Abstract
Background:
The COVID-19 pandemic has disproportionately affected low-income and racial/ethnic minority populations in the United States. However, it is unknown whether hospitalized patients with COVID-19 from socially vulnerable communities experience higher rates of death and/or major adverse cardiovascular events (MACEs). Thus, we evaluated the association between county-level social vulnerability and in-hospital mortality and MACE in a national cohort of hospitalized COVID-19 patients.
Methods:
Our study population included patients with COVID-19 in the American Heart Association COVID-19 Cardiovascular Disease Registry across 107 US hospitals between January 14, 2020 to November 30, 2020. The Social Vulnerability Index (SVI), a composite measure of community vulnerability developed by Centers for Disease Control and Prevention, was used to classify the county-level social vulnerability of patients’ place of residence. We fit a hierarchical logistic regression model with hospital-level random intercepts to evaluate the association of SVI with in-hospital mortality and MACE.
Results:
Among 16 939 hospitalized COVID-19 patients in the registry, 5065 (29.9%) resided in the most vulnerable communities (highest national quartile of SVI). Compared with those in the lowest quartile of SVI, patients in the highest quartile were younger (age 60.2 versus 62.3 years) and more likely to be Black adults (36.7% versus 12.2%) and Medicaid-insured (31.1% versus 23.0%). After adjustment for demographics (age, sex, race/ethnicity) and insurance status, the highest quartile of SVI (compared with the lowest) was associated with higher likelihood of in-hospital mortality (OR, 1.25 [1.03–1.53]; P=0.03) and MACE (OR, 1.26 [95% CI, 1.05–1.50]; P=0.01). These findings were not attenuated after accounting for clinical comorbidities and acuity of illness on admission.
Conclusions:
Patients hospitalized with COVID-19 residing in more socially vulnerable communities experienced higher rates of in-hospital mortality and MACE, independent of race, ethnicity, and several clinical factors. Clinical and health system strategies are needed to improve health outcomes for socially vulnerable patients.
Keywords: cardiovascular outcomes, COVID-19, ethnicity, health disparities, pandemic
What Is Known
The COVID-19 pandemic has disproportionately affected low-income and racial/ethnic minority populations in the United States.
While it is known that on a population level patients with COVID-19 residing in socially vulnerable communities have worse outcomes, it is unknown whether these patterns hold true once they are hospitalized.
What the Study Adds
Hospitalized patients from socially vulnerable communities have higher likelihood of in-hospital mortality and major adverse cardiovascular events after adjusting for demographics (age, sex, race/ethnicity) and insurance status.
These findings were not attenuated after accounting for clinical comorbidities and acuity of illness on admission, suggesting that other mechanistic pathways maybe responsible for these health disparities.
See Editorial by Khan
The COVID-19 pandemic has disproportionately affected socioeconomically disadvantaged populations in the United States.1–7 Several studies have shown that COVID-19 case rates have been highest in low-income and racial and ethnically diverse communities.8–10 At the same time, these communities have also experienced markedly higher death rates due to COVID-19.11,12
Although disparities in COVID-19 case rates and mortality have been well-documented at the ecological level, less is known about the clinical course of adults from socially vulnerable communities who are hospitalized with the disease. There are several potential reasons why hospitalized COVID-19 patients from vulnerable neighborhoods might experience worse clinical outcomes, including delays in access to hospital care, higher acuity of illness at the time of presentation, an increased likelihood of being admitted to under-resourced, overly-strained health care systems, and a higher burden of comorbid conditions that influence COVID-19 outcomes. The American Heart Association’s (AHA) COVID-19 Cardiovascular Disease (CVD) Registry is a national registry that captures detailed clinical data on patients hospitalized with COVID-19 across 107 hospitals and provides a unique opportunity to understand the association of community-level social vulnerability with outcomes among hospitalized patients. Understanding these patterns is critically important, and could inform health system, community, and public health strategies to reduce inequities in COVID-19 outcomes in the United States.
Therefore, in this study, we linked the AHA COVID-19 Registry with the Centers for Disease Control and Prevention Social Vulnerability Index (SVI)—a composite measure of community-level socioeconomic status, household composition and disability, minority status and language, and housing type and transport—to answer 3 questions.13,14 First, do patients from socially vulnerable communities who are hospitalized with COVID-19 experience worse in-hospital outcomes (death and/or major adverse cardiovascular events) than those from less vulnerable communities? If so, to what extent are these patterns explained by differences in the burden of comorbid conditions and acuity of illness at the time of admission? And third, do clinical outcomes for patients from socially vulnerable communities vary across US hospitals?
