Abstract
Epiphrenic diverticulum is a rare condition associated with esophageal motor disorder, and it is often asymptomatic, with a well-established surgical indication. The present study aims to report a case of a giant epiphrenic diverticulum in a 68-year-old male patient who, due to the symptoms, opted for surgical treatment using the daVinci® system. Robotic surgery consisting of esophageal diverticulectomy with cardiomyotomy was performed. The patient had an excellent recovery with an abbreviated hospitalization, return to food, and satisfactory routine activity.
Keywords: Chest, Diverticulum, Esophagus, Robotic, Surgery
INTRODUCTION
Esophageal diverticula are divided into cervical (pharyngoesophageal), middle third and lower third (epiphrenic). Epiphrenic diverticula are abnormal saccular protrusions of esophageal lumen through the muscle layer, caused by an increase in intra-esophageal pressure, and are commonly linked to esophageal motor disorders.1–6 They are false diverticula, due to the involvement of only the mucosa and submucosa,2–3 being very rare. In the United States, the prevalence is approximately 15 per 100,000.5 Treatment depends on the intensity of symptoms and the risk of potential complications, such as bleeding and perforation. Currently, diverticulectomy with cardiotomy and laparoscopic fundoplication is the surgical treatment of choice.3,6
CASE REPORT
A 68-year-old male patient complaining of epigastric pain, vomiting and postprandial regurgitation, dysphagia, and heartburn. Over the past three years, there has been progressive dysphagia and worsening of halitosis. The investigation started with an upper digestive endoscopy that showed a sizeable diverticular ostium, full of food waste, just above the gastroesophageal transition. For a better therapeutic plan, a contrasted esophagus-stomach-duodenal radiograph was requested, which corroborated the endoscopy's finding, presenting a sizeable diverticular formation (90.6 × 60.2 cm along the left and anterior lateral contour of the lower third of the esophagus, projecting into the posterior mediastinum. Finally, the postponement was given by a computed tomography scan of the chest, which demonstrated a sizeable diverticular formation in the lateral wall of the distal esophagus, with a large neck (20.4 cm), measuring 70.6 × 60.3 cm, in the axial plane, containing residues forming a level.
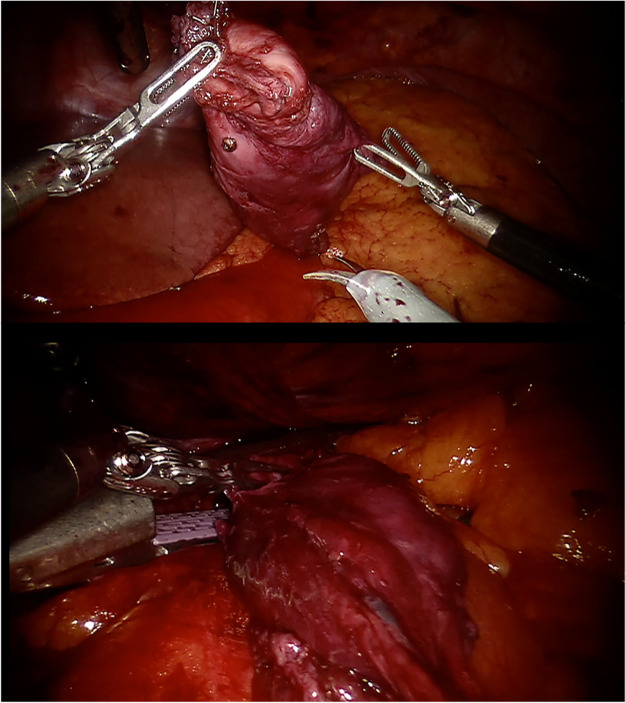
A 5 mm trocar was placed next to the xiphoid appendix to open space near the liver. A 12 mm trocar was inserted in the upper right quadrant of the abdomen in the topography of the anterior axillary line. The robotic platform was allocated, allowing the start of docking and surgery. Diverticula of the thoracic esophagus measured approximately 7 cm long and 3 cm in diameter by endoscopy. For access to the thoracic cavity was required dissection of this hiatus hernia and lysis of adhesions of the robotic arm. The diverticula approach was made by using endoscopy to empty the content and make the dissection of the cavity easier. We proceeded with the partial opening of the esophageal pillar for better closure of the diverticulum ostium and the esophageal diverticulectomy stapling with three purple loads from the universal automatic stapler iDrive Ultra, associated with esophageal myotomy. (Figure 1)
Figure 1.
Top image: Isolation of the diverticullum after careful dissection. Bottom image: Diverticulectomy using stapler. An esophageal myotomy was added after diverticulectomy to avoid recurrence.
