Abstract
Somatic symptom disorder, illness anxiety disorder, and functional syndromes are characterized by burdensome preoccupation with somatic symptoms. Etiological models propose either increased interoceptive accuracy through hypervigilance to the body, or decreased and biased interoception through top-down predictions about sensory events. This systematic review and meta-analysis summarizes findings of 68 studies examining interoceptive accuracy and 8 studies examining response biases in clinical or non-clinical groups. Analyses yielded a medium population effect size for decreased interoceptive accuracy in functional syndromes, but no observable effect in somatic symptom disorder and illness anxiety disorder. The overall effect size was highly heterogeneous. Regarding response bias, there was a small significant effect in somatic symptom disorder and illness anxiety disorder. Our findings strengthen the notion of top-down factors that result in biased rather than accurate perception of body signals in somatic symptom disorder and illness anxiety disorder.
Introduction
Interoception in the etiology of somatic symptom and related disorders
Somatic symptom and related disorders are characterized by distressing somatic symptoms and their interference with daily life. Thoughts, affect and behavior concerning the symptoms are unreasonable and result in extensive personal burden such as excessive preoccupation and societal costs like increased medical utilization [1–5]. Unfortunately, psychotherapy for these disorders has merely moderate effects [for cognitive behavioral treatment, see 6, 7]. Enhancing knowledge about pathological mechanisms is therefore essential [8]. Interoception, as the processing, integration, and interpretation of bodily signals, is a promising candidate in this regard [9]. Some etiological approaches propose increased, but others decreased and biased sensitivity for interoceptive signals [8].
Based on findings of higher levels of arousal and perceptual sensitivity [10] and lower pain tolerance in hypochondriasis [11, 12] and chronic pain [13], it was assumed that illness anxiety and somatic symptom burden result from misinterpreted perception of actual physiological changes. According to this theory, affected individuals perceive even the slightest fluctuations in physiological signals because of heightened attention to the body. Body signals are then misinterpreted as pathological, uncomfortable, and stressful, which in turn reinforces hypervigilant attention to the body. Thereby symptoms are maintained [14, 15]. In these etiological frameworks, individuals with high somatic symptom burden are assumed to exhibit higher interoceptive accuracy (IAcc). Contrary to this notion, the predictive coding perspective proposes that symptoms unfold increasingly independent of actual physiological changes over the course of somatic symptom and related disorders [16]. According to this view, somatic symptoms result from individual prediction models, rather than the processing of somatosensory input per se. To construct a perception, the brain matches predictions with somatosensory input. Although predictions need not be correct, they can still be given more weight when physiological stimuli are ambiguous [17]. In other words, somatic symptoms might be perceived independently of psychophysiological changes, when they are predicted as the most likely input. Physical changes are also more likely experienced as signs of an illness when the individual model predicts that their most likely cause is an illness. The less detailed sensory signals are processed, the more likely predictions about the presence of symptoms and disease will lead to the perception of symptoms. Attention, negative affect and gender are assumed to moderate these processes [16]. Therefore, reduced and biased interoception is hypothesized in the context of somatic symptom disorders [16]. Biased perception presumably follows a “better safe than sorry” approach, where patients affirm bodily symptoms more readily and answer more liberally in ambiguous situations [18]. In other words, threat-related predictions dominate perceptual processes and lead to illusory sensations, an information processing style that might be common in psychopathology [16].
However, empirical findings on IAcc are heterogeneous, showing increased [19, 20], unchanged [21–24], and diminished IAcc [25–28] in somatic symptom disorders. Concerning interoceptive biases, a number of studies documented a more liberal response bias (RB) in people with somatoform symptoms [19, 29–31].
Aims of this article
In the light of recent advances in interoception research, our aim was to assess both IAcc and RB in different diagnostic categories of somatic symptom and related disorders in a comprehensive systematic review and meta-analysis. We give an overview of the methods used in prior studies investigating IAcc and RB and conduct statistical analyses to calculate population effect sizes, identify potential moderators and check for publication bias. This overview was generated without preregistration or external protocol.
Methods
Diagnostic conceptualization
Conceptualization of somatic symptom and related disorders is difficult, inconsistent [32, 33], and recently underwent remarkable changes at least partially motivated by the lack of recognition of “somatoform disorders” in primary care and other medical settings [32]. Concerning somatic symptom disorder, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-5, 5] introduced symptom-related abnormal behaviors, thoughts, and feelings as diagnostic criteria, while lack of medical explanation was dropped. Psychological mechanisms also play a role in the maintenance of functional syndromes [34, 35]. Moreover, patients suffering from functional syndromes often report symptoms outside of their respective symptom complex [36–39]. Consequently, quite a few authors emphasize the overlap between different somatic symptom and functional disorders [e.g. 37, 40, 41].
However, DSM-5 has been criticized for bringing together heterogeneous clinical conditions, as it is yet unclear whether medically explained and unexplained somatic symptoms involve similar mechanisms [33]. As research following DSM-5 criteria for somatic symptom and related disorders is limited, current knowledge relates to previous DSM conceptualizations that highlighted the absence of satisfactory medical explanations of bodily symptoms rather than psychological mechanisms [42].
Against this background, we chose to aggregate diverse concepts of somatic symptom and related disorders, using the DSM-5 label as an umbrella term. We included previous and current psychological classifications as well as functional syndromes with unknown biomedical etiology. This inclusive approach prevents a loss of power and allows unfolding both mutual and distinct characteristics of these clinical pictures with regard to IAcc.
Information sources and search strategies
We searched PsychInfo, Medline, Web of Science, and ProQuest Dissertations & Theses databases on June 24th, 2016, using keywords such as “interocept*”, “propriocept*”, and “health anxiety”, “somatoform”, “fibromyalgia” as well as other terms for somatoform and functional syndromes (see S1 Table). The search was updated on November 3rd, 2020, using the same search terms. We scanned bibliographical references of the included studies and checked for studies that cited the included studies published before 2000 using cited reference searches on Web of Science. If relevant statistical outcomes were not reported in an article, the corresponding author was contacted up to three times and asked to provide us with the data.
Study selection
Two of the authors assessed the eligibility of studies. The third author was consulted in case of disagreement, and discrepancies were solved by consensus. All authors agreed on the final inclusion of studies (k = 69).
General eligibility criteria
Articles in English or German language were considered for inclusion. We included studies comparing an experimental group diagnosed with somatic symptom disorder, illness anxiety disorder, or functional syndromes with a gender-matched healthy control population. We also included studies that assessed correlations between symptoms of these categories and IAcc/RB outcomes in non-clinical samples. We did not set any other restriction concerning study design.
Participant characteristics
We only included studies testing adult samples. In clinical samples, the experimental group had to be diagnosed based on either a standardized classification system such as the DSM or ICD, disorder-specific criteria, or by evaluation of an expert in the field. Based on comprehensive research on specific diagnoses, we included only functional syndromes for which no sufficient organic etiology is known and verified (i.e., cervical dystonia, cervicogenic headache, functional vestibular symptoms). Physiological abnormalities were accepted if they had not preceded symptom onset, such as muscle tension in headache. Samples with potential or confirmed underlying organic causes for functional syndromes were excluded (e.g. [43, 44]). Non-clinical samples were included when a correlation between interoceptive measures and an established symptom questionnaire was provided.
Task characteristics
While initial concepts of interoception solely referred to visceral afferent information [45], recent definitions include stimuli arising anywhere in the body, such as the skin and proprioceptive functions [46, 47]. This definition redundantizes the separation between “interoception” vs. “exteroception”, arguing that not the stimulus origin but the perception in the central nervous system are decisive [48].
We considered tasks measuring different interoceptive domains that result in a quantifiable measure of IAcc: the perception of visceral, skin conductance, and muscle information, perception of body position, and perception of tactile stimulation on skin. We did not include tasks prone to interference by abilities other than IAcc, such as proprioceptive tasks allowing visual feedback [e.g. in 49]. Tasks that used symptom induction [as in 50] or explicit impediment of IAcc [e.g. using additional weights in a proprioceptive task in 51, 52] were excluded.
Outcome characteristics
The outcome for IAcc had to be a quantifiable match between an objectively measured physiological signal and its perception. For example, correlation scores of self-report and physiological measures, threshold scores referring to the lowest intensity at which an individual perceives a certain stimulus, reversed error scores, or values based on signal detection theory were included. In the somatic signal detection task, stimuli selection is based on a thresholding procedure that leads to similar d’ scores across participants. Therefore, d’ is not a meaningful score in this task when comparing accuracy between groups. Here, thresholding scores were used as measures of accuracy.
RB outcomes were considered for separate analyses. We included values derived from signal detection theory such as c, and β, a nonparametric measure of RB [53].
Data extraction and analysis
Two of the authors independently extracted the following study data: sample size, task, diagnosis, symptom-specific questionnaires, and primary outcome measures. Relevant outcome parameters for IAcc and RB were abstracted to an Excel sheet (Version 16.43) and analyzed using the metafor package [54] for R (Version 3.3.1).
Calculation of effect sizes
We computed effect sizes expressed as correlation coefficients r from outcome measures reported in the included studies (means and sample sizes, z-scores and sample sizes, or F-scores and their denominator degrees of freedom). Coefficients were computed such that negative values represent lower IAcc in the experimental group than the control group. Correlation coefficients were computed as outlined in [55] and [56]. For RB, effect sizes were calculated such that negative values indicated a more liberal response style in the experimental group.
For studies providing multiple results, we followed Rosenthal’s [57] recommendation in averaging z-transformed r’s such that each study would contribute a single effect size estimate to the overall analysis. If multiple study outcomes could be assigned to superordinate categories within that study, lower order outcomes (e.g., different task outcomes) were averaged before averaging higher order outcomes (e.g., different experimental groups). Quantities of averaged outcomes are shown in S2 Table. Two studies reported multiple outcomes for non-clinical illness anxiety [29, 58]. Here, we chose to only extract data of the WI [59], as this represents a widely accepted measure of non-clinical illness anxiety and thus allows comparability across studies.
Method of meta-analysis
We calculated random-effects models with standardized correlations (rz) according to Hedges and Vevea [60]. Their method provides Q statistics of homogeneity of effect sizes. This test has low power when few studies are included [61], but is too sensitive when the number of included studies is high [62]. As additional measures of heterogeneity, H2 and I2 according to Higgins and Thompson [63] are reported. For H2 values exceeding 1.5, considerable caution is advised [63]. Although official criteria for the interpretation of I2 are lacking, values ≥ 75% are considered high [62].
We conducted four separate moderator analyses using mixed models [64] with the following categorical moderators: 1) sample (clinical, non-clinical), 2) diagnosis (functional syndromes, somatic symptom disorder, illness anxiety disorder), 3) interoceptive domain (visceral/muscle perception, tactile, proprioceptive), and 4) task type (signal detection, thresholding procedure, heartbeat mental tracking, position sense, rubber hand illusion, and correlational tasks). Subgroup analyses were calculated for significant moderators.
Risk of bias evaluation
Standardized checklists for risk of bias are provided for epidemiological [65] and intervention studies [66]. We based our risk of bias evaluation on Di Lernia and colleagues [67]. Assessment criteria included sampling and matching procedures, citation of assessment protocols, and handling of missing data. We did not check for IAcc interference factors, as these vary strongly depending on bodily domain and task type. Furthermore, there are no scientific standards for most domains (with exception of the cardiovascular body domain). Two of the authors rated the criteria and solved discrepancies by consensus.
Publication bias assessment
The trim and fill method according to Duval and Tweedie [68] was applied to a funnel plot of z-transformed correlations and standard errors. Egger’s regression test for funnel plot asymmetry [69], Rosenthal’s fail safe N [70], and Begg and Mazumdar’s rank correlation test [71] are also reported. In addition, Vevea and Woods’ [72] sensitivity analysis was conducted to quantify the likely effect of publication bias, using the R code by Field and Gillet [64].
