Abstract
Background:
Neck pain is a common musculoskeletal symptom that has negative effects on quality of life and work productivity. Acupuncture has been widely used for neck pain, and a number of randomized controlled trials (RCTs) and systematic reviews (SRs) have evaluated its effectiveness. However, previous studies have obtained inconsistent results regarding the effects of acupuncture for neck pain, and there is no SR for the comparative efficacy and safety of various types of acupuncture. Therefore, we herein conducted a SR and network meta-analysis to compare and rank different types of acupuncture with respect to their effectiveness in treating neck pain.
Methods:
We searched 9 electronic databases for relevant RCTs published from their inception to July 1, 2021. Pairwise meta-analyses and network meta-analysis were performed with R software using the frequentist framework. Change of pain intensity was assessed as the primary outcome, and change of pain-related disability and efficacy rate were assessed as secondary outcomes. The Cochrane risk of bias tool and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) instrument were used to evaluate the quality of the included RCTs and the certainty of the evidence.
Results:
A total of 65 RCTs involving 5266 participants and 9 interventions were included. Three network meta-analyses were constructed for the following: pain intensity (42 RCTs, 3158 participants), pain-related disability (21 RCTs, 1581 participants), and efficacy rate (40 RCTs, 3512 participants). The results indicated that fire acupuncture, electroacupuncture, and warm acupuncture were more effective than manual acupuncture in terms of pain intensity reduction and efficacy rate, and that electroacupuncture decreased pain-related disability more effectively than manual acupuncture. Fire acupuncture ranked first among the 9 interventions. The overall q of evidence was very low according to the GRADE assessment. The reported adverse events were not serious.
Conclusion:
Fire acupuncture, warm acupuncture, acupoint catgut embedding, and electroacupuncture ranked higher than other interventions (usual care, sham acupuncture, no treatment) in reducing the pain and disability index scores and the efficacy rate. However, the included trials were evaluated as being of low quality; thus, we recommend additional well-designed RCTs with larger sample sizes to confirm these findings.
Systematic review registration:
PROSPERO, CRD42021235274.
Keywords: acupuncture, neck pain, network meta-analysis, systematic review, randomized controlled trials
1. Introduction
Neck pain is defined as pain, muscle tension, or stiffness that is anatomically localized below the superior nuchal line and above the scapular line from the back, and below the superior nuchal line and the external occipital protuberance line and above the superior border of the clavicle and the suprasternal notch from the side and front.[1] A large proportion of the population (22–70%) suffers from neck pain at some point in the lifespan, and the prevalence of neck pain increases with age.[2] The pain and disability related to neck pain can considerably impact an individual’s quality of life and work productivity and increase the global burden of health care expenditure.[3]
Most patients with neck pain receive conservative treatments, such as oral medication, injection, massage, and/or physical therapy unless they have cervical fracture or severe cervical neuropathy.[2] However, some of these treatments have limited evidence supporting their efficacy against neck pain and/or carry potential complications, such as the elevated risk for cardiovascular disease, renal toxicity, nerve injury, infection, epidural hemorrhage, and/or subarachnoid penetration.[4–6]
Acupuncture is widely used to treat musculoskeletal pain in many countries.[7,8] An estimated 3 million American adults receive acupuncture treatment each year for musculoskeletal pain, which is the most common condition treated by this modality in the United States.[9] One study conducted in 15 European countries found that 13% of patients with pain seek acupuncture treatment in addition to conventional medication.[10] According to clinical practice guidelines for neck pain using traditional Korean medicine, various acupuncture therapies, including manual acupuncture (MA), electroacupuncture (EA), warm acupuncture (WA), fire acupuncture (FA), and acupoint catgut embedding (ACE), can relieve symptoms related to neck pain.[11]
While a number of randomized controlled trials (RCTs), systematic reviews (SRs), and meta-analyses have reported pairwise comparisons of different types of acupuncture or acupuncture versus an inactive control,[11–13] the existing literature does not allow us to compare the effectiveness of various types of acupuncture therapies. Furthermore, in some SRs, the results regarding the effects of acupuncture treatment were observed inconsistently depending on which comparison group was designated.[13–15] Therefore, the literature does not currently provide clinicians with clear guidelines on what types of acupuncture therapies are most effective in treating neck pain.
Network meta-analysis is a quantitative synthesis of evidence for various treatments of the same indication; it combines direct and indirect evidence into a single analysis of potential treatment effect and allows the user to rank the available treatments according to the effect size.[16] Thus, network meta-analysis could be used to evaluate the relative effectiveness of different types of acupunctures, even if the interventions have never been compared directly in clinical trials.
Here, we used frequentist network meta-analysis to compare and rank the effectiveness and safety of different types of acupuncture therapies and other interventions for treating neck pain.
2. Methods
This SR and network meta-analysis is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement and PRISMA extension for network meta-analyses.[17,18] This study was registered on PROSPERO under number CRD42021235274, and a detailed protocol was published elsewhere.[19]
2.1. Search strategy
Ovid-MEDILINE, EMBASE, Cochrane library, China National Knowledge Infrastructure (CNKI), Korea Med, Korean medical database (KMBASE), Korean Studies Information Service System (KISS), ScienceON, and Oriental Medicine Advanced Searching Integrated System (OASIS) were searched on July 1, 2021, with the limitation of Chinese, English, and Korean language. We used the following combination of MeSH terms and free words to search the literature: (1) neck-pain-related terms (such as neck pain, cervical pain, cervicodynia, cervicalgia, cervical intervertebral disc displacement/degeneration, cervical spondylosis), (2) various acupuncture treatments (such as manual acupuncture, electroacupuncture, warm acupuncture, fire acupuncture, acupoint catgut embedding), and (3) randomized controlled trial. The search strategy was initially developed for the Ovid-MEDILINE databases; we subsequently adjusted it to the requirements of the other databases. In addition, missing literature was included from the reference lists of the retrieved SRs (see Appendix S1, Supplemental Digital Content, http://links.lww.com/MD/G898, which shows the detailed retrieval strategies for all databases).
2.2. Eligibility criteria
2.2.1. Participants.
Patients who had cervical pain or cervical intervertebral disc herniation with or without radicular symptoms and aged 18 years above were enrolled, regardless of gender, disease course, or disease severity. Only patients lacking a specific reason for the condition (e.g., whiplash or traumatic injury) were included.
2.2.2. Intervention and comparison.
We included 5 types of acupuncture therapies: MA, EA, WA, FA, and ACE. In this network meta-analysis, each acupuncture treatment defined only a single use of these 5 types, as this allowed us to compare the effects of different acupuncture treatments for neck pain. As comparators, we included sham acupuncture (SA), usual care (UC), western medicine (WM), no treatment (NT; wait list), and one of the abovementioned acupuncture therapies.
