) and Autism Diagnostic Observation Schedule (ADOS) | Parents | Not informed | - | 1.8:1 |
| Capone et al. 29 , 2005 | Individuals with DS | 131 | 2 to 21 | Behavior questionnaires, semi-structured neurological development assessment and observation during play or social interactions | Parents | DSM-IV | 12.9% | 2.7:1 |
| DiGuiseppi et al. 8 , 2010 | Individuals with DS born between January 1, 1996, and December 21, 2003, and who had a caregiver who spoke English or Spanish fluently | 123 | 2 to 21 | Behavior questionnaires, semi-structured neurological development assessment and observation during play or social interactions | Parents | DSM-IV TR | AUT 6.4% TEA 11.8% Total 18.2% | 1.86:1 |
| Moss et al. 30 , 2013 | Participants were included if there was information on the date of birth and diagnosis of DS from a professional (physician, clinical geneticist, pediatrician or other), if at least 75% of the SCQ (Rutter et al., 2003) had been completed and if the participant with SD was at least 4 years of age. | 108 | 4 to 62 | Social Communication Questionnaire (SCQ) | Parents | Not informed | 19% | 0.7:1 |
| Warner et al. 31 , 2014 | Individuals with DS | 160 | 4 to 40 | Lifetime version of the Social Communication Questionnaire (SCQ) and Strengths and Difficulties Questionnaire | Parents | Not informed | AUT 16,5% TEA 37.7% | 1.2:1 |
Regarding prevalence, there was variation in the results among the studies, as well as in the proportions of men and women in the sample composition. There was also heterogeneity among diagnostic outcomes, such as invasive developmental disorder (according to DSM-IV), ASD and autism, which were also related to the use of each diagnostic criterion.
Among the internationally validated scales for diagnosing ASD, eleven were used in the fifteen studies included in the systematic review. Seven of the tools used have a questionnaire format, for application to the children’s guardians (ADI-R, AutBC, ABC, SCQ, SCQ-L, PDD-MRS and SDQ), and the other four tools present the possibility of observation of the individual and interviewing the person responsible for the subject (ADOS, A-PL-ADOS, CARS and MCHAT). Among the tools used, four presented the diagnostic proposal (ADI-R, ADOS, A-PL-ADOS and CARS) and seven, the screening proposal (AutBC, ABC, SCQ, SCQ-L, PDD-MRS, M-CHAT and SDQ).
The minimum age at which subjects could be evaluated using these tools was 12 months, and two tools (A-PL-ADOS and PDD-MRS) were developed to evaluate individuals with cognitive impairments. There were differences in sensitivity and specificity, as presented in the table 4. It is important to highlight that sensitivity and specificity data may vary according to the study and the number of applications of the tool.
Table 4. General characteristics of the tools used for ASD evaluation*, **, ***.
| Tool | Description | Age | Sensitivity | Specificity | Amount of use (n = 15) |
|---|---|---|---|---|---|
| Autism Diagnostic Interview- Revised (ADI-R) 34 | [Diagnosis] Standardized questionnaire in accordance with DSM-IV criteria. This is an early childhood evaluation that checks social relationships, communication and repetitive behaviors. | from 18 months | 0.52 | 0.84 | 8 |
| Autism Diagnostic Observation Schedule (ADOS) 34 35 | [Diagnosis] This is a semi-structured evaluation tool that enables observation of four areas: social interaction, communication, play and repetitive behaviors. | from 12 months | 0.94 | 0.80 | 5 |
| Adapted Pre-Linguistic Autism Diagnostic Observation Schedule (A-PL-ADOS) 36 | [Diagnosis] Tool developed for diagnosing autism that enables observation of children and adults with severe/profound cognitive impairments | from 3 years | 0.82 | 0.85 | 1 |
| Autism Behavior Checklist (AutBC) 37 | [Screening] Tool based on parents’ responses that evaluates behaviors associated with autism, in five subscales: sensory; interaction; body and object use; language; and social and self-help. | from 24 months | 0.77 | 0.91 | 2 |
| Aberrant Behavior Checklist (ABC) 38 | [Screening] This is a 58-item questionnaire that evaluates the severity of behaviors on five subscales: irritability; lethargy/social impairment; stereotyping; hyperactivity; and inadequate speech. | from 5 years | 0.4-0.74 | 0.3-0.75 | 1 |
| Childhood Autism Rating Scale (CARS) 34 | [Diagnosis] This is an tool for behavioral observations. It evaluates 15 items taking into account the symptoms for diagnosing ASD that are described in the DSM-IV | from 24 months | 0.80 | 0.88 | 2 |
| Archival Social Communication Questionnaire (SCQ) 390 | [Screening] This is a tool for evaluating individuals who are considered at risk of autism. It evaluates qualitative deficiencies in reciprocal social interaction and communication, as well as repetitive and stereotyped behavior | from 4 years | 0.88 | 0.72 | 6 |