Results
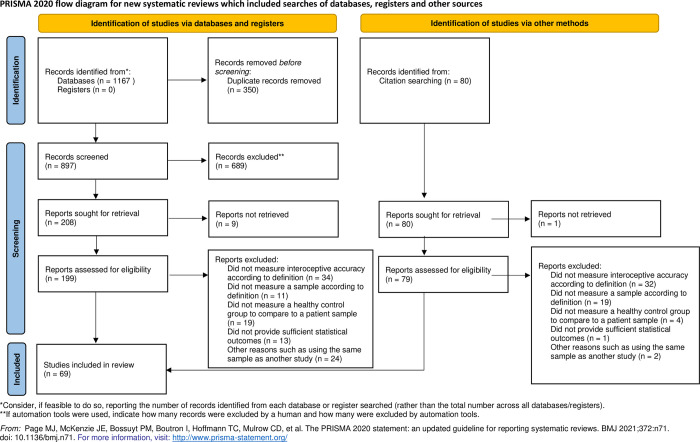
Fig 1 shows the search process in a flow chart according to the PRISMA statement [73].
Fig 1. PRISMA flow chart of study inclusion.
Study characteristics
Characteristics of the studies varied considerably (see S2 Table for a detailed overview). Two articles were written in German, the remaining articles were written in English.
Samples
The majority of included studies assessed clinical samples (k = 54 vs. k = 15). Most studies (k = 43) examined functional syndromes such as fibromyalgia, dystonia, or neck pain, using a variety of diagnostic instruments (see S2 Table). Somatic symptom disorder was assessed in 23 studies and illness anxiety disorder in 6 studies. Clinical samples were most commonly diagnosed using the ICD-10 [74] and DSM-IV [75]. Questionnaires for non-clinical somatic symptoms and illness anxiety included the Patient Health Questionnaire [76], the Checklist for Symptoms in Daily Life [77], and the Whiteley Index [59].
IAcc and RB tasks
Interoception was assessed in the cardiovascular, muscular, proprioceptive, respiratory, electrodermal, and tactile body domain with a great variety of task types. We classified the tasks into the following six task types: heartbeat mental tracking tasks, signal detection tasks, thresholding procedures, position sense tasks, the rubber hand illusion paradigm, and correlational tasks. A description of task types can be found in S3 Table.
Results of data analyses
Effects of IAcc
Effect sizes of all studies are shown in Table 1. The mean effect size based on Hedges and Vevea’s random-effects model for IAcc was rz = -.196, a small effect according to Cohen [78], with a 95% confidence interval of rz = -.282 (lower) and rz = -.110 (upper). The associated z-score was highly significant (z = 4.46, p < .001). Estimated between-study variance was τ2 = .106, I2 = 85.70%, H2 = 6.99. Q test of homogeneity of effect sizes was significant Q = 312.74, df = 67, p < .001). The calculations suggest considerable variations in the effect sizes.
Table 1. Effect sizes of interoceptive accuracy (unstandardized r) for included studies.
| First author (reference) | Diagnosis/symptoms of experimental group | Task | N | IAcc |
|---|---|---|---|---|
| Somatic symptom disorders/illness anxiety disorders | ||||
| Barsky [79] | Hypochondriasis | Heartbeat discrimination task | 105 | .0851 |
| Bogaerts [50] | High symptom reporters | Rebreathing task | 58 | -.0368 |
| Bräscher [80] | Healthy participants with varying levels of somatic symptoms | Heartbeat mental tracking task | 60 | -.0450 |
| Ferentzi [81] | Healthy participants with varying levels of somatic symptoms | Heartbeat mental tracking task; elbow joint position matching task | 109 | .0115 |
| Haenen [82] | Hypochondriasis | Tactile two-point discrimination task | 51 | .1043 |
| Katzer [29] | Healthy participants with varying levels of somatic symptoms/illness anxiety | SSDT (tactile threshold) | 67 | .1554 |
| Katzer [19] | Somatoform disorders | SSDT (tactile threshold) | 65 | .2605 |
| Krautwurst [58] | Healthy participants varying levels of somatic symptoms/illness anxiety | Signal detection task for NSCF; heartbeat mental tracking task | 100 | -.0909 |
| Krautwurst [83] | Illness anxiety disorder | Signal detection task for NSCF; heartbeat mental tracking task | 107 | .1627 |
| Lee [84] | Somatic symptom disorder | Heartbeat perception task | 43 | .0087 |
| Meyerholz [85] | Healthy participants with varying levels of somatic symptoms | Heartbeat mental tracking task | 100 | .0100 |
| Miles [86] | High symptom reporters | Rubber hand illusion task | 40 | .2774 |
| Perepelkina [87] | Somatoform disorder | Rubber and virtual hand illusion task | 33 | .0055 |
| Petersen [18] | High symptom reporters | Breathing resistance task | 50 | .2616 |
| Pollatos [25] | Multisomatoform disorder | Heartbeat mental tracking task | 46 | -.3008 |
| Rodic [88] | Healthy participants with varying levels of somatic symptoms | Tactile perception task | 179 | -.0804 |
| Sachse [28] | Psychological Factors Affecting Other Medical Conditions | Heartbeat tracking task, heartbeat mental tracking task | 66 | -.3377 |
| Sarnoch [89] | High symptom reporters | Muscle tension perception task | 13 | -.5342 |
| Schäfer [23] | Somatization disorder, pain disorder, undifferentiated somatoform disorder | Heartbeat mental tracking task | 50 | -.0121 |
| Scholz [20] | High symptom reporters | Muscle tension perception task | 40 | .2939 |
| Schonecke [27] | Functional cardiac disorder | Heartbeat discrimination task | 49 | -.5159 |
| Schröder [24] | Noncardiac chest pain | 91 | -.0235 | |
| Schulz [90] | High symptom reporters | Heartbeat mental tracking task; heartbeat discrimination task | 58 | -.0075 |
| Weiss [26] | Multisomatoform disorder | Heartbeat mental tracking task | 60 | -.3439 |
| Witthöft [91] | Healthy participants with varying levels of somatic symptoms | Heartbeat mental tracking task | 316 | -.0300 |
| Functional syndromes | ||||
| Akyol [92] | Fibromyalgia | Knee repositioning task | 105 | -.0296 |
| Anastasopoulos [93] | Spasmodic torticollis | Subjective vertical task | 51 | -.1681 |
| Bara-Jimenez [94] | Focal dystonia of the right hand | Tactile temporal discrimination task | 27 | -.4369 |
| Bara-Jimenez [95] | Focal dystonia of the right hand | Spatial localization task, tactile gap detection task | 30 | -.5038 |
| Bardal [51] | Fibromyalgia | Shoulder repositioning task | 50 | -.0740 |
| Borg [96] | Fibromyalgia | Heartbeat mental tracking task | 42 | .1260 |
| Brun [97] | Fibromyalgia | Arm positioning matching task | 40 | .0387 |
| Celenay [98] | Fibromyalgia | Trunk repositioning task | 30 | -.5260 |
| Cheng [99] | Neck pain | Head repositioning task | 24 | -.4071 |
| Demartini [100] | Psychogenic non-epileptic seizures and functional motor symptoms | Heartbeat mental tracking task | 40 | -.0939 |
| Demartini [101] | Functional motor symptoms | Heartbeat mental tracking task | 40 | -.0892 |
| De Pauw [102] | Cervical dystonia | Head repositioning task | 94 | -.2635 |
| De Zoete [103] | Neck pain | Head and trunk repositioning task | 100 | -.0482 |
| Dumas [104] | Cervicogenic headache, migraine | Head repositioning task | 37 | -.0890 |
| Duschek [105] | Fibromyalgia | Heartbeat mental tracking task | 76 | -.2498 |
| Edmondston [106] | Postural neck pain | Head, neck and shoulder repositioning task | 43 | -.0569 |
| Elsig [107] | Neck pain | Tactile discimination task; head repositioning task | 60 | -.2509 |
| Fiorio [108] | DYT1 manifesting dystonia | Tactile temporal discrimination task | 39 | .1321 |
| Fiorio [109] | Blepharospasm | Tactile temporal discrimination task | 20 | -.7360 |
| Fiorio [110] | Focal hand dystonia, non-hand dystonia | Rubber hand illusion task | 22 | -.5349 |
| Gajdos [111] | High gastrointestinal symptom reporters | Heartbeat mental tracking task | 72 | .1170 |
| Goncalves [112] | Chronic neck pain | Head repositioning task | 66 | -.2657 |
| Grip [113] | Neck pain | Head repositioning task | 43.75a | -.0667 |
| Jungilligens [114] | Dissociative seizures | Heartbeat mental tracking task | 40 | -.0931 |
| Katschnig [115] | Fixed Dystonia | Tactile temporal discrimination task | 21 | -.4058 |
| Koreki [116] | Functional seizures | Heartbeat mental tracking task; heartbeat discrimination task | 71 | -.2657 |
| Kristjansson [117] | Neck pain | Head repositioning task; trunk rotation task; figure-of-eight movement task | 41 | -.1103 |
| Lee [118] | Non-clinical daily and weekly neck pain | Head repositioning task | 85.5a | -.2594 |
| Marinelli [119] | Cervical Dystonia | Reaching movement task | 20 | -.5466 |
| Morgante [120] | Primary torsion dystonia and psychogenic dystonia | Tactile temporal discrimination task | 26 | -.9622 |
| Nijs [121] | Chronic fatigue syndrome | Leg repositioning task | 137 | -.1475 |
| Pick [122] | Functional neurological disorder | Heartbeat mental tracking task | 39 | .0090 |
| Pinsault [123] | Neck pain | Head repositioning task | 14 | -.4602 |
| Ricciardi [124] | Functional movement disorders | Heartbeat mental tracking task | 33 | -.8568 |
| Rost [125] | Fibromyalgia | Heartbeat mental tracking task | 92 | .1413 |
| Sanger [126] | Focal hand dystonia | Tactile temporal discrimination task | 19 | -.5651 |
| Scontrini [127] | Blepharospasm, cervical, hand, and laryngeal dystonia | Tactile temporal discrimination task | 41 | -.5001 |
| Sjölander [128] | Neck pain | Head repositioning task | 25 | -.2428 |
| Tinazzi [129] | Generalized dystonia, hand dystonia, and segmental dystonia involving the right arm and trunk | Tactile temporal discrimination task | 16 | -.7420 |
| Tinazzi [130] | Generalized dystonia, hand dystonia, and segmental dystonia involving the right arm and trunk | Tactile temporal discrimination task | 22 | -.8582 |
| Ulus [131] | Fibromyalgia | Knee repositioning task | 60 | -.0541 |
| Valenzuela-Moguillansky [132] | Fibromyalgia | Heartbeat detection task | 59 | -.0174 |
| Woodhouse [133] | Chronic neck pain | Head repositioning task | 114 | -.1335 |
Note. a Sample sizes averaged over tasks/conditions.
Moderator analyses showed that sample (clinical or non-clinical) was a significant moderator, Q = 5.19, p = .023, I2 = 84.44%, H2 = 6.43. Likewise, diagnosis (functional syndromes, somatic symptom disorder, illness anxiety disorder) had a significant impact on the population effect size, Q = 8.94, p = .003, I2 = 83.68%, H2 = 6.13. The effect size was not significantly affected by interoceptive domain (visceral/muscle perception, tactile, proprioceptive), Q = 0.46, p = 0.500, I2 = 85.49%, H2 = 6.89, or task type (signal detection, thresholding procedure, heartbeat mental tracking, position sense, rubber hand illusion, and correlational tasks), Q = 0.00, p = 0.947, I2 = 84.92%, H2 = 6.63.
Subgroup analyses were conducted for all levels of the significant moderators sample and diagnosis (see Table 2). Effect size for IAcc was considerably higher in clinical samples (rz = -.251) than non-clinical samples (rz = -.014), with a significantly associated z-score but also high heterogeneity in studies with clinical samples. Regarding diagnosis, only studies with functional syndrome samples showed a significant effect size of rz = -.308.