2.2.3. Outcome measures.
The included studies were required to have one of the following outcomes: (i) as a primary outcome, pain intensity measured by the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS); and (ii) as secondary outcomes, pain-related disability evaluated by the Neck Disability Index (NDI) or Neck Pain Questionnaire (NPQ), and the efficacy rate.
2.3. Study selection and data extraction
All identified studies were imported into Endnote X20 (ISI Research Soft, USA). The titles and abstracts were read and studies that were duplicate or did not meet the inclusion criteria were excluded. For each identified study, 2 reviewers (E-J Noh and S-H Oh) reviewed the full text and extracted the data using a standardized extraction table. At either stage, any discrepancy in the study inclusion or data extracted was resolved by a third reviewer (H-R Jo).
Study characteristics (author and year of publication), sample size, age, intervention, comparator, treatment frequency, duration, outcomes, results, and adverse events were recorded. Means and standardized differences at baseline and the end point of the treatment period were extracted.
2.4. Quality assessment
Two reviewers (S-J Choi and D-I Kim) independently used the risk of bias tool of Cochrane Collaborations to evaluate the methodological quality of the included studies. Each study was rated as high, low, or unclear for the following 7 domains: random sequence generation, allocation concealment, participant and personnel blinding, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. A third reviewer (H-R Jo) resolved any disagreement as necessary.
2.5. Statistical analysis
All analyses were performed in R software (http://www.r-project.org/; version 4.0.3) using the “meta” and “netmeta” packages. A randomized effects model was used to perform a pairwise meta-analysis for each pair of interventions, applying the standardized mean difference (SMD), relative risk (RR), and 95% confidence interval (CI) to synthesize dichotomous or continuous outcomes. Heterogeneity was evaluated by the I2 value, with I2 < 50% taken as representing little or no obvious heterogeneity. A network meta-analysis was performed using a frequentist method. League tables and P-scores were used to present the ranking of direct and indirect effect estimates and the 95% CI for all comparisons of interventions in the network. According to Rücker et al, the P-score can be interpreted as a cumulative ranking under the surface curve (SUCRA) for frequentist analysis.[20] We first evaluated the difference between direct and indirect evidences for the same comparison, using global I2 and P values, and then assessed the inconsistency for each intervention using the node-splitting analysis method.
2.6. GRADE assessment
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) method was used to evaluate the quality of evidence for each outcome. Based on the assessment of each study limitation, inconsistency, indirectness, imprecision, and publication bias, the quality of the evidence can be maintained or downgraded to moderate, low, or very low quality.[21] Given that the quality of evidence might differ across paired comparisons, a GRADE approach previously adapted for network meta-analysis was used for each pairwise comparison.[22,23]
2.7. Publication bias and sensitivity analysis
We evaluated the small-sample effect or publication bias in each network meta-analysis by comparison-adjusted funnel plots. In addition, we conducted a sensitivity analysis by excluding studies with a higher risk of bias or a smaller sample size (<10 per group).
2.8. Ethics approval
No ethical approval was not needed because data from previously published studies in which informed consent was obtained by primary investigators were retrieved and analyzed.
3. Results
3.1. Search results
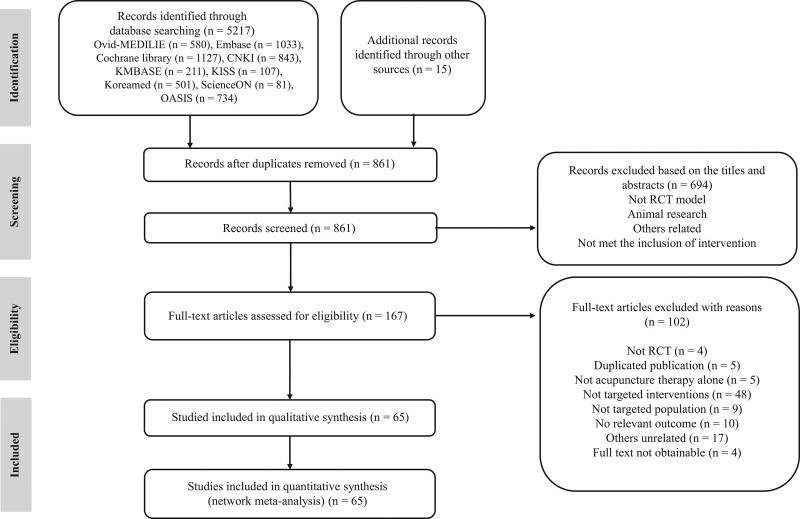
In total, 5217 RCTs were retrieved from the database searches and a further 15 studies were added manually. After the article title and abstract were read, 4371 duplicate records were removed and 694 records that did not meet the inclusion criteria were removed. Based on full-text assessments, a further 102 articles were discarded for the reasons listed in Figure 1. Eventually, 65 studies were included in the network meta-analysis (Fig. 1).
Figure 1.
Flow chart of article searching and selection.
3.2. Characterization of the included RCTs
The 65 selected RCTs included a total of 5266 participants and had sample sizes varying from 17 to 220 patients. Most were conducted in China; of the others, 6 were conducted in Iran,[24–29] 3 in Spain,[30–32] 2 in Turkey,[33,34] and 1 each from Taiwan,[35] Japan,[36] Germany,[37] Korea,[38] Belgium,[39] and the United States.[40] Sixty-two were 2-arm trials and the remaining 3 were 3-arm trials. Nine interventions were applied, including 6 types of acupuncture therapies (MA, EA, WA, FA, ACE, SA), WM, NT (waitlist), and UC (exercise, pressure release, Kinesiotaping). The treatment period of intervention ranged from 1 day to 9 weeks. Pain intensity was reported in 42 studies; of them, 39 used VAS and 3 used NRS. Pain-related disability was reported in 21 studies; of them, 11 used NDI and 10 used NPQ. The efficacy rate was reported in 41 studies. The characteristics of the included studies are presented in Table 1.
Table 1.