Methods
Because of the sensitive nature of the data collected for this study, requests to access the dataset from qualified researchers trained in human subject confidentiality protocols may be sent to the American Heart Association: Get With The Guidelines Hospital Level Research at qualityresearch@heart.org.
Study Population
We used the AHA COVID-19 CVD Registry, which includes COVID-19 hospitalizations across 107 hospitals in the United States, to identify adults age 18 years or older who were hospitalized with COVID-19 between January 14, 2020 and November 30, 2020. The AHA COVID-19 CVD Registry is powered by the Get With The Guidelines quality improvement program. To minimize data collection bias, partner sites are instructed to provide data on consecutive hospitalized COVID-19 patients who are 18 years or older, regardless of CVD status. Participation in this quality improvement registry was either approved or waived by the respective Institutional Review Boards (IRB) of the participating hospitals. Details on the design and deployment of the registry have been previously described.15
Data Collection
Over 200 data elements were collected including patient demographics, zip code, insurance status, hospital admission and disposition dates, presenting symptoms and admission clinical features, and disposition.15 Detailed information on hospital course including medication use and therapeutics as part of either a clinical trial or routine care were collected. Patients with incomplete clinical information were excluded from the analyses. The Get With The Guidelines programs are provided by the American Heart Association with IQVIA (Parsippany, New Jersey) serving as the data collection and coordination center. Data from the American Heart Association’s COVID-19 available through the AHA’s Precision Medicine Platform was used for the present analyses.
Social Vulnerability Index
The 2018 county-level SVI was obtained from the Centers for Disease Control and Prevention Geospatial Research, Analysis, and Services Program database.13,14 The index combines statistical data from the US Census Bureau on 15 variables, grouped into 4 themes: socioeconomic status, housing composition and disability, minority status and language, and housing type and transport (Table S1). Each of these variables are then ranked from lowest to highest vulnerability across census tracts in the United States and a county-level percentile rank is calculated for each variable, theme, and overall SVI (higher percentile ranks indicating higher social vulnerability). We cross-walked individual patient zip codes to determine the county-level SVI for each patient in the registry.16 We then categorized patients into quartiles based on their national SVI ranking, with Quartile 4 capturing those who were most socially vulnerable, consistent with prior studies.3,6
Outcomes
The primary outcome was in-hospital all-cause mortality. Secondary outcome was major adverse cardiovascular events, defined as a composite of MI, stroke, new-onset heart failure, cardiogenic shock, and death.
Statistical Analyses
Baseline demographics, clinical characteristics, admission features, and in-hospital treatments were reported as percentages for categorical variables and median and interquartile range for continuous variables by quartiles of SVI. In addition to measured values, rates of measurement are also presented. Categorical variables were compared using χ2 test, while continuous variables were compared using 2-sided t tests.
We then fit a hierarchical logistic regression model with hospital-level random intercepts to evaluate the association between SVI quartile and patient-level outcomes. Our models sequentially adjusted for each of the following variables: age and sex (Model 1), race/ethnicity (Model 2), and insurance status (Model 3). To determine whether differences in the burden of comorbidities and severity of illness at the time of presentation mediated any observed association between SVI and outcomes, we included key comorbidities (prior coronary artery disease, prior heart failure, cerebrovascular disease, atrial fibrillation/flutter, chronic kidney disease, diabetes, hypertension, smoking/e-cigarette use, cancer, pulmonary disease, immune disorder, pulmonary embolism/deep venous thrombosis, and obesity) and clinical features to account for acuity of illness at time of admission (days from symptom onset to hospital arrival, fever [temperature >38 °C], tachycardia [heart rate >100 beats/min], hypotension [systolic blood pressure <90 mm Hg], hypoxia [oxygen saturation <94% or need for supplemental oxygen], and pulmonary infiltrate present on chest radiograph or computed tomography) in Models 4 and 5, respectively. As an additional analysis, we fit linear regression models with hospital-level random intercepts to evaluate the association of each SVI subcomponent and patient-level outcomes, making similar adjustments as the primary analysis models described above.
Because changes over the course of the pandemic (eg, health system strain, care delivery) might influence the association between social vulnerability and clinical outcomes, we divided our patient population according to whether they were hospitalized during the first half of the year (January 14, 2020 to June 30, 2020) or later (July 1, 2020 to November 30, 2020). We then included an interaction term in our models to examine the association between social vulnerability and outcomes and time of year (January 14 to June 30 versus July 1 to November 30).