Table 2. Results of separate random-effects subgroup analyses for interoceptive accuracy according to diagnosis, task, and sample.
| Subgroup | k | 95% confidence interval for estimated rz | z | τ 2 | Q a | I 2 | H 2 | ||
|---|---|---|---|---|---|---|---|---|---|
| lower | mean | upper | |||||||
| Sample | |||||||||
| Clinical | 54 | -.355 | -.251 | -.146 | -4.71*** | .126 | 273.85*** | 85.91 | 7.10 |
| Non-clinical | 14 | -.077 | -.014 | .050 | -0.42 | .002 | 20.38 | 16.43 | 1.20 |
| Diagnosis | |||||||||
| SSD | 22 | -.137 | -.049 | .038 | -1.11 | .026 | 53.20*** | 65.15 | 2.87 |
| IAD | 6 | -.037 | .053 | .142 | 1.15 | .002 | 5.76 | 16.55 | 1.20 |
| FS | 43 | -.430 | -.308 | -.186 | -4.96*** | .137 | 216.84*** | 86.30 | 7.30 |
Note. SSD = somatic symptom disorder; IAD = illness anxiety disorder, FS = functional syndrome
a df = k– 1
*p < .05
**p < .01
***p < .001
Effects of RB
Effect sizes are shown in Table 3. For measures of RB, there was an estimated mean rz of -.163, with lower and upper confidence bounds of -.252 and -.075, respectively. The associated z-score was significant, z = -3.63, p < .001. The estimated between study variance τ2 was .002, I2 = 14.64%, H2 = 1.17, and Q statistics of homogeneity were not significant, Q = 7.62, df = 7, p = .367).
Table 3. Effect sizes of response bias (unstandardized r) for included studies.
| First author (reference) | Diagnosis/symptoms of experimental group | Task | N | RB |
|---|---|---|---|---|
| Brown [30] | High symptom reporters | SSDT | 80 | -.2022 |
| Katzer [29] | Healthy participants with varying levels of somatic symptoms/illness anxiety | SSDT | 67 | -.3550 |
| Katzer [19] | Somatoform disorders | SSDT | 65 | -.1264 |
| Krautwurst [58] | Healthy participants with varying levels of somatic symptoms/illness anxiety | Signal detection task for NSCF | 100 | -.1104 |
| Krautwurst [83] | Illness anxiety disorder | Signal detection task for NSCF | 107 | -.2505 |
| Petersen [18] | High symptom reporters | Breathing resistance task | 50 | -.1597 |
| Schäfer [23] | Somatization disorder, pain disorder, undifferentiated somatoform disorder | Heartbeat discrimination task | 50 | -.1285 |
| Schröder [24] | Noncardiac chest pain | Heartbeat discrimination task | 91 | .0352 |
Note. RB = response bias
Risk of bias evaluation
The risk of bias of studies included into this systematic review was quite heterogeneous (see S4 Table for details of the risk of bias assessment). Across all studies and criteria, 51.4% were rated “yes” (indicating low risk of bias). Risk of bias indicators differed across criteria: For example, 84.1% described or cited a protocol for IAcc assessment in their study, but less than half (46.4%) provided statistics for age matching their study groups. Risk of bias indicators also differed with regard to study sample: For example, more studies examining somatic symptom disorder and illness anxiety disorder samples described replicable sampling methods than studies examining functional syndrome samples (62.7% vs. 38.1%).
Publication bias analyses
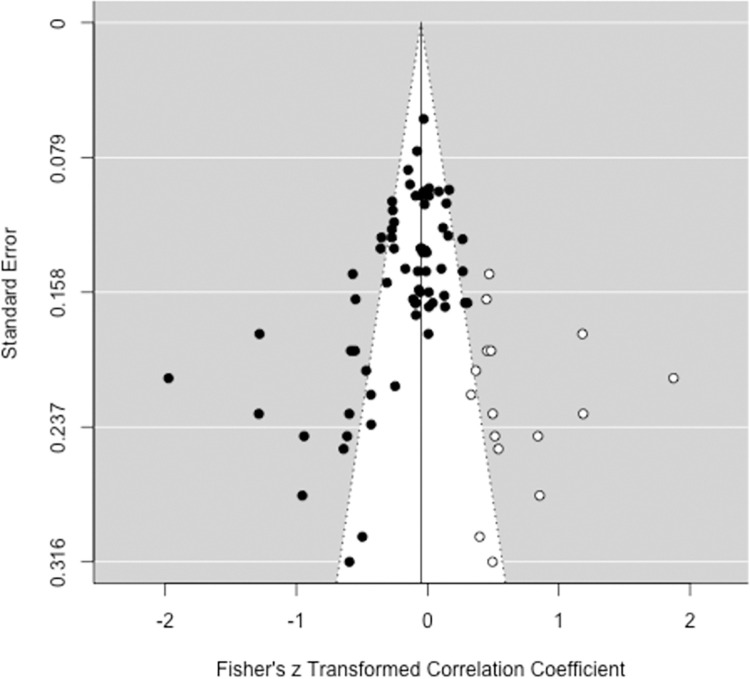
Regarding IAcc outcomes, there was noticeable asymmetry in the funnel plot of studies’ z-standardized effect estimates and standard errors (see Fig 2). By means of the trim and fill method [68], 16 data points were augmented on the right side of the funnel plot, which shows that studies with negative correlations, some of them very strong, are overrepresented. It should however be noted that the trim and fill method is problematic when moderator effects are expected [54]. Between-study heterogeneity might have had an effect on the distribution of data. In our selection, four studies that reported effect sizes < -.5 were conducted by the same workgroup [109, 120, 129, 130] with similar patient samples (dystonia). Similarly, with few exceptions, the positive correlations are based on samples with somatic symptom disorder or illness anxiety disorder, suggesting that subgroup effects skew the plot. Egger’s regression test confirmed significant funnel plot asymmetry, z = -5.444, p < .001.
Fig 2. Funnel plot with trim and fill method applied to z-transformed correlations and standard errors of interoceptive accuracy (k = 68).
Created with the metafor package [54] for R (Version 3.3.1).
Rosenthal’s [70] fail safe N test revealed that 2232 new, unpublished, filed, or unretrieved studies would be required to turn the significant result into a non-significant one. Begg and Mazumdar rank correlation test for a random-effects model showed significant publication bias across all studies (τB = -.330, p < .001). Sensitivity analysis based on Vevea and Woods [72] revealed minor changes in population effect size estimates (unadjusted rz = -.195) in case of moderate and severe two-tailed selection (rz = -.181; rz = -.165), but considerable changes in case of moderate and severe one-tailed selection (rz = -.271; rz = -.704).
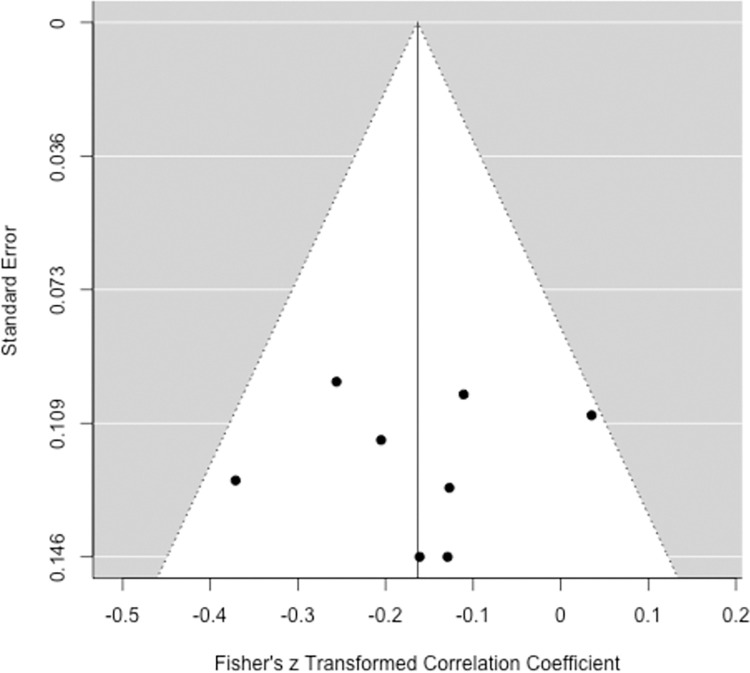
For RB outcomes, the funnel plot with z transformed correlations was symmetric and no data points were augmented using the trim and fill method (see Fig 3). Neither Egger’s regression test, z = -0.19, p = .842, nor Begg and Mazumdar rank correlation test, τB = -.036, p = .901, showed evidence of publication bias. Rosenthal’s [70] fail safe N was 38. Sensitivity analysis showed the largest changes in effect size estimation for severe one-tailed publication bias (rz = —.236, unadjusted rz = -.163) and smaller changes for moderate one-tailed (rz = -.173) as well as moderate and severe two-tailed selection (rz = -.148, rz = -.124).
Fig 3. Funnel plot applied to z-transformed correlations and standard errors of response bias (k = 8).
No data points were augmented by the trim and method. Created with the metafor package [54] for R (Version 3.3.1).
Discussion
Interoceptive accuracy and response bias
We found a small overall effect size of reduced IAcc, which was moderated by diagnosis and by whether the sample was clinical or non-clinical. Subgroup analyses showed that while IAcc was significantly reduced in functional syndromes, it was not altered in somatic symptom disorder and illness anxiety disorder. This contradicts models that assume lower perceptual thresholds for body signals in these disorders. In line with this, studies homogeneously showed a more liberal RB, reflecting a “better safe than sorry” approach [18]. A liberalization of decision strategies in the formation of somatic symptom and related disorders is compatible with predictive coding theory: symptom report decoupled from sensory input should occur when learned knowledge about the world (“priors”) predicts the presence of symptoms/stimuli with a high level of confidence [16]. Over the course of time, the experience of symptoms may increasingly depend on contextual cues that confirm the underlying disease model rather than on perceived physiological sensations [134–142]. Assuming that a sensation is a “symptom” rather than a “benign sensation” can then turn into the prior with the highest precision in somatic symptom and related disorders.
The overall effect of reduced IAcc was characterized by high heterogeneity, which was only partly resolved by including moderators. Therefore, the general and subgroup effects of IAcc have to be interpreted with caution. Possible explanations for the heterogeneity will be discussed in the following.
Sources of heterogeneity in interoceptive accuracy: Differences between diagnostic groups
There was a medium effect size of reduced IAcc for functional syndromes, but effect sizes around zero for somatic symptom disorder or illness anxiety disorder samples. Differences in IAcc between diagnoses are surprising, considering substantial overlap of disorders that are not attributable to verified organic dysfunctions [41].
These differences could be due to underlying pathological differences between diagnostic groups. IAcc measurements might be affected by specific symptoms. In functional syndromes, the symptoms often affect one or few body parts and remain relatively stable across time. In somatic symptom and related disorders, symptoms are highly variable and typically co-occur [143]. In fact, DSM-IV diagnosis of somatoform disorder required the co-occurrence of symptoms in at least four different body sites or functions [75]. Yet, more importantly, illness anxiety does not necessarily involve any somatic symptoms. Therefore, abnormalities of IAcc in somatic symptom and related disorders would have to be very generalized in order to produce a common effect. In contrast, specific distortions in functional syndromes such as neck pain might more easily result in measurably lower IAcc assessed in this domain. It should also be noted that dystonia was by far the most frequently diagnosed disorder and might have had a particularly strong impact on the mean effects size in functional syndromes.
We believe that interoceptive domain and task type must be considered in the interpretation of our results despite nonsignificant moderator effects, because there was a strong entanglement of the three moderators diagnosis, task type, and interoceptive domain. For example, studies investigating somatic symptom disorder and illness anxiety disorder predominantly used visceral tasks, while none of the studies investigating dystonia did so. Studies assessing functional syndromes often measured IAcc in affected body parts, such as using head repositioning tasks in neck pain. In this case, muscle tension in case of neck pain might impair patients’ abilities to perceive interoceptive signals in the neck region. Arguably, individual symptoms and IAcc measurements are therefore more closely related in studies assessing functional syndromes, and impaired IAcc might result from physiological dysfunction rather than generally impaired perception of body signals. In contrast, IAcc outcomes for body regions specifically affected by symptoms of somatic symptom disorder were relatively rare [with few exceptions: e.g. cardiac vs. non-cardiac chest pain, 24, or heartbeat detection tasks in functional cardiac disorder, 27]. On the other hand, only about half of the dystonia studies assessed IAcc in the affected body part and one study provided direct evidence for a generalized proprioceptive impairment by comparing affected and non-affected body parts [99]. Interestingly, most theories conceptualize interoception as a homogenous construct across assessment domains [144]. However, while a few studies found cross-modal intercorrelations [gastrointestinal and cardiac domain: 145, 146, cardiac domain and body ownership: 147, cardiac and respiratory domain: 148], most others did not [skin conductance and cardiac domain: 58, 83, 149, 150, cardiac, sweat gland, and respiratory perception: 151, propriocption as well as cardiac, gastric, and taste perception: 152]. This could also be due to the fact that there are hardly any studies that measure body domains with comparable task types (type of demand, difficulty).
