Abstract
People living in unsafe neighborhoods often report poor health. The reasons for this are multi-faceted, but one possibility is that unsafe neighborhoods create a situation of chronic stress, which may deplete people’s resources to cope with the daily stressors of life. How people respond to daily stressors (e.g., with increased self-reported negative affect and physical symptoms) is positively associated with health problems and may thus be one pathway linking perceptions of neighborhood safety to poor health. The current study investigated the relationship between neighborhood safety concerns, daily stressors, affective well-being, and physical health symptoms in a national sample of adults from the Midlife in the United States Study II (n = 1748). In 2004, participants reported neighborhood safety concerns and history of chronic stress exposure. Across eight days, they also reported daily stressors, physical symptoms and negative affect. Greater neighborhood safety concerns were associated with higher negative affect and more physical symptoms, adjusting for other sources of chronic stress. Moreover, lower perceived neighborhood safety was related to greater increases in negative affect and physical symptoms on days during which stressors were reported, even after accounting for established interactions between daily stressors and other sources of chronic stress. Exposure to neighborhoods perceived as unsafe is associated with poorer daily well-being and exacerbated responses to daily stressors, which may serve as an individual-level pathway contributing to poorer health among people living in neighborhoods perceived as unsafe.
Keywords: Affect, Stressors, Symptoms, Neighborhoods, Health
Neighborhood safety concerns and daily well-being: a national diary study
Neighborhoods are places where people live and often work and engage in recreational activities. They are also inherently social places where many interpersonal processes unfold. Because a substantial portion of a person’s time is spent in his or her neighborhood, exposure to these spaces is fairly chronic. Thus, among individuals who perceive their immediate surroundings as unsafe, neighborhoods may be a source of chronic stress. Evidence indicates that under situations of chronic stress, relatively minor daily stressors such as an argument with a member of one’s social network take a stronger toll on daily well-being. (Sliwinski et al., 2009) In turn, heightened responses to daily stressors, such as greater increases in negative affect and physical symptoms (e.g., headaches), are associated with long-term mental and physical health problems. (Charles et al., 2013; Leger et al., 2016; Piazza et al., 2013) It is well-established that individuals living in lower income neighbor-hoods are exposed to more objective, neighborhood-level stressors, such as trash in public spaces, vandalism, pollution, noise, and crime, and exposure to these types of stressors has been linked with worse health outcomes. (Aneshensel, 2010; Diez Roux and Mair, 2010) In the current study, we examine a relatively less explored question: whether perceptions of neighborhood safety are associated with daily affective and physical well-being, and whether these perceptions are linked with how people respond to the daily stressors (e.g., arguments) in their private lives (e.g., at work and at home).
Neighborhoods and health
A large literature demonstrates more prevalent and incident health problems among people with negative views of their neighborhoods. (Baum et al., 2009; Robinette et al., 2019; Robinette et al., 2017) For example, one study showed that the link between objective neighborhood socioeconomic deprivation and health was largely accounted for by an individual’s neighborhood safety concerns. (Wen et al., 2006) In addition, results of a recent co-twin control design using 686 twin pairs from the Midlife in the United States study revealed that male twins who viewed their neighborhoods as relatively less safe exhibited greater physiological dysregulation than their co-twins who viewed their neighborhoods as relatively safer. (Robinette and Beam, 2018) Findings yielded quasi-causal support for the role of perceived neighborhood safety on health among men, given that twins share some degree of their genes (100 percent among monozygotic, identical twins and 50 percent among dizygotic, fraternal twins) and completely share their early family environments when reared together, circumventing several potential third variable confounds.
This literature has also revealed individual-level pathways partially linking residents’ appraisals of their neighborhoods to health-related outcomes. For example, neighborhood safety concerns have been related to worse health behaviors such as smoking (Robinette et al., 2016) and lower levels of physical activity, 13,14 both of which predict poorer health among residents. (Meyer et al., 2014; Robinette et al., 2016) People who perceive their neighborhoods as less cohesive (i.e., neighbors cannot trust or count on one another) also exhibit worse physiological health and well-being, which is partially accounted for by more symptoms of anxiety and lower self-reported physical activity. (Robinette et al., 2016; Robinette et al., 2017) Moreover, these effects appear to have long-term repercussions. In one study, for example, 378 adolescents rated the safety of their Michigan neighborhoods when they were in the 9th grade. (Assari et al., 2015) Twelve years later, those individuals who had rated their neighborhoods in youth as unsafe were more likely to rate their health as poorer in young adulthood. In a much larger US national study, midlife and older adults reported more chronic health conditions if they had, 10 years earlier, reported lower perceived neighborhood safety. (Robinette et al., 2016) Together, this evidence indicates that neighborhood appraisals may relate to long-term health and well-being through residents’ cognitive, emotional, and behavioral functioning.
Neighborhoods and daily stress
Further research has illuminated another potential individual-level affective pathway linking neighborhood perceptions to residents’ health: through daily stress processes. In a study of US adults, for example, those living in neighborhoods perceived as cohesive reported daily stressors such as arguments less often over an eight-day diary study than did those living in areas perceived as less cohesive. (Robinette et al., 2013) Furthermore, the daily stressors that were reported by people living in cohesive neighborhoods elicited smaller increases in negative affect, even after adjusting for the well-established buffering effect of perceived support from friends, family members, and spouses. (Robinette et al., 2013) These findings indicate that neighborhood-level support may serve as a buffer against the pernicious effects of daily stressors on well-being.
At first glance, daily stressors seem fairly benign: a higher-than-normal workload, a last-minute cancellation from a baby-sitter, a disagreement with a colleague. Due to their temporary nature, these quotidian stressors are viewed as relatively innocuous. Yet, the effect of these stressors may aggregate over time. (Almeida, 2005) For example, people who respond with greater negative affect on stressor days, compared to non-stressor days, report worse mental (Charles et al., 2013) and physical health (Piazza et al., 2013) nearly a decade later. Over time, heightened responses can accumulate and exert a negative effect on health; although the stressors that people encounter vary from day-to-day, an individual’s response tendencies have important implications for their ultimate health. Thus, the proximal influences of daily stressors on affect and well-being may serve as indices of differential vulnerability shaped by individual, social, and contextual factors. (Sliwinski et al., 2009)
Moreover, because people living in unsafe neighborhoods may limit their time spent outdoors, (Bennett et al., 2007) their ability to engage socially with their neighbors or cultivate ties with those in the neighborhood who may provide informational, emotional, or instrumental support may also be reduced. (Raudenbush, 2003; Wright and Fisher, 2003) Without this social capital, people in neighborhoods perceived as unsafe may have fewer resources with which to cope with daily stressors. Residents who feel unsafe in their immediate surroundings may also experience a chronic sense of vigilance, which could gradually deplete their resources for coping with daily stressors. (Robinette et al., 2016) This hypothesis is informed by the model of reserve capacity, which states that throughout life, people acquire a reserve of resources that allows them to traverse adverse circumstances (e.g., social support, perceived control). When a stressor occurs, a person can draw on their reserve to maintain well-being. If a person has adequate reserve, they will be able to accommodate or cope successfully with the stressor. If, however, a stressor overwhelms a person beyond those reserves, decreased affective well-being results. (Gallo and Matthews, 2003) People living in unsafe neighborhoods may be exposed to situations that limit their ability to build a reserve. They also may develop habits that erode their existing reserve. For example, fearing for one’s safety may limit time spent outdoors engaging in activities that build a reserve, such as exercising and building a proximal social network. (Meyer et al., 2014; Raudenbush, 2003) Similarly, feeling unsafe in one’s neighborhood has been linked with increased vigilance and engagement in poor health habits, (Robinette et al., 2016) both of which can erode one’s physical reserve.