Characteristics of the included studies.
| Intervention | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study ID | Sample size (E/C) | Mean age (yrs) (E/C) | Experimental group | Control group | Frequency, duration | Treatment period (weeks) | Outcome | Results | Adverse event (n) |
| Acupuncture | |||||||||
| Ho 2017[41] | 77/77 | 45.53 ± 8.74/44.51 ± 9.48 | MA | SA | 3 times per week, 30 min | 2 | VAS, NPQ, SF-36 | 1. VAS: E > C (P < .001) | No serious AEs. |
| 2. NPQ: E > C (P = .008) | E: local transient bruises (n = 11) | ||||||||
| 3. SF-36: E > C (P = .003) | |||||||||
| Tekin 2013[33] | 22/17 | 42.9 ± 10.9/ 42.0 ± 12.0 | MA | SA | Twice per week (2 weeks), once per week (until end point) | 4 | VAS, SF-36 | 1. VAS: E > C (P = .000) | NR |
| 2. SF-36: E > C (P < .05) | |||||||||
| Chou 2011[35] | 15/15 | 34.1 ± 10.7/ 33.9 ± 8.3 | MA | SA | NR | 1 day | NRS, PPT, ROM, mean amplitude of EPN | 1. NRS: E > C | NR |
| 2. PPT: E > C | |||||||||
| 3. ROM: E > C | |||||||||
| 4. Mean amplitude of EPN : E > C (all P < .05) | |||||||||
| Nabeta 2002[36] | 17/17 | 34.2 ± 10.8/ 30.8 ± 12.0 | MA | SA | Once a week, 5 min | 3 | VAS, PPT | 1. VAS: E = C | NR |
| 2. PPT: E > C (P < .05) | |||||||||
| Irnich 2001[37] | 56/61 | 52.3 ± 13.3/52.2 ± 13.2 | MA | SA | 5 times, 30 min | 3 | VAS, ROM, SF-36 | 1. VAS: E = C | No serious AEs. |
| 2. ROM: E = C | Mild reactions (sweating, low blood pressure): E (n = 17), C (n = 12) | ||||||||
| 3. SF-36: E = C | |||||||||
| Raeissadat 2018[24] | 23/22 | 41.6 ± 6.8/39.4 ± 7.7 | MA | WM (2cc of 2% lidocaine injection) | Once per week | 3 | VAS, PPT, ROM, NDI | 1. VAS: E < C | No serious AEs. |
| 2. PPT: E < C | E: local transient flare reaction (n = 1) | ||||||||
| 3. ROM: E < C | |||||||||
| 4. NDI: E < C (all P > .05) | |||||||||
| Wang 2015[42] | 51/47 | 43 ± 12/48 ± 9 | MA | WM(medical solution 2 mL injection; 2.5 mL of 2% lidocaine, 500 mg of mecobalamin, 2.5 mg of dexamethasone sodium phosphate, 12 mL of 0.9% saline) | 5 times per week, 30 min | 2 | VAS, rotate-cervix test positive, dizziness score, efficacy rate | 1. VAS: E > C | No serious AEs. |
| 2. Rotate-cervix test positive: E > C | Subcutaneous blood stasis in both groups. | ||||||||
| 3. Dizziness score: E > C | |||||||||
| 4. Efficacy rate: E > C (all P < .05) | |||||||||
| Cho 2014[38] | 15/15 | 39.1 ± 9.0/38.2 ± 10.2 | MA | WM (zaltoprofen 80 mg daily, 3 times per day) | 3 times per week, 15 min | 3 | VAS, NDI, BDI, SF-36, EQ-5D | 1. VAS: E = C | None |
| 2. NDI: E = C | |||||||||
| 3. BDI: E = C | |||||||||
| 4. SF-36: E = C | |||||||||
| 5. EQ-5D: E = C | |||||||||
| Fu 2005[43] | 55/47 | 34.20 ± 7.61/ 35.24 ± 6.67 | MA | WM (0.1 mL lidocaine, injected into each acupoint, twice a week, total 4 week) | Twice a week, | 4 | efficacy rate, VAS, PRI, dizziness score | 1. Efficacy rate: E > C | None |
| 30 min | (P = .006) | ||||||||
| 2. VAS: E = C | |||||||||
| 3. PRI: E > C (P < .05) | |||||||||
| 4. Dizziness score: E > C (P < .05) | |||||||||
| Tabatabaiee 2019[25] | 20/20/20 | 23.6 ± 1.81/ | MA | C1: UC (Pressure release) | Twice per week, | 3–4 | ROM, PPT, VAS | 1. ROM: E = C2 > C1 | NR |
| C1: 23.5 ± 1.6 | C2: WM(Phonophoresis with betamethasone) | No retention | (7 times) | 2. PPT: E = C2 > C1 | |||||
| C2: 23.9 ± 3.09 | 3 times per week | 3. VAS: E = C2 > C1 (all P < .001) | |||||||
| Nejati 2021[26] | 37/38 | 40.62 ± 8.52/ 47.32 ± 10.23 | MA | UC (stretching, strengthening exercises) | Twice per week | 6 | NDI, Neck pain and disability scale | 1. NDI: E = C | None |
| 2. Neck pain and disability scale: E = C | |||||||||
| Arias-Buria 2020[30] | 15/15 | 21 ± 3/22 ± 2 | MA | UC (pressure release) | 1 time, | 1 day | NRS, NDI, inspiratory vital capacity | 1. NRS: E = C | None |
| no retention | 2. NDI: E = C | ||||||||
| 3. Inspiratory vital capacity: E > C (P < .05) | |||||||||
| Ziaeifer 2019[27] | 16/17 | 30.06 ± 9.87/ | MA | UC (pressure release) | 3 times per week, no retention | 1 | VAS, DASH, NPQ | 1. VAS: E > C (P = .02) | NR |
| 26.5 ± 8.57 | 2. DASH: E = C | ||||||||
| 3. NPQ: E = C | |||||||||
| Meulemeester 2017[39] | 20/22 | 36.1 ± 10.7/40.5 ± 8.3 | MA | UC (pressure release) | Once per week, | 4 | NDI, NRS, PPT, tone, elasticity, stiffness | 1. NDI: E = C | No serious AEs. |
| No retention | 2. NRS: E = C | E: postneedling soreness | |||||||
| 3. PPT: E = C | |||||||||
| 4. Tone: E = C | |||||||||
| 5. Elasticity: E = C | |||||||||
| 6. Stiffness: E = C | |||||||||
| Ziaeifer 2016[28] | 14/17 | 30.78 ± 10.39/26.69 ± 9.4 | MA | UC (ischemic compression) | 3 times per week | 1 | VAS, PPT | 1. VAS: E < C | NR |
| (48-hour interval between sessions) for each group | 2. PPT: E < C | ||||||||
| Hayta 2016[34] | 28/27 | NR | MA | UC (Kinesiotaping) | Twice per week | 2 | VAS, NDI, Nottingham Health Profile | 1. VAS: E = C | NR |
| 10–20 min | 2. NDI: E = C | ||||||||
| 3. Nottingham Health Profile: E = C | |||||||||
| Ziaeifer 2014[29] | 16/17 | 30.06 ± 9.87/ 26.50 ± 8.57 | MA | UC (ischemic compression) | 3 times per week, no retention | 1 | VAS, PPT, DASH | 1. VAS: E > C (P = .01) | NR |
| 2. PPT: E = C | |||||||||