There was a similar overlap between task type and diagnosis. For example. with one exception, position sense tasks were only used in functional syndrome samples. Signal detection tasks were used in all diagnostic groups, but with different paradigms (e.g., tactile spatial localization tasks and temporal discrimination tasks were only assessed in functional syndrome samples). Few studies had used correlational tasks or the rubber hand illusion task. On the other hand, the mental tracking task was used across diagnoses.
A short evaluation of conducted task types
It is important to acknowledge that all task types have different advantages and disadvantages. Test and retest reliability of position sense tasks was merely moderate [153] and results depended on outcome variable [154]. Short term reliability of tactile signal detection tasks and thresholding procedures was good [19, 29], but might vary depending on examined parts of the skin or when assessed long term [155]. An external stimulation is necessary in theses task types, which excludes them from narrow definitions of interoception.
Although the separation of sensitivity and bias according to signal detection approaches is of especial interest for testing etiological assumptions for somatic symptom and related disorders, most task types do not allow this differentiation. For example, the mental tracking task is reliable and easy to administer, but the heartbeat perception score is an amalgam of sensitivity and response bias, with liberal decisions resulting in increased accuracy scores [156]. A lack of group differences in this task may be because poorer sensitivity is compensated for by increased liberality. The validity of this task type has consequently been questioned [157, 158]. Discrimination tasks, on the other hand, have been criticized for their high level of difficulty, leading to low IAcc scores with low variability [18, 157]. In a similar vein, the signal detection task in the electrodermal body domain is only well suited for specific samples due to its high degree of difficulty and temporal length [58, 83, 159, 160].
Strengths and limitations of this systematic review
Taken together, the results summarized in our review do not confirm assumptions about abnormalities regarding IAcc for somatic symptom disorder or illness anxiety disorder. We did, however, find abnormalities of IAcc for a broad range of functional syndromes, implying IAcc to be a more relevant underlying mechanism in these disorders. Due to high heterogeneity these results have to be interpreted cautiously. To our knowledge, this is the first systematic review that systematically covers a broad variety of IAcc concepts in various functional and somatic symptoms and disorders.
When evaluating our results, both risks and advantages of bringing together heterogeneous samples and methods in meta-analyses should be carefully considered [55]. In our selection of studies, participants differed broadly in diagnoses. Methods of assessing IAcc differed considerably between diagnostic groups. Some of them, such as heartbeat detection tasks, have been criticized because of their psychometric limitations [161]. We dealt with this issue by considering moderators and analyzing subsamples. However, we cannot rule out that these factors affected our results.
We only included “neutral” task conditions into the systematic review. However, interoceptive measures might be more clinically sensitive if related to perturbations of physiological functioning [compare 9]. For example, healthy individuals with high negative affectivity were significantly less accurate in estimating breathing sensations presented in a distressing frame than a pleasant frame, while framing did not have an impact on accuracy in individuals with low negative affectivity [135]. It is conceivable that IAcc increases or decreases in a threatening context such as pain induction because of its inherent association with negative affectivity [46]. Previous research indicated lower pain thresholds in patients with somatoform pain disorders [162] and illness anxiety disorder [163]. Then again, no abnormalities of pain thresholds were found in patients with multisomatoform disorder [164] and somatoform disorder [26] in comparison to healthy controls. Evidence is yet too sparse to confirm differences of IAcc between “negative affect” and “neutral” conditions.
Another possible limitation relates to risk of bias in the included studies. All in all, methodological quality was reasonably good for the majority of studies. However, we did find risk of bias for some aspects that would be easy to prevent (such as describing replicable sampling methods).
An issue relevant to all meta-analyses is publication bias. Despite a comprehensive literature search considering grey literature such as dissertations, we found evidence of publication bias in our sample, with an overrepresentation of strong negative effect sizes. Therefore, we cannot rule out that the true effect of IAcc is lower than calculated in this meta-analysis.
Finally, our study sample regarding RB in somatic symptom and related disorders is small. Our findings with regard to a more liberal RB are therefore preliminary, and more data-driven studies are needed to extend these findings.
Future directions
This systematic review focused on two facets of interoception: IAcc and RB. While our findings contradict the assumption of generally altered IAcc, somatic symptom and related disorders patients might show higher or lower IAcc under certain conditions (e.g., when symptom schemata are activated), or in certain domains (e.g., those affected by symptoms). Besides, IAcc and RB are not mutually exclusive and have to be addressed independently. They might interact differentially depending on psychological factors as affect or cognition [18]. For example, a positive relation of IAcc and RB was shown in case of increased uncertainty about stimuli [18]. For such highly ambiguous stimuli, extreme decision strategies can be successful and adaptive [18].
There is a clear need for high-quality multilevel studies [9] to tackle different interoceptive domains and link various aspects of interoception. Interoception is a multifaceted process ranging from peripheral signal perception to higher cognitive processes such as attention, attribution, and decision-making [9]. Ideally, future research will be able to integrate findings on lower level processing [165] and higher-level processing [e.g. the impact of categorization on interoceptive processing, 136]. Recent advances in interoceptive techniques using sensing perturbation [166, 167] could provide further insight into bottom-up interoceptive processes, while manipulations of expectations [e.g. 50, 135] could help to explore top-down interoceptive processing in somatic symptom and related disorders. The predominance of interoceptive measures in certain body domains within diagnostic categories (e.g., proprioceptive tasks in functional syndromes) should be addressed by using a greater variety of tasks in different interoceptive domains. Furthermore, a development of signal detection tasks with comparable difficulty for different body domains would be desirable (for a new approach in the cardiovascular body domain see [156]). The risk of bias criteria assessment can inform the experimental set ups of future studies. However, even within task types, different forms of implementation can lead to strongly diverging results [168]. Therefore, achieving a better comparability of different studies would also require the research field to agree on relevant control variables and quality standards [e.g., 168].
Furthermore, future research should follow up on first findings of beneficial effects of biofeedback training [21, 85] and interoceptive exposure [169] in patients with somatic symptom and related disorders. Importantly, researchers should refer to the proposed taxonomies of interoception [9] to allow an integration of findings on the various dimensions of interoceptive processing.
Conclusions
In this systematic review and meta-analysis, IAcc was assessed in somatic symptom and related disorders in the light of different theoretical approaches. We found diminished IAcc in functional syndromes and a more liberal RB in somatic symptom disorders and illness anxiety disorder. These findings are consistent with the predictive coding theory, which highlights a decoupling of somatosensory input and the perception of body sensations. However, the RB effect was only based on the few studies that had distinguished between IAcc and RB in their experimental setup. Consequently, future research should consider this distinction to further elucidate the relationship between these two facets of interoception.
Finally, we would like to encourage researchers to use different tasks and assess various interoceptive domains. Future study designs should address interoception both in contexts closely and more distantly related to potential dysfunctions. Using multifaceted approaches will help to provide ecologically valid results and to explore the relevance of symptom specificity as originally suggested by Malmo and Shagass [170].
Supporting information
(DOCX)
TS = topic, TI = title.
(DOCX)
CFS = chronic fatigue syndrome, CFS-APQ = Chronic Fatigue Syndrome Activities and Participation Questionnaire, CG = control group, CSD = Checklist for Symptoms in Daily Life, EG = experimental group, FIQ = Fibromyalgia Impact Questionnaire, HAF-17 = Cardiac Anxiety Questionnaire [Herzangstfragebogen], IAcc = interoceptive accuracy, IQR = interquartile range, M = mean, Mdn = Median, MIHT = Multidimensional Inventory of Hypochondriacal Traits, NA = not available, n.s. = not significant, NSCF = nonspecific skin conductance fluctuations, PHQ-15/PHQ-D = Patient Health Questionnaire, RB = response bias, SD = standard deviation, SDQ/SDQ-20 = Somatoform Dissociation Questionnaire, SE = standard error, SOMS = Screening for Somatoform Symptoms, SSAS = Somatosensory Amplification Scale, SSDT = Somatic Signal Detection Task, TWSTRS = Toronto Western Spasmodic Torticollis Rating Scale, WGO-IBS = World Gastroenterology Organisation–Irritable Bowel Syndrome Questionnaire, WI = Whiteley Index. a Number of participants included into data analysis. b These numbers were calculated on the basis of data supplied by the authors. c Only tasks/outcomes included in effect size calculation are listed here. d Number of outcomes included into data analysis. e < indicates a more liberal response bias, > a more conservative response bias in the EG compared to the CG. e Refers to the total sample. f Difference between target and actual position.
(DOCX)
(DOCX)
Yes (low risk of bias); no (high risk of bias);? (unclear); NA (not applicable).
(DOCX)
Acknowledgments
We would like to thank Jessica Napieralski and Natalie Schmitz for assisting in the structuring of the data. We also want to thank all authors who responded to our requests and kindly provided us with their data to include into this systematic review.
Data Availability
The data that support the findings of this study are openly available in “figshare” at (https://doi.org/10.6084/m9.figshare.8326523.v1).