Research has clearly demonstrated links between low neighborhood socioeconomic status and increased exposure to neighborhood-level stressors such as crime; (Aneshensel, 2010; Diez Roux and Mair, 2010) however, there is a paucity of research investigating whether neighborhood safety concerns increase the degree to which people respond to daily stressors in the personal realm. This is an important area of inquiry, as research indicates that people who experience greater increases in negative affect and physical symptoms in relation to the minor stressors of daily life are more likely to show poorer health both in the short-term (Mallers et al., 2004; Stawski et al., 2013) and long-term. (Charles et al., 2013; Piazza et al., 2013)
To our knowledge, only two studies have examined the link between neighborhood safety perceptions and daily stressors. The first involved 96 low-income women living in the Boston area. (Caspi et al., 1987) Neighborhood safety concerns exacerbated the relationship between daily stressors and negative mood, such that negative mood increased more on stressor days (and lingered the day after stressors) among women living in neighborhoods perceived as unsafe. More recently, Scott and colleagues examined whether perceived neighborhood safety predicted negative affect in response to stressors using an ecological momentary assessment (EMA) protocol. (Scott et al., 2018) In this diverse group of 233 residents living in the same zip-code in the Bronx, people who reported lower perceived neighborhood safety experienced greater increases in negative affect following a stressor during the most recent EMA reporting period. (Scott et al., 2018) The current study extends this line of research by examining whether neighborhood safety concerns predict negative affect and physical symptom responses to daily stressors in a national US sample. Daily physical symptoms, such as a headache, muscle tension, or cough, are more likely to occur on days stressors are encountered (Almeida, 2005) and have been linked to future health problems. (Charles et al., 2013; Leger et al., 2016) Yet, no studies to our knowledge have examined the links between perceived neighborhood safety, daily stressors and physical symptoms.
The present study
The current study examines associations between neighborhood safety concerns, daily stressors, negative affect, and physical symptoms among a national sample of US men and women. We hypothesize that greater neighborhood safety concerns will be associated with higher negative affect, more physical symptoms, and greater increases in negative affect and physical symptoms in response to daily stressors within people’s private lives. Given that researchers have observed that situations of chronic stress exacerbate the effects of daily stressors on well-being, (Sliwinski et al., 2009; Hammen et al., 2009) we also examine whether our hypotheses would be supported even after adjusting for other sources of chronic stress over the lifespan and their interaction with daily stressors.
Fig. 1.
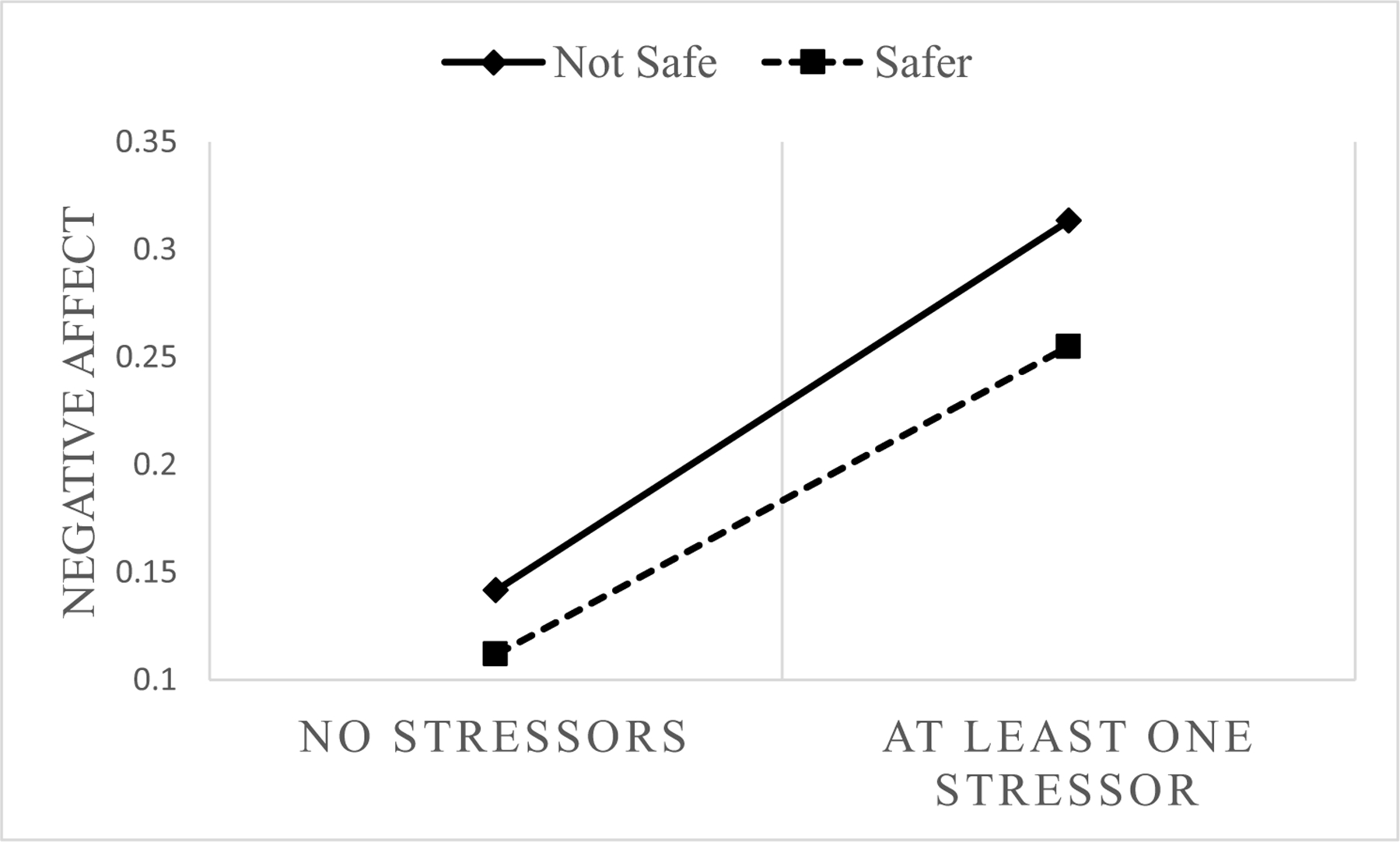
Neighborhood safety x stressor interaction in relation to negative affect among midlife and older adults. A dichotomous perceived neighborhood safety variable was constructed for visualization purposes only, where individuals providing the highest rating of neighborhood safety (a value of 4 on a 1–4 scale) were coded as Safe, and all others were coded as Not Safe, given the strong skewness of the neighborhood safety variable. Figure adjusted for race/ethnicity, individual education, sex, age, levels of neuroticism, neighborhood income, mean number of stressors over the diary period, weekday versus weekend day, and chronic stressors in childhood, adulthood, and over the lifespan as well as interactions between these sources of chronic stress and self-reported daily stressors.