Statistical analyses were performed using SAS software (version 9.4, SAS Institute, Cary, NC), and 2-tailed P <0.05 were considered significant for all statistical tests.
Results
Baseline Characteristics
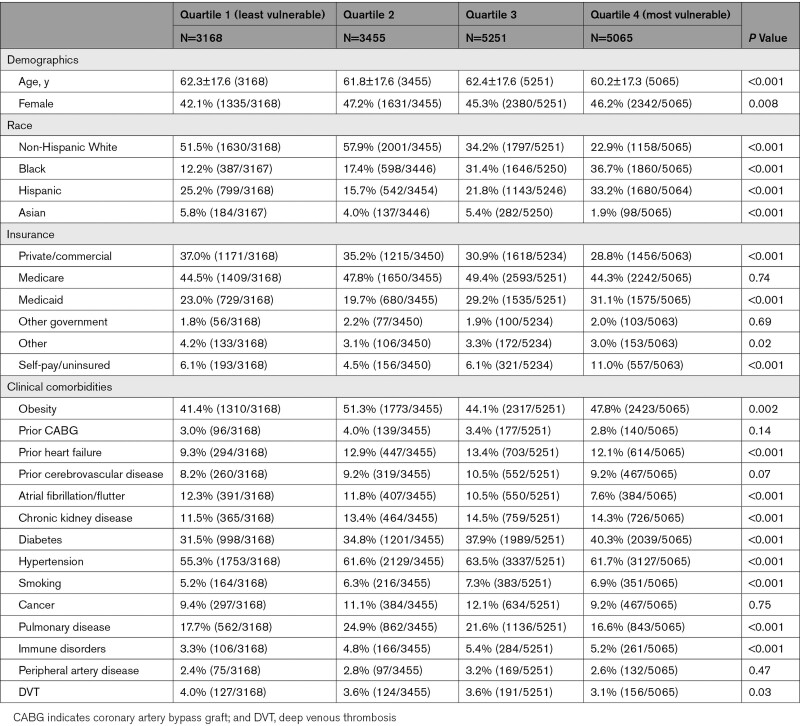
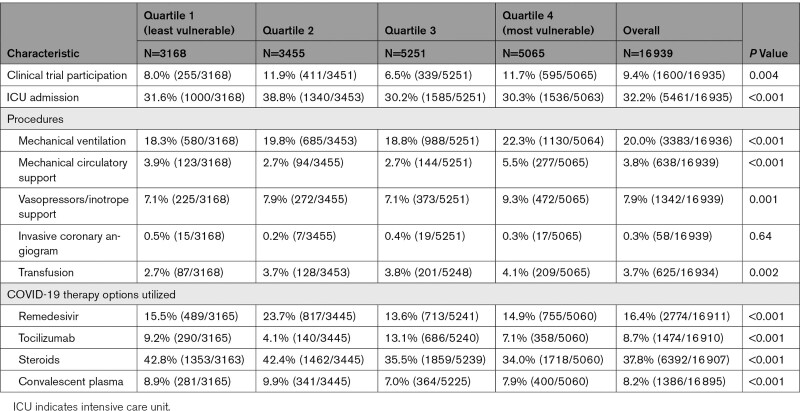
There were 20 925 patients hospitalized from January 14, 2020 to November 30, 2020, of whom 16 939 had complete clinical information and were included in the analysis (Figure S1). Patients in the most vulnerable counties (Quartile 4), compared in the least vulnerable (Quartile 1), were younger (mean age: 60.2 years versus 62.3 years; P<0.001), more likely to be Black individuals (36.7% versus 12.2%; P<0.001) and insured by Medicaid (31.1% versus 23.0%, P<0.001; Table 1). Clinical comorbidities are also shown in Table 1, while information on timing of presentation and COVID-19 diagnosis, clinical features at time of admission, and laboratory values on admission are shown in Table S2. Patients from most vulnerable counties were more likely to require mechanical ventilation (22.3% versus 18.3%; P<0.001), mechanical circulatory support (5.5% versus 3.9%; P<0.001), and vasopressor or inotrope support (9.3% versus 7.1%; P=0.001) than those from the least vulnerable counties, but were less likely to receive key therapies (steroid treatment: 34.0% versus 42.8%; P<0.001; Table 2).