Funding Statement
This work was partially funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) – 403266317. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Barsky AJ, Ettner SL, Horsky J, Bates DW. Resource utilization of patients with hypochondriacal health anxiety and somatization. Med Care. 2001;39(7):705–15. Epub 2001/07/18. doi: 10.1097/00005650-200107000-00007 . [DOI] [PubMed] [Google Scholar]
- 2.Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry. 2005;62(8):903–10. Epub 2005/08/03. doi: 10.1001/archpsyc.62.8.903 . [DOI] [PubMed] [Google Scholar]
- 3.Crane D, Morton L., Fawcett D., Moore A., Larson J., & Sandberg J. Somatoform Disorder: Treatment Utlization and Cost by Mental Health Professions. Contemporary Family Therapy. 2012;34:322–33. [Google Scholar]
- 4.Romeyke T, Scheuer HC, Stummer H. Inpatient hospital costs and length of stay for the treatment of affective and somatoform disorders—evidence from Germany. Risk Manag Healthc Policy. 2014;7:245–52. Epub 2014/12/17. doi: 10.2147/RMHP.S73724 ; PubMed Central PMCID: PMC4259502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 6.Looper KJ, Kirmayer LJ. Behavioral medicine approaches to somatoform disorders. J Consult Clin Psychol. 2002;70(3):810–27. Epub 2002/07/02. . [PubMed] [Google Scholar]
- 7.Kleinstäuber M, Witthöft M, Hiller W. Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: a meta-analysis. Clin Psychol Rev. 2011;31(1):146–60. Epub 2010/10/06. doi: 10.1016/j.cpr.2010.09.001 . [DOI] [PubMed] [Google Scholar]
- 8.Martin A, Van den Bergh O. Medically Unexplained Symptoms and Bodily Distress. Zeitschrift für Psychologie. 2020;228(2):65–7. doi: 10.1027/2151-2604/a000399 [DOI] [Google Scholar]
- 9.Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, et al. Interoception and Mental Health: A Roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(6):501–13. Epub 2018/06/10. doi: 10.1016/j.bpsc.2017.12.004 ; PubMed Central PMCID: PMC6054486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanback JW, Revelle W. Arousal and Perceptual Sensitivity in Hypochondriacs. J Abnorm Psychol. 1978;87(5):523–30. WOS:A1978FV70400008. doi: 10.1037//0021-843x.87.5.523 [DOI] [PubMed] [Google Scholar]
- 11.Bianchi GN. Origins of Disease Phobia. Aust Nz J Psychiat. 1971;5(4):241–57. WOS:A1971Y068600005. doi: 10.1080/00048677109159654 [DOI] [PubMed] [Google Scholar]
- 12.Bianchi GN. Patterns of Hypochondriasis—Principal Components Analysis. Brit J Psychiat. 1973;122(570):541–8. WOS:A1973P594900004. doi: 10.1192/bjp.122.5.541 [DOI] [PubMed] [Google Scholar]
- 13.Merskey H, Evans PR. Variations in Pain Complaint Threshold in Psychiatric and Neurological Patients with Pain. Pain. 1975;1(1):73–9. WOS:A1975AL62500004. doi: 10.1016/0304-3959(75)90006-8 [DOI] [PubMed] [Google Scholar]
- 14.Barsky AJ, Wyshak G. Hypochondriasis and Somatosensory Amplification. Brit J Psychiat. 1990;157:404–9. WOS:A1990DY75100016. doi: 10.1192/bjp.157.3.404 [DOI] [PubMed] [Google Scholar]
- 15.Rief W, Broadbent E. Explaining medically unexplained symptoms-models and mechanisms. Clinical Psychology Review. 2007;27(7):821–41. WOS:000250192700004. doi: 10.1016/j.cpr.2007.07.005 [DOI] [PubMed] [Google Scholar]
- 16.Van den Bergh O, Witthöft M, Petersen S, Brown RJ. Symptoms and the body: Taking the inferential leap. Neurosci Biobehav R. 2017;74:185–203. WOS:000395605200012. doi: 10.1016/j.neubiorev.2017.01.015 [DOI] [PubMed] [Google Scholar]
- 17.Edwards MJ, Adams RA, Brown H, Pareés I, Friston KJ. A Bayesian account of ‘hysteria’. Brain. 2012;135(11):3495–512. doi: 10.1093/brain/aws129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen S, Van Staeyen K, Vogele C, von Leupoldt A, Van den Bergh O. Interoception and symptom reporting: disentangling accuracy and bias. Front Psychol. 2015;6:732. Epub 2015/06/20. doi: 10.3389/fpsyg.2015.00732 ; PubMed Central PMCID: PMC4454884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katzer A, Oberfeld D, Hiller W, Gerlach AL, Witthöft M. Tactile Perceptual Processes and Their Relationship to Somatoform Disorders. J Abnorm Psychol. 2012;121(2):530–43. WOS:000304131400023. doi: 10.1037/a0026536 [DOI] [PubMed] [Google Scholar]
- 20.Scholz OB, Ott R, Sarnoch H. Proprioception in somatoform disorders. Behav Res Ther. 2001;39(12):1429–38. WOS:000172364700004. doi: 10.1016/s0005-7967(00)00108-x [DOI] [PubMed] [Google Scholar]
- 21.Schäfer M, Egloff B, Gerlach AL, Witthöft M. Improving heartbeat perception in patients with medically unexplained symptoms reduces symptom distress. Biol Psychol. 2014;101:69–76. WOS:000340838800009. doi: 10.1016/j.biopsycho.2014.05.012 [DOI] [PubMed] [Google Scholar]
- 22.Mussgay L, Klinkenberg N, Ruddel H. Heart beat perception in patients with depressive, somatoform, and personality disorders. J Psychophysiol. 1999;13(1):27–36. WOS:000080878300004. [Google Scholar]
- 23.Schäfer M, Egloff B, Witthöft M. Is Interoceptive Awareness Really Altered in Somatoform Disorders? Testing Competing Theories With Two Paradigms of Heartbeat Perception. J Abnorm Psychol. 2012;121(3):719–24. WOS:000307482700018. doi: 10.1037/a0028509 [DOI] [PubMed] [Google Scholar]
- 24.Schröder S, Gerlach AL, Achenbach S, Martin A. The Relevance of Accuracy of Heartbeat Perception in Noncardiac and Cardiac Chest Pain. Int J Behav Med. 2015;22(2):258–67. WOS:000351523600012. doi: 10.1007/s12529-014-9433-3 [DOI] [PubMed] [Google Scholar]
- 25.Pollatos O, Dietel A, Herbert BM, Wankner S, Wachsmuth C, Henningsen P, et al. Blunted autonomic reactivity and increased pain tolerance in somatoform patients. Pain. 2011;152(9):2157–64. Epub 2011/06/24. doi: 10.1016/j.pain.2011.05.024 . [DOI] [PubMed] [Google Scholar]
- 26.Weiss S, Sack M, Henningsen P, Pollatos O. On the Interaction of Self-Regulation, Interoception and Pain Perception. Psychopathology. 2014;47(6):377–82. WOS:000345661400005. doi: 10.1159/000365107 [DOI] [PubMed] [Google Scholar]
- 27.Schonecke OW. Functional cardiac disorder and cardiac perception: Attempts of quantification. In: Schonecke OW, Vaitl D, Schandy R, editors. From the heart to the brain: The psychophysiology of circulation—brain interaction. Frankfurt/Main: Peter Lang-Verlag; 1995. [Google Scholar]
- 28.Sachse R. [Heart beat perception in patients with psychosomatic disorders: distracting attention from personal physical processes]. Psychother Psychosom Med Psychol. 1994;44(8):284–92. Epub 1994/08/01. . [PubMed] [Google Scholar]
- 29.Katzer A, Oberfeld D, Hiller W, Witthöft M. Tactile perceptual processes and their relationship to medically unexplained symptoms and health anxiety. J Psychosom Res. 2011;71(5):335–41. Epub 2011/10/18. doi: 10.1016/j.jpsychores.2011.03.009 . [DOI] [PubMed] [Google Scholar]
- 30.Brown RJ, Brunt N, Poliakoff E, Lloyd DM. Illusory touch and tactile perception in somatoform dissociators. J Psychosom Res. 2010;69(3):241–8. Epub 2010/08/17. doi: 10.1016/j.jpsychores.2009.11.010 . [DOI] [PubMed] [Google Scholar]
- 31.Brown RJ, Skehan D, Chapman A, Perry EP, McKenzie KJ, Lloyd DM, et al. Physical symptom reporting is associated with a tendency to experience somatosensory distortion. Psychosom Med. 2012;74(6):648–55. Epub 2012/07/04. doi: 10.1097/PSY.0b013e3182595358 . [DOI] [PubMed] [Google Scholar]
- 32.Murray AM, Toussaint A, Althaus A, Lowe B. The challenge of diagnosing non-specific, functional, and somatoform disorders: A systematic review of barriers to diagnosis in primary care. J Psychosom Res. 2016;80:1–10. WOS:000368323900001. doi: 10.1016/j.jpsychores.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 33.Rief W, Martin A. How to Use the New DSM-5 Somatic Symptom Disorder Diagnosis in Research and Practice: A Critical Evaluation and a Proposal for Modifications. Annu Rev Clin Psycho. 2014;10:339–67. WOS:000336428200014. doi: 10.1146/annurev-clinpsy-032813-153745 [DOI] [PubMed] [Google Scholar]
- 34.Cella M, White PD, Sharpe M, Chalder T. Cognitions, behaviours and co-morbid psychiatric diagnoses in patients with chronic fatigue syndrome. Psychol Med. 2013;43(2):375–80. WOS:000313066400013. doi: 10.1017/S0033291712000979 [DOI] [PubMed] [Google Scholar]
- 35.Nijs J, Roussel N, Van Oosterwijck J, De Kooning M, Ickmans K, Struyf F, et al. Fear of movement and avoidance behaviour toward physical activity in chronic-fatigue syndrome and fibromyalgia: state of the art and implications for clinical practice. Clin Rheumatol. 2013;32(8):1121–9. WOS:000322387300002. doi: 10.1007/s10067-013-2277-4 [DOI] [PubMed] [Google Scholar]
- 36.Nimnuan C, Rabe-Hesketh S, Wessely S, Hotopf M. How many functional somatic syndromes? J Psychosom Res. 2001;51(4):549–57. WOS:000171598400001. doi: 10.1016/s0022-3999(01)00224-0 [DOI] [PubMed] [Google Scholar]
- 37.Aaron LA, Buchwald D. A review of the evidence for overlap among unexplained clinical conditions. Ann Intern Med. 2001;134(9):868–81. WOS:000168543100011. doi: 10.7326/0003-4819-134-9_part_2-200105011-00011 [DOI] [PubMed] [Google Scholar]
- 38.Yunus MB. Fibromyalgia and overlapping disorders: The unifying concept of central sensitivity syndromes. Semin Arthritis Rheu. 2007;36(6):339–56. WOS:000247151800002. doi: 10.1016/j.semarthrit.2006.12.009 [DOI] [PubMed] [Google Scholar]
- 39.Kanaan RAA, Lepine JP, Wessely SC. The association or otherwise of the functional somatic syndromes. Psychosomatic Medicine. 2007;69(9):855–9. WOS:000251204900008. doi: 10.1097/PSY.0b013e31815b001a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Borchers AT, Gershwin ME. Fibromyalgia: A Critical and Comprehensive Review. Clin Rev Allerg Immu. 2015;49(2):100–51. WOS:000362902500002. doi: 10.1007/s12016-015-8509-4 [DOI] [PubMed] [Google Scholar]
- 41.Fink P, Schroder A. One single diagnosis, bodily distress syndrome, succeeded to capture 10 diagnostic categories of functional somatic syndromes and somatoform disorders. J Psychosom Res. 2010;68(5):415–26. WOS:000277189900004. doi: 10.1016/j.jpsychores.2010.02.004 [DOI] [PubMed] [Google Scholar]
- 42.Rief W, Isaac M. Are somatoform disorders ’mental disorders’? A contribution to the current debate. Curr Opin Psychiatr. 2007;20(2):143–6. doi: 10.1097/YCO.0b013e3280346999 WOS:000244633200008. [DOI] [PubMed] [Google Scholar]
- 43.Revel M, Andre-Deshays C, Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991;72(5):288–91. Epub 1991/04/01. . [PubMed] [Google Scholar]
- 44.Tinazzi M, Fasano A, Di Matteo A, Conte A, Bove F, Bovi T, et al. Temporal discrimination in patients with dystonia and tremor and patients with essential tremor. Neurology. 2013;80(1):76–84. Epub 2012/12/18. doi: 10.1212/WNL.0b013e31827b1a54 . [DOI] [PubMed] [Google Scholar]
- 45.Sherrington CS. The christening of physiology. Arch Neerl Physiol Homme Anim. 1948;28(3–4):369–72. Epub 1948/01/01. . [PubMed] [Google Scholar]
- 46.Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3(8):655–66. WOS:000177447800016. doi: 10.1038/nrn894 [DOI] [PubMed] [Google Scholar]
- 47.Khalsa SS, Rudrauf D, Feinstein JS, Tranel D. The pathways of interoceptive awareness. Nat Neurosci. 2009;12(12):1494–6. Epub 2009/11/03. doi: 10.1038/nn.2411 ; PubMed Central PMCID: PMC2787640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ceunen E, Vlaeyen JW, Van Diest I. On the Origin of Interoception. Front Psychol. 2016;7:743. Epub 2016/06/01. doi: 10.3389/fpsyg.2016.00743 ; PubMed Central PMCID: PMC4876111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Treleaven J, Takasaki H. High variability of the subjective visual vertical test of vertical perception, in some people with neck pain—Should this be a standard measure of cervical proprioception? Man Ther. 2015;20(1):183–8. Epub 2014/09/23. doi: 10.1016/j.math.2014.08.005 . [DOI] [PubMed] [Google Scholar]
- 50.Bogaerts K, Millen A, Li W, De Peuter S, Van Diest I, Vlemincx E, et al. High symptom reporters are less interoceptively accurate in a symptom-related context. J Psychosom Res. 2008;65(5):417–24. WOS:000260687900003. doi: 10.1016/j.jpsychores.2008.03.019 [DOI] [PubMed] [Google Scholar]
- 51.Bardal EM, Roeleveld K, Ihlen E, Mork PJ. Micro movements of the upper limb in fibromyalgia: The relation to proprioceptive accuracy and visual feedback. J Electromyogr Kines. 2016;26:1–7. WOS:000370187700003. doi: 10.1016/j.jelekin.2015.12.006 [DOI] [PubMed] [Google Scholar]
- 52.Bardal EM, Roeleveld K, Johansen TO, Mork PJ. Upper limb position control in fibromyalgia. Bmc Musculoskel Dis. 2012;13. Artn 186. WOS:000312404900002. doi: 10.1186/1471-2474-13-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stanislaw H, Todorov N. Calculation of signal detection theory measures. Behav Res Methods Instrum Comput. 1999;31(1):137–49. Epub 1999/09/25. doi: 10.3758/bf03207704 . [DOI] [PubMed] [Google Scholar]
- 54.Viechtbauer W. Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software. 2010;36(3):1–48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 55.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. New Jersey, USA: John Wiley & Sons, Ltd; 2009. [Google Scholar]
- 56.Friedman H. Simplified Determinations of Statistical Power, Magnitude of Effect and Research Sample Sizes. Educ Psychol Meas. 1982;42(2):521–6. WOS:A1982NV54100014. [Google Scholar]
- 57.Rosenthal R. Meta-analytic procedures for social research. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 58.Krautwurst S, Gerlach AL, Gomille L, Hiller W, Witthöft M. Health anxiety—An indicator of higher interoceptive sensitivity? J Behav Ther Exp Psy. 2014;45(2):303–9. WOS:000334013400012. [DOI] [PubMed] [Google Scholar]
- 59.Pilowsky I. Dimensions of hypochondriasis. The British journal of psychiatry: the journal of mental science. 1967;113(494):89–93. doi: 10.1192/bjp.113.494.89 . [DOI] [PubMed] [Google Scholar]
- 60.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological methods. 1998;3(4):486–504. WOS:000077640200006. [Google Scholar]
- 61.Gavaghan DJ, Moore AR, McQuay HJ. An evaluation of homogeneity tests in meta-analyses in pain using simulations of individual patient data. Pain. 2000;85(3):415–24. Epub 2000/04/27. doi: 10.1016/S0304-3959(99)00302-4 . [DOI] [PubMed] [Google Scholar]
- 62.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. Epub 2003/09/06. doi: 10.1136/bmj.327.7414.557 ; PubMed Central PMCID: PMC192859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. Epub 2002/07/12. doi: 10.1002/sim.1186 . [DOI] [PubMed] [Google Scholar]
- 64.Field AP, Gillett R. How to do a meta-analysis. Brit J Math Stat Psy. 2010;63(3):665–94. WOS:000284251100011. [DOI] [PubMed] [Google Scholar]
- 65.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. Epub 2014/07/22. doi: 10.1016/j.ijsu.2014.07.013 . [DOI] [PubMed] [Google Scholar]
- 66.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. Epub 2011/10/20. doi: 10.1136/bmj.d5928 ; PubMed Central PMCID: PMC3196245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Di Lernia D, Serino S, Riva G. Pain in the body. Altered interoception in chronic pain conditions: A systematic review. Neurosci Biobehav R. 2016;71:328–41. WOS:000390502100022. doi: 10.1016/j.neubiorev.2016.09.015 [DOI] [PubMed] [Google Scholar]
- 68.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. Epub 2000/07/06. doi: 10.1111/j.0006-341x.2000.00455.x . [DOI] [PubMed] [Google Scholar]
- 69.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–34. Epub 1997/10/06. doi: 10.1136/bmj.315.7109.629 ; PubMed Central PMCID: PMC2127453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rosenthal R. The File Drawer Problem and Tolerance for Null Results. Psychol Bull. 1979;86(3):638–41. WOS:A1979JS26200011. [Google Scholar]
- 71.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. Epub 1994/12/01. . [PubMed] [Google Scholar]
- 72.Vevea JL, Woods CM. Publication bias in research synthesis: sensitivity analysis using a priori weight functions. Psychological methods. 2005;10(4):428–43. Epub 2006/01/06. doi: 10.1037/1082-989X.10.4.428 . [DOI] [PubMed] [Google Scholar]
- 73.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.World Health Organization. International statistical classification of diseases and related health problems. 10th ed2016.