Fig. 2.
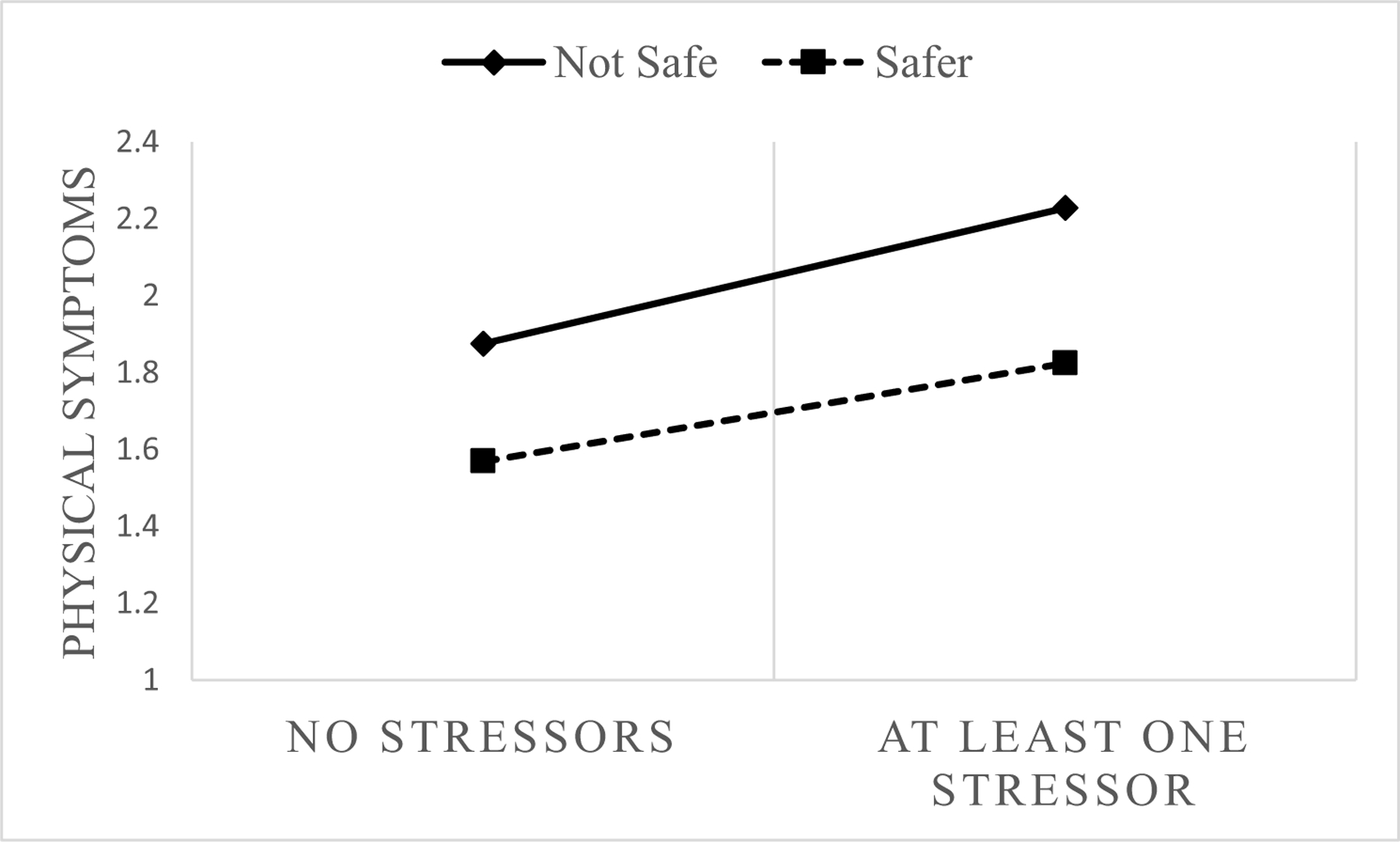
Neighborhood safety x stressor interaction in relation to physical symptoms among midlife and older adults. A dichotomous perceived neighborhood safety variable was constructed for visualization purposes only, where individuals providing the highest rating of neighborhood safety (a value of 4 on a 1–4 scale) were coded as Safe, and all others were coded as Not Safe, given the strong skewness of the neighborhood safety variable. Figure adjusted for race/ethnicity, individual education, sex, age, levels of neuroticism, neighborhood income, mean number of stressors over the diary period, weekday versus weekend day, and chronic stressors in childhood, adulthood, and over the lifespan as well as interactions between these sources of chronic stress and self-reported daily stressors.
Data and methods
Participants and procedure
This study was conducted using data from the second wave of The Midlife in the United States (MIDUS II, 2004) Survey, (Brim et al., 2004) which was originally designed to assess psychological, emotional, and physical health among midlife and older adults. MIDUS II participants reported how safe they felt in their neighborhoods and whether they experienced a series of chronic stressors over their lifetime. A subset of these participants (n = 2022) then completed the National Study of Daily Experiences II (NSDE II), an eight-day diary study collected by telephone interviews. (Almeida, 2005) Each day, participants reported whether they had experienced any stressors, physical symptoms, or negative affect. Because low-income individuals are more likely to live in neighborhoods with more disorder (noise, trash, vandalism, traffic), (Steptoe and Feldman, 2001) we also adjusted for an index of individual SES (education). The analytic sample in the present study include NSDE II participants who responded to questions about neighborhood safety and other covariates in our analytic models (n = 1748). The study was completed using ethical guidelines with the approval of The Pennsylvania State University and The University of Wisconsin’s Institutional Boards of Review.