Table 1.
Baseline Characteristics of Patients Hospitalized With COVID-19 by County-Level Social Vulnerability Index Quartile
Table 2.
In-Hospital Treatment Patterns for Patients Hospitalized With COVID-19 by County-Level Social Vulnerability Index Quartiles
In-Hospital Mortality
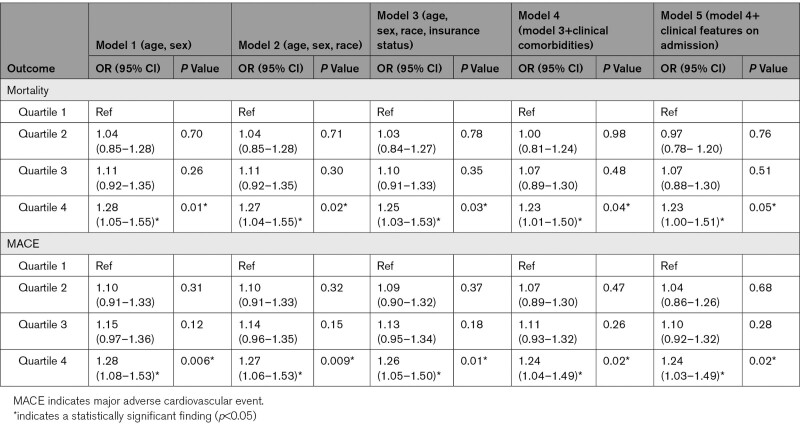
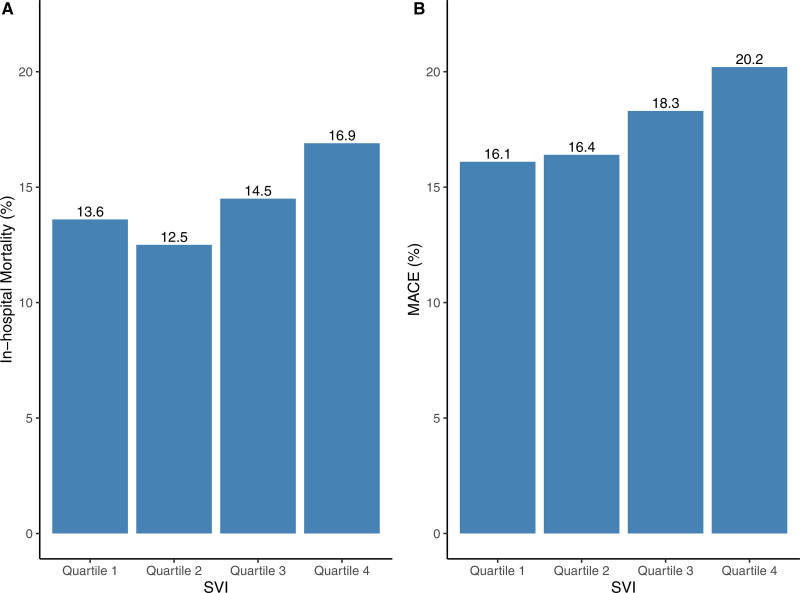
In-hospital mortality rates were higher among patients from the most vulnerable counties (16.9% in quartile 4 versus 13.6% in quartile 1; P<0.001), and these patterns were consistent across all age strata (Figure; Table S3). After adjustment for demographics (age, sex, race, insurance status) and clinical comorbidities, living in the most vulnerable neighborhoods (quartile 4) was associated with a higher likelihood of in-hospital mortality (adjusted OR, 1.23 [95% CI, 1.01–1.50]; P=0.04) relative to the least vulnerable counties (quartile 1; reference). The association was not attenuated after accounting for acuity of illness (clinical features) at the time of admission (Table 3). In the SVI subcomponent analysis, only socioeconomic status was significantly associated with in-hospital mortality (Table S4). In addition, the association between social vulnerability and in-hospital mortality was most pronounced during the first half of 2020 (interaction between social vulnerability and death and time period, 0.04; Table S5).
Table 3.
Association of County-Level Social Vulnerability With In-Hospital Mortality and MACE Among Patients Hospitalized for COVID-19
Figure.
A, In-hospital mortality and (B) major adverse cardiovascular event (MACE) rates for hospitalized COVID-19 patients by county-level social vulnerability index quartiles. Quartile 1 represents the least vulnerable quartile, while quartile 4 represents the most vulnerable quartile. MACE is defined as a composite of myocardial infarction, stroke, new-onset heart failure, cardiogenic shock and death. SVI indicates Social Vulnerability Index.