| 3. DASH: E = C | |||||||||
| Fu 2013[44] | 30/30 | 41.53 ± 9.41/42.57 ± 10.32 | MA | UC (McKenzie exercise) | 5 times per week, 30 min | 2 | Efficacy rate, cervical spine function assessment (total, clinical symptoms, clinical examination, daily life actions) | 1. Efficacy rate: E > C (P < .05) | NR |
| 2. Cervical spine function assessment | |||||||||
| - Total score: E > C | |||||||||
| (P < .001) | |||||||||
| - Clinical symptoms: | |||||||||
| E > C (P < .05) | |||||||||
| - Clinical examination: | |||||||||
| E > C (P < .05) | |||||||||
| - Daily life actions: E = C | |||||||||
| Mejuto-Vazquez 2014[31] | 9/8 | 25 ± 4/24 ± 7 | MA | NT | No retention | 1 day | NRS, PPT, ROM | 1. NRS: E > C (P < .01) | No serious AEs. |
| 2. PPT: E > C (P < .01) | E:postneedling soreness (n = 8) | ||||||||
| 3. ROM: E > C (P < .01) | |||||||||
| Electroacupuncture | |||||||||
| Chen 2019[40] | 46/33/30 | mean 55/ | EA | C1: SA | Twice per week, 30 min | 3 | VAS, SF-36 | 1. VAS | No serious AEs. |
| C1: mean 53/C2: mean 51 | C2: NT | E = C1 | E: acupuncture-related | ||||||
| E > C2 (P = .003) | uncomfortableness (n = 1) | ||||||||
| C1 = C2 | |||||||||
| 2. SF-36 | |||||||||
| - physical functioning, pain | |||||||||
| E = C1 | |||||||||
| E > C2 (P = .001) | |||||||||
| C1 = C2 | |||||||||
| - role functioning/physical | |||||||||
| E = C1 | |||||||||
| E > C2 (P = .032) | |||||||||
| C1 = C2 | |||||||||
| - role functioning/emotional, social functioning, emotional well-being | |||||||||
| E = C1 | |||||||||
| E = C2 | |||||||||
| C1 = C2 | |||||||||
| - Energy/fatigue | |||||||||
| E = C1 | |||||||||
| E > C2 (P = .007) | |||||||||
| C1 = C2 | |||||||||
| - general health E = C1 | |||||||||
| E > C2 (P = .03) | |||||||||
| C1 = C2 | |||||||||
| Cui 2016[45] | 37/30 | 47.03 ± 14.19/49.27 ± 10.96 | EA | SA | 3 times per week, 30 min | 4 | NPQ, MPQ, SF-36, efficacy rate | 1. NPQ: E = C | None |
| 2. MPQ: E = C | |||||||||
| 3. SF-36: E = C | |||||||||
| 4. Efficacy rate: E = C | |||||||||
| Feng 2014[46] | 17/18/19 | 20–60 | EA | C1: SA | 3 times per week, 30 min | 4 | NPQ, MPQ, VAS, PPT | 1. NPQ: E > C1 = C2 | NR |
| C2: NT | 2. MPQ: E > C1 = C2 | ||||||||
| 3. VAS: E > C1 = C2 | |||||||||
| 4. PPT: E > C1 = C2 (all P < .05) | |||||||||
| Zhang 2013[47] | 103/103 | mean 45.8 | EA | SA | 3 times per week, 45 min | 3 | NPQ, symptom score, SF-36 | 1. NPQ: E = C | No serious AEs. |
| 2. Symptom score: E = C | E:increased neck pain (n = 1), headache (n = 2), dizziness (n = 1), pain at acupuncture point (n = 1),local transient bruises(n = 2), chest discomfort (n = 1) | ||||||||
| 3. SF-36: E = C | C:increased neck pain (n = 2), headache (n = 1), dizziness (n = 1), itching palm (n = 1), warmth at the back (n = 1) | ||||||||
| Li 2008[48] | 42/52 | E: 47.40 ± 8.75 | EA | WM (Fenbid capsules 300 mg, once a day) | Once every other day, 20 min | 3 | efficacy rate | 1. Efficacy rate: E > C (P < .05) | NR |
| C: NR | |||||||||
| Yan 2006[49] | 78/78 | mean 48.5/47.3 | EA | WM (Ibuprofen 2 tablets, enteric-coated aspirin tablets 0.3g, vitamin B1, 20 mg, twice per day) | Once per day, 30 min | 10 days | efficacy rate | 1. Efficacy rate: E > C (P < .01) | NR |
| Diethelm 2014[50] | 30/30 | 42.27 ± 11.79/50.77 ± 10.79 | EA | UC (Kinesiotaping) | Twice per week, 30 min | 4 | VAS, MPQ, efficacy rate | 1. VAS: E > C (P = .016) | NR |
| 2. MPQ: E > C (P < .01) | |||||||||
| 3. Efficacy rate: E > C (P < .05) | |||||||||
| Yang 2020[51] | 30/30 | total 47.63 ± 3.72 | EA | MA | 3 times per week, 30 min | 4 | Cervical spondylosis symptom scale, VAS, NDI, Serum IL-6, efficacy rate | 1. Cervical spondylosis symptom scale: E > C (P < .01) | NR |
| 2. VAS: E > C (P < .01) | |||||||||
| 3. NDI: E > C (P < .01) | |||||||||
| 4. Serum IL-6 (P < .01) | |||||||||
| 5. Efficacy rate (P < .05) | |||||||||
| Garcia-De-Miguel 2020[32] | 22/22 | 24.14 ± 9.39/25.45 ± 8.53 | EA | MA | 1 time, | 1 day | VAS, NDI, PPT, ROM, Side bending strength | 1. VAS: E = C | NR |
| E: 20 min, | 2. NDI: E > C (P < .05) | ||||||||
| C: no retention | 3. PPT: E > C (P < .01) | ||||||||
| 4. ROM: E = C | |||||||||
| 5. Side bending strength: E = C | |||||||||
| Huang 2018[52] | 45/45 | 41 ± 10/42 ± 9 | EA | MA | once every other day, 20 min | 3 | symptom and physical sign score, VAS, efficacy rate | 1. Symptom and physical sign score: E > C | NR |
| 2. VAS: E > C | |||||||||
| 3. Efficacy rate: E > C (all P < .05) | |||||||||
| Chen Y 2016[53] | 30/30 | mean 45/45 | EA | MA | once every other day, 30 min | 4 | TTYS, MPQ, efficacy rate | 1. TTYS: E > C (P < .05) | None |
| 2. MPQ: E > C (P < .05) | |||||||||
| 3. Efficacy rate: E > C (P < .05) | |||||||||
| Chen G 2016[54] | 30/30 | 32.83 ± 8.94/ 34.66 ± 8.92 | EA | MA | once per day, 30 min | 1 | PPI, PRI, | 1. PPI: E > C | NR |
| VAS, ROM, efficacy rate, symptom and sign score | 2. PRI: E > C | ||||||||
| 3.VAS: E > C | |||||||||
| 4. ROM: E > C | |||||||||
| 5. Efficacy rate: E > C | |||||||||
| 6. Symptom and sign score: E > C (all P < .05) | |||||||||
| Tian 2015[55] | 30/30 | 39.12 ± 7.85/ 41.33 ± 9.33 | EA | MA | once per day, | 4 | NPQ, MPQ | 1. NPQ: E > C (P < .01) | NR |