| Social Communication Questionnaire - Lifetime Version (SCQ-L) 40 | [Screening] This version of the SCQ focuses on the child's development history, providing a total score that identifies individuals who may have autism and should be referred for a more thorough evaluation. The evaluation is practically unaffected by age, gender, language level and IQ performance | from 4 years | 0.78 | 0.47 | 1 |
| Pervasive Developmental Disorder in Mental Retardation Scale PDD- MRS 41 | [Screening] This is an ASD assessment tool that was developed for people with DS based on the DSM-IV-R criteria. It assesses the quality of social interactions with adults and colleagues, language and speech problems and aspects of behavior | from 2 years | 0.92 | 0.92 | 1 |
| Modified Checklist for Autism in Toddlers (M-CHAT) 42 | [Screening] This is a tool that is easy to apply and accessible, and it assesses psychometric properties. The caregiver responds to 23 yes/no items. Failure in three items or 2 out of 6 critical items (focus on joint attention, social orientation and imitation) indicates a risk of autism. | 18 to 24 months | 0.34 | 0.93 | 1 |
| Strengths and Difficulties Questionnaire (SDQ) 43 | [Screening] This is an evaluation of 25 items that assesses the psychological condition of children and young people. It generates scores for emotional symptoms, behavioral problems, hyperactivity, peer problems and social behavior. | 3 to 16 years | 0.63 | 0.94 | 1 |
Tests may vary according to more current versions, such as age references and values for specificity and sensitivity; **Sensitivity and specificity data may vary according to studies and the way in which the tests are applied (single or double application); ***This table reports the ASD assessment tools contained in the studies included that are standardized.
DISCUSSION
Several studies in this review evaluated identification of autism in the population with Down syndrome. It has been suggested in the existing literature that children with DS are different from those with DS and ASD 28 .
In the present study, 15 studies with poor quality of evidence, according to the criteria proposed by EPHPP (Effective Public Health Practice Project - Quality Assessment Toll for Quantitative Studies), were included. Their poor quality was mainly due to the selection bias and confounding factors present in them. In these studies, 11 different assessment tools were used, two of which are specifically directed to analysis of people with intellectual disabilities. No specific tool or scale for evaluating ASD in DS was found. The studies evaluated show that there is a need for greater dissemination of standardized scales for diagnosing ASD, since screening scales are not diagnostically definitive. It is also worth noting that in three studies it was not possible to identify the diagnostic criteria used.
Identification of early signs of autism risk has been widely studied in the general population, since the diagnosis tends to be made at the age of around three years. However, parents already report changes in the first year of life 44 .
Studies have reported that the stability of the ASD diagnosis in the general population reaches the rate of 75% around the age of three years. Identification of early signs of autism risk thus appears to provide a possibility for prevention and reduction of this disease 45 .
With the growing recognition through studies that a portion of the population with DS will present ASD in association with this, there is a need to identify early signs of risk and implement treatment as soon as these signs have been identified. This important for reducing the impacts of this comorbidity 7 .
Despite the persistent interest of the scientific community in this subject, only the study by Ortiz et. al 22 presented an outcome related to identification of early signs of autism risk in the population with DS.
In that retrospective study, the most significant early signs from the perspective of expert evaluators were identified through home videos of children who had already been diagnosed with autism. These evaluations were made through an instrument based on the Modified Checklist for Autism in Toddlers (M-CHAT) and the Autism Diagnostic Interview-Revised (ADI-R). The main findings were associated with absence of shared attention, reduced interest in other people, lack of eye contact, absence of imitation and the presence of repetitive and stereotyped movements. It was also pointed out in that study that, even with the difficulty of the DS population in processing stimuli, the clinician's watchful eye is needed in order to detect difficulties regarding shared attention and interest in social contact, and thus enable early diagnosis of ASD and effective intervention.
