Abstract
BACKGROUND
As many as one-in-three unintended births occur in Africa. These births have the potential to adversely impact women’s health, but data and design limitations have complicated efforts to understand their consequences. Moreover, there is growing evidence that women often feel happy about an unintended pregnancy and this heterogeneity may be important for identifying the births that are – and those that are not – harmful to women’s health.
OBJECTIVE
To assess whether having an unintended birth precipitates health declines for young women in a high-fertility, high-morbidity context, and whether women’s emotional reaction to the pregnancy foreshadows the consequences of the resulting birth.
METHODS
We use closely spaced panel data from 896 young women in Malawi that include prospective measures of fertility timing desires captured only months before conception and a contemporaneous measure of emotional reaction to the pregnancy. We run lagged dependent variable regression models of self-rated health that account for health and sociodemographic conditions prior to pregnancy and compare women with unintended births to women with intended births and to an alternative comparison group: women who avoid an unintended birth. We then disaggregate unintended births by women’s emotional reaction after learning of the pregnancy.
RESULTS
Women who had an unintended birth but initially had a positive reaction to the pregnancy did not experience a decline in health after birth. Women who had a more negative reaction, however, experienced marked reductions in self-rated health, even years after the birth.
CONTRIBUTION
Our findings highlight meaningful heterogeneity in the consequences of unintended fertility for women’s health and offer insights into the unintended births that put women at greatest risk of health decline.
Keywords: unintended births, fertility, women’s health, panel study, Malawi
INTRODUCTION
Worldwide, 23% of births are estimated to be unintended, either coming when no more children are wanted or sooner than desired (Bearak, Popinchalk, Alkema, and Sedgh 2018). Nearly 90% of such births are to women in low-income regions, with approximately one-in-three occurring in Africa due to high fertility and constraints to family planning (Bearak et al. 2018; United Nations 2019).1 The concentration of unintended births on the continent makes it critically important to understand their impact on health, and on women’s health specifically because so little is known. Most research on the risks of unintended births for women’s health focuses on maternal health in pregnancy and the postpartum period, yet the implications of having an unanticipated child could extend well beyond the postpartum period to scar women’s general physical and mental health even years later (Brittain, Phillips, Zerbe, Abrams, and Myer 2019; Gipson, Koenig, and Hindin 2008; Herd, Higgins, Sicinski, and Merkurieva 2016; Yeatman and Smith‐Greenaway 2018). Serious measurement and design challenges in this area, however, leave open the possibility that identified relationships are driven by retrospective reporting biases rather than true impacts (Gipson et al. 2008).
Furthermore, accumulating research demonstrates that there is heterogeneity in women’s emotional reaction to an unintended pregnancy. Paradoxically, some women immediately report feeling happy about an unintended pregnancy (Aiken, Westhoff, Trussell, and Castaño 2016; Santelli, Lindberg, Orr, Finer, and Speizer 2009). These women may be signaling that they can adapt to this new, unanticipated development, and the resulting birth may have limited adverse consequences for their health. Conversely, women who react negatively to an unintended pregnancy may be those most vulnerable to negative impacts of the birth. Identifying whether—and which—unintended births harm women’s health could inform the development of antenatal and postnatal interventions that identify and support those women at greatest risk of adverse health.
To address these questions, we use novel longitudinal data to assess the health consequences of having an unintended birth for young women in the context of Malawi. Malawi is characterized by high rates of unintended pregnancy and severe restrictions on legal abortion, meaning that relatively lower proportions of unintended pregnancies end in abortion (Bearak et al. 2018; Lavelanet, Schlitt, Johnson, and Ganatra 2018; National Statistical Office (NSO) [Malawi] and ICF 2017).2 Because women face substantial obstacles to terminating unintended pregnancies—even those met with distress and unhappiness—we are able to study whether the health consequences of unintended births vary by women’s initial emotional reactions to the pregnancies. Our data feature information from a population-based sample of women who were interviewed and tested for pregnancy every four months over a period of two and a half years, allowing us to identify pregnancies as intended or unintended based on women’s desires expressed four months prior. Additionally, when women were newly pregnant, they were asked how they felt about the pregnancy, which allows us to incorporate women’s emotional reaction into our analysis of how unintended births influence health. We use these data, along with pre-pregnancy health and sociodemographic traits, to identify the consequences of having an unintended birth on women’s self-rated health three to five years later.
BACKGROUND
Data and Design Challenges for Understanding the Consequences of Unintended Births for Women’s Health
The empirical evidence on the implications of unintended births for women’s health is limited, not just because few studies look beyond the postpartum period, but also because design challenges make the relationships particularly difficult to disentangle when using cross-sectional data (Gipson et al. 2008). One challenge relates to whether observed correlations between unintended births and women’s health reflect real consequences or simply preexisting differences between women who have and do not have unintended births. For example, a study of children’s health in the United Kingdom concluded that “births after unplanned conceptions are mainly a symptom rather than a source of disadvantage” (de la Rochebrochard and Joshi 2013: 910). Some situational factors, such as poverty, may put women at elevated risk of unintended pregnancy and make them more susceptible to poor health (Herd et al. 2016; Ikamari, Izugbara, and Ochako 2013; Kost and Lindberg 2015). Additionally, poor health itself has been shown to predict unintended pregnancy (J. A. Hall et al. 2016; K. S. Hall, Richards, and Harris 2017). Even longitudinal studies tend to lack pre-pregnancy health data (e.g., Herd et al. 2016; Faisal-Cury et al. 2017), which makes it hard to determine whether unintended fertility leads to a decline in women’s health or simply reflects their preexisting poor health.
A second challenge relates to the retrospective reporting of pregnancy desires.3 Survey questions tend to ask women retrospectively, birth-by-birth whether, at the time they became pregnant (often years earlier), they wanted to be pregnant then or at some later time, which researchers use to classify pregnancies – and the resulting births – as intended or unintended (Gipson et al. 2008). Research has shown, however, that intentions measured after birth differ from a mother’s report about the same pregnancy before conceiving or while pregnant (Barber and Gatny 2021; Bishai, Razzaque, Christiansen, Mustafa, and Hindin 2015; Joyce, Kaestner, and Korenman 2000; Koenig, Acharya, Singh, and Roy 2006; Rosenzweig and Wolpin 1993). Ex-post rationalization, recall bias, and social desirability bias may drive mothers to report a pregnancy as intended, regardless of whether it was at the time. Especially concerning for understanding the health implications of unintended fertility is evidence that health outcomes can influence mothers’ retrospective reporting of the intentionality of their pregnancies (Rosenzweig and Wolpin 1993; Smith-Greenaway and Sennott 2016). This evidence opens the door to the possibility that a mother’s own poor health could shape her retrospective reporting of a pregnancy as unintended, driving a spurious correlation.
We address these challenges using panel data that begin prior to conception and include a prospective measure of pregnancy desires, socioeconomic characteristics, and pre-pregnancy health.
Another inherent challenge in research on unintended births stems from identifying the appropriate comparator: to whom do we make comparisons when studying their health consequences? The vast majority of what is known about unintended births comes from comparing women who experienced an unintended birth to women who experienced an intended one. Although such a comparison may be convenient, it may also be inappropriate because these women are fundamentally different in their fertility desires, which likely correspond with other traits. Arguably, the more appropriate counterfactual to women who have an unintended birth is women who similarly wish to avoid having a birth and do not have one.