Histopathological examination revealed an esophageal end segment measuring 7 cm long and 3 cm in diameter with irregular muscle subepithelial layer and extensive hemorrhage. The patient's postoperative evaluation was standard, without any complication, and was discharge from the hospital on the fourth day post-surgery.
DISCUSSION
The epiphrenic diverticulum is located above the lower esophageal sphincter, within 10–15 cm of the distal esophagus, usually 4–8 cm from the esophageal-gastric junction. The incidence of 15% of the diverticulum can be identified in the lower esophagus. Most presented on the right posterolateral wall, differently from what was found in the case described, in which the diverticulum presented on the left anterolateral wall.1–6
The size of the diverticula varies from 1 to 14 cm, with an average of 7.4 cm, but the severity of the symptoms is not directly related to their size.4 When symptomatic, which occurs in 15% – 20% of cases, they present with dysphagia, regurgitation, nausea and vomiting, heartburn, halitosis, weight loss, broncho aspiration, respiratory infections, and retrosternal pain.2,4
They are associated with esophageal motor disorders in more than two-thirds of cases. Reflux esophagitis can contribute to the occurrence of this type of diverticulum because of the motor disorder secondary to gastroesophageal reflux disease. Epiphrenic diverticulum is concomitant with achalasia in 60% of cases. The removal of the diverticulum is indicated when the symptoms have complications with a history of bronchoaspiration and dilated esophagus. Therefore, the treatment can be conservative in patients with a small diverticulum (less than 3 cm).7
The diagnosis is made by the contrasted examination of the esophagus-stomach-duodenum. Upper gastrointestinal endoscopy corroborates the diagnosis and is of great value in the differential diagnosis of complications. Esophageal manometry is essential to define associated motor disorders and guide treatment. And computed tomography can also be helpful in the diagnosis2,7
Surgical treatment is recommended when the patient is symptomatic or in the presence of complications, such as hemorrhage, inflammation, fistulas, and perforation to the mediastinum, or in the presence of squamous cell carcinoma, which is uncommon. Procedures that relieve obstruction below the diverticulum, such as large or short myotomies, may be associated with motor disorders.1–7
Currently, several minimally invasive alternatives are available, including procedures by thoracoscopy or by transhiatal laparoscopy. The most used access is laparoscopic, with better exposure of the gastroesophageal transition, facilitating myotomy, and fundoplication.6–8,11 The main advantages of the laparoscopic approach compared to thoracotomy is greater safety, less postoperative pain, shorter hospital stays and systemic inflammatory response, and a faster return to work activities. However, there are still few reports of similar treatment using the robotic platform that results are expected to be close to better than laparoscopy.5,9,16–21
When performed properly, these procedures have a high success rate, with few associated complications. Mortality from surgical treatment varies between 0% – 9% and morbidity, around 20%.4,10 It is crucial to perform partial fundoplication to avoid reflux disease, protecting the esophageal mucosa from possible complications.12–15
The main complications of surgical treatment are empyema, abscesses, and fistulas; which must be quickly identified and treated. In addition, failure to perform esophageal myotomy may result in a high-pressure zone of the staple line of the resected diverticulum, causing it to rupture.3,4
CONCLUSION
This case report represents the success of the treatment of a rare condition using abdominal robotic-assisted surgery. It presented outcomes similar to other minimally invasive approaches, including a short stay in the hospital and returning to usual daily activity. Alternative ways could be used performing standard surgeries; however, the robotic option is safer and reproducible in almost all world centers.
Footnotes
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Informed consent: Dr. Joao Vicente M. Grossi declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Renato Sommer, Department of Surgery, Moinhos de Vento Hospital, Porto Alegre, Brazil..
Joao Vicente Machado Grossi, Department of Surgery, Moinhos de Vento Hospital, Porto Alegre, Brazil..
Gabriela Rumi Grossi Harada, Academic of Medicine - Feevale - Novo Hamburgo, Brazil..
Mauricio Krug Seabra, Department of Surgery, Moinhos de Vento Hospital, Porto Alegre, Brazil..
Leandro Totti Cavazzola, Department of Surgery, Clinicas de Porto Alegre Hospital, Porto Alegre, Brazil..
Artur Pacheco Seabra, Department of Surgery, Moinhos de Vento Hospital, Porto Alegre, Brazil..