Major Adverse Cardiovascular Events
Observed rates of major adverse cardiovascular event were highest among patients from the most vulnerable counties (20.2% in quartile 4 versus 16.1% in quartile 1, P<0.001; Figure). The rate of acute coronary syndrome (ACS) was higher among COVID-19 patients from most vulnerable counties (3.4% versus 2.4%, P=0.01; Table S3), but these patients were not less likely to receive invasive coronary angiogram and/or revascularization (Table S6). Cardiac arrest (7.1% versus 3.2%; P<0.001) was more common among most vulnerable patients while other cardiovascular events (new-onset heart failure, stroke, myocarditis, ventricular arrhythmia, cardiogenic shock) occurred at similar rates between most and least vulnerable SVI quartiles (Table S4).
After adjustment for age, sex, race, and insurance status, patients living in the most vulnerable neighborhoods, compared with those from the least vulnerable counties, were more likely to experience major adverse cardiovascular event (OR, 1.26 [95% CI, 1.05–1.50]; P=0.01). The association was not significantly attenuated after adjusting for co-morbidities and acuity of illness at the time of admission (OR, 1.24 [95% CI, 1.03–1.49]; P=0.02; Table 3). In addition, these patterns did not significant differ over the course of the year (interaction between social vulnerability and major adverse cardiovascular event and time period; P=0.71; Table S5).
Discussion
In this study of patients hospitalized with COVID-19 across US hospitals, we find that those living in the most socially vulnerable counties were ≈25% more likely to experience an in-hospital death compared with individuals living in the least vulnerable counties, even after adjustment for demographics (age, sex, race) and insurance payor. These associations were most pronounced during the first wave of the COVID-19 pandemic. In addition, socially vulnerable patients were also significantly more likely to experience major adverse cardiovascular events than their less vulnerable counterparts. These patterns were not explained by differences in the burden of clinical comorbidities nor acuity of illness at the time of hospital presentation.
Given the emergence of novel variants of COVID-19, there is growing concern that persons residing in socially vulnerable communities may continue to disproportionately bear the burden of the pandemic. While ecological and population-based studies during the early phase of the pandemic found that low-income communities experienced worse COVID-19 outcomes,3,5 we use more contemporary, granular data from a national registry to demonstrate that on an individual patient-level, those from the most socially vulnerable communities experience worse in-hospital outcomes. Although Black and Latinx adults have been disproportionately affected by the pandemic due to long-standing structural and systemic inequities,11,17–19 the disparities that we observed between individuals from low versus high social vulnerability communities persisted even after accounting for race and ethnicity in our study. In addition, our finding that these patterns were not explained by differences in the underlying burden of comorbidities or severity of illness at the time of presentation is important and suggests that other factors may be driving these disparities.
There are a few potential mechanisms that might explain higher in-hospital death rates among patients from socially vulnerable communities. Living in crowded households or working in front-line jobs increases the risk of exposure to SARS-CoV-2.20 These factors may also lead to a higher viral load among patients from socially vulnerable communities,21 a variable that was not captured in our study, but is associated with increased disease severity and mortality.22 Persons residing in socially vulnerable communities also experience higher pollution burden, which is a known risk factor for COVID-19 outcomes.23 In addition, climate patterns (eg, humidity, temperature) may, at least in part, be on the causal pathway through which socially vulnerable communities have worse COVID-19 outcomes. Although differences in acuity of illness at the time of admission were generally similar across social vulnerability groups, patients from the most vulnerable neighborhoods were more likely to require mechanical ventilation, circulatory support, and vasopressors/inotropic support during their hospital stay. Disentangling the extent to which this variation in the clinical trajectory of patients during a hospitalization reflect differences in the quality or intensity of hospital care remains an important area for future study. For example, prior studies have shown that the inpatient care of socially vulnerable patients tend to be concentrated at hospitals that deliver lower quality care, and we found that patients from most vulnerable communities were less likely to be treated with important evidence-based medications (eg, steroid therapy).24
Another key finding of our study is that patients from the most socially vulnerable communities were more likely to experience major adverse cardiovascular events during hospitalization than their less vulnerable counterparts. Mounting evidence suggests a strong association between COVID-19 and acute cardiovascular injury—nearly 1 in 5 patients in our study experienced a cardiovascular event during hospitalization.25,26 Neighborhood socioeconomic disadvantage is a well-recognized risk factor for both cardiovascular risk factors and disease, and so it is perhaps not surprising that adverse cardiovascular events were most common in patients from the most vulnerable communities.27–33 Although clinical comorbidities did not fully explain the association between social vulnerability and cardiovascular events in our study, it is possible that most vulnerable patients were less likely to be on cardioprotective medications, making them more susceptible to adverse cardiovascular events. In addition, other important factors not accounted for in our study, including environmental stressors,34 may contribute to the higher risk of major adverse cardiovascular events among vulnerable patients with COVID-19 and warrant further study.