This is not the first study to take interest in such a comparison. Researchers in the U.S. Turnaway Study (Foster 2021), for example, studied women who share a desire to avoid an unintended birth by comparing women denied an abortion because they exceeded the gestational limit to women who obtained an abortion when just under that limit. Women who had unintended births because they were denied abortion had slightly worse trajectories of self-rated health than women who shared their desire to not have a child and successfully obtained an abortion, but these differences were not always meaningful (Ralph, Mauldon, Biggs, and Foster 2019). Our study takes a complementary approach by comparing women who had an unintended birth to women who also had a prospective interest in not having a birth and never had one.
Finally, research, largely from high-income settings, has argued that not all unintended pregnancies are experienced similarly; instead, some women respond to unintended pregnancies with happiness, others with sadness, and still others with indifference (Carson et al. 2011; Sable and Wilkinson 1998; Santelli et al. 2009). Women’s immediate emotional receptivity to pregnancy – not just whether it is planned – may be relevant to understanding its subsequent implications for women’s health, even years later (Aiken et al. 2016; Blake et al. 2007; Sable and Libbus 2000; Gomez et al. 2019). Women who report that they are pleased with the news of an unintended pregnancy may not be as vulnerable to its health consequences as those who are indifferent to or upset by it, although the nascent evidence is mixed (Baba et al. 2020; Barton, Redshaw, Quigley, and Carson 2017; Blake et al. 2007). We assess whether women’s emotions about their unintended pregnancy soon after learning of it can help identify the unintended births that eventually produce adverse health outcomes.
Unintended Birth and Women’s Health in Malawi
Even as women’s variable reactions toward unintended pregnancies may be salient to understanding their health trajectories, there are reasons to anticipate that any unintended birth could compromise women’s health in Malawi and elsewhere. Unintended pregnancies are often recognized at later gestations (Joyce et al. 2000; Kost and Lindberg 2015), which helps to explain why they are also associated with delayed antenatal care and delivery outside of a health facility, both of which are risk factors for maternal morbidity (Gage 1998; Marston and Cleland 2003; Singh, Chalasani, Koenig, and Mahapatra 2012). Studies from Malawi found that many women anticipated they would experience health problems if they became pregnant sooner than desired, and women who experienced such pregnancies indeed had higher levels of postpartum depression (J. A. Hall et al. 2018; Machiyama et al. 2015). Furthermore, unintended childbearing could set off a cascade of hardships that might precipitate a longer-term decline in health. For example, the cost of caring for a child who was not intended could exacerbate the economic situation of chronically poor households (Devereux, Baulch, Phiri, and Sabates-Wheeler 2006). Greater poverty could prevent women from seeking medical care (Zere, Moeti, Kirigia, Mwase, and Kataika 2007) and harm their physical health through food insecurity (Misselhorn 2005). An unintended pregnancy could push women to drop out of school or hastily marry their partner; it could also create marital stress and dissolution, which in turn could disrupt women’s access to their husbands’ time and resources (Levandowski et al. 2012; Lewinsohn et al. 2018; Smith-Greenaway and Clark 2017). Finally, unintended births to young women frequently occur outside of marriage, which carries stigma and social consequences such as loss of economic and social support that could impact their health (J. A. Hall et al. 2016; Levandowski et al. 2012).
Together, this suggests that relative to women who had no pregnancy, Malawian women who have unintended births will be at risk of worsening health. Even so, evidence of health decline following an unintended birth could stem simply from the risks associated with childbearing in a context of high maternal morbidity. It may be that any additional pregnancy and birth—even if intended—could negatively impact women’s health (Munk-Olsen, Laursen, Pedersen, Mors, and Mortensen 2006; Thompson, Roberts, Currie, and Ellwood 2002). This is especially true in the Malawian context where high-quality obstetric care is not widely available (Kongnyuy, Hofman, Mlava, Mhango, and Van Den Broek 2009). This possibility underscores the value of considering an alternative comparison group. If the health cost associated with unintended birth is due simply to having had a child, there should be few—if any—health consequences of an unintended birth for women relative to those who had an intended birth.
On the other hand, in a pronatal context such as Malawi, many unintended pregnancies may be met with positive emotions, and could potentially confer social and psychological benefits in an environment where motherhood is so highly valued (Yeatman and Trinitapoli 2013; Smith-Greenaway and Yeatman 2020). Few studies have documented women’s emotional responses to unintended pregnancies in sub-Saharan settings, but the limited evidence finds unsurprisingly that many women react to unintended pregnancies with happiness (Choi et al. 2019). These women’s positive emotional reaction to the pregnancy may be a valuable way to identify those pregnancies that women feel they can cope with, and thus that will not be as consequential for their health. In contrast, women who both do not intend to become pregnant and do not feel happy about it once they become pregnant, may be foretelling the challenges that they go on to face. That is, these women may be most likely to face the expected social, economic, and relational consequences of having an unintended birth, which we hypothesize will translate to declines in health over time.
DATA AND METHODS
Data and Sample
We use data from the first two phases of Tsogolo la Thanzi (TLT), a longitudinal study in Malawi conducted between 2009 and 2015 (Yeatman, Chilungo, Lungu, Namadingo, and Trinitapoli 2019). TLT began in 2009 from a simple random sample of women between the ages of 15 and 25 living within a 7-km radius of the center of Balaka, a town and district capital in southern Malawi surrounded by rural villages. The age-restricted sample of young Malawian women living within a single community allows us to hold constant community-level confounders such as access to contraception and the underlying disease burden.
TLT originally enrolled 1,505 women who were followed prospectively over six years. Between 2009 and 2011, respondents were interviewed eight times with each interview spaced four months apart. After a 3.5-year interval, respondents were then re-interviewed in 2015 (N=1,200; 80% retention) when they were between 21 and 31 years old. Female interviewers administered all interviews in Chichewa in private rooms at a central research center.
During each wave of TLT, respondents were asked about fertility timing desires, marital status, socioeconomic conditions, and self-rated health. Women then took a urine hCG pregnancy test. The acceptance rate for tests was 88% with current menstruation the modal reason given for refusals. Self-reported pregnancy and reproductive history data complement the pregnancy test data making it possible for us to identify conceptions and estimate the wave after which they occurred when pregnancy tests were refused. These data allow us to identify pregnancies early and classify them according to women’s timing desires expressed at the preceding wave, an average of approximately two months, and not longer than four months, before a conception could be recognized. Following pregnancy testing, women with new and ongoing pregnancies completed a pregnancy questionnaire that asked when they found out they were pregnant and their emotional reaction at the time.
We limit our analytic sample to the 896 women who either had an unintended birth, an intended birth, or no birth as intended (defined operationally below) and completed a follow-up interview in 2015. Women who were re-interviewed in 2015 (80% of the original sample) did not differ from the wave 1 sample on most sociodemographic traits with the exception of being more likely to have been born locally and to have lower education (Yeatman et al. 2019).4
Dependent Variable
Our analytic goal is to understand whether having an unintended birth from a pregnancy that began between 2009 and 2011 influences women’s health in 2015. To assess this, we use women’s self-rated health in 2015 (three-to-five years after the focal birth) as the dependent variable and employ a modeling strategy that controls for women’s self-rated health at the wave before pregnancy. Self-rated health is a holistic measure of health that correlates with indicators of physical, mental, and functional health and predicts mortality in diverse populations (Idler and Benyamini 1997; Wilson 2001; Singh-Manoux et al. 2006; DeSalvo et al. 2006), including sub-Saharan African settings (Debpuur, Welaga, Wak, and Hodgson 2010), with some evidence that it is a better predictor of mortality than many biomarkers (Goldman, Glei, and Weinstein 2017). In Malawi, self-rated health is positively correlated with literacy, wealth, and completing primary school and negatively correlated with age (Smith-Greenaway 2015).