| 30 min | efficacy rate | 2. MPQ: E > C (P < .01) | |||||||
| 3. Efficacy rate: E = C | |||||||||
| Chen 2015[56] | 30/30 | 31–75 | EA | MA | once per day, 30 min | 4 | efficacy rate, PRI, VAS, PPI, mean treatment time | 1. Efficacy rate: E = C | NR |
| 2. PRI: E > C (P < .01) | |||||||||
| 3.VAS: E > C (P < .01) | |||||||||
| 4. PPI: E > C (P < .01) | |||||||||
| 5. Mean treatment time: E > C (P < .01) | |||||||||
| Liu 2014[57] | 30/30 | 43.27 ± 11.67/ 40.23 ± 11.37 | EA | MA | once per day, 30 min | 3 | symptom and sign score, MPQ, F wave conduction velocity (median nerve, ulnar nerve), efficacy rate | 1.Symptom and sign score: E > C | NR |
| 2. MPQ: E > C | |||||||||
| 3. F wave conduction velocity: E > C | |||||||||
| 4. Efficacy rate: E > C (all P < .05) | |||||||||
| Jin 2013[58] | 30/30 | 44.60 ± 1.78/ 41.10 ± 1.94 | EA | MA | once per day, | 2 | efficacy rate, PRI, VAS, | 1. Efficacy rate: E = C | No serious AEs. |
| 30 min | PPI, TTYS | 2. PRI: E = C | Anxiety in both groups. | ||||||
| 3. VAS: E = C | |||||||||
| 4. PPI: E = C | |||||||||
| 5. TTYS: E > C (P < .05) | |||||||||
| Zhang 2011[59] | 57/49 | 21–77 | EA | MA | once per day, 30 min | 3 | efficacy rate, curative rate | 1. Efficacy rate: E = C | NR |
| 2. Curative rate: E > C (P < .05) | |||||||||
| Yang 2011[60] | 36/36 | 42.18/41.32 | EA | MA | 5 times per week, 30 min | 4 | VAS, efficacy rate | 1. VAS: E > C (P < .01) | NR |
| 2. Efficacy rate: E > C (P < .05) | |||||||||
| Ji 2015[61] | 29/29 | NR | EA | MA | 5 times per week, 30 min | 4 | NPQ, VAS, SF-36 | 1. NPQ: E > C | NR |
| 2. VAS: E > C3. SF-36: E > C (all P < .05) | |||||||||
| Wang 2010[62] | 35/35 | 38.29 ± 10.72/ 36.96 ± 11.21 | EA | MA | once every other day, 20 min | 10 days | NPQ, MPQ, VAS, SF-36, efficacy rate | 1. NPQ: E > C (P < .01) | None |
| 2. MPQ: E > C (P < .01) | |||||||||
| 3. VAS: E > C (P < .01) | |||||||||
| 4. SF-36: E > C (P < .05) (except physical functioning and role physical: E = C) | |||||||||
| 5. Efficacy rate: E > C (P = .03) | |||||||||
| Liu 2010[63] | 30/30 | 40.93 ± 11.25/ 42.03 ± 11.61 | EA | MA | once per day, 30 min | 3 | symptom and sign score, efficacy rate, PRI | 1.Symptom and sign score: E > C | NR |
| 2. Efficacy rate: E > C | |||||||||
| 3. PRI: E > C (all P < .05) | |||||||||
| Lai 2010[64] | 35/35 | NR | EA | MA | once per day, | 4 | symptom score, Chinese medicine symptom score, VAS, PRI, PPI, efficacy rate | 1. Symptom score: E > C | None |
| 30 min | 2 Chinese medicine symptom score: E > C | ||||||||
| 3. VAS: E > C | |||||||||
| 4. PRI: E > C | |||||||||
| 5. PPI: E > C (1–5 all P < .01) | |||||||||
| 6. Efficacy rate: E = C | |||||||||
| Yang 2009[65] | 100/100 | 23–77 | EA | MA | once per day, 30 min | 10–30 days | efficacy rate, | 1. Efficacy rate: E > C | NR |
| curative rate | 2. Curative rate: E > C (all P < .05) | ||||||||
| Ding 2009[66] | 30/30 | 41.05 ± 9.65/42.50 ± 7.63 | EA | MA | 5 times per week, 30 min | 3 | symptoms scores, efficacy rate | 1. Symptoms scores: E > C (P < .01) | NR |
| 2. Efficacy rate: E > C (P < .05) | |||||||||
| Yu 2007[67] | 30/30 | 46.19 ± 10.88/ 43.64 ± 14.63 | EA | MA | once per day, | 3 | symptom and sign score, PRI, VAS, PPI, efficacy rate | 1. Symptom and sign score: E > C (P < .05) | NR |
| 30 min | 2. PRI: E > C (P < .001) | ||||||||
| 3. VAS: E > C (P < .05) | |||||||||
| 4. PPI: E > C (P < .001) | |||||||||
| 5. Efficacy rate: E > C (P < .05) | |||||||||
| Warm acupuncture | |||||||||
| Chen 2020[68] | 40/40 | NR | WA | MA | once every other day, 20–30 min | 6 | efficacy rate, symptoms score, SF-36, NPQ, VAS | 1. Efficacy rate: E > C | None |
| 2. Symptoms score: E > C | |||||||||
| 3. NPQ: E > C | |||||||||
| 4. VAS: E > C | |||||||||
| 5. SF-36: E > C (all P < .05) | |||||||||
| Ju 2019[69] | 60/60 | 48.55 ± 11.63/ 46.27 ± 11.51 | WA | MA | E: once per week, 20 min | 3 | assessment scale for cervical spondylosis, improvement index, improvement rate, symptom score, VAS | 1. Assessment scale for cervical spondylosis: E > C (P < .01) | None |
| C: 6 times per week, 30 min | 2. Improvement index: E = C | ||||||||
| 3. Improvement rate: E = C | |||||||||
| 4. Symptom score: E > C (P < .01) | |||||||||
| 5. VAS: WA > MA(P < .01) | |||||||||
| Xu 2017[70] | 110/110 | 56.2 ± 9.4/ | WA | MA | twice per day | 2 | efficacy rate, VAS | 1. Efficacy rate: E > C | NR |
| 56.4 ± 9.3 | 2. VAS: E > C (all P < .05) | ||||||||
| Guo 2015[71] | 30/30 | 24.07 ± 3.41/ 24.70 ± 2.95 | WA | MA | once every other day, 30 min | 2 | NPQ, MPQ, efficacy rate | 1. NPQ: E > C (P < .05) | None |
| 2. MPQ: E > C (P < .01) | |||||||||
| 3. Efficacy rate: E > C (P < .05) | |||||||||
| Zhou 2014[72] | 30/30 | mean 39.2/43.3 | WA | MA | once per day, | 10 days | efficacy rate, TTYS, VAS | 1. Efficacy rate: E > C | None |
| 30 min | 2. TTYS: E > C3. VAS: E > C (all P < .05) | ||||||||
| Lin Z 2012[73] | 40/40 | mean 60.25/58.24 | WA | MA | once every other day | 9 | TTYS, efficacy rate | 1. TTYS: E > C (P < .05) | NR |
| 2. Efficacy rate: E = C | |||||||||