Screening tests are indicated for all children, including those with DS, since it is already possible to start intervention at an early age, for rehabilitation of children with a probable diagnosis of autism as a comorbidity 17 . One of the differential diagnoses of autism is intellectual disability, but it is noteworthy that both in children with DS and in those with ASD, the comorbidity of intellectual disability is also frequent, thus requiring assessment using specific cognitive scales. This differential diagnosis becomes more difficult as the cognitive impact increases 7 24 28 . Because of this complexity, it has been reported that the diagnosis of ASD in DS is made at older ages than in the general population 13 16 .
The diagnostic criteria most used as a reference, according to the studies included in the present review, were the DSM criteria. Most of the studies included in the present review used the DSM-IV and DSM-IV-TR as references, consequent to the years in which they were published 6 - 8 18 24 25 27 30 32 .
It is known that there is a relationship between intellectual disability and ASD and that, when the intellectual limitation is more significant, autism symptoms will be more evident. Thus, according to the DSM-V criteria, the individual must present a difference between these two impairments for there to be an additional diagnosis of ASD in cases of DS 33 .
In the ICD version 11, which is still in a preliminary version that is available on the WHO website, infantile autism and Asperger's syndrome are incorporated into ASD. Furthermore, categories have been created for this disorder, with and without intellectual and functional impairment 45 .
In the studies included in this review, wide variation in the prevalence of ASD in cases of DS was observed. All studies evaluating the prevalence of ASD in cases of DS found higher rates of the disorder than in the general population 8 28 30-32 . These studies also indicated that there was higher prevalence of ASD among men 8 280 30 32 and among DS individuals with greater cognitive impairment.
Several factors may influence the data on the prevalence of ASD in DS. The studies included point to possible influences relating to the diagnostic criterion used, sample recruitment method, socioeconomic aspects of the population studied, age, evaluation method (direct observation or interviews with parents or teachers), proportions between men and women and intellectual functioning. Because of all these different factors, it is not yet possible to specify the prevalence of the disorder in cases of DS. However, there is still consensus that the prevalence is higher than in the general population. This causes us to remain alert to occurrences of this comorbidity in the population with DS.
In this systematic review, the importance of applying a validated instrument for formal evaluation of ASD during the follow-up of children with DS was observed. One important point in choosing instruments is that screening tests show higher rates of false-positive ASD diagnoses in the population with DS 7 8 28 . This occurs because the screening instruments are affected by cognitive impacts and other conditions associated with DS 8 .
It has been shown that the Social Communication Questionnaire (SCQ) has higher sensitivity and lower specificity rates, when used in the population with DS. However, performance data regarding ASD assessment tools remain limited among individuals with DS 7 8 .
In the studies included in this systematic review, the tools most used were the Autism Diagnostic Interview-Revised (ADI-Re) and the Autism Diagnostic Observation Schedule (ADOS), which are diagnostic tools that have not yet been validated in Brazil. Also used was the Archival Social Communication Questionnaire (SCQ), which is a screening tool already validated for use in Brazilian populations. When using these tools, it is important to verify the necessary adjustments for lower levels of intellectual functioning, as seen in cases of intellectual disability, whenever possible 24 .
Studies have indicated that screening tools such as M-CHAT R and SCQ should be used only for initial evaluations, since they are not sufficient to determine the diagnosis 24 27 31 . Even though it has been shown that the SCQ presents good convergence with gold standard tools, this application alone is not enough for the diagnosis. Thus, the diagnosis should be reached by also considering anamnesis, interviews, physical examinations, detailed observation and application of validated diagnostic scales 27 31 .
Star et al. 24 evaluated individuals with DS in association with severe or profound intellectual disability. The Autism Diagnostic Interview-Revised (ADI-R) and Adapted Pre-Linguistic Autism Diagnostic Observation Schedule (A-PL-ADOS) were used as tools. The latter is an instrument for evaluating nonverbal children and adults who have severe and profound intellectual limitations. In a sample of 13 individuals who had DS with serious intellectual impairments, five met the diagnostic criterion for autism. That study, despite its small sample, demonstrated that not all individuals who have serious intellectual impediments will be diagnosed with ASD.
Several studies have compared the profiles of individuals with ASD and DS, and those with DS only. These data show that individuals with ASD and DS have greater social withdrawal, aggressive behaviors and anxiety and worse social engagement than children with DS 7 18 25 27 28 30 31 . In addition, individuals with both diagnoses show lower levels of adaptive functioning 18 and higher levels of repetitive and stereotyped behaviors, compared with those with DS alone 6 25 27 .