- 75.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. ed. Washington, DC: Author; 2000. [Google Scholar]
- 76.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. Epub 2002/03/27. doi: 10.1097/00006842-200203000-00008 . [DOI] [PubMed] [Google Scholar]
- 77.Wientjes CJ, Grossman P. Overreactivity of the psyche or the soma? Interindividual associations between psychosomatic symptoms, anxiety, heart rate, and end-tidal partial carbon dioxide pressure. Psychosom Med. 1994;56(6):533–40. Epub 1994/11/01. doi: 10.1097/00006842-199411000-00009 . [DOI] [PubMed] [Google Scholar]
- 78.Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1988. [Google Scholar]
- 79.Barsky AJ, Brener J, Coeytaux RR, Cleary PD. Accurate awareness of heartbeat in hypochondriacal and non-hypochondriacal patients. J Psychosom Res. 1995;39(4):489–97. Epub 1995/05/01. doi: 10.1016/0022-3999(94)00166-3 . [DOI] [PubMed] [Google Scholar]
- 80.Bräscher AK, Schulz SM, Van den Bergh O, Witthöft M. Prospective study of nocebo effects related to symptoms of idiopathic environmental intolerance attributed to electromagnetic fields (IEI-EMF). Environ Res. 2020;190. ARTN 110019 WOS:000576671000001. [DOI] [PubMed] [Google Scholar]
- 81.Ferentzi E, Horvath A, Koteles F. Do body-related sensations make feel us better? Subjective well-being is associated only with the subjective aspect of interoception. Psychophysiology. 2019;56(4):e13319. Epub 2019/01/11. doi: 10.1111/psyp.13319 . [DOI] [PubMed] [Google Scholar]
- 82.Haenen MA, Schmidi AJ, Schoenmakers M, van den Hout MA. Tactual sensitivity in hypochondriasis. Psychother Psychosom. 1997;66(3):128–32. Epub 1997/01/01. doi: 10.1159/000289122 . [DOI] [PubMed] [Google Scholar]
- 83.Krautwurst S, Gerlach AL, Witthöft M. Interoception in pathological health anxiety. J Abnorm Psychol. 2016;125(8):1179–84. doi: 10.1037/abn0000210 [DOI] [PubMed] [Google Scholar]
- 84.Lee D, Kim SJ, Cheon J, Hwang EH, Jung YC, Kang JI. Characteristics of Autonomic Activity and Reactivity During Rest and Emotional Processing and Their Clinical Correlations in Somatic Symptom Disorder. Psychosomatic Medicine. 2018;80(8):690–7. WOS:000447173000001. doi: 10.1097/PSY.0000000000000622 [DOI] [PubMed] [Google Scholar]
- 85.Meyerholz L, Irzinger J, Witthöft M, Gerlach AL, Pohl A. Contingent biofeedback outperforms other methods to enhance the accuracy of cardiac interoception: A comparison of short interventions. J Behav Ther Exp Psychiatry. 2019;63:12–20. Epub 2018/12/18. doi: 10.1016/j.jbtep.2018.12.002 . [DOI] [PubMed] [Google Scholar]
- 86.Miles E, Poliakoff E, Brown RJ. Medically unexplained symptom reports are associated with a decreased response to the rubber hand illusion. J Psychosom Res. 2011;71(4):240–4. Epub 2011/09/14. doi: 10.1016/j.jpsychores.2011.04.002 . [DOI] [PubMed] [Google Scholar]
- 87.Perepelkina O, Romanov D, Arina G, Volel B, Nikolaeva V. Multisensory mechanisms of body perception in somatoform disorders. J Psychosom Res. 2019;127. ARTN 109837 WOS:000503320200005. doi: 10.1016/j.jpsychores.2019.109837 [DOI] [PubMed] [Google Scholar]
- 88.Rodic D, Meyer AH, Lieb R, Meinlschmidt G. The Association of Sensory Responsiveness with Somatic Symptoms and Illness Anxiety. Int J Behav Med. 2016;23(1):39–48. Epub 2015/04/22. doi: 10.1007/s12529-015-9483-1 . [DOI] [PubMed] [Google Scholar]
- 89.Sarnoch H, Adler F, Scholz OB. Die Wahrnehmung propriozeptiver Reize in Abhängigkeit von der Somatisierungstendenz. Verhaltenstherapie und Verhaltensmedizin. 1997;18:419–28. [Google Scholar]
- 90.Schulz A, Rost S, Flasinski T, Dierolf AM, Lutz APC, Munch EE, et al. Distinctive body perception mechanisms in high versus low symptom reporters: A neurophysiological model for medically-unexplained symptoms. J Psychosom Res. 2020;137:110223. Epub 2020/09/01. doi: 10.1016/j.jpsychores.2020.110223 . [DOI] [PubMed] [Google Scholar]
- 91.Witthöft M, Bräscher AK, Jungmann SM, Koteles F. Somatic Symptom Perception and Interoception A Latent-Variable Approach. Z Psychol. 2020;228(2):100–9. WOS:000535722000005. [Google Scholar]
- 92.Akyol Y, Ulus Y, Tander B, Bilgici A, Kuru O. Muscle Strength, Fatigue, Functional Capacity, and Proprioceptive Acuity in Patients With Fibromyalgia. Turk Fiz Tip Rehab D. 2013;59(4):292–8. WOS:000340589000005. [Google Scholar]
- 93.Anastasopoulos D, Bhatia K, Bisdorff A, Bronstein AM, Gresty MA, Marsden CD. Perception of spatial orientation in spasmodic torticollis .1. The postural vertical. Mov Disord. 1997;12(4):561–9. WOS:A1997XM20000012. doi: 10.1002/mds.870120413 [DOI] [PubMed] [Google Scholar]
- 94.Bara-Jimenez W, Shelton P, Sanger TD, Hallett M. Sensory discrimination capabilities in patients with focal hand dystonia. Ann Neurol. 2000;47(3):377–80. WOS:000085731700016. [PubMed] [Google Scholar]
- 95.Bara-Jimenez W, Shelton P, Hallett M. Spatial discrimination is abnormal in focal hand dystonia. Neurology. 2000;55(12):1869–73. WOS:000166018800020. doi: 10.1212/wnl.55.12.1869 [DOI] [PubMed] [Google Scholar]
- 96.Borg C, Chouchou F, Dayot-Gorlero J, Zimmerman P, Maudoux D, Laurent B, et al. Pain and emotion as predictive factors of interoception in fibromyalgia. J Pain Res. 2018;11:823–35. WOS:000431255700001. doi: 10.2147/JPR.S152012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brun C, McCabe CS, Mercier C. The Contribution of Motor Commands to the Perturbations Induced by Sensorimotor Conflicts in Fibromyalgia. Neuroscience. 2020;434:55–65. Epub 2020/03/23. doi: 10.1016/j.neuroscience.2020.03.017 . [DOI] [PubMed] [Google Scholar]
- 98.Celenay ST, Mete O, Coban O, Oskay D, Erten S. Trunk position sense, postural stability, and spine posture in fibromyalgia. Rheumatol Int. 2019;39(12):2087–94. WOS:000505166800009. doi: 10.1007/s00296-019-04399-1 [DOI] [PubMed] [Google Scholar]
- 99.Cheng CH, Wang JL, Lin JJ, Wang SF, Lin KH. Position accuracy and electromyographic responses during head reposition in young adults with chronic neck pain. J Electromyogr Kines. 2010;20(5):1014–20. WOS:000280576100031. doi: 10.1016/j.jelekin.2009.11.002 [DOI] [PubMed] [Google Scholar]
- 100.Demartini B, Goeta D, Barbieri V, Ricciardi L, Canevini MP, Turner K, et al. Psychogenic non-epileptic seizures and functional motor symptoms: A common phenomenology? J Neurol Sci. 2016;368:49–54. Epub 2016/08/20. doi: 10.1016/j.jns.2016.06.045 . [DOI] [PubMed] [Google Scholar]
- 101.Demartini B, Goeta D, Romito L, Anselmetti S, Bertelli S, D’Agostino A, et al. Anorexia Nervosa and Functional Motor Symptoms: Two Faces of the Same Coin? J Neuropsychiatry Clin Neurosci. 2017;29(4):383–90. Epub 2017/06/01. doi: 10.1176/appi.neuropsych.16080156 . [DOI] [PubMed] [Google Scholar]
- 102.De Pauw J, Mercelis R, Hallemans A, Michiels S, Truijen S, Cras P, et al. Cervical sensorimotor control in idiopathic cervical dystonia: A cross-sectional study. Brain Behav. 2017;7(9):e00735. Epub 2017/09/28. doi: 10.1002/brb3.735 ; PubMed Central PMCID: PMC5607536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.De Zoete RMJ, Osmotherly PG, Rivett DA, Snodgrass SJ. No Differences Between Individuals With Chronic Idiopathic Neck Pain and Asymptomatic Individuals on 7 Cervical Sensorimotor Control Tests: A Cross-sectional Study. J Orthop Sport Phys. 2020;50(1):33–43. WOS:000505052000005. doi: 10.2519/jospt.2020.8846 [DOI] [PubMed] [Google Scholar]
- 104.Dumas JP, Arsenault AB, Boudreau G, Magnoux E, Lepage Y, Bellavance A, et al. Physical impairments in cervicogenic headache: traumatic vs. nontraumatic onset. Cephalalgia. 2001;21(9):884–93. WOS:000173046000005. doi: 10.1046/j.1468-2982.2001.00264.x [DOI] [PubMed] [Google Scholar]
- 105.Duschek S, Montoro CI, del Paso GAR. Diminished Interoceptive Awareness in Fibromyalgia Syndrome. Behav Med. 2017;43(2):100–7. WOS:000402671700003. doi: 10.1080/08964289.2015.1094442 [DOI] [PubMed] [Google Scholar]
- 106.Edmondston SJ, Chan HY, Ngai GC, Warren ML, Williams JM, Glennon S, et al. Postural neck pain: an investigation of habitual sitting posture, perception of ’good’ posture and cervicothoracic kinaesthesia. Man Ther. 2007;12(4):363–71. Epub 2006/09/12. doi: 10.1016/j.math.2006.07.007 . [DOI] [PubMed] [Google Scholar]
- 107.Elsig S, Luomajoki H, Sattelmayer M, Taeymans J, Tal-Akabi A, Hilfiker R. Sensorimotor tests, such as movement control and laterality judgment accuracy, in persons with recurrent neck pain and controls. A case-control study. Manual Ther. 2014;19(6):555–61. WOS:000347721000009. doi: 10.1016/j.math.2014.05.014 [DOI] [PubMed] [Google Scholar]
- 108.Fiorio M, Gambarin M, Valente EM, Liberini P, Loi M, Cossu G, et al. Defective temporal processing of sensory stimuli in DYT1 mutation carriers: a new endophenotype of dystonia? Brain. 2007;130:134–42. WOS:000243061500012. doi: 10.1093/brain/awl283 [DOI] [PubMed] [Google Scholar]
- 109.Fiorio M, Tinazzi M, Scontrini A, Stanzani C, Gambarin M, Fiaschi A, et al. Tactile temporal discrimination in patients with blepharospasm. J Neurol Neurosurg Psychiatry. 2008;79(7):796–8. Epub 2007/11/08. doi: 10.1136/jnnp.2007.131524 . [DOI] [PubMed] [Google Scholar]
- 110.Fiorio M, Weise D, Onal-Hartmann C, Zeller D, Tinazzi M, Classen J. Impairment of the rubber hand illusion in focal hand dystonia. Brain. 2011;134:1428–37. WOS:000290818600022. doi: 10.1093/brain/awr026 [DOI] [PubMed] [Google Scholar]