References:
- 1.Balci B, Kilinc G, Calik B, et al. Robotic-assisted transthoracic esophageal diverticulectomy. JSLS. 2018;22(2):e2018.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sato H, Takeuchi M, Hashimoto S, et al. Esophageal diverticulum: new perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol. 2019;25(12):1457–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinclair A. Diverticular disease of the gastrointestinal tract. Prim Care. 2017;44(4):643–654. [DOI] [PubMed] [Google Scholar]
- 4.Westcott CJ, O'Connor S, Preiss JE, et al. Myotomy-first approach to epiphrenic esophageal diverticula. J Laparoendosc Adv Surg Tech A. 2019;29(6):726–729. [DOI] [PubMed] [Google Scholar]
- 5.Howell RJ, Giliberto JP, Harmon J, et al. Open versus endoscopic surgery of Zenker's diverticula: a systematic review and meta-analysis. Dysphagia. 2019;34(6):930–938. [DOI] [PubMed] [Google Scholar]
- 6.Andrási L, Paszt A, Simonka Z, et al. Laparoscopic surgery for epiphrenic esophageal diverticulum. JSLS. 2018;22(2):e2017.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feußner H, Hüser N, Wilhelm D, et al. Operative therapie von divertikeln der speiseröhre: endoskopisch oder offen? [Surgical treatment of esophageal diverticula: endoscopic or open approach?]. Chirurg. 2017;88(3):196–203. [DOI] [PubMed] [Google Scholar]
- 8.Andolfi C, Wiesel O, Fisichella PM, et al. Surgical treatment of epiphrenic diverticulum: technique and controversies. J Laparoendosc Adv Surg Tech A. 2016;26(11):905–910. [DOI] [PubMed] [Google Scholar]
- 9.Eroglu A, Aydin Y, Altuntas B. A minimally invasive surgery for thoracic esophageal diverticula. Ann Thorac Surg. 2016;102(3):1027. [DOI] [PubMed] [Google Scholar]
- 10.Fiorelli A, Izzo AC, Arrigo E, et al. Resection of esophageal diverticulum through uniportal video-assisted thoracoscopic surgery. Ann Transl Med. 2018;6(10):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tartaglia N, Pavone G, Di Lascia A, et al. Robotic voluminous paraesophageal hernia repair: a case report and review of the literature. J Med Case Rep. 2020;14(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Connor SC, Mallard M, Desai SS, et al. Robotic versus laparoscopic approach to hiatal hernia repair: results after 7 years of robotic experience. Am Surg. 2020;86(9):1083–1087. [DOI] [PubMed] [Google Scholar]
- 13.Vasudevan V, Reusche R, Nelson E, et al. Robotic paraesophageal hernia repair: a single-center experience and systematic review. J Robot Surg. 2018;12(1):81–86. [DOI] [PubMed] [Google Scholar]
- 14.Ekeke CN, Vercauteren M, Baker N, et al. Surgical techniques for robotically-assisted laparoscopic paraesophageal hernia repair. Thorac Surg Clin. 2019;29(4):369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerull WD, Cho D, Kuo I, Arefanian S, et al. Robotic approach to paraesophageal hernia repair results in low long-term recurrence rate and beneficial patient-centered outcomes. J Am Coll Surg. 2020;231(5):520–526. [DOI] [PubMed] [Google Scholar]
- 16.Elola-Olaso AM, Mullett TW, Gagliardi RJ. Epiphrenic diverticulum: robotic-assisted transhiatal approach. Surg Laparosc Endosc Percutan Tech. 2009;19(5):e184–188. [DOI] [PubMed] [Google Scholar]
- 17.Hukkeri VS, Jindal S, Qaleem M, Tandon V, Govil D. Robotic transhiatal excision of epiphrenic diverticula. J Robot Surg. 2016;10(4):365–368. Epub May 6, 2016. [DOI] [PubMed] [Google Scholar]
- 18.Alecu L, Bărbulescu M, Ursuţ B, Braga V, Slavu I. Large oesophageal epiphrenic diverticulum resected by transhiatal robotic-assisted approach – case report. Chirurgia (Bucur). 2015;110(1):72–77. [PubMed] [Google Scholar]
- 19.Pernazza G, Monsellato I, Pende V, Alfano G, Mazzocchi P, D'Annibale A. Fully robotic treatment of an epiphrenic diverticulum: report of a case. Minim Invasive Ther Allied Technol. 2012;21(2):96–100. Epub Mar 14, 2011. [DOI] [PubMed] [Google Scholar]
- 20.Hanna JM, Onaitis MW. Robotic benign esophageal procedures. Thorac Surg Clin. 2014;24(2):223–229. [DOI] [PubMed]
- 21.Caso R, Chang H, Marshall MB. Evolving options in management of minimally invasive diverticular disease: a single surgeon's experience and review of the literature. J Laparoendosc Adv Surg Tech A. 2019;29(6):780–784. Epub Jan 8, 2019 [DOI] [PubMed] [Google Scholar]