At each interview, respondents were asked, “In general, would you say your health now is…” and read the response categories, which were as follows: “excellent”, “very good”, “good”, “fair”, or “poor”. Following others (e.g., Zhang et al. 2020; Ralph et al. 2019), we dichotomize self-rated health to focus on those women who report the worst two health outcomes and refer to this group as having “fair or poor self-rated health”. Although this is a relatively rare outcome in our young sample, these women select the responses without positive valences5 suggesting that they perceive their health as being of low quality.
Key Independent Variables
Unintended Birth, Intended Birth, No Birth as Intended
We identify three groups of women that together comprise the analytic sample: women who had an unintended birth from a pregnancy that began between 2009 and 2011 (key group of interest; “unintended birth”; N=297); (2) women who had an intended birth from a pregnancy that began between 2009 and 2011 (standard comparison; “intended birth”; N=181); and (3) women who expressed no intention to become pregnant and who did not become pregnant between 2009 and 2011 (alternative counterfactual; “no birth as intended”; N=418). We restrict our focus to births resulting from incident pregnancies between 2009 and 2011 because these are the only pregnancies on which we have closely spaced prospective fertility timing desires, which are essential given the flexibility of women’s fertility timing desires in the context (Sennott and Yeatman 2012; Trinitapoli and Yeatman 2018). We exclude births for which fertility desires could not be assessed within four months of conception due to missing survey waves (N=14).
At each wave, women were asked, “how long would you like to wait before having your first/next child?” Response categories included “ASAP, “within 2 years”, “2–3 years”, “3–4 years”, “4–5 years”, “5 or more years”, “no preference/whenever”, “don’t want a(nother) child,” and “don’t know”. We use fertility timing desires from the wave before the pregnancy was first identified (see Figure 1) to classify subsequent births as either intended or unintended. We classify births as unintended if, at the wave before the conception occurred, a woman reported that she did not want her next birth for at least 2 years but became pregnant within 4 months. We classify births as intended if a woman became pregnant within four months of reporting wanting a birth ASAP or within the next 2 years.6
Figure 1:

Timeline of Tsogolo la Thanzi and data points used in analysis, 2009–2015
Note: In total, TLT consisted of nine waves of data collection. The first eight waves took place between 2009 and 2011 and were spaced four months apart. The final wave occurred in 2015 after a 3.5-year inter-survey period.
We use these designations to identify groups of women who had an unintended birth or an intended birth.7 We classify women as having no birth as intended if they clearly and consistently (at each point asked between 2009 and 2011) expressed a desire to delay a birth for at least two years, and did not conceive during this period. Women were excluded from this group if they were interviewed fewer than three times between 2009 and 2011. This exclusion criterion made this group more comparable to the group of women with an unintended birth in terms of study participation (see Table 1). Three additional women were excluded from this group because they had tubal ligations.
Table 1:
Baseline sociodemographic characteristics of analytic sample of women enrolled in Tsogolo la Thanzi, by reproductive outcome over study period
| Unintended Birth | Intended Birth | p-value | No Birth as Intended | p-value | |
|---|---|---|---|---|---|
| Fair or poor self-rated health, % | 3.0 | 3.3 | 0.863 | 2.6 | 0.750 |
| Age, mean (SD) | 20.3 (3.3) | 21.4 (2.8) | <0.001 | 19.3 (3.4) | <0.001 |
| Marital status, % | <0.001 | <0.001 | |||
| Married | 48.2 | 74.6 | 29.4 | ||
| Formerly married | 11.1 | 8.3 | 6.9 | ||
| Never married | 40.7 | 17.1 | 63.6 | ||
| Year of education, mean (SD) | 7.4 (2.7) | 6.8 (3.0) | 0.024 | 8.8 (2.8) | <0.001 |
| Enrolled in school, % | 30.6 | 2.2 | <0.001 | 55.7 | <0.001 |
| High SES, % | 17.9 | 14.9 | 0.406 | 35.2 | <0.001 |
| Parity, mean (SD) | 1.1 (1.1) | 1.1 (1.0) | 0.926 | 0.8 (1.1) | <0.001 |
| Nulliparous | 38.0 | 32.0 | 0.185 | 57.7 | <0.001 |
| Baseline wave, mean (SD) | 4.0 (1.9) | 3.7 (1.9) | 0.041 | 3.8 (1.9) | 0.135 |
| Total interviews (max=9), mean (SD) | 8.8 (0.7) | 8.7 (0.8) | 0.205 | 8.5 (1.3) | <0.001 |
| N | 297 | 181 | 418 |
Note: Significance tests are t-tests or chi-squared tests relative to the unintended birth group.
Emotional Response to Unintended Pregnancy
To test for variation in the health implications of an unintended birth, we measure how women reacted to learning of the focal pregnancy. Pregnant women were asked a questionnaire following pregnancy testing. This short questionnaire asked women, “When you first found out about this pregnancy, how did you take the news?” Response categories included “very good”, “good”, “neither good nor bad”, “bad” and “very bad”. One hundred and forty-one women, just under half of those with unintended births, first learned of their pregnancy through testing at the TLT research center and thus answered the question at the time they learned of their pregnancy. The other half of women who knew or suspected they were pregnant before the interview, answered this question retrospectively but within a few weeks of learning of their pregnancy. We found no evidence that women’s emotional reactions to pregnancy differed according to whether they had just found out versus reported having known of their pregnancy prior to the survey. We disaggregate unintended births according to whether the woman reported that the pregnancy was very good/good news (“positive reaction”) versus those that did not (“negative reaction”).8 Two women are missing pregnancy questionnaires and thus data on their emotional reactions to their unintended pregnancy. We exclude them from the emotion analysis but rerun all models with these women in each category. The results were not sensitive to the inclusion or categorization of these women.
Statistical Analysis and Control Variables
We begin by describing the pre-pregnancy contextual and sociodemographic characteristics of women in each of the three analytic groups (i.e., unintended birth, intended birth, no birth as intended). For women who have no birth as intended, there is no clear “pre-pregnancy” wave. Thus, for this group we measure their sociodemographic characteristics at a randomly selected wave following the distribution of pre-pregnancy waves for women in the other groups (see Table 1).9 Hereafter, we use the term “baseline” to refer to the pre-pregnancy wave for women with unintended or intended births and to the randomly allocated wave for women with no birth as intended.
We then estimate lagged dependent variable regression models that control for baseline self-rated health to examine whether the health of women with unintended births differs in 2015 relative to women with intended births and to women with no birth as intended. These models allow us to identify differences in health net of prior health.
Because fair or poor self-rated health is rare among our young sample of women, we adopt a penalized likelihood estimation method (Firth 1993; Heinze and Schemper 2002) and use the Firth logistic regression (firthlogit in Stata). This adjustment reduces bias that can occur due to small cell sizes by penalizing the likelihood and allowing convergence to finite estimates.
In addition to accounting for baseline self-rated health, models include control variables also measured at baseline, the same wave as the fertility desires used to classify births.10 Models control for age, years of education, current school enrollment, relative affluence (top quartile of sample socioeconomic status estimated using a principal components analysis of structural assets and durable household goods) (see Bachan 2014 for details), marital status (married, never married, formerly married), and parity.