Measures
The primary predictor variables in this study were neighborhood safety concerns, a daily stressor variable representing whether the participant had experienced any stressors on a given day, and the interaction between the two variables. The outcomes of interest, examined in separate models, were self-reported levels of negative affect and number of physical symptoms. For each outcome, we examined both the overall level (Model 1) as well as change (Model 2) in negative affect or physical symptoms in response to the constructed daily stressor variable, indicated as stressor (1) versus non-stressor (0) days.
Perceived neighborhood safety.
The MIDUS II self-administered questionnaire, completed by all MIDUS II respondents prior to enrollment in or completion of sub-studies such as NSDE II, included two items asking participants about neighborhood safety. Participants rated their agreement with the following: “I feel safe being out alone in my neighborhood during the daytime/at night”, (Keyes, 1998) using a Likert-type scale, ranging from 1 = a lot, 2 = a little, 3 = some, and 4 = not at all. Responses to these items were first reversed-coded such that higher values would represent participant’s feeling safer in their neighborhoods for ease of interpretation. These items were then averaged so that higher mean scores indicated that individuals felt safer in their neighborhoods.
Stressors.
After completion of the MIDUS II self-administered questionnaire, a subset of respondents completed NSDE II. NSDE II participants completed daily telephone interviews over an eight-day period in which they reported any daily stressors they had experienced using the Daily Inventory of Stressful Experiences (DISE). (Almeida et al., 2002) Stressors included arguments; avoided arguments; stressors at work, school, or at home; discrimination; network stressors (i.e., experienced by a member of your social network); and any other stressors.
Stressor data were examined in two separate ways. First, for each of the study days, a dichotomous variable was constructed which indicated either that no stressors were reported (coded 0) or that one or more stressors were reported that day (coded 1). This dichotomous variable was used as a primary predictor variable in all models. Second, the total number of stressors across all types of stressors were summed for each day. The totals that were generated for each of the study days were then averaged over the eight days, allowing for the construction of a variable defining the average number of stressors reported over the diary period. (Hoffman and Stawski, 2009) This person-level variable was used as a covariate in our statistical models, given that people who experience, on average, more daily stressors over the diary period may experience greater increases in negative affect or physical symptoms in response to each individual stressor that is reported.
Negative affect.
Each day, NSDE II participants reported how often they had experienced 14 negative emotions (e.g., restless, nervous, worthless) since the previous telephone interview; (Almeida and Kessler, 1998; Mroczek and Kolarz, 1998; Watson et al., 1988) Interviews were conducted once a day over the eight-day diary period, such that participants were asked about their negative affect in the previous 24 hours. Responses ranged from 0 (none of the time) to 4 (all of the time). Higher averaged values represented higher negative affect. Reliability for the negative affect scale across negative affect items within day ranged from α=0.83–0.85 across each of the eight study days.
Physical symptoms.
During each interview, NSDE II participants were asked if they had experienced any of 28 physical symptoms since the previous interview. Symptoms included items such as headache, nausea, and fatigue. (Larsen and Kasimatis, 1991) Items for which respondents answered ‘yes’ were summed so that higher values reflected more physical symptoms.
Covariates.
The primary aim of the present analyses was to determine whether living in a neighborhood perceived as unsafe (assessed in MIDUS II) would be related to well-being and changes to well-being in response to daily stressors (assessed in NSDE II). Given previous research indicating that chronic stressors amplify the effects of acute stressors on well-being, (Hammen et al., 2009) we included childhood, recent, and lifetime (major) stressors and their interactions with daily (minor) stressors as covariates in our models. Childhood events included 9 items (e.g., repeated a year/dropped out of school, father/mother unemployed, parental drinking/drug problems) to which participants reported yes (coded 1) or no (coded 0). Recent events, or those that occurred within the previous five years, included 20 items (yes = 1/no = 0) such as fired from job, unemployed, parents died or divorced, spouse engaged in infidelity, sibling or child died, loss of home, physically or sexually assaulted, or incarcerated. Lifetime stressors included the same list of 20 items (yes = 1/no = 0), plus an additional three (homelessness, no home telephone, divorced or widowed), but were reported to have occurred more than 5 years ago. ‘Yes’ responses were summed across the 9 childhood, 20 recent (within the last 5 years), and 23 lifetime (more than 5 years ago) stressors, creating three separate count variables, with higher values indicating a greater number of childhood, recent, or lifetime stressors.
Median household income of the census tract was collected from the 2000 U.S. decennial census data set to minimize concern that significant findings are driven by area-based poverty. An incremental census tract income variable was created so that estimates could be interpreted as the change in outcome (e.g., negative affect, physical symptoms) for every $10,000 increase in census tract income. Participants were asked about their highest level of education, which was re-coded as 0 = less than high school, 1 = high school or GED, 2 = some college, 3 = 4-year degree, 4 = some graduate school or higher. Age was coded in five-year increments, and we also included gender as a covariate. Given the small proportion of people from all racial/ethnic groups other than non-Hispanic white in this sample, race/ethnicity was included as a dichotomous indicator, coded 0 = non-Hispanic White and 1 = “Other.” We also included levels of neuroticism to adjust for potential common source bias. Levels of neuroticism were assessed with four items assessing the degree to which participants felt moody, worrying, nervous, or calm. (Rossi AS. Chapter 7 2001) Responses to these items ranged from 1 (a lot) to 4 (not at all), with the item assessing ‘calm’ reverse-coded. Higher scores on the averaged variable indicated higher levels of neuroticism (α = 0.75).
Statistical analyses
To examine whether neighborhood safety concerns were related to self-reported negative affect and physical symptoms, and whether these neighborhood safety concerns were related to the magnitude of change in negative affect and physical symptoms in response to daily stressors, we conducted multi-level models using SAS PROC MIXED. In these analyses, daily stressors, negative affect, and physical symptoms (Level 1) are nested within-person (Level 2). Daily stressors, negative affect, and physical symptoms were not expected to be stable, but rather to fluctuate over the eight-day diary period. In Model 1, for each outcome (negative affect or physical symptoms), we predicted that daily stressors, an individual-level and time-varying variable, would partially explain daily variability in negative affect and physical symptoms, adjusting for individual education, age, gender, race/ethnicity neighborhood income, the average number of stressors reported over the diary period, whether reports were given on a weekday or over the weekend, and levels of neuroticism. In Model 2, we examined the robustness of this hypothesized main effect by further adjusting for chronic stressors in childhood, adulthood, and over the lifespan.