The US has repeatedly experienced resurgences of COVID-19 cases, due to emergence of novel variants. COVID-19 vaccination rates remain lowest among vulnerable-communities, due in part to reduced access and uptake.35 Socially vulnerable communities have already disproportionately borne the direct and collateral effects of the pandemic,36,37 and our findings highlight the importance of intensifying public health efforts to mitigate the spread of the disease in these communities. At the same time, our results also highlight that targeted health system strategies are needed to improve inpatient care and outcomes for socially vulnerable patients hospitalized with COVID-19. More broadly, public health strategies that expand access to COVID-19 testing38 and increase vaccination rates,39 coupled with policies that encourage vulnerable populations to seek care (eg, paid leave when infected), rather than impeding access to care (eg, public charge rule40), could help reduce inequities in COVID-19 outcomes.
Limitations
There are several limitations to consider. First, we evaluated the association between social vulnerability and clinical outcomes among hospitalized patients, and individuals with COVID-19 who were treated as an outpatient were not included. Second, our study included 107 hospitals that participated in the AHA COVID-19 CVD Registry; therefore, our results may not be generalizable to all US hospitals. However, participating hospitals are located in regions across the US, and we were able to examine detailed demographic and clinical information (eg, vitals, laboratories, treatment) about patients hospitalized with COVID-19 at these sites. Third, since data were extracted from an on-going observational quality improvement registry, clinical outcomes were not independently validated. Finally, a patient’s residential level vulnerability was assessed at the county-level rather than at the zip code level given the limitations of the dataset. Future studies should attempt to examine residential social vulnerability at a further granular level.
Conclusions
In this nationwide study of patients hospitalized with COVID-19, we find that those residing in the most socially vulnerable counties were significantly more likely to experience an in-hospital death compared with individuals living in the least vulnerable counties. These disparities were most pronounced during the first wave of the pandemic. In addition, major adverse cardiovascular event occurred more frequently among patients from the most vulnerable neighborhoods. Clinical and health system strategies are needed to improve in-hospital outcomes for socially vulnerable patients, especially during public health emergencies.
Article Information
Sources of Funding
The American Heart Association 0000031288, Abraham J. & Phyllis Katz Foundation, Byron Williams Jr, MD Fellowship Fund and the National Institutes of Health K23HL148525, R01HL164561, R01HL157530, T32 HL130025, and T32 HL007745-26A1.
Disclosures
Dr Wadhera receives research support from the National Heart, Lung, and Blood Institute (K23HL148525, R01HL164561) at the National Institutes of Health. He currently serves as a consultant for Abbott, outside the submitted work. Dr Yeh receives research support from the National Heart, Lung, and Blood Institute (R01HL157530) for the study of COVID-19 outcomes. He receives research funding and consulting fees from Abbott Vascular, AstraZeneca, Boston Scientific, and Medtronic outside of the submitted work. All other authors report no disclosures relevant to this work.
Supplemental Material
Supplemental Methods/Results
Figure S1
Tables S1–S6
Supplementary Material
Nonstandard Abbreviations and Acronyms
- AHA
- American Heart Association
- CDC
- Centers for Disease Control and Prevention
- CVD
- cardiovascular disease
- MACE
- major adverse cardiovascular event
- SVI
- Social Vulnerability Index
This manuscript was sent to Khurram Nasir, MD, MPH, MSc, Senior Guest Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCOUTCOMES.121.008612.
For Sources of Funding and Disclosures, see page 617.
Contributor Information
Shabatun J. Islam, Email: sjisla2@emory.edu.
Gargya Malla, Email: gargya.malla@gmail.com.
Robert W. Yeh, Email: bobbyyeh@gmail.com.
Arshed A. Quyyumi, Email: aquyyum@emory.edu.
Dhruv S. Kazi, Email: dkazi@bidmc.harvard.edu.