Finally, to test whether the impact of an unintended birth varies by women’s emotional response to the pregnancy, we disaggregate women with an unintended birth by their initial reaction to the pregnancy. We re-estimate lagged dependent variable Firth logistic regression models that compare women who had an unintended birth towards which they had a positive reaction and women who had an unintended birth towards which they had a negative reaction to women who had an intended birth, and then separately to women who had no birth as intended.
RESULTS
Of the 897 women in our analytic sample, 297 (33%) had a birth resulting from an unintended pregnancy that occurred between waves 1 and 8 (2009–2011), 181 women (20%) only had births resulting from intended pregnancies, and 418 women (47%) had no birth as intended during the same period. Table 1 shows how these women differ demographically at baseline. Notably, women with intended births and no birth as intended are the least similar; women who had unintended births fall demographically in-between these women. Women who subsequently have an intended birth are older, more likely to be married, less educated, and less likely to be enrolled in school than women who go on to have an unintended birth. In contrast, women who had no birth as intended are younger, less likely to be married, more educated, more likely to be in school, of higher SES, and less likely to already be mothers.
Among women who had an unintended birth, Table 2 shows that 44% had a positive reaction (N=130) and 56% had a negative reaction (N=165) to their unintended pregnancies. These women have similar profiles before their pregnancies: they are alike in age, marital status, years of education, parity, and socioeconomic status. Women who have a negative emotional reaction to their unintended pregnancy, however, are more likely to be in school at baseline. Given that pregnancy in this context disrupts school attendance and is socially stigmatized, it is unsurprising that these women have negative reactions to these births. Additionally, these women are almost twice as likely as women with positive reactions to want to delay their next birth for at least five years (27% vs. 14%), suggesting that these births are occurring far earlier than women planned.
Table 2:
Baseline sociodemographic characteristics of women enrolled in Tsogolo la Thanzi who later had an unintended birth, disaggregated by their emotional reaction to the pregnancy
| Unintended Birth | |||
|---|---|---|---|
| Positive reaction | Negative reaction | p-value | |
| Fair or poor self-rated health, % | 2.3 | 3.6 | 0.512 |
| Age, mean (SD) | 20.6 (2.9) | 20.1 (3.5) | 0.170 |
| Marital status, % | 0.293 | ||
| Married | 53.1 | 44.9 | |
| Formerly married | 11.5 | 10.9 | |
| Never married | 35.4 | 44.2 | |
| Year of education, mean (SD) | 7.3 (3.0) | 7.5 (2.5) | 0.609 |
| Enrolled in school, % | 22.3 | 37.0 | 0.007 |
| High SES, % | 20.0 | 15.8 | 0.342 |
| Parity, mean (SD) | 1.1 (1.0) | 1.1 (1.1) | 0.786 |
| Nulliparous | 33.9 | 40.6 | 0.234 |
| Baseline wave, mean (SD) | 4.1 (1.9) | 4.0 (1.9) | 0.680 |
| Learned of pregnancy at TLT | 45.4 | 49.7 | 0.462 |
| Wanted to wait 5+ years to have a(nother) child | 13.9 | 26.7 | 0.007 |
| Percent of unintended births | 44.1 | 55.9 | |
| N | 130 | 165 | |
Note: Two women with unintended births were excluded for lacking data on emotional reaction. Significance tests are t-tests or chi-squared tests.
Figure 2 illustrates the trajectories of fair or poor self-rated health for each group of women between baseline and 2015 without adjusting for their compositional differences. In general, it is uncommon for young women in the sample to report fair or poor self-rated health. At their baseline wave, women who subsequently have an intended birth, an unintended birth, or no birth as intended report similar levels of fair or poor self-rated health. Over the study period, however, the prevalence of fair or poor self-rated health among all three subgroups increases, although the increase is largest among women who experience an unintended birth (3.0% to 7.7%). Women with intended births have more modest increases in fair or poor self-rated health and women with no birth as intended experience the smallest change over time.
Figure 2:

Percent of women in fair or poor self-rated health by subgroup over time, 2009–2015
Note: “Pre-pregnancy” data for women in the no birth as intended group came from a randomly assigned wave between 2009–2011. “After birth” refers to the 2015 TLT survey wave for all respondents.
Table 3 presents the Firth logistic regression model results of the relationship between having an unintended birth and fair or poor self-rated health in 2015 net of baseline fair or poor self-rated health. The first two models compare women who had an unintended birth to women who had an intended birth (comparison group A). The second two models compare women who had an unintended birth to those who had no birth as intended (comparison group B). In the models that only include a lagged measure of self-rated health (models A1 and B1), women who had an unintended birth do not differ from women who had an intended birth (OR: 1.278, 95% CI: 0.615, 2.657), but have somewhat elevated odds of fair or poor self-rated health than women who had no birth as intended (OR: 1.842, 95% CI: 0.982, 3.453). When baseline controls are in the models (models A2 and B2), the odds ratios for fair or poor self-rated health among women who had an unintended birth are indistinguishable from both women who had an intended birth (OR: 1.554, 95% CI: 0.697, 3.462) and women who had no birth as intended (OR: 1.531, 95% CI: 0.784, 2.988).11
Table 3:
Firth logistic regression model results of fair or poor self-rated health associated with having an unintended birth using two comparison groups
| Comparison Group A: Intended Birth | Comparison Group B: No Birth as Intended | |||
|---|---|---|---|---|
| Model | A1 | A2 | B1 | B2 |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Unintended birth | 1.278 (0.615, 2.657) | 1.554 (0.697, 3.462) | 1.842 (0.982, 3.453) | 1.531 (0.784, 2.988) |
| Baseline controls | ||||
| Fair or poor self-rated health | 3.853 (1.117, 13.289) | 2.571 (0.687, 9.616) | 3.356 (1.012, 11.128) | 2.288 (0.656, 7.977) |
| Age | 1.043 (0.873, 1.245) | 1.056 (0.886, 1.259) | ||
| Marital status (ref: married) | ||||
| Formerly married | 2.884 (1.211, 6.870) | 3.263 (1.426, 7.467) | ||
| Never married | 0.464 (0.114, 1.885) | 0.932 (0.238, 3.654) | ||
| Years of education | 0.959 (0.829, 1.111) | 0.987 (0.856, 1.137) | ||
| Enrolled in school | 1.153 (0.276, 4.824) | 1.497 (0.445, 5.033) | ||
| High SES | 0.219 (0.041, 1.180) | 0.563 (0.224, 1.428) | ||
| Parity | 0.738 (0.420, 1.295) | 1.162 (0.673, 2.002) | ||
| N | 478 | 478 | 715 | 715 |
These models, however, treat unintended births uniformly, concealing differences in how these women reacted to the pregnancy. Figure 3 replicates the descriptive data presented in Figure 2 but separates women with an unintended birth based on their initial reaction to the unintended pregnancy. Here, we see that being in fair or poor self-rated health is rare for both sets of women at their baseline wave. Over the study period, the prevalence of fair or poor self-rated health for women who felt positive about their unintended pregnancy is similar in slope to women who had an intended birth and to women who had no birth as intended. In other words, over the intervening six years, there is only a relatively modest increase in the prevalence of fair or poor self-rated health for these three groups of women. In contrast, the prevalence of fair or poor self-rated health increases steeply (from 3.6% to 10.9%) among women who have a birth from an unintended pregnancy towards which they reacted negatively.