- 111.Gajdos P, Chriszto Z, Rigo A. The association of different interoceptive dimensions with functional gastrointestinal symptoms. J Health Psychol. 2020:1359105320929426. Epub 2020/06/17. doi: 10.1177/1359105320929426 . [DOI] [PubMed] [Google Scholar]
- 112.Goncalves C, Silva AG. Reliability, measurement error and construct validity of four proprioceptive tests in patients with chronic idiopathic neck pain. Musculoskelet Sci Pract. 2019;43:103–9. Epub 2019/08/04. doi: 10.1016/j.msksp.2019.07.010 . [DOI] [PubMed] [Google Scholar]
- 113.Grip H, Sundelin G, Gerdle B, Karlsson JS. Variations in the axis of motion during head repositioning—A comparison of subjects with whiplash-associated disorders or non-specific neck pain and healthy controls. Clin Biomech. 2007;22(8):865–73. WOS:000249643200001. doi: 10.1016/j.clinbiomech.2007.05.008 [DOI] [PubMed] [Google Scholar]
- 114.Jungilligens J, Wellmer J, Schlegel U, Kessler H, Axmacher N, Popkirov S. Impaired emotional and behavioural awareness and control in patients with dissociative seizures. Psychol Med. 2020;50(16):2731–9. Epub 2019/10/19. doi: 10.1017/S0033291719002861 . [DOI] [PubMed] [Google Scholar]
- 115.Katschnig P, Edwards MJ, Schwingenschuh P, Aguirregomozcorta M, Kagi G, Rothwell JC, et al. Mental Rotation of Body Parts and Sensory Temporal Discrimination in Fixed Dystonia. Mov Disord. 2010;25(8):1061–7. WOS:000279044600014. doi: 10.1002/mds.23047 [DOI] [PubMed] [Google Scholar]
- 116.Koreki A, Garfkinel SN, Mula M, Agrawal N, Cope S, Eilon T, et al. Trait and state interoceptive abnormalities are associated with dissociation and seizure frequency in patients with functional seizures. Epilepsia. 2020;61(6):1156–65. Epub 2020/06/06. doi: 10.1111/epi.16532 ; PubMed Central PMCID: PMC7737228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kristjansson E, Dall’Alba P, Jull G. A study of five cervicocephalic relocation tests in three different subject groups. Clin Rehabil. 2003;17(7):768–74. WOS:000186152000011. doi: 10.1191/0269215503cr676oa [DOI] [PubMed] [Google Scholar]
- 118.Lee HY, Wang JD, Yao G, Wang SF. Association between cervicocephalic kinesthetic sensibility and frequency of subclinical neck pain. Manual Ther. 2008;13(5):419–25. WOS:000259379700007. doi: 10.1016/j.math.2007.04.001 [DOI] [PubMed] [Google Scholar]
- 119.Marinelli L, Pelosin E, Trompetto C, Avanzino L, Ghilardi MF, Abbruzzese G, et al. In idiopathic cervical dystonia movement direction is inaccurate when reaching in unusual workspaces. Parkinsonism Relat D. 2011;17(6):470–2. WOS:000292948500015. doi: 10.1016/j.parkreldis.2011.01.017 [DOI] [PubMed] [Google Scholar]
- 120.Morgante F, Tinazzi M, Squintani G, Martino D, Defazio G, Romito L, et al. Abnormal tactile temporal discrimination in psychogenic dystonia. Neurology. 2011;77(12):1191–7. WOS:000295027800017. doi: 10.1212/WNL.0b013e31822f0449 [DOI] [PubMed] [Google Scholar]
- 121.Nijs J, Aerts A, De Meirleir K. Generalized joint hypermobility is more common in chronic fatigue syndrome than in healthy control subjects. J Manip Physiol Ther. 2006;29(1):32–9. WOS:000234605000005. doi: 10.1016/j.jmpt.2005.11.004 [DOI] [PubMed] [Google Scholar]
- 122.Pick S, Rojas-Aguiluz M, Butler M, Mulrenan H, Nicholson TR, Goldstein LH. Dissociation and interoception in functional neurological disorder. Cogn Neuropsychiatry. 2020;25(4):294–311. Epub 2020/07/09. doi: 10.1080/13546805.2020.1791061 . [DOI] [PubMed] [Google Scholar]
- 123.Pinsault N, Vuillerme N, Pavan P. Cervicocephalic relocation test to the neutral head position: assessment in bilateral labyrinthine-defective and chronic, nontraumatic neck pain patients. Arch Phys Med Rehabil. 2008;89(12):2375–8. Epub 2008/12/09. doi: 10.1016/j.apmr.2008.06.009 . [DOI] [PubMed] [Google Scholar]
- 124.Ricciardi L, Demartini B, Crucianelli L, Krahe C, Edwards MJ, Fotopoulou A. Interoceptive awareness in patients with functional neurological symptoms. Biol Psychol. 2016;113:68–74. Epub 2015/11/04. doi: 10.1016/j.biopsycho.2015.10.009 . [DOI] [PubMed] [Google Scholar]
- 125.Rost S, Van Ryckeghem DM, Schulz A, Crombez G, Vogele C. Generalized hypervigilance in fibromyalgia: Normal interoceptive accuracy, but reduced self-regulatory capacity. J Psychosom Res. 2017;93:48–54. Epub 2017/01/22. doi: 10.1016/j.jpsychores.2016.12.003 . [DOI] [PubMed] [Google Scholar]
- 126.Sanger TD, Tarsy D, Pascual-Leone A. Abnormalities of spatial and temporal sensory discrimination in writer’s cramp. Mov Disord. 2001;16(1):94–9. WOS:000166762900014. doi: [DOI] [PubMed] [Google Scholar]
- 127.Scontrini A, Conte A, Defazio G, Fiorio M, Fabbrini G, Suppa A, et al. Somatosensory temporal discrimination in patients with primary focal dystonia. J Neurol Neurosurg Psychiatry. 2009;80(12):1315–9. Epub 2009/06/23. doi: 10.1136/jnnp.2009.178236 . [DOI] [PubMed] [Google Scholar]
- 128.Sjolander P, Michaelson P, Jaric S, Djupsjobacka M. Sensorimotor disturbances in chronic neck pain—range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther. 2008;13(2):122–31. Epub 2007/01/02. doi: 10.1016/j.math.2006.10.002 . [DOI] [PubMed] [Google Scholar]
- 129.Tinazzi M, Frasson E, Bertolasi L, Fiaschi A, Aglioti S. Temporal discrimination of somesthetic stimuli is impaired in dystonic patients. Neuroreport. 1999;10(7):1547–50. WOS:000080653300029. doi: 10.1097/00001756-199905140-00028 [DOI] [PubMed] [Google Scholar]
- 130.Tinazzi M, Fiaschi A, Frasson E, Fiorio M, Cortese F, Aglioti SM. Deficits of temporal discrimination in dystonia are independent from the spatial distance between the loci of tactile stimulation. Mov Disord. 2002;17(2):333–8. WOS:000174740500015. doi: 10.1002/mds.10019 [DOI] [PubMed] [Google Scholar]
- 131.Ulus Y, Akyol Y, Tander B, Bilgici A, Kuru O. Knee Proprioception and Balance in Turkish Women With and Without Fibromyalgia Syndrome. Turk Fiz Tip Rehab D. 2013;59(2):128–32. WOS:000321475100009. [Google Scholar]
- 132.Valenzuela-Moguillansky C, Reyes-Reyes A, Gaete MI. Exteroceptive and Interoceptive Body-Self Awareness in Fibromyalgia Patients. Front Hum Neurosci. 2017;11:117. Epub 2017/03/30. doi: 10.3389/fnhum.2017.00117 ; PubMed Central PMCID: PMC5346579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Woodhouse A, Vasseljen O. Altered motor control patterns in whiplash and chronic neck pain. Bmc Musculoskel Dis. 2008;9. Artn 90 WOS:000257493700001. doi: 10.1186/1471-2474-9-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Petersen S, Ritz T. The role of fearful beliefs in the relationship between situational self-awareness and report of breathing-related sensations. Brit J Health Psych. 2011;16:359–72. WOS:000289484900011. doi: 10.1348/135910710X509900 [DOI] [PubMed] [Google Scholar]
- 135.Bogaerts K, Notebaert K, Van Diest I, Devriese S, De Peuter S, Van den Bergh O. Accuracy of respiratory symptom perception in different affective contexts. J Psychosom Res. 2005;58(6):537–43. WOS:000232258500009. doi: 10.1016/j.jpsychores.2004.12.005 [DOI] [PubMed] [Google Scholar]
- 136.Petersen S, Schroijen M, Molders C, Zenker S, Van den Bergh O. Categorical Interoception Perceptual Organization of Sensations From Inside. Psychol Sci. 2014;25(5):1059–66. WOS:000335549100001. doi: 10.1177/0956797613519110 [DOI] [PubMed] [Google Scholar]
- 137.Corneille O, Klein O, Lambert S, Judd CM. On the role of familiarity with units of measurement in categorical accentuation: Tajfel and Wilkes (1963) revisited and replicated. Psychol Sci. 2002;13(4):380–3. WOS:000176591200013. doi: 10.1111/1467-9280.00468 [DOI] [PubMed] [Google Scholar]
- 138.De Peuter S, Van Diest I, Lemaigre V, Li W, Verleden G, Demedts M, et al. Can subjective asthma symptoms be learned? Psychosomatic Medicine. 2005;67(3):454–61. WOS:000229349800017. doi: 10.1097/01.psy.0000160470.43167.e2 [DOI] [PubMed] [Google Scholar]
- 139.van den Bergh O, Kempynck PJ, van de Woestijne KP, Baeyens F, Eelen P. Respiratory learning and somatic complaints: a conditioning approach using CO2-enriched air inhalation. Behav Res Ther. 1995;33(5):517–27. Epub 1995/06/01. doi: 10.1016/0005-7967(94)00080-4 . [DOI] [PubMed] [Google Scholar]
- 140.Van den Bergh O, Stegen K, Van de Woestijne KP. Learning to have psychosomatic complaints: Conditioning of respiratory behavior and somatic complaints in psychosomatic patients. Psychosomatic Medicine. 1997;59(1):13–23. WOS:A1997WF12100003. doi: 10.1097/00006842-199701000-00003 [DOI] [PubMed] [Google Scholar]
- 141.Van den Bergh O, Winters W, Devriese S, Van Diest I. Learning subjective health complaints. Scand J Psychol. 2002;43(2):147–52. Epub 2002/05/15. doi: 10.1111/1467-9450.00280 . [DOI] [PubMed] [Google Scholar]
- 142.Janssens T, Verleden G, De Peuter S, Van Diest I, Van den Bergh O. Inaccurate perception of asthma symptoms: a cognitive-affective framework and implications for asthma treatment. Clin Psychol Rev. 2009;29(4):317–27. Epub 2009/03/17. doi: 10.1016/j.cpr.2009.02.006 . [DOI] [PubMed] [Google Scholar]
- 143.Kroenke K. A Practical and Evidence-Based Approach to Common Symptoms A Narrative Review. Ann Intern Med. 2014;161(8):579–U82. WOS:000343906800019. doi: 10.7326/M14-0461 [DOI] [PubMed] [Google Scholar]