Wei Tian, Email: wtian@bidmc.harvard.edu.
Yang Song, Email: ysong5@bidmc.harvard.edu.
Aditi Nayak, Email: anayak5@emory.edu.
Anurag Mehta, Email: anurag.mehta@emory.edu.
Yi-An Ko, Email: yi-an.ko@emory.edu.
James A. de Lemos, Email: james.delemos@utsouthwestern.edu.
Fatima Rodriguez, Email: frodrigu@stanford.edu.
Abhinav Goyal, Email: agoyal4@emory.edu.
References
- 1.Gaynor TS, Wilson ME. Social vulnerability and equity: the disproportionate impact of COVID-19. Public Adm Rev. 2020;80:832–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karaye IM, Horney JA. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am J Prev Med. 2020;59:317–325. doi: 10.1016/j.amepre.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khazanchi R, Beiter ER, Gondi S, Beckman AL, Bilinski A, Ganguli I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J Gen Intern Med. 2020;35:2784–2787. doi: 10.1007/s11606-020-05882-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim SJ, Bostwick W. Social Vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav. 2020;47:509–513. doi: 10.1177/1090198120929677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nayak A, Islam SJ, Mehta A, Ko YA, Patel SA, Goyal A, Sullivan S, Lewis TT, Vaccarino V, Morris AA, et al. Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. medRxiv. 2020. doi: 10.1101/2020.04.10.20060962 [Google Scholar]
- 6.Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. PLoS One. 2021;16:e0248702. doi: 10.1371/journal.pone.0248702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nayak A, Islam SJ, Mehta A, Quyyumi AA. Letter to the editor in response to Khazanchi et al. J Gen Intern Med. 2021;36:1113–1114. doi: 10.1007/s11606-021-06594-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muñoz-Price LS, Nattinger AB, Rivera F, Hanson R, Gmehlin CG, Perez A, Singh S, Buchan BW, Ledeboer NA, Pezzin LE. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. 2020;3:e2021892. doi: 10.1001/jamanetworkopen.2020.21892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- 10.Podewils LJ, Burket TL, Mettenbrink C, Steiner A, Seidel A, Scott K, Cervantes L, Hasnain-Wynia R. Disproportionate incidence of COVID-19 infection, hospitalizations, and deaths among persons identifying as Hispanic or Latino - Denver, Colorado March-October 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1812–1816. doi: 10.15585/mmwr.mm6948a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Figueroa JF, Wadhera RK, Mehtsun WT, Riley K, Phelan J, Jha AK. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties. Healthc (Amst). 2021;9:100495. doi: 10.1016/j.hjdsi.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease control and prevention’s social vulnerability index. J Environ Health. 2018;80:34–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homeland Secur Emergency Manage. 2011;8:1–24. [Google Scholar]
- 15.Alger HM, Rutan C, Williams JH, 4th, Walchok JG, Bolles M, Hall JL, Bradley SM, Elkind MSV, Rodriguez F, Wang TY, et al. American Heart Association COVID-19 CVD registry powered by get with the guidelines. Circ Cardiovasc Qual Outcomes. 2020;13:e006967. doi: 10.1161/CIRCOUTCOMES.120.006967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson R, Din A. Understanding and enhancing the US department of housing and urban development’s ZIP code crosswalk files. Cityscape. 2018;20:277–294. [Google Scholar]
- 17.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, Spencer H, Rusek M, Anderson J, Veazie S, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021;174:362–373. doi: 10.7326/M20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez F, Solomon N, de Lemos JA, Das SR, Morrow DA, Bradley SM, Elkind MSV, Williams JH, Holmes D, Matsouaka RA, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 cardiovascular disease registry. Circulation. 2021;143:2332–2342. doi: 10.1161/CIRCULATIONAHA.120.052278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood). 2020;39:1984–1992. doi: 10.1377/hlthaff.2020.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rader B, Scarpino SV, Nande A, Hill AL, Adlam B, Reiner RC, Pigott DM, Gutierrez B, Zarebski AE, Shrestha M, et al. Crowding and the shape of COVID-19 epidemics. Nat Med. 2020;26:1829–1834. doi: 10.1038/s41591-020-1104-0 [DOI] [PubMed] [Google Scholar]