The first novel contribution of our research to this literature, how-ever, is the additional hypothesis that neighborhood safety concerns would exacerbate the links between daily stressors and self-reported levels of negative affect and physical symptoms. In Model 3 for each outcome, we added an interaction term between the daily stressor variable (0 = no stressors reported that day, 1 = at least one stressor reported that day) and perceptions of neighborhood safety. We hypothesized that people living in neighborhoods perceived as less safe would show greater increases in negative affect and physical symptoms on stressor days, relative to non-stressor days, compared to those living in neighborhoods perceived as safer. As a more stringent test of this hypothesis, we further adjusted for interactions between self-reported daily stressors and childhood, adulthood, and lifetime chronic stressors in Model 4.
Results
A description of the participants can be found in Table 1. People generally reported feeling safe in their neighborhoods. Levels of negative affect were somewhat low on a scale from 0–4, and although there was a fairly large range, on average, participants reported few physical symptoms. Participants, on average, reported few chronic stressors in childhood, adulthood, and over the lifespan. The sample was fairly well-educated, with roughly 70% having achieved some college or more education. Participants lived in neighborhoods spanning a wide range of median household income levels. The sample was primarily non-Hispanic White and included slightly more women than men.
Table 1.
Description of midlife and older adult participants, n = 1748.
| M (sd) | Range | |
|---|---|---|
| Negative Affect | 0.19 (0.25) | 0.0–2.54 |
| Physical Symptoms | 1.84 (1.84) | 0.0–16.4 |
| Neighborhood Safety | 3.67 (0.50) | 1.0–4.0 |
| Individual Education | ||
| Less than High School | 4.98% | |
| High School or GED | 24.43% | |
| Some College | 30.03% | |
| 4-Year Degree | 20.77% | |
| Some Graduate School | 19.79% | |
| Neighborhood Income ($) | 48,694 (20,183) | 10,457–169,559 |
| Average Number of Stressors | 0.53 (0.46) | 0.0–4.0 |
| Age | 56.72 (12.18) | 33–84 |
| Gender (% female) | 56.41 | |
| Race/Ethnicity | ||
| White | 92.73% | |
| Black | 3.09% | |
| Native American | 1.37% | |
| Asian | 0.34% | |
| Other | 2.46% | |
| Childhood Stressors | 1.11 (1.13) | 0–7 |
| Adulthood Stressors | 0.37 (0.67) | 0–6 |
| Lifetime Stressors | 2.83 (2.02) | 0–11 |
Negative affect
Results of Model 1 indicated that people reporting at least one stressor on any day (compared to reporting no stressors) had significantly higher negative affect (coef. = 0.16, p < 0.001). People living in neighborhoods perceived as less safe (people reported lower safety) reported significantly higher levels of negative affect, as indicated by the negative coefficient in Table 2 (coef. = −0.05, p < 0.001). Achieving lower levels of education and reporting more symptoms of neuroticism and more stressors over the diary period were each significantly associated with higher negative affect. People generally reported higher negative affect on weekdays relative to days that fell on a weekend.
Table 2.
Multi-level models predicting negative affect among midlife and older adults (est. [SE]), n = 1748.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | 0.29 (0.06) | 0.25 (0.06) | 0.06 (0.04) | 0.09 (0.04) |
| Stressor Day a | 0.16*** (0.00) | 0.16*** (0.00) | 0.16*** (0.00) | 0.16*** (0.00) |
| Neighborhood Safety | −0.05*** (0.01) | −0.05*** (0.01) | 0.08*** (0.01) | 0.08*** (0.01) |
| Stressor Day x Neighborhood Safety | −0.04*** (0.01) | −0.04*** (0.01) | ||
| Age | −0.00 (0.00) | 0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Gender | −0.01 (0.01) | −0.01 (0.01) | −0.01 (0.01) | −0.01 (0.01) |
| Individual Education | −0.01** (0.00) | −0.01 (0.00) | −0.01 (0.00) | −0.01 (0.00) |
| Neighborhood Income | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Weekend b | −0.03*** (0.00) | −0.03*** (0.00) | −0.03*** (0.00) | −0.03*** (0.00) |
| Other Race/Ethnicity c | −0.01(0.02) | −(0.01) (0.02) | −0.01 (0.02) | −0.02 (0.02) |
| Average Stressors | 0.16*** (0.01) | 0.15*** (0.01) | 0.15*** (0.01) | 0.15*** (0.01) |
| Levels of Neuroticism | 0.10*** (0.01) | 0.09*** (0.01) | 0.09*** (0.01) | 0.09*** (0.01) |
| Childhood Stressors | 0.01* (0.00) | 0.01* (0.00) | 0.01* (0.00) | |
| Recent Stressors | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) | |
| Lifetime Stressors | 0.01* (0.00) | 0.01* (0.00) | 0.01* (0.01) | |
| Stressor Day x Childhood Stressors | 0.00 (0.01) | |||
| Stressor Day x Recent Stressors | 0.02*** (0.00) | |||
| Stressor Day x Lifetime Stressors | 0.02*** (0.00) |
Note. In Models 3 and 4, z scores representing neighborhood safety concerns and all chronic stress variables were used for interpretation of main effects in models with interaction terms.
Compared to non-stressor day
Compared to week day
Compared to non-Hispanic Whites; Gender coded 1 = men, 2 = women
P < .05
P < .01
P < .001; two-tailed test
Table 3.