At younger ages, when verbal communication skills are still developing, and especially in cases of DS (since delayed communication is expected in such cases), these characteristics will be more related to the qualitative aspects of communication (shared attention, interest, eye contact and imitation). Repetitive movements and stereotyping may also occur 23 .
In older children, when speech is present, more stereotyped and repetitive speech is expected. When speech is absent, limitation or absence of gesticulation with communicative objectives is observed. Greater aggressiveness in social contact, lack of symbolic and functional play, as well as a tendency to align objects and have restricted interests, can also be observed 7 9 25 .
To make the diagnosis of ASD in DS, it is also necessary to consider the interference of factors associated with the syndrome. Sensory conditions, such as hearing loss and motor difficulties, for example hypotonia, can affect the time and fluidity of these individuals’ social and communicative behaviors. These signs are identified through screening methods, but differ qualitatively from the difficulty in basic social relationships seen in autism and may be misinterpreted if the examiner is not aware of the aspects relating to DS. Furthermore, it has been suggested that individuals with DS demonstrate executive function deficits that affect social and communicative relationships, but in a different way from the reciprocity problems associated with autism 8 .
Moreover, regarding the diagnosis of ASD, it is important to consider the conditions within which a differential diagnosis is necessary. Down Syndrome Disintegrative Disorder (DSDD) has been described as a clinical syndrome in which people with DS may experience adaptive, social and cognitive regression. Although DSDD may present symptoms similar to those of ASD, its onset is later, generally occurring between the first and third decades of life. Also, in DSDD there are other symptoms such as catatonia and insomnia. The differential diagnosis should be based on a comprehensive psychosocial and medical assessment of possible secondary causes of behavioral change and regression 46 .
Thus, to diagnose ASD in DS, clinicians should select appropriate tools, conduct analysis on intellectual development and functioning, make direct observations and conduct analysis on communication and social interaction and other aspects of social engagement, which are fundamental for distinguishing ASD from other developmental delays 8 .
It is also worth mentioning the challenges faced by families with regard to the diagnosis of ASD. In a systematic review of the literature, it was observed that these challenges start with the search for a diagnosis, which may take a long time to be reached. There is the difficulty in dealing with the symptoms, and even in achieving access to rehabilitation, education and leisure services. These data emphasize the need to seek a systematic approach, starting from the time at which ASD is diagnosed, through appropriate care plans and support networks for children with ASD and their families 47 . These challenges are observed in the general population and may become greater in cases in which there is already a diagnosis of DS.
The present study had limitations with regard to the methodological and diagnostic system variations present in the 15 studies included, given that these factors interfere with identifying the best diagnostic practices. Future studies should use meta-analyses to address methodologies, in order to extract psychometric data from diagnostic practices in the population with DS.
Although we were unable to identify the most appropriate tool for evaluating ASD in DS, since the psychometric qualities of these tools are not well delimited for this population, this systematic review allowed us to understand that the clinical diagnosis of ASD in DS should not focus only on test results. Clinical experience and interdisciplinary evaluation will allow greater understanding of whether there is any qualitative difference in social engagement and cognitive impairment that would justify the second diagnosis of ASD in DS.
We highlight the need for early evaluation and intervention in cases of ASD associated with DS, since these will be determinants for better development, quality of life and social inclusion.
In conclusion, individuals with DS have higher prevalence of ASD than the general population, and screening should be universal, to enable early detection of signs and effective intervention, thus improving the prognosis in relation to the potential for development and better quality of life. The present systematic review showed that use of ASD diagnostic tools in the population with DS requires careful complementary and multidisciplinary clinical evaluation. In addition, there is a need to evaluate the psychometric properties of these tools in the population with DS, and whether tools that were created to evaluate people with intellectual disabilities present more affirmative results for the population with DS.
The need for additional diagnoses of ASD among individuals with DS should be determined based on the qualitative difference between social and cognitive impairments. It is also important to highlight the need to assess signs of autism risk in the first year of life, so that it becomes possible to analyze the qualitative aspects of social interaction and thus to initiate more timely intervention.
It is necessary to provide tools for early detection of autism risk among infants and for diagnostic evaluation of ASD in DS, based on developmental analyses in healthcare services, so that better results can be achieved with earlier interventions.