| Garov 2016[74] | 30/30 | 42.81 ± 12.76/ 40.45 ± 12.99 | WA | EA | 5 times per week, 30 min | 2 | TTYS, VAS | 1. TTYS: E = C | E: subcutaneous bleeding (n = 1), burn (n = 1)C: subcutaneous bleeding (n = 1), dizziness (n = 1) |
| 2. VAS: E = C | |||||||||
| Su 2015[75] | 30/30 | 39 ± 11/44 ± 12 | WA | EA | once every other day, 20 min | 2 | PRI, VAS, PPI, efficacy rate, the counts of red and yellow tender points | 1. PRI: E > C | NR |
| 2. VAS: E > C | |||||||||
| 3. PPI: E > C | |||||||||
| 4. Efficacy rate: E > C | |||||||||
| 5. The counts of red tender points: E > C | |||||||||
| 6. The counts of yellow tender points: E > C (all P < .05) | |||||||||
| Lin J 2012[76] | 30/30 | 18–65 | WA | EA | once every other day, 30 min | 4 | VAS, NPQ, efficacy rate | 1. VAS: E > C (P = .01) | None |
| 2. NPQ: E > C (P = .04) | |||||||||
| 3. Efficacy rate: E = C | |||||||||
| Fire acupuncture | |||||||||
| Qui 2015[77] | 31/31 | 44.12 ± 11.21/ | FA | MA | E: twice per week, no retention | 3 | symptom and sign scores, efficacy rate | 1. Symptom and sign score: E > C (P < .05) | NR |
| 43.58 ± 10.02 | C: once per day, 30 min | 2. Efficacy rate: E > C (P < .05) | |||||||
| Sun 2015[78] | 100/100 | 46 ± 12/46 ± 14 | FA | MA | once per day | 3 | VAS, PPI, PRI, | 1. VAS: E > C | NR |
| E: no retention | efficacy rate | 2. PPI: E > C | |||||||
| C: 20 min | 3. PRI: E > C | ||||||||
| 4. Efficacy rate: E > C (all P < .01) | |||||||||
| Zhao 2013[79] | 30/30 | 18–60 | FA | EA | E: once per 5 days, no retention | 4 | MPQ, NPQ, NDI, EMG (trapezius muscle, sternocleidomastoid muscle), efficacy rate | 1. MPQ: E > C (P < .01) | NR |
| 2. NPQ: E > C (P < .01) | |||||||||
| C: once per day, 30 min | 3. NDI: E > C (P < .05) | ||||||||
| 4. EMG: E = C | |||||||||
| 5. Efficacy rate: E > C (P < .01) | |||||||||
| Acupoint catgut embedding | |||||||||
| Cheng 2018[80] | 73/73 | 52.8 ± 5.2/ | ACE | MA | E: once every 15 days | 4 | symptoms scores, efficacy rate | 1. Symptoms scores: E > C (P < .05) | NR |
| 51.5 ± 5.2 | C: once per day, 30 min | 2. Efficacy rate: E > C (P < .05) | |||||||
| Qui C 2015[81] | 63/63 | 38 ± 8/37 ± 9 | ACE | MA | E: once per 2 weeks | 4 | efficacy rate | 1. Efficacy rate: E > C (P < .05) | NR |
| C: once per day, 20–30 min | |||||||||
| Wang 2016[82] | 35/35 | mean 52/54 | ACE | MA | E: once per week | 3 | symptom and sign score, VAS, PPI, efficacy rate | 1.Symptom and sign score: E = C | NR |
| C: once per day, 20 min | 2. VAS: E = C | ||||||||
| 3. PPI: E > C (P < .05) | |||||||||
| 4. Efficacy rate: E > C (P < .05) | |||||||||
| Li 2015[83] | 43/43 | 56.3 ± 8.5/ 57.1 ± 7.3 | ACE | MA | E: once per week | 4 | clinical symptoms and function evaluation, VAS, PRI, PPI, efficacy rate | 1. Clinical symptoms and function evaluation: E > C | NR |
| C: once per day, 30 min | 2. VAS: E > C | ||||||||
| 3. PRI: E > C | |||||||||
| 4. PPI: E > C | |||||||||
| 5. Efficacy rate: E > C (all P < .05) | |||||||||
| Zhao 2015[84] | 60/60 | 27.5 ± 2.4/ 28.0 ± 2.6 | ACE | MA | once per day C: 30 min | 10 days | efficacy rate | 1. Efficacy rate: E > C (P < .01) | NR |
| Ding 2012[85] | 58/62 | 29 ± 8/30 ± 9 | ACE | MA | E: once per week | 2 | efficacy rate, NDI, VAS | 1. Efficacy rate: E > C | NR |
| C: once per day, 30 min | 2. NDI: E > C3. VAS: E > C (all P < .05) | ||||||||
| Feng 2012[86] | 117/98 | 38.9 ± 7.6/ | ACE | MA | E: once per 2 weeks | 4 | NDI, VAS | 1. NDI: E > C (P < .05) | NR |
| 40.1 ± 8.7 | C: once every other day, 30 min | 2. VAS: E > C (P < .05) | |||||||
| Xian 2012[87] | 30/30 | 48.70 ± 7.15/47.53 ± 7.31 | ACE | MA | E: once per week | 2 | Cervical spondylosis score, MPQ, efficacy rate | 1. Cervical spondylosis score: E > C (P = .01) | No serious AEs. |
| C: 6 times per week, 30 min | 2. MPQ: E > C (P < .01) | E:subcutaneous bleeding (n = 2) | |||||||
| 3. Efficacy rate: E > C (P = .01) | |||||||||
| Zou 2016[88] | 30/30 | 49.67 ± 7.95/50.73 ± 7.60 | ACE | MA | E: once per week | 4 | Cervical spondylopathy symptoms and function evaluation scale, MPQ, efficacy rate | 1. Cervical Spondylopathy Symptoms and Function Evaluation Scale: E > C (P = .03) | NR |
| C: once per day, 15–20 min | 2. MPQ: E > C (P = .03) | ||||||||
| 3. Efficacy rate: E > C (P = .03) | |||||||||
E, experimental group; C, control group. The total efficacy rate was calculated as the number of cured and improved cases.ACE, acupoint catgut embedding; AE, adverse event; BDI, Beck Depression Inventory; DASH, Disabilities of the Arm, Shoulder, and Hand Questionnaire; EA, electroacupuncture; EMG, Electromyography; EPN, the end-plate noise; EQ-5D, Euroqol 5D health utility; FA, fire acupuncture; IL, interleukin; MA, manual acupuncture; MPQ, McGill Pain Questionnaire; NDI, Neck Disability Index; NPQ, Neck Pain Questionnaire; NR, not reported; NRS, numeral rating scale; NT, no treatment; PPI, present pain intensity; PPT, pain pressure threshold; PRI, pain rating index; ROM, range of motion; SA, sham acupuncture; SF-36, 36-Item Short Form Health Survey; TTYS, Total Tanaka Yasuku Score; UC, usual care; VAS, Visual Analog Scale; WA, warm acupuncture; WM, Western medicine.