- 22.Fajnzylber J, Regan J, Coxen K, Corry H, Wong C, Rosenthal A, Worrall D, Giguel F, Piechocka-Trocha A, Atyeo C, et al. ; Massachusetts Consortium for Pathogen Readiness. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nat Commun. 2020;11:5493. doi: 10.1038/s41467-020-19057-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pozzer A, Dominici F, Haines A, Witt C, Münzel T, Lelieveld J. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc Res. 2020;116:2247–2253. doi: 10.1093/cvr/cvaa288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in South, care for sharply higher shares of elderly black, Hispanic, and medicaid patients. Health Aff (Millwood). 2011;30:1904–1911. doi: 10.1377/hlthaff.2011.0027 [DOI] [PubMed] [Google Scholar]
- 25.Chung MK, Zidar DA, Bristow MR, Cameron SJ, Chan T, Harding CV, 3rd, Kwon DH, Singh T, Tilton JC, Tsai EJ, et al. COVID-19 and cardiovascular disease: from bench to bedside. Circ Res. 2021;128:1214–1236. doi: 10.1161/CIRCRESAHA.121.317997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5:751–753. doi: 10.1001/jamacardio.2020.1105 [DOI] [PubMed] [Google Scholar]
- 27.Diez Roux AV, Mujahid MS, Hirsch JA, Moore K, Moore LV. The impact of neighborhoods on CV risk. Glob Heart. 2016;11:353–363. doi: 10.1016/j.gheart.2016.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL; Atherosclerosis Risk in Communities Study. Neighbourhood characteristics and mortality in the atherosclerosis risk in communities study. Int J Epidemiol. 2004;33:398–407. doi: 10.1093/ije/dyh063 [DOI] [PubMed] [Google Scholar]
- 29.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- 30.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the multi-ethnic study of atherosclerosis). Obesity (Silver Spring). 2013;21:621–628. doi: 10.1002/oby.20255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barber S, Hickson DA, Wang X, Sims M, Nelson C, Diez-Roux AV. Neighborhood disadvantage, poor social conditions, and cardiovascular disease incidence among African American Adults in the Jackson heart study. Am J Public Health. 2016;106:2219–2226. doi: 10.2105/AJPH.2016.303471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–589. doi: 10.1093/jurban/jtg065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Islam SJ, Kim JH, Baltrus P, Topel ML, Liu C, Ko YA, Mujahid MS, Vaccarino V, Sims M, Mubasher M, et al. Neighborhood characteristics and ideal cardiovascular health among black adults: results from the Morehouse-Emory Cardiovascular (MECA) Center for health equity. Ann Epidemiol. 2022;65:120.e1–120.e10. doi: 10.1016/j.annepidem.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Di Q, Dai L, Wang Y, Zanobetti A, Choirat C, Schwartz JD, Dominici F. Association of short-term exposure to air pollution with mortality in older adults. JAMA. 2017;318:2446–2456. doi: 10.1001/jama.2017.17923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barry V, Dasgupta S, Weller DL, Kriss JL, Cadwell BL, Rose C, Pingali C, Musial T, Sharpe JD, Flores SA, et al. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity - United States, December 14, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:818–824. doi: 10.15585/mmwr.mm7022e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77:159–169. doi: 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wadhera RK, Figueroa JF, Rodriguez F, Liu M, Tian W, Kazi DS, Song Y, Yeh RW, Joynt Maddox KE. Racial and ethnic disparities in Heart and cerebrovascular disease deaths during the COVID-19 pandemic in the United States. Circulation. 2021;143:2346–2354. doi: 10.1161/CIRCULATIONAHA.121.054378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lewis NM, Friedrichs M, Wagstaff S, Sage K, LaCross N, Bui D, McCaffrey K, Barbeau B, George A, Rose C, et al. Disparities in COVID-19 incidence, hospitalizations, and testing, by area-level deprivation - Utah, March 3-July 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1369–1373. doi: 10.15585/mmwr.mm6938a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balasuriya L, Santilli A, Morone J, Ainooson J, Roy B, Njoku A, Mendiola-Iparraguirre A, O’Connor Duffany K, Macklin B, Higginbottom J, et al. COVID-19 vaccine acceptance and access among black and latinx communities. JAMA Netw Open. 2021;4:e2128575. doi: 10.1001/jamanetworkopen.2021.28575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Figueroa J, Molina F, Sommers BD. The Trump administration’s ‘public charge’ rule and COVID-19: bad policy at the worst time. 2020. https://www.statnews.com/2020/08/21/the-trump-administrations-public-charge-rule-and-covid-19-bad-policy-at-the-worst-time/. Accessed February 5, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.