Figure 3:
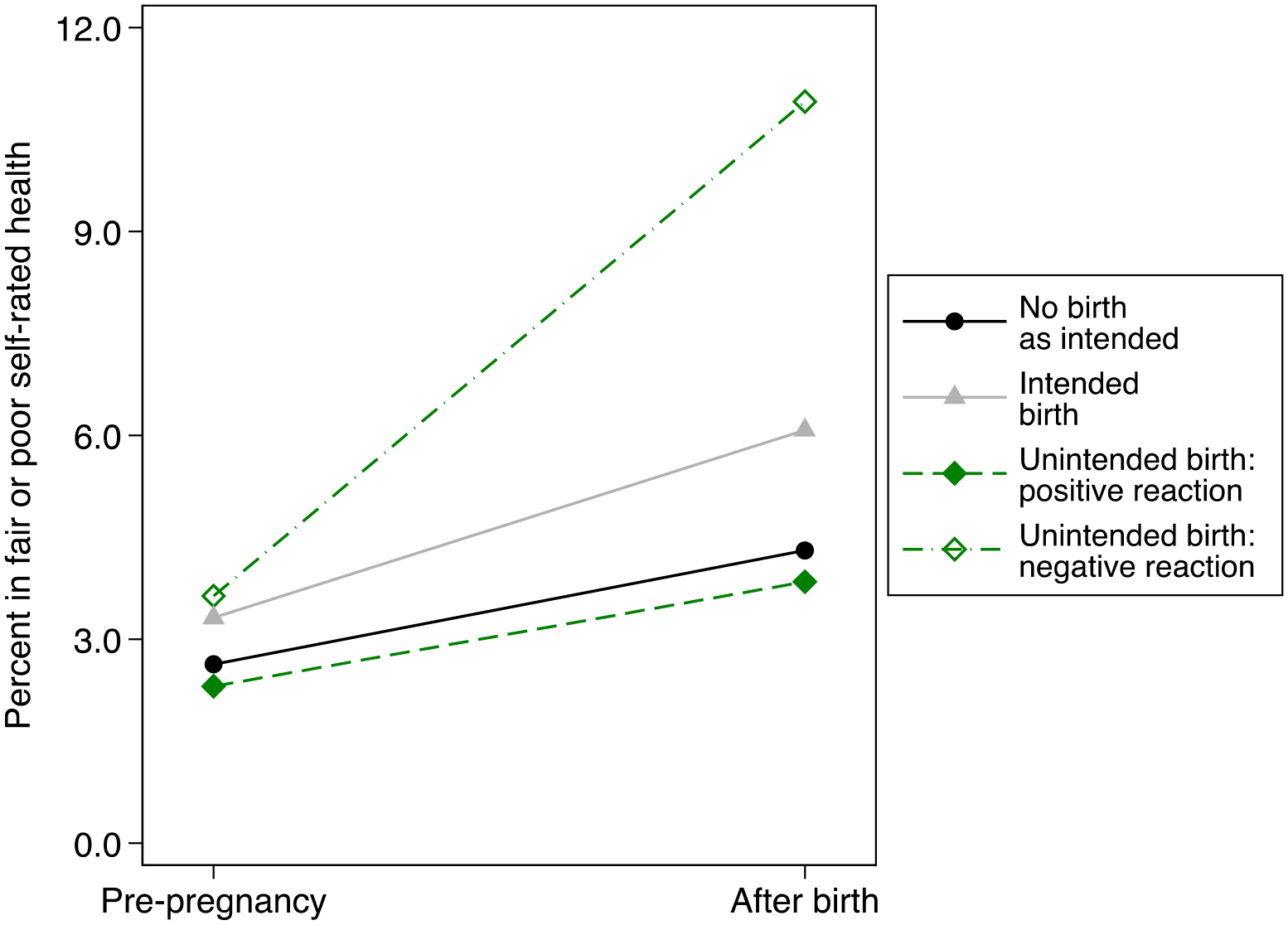
Percent of women in fair or poor self-rated health over time disaggregated by emotional reaction to unintended pregnancy, 2009–2015
Note: “Pre-pregnancy” data for women in the no birth as intended group came from a randomly assigned wave between 2009–2011. “After birth” refers to the 2015 TLT survey wave for all respondents.
Table 4 presents the lagged dependent variable model results wherein we disaggregate women who had unintended births by their earlier emotional reaction to the pregnancy. The results show a clear divergence in the health implications of an unintended birth for women who had a positive versus a negative reaction to their unintended pregnancies. In the model with baseline controls (model A4), women who felt negative about their unintended pregnancy have twice the odds (OR: 2.503, 95% CI: 1.045, 5.996) of being in fair or poor self-rated health relative to women who had an intended birth. Women who had a positive reaction to their unintended pregnancy do not differ from women with an intended birth in their odds of having fair or poor self-rated health (OR: 0.821, 95% CI: 0.281, 2.400). Similarly, as shown in model B4, women with a negative reaction to their unintended pregnancy have twice the odds of being in fair or poor self-rated health relative to women who had no birth as intended (OR: 2.141, 95% CI: 1.060, 4.326). Yet, women with a positive reaction to their unintended pregnancy do not differ in their odds of fair or poor self-rated health (OR: 0.786, 95% CI: 0.284, 2.173).
Table 4:
Firth logistic regression model results of fair or poor self-rated health associated with having an unintended birth that was met with a positive or negative reaction using two comparison groups
| Comparison Group A: Intended Birth | Comparison Group B: No Birth as Intended | |||
|---|---|---|---|---|
| Model | A3 | A4 | B3 | B4 |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Unintended birth | ||||
| Positive reaction | 0.662 (0.233, 1.877) | 0.821 (0.281, 2.400) | 0.953 (0.360, 2.522) | 0.786 (0.284, 2.173) |
| Negative reaction | 1.852 (0.858, 3.998) | 2.503 (1.045, 5.996) | 2.675 (1.366, 5.239) | 2.141 (1.060, 4.326) |
| Baseline controls | ||||
| Fair or poor self-rated health | 3.630 (1.038, 12.703) | 2.211 (0.567, 8.613) | 3.179 (0.946, 10.684) | 2.108 (0.587, 7.573) |
| Age | 1.055 (0.883, 1.260) | 1.066 (0.894, 1.271) | ||
| Marital status (ref: married) | ||||
| Formerly married | 2.820 (1.166, 6.824) | 3.135 (1.359, 7.232) | ||
| Never married | 0.450 (0.111, 1.831) | 0.897 (0.229, 3.506) | ||
| Years of education | 0.958 (0.826, 1.112) | 0.983 (0.851, 1.135) | ||
| Enrolled in school | 0.908 (0.214, 3.856) | 1.303 (0.388, 4.372) | ||
| High SES | 0.223 (0.043, 1.273) | 0.576 (0.227, 1.460) | ||
| Parity | 0.685 (0.388, 1.209) | 1.069 (0.617, 1.851) | ||
| N | 476 | 476 | 713 | 713 |
DISCUSSION
Our study advances understanding of the consequences of unintended births for women’s health by using longitudinal data with a rare set of characteristics that help address many of the design challenges in this research area. We use prospective fertility desires measured within months of conception and incorporate pre-pregnancy measures of women’s health into our analysis to identify whether women’s health worsens following an unintended birth.