References
- Irving C, Basu A, Richmond S, Burn J, Wren C. Twenty-year trends in prevalence and survival of Down syndrome. Eur J Hum Genet. 2008;16(11):1336–1340. doi: 10.1038/ejhg.2008.122. [DOI] [PubMed] [Google Scholar]
- Rachubinski AL, Hepburn S, Elias ER, Gardiner K, Shaikh TH. The co-occurrence of Down syndrome and autism spectrum disorder: is it because of additional genetic variations? Prenat Diagn. 2017;37(1):31–36. doi: 10.1002/pd.4957. [DOI] [PubMed] [Google Scholar]
- American Psychistric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-V) 5. American Psychistric Association; 2013. 991 [Google Scholar]
- Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ. 2020;69(4):1–12. doi: 10.15585/mmwr.ss6904a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandin S, Lichtenstein P, Kuja-Halkola R, Larsson H, Hultman CM, Reichenberg A. The familial risk of autism. JAMA. 2014;311(17):1770–1777. doi: 10.1001/jama.2014.4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepburn S, Philofsky A, Fidler DJ, Rogers S. Autism symptoms in toddlers with Down syndrome: a descriptive study. J Appl Res Intellect Disabil. 2008;21(1):48–57. doi: 10.1111/j.1468-3148.2007.00368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandolfi V, Caroline IM, Charles A. Screening for autism spectrum disorder in children with Down syndrome: An evaluation of the Pervasive Developmental Disorder in Mental Retardation Scale. J Intellect Dev Dis. 2017;43(1):61–72. [Google Scholar]
- DiGuiseppi C, Hepburn S, Davis JM, Fidler DJ, Hartway S, Lee NR. Screening for autism spectrum disorder in children with Down syndrome: An evaluation of the Pervasive Developmental Disorder in Mental Retardation Scale. J Dev Behav Pediatr. 2010;31:181–191. doi: 10.1097/DBP.0b013e3181d5aa6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman NC, Gray KM, Taffe JR, Cornish KM. A cross-syndrome evaluation of a new attention rating scale: the scale of attention in intellectual disability. Res Dev Disabil. 2016;57:18–28. doi: 10.1016/j.ridd.2016.06.005. [DOI] [PubMed] [Google Scholar]
- García-Primo P, Hellendoorn A, Charman T, Roeyers H, Dereu M, Roge B, et al. Screening for autism spectrum disorders: state of the art in Europe. Eur Child Adolesc Psychiatry. 2014;23(11):1005–1021. doi: 10.1007/s00787-014-0555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channell MM, Phillips BA, Loveall SJ, Conners FA, Bussanich PM, Klinger LG. Patterns of autism spectrum symptomatology in individuals with Down syndrome without comorbid autism spectrum disorder. J Neurodev Disord. 2015;7(1):5. doi: 10.1186/1866-1955-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Jones EJH, Dawson G, Kelly J, Estes A, Webb SJ. Parent-delivered early intervention in infants at risk for ASD: effects on electrophysiological and habituation measures of social attention. Autism Res. 2017;10(5):961–972. doi: 10.1002/aur.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel L, Singh A, Koegel R, Hollingsworth J, Bradshaw J. Assessing and improving early social engagement in infants. J Posit Behav Interv. 2014;16(2):69–80. doi: 10.1177/1098300713482977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laznik MC, Burnod Y. Szejer M, Kupfer MC, compilers. In: Luzes sobre a clínica e o desenvolvimento de bebês: novas pesquisas, saberes e intervenções. 2. São Paulo (SP): Instituto Langage; 2016. O ponto de vista dinâmico neuronal sobre as intervenções precoces; pp. 13–30. [Google Scholar]
- Berger JM, Rohn TT, Oxford JT. Autism as the early closure of a neuroplastic critical period normally seen in adolescence. Biol Syst Open Access. 2013;1 doi: 10.4172/2329-6577.1000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce K, Gazestani VH, Bacon E, Barnes CC, Cha D, Nalabolu S, et al. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. 2019;173(6):578–587. doi: 10.1001/jamapediatrics.2019.0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parlato-Oliveira E Saint-Georges. Parlato-Oliveira E, Szejer M. O Bebê e os desafios da cultura. São Paulo (SP): Instituto Langage; 2019. Da clínica do bebê à avaliação do tratamento: uma microanálise transdisciplinar; pp. 69–79. [Google Scholar]