Multi-level models predicting physical symptoms among midlife and older adults (est. [SE]), n = 1748
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | 1.26 (0.50) | 0.39 (0.50) | −0.80 (0.33) | −0.22 (0.33) |
| Stressor Day a | 0.30*** (0.03) | 0.30*** (0.03) | 0.30*** (0.03) | 0.30*** (0.03) |
| Neighborhood Safety | −0.39*** (0.09) | −0.32*** (0.08) | 0.43*** (0.09) | 0.42*** (0.09) |
| Stressor Day x Neighborhood Safety | −0.18*** (0.05) | −0.15** (0.05) | ||
| Age | 0.08*** (0.02) | 0.08*** (0.02) | 0.08*** (0.02) | 0.08*** (0.02) |
| Gender | 0.22** (0.09) | 0.31*** (0.08) | 0.31*** (0.08) | 0.31*** (0.08) |
| Individual Education | −0.18*** (0.04) | −0.12*** (0.04) | −0.12*** (0.04) | −0.12*** (0.04) |
| Neighborhood Income | −0.04 (0.02) | −0.03 (0.02) | −0.03 (0.02) | −0.03 (0.02) |
| Weekend b | −0.16*** (0.03) | −0.16*** (0.03) | −0.16*** (0.03) | −0.16*** (0.03) |
| Other Race/Ethnicityc | 0.11 (0.16) | −0.00 (0.16) | 0.00 (0.16) | 0.01 (0.16) |
| Average Stressors | 0.93***(0.10) | 0.76*** (0.10) | 0.76*** (0.10) | 0.76*** (0.10) |
| Levels of Neuroticism | 0.53*** (0.07) | 0.49*** (0.07) | 0.49*** (0.07) | 0.49*** (0.07) |
| Childhood Stressors | 0.15*** (0.04) | 0.15*** (0.04) | 0.18*** (0.05) | |
| Recent Stressors | 0.24*** (0.06) | 0.24*** (0.06) | 0.20*** (0.05) | |
| Lifetime Stressors | 0.11*** (0.02) | 0.11*** (0.02) | 0.32*** (0.05) | |
| Stressor Day x Childhood Stressors | 0.02 (0.03) | |||
| Stressor Day x Recent Stressors | 0.04 (0.03) | |||
| Stressor Day x Lifetime Stressors | 0.15 (0.03) |
Note. In Models 3 and 4, z scores representing neighborhood safety concerns and all chronic stress variables were used for interpretation of main effects in models with interaction terms.
P < .05
P < .01
P < .001; two-tailed test
Compared to non-stressor day
Compared to week day
Compared to non-Hispanic Whites; Gender coded 1 = men, 2 = women
In Model 2, chronic stress in childhood, adulthood, and over the lifespan were included as covariates. Model results remained unchanged after the inclusion of these additional covariates, with a greater number of stressors reported in childhood and over the lifespan significantly associated with higher negative affect. Stressors that were unique to adulthood (i.e., those that were reported within the previous five years) were not significantly associated with negative affect.
The neighborhood safety x daily stressor interaction was added in Model 3. The interaction was significant and revealed that negative affect was higher on stressor days relative to non-stressor days, and this was more pronounced for those living in neighborhoods perceived as less safe (coef. = −0.04, p < 0.001). In Model 4, we tested the robustness of this significant interaction by including all interactions between daily stressors and chronic stressors from childhood, adulthood, and over the lifespan. In this final model, the significant interaction between daily stressors and neighborhood safety concerns remained (coef. = −0.04, p < 0.001). Chronic stressors over the lifespan were significantly associated with higher levels of negative affect. Moreover, significant interactions between daily stressors and chronic stressors in adulthood and over the lifespan, although not in childhood, indicated that these sources of chronic stress amplified the effect of daily stressors on negative affect.
Physical symptoms
In Model 1, significantly more physical symptoms were reported on stressor days, relative to non-stressor days (coef. = 0.30, p < 0.001). Individuals living in neighborhoods perceived as less safe reported significantly more physical symptoms (coef. = −0.39, p < 0.001). Older adults, women, and those with less education reported significantly more physical symptoms. People reporting more stressors over the diary period and more symptoms of neuroticism reported significantly more physical symptoms, and people generally reported more physical symptoms on weekdays relative to days that fell on the weekend. Results of Model 2 indicated that individuals who reported more childhood, recent, and lifetime stressors reported significantly more physical symptoms.
Model 3 introduced the daily stressor x neighborhood safety concern interaction. This interaction was significant, suggesting that perceiving one’s neighborhood as less safe exacerbated the effect of daily stressors on physical symptoms (coef. = −0.18, p < 0.001). Model 4 included interactions between daily stressors and chronic stressors reported in childhood, adulthood, and over the lifespan. Results of this model suggested that stressors reported in childhood and adulthood did not significantly interact with daily stressors in relation to self-reported physical symptoms. However, among those who reported more life-time stressors, there was an even greater increase in self-reported physical symptoms in relation to daily stressors. Importantly, the neighborhood safety concern x daily stressor interaction remained significant after the inclusion of these additional interactions (coef. =−0.15, p < 0.01).
Discussion
Results of the present analyses revealed that neighborhood safety concerns play a role in the link between daily stressors, negative affect and physical well-being. People who felt less safe in their neighborhoods reported higher negative affect and more physical symptoms, and these effects were stronger on stressor days compared to non-stressor days. These findings remained unchanged even after adjusting for individual-level education, neighborhood-level income, age, race/ethnicity, levels of neuroticism and gender. They also persisted after adjusting for well-known interactions with other sources of chronic stress such as divorce or death of a loved one, loss of one’s job or unemployment, or physical or sexual assault. Results of the current study build on a large literature positing an individual level, stress-mediated pathway linking perceived neighborhood features and residents’ health.
Neighborhood Perceptions.
Neighborhood safety concerns do not represent a derived variable, nor does it summarize the characteristics of a group of people living in the same neighborhood, such as the case with neighborhood socioeconomic status. (Diez Roux, 2003) Instead, these perceptions represent a rating of the neighborhood context, albeit from the viewpoint of the residents, and therefore subjective in nature. (Diez Roux and Mair, 2010) Some researchers argue that assessments of neighborhood safety require the perspectives of local residents, and direct observation is not necessary or even appropriate.18 Residents spend a more significant amount of time in their respective neighborhoods than do researchers who make brief observations, and the most pernicious cues of disorder or threats of harm likely appear after dark when observers have left the neighborhood. (Raudenbush, 2003)
In response, the goal of the present study was to examine daily stress processes in the context of participants’ perceptions of safety concerns, which reflect the ongoing challenges residents experience on a day-to-day basis. In the current study, daily stressors were more detrimental to the well-being of people living in neighborhoods perceived as unsafe. This could, in part, be due to lower levels of reserve capacity, which posits that repeated or chronic exposure to stressors can deplete an individual’s reserve of psychosocial resources from which to draw during challenging experiences. (Gallo and Matthews, 2003) However, to accurately test these hypotheses, future studies will need to examine these associations longitudinally, taking into account factors such as social support, vigilance and health behaviors.