We find that unintended births in Malawi correspond with substantial declines in self-rated health for some, but not all, women. The detrimental health impacts are concentrated among the women who expressed immediate, negative feelings about their unintended pregnancy. In contrast, women who had a positive reaction to their unintended pregnancy are buffered from health declines after giving birth. Importantly, the health costs associated with those unintended births that are met with negative reactions are evident regardless of whether we compare women with unintended births to women with intended births, the traditional comparator, or to women also at risk of an unintended birth but who avoided having one. These findings make clear that health declines are not simply due to having a birth, or even to having an unintended birth necessarily, but rather to having particular unintended births.
What explains the prescience of women’s initial, emotional reaction to an unintended pregnancy? That a single measure of women’s emotional posture when first having learned of the pregnancy is indicative of its health consequences multiple years later attests to the importance of extending beyond a focus on timing preferences alone, to consider women’s general disposition toward a pregnancy (Gomez et al. 2019; Aiken et al. 2016). Although it is possible that a positive reaction to an unintended pregnancy could be driven principally by unmeasured personality traits that aid women in being resilient and adaptable, we suspect that it is a much more comprehensive proxy of whether women anticipate their social, economic, and marital circumstances can cope with an unintended birth. The sociodemographic traits of women who responded to their unintended pregnancies with different emotions are broadly similar. Nonetheless, their differences may allude to the underlying processes that we suspect explain their divergent reactions and ultimately their varied health outcomes. For instance, women with negative or neutral responses were more likely to be in school. In Malawi, pregnancy is grounds for school expulsion, meaning that a birth would curtail a woman’s education, forcing her to put her school aspirations, and possibly other aspirations, aside. Additionally, these women were more likely to express not wanting a child for several years, further suggesting that women’s adverse reactions help to identify the births that are most disruptive and stress-inducing.
Regardless of the precise explanations, however, the results confirm that a woman’s feelings about her unintended pregnancy is a harbinger of its future health consequences. Fertility research should continue to expand beyond a narrow focus on intentions to better incorporate women’s emotional reactions to their unintended pregnancies and to consider whether the consequences extend to children in addition to the women who have them.
Despite its many strengths, our study has limitations. First, although TLT took great effort to measure every pregnancy at closely spaced intervals (i.e., pregnancy testing, closely spaced waves, self-reported measures of miscarriage and abortion), some pregnancies, including those ending in abortion, may be missed. Because our central focus is the impact of an unintended birth, this mainly introduces heterogeneity to our alternative comparison group of women who had no birth as intended. That is, despite our repeated confirmation of negative pregnancy tests among these women at four-month intervals, it is possible that some could have had an unintended pregnancy during the study period that was not identified (but nonetheless avoided an unintended birth). The potential that some women in this group had an unintended pregnancy is likely to make our estimate of the impact of an unintended birth conservative given the risks associated with the mostly unsafe abortions in the context (Polis et al. 2017).
Another limitation is our reliance on a single, self-rated measure of health. Even as this indicator is frequently used in population health studies and has been shown to be predictive of adverse health outcomes relative to biomarkers (Goldman, Glei, and Weinstein 2017), its holistic nature makes it difficult to ascertain the nature of the health decline we identify. Is lower self-rated health principally reflecting the presence of physical health problems or women’s worse psychological wellbeing? Although this global measure disallows us from identifying the specific source of women’s poor health, in a population sample of young women many of whom do not access routine medical care it is difficult to imagine a superior, validated measure. Indeed, we are encouraged by the recent inclusion of a measure of self-rated health in the Demographic and Health Surveys Phase VIII. This inclusion recognizes that women’s general health is deserving of greater understanding and will allow research to link women’s reproductive experiences to their health with nationally representative cross-sectional data.
The focus on young women could also be viewed as a limitation. The vast majority of young women in our study expressed a desire for (more) children eventually, suggesting that most of the unintended births we study could be more aptly described as ‘mistimed’ births. It is possible that these births are less disruptive to women’s lives and health relative to unintended births to older women who planned to stop childbearing. Older women may also experience more dramatic health reductions resulting from an additional birth—particularly those they know they cannot handle—than the still notable declines that we observe here. Even as the youthful nature of our sample could produce more conservative results, our findings emphasize the need to understand how unintended births reroute young women’s lives and lead to longer-term disadvantage. For these young women, many of the births that occurred earlier than desired were met with adverse reactions and eventual health decline.
Finally, while our intensive study design with closely spaced panels and pregnancy testing is a major study strength, it comes with the limitation of being singularly focused on a small geographic area. As a result, our findings are specific to this community in Malawi. Despite the unique characteristics of our data and context, however, we anticipate that our broader framework on the role of emotions in buffering the impact of an unintended birth will apply elsewhere.
Unintended fertility is common and will continue to be so. Our study shows that many unintended births are detrimental to women’s health, particularly those that elicit negative feelings. Health care providers should consider women’s emotional reaction to their pregnancies as a tool for identifying the women at greatest risk for poor outcomes, and thus most in need of antenatal, postnatal, and childrearing support. Nonetheless, it is encouraging that almost half of the unintended pregnancies resulting in births in our sample were met with happiness. In contexts where women have access to safe abortion, the percent of unintended births that are met with positive emotions is likely to be even higher. Broadening access to safe abortion care in Malawi and across sub-Saharan Africa will afford women the agency to avoid unintended births that they can so presciently identify will be harmful to their wellbeing.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R03-HD097360) and by the NICHD-funded University of Colorado Population Center (P2C HD066613). Tsogolo la Thanzi is a research project designed by Jenny Trinitapoli and Sara Yeatman and funded by grants R01-HD058366, R01-HD077873, and R03-HD095690 from NICHD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank Stephanie Chamberlin for excellent research assistance.
Footnotes
Authors’ calculation based on estimates in Bearak et al. 2018 on percent of births unintended and UN estimates of live births by region.
As in most sub-Saharan African countries, abortion is illegal in Malawi except to save the life of the mother. Abortions occur (Polis et al. 2017) but to a lesser extent than in political-historical contexts with more liberal abortion access (see also Herd et al. 2016). For example, Polis et al. 2017 estimate that 30% of unintended pregnancies in Malawi end in abortion as compared to 61% worldwide (Bearak et al. 2020).
Like most research on unintended fertility, we measure women’s fertility desires rather than intentions. Although a minority of surveys measure intentions, most (e.g., NSFG, DHS, PRAMS) more accurately measure desires (e.g., “did you yourself want to have a(nother) baby?”; “how long would you like to wait before the birth of a(nother) child”?). Researchers have long recognized the overlap in these terms, particularly from the perspective of respondents and after translation (Kodzi, Johnson, and Casterline, 2010). Nonetheless, we clarify our reliance on questions about women’s desires when describing our operationalization but use the dominant language of “intended” and “unintended” when characterizing births and discussing the literature.
The analytic sample excludes three women who would have otherwise met the sample inclusion criteria but died prior to 2015. Two of these women had intended births and one had an unintended birth. The findings were not sensitive to the exclusion of these women. Other sample exclusion criteria are described under key independent variables.
The Chichewa word used for fair, choncho, has a negative connotation.
Because relatively few women in our young sample reported not wanting a(nother) child, we do not differentiate between “mistimed” versus “unwanted” births. Eleven women with unintended births reported not wanting a(nother) birth the wave before conception. Additionally, one woman reported “no preference/whenever” the wave before conception and was coded as having an intended birth.