- Olliac B, Crespin G, Laznik M-C, El Ganouni OCI, Sarradet J-L, Bauby C, et al. Infant and dyadic assessment in early community-based screening for autism spectrum disorder with the PREAUT grid. PLoS One. 2017;12(12):e0188831. doi: 10.1371/journal.pone.0188831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler A, Perelli V, Bozza M, Bargagna S. The autistic phenotype in Down syndrome: differences in adaptive behaviour versus Down syndrome alone and autistic disorder alone. Funct Neurol. 2011;26(3):151–158. [PMC free article] [PubMed] [Google Scholar]
- Greenspan SI, Brazelton TB, Cordero J, Solomon R, Bauman ML, Robinson R, et al. Guidelines for early identification, screening, and clinical management of children with autism spectrum disorders. Pediatrics. 2008;121(4):828–830. doi: 10.1542/peds.2007-3833. [DOI] [PubMed] [Google Scholar]
- Effective Public Health Practice Project Hamilton . R: quality assessment tool for quantitative studies. Canadá (CA): R Quality Assessment Tool for Quantitative Studies; [2019 Jul 17]. Internet. Available from: https://www.ephpp.ca/quality-assessment-tool-for-quantitative-studies/ [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz B, Videla L, Gich I, Alcacer B, Torres D, Jover I, Videla S. Early warning signs of autism spectrum disorder in people with Down syndrome. Int Med Rev Down Syndr. 2017;21(1):3–11. doi: 10.1016/j.sdeng.2017.01.001. [DOI] [Google Scholar]
- Starr EM, Berument SK, Tomlins M, Papanikolaou K, Rutter M. Brief report: autism in individuals with Down syndrome. J Autism Dev Disord. 2005;35(5):665–673. doi: 10.1007/s10803-005-0010-0. [DOI] [PubMed] [Google Scholar]
- Carter JC, Capone GT, Gray RM, Cox CS, Kaufmann WE. Autistic-spectrum disorders in Down syndrome: further delineation and distinction from other behavioral abnormalities. Am J Med Genet B Neuropsychiatr Genet. 2007;144B(1):87–94. doi: 10.1002/ajmg.b.30407. [DOI] [PubMed] [Google Scholar]
- Ji NY, Capone GT, Kaufmann WE. Autism spectrum disorder in Down syndrome: cluster analysis of aberrant behaviour checklist data supports diagnosis. J Intellect Disabil Res. 2011;55(11):1064–1077. doi: 10.1111/j.1365-2788.2011.01465.x. [DOI] [PubMed] [Google Scholar]
- Magyar CI, Pandolfi V, Dill CA. An initial evaluation of the Social Communication Questionnaire for the assessment of autism spectrum disorders in children with Down syndrome. J Dev Behav Pediatr. 2012;33(2):134–145. doi: 10.1097/DBP.0b013e318240d3d9. [DOI] [PubMed] [Google Scholar]
- Godfrey M, Hepburn S, Fidler DJ, Tapera T, Zhang F, Rosenberg CR, et al. Autism Spectrum Disorder (ASD) symptom profiles of children with comorbid Down Syndrome (DS) and ASD: a comparison with children with DS-only and ASD-only. Res Dev Disabil. 2019;89:83–93. doi: 10.1016/j.ridd.2019.03.003. [DOI] [PubMed] [Google Scholar]
- Oxelgren UW, Myrelid Å, Annerén G, Ekstam B, Göransson C, Holmbom A, et al. Prevalence of autism and attention-deficit-hyperactivity disorder in Down syndrome: a population-based study. Dev Med Child Neurol. 2017;59(3):276–283. doi: 10.1111/dmcn.13217. [DOI] [PubMed] [Google Scholar]
- Capone GT, Grados MA, Kaufmann WE, Bernad-Ripoll S, Jewell A. Down syndrome and comorbid autism-spectrum disorder: characterization using the aberrant behavior checklist. Am J Med Genet A. 2005;134(4):373–380. doi: 10.1002/ajmg.a.30622. [DOI] [PubMed] [Google Scholar]
- Moss J, Richards C, Nelson L, Oliver C. Prevalence of autism spectrum disorder symptomatology and related behavioural characteristics in individuals with Down syndrome. Autism. 2013;17(4):390–404. doi: 10.1177/1362361312442790. [DOI] [PubMed] [Google Scholar]
- Warner G, Moss J, Smith P, Howlin P. Autism characteristics and behavioural disturbances in ~ 500 children with Down's syndrome in England and Wales. Autism Res. 2014;7(4):433–441. doi: 10.1002/aur.1371. [DOI] [PubMed] [Google Scholar]