These findings further support sociological frameworks for under-standing the complex relationships between stressors. The Stress Process Model, (Pearlin et al., 1981) for example, proposes that stressful life events lead to mental health challenges through a process involving the gradual depletion of personal resources. At the same time, support from members of one’s social network and adaptive coping mechanisms, or lack thereof, may buffer or exacerbate, respectively, the impact of undesirable life events on mental health. In the neighborhood context, perceived neighborhood cohesion is posited to serve as a social resource that reduces the affective and physical consequences of daily stressors such as those assessed in the current study. (Robinette et al., 2013) Maintaining residence in a neighborhood perceived as unsafe, on the other hand, can be thought of as a chronic, undesirable circumstance, which may gradually deplete personal resources and thus exacerbate the daily stressor-well-being association, as was observed in the present analyses. Those who perceived their neighborhoods as unsafe may have either maintained more negative appraisals of the stressors they reported or could have perceived less support availability, especially since those who feel unsafe in their neighborhoods are less likely to engage with others in those same environments. (Raudenbush, 2003; Wright and Fisher, 2003)
Limitations and future directions
We have noted many strengths of the present study, but also acknowledge some of the limitations. First, many of the variables used in the present analyses were self-reported, and this methodological consideration has implications for the degree to which common source bias could have played a role in the findings. Several points, however, minimize our concern that this bias disqualifies our findings. First, we statistically adjusted for levels of neuroticism that could have facilitated the viewing of one’s own circumstances through negative lenses. Although dispositional characteristics such as neuroticism are somewhat consistent over time (Costa et al., 1986), perceptions of neighborhood safety and disorder vary substantially (Doran and Lees, 2005). Second, variability in perceptions of neighborhood disorder, of which safety concerns are part and parcel, often coincide with objective changes within a neighborhood, such as the deterioration of structures in the neighborhood. Furthermore, participants responded to only two questions regarding the degree to which they would feel safe walking around in their neighborhoods during the day and evening, precluding more nuanced evaluations of what determines participants’ safety concerns. Future investigation of these more nuanced evaluations will require more indicators of participants’ neighborhood contexts, including crime rates.
Third, although we view the use of a large national sample to be a strength of the present study, our sample was primarily non-Hispanic white and included people living in neighborhoods perceived to be relatively safe. We note, however, that a previous study investigating the neighborhood safety-daily stressor interactions yielded similar findings in a smaller, yet more diverse, predominantly Spanish-speaking sample. (Caspi et al., 1987) Combined, our study and others (Caspi et al., 1987) suggest that neighborhood safety concerns exacerbate the effect of daily stressors on well-being across members of various cultural groups. Future tests of these hypotheses should nevertheless use larger, more diverse samples representing a wider range of racial/ethnic backgrounds and neighborhood types. People from diverse racial/ethnic backgrounds may experience different levels of exposure to neighborhood adversity and may also differentially interpret neighborhood cues as sources of threat. Relatedly, future research could incorporate qualitative or ethnographic approaches that provide a richer description of which cues result in individual perceptions of threat or increase peoples’ sense of safety in their neighborhoods.
Lastly, the cross-sectional data in the present study precludes the ability to examine the possibility that increased reports of daily stressors predict greater neighborhood safety concerns. Reports of neighborhood safety in the present study, however, were given prior to completion of the daily diary study, and as such, temporally precede reports of stressors, negative affect, and physical symptoms. Notwithstanding the current limitations, our results add strength to the notion that chronic exposure to neighborhood safety concerns may lead to reduced daily well-being. How susceptible one is to daily stressors has important implications for long-term mental and physical health, (Charles et al., 2013; Piazza et al., 2013) and our results indicate how safe one feels in his or her neighborhood may inform individuals’ susceptibility.
Conclusions and policy implications
In the present analyses, we described a potential pathway linking neighborhood safety concerns and health: negative affect and physical symptom responses to daily stressors. The policy implications inherent in this research are that modifiable aspects of neighborhoods which cue potential threats of harm, including signs of physical decay and disorder (trash, vandalism), when improved, may reduce safety concerns and increase neighborhood-level sociability. Reduced safety concerns and increased sociability together may reduce the toll that daily stressors take on our daily well-being, which is important for both mental and physical health. Despite the literature indicating links between neighborhood features and individuals’ health, neighborhood interventions have proven difficult. (Haymann and Fischer, 2003) One reason for this is that it remains mostly unclear how best to change neighborhoods for the purpose of improving health. However, the present results indicate the importance of identifying factors related to the degree to which people feel safe in their neighborhoods. By increasing perceived neighborhood safety, it may be possible to improve residents’ daily health and well-being, which could have long-term repercussions for overall health.
Acknowledgment
This work was supported by a National Institutes of Health/National Institute on Aging training grant (T32-AG000037–37); a NIH/NIA career development grant (K99AG055699–02 4R00AG055699–03 to the first author); and a NIH/NIA grant (R03-AG047955 to the second author).
Footnotes
Declaration of Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Sliwinski MJ, Almeida DM, Smyth J, Stawski RS, 2009. Intraindividual change and variability in daily stress processes: Findings from two measurement-burst dairy studies. Psychol. Aging 24, 828–840, 10.1037/a0017925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski M, Almeida DM, 2013. The wear-and tear of daily stressors on mental health. Psychol. Sci 24, 733–741 doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leger KA, Charles ST, Ayanian JZ, Almeida DM, 2016. The association of daily physical symptoms and future health. Soc. Sci. Med 143, 241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Slwinski M, Mogle J, Almeida DM, 2013. Affective reactivity to daily stressors and long-term risk of reporting a chronic health condition. Ann. Behav. Med 45, 110–120 doi: 10.1007/s12160-012-9423-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel CS, 2010. Neighborhood as a social context of the stress process. In: Avison WR, Aneshensel CS, Schieman S, Wheaton B (Eds.), Advances in the Conceptualization of the Stress Process Springer, New York, NY, pp. 35–52. [Google Scholar]