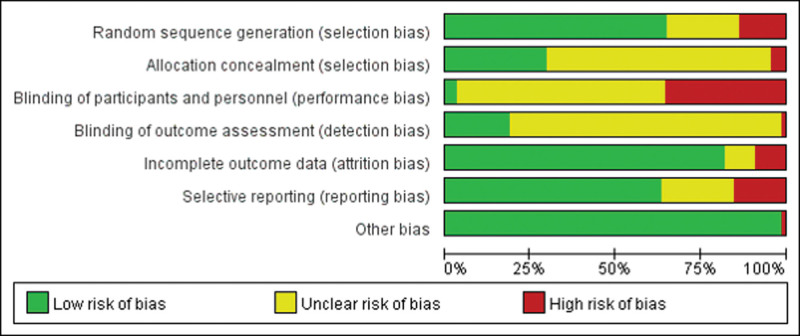
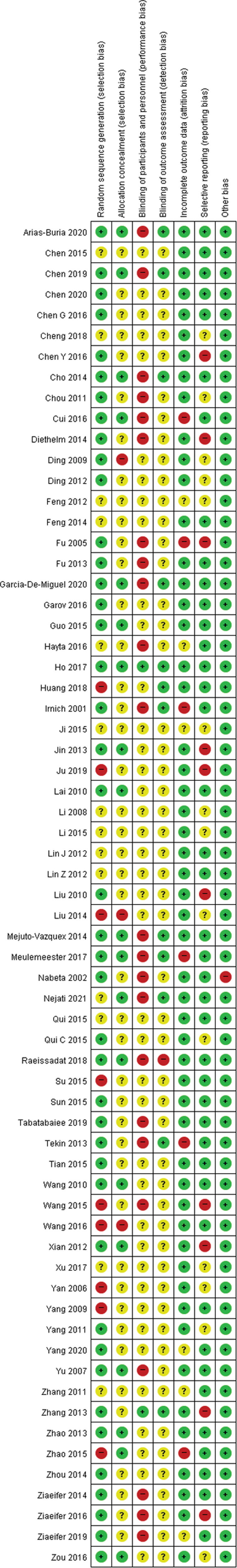
3.3. Risk of bias and quality assessment
The quantitative results of our risk of bias assessment are presented in Figures 2 and 3. Forty-two RCTs were rated as having a low risk of bias in random sequence generation: Of them, 26[25,30–33,35–38,40,41,45,47,51, 53,54,60,62–64,67,71,74,79,87,88] used various computerized randomization programs, 11[43,44,50,55,58,66,68,72,78,81,85] used random number tables, 3[27–29]used coin tossing, and 2[24,39] used block randomization. In terms of allocation in the RCTs, 19 studies[24,26,30–32,38–41,45,58,62,64,67,71,79,84,87,88] described proper allocation concealment (the use of sealed envelopes or independent researchers). Because of the nature of the interventions, performance bias was high in most studies; only 2 studies[41,47] were assessed as having a low risk of bias in participant blinding due to the use of nonpenetrating SA. The detection bias had low risk in 12 RCTs[26,30–33,37–41,47,52] that used independent assessors. Six RCTs[33,37,39,43,45,84] were rated as high risk for attrition bias because they had large amounts of missing data, and 6 RCTs[27,34,51,59,61,86] were rated as having unclear risk of bias for attrition because the reasons for the missing data were not stated. Ten RCTs[28,42,43,47,50,53,58,63,69,87] did not report complete results, and therefore were assessed as a high risk for bias in selective reporting. One study[36] that had volunteer bias was judged to have high risk of other bias.
Figure 2.
Risk of bias graph.
Figure 3.
Risk of bias for the included randomized controlled trials.
3.4. Pairwise meta-analysis
3.4.1. Pain intensity.
Fourteen pairwise meta-analyses were performed to compare the effectiveness of different acupuncture therapies in reducing pain intensity. MA was more effective in reducing pain intensity than SA (5 RCTs, SMD –1.11, 95% CI: –1.78 to –0.43; P = .0013) and UC (6 RCTs, SMD –0.59, 95% CI: –1.08 to –0.10; P = .0176). EA significantly reduced pain intensity compared to UC (1 RCT, SMD –0.75, 95% CI: –1.28 to –0.23; P = .0050). Compared to MA and other acupuncture therapies, WA, FA, and ACE had significantly better effects on pain intensity reduction (4 RCTs, SMD –0.96, 95% CI: –1.24 to –0.68, P < .0001; 1 RCT, SMD –1.76, 95% CI: –2.08 to –1.43, P < .0001; and 4 RCTs, SMD –0.67, 95% CI: –1.18 to –0.17, P = .0091, respectively). WA was more effective in reducing pain intensity compared to EA (3 RCTs, SMD –0.61, 95% CI: –1.22 to –0.00, P = .0486). When compared to NT, SA was significantly better at relieving pain intensity (1 RCTs, SMD –0.52, 95% CI: –1.02 to –0.01, P = .0439). There were obvious heterogeneities (I2 > 50%) in the above pairs, except for the comparison between WA and MA. There was no statistically significant difference between MA and WM, MA and NT, EA and SA, EA and NT, or EA and MA (Table 2).
Table 2.