- 144.Murphy J, Brewer R, Catmur C, Bird G. Interoception and psychopathology: A developmental neuroscience perspective. Dev Cogn Neurosci. 2017;23:45–56. Epub 2017/01/13. doi: 10.1016/j.dcn.2016.12.006 ; PubMed Central PMCID: PMC6987654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Herbert BM, Muth ER, Pollatos O, Herbert C. Interoception across Modalities: On the Relationship between Cardiac Awareness and the Sensitivity for Gastric Functions. Plos One. 2012;7(5). ARTN e36646 WOS:000305338200036. doi: 10.1371/journal.pone.0036646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whitehead WE, Drescher VM. Perception of Gastric Contractions and Self-Control of Gastric-Motility. Psychophysiology. 1980;17(6):552–8. WOS:A1980KQ19900006. doi: 10.1111/j.1469-8986.1980.tb02296.x [DOI] [PubMed] [Google Scholar]
- 147.Tsakiris M, Tajadura-Jimenez A, Costantini M. Just a heartbeat away from one’s body: interoceptive sensitivity predicts malleability of body-representations. P Roy Soc B-Biol Sci. 2011;278(1717):2470–6. WOS:000292592000009. doi: 10.1098/rspb.2010.2547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Steptoe A, Noll A. The perception of bodily sensations, with special reference to hypochondriasis. Behav Res Ther. 1997;35(10):901–10. Epub 1997/12/24. doi: 10.1016/s0005-7967(97)00055-7 . [DOI] [PubMed] [Google Scholar]
- 149.Ehlers A, Breuer P. Increased Cardiac Awareness in Panic Disorder. J Abnorm Psychol. 1992;101(3):371–82. WOS:A1992JF69800001. doi: 10.1037//0021-843x.101.3.371 [DOI] [PubMed] [Google Scholar]
- 150.Garfinkel SN, Manassei MF, Hamilton-Fletcher G, den Bosch YI, Critchley HD, Engels M. Interoceptive dimensions across cardiac and respiratory axes. Philos T R Soc B. 2016;371(1708). ARTN 20160014 WOS:000387766300011. doi: 10.1098/rstb.2016.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Steptoe A, Vogele C. Individual-Differences in the Perception of Bodily Sensations—the Role of Trait Anxiety and Coping Style. Behav Res Ther. 1992;30(6):597–607. WOS:A1992JU12800005. doi: 10.1016/0005-7967(92)90005-2 [DOI] [PubMed] [Google Scholar]
- 152.Ferentzi E, Bogdany T, Szabolcs Z, Csala B, Horvath A, Koteles F. Multichannel Investigation of Interoception: Sensitivity Is Not a Generalizable Feature. Front Hum Neurosci. 2018;12:223. Epub 2018/06/19. doi: 10.3389/fnhum.2018.00223 ; PubMed Central PMCID: PMC5992275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lonn J, Crenshaw AG, Djupsjobacka M, Johansson H. Reliability of position sense testing assessed with a fully automated system. Clin Physiol. 2000;20(1):30–7. WOS:000085367300006. doi: 10.1046/j.1365-2281.2000.00218.x [DOI] [PubMed] [Google Scholar]
- 154.Elangovan N, Herrmann A, Konczak J. Assessing Proprioceptive Function: Evaluating Joint Position Matching Methods Against Psychophysical Thresholds. Phys Ther. 2014;94(4):553–61. WOS:000333876900011. doi: 10.2522/ptj.20130103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Catley MJ, Tabor A, Wand BM, Moseley GL. Assessing tactile acuity in rheumatology and musculoskeletal medicine-how reliable are two-point discrimination tests at the neck, hand, back and foot? Rheumatology. 2013;52(8):1454–61. WOS:000321735000019. doi: 10.1093/rheumatology/ket140 [DOI] [PubMed] [Google Scholar]
- 156.Pohl A, Hums AC, Kraft G, Köteles F, Gerlach AL, Witthöft M. Cardiac interoception: A novel signal detection approach and relations to somatic symptom distress. Psychol Assess. 2021;33(8):705–15. Epub 2021/04/09. doi: 10.1037/pas0001012 . [DOI] [PubMed] [Google Scholar]
- 157.Brener J, Ring C. Towards a psychophysics of interoceptive processes: the measurement of heartbeat detection. Philos Trans R Soc Lond B Biol Sci. 2016;371(1708):20160015. Epub 2016/10/10. doi: 10.1098/rstb.2016.0015 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zamariola G, Maurage P, Luminet O, Corneille O. Interoceptive accuracy scores from the heartbeat counting task are problematic: Evidence from simple bivariate correlations. Biol Psychol. 2018;137:12–7. doi: 10.1016/j.biopsycho.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 159.Andor T, Gerlach AL, Rist F. Superior perception of phasic physiological arousal and the detrimental consequences of the conviction to be aroused on worrying and metacognitions in GAD. J Abnorm Psychol. 2008;117(1):193–205. WOS:000252990000016. doi: 10.1037/0021-843X.117.1.193 [DOI] [PubMed] [Google Scholar]
- 160.Lau P, Miesen M, Wunderlich R, Stein A, Engell A, Wollbrink A, et al. The Relevance of Interoception in Chronic Tinnitus: Analyzing Interoceptive Sensibility and Accuracy. Biomed Res Int. 2015;2015:487372. doi: 10.1155/2015/487372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ring C, Brener J, Knapp K, Mailloux J. Effects of heartbeat feedback on beliefs about heart rate and heartbeat counting: A cautionary tale about interoceptive awareness. Biol Psychol. 2015;104:193–8. WOS:000348034700070. doi: 10.1016/j.biopsycho.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 162.Egloff N, Camara RJ, von Kanel R, Klingler N, Marti E, Ferrari ML. Hypersensitivity and hyperalgesia in somatoform pain disorders. Gen Hosp Psychiatry. 2014;36(3):284–90. Epub 2014/03/22. doi: 10.1016/j.genhosppsych.2014.01.011 . [DOI] [PubMed] [Google Scholar]
- 163.Gramling SE, Clawson EP, McDonald MK. Perceptual and cognitive abnormality model of hypochondriasis: amplification and physiological reactivity in women. Psychosom Med. 1996;58(5):423–31. Epub 1996/09/01. doi: 10.1097/00006842-199609000-00005 . [DOI] [PubMed] [Google Scholar]
- 164.Pollatos O, Herbert BM, Wankner S, Dietel A, Wachsmuth C, Henningsen P, et al. Autonomic imbalance is associated with reduced facial recognition in somatoform disorders. J Psychosom Res. 2011;71(4):232–9. WOS:000295149900005. doi: 10.1016/j.jpsychores.2011.03.012 [DOI] [PubMed] [Google Scholar]
- 165.Pollatos O, Herbert BM, Mai S, Kammer T. Changes in interoceptive processes following brain stimulation. Philos Trans R Soc Lond B Biol Sci. 2016;371(1708). Epub 2017/01/13. doi: 10.1098/rstb.2016.0016 ; PubMed Central PMCID: PMC5062104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hassanpour MS, Simmons WK, Feinstein JS, Luo Q, Lapidus RC, Bodurka J, et al. The Insular Cortex Dynamically Maps Changes in Cardiorespiratory Interoception. Neuropsychopharmacology. 2018;43(2):426–34. Epub 2017/07/21. doi: 10.1038/npp.2017.154 ; PubMed Central PMCID: PMC5729563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Khalsa SS, Rudrauf D, Sandesara C, Olshansky B, Tranel D. Bolus isoproterenol infusions provide a reliable method for assessing interoceptive awareness. Int J Psychophysiol. 2009;72(1):34–45. Epub 2008/10/16. doi: 10.1016/j.ijpsycho.2008.08.010 ; PubMed Central PMCID: PMC3085829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Corneille O, Desmedt O, Zamariola G, Luminet O, Maurage P. et al. (2020), A heartfelt response to Zimprich and Ainley (2020)’s commentaries: Acknowledging issues with the HCT would benefit interoception research. Biol Psychol. 2020;152:107869. doi: 10.1016/j.biopsycho.2020.107869 [DOI] [PubMed] [Google Scholar]
- 169.Craske MG, Wolitzky-Taylor KB, Labus J, Wu S, Frese M, Mayer EA, et al. A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behav Res Ther. 2011;49(6–7):413–21. WOS:000292224000006. doi: 10.1016/j.brat.2011.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Malmo RB, Shagass C. Physiologic Study of Symptom Mechanisms in Psychiatric Patients under Stress. Psychosomatic Medicine. 1949;11(1):25–9. WOS:A1949UZ69600003. doi: 10.1097/00006842-194901000-00004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
TS = topic, TI = title.
(DOCX)
CFS = chronic fatigue syndrome, CFS-APQ = Chronic Fatigue Syndrome Activities and Participation Questionnaire, CG = control group, CSD = Checklist for Symptoms in Daily Life, EG = experimental group, FIQ = Fibromyalgia Impact Questionnaire, HAF-17 = Cardiac Anxiety Questionnaire [Herzangstfragebogen], IAcc = interoceptive accuracy, IQR = interquartile range, M = mean, Mdn = Median, MIHT = Multidimensional Inventory of Hypochondriacal Traits, NA = not available, n.s. = not significant, NSCF = nonspecific skin conductance fluctuations, PHQ-15/PHQ-D = Patient Health Questionnaire, RB = response bias, SD = standard deviation, SDQ/SDQ-20 = Somatoform Dissociation Questionnaire, SE = standard error, SOMS = Screening for Somatoform Symptoms, SSAS = Somatosensory Amplification Scale, SSDT = Somatic Signal Detection Task, TWSTRS = Toronto Western Spasmodic Torticollis Rating Scale, WGO-IBS = World Gastroenterology Organisation–Irritable Bowel Syndrome Questionnaire, WI = Whiteley Index. a Number of participants included into data analysis. b These numbers were calculated on the basis of data supplied by the authors. c Only tasks/outcomes included in effect size calculation are listed here. d Number of outcomes included into data analysis. e < indicates a more liberal response bias, > a more conservative response bias in the EG compared to the CG. e Refers to the total sample. f Difference between target and actual position.
(DOCX)
(DOCX)
Yes (low risk of bias); no (high risk of bias);? (unclear); NA (not applicable).
(DOCX)
Data Availability Statement
The data that support the findings of this study are openly available in “figshare” at (https://doi.org/10.6084/m9.figshare.8326523.v1).