- Diez Roux AV, Mair C, 2010. Neighborhoods and health. Ann. N. Y. Acad. Sci 1186, 125–145. [DOI] [PubMed] [Google Scholar]
- Baum B, Ziersch AM, Zhang G, Osborne K, 2009. Do perceived neighbourhood cohesion and safety contribute to neighborhood in health? Health Place 15, 925–934, 10.1016/j.healthplace.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Robinette JW, Boardman JD, Crimmins E, 2019. Differential vulnerability to neighborhood disorder: a gene x environment interaction study. J. Epidemiol. Commun. H 73 (5), 388–392 doi: 10.1136/jech-2018-211373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinette JW, Charles ST, Gruenewald TL, 2017. Neighborhood cohesion, neighborhood disorder, and cardiometabolic risk. Soc. Sci. Med 198, 70–76, 10.1016/j.socscimed.2017.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M, Hawkley C, Cacioppo JT, 2006. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: an analysis of older adults in Cook County, Illinois. Soc. Sci. Med 63, 2575–2590 doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Robinette JW, Beam RC, 2018. A genetically-informed study of neighborhoods and health: results from the MIDUS twin sample. J. Gerontol. B Soc. Sci doi: 10.1093/geronb/gby157. [DOI] [PMC free article] [PubMed]
- Robinette JW, Charles ST, Gruenewald TL, 2016. Vigilant at home: longitudinal analyses of neighborhood safety perceptions and health. SSM Popul. Health 2, 525–530, 10.1016/j.ssmph.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, McNeill LH, Wolin KY, Duncan DT, Puleo E, Emmons KM, 2007. Safe to walk? Neighborhood safety and physical activity among public housing residents. PLoS Med 4, 1599–1606 doi: 10.1371/journal.pmed.0040306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer OL, Castro-Schilo L, Aguilar-Gaxiola S, 2014. Determinants of mental health and self-rated health: a model of socioeconomic status, neighborhood safety, and physical activity. Am. J. Public Health 104, 1734–1741 doi: 10.2015/AJPH.2014.302003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, Caldwel CH, Zimmerman MA, 2015. Perceived neighborhood safety during adolescence predicts subsequent deterioration of subjective health two decades later: gender differences in a racially-diverse sample. Int. J. Prev. Med 6, 117 doi: 10.4103/2008-7802.170431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinette JW, Charles ST, Mogle JA, Almeida D, 2013. Neighborhood cohesion and daily well-being: Results from a diary study. Soc. Sci. Med 96, 174–182, 10.1016/j.socscimed.2013.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, 2005. Resilience and vulnerability to daily stressors assessed via diary methods. Curr. Dir. Psychol. Sci 14, 62–68 doi: 10.1111/j.0963-7214.2005.00336.x. [DOI] [Google Scholar]
- Raudenbush SW, 2003. The quantitative assessment of neighborhood social environments. In: Kawachi I, Berkman LF (Eds.), Neighborhoods and Health Oxford University Press, New York, NY, pp. 112–131. [Google Scholar]
- Wright RJ, Fisher EB, 2003. Putting asthma into context: community influences on risk, behavior, and intervention. In: Kawachi I, Berkman LF (Eds.), Neighborhoods and Health Oxford University Press, New York, NY, pp. 233–262. [Google Scholar]
- Gallo LC, Matthews KA, 2003. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol. Bull 129, 10–51. [DOI] [PubMed] [Google Scholar]
- Mallers MH, Almeida DM, Neupert SD, 2004. Women’s daily physical health symptoms and stressful experiences across adulthood. Psychol. Health 20, 89–403, 10.1080/08870440512331317698. [DOI] [Google Scholar]
- Stawski RS, Cichy KE, Piazza JR, Almeida DM, 2013. Associations among daily stressors and salivary cortisol: findings from the National Study of Daily Experiences. Psychoneuroendocrinology 38, 2654–2665 doi: 10.1016/j.psyneuen.2013/06/023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Bolger N, Eckenrode J, 1987. Linking person and context in the daily stress process. J. Pers. Soc. Psychol 52, 84–195. [DOI] [PubMed] [Google Scholar]
- Scott SB, Munoz E, Mogle JA, Gamaldo AA, Smyth JM, Sliwinski MJ, 2018. Perceived neighborhood characteristics predict severity and emotional response to daily stressors. Soc. Sci. Med 200, 262–270 doi: 10.1016/j.socscimed.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, Brennan PA, 2009. Chronic and acute stress and the prediction of major depression in women. Depress. Anxiety 26, 718–723 doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brim R, Ryff CD, Kessler RC, 2004. The MIDUS national survey: an overview. In: Brim R, Ryff CD, Kessler RC (Eds.), How Healthy Are We: A National Study of Well-Being at Midlife The University of Chicago Press, Chicago, IL, pp. 1–36. [Google Scholar]
- Steptoe A, Feldman PJ, 2001. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann. Behav. Med 23, 177–185. [DOI] [PubMed] [Google Scholar]
- Keyes CLM, 1998. Social well-being. Soc. Psychol. Q 61, 121–137. Retrieved from. http://www.jstor.org/stable/2787065. [Google Scholar]
- Almeida DM, Wethington E, Kessler RC, 2002. The Daily Inventory of Stressful Events: An interview-based approach for measuring daily stressors. Assessment 9, 41–55, 55. 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- Hoffman L, Stawski RS, 2009. Persons as context: Evaluating between-person and within-person effects in longitudinal analysis. Res. Hum. Dev 6, 97–120, 10.1080/15427600902911189. [DOI] [Google Scholar]
- Almeida DM, Kessler RC, 1998. Everyday stressors and gender differences in daily distress. J. Pers. Soc. Psychol 75, 670–680 doi: 10.1177/002214650404500101. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Kolarz CM, 1998. The effect of age on positive and negative affect: a developmental perspective on happiness. J. Pers. Soc. Psychol 75, 1333–1349 doi: 10.1037/0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A, 1988. Development and validation of brief measures of positive and negative affect: the PANAS Scales. J. Pers. Soc. Psychol 54, 1063–1070, 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Kasimatis M, 1991. Day-to-day physical symptoms: individual differences in the occurrence, duration, and emotional concomitants of minor daily illnesses. J. Pers 59, 387–423 doi: 10.1111/j.1467-6494.1991.tb00254.x. [DOI] [PubMed] [Google Scholar]
- Rossi AS. Chapter 7, 2001. Developmental roots of adult social responsibility. In: Rossi AS (Ed.), Caring and Doing for Others: Social Responsibility in the Domains of Family, Work, and Community University of Chicago Press, Chicago, pp. 227–320. [Google Scholar]
- Diez Roux AV The examination of neighborhood effects on health: Conceptual and methodological issues related to the presence of multiple levels of organization. In: Kawachi I, Berkman LF, eds. Neighborhoods and Health New York, NY: Oxford University Press; 2003. [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT, 1981. The stress process. J. Health Soc. Behav 22, 337–356 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR, Zonderman AB, Barbano HE, Lebowitz B, Larson DM, 1986. Cross-sectional studies of personality in a national study: stability in neuroticism, extroversion, and openness. Psychol. Aging 1, 144–149. [PubMed] [Google Scholar]
- Doran BJ, Lees BG, 2005. Investigating the spatiotemporal links between disorder, crime, and the fear of crime. Prof. Geogr 57, 1–12. [Google Scholar]
- Haymann J, Fischer A Neighborhoods, health research, and its relevance to public policy. In L Kawachi I, Berkman LF, eds. Neighborhoods and Health New York, NY: Oxford University Press; 2003:335–347. [Google Scholar]