It is rare but possible for women to have two incident pregnancies between 2009 and 2011 that both resulted in live births. Because our conceptual framework focuses on the consequences of an unintended birth, we follow previous studies (e.g., Herd et al. 2016) and group the eight women who had both an intended and an unintended birth in the unintended birth category.
Our conceptual framework leads us to focus exclusively on the emotional reaction of women with births from unintended pregnancies; however, some women with intended births report negative emotional reactions to their pregnancies as has been found elsewhere (Blake et al. 2007). Seventy-six percent of women with intended births reported a good or very good reaction to learning of their pregnancy in comparison to 44% of women with unintended births.
As a sensitivity test, we reran all analyses using wave 1 as the baseline for measures of self-rated health and control variables (however, we still relied on the wave prior to conception for women’s fertility desires). The results were consistent (see Supplementary Table 1).
We do not include covariates measured in 2015 in the models because of the potential for these variables to be on the causal pathway. That is, an unintended birth might lead to health decline by precipitating changes in relationships or economic circumstances. Although understanding the mechanisms through which unintended fertility might impact health is important, it is beyond the scope of the present study, and we maintain our focus on identifying the presence of any health impacts and whether they vary by emotional reaction.
As a sensitivity test, we reran the models using the full sample (N=896) and a categorical variable for the subgroups of women. The results were consistent (see Supplementary Table 2).
DATA AVAILABILITY
This research uses data from Tsogolo la Thanzi. Study instruments are available at https://tsogololathanzi.uchicago.edu/ and the data are available through restricted data user agreements managed by Data Sharing for Demographic Research (DSDR) at the University of Michigan.
REFERENCES
- Aiken AR, Westhoff CL, Trussell J, and Castaño PM (2016). Comparison of a timing‐based measure of unintended pregnancy and the London Measure of Unplanned Pregnancy. Perspectives on Sexual and Reproductive Health 48(3): 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baba S, Kimura T, Ikehara S, Honjo K, Eshak ES, Sato T, and Iso H (2020). Impact of intention and feeling toward being pregnant on postpartum depression: the Japan Environment and Children’s Study (JECS). Archives of Women’s Mental Health 23(1): 131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachan LK (2014). Anticipatory child fostering and household economic security in Malawi. Demographic Research 30: 1157–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber J, and Gatny H (2021). The social context of retrospective-prospective changes in pregnancy desire during the transition to adulthood: The role of fathers and intimate relationships. Demographic Research 44: 899–940. [Google Scholar]
- Barton K, Redshaw M, Quigley MA, and Carson C (2017). Unplanned pregnancy and subsequent psychological distress in partnered women: a cross-sectional study of the role of relationship quality and wider social support. BMC Pregnancy and Childbirth 17(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearak J, Popinchalk A, Ganatra B, Moller A-B, Tunçalp Ö, Beavin C, … Alkema L (2020). Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. The Lancet Global Health 8(9): e1152–e1161. [DOI] [PubMed] [Google Scholar]
- Bearak J, Popinchalk A, Alkema L, and Sedgh G (2018). Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. The Lancet Global Health 6(4): e380–e389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishai D, Razzaque A, Christiansen S, Mustafa AG, and Hindin M (2015). Selection bias in the link between child wantedness and child survival: Theory and data from Matlab, Bangladesh. Demography 52(1): 61–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake SM, Kiely M, Gard CC, El‐Mohandes AA, El‐Khorazaty MN, and Initiative ND (2007). Pregnancy intentions and happiness among pregnant black women at high risk for adverse infant health outcomes. Perspectives on Sexual and Reproductive Health 39(4): 194–205. [DOI] [PubMed] [Google Scholar]
- Brittain K, Phillips TK, Zerbe A, Abrams EJ, and Myer L (2019). Long-term effects of unintended pregnancy on antiretroviral therapy outcomes among South African women living with HIV. AIDS 33(5): 885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson C, Kelly Y, Kurinczuk JJ, Sacker A, Redshaw M, and Quigley MA (2011). Effect of pregnancy planning and fertility treatment on cognitive outcomes in children at ages 3 and 5: longitudinal cohort study. BMJ 343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KW, Smit JA, Coleman JN, Mosery N, Bangsberg DR, Safren SA, and Psaros C (2019). Mapping a syndemic of psychosocial risks during pregnancy using network analysis. International Journal of Behavioral Medicine 26(2): 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de La Rochebrochard E, and Joshi H (2013). Children born after unplanned pregnancies and cognitive development at 3 years: social differentials in the United Kingdom Millennium Cohort. American Journal of Epidemiology 178(6): 910–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debpuur C, Welaga P, Wak G, and Hodgson A (2010). Self-reported health and functional limitations among older people in the Kassena-Nankana District, Ghana. Global Health Action 3(1): 2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, and Muntner P (2006). Mortality prediction with a single general self-rated health question. Journal of General Internal Medicine 21(3): 267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devereux S, Baulch B, Phiri A, and Sabates-Wheeler R (2006). Vulnerability to chronic poverty and malnutrition in Malawi. Lilongwe, Malawi: DFID Malawi. [Google Scholar]
- Faisal-Cury A, Menezes PR, Quayle J, and Matijasevich A (2017). Unplanned pregnancy and risk of maternal depression: secondary data analysis from a prospective pregnancy cohort. Psychology, Health and Medicine 22(1): 65–74. [DOI] [PubMed] [Google Scholar]
- Firth D (1993). Bias reduction of maximum likelihood estimates. Biometrika 80(1): 27–38. [Google Scholar]
- Foster DG (2021). The Turnaway Study: Ten years, a thousand women, and the consequences of having—or being denied—an abortion. Simon and Schuster. [Google Scholar]
- Gage AJ (1998). Premarital childbearing, unwanted fertility and maternity care in Kenya and Namibia. Population Studies 52(1): 21–34. [Google Scholar]
- Gipson J, Koenig M, and Hindin M (2008). The effects of unintended pregnancy on infant, child, and parental health: A review of the literature. Studies in Family Planning 39(1): 18–38. [DOI] [PubMed] [Google Scholar]
- Goldman N, Glei DA, and Weinstein M (2017). The best predictors of survival: Do they vary by age, sex, and race? Population and Development Review 43(3): 541–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez AM, Arteaga S, Villaseñor E, Arcara J, and Freihart B (2019). The misclassification of ambivalence in pregnancy intentions: a mixed‐methods analysis. Perspectives on Sexual and Reproductive Health 51(1): 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JA, Barrett G, Copas A, Phiri T, Malata A, and Stephenson J (2018). Reassessing pregnancy intention and its relation to maternal, perinatal and neonatal outcomes in a low-income setting: A cohort study. PLOS ONE 13(10): e0205487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JA, Barrett G, Phiri T, Copas A, Malata A, and Stephenson J (2016). Prevalence and determinants of unintended pregnancy in Mchinji District, Malawi; using a conceptual hierarchy to inform analysis. PLOS ONE 11(10): e0165621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Richards JL, and Harris KM (2017). Social disparities in the relationship between depression and unintended pregnancy during adolescence and young adulthood. Journal of Adolescent Health 60(6): 688–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze G, and Schemper M (2002). A solution to the problem of separation in logistic regression. Statistics in Medicine 21(16): 2409–2419. [DOI] [PubMed] [Google Scholar]