- Randall M, Egberts KJ, Samtani A, Scholten RJ, Hooft L, Livingstone N, et al. Diagnostic tests for Autism Spectrum Disorder (ASD) in preschool children. Cochrane Database Syst Rev. 2018;7(7):CD009044. doi: 10.1002/14651858.CD009044.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardo MV, Lai M-C, Baron-Cohen S. Big data approaches to decomposing heterogeneity across the autism spectrum. Mol Psychiatry. 2019;24(10):1435–1450. doi: 10.1038/s41380-018-0321-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185–212. doi: 10.1007/BF02211841. [DOI] [PubMed] [Google Scholar]
- Berument SK, Starr E, Pickles A, Tomlins M, Papanikolauou K, Lord C, et al. Pre-linguistic autism diagnostic observation schedule adapted for older individuals with severe to profound mental retardation: a pilot study. J Autism Dev Disord. 2005;35(6):821–829. doi: 10.1007/s10803-005-0027-4. [DOI] [PubMed] [Google Scholar]
- Eaves RC, Campbell HA, Chambers D. Criterion‐Related and construct validity of the pervasive developmental disorders rating scale and the autism behavior checklist. Psychol Sch. 2000;37(4):311–321. doi: 10.1002/1520-6807(200007)37:4<323::AID-PITS2>3.0.CO;2-S. [DOI] [Google Scholar]
- Rojahn J, Aman MG, Matson JL, Mayville E. The Aberrant Behavior checklist and the behavior problems inventory: convergent and divergent validity. Res Dev Disabil. 2003;24(5):391–404. doi: 10.1016/s0891-4222(03)00055-6. [DOI] [PubMed] [Google Scholar]
- Chandler S, Charman T, Baird G, Simonoff E, Loucas T, Meldrum D, et al. Validation of the social communication questionnaire in a population cohort of children with autism spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(10):1324–1332. doi: 10.1097/chi.0b013e31812f7d8d. [DOI] [PubMed] [Google Scholar]
- Sappok T, Diefenbacher A, Gaul I, Bölte S. Validity of the social communication questionnaire in adults with intellectual disabilities and suspected autism spectrum disorder. Am J Intellect Dev Disabil. 2015;120(3):203–214. doi: 10.1352/1944-7558-120.3.203. [DOI] [PubMed] [Google Scholar]
- Kraijer D, Bildt A. The PDD-MRS: an instrument for identification of autism spectrum disorders in persons with mental retardation. J Autism Dev Disord. 2005;35(4):499–513. doi: 10.1007/s10803-005-5040-0. [DOI] [PubMed] [Google Scholar]
- Stenberg N, Bresnahan M, Gunnes N, Hirtz D, Hornig M, Lie KK, et al. Identifying children with autism spectrum disorder at 18 months in a general population sample. Paediatr Perinat Epidemiol. 2014;28(3):255–262. doi: 10.1111/ppe.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cury CR, Golfeto JH. Strengths and difficulties questionnaire (SDQ): a study of school children in Ribeirão Preto. Braz J Psychiatry. 2003;25(3):139–145. doi: 10.1590/s1516-44462003000300005. [DOI] [PubMed] [Google Scholar]
- Chawarska K, Klin A, Paul R, Volkmar F. Autism spectrum disorder in the second year: stability and change in syndrome expression. J Child Psychol Psychiatry. 2007;48(2):128–138. doi: 10.1111/j.1469-7610.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- LaSalle JM. Epigenomic strategies at the interface of genetic and environmental risk factors for autism. J Hum Genet. 2013;58(7):396–401. doi: 10.1038/jhg.2013.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, et al. Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry. 2019;18(1):3–19. doi: 10.1002/wps.20611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosso M, Fremion E, Santoro SL, Oreskovic NM, Chitnis T, Skotko BG, et al. Down syndrome disintegrative disorder: a clinical regression syndrome of increasing importance. Pediatrics. 2020;145(6):e20192939. doi: 10.1542/peds.2019-2939. [DOI] [PubMed] [Google Scholar]
- Gomes PTM, Lima LHL, Bueno MKG, Araújo LA, Souza NM. Autismo no Brasil, desafios familiares e estratégias de superação: revisão sistemática. J Pediatr (Rio J) 2015;91(2):111–121. doi: 10.1016/j.jped.2014.08.009. [DOI] [PubMed] [Google Scholar]