- Herd P, Higgins J, Sicinski K, and Merkurieva I (2016). The implications of unintended pregnancies for mental health in later life. American Journal of Public Health 106(3): 421–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, and Benyamini Y (1997). Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior: 21–37. [PubMed] [Google Scholar]
- Ikamari L, Izugbara C, and Ochako R (2013). Prevalence and determinants of unintended pregnancy among women in Nairobi, Kenya. BMC Pregnancy and Childbirth 13(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce T, Kaestner R, and Korenman S (2000). The stability of pregnancy intentions and pregnancy-related maternal behaviors. Maternal and Child Health Journal 4(3): 171–178. [DOI] [PubMed] [Google Scholar]
- Kodzi IA, Johnson DR, and Casterline JB (2010). Examining the predictive value of fertility preferences among Ghanaian women. Demographic Research 22: 965–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig MA, Acharya R, Singh S, and Roy TK (2006). Do current measurement approaches underestimate levels of unwanted childbearing? Evidence from rural India. Population Studies 60(3): 243–256. [DOI] [PubMed] [Google Scholar]
- Kongnyuy EJ, Hofman J, Mlava G, Mhango C, and Van Den Broek N (2009). Availability, utilisation and quality of basic and comprehensive emergency obstetric care services in Malawi. Maternal and Child Health Journal 13(5): 687–694. [DOI] [PubMed] [Google Scholar]
- Kost K, and Lindberg L (2015). Pregnancy intentions, maternal behaviors, and infant health: Investigating relationships with new measures and propensity score analysis. Demography 52(1): 83–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavelanet AF, Schlitt S, Johnson BR, and Ganatra B (2018). Global abortion policies database: A descriptive analysis of the legal categories of lawful abortion. BMC International Health and Human Rights 18(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levandowski BA, Kalilani‐Phiri L, Kachale F, Awah P, Kangaude G, and Mhango C (2012). Investigating social consequences of unwanted pregnancy and unsafe abortion in Malawi: The role of stigma. International Journal of Gynecology and Obstetrics 118: S167–S171. [DOI] [PubMed] [Google Scholar]
- Lewinsohn R, Crankshaw T, Tomlinson M, Gibbs A, Butler L, and Smit J (2018). “This baby came up and then he said,“I give up!”: The interplay between unintended pregnancy, sexual partnership dynamics and social support and the impact on women’s well-being in KwaZulu-Natal, South Africa. Midwifery 62: 29–35. [DOI] [PubMed] [Google Scholar]
- Machiyama K, Baschieri A, Dube A, Crampin AC, Glynn JR, French N, and Cleland J (2015). An assessment of childbearing preferences in northern Malawi. Studies in Family Planning 46(2): 161–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marston C, and Cleland J (2003). Do unintended pregnancies carried to term lead to adverse outcomes for mother and child? An assessment in five developing countries. Population Studies 57(1): 77–93. [DOI] [PubMed] [Google Scholar]
- Misselhorn AA (2005). What drives food insecurity in southern Africa? A meta-analysis of household economy studies. Global Environmental Change: 15(1): 33–43. [Google Scholar]
- Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, and Mortensen PB (2006). New parents and mental disorders: a population-based register study. JAMA 296(21): 2582–2589. [DOI] [PubMed] [Google Scholar]
- National Statistical Office (NSO) [Malawi] and ICF (2017). Malawi demographic and health survey 2015–2016. Zomba, Malawi and Rockville, Maryland, USA: NSO and ICF. [Google Scholar]
- Polis CB, Mhango C, Philbin J, Chimwaza W, Chipeta E, and Msusa A (2017). Incidence of induced abortion in Malawi, 2015. PLOS ONE 12(4): e0173639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralph LJ, Mauldon J, Biggs MA, and Foster DG (2019). A prospective cohort study of the effect of receiving versus being denied an abortion on educational attainment. Women’s Health Issues 29(6): 455–464. [DOI] [PubMed] [Google Scholar]
- Rosenzweig MR, and Wolpin KI (1993). Maternal expectations and ex post rationalizations: The usefulness of survey information on the wantedness of children. Journal of Human Resources 28(2): 205–229. [Google Scholar]
- Sable MR, and Libbus MK (2000). Pregnancy intention and pregnancy happiness: Are they different? Maternal and Child Health Journal 4(3): 191–196. [DOI] [PubMed] [Google Scholar]
- Sable MR, and Wilkinson DS (1998). Pregnancy intentions, pregnancy attitudes, and the use of prenatal care in Missouri. Maternal and Child Health Journal 2(3): 155–165. [DOI] [PubMed] [Google Scholar]
- Santelli JS, Lindberg LD, Orr MG, Finer LB, and Speizer I (2009). Towards a multidimensional measure of pregnancy intentions: Evidence from the United States. Studies in Family Planning 40(2): 87–100. [DOI] [PubMed] [Google Scholar]
- Sennott C, and Yeatman S (2012). Stability and change in fertility preferences among young women in Malawi. International Perspectives on Sexual and Reproductive Health 38(1): 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A, Chalasani S, Koenig MA, and Mahapatra B (2012). The consequences of unintended births for maternal and child health in India. Population Studies 66(3): 223–239. [DOI] [PubMed] [Google Scholar]
- Smith-Greenaway E, and Yeatman S (2020). Unrealized educational expectations and mental health: Evidence from a low-income country. Social Forces 98(3): 1112–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Greenaway E, and Clark S (2017). Variation in the link between parental divorce and children’s health disadvantage in low and high divorce settings. SSM-Population Health 3: 473–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Greenaway E, and Sennott C (2016). Death and desirability: retrospective reporting of unintended pregnancy after a child’s death. Demography 53(3): 805–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Greenaway E (2015). Are literacy skills associated with young adults’ health in Africa? Evidence from Malawi. Social Science and Medicine 127: 124–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JF, Roberts CL, Currie M, and Ellwood DA (2002). Prevalence and persistence of health problems after childbirth: Associations with parity and method of birth. Birth 29(2): 83–94. [DOI] [PubMed] [Google Scholar]
- Trinitapoli J, and Yeatman S (2018). The flexibility of fertility preferences in a context of uncertainty. Population and Development Review 44(1): 87–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. (2019). World Population Prospects. New York, NY: United Nations. https://population.un.org/wpp/. Accessed January 15, 2021. [Google Scholar]
- Wilson SE (2001). Socioeconomic status and the prevalence of health problems among married couples in late midlife. American Journal of Public Health 91(1): 131–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman S, Chilungo A, Lungu S, Namadingo H, and Trinitapoli J (2019). Tsogolo la Thanzi: A longitudinal study of young adults living in Malawi’s HIV epidemic. Studies in Family Planning 50(1): 71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman S, and Smith‐Greenaway E (2018). Birth Planning and Women’s and Men’s Health in Malawi. Studies in Family Planning 49(3): 213–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman S, and Trinitapoli J (2013). “I will give birth but not too much”: HIV-positive childbearing in rural Malawi. In: Liamputtong P(ed.). Women, motherhood and living with HIV/AIDS. Dordrecht: Springer: 93–109. [Google Scholar]
- Zere E, Moeti M, Kirigia J, Mwase T, and Kataika E (2007). Equity in health and healthcare in Malawi: Analysis of trends. BMC Public Health 7(78). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Solazzo A, and Gorman BK (2020). Education and health: The joint role of gender and sexual identity. SSM-Population Health 12: 100668. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This research uses data from Tsogolo la Thanzi. Study instruments are available at https://tsogololathanzi.uchicago.edu/ and the data are available through restricted data user agreements managed by Data Sharing for Demographic Research (DSDR) at the University of Michigan.