Pairwise meta-analysis of pain intensity.
| Comparison | Number | SMD (95% CI) | P | I 2 |
|---|---|---|---|---|
| MA vs SA | 5 | –1.11 [–1.78, –0.43] | .0013 | 86.6% |
| MA vs WM | 5 | 0.01 [–0.39, 0.40] | .9753 | 63.7% |
| MA vs UC | 6 | –0.59 [–1.08, –0.10] | .0176 | 67.0% |
| MA vs NT | 2 | –0.71 [–1.83, 0.40] | .2102 | 68.6% |
| EA vs SA | 1 | –0.09 [–0.53, 0.36] | .7086 | – |
| EA vs UC | 1 | –0.75 [–1.28, –0.23] | .0050 | – |
| EA vs NT | 2 | –1.00 [–2.02, 0.01] | .0525 | 80.8% |
| EA vs MA | 12 | –0.75 [–1.57, 0.07] | .0739 | 95.5% |
| WA vs MA | 4 | –0.96 [–1.24, –0.68] | <.0001 | 49.8% |
| WA vs EA | 3 | –0.61 [–1.22, –0.00] | .0486 | 74.4% |
| FA vs MA | 1 | –1.76 [–2.08, –1.43] | <.0001 | – |
| ACE vs MA | 4 | –0.67 [–1.18, –0.17] | .0091 | 85.5% |
| WM vs UC | 1 | –1.16 [–1.83, –0.48] | .0008 | – |
| SA vs NT | 1 | –0.52 [–1.02, –0.01] | .0439 | – |
ACE = acupoint catgut embedding, CI = confidence interval, EA = electroacupuncture, FA = fire acupuncture, MA = manual acupuncture, NT = no treatment, SA = sham acupuncture, SMD = standardized mean difference, UC = usual care, WA = warm acupuncture, WM = Western medicine.
3.4.2. Pain-related disability.
Eleven pairwise meta-analyses were generated to investigate the ability of different acupuncture therapies to reduce pain-related disability. MA reduced disability significantly more than SA (1 RCT, SMD –0.78, 95% CI: –1.10 to –0.45; P < .0001). EA showed a significantly greater reduction in disability compared with NT (1 RCT, SMD –1.02, 95% CI: –1.72 to –0.32; P = .0044) and MA (5 RCTs, SMD –2.18, 95% CI: –3.53 to –0.83; P = .0016). Compared to MA and the other acupuncture therapies, WA and ACE significantly decreased disability (2 RCTs, SMD –0.68, 95% CI: –1.02 to –0.34; P < .0001; and 2 RCTs, SMD –0.31, 95% CI: –0.53 to –0.10; P = .0046, respectively). FA was more effective in reducing pain-related disability compared with EA (1 RCT, SMD –0.60, 95% CI: –1.12 to –0.08; P = .0228). Comparing EA (I2 = 95.6%) with MA showed obvious heterogeneity. The remaining 5 pairs were not statistically different in pain-related disability (Table 3).
Table 3.
Pairwise meta-analysis of pain-related disability.
| Comparison | Number | SMD (95% CI) | P | I 2 |
|---|---|---|---|---|
| MA vs SA | 1 | –0.78 [–1.10, –0.45] | <.0001 | – |
| MA vs WM | 2 | 0.55 [–0.22, 1.31] | .1607 | 59.7% |
| MA vs UC | 4 | –0.40 [–1.13, 0.33] | .2792 | 83.0% |
| EA vs SA | 3 | –0.31 [–0.77, 0.15] | .1815 | 63.3% |
| EA vs NT | 1 | –1.02 [–1.72, –0.32] | .0044 | – |
| EA vs MA | 5 | –2.18 [–3.53, –0.83] | .0016 | 95.6% |
| WA vs MA | 2 | –0.68 [–1.02, –0.34] | <.0001 | 0% |
| WA vs EA | 1 | –0.34 [–0.85, 0.17] | .1968 | – |
| FA vs EA | 1 | –0.60 [–1.12, –0.08] | .0228 | – |
| ACE vs MA | 2 | –0.31 [–0.53, –0.10] | .0046 | 0% |
| SA vs NT | 1 | –0.12 [–0.76, 0.53] | .7199 | – |
ACE = acupoint catgut embedding, CI = confidence interval, EA = electroacupuncture, FA = fire acupuncture, MA = manual acupuncture, NT = no treatment, SA = sham acupuncture, SMD = standardized mean difference, UC = usual care, WA = warm acupuncture, WM = Western medicine.
3.4.3. Efficacy rate.
Twelve pairwise meta-analyses were performed to compare the efficacy rates of different acupuncture treatments. Compared to MA and other acupuncture treatments, EA, WA, FA, and ACE each yielded a significantly higher efficacy rate (15 RCTs, RR 1.12, 95% CI: 1.08 to 1.17; P < .0001, I2 = 0%; 5 RCTs, RR 1.13, 95% CI: 1.06 to 1.20; P = .0003, I2 = 4.4%; 2 RCTs, RR 1.28, 95% CI: 1.16 to 1.42; P < .0001, I2 = 0%; and 7 RCTs, RR 1.12, 95% CI: 1.05 to 1.20; P = .0009, I2 = 42.4%, respectively). The remaining 8 pairs were not statistically different in their efficacy rates (Table 4).
Table 4.
Pairwise meta-analysis of efficacy rate.
| Comparison | Number | RR (95% CI) | P | I 2 |
|---|---|---|---|---|
| MA vs WM | 2 | 1.10 [0.89, 1.37] | .3825 | 85.0% |
| MA vs UC | 1 | 1.12 [0.93, 1.35] | .2335 | – |
| EA vs SA | 1 | 1.46 [0.80, 2.67] | .2204 | – |
| EA vs WM | 2 | 1.19 [0.99, 1.44] | .0621 | 69.6% |
| EA vs UC | 1 | 1.17 [0.93, 1.48] | .1730 | – |
| EA vs MA | 15 | 1.12 [1.08, 1.17] | <.0001 | 0% |
| WA vs MA | 5 | 1.13 [1.06, 1.20] | .0003 | 4.4% |
| WA vs EA | 2 | 1.14 [1.00, 1.31] | .0580 | 0% |
| FA vs MA | 2 | 1.28 [1.16, 1.42] | <.0001 | 0% |
| FA vs EA | 1 | 1.22 [0.98, 1.52] | .0788 | – |
| ACE vs MA | 7 | 1.12 [1.05, 1.20] | .0009 | 42.4% |
| ACE vs EA | 1 | 1.12 [0.93, 1.35] | .2335 | – |
ACE = acupoint catgut embedding, CI = confidence interval, EA = electroacupuncture, FA = fire acupuncture, MA = manual acupuncture, RR = relative risk, SA = sham acupuncture, UC = usual care, WA = warm acupuncture, WM = Western medicine.
3.5. Results of network meta-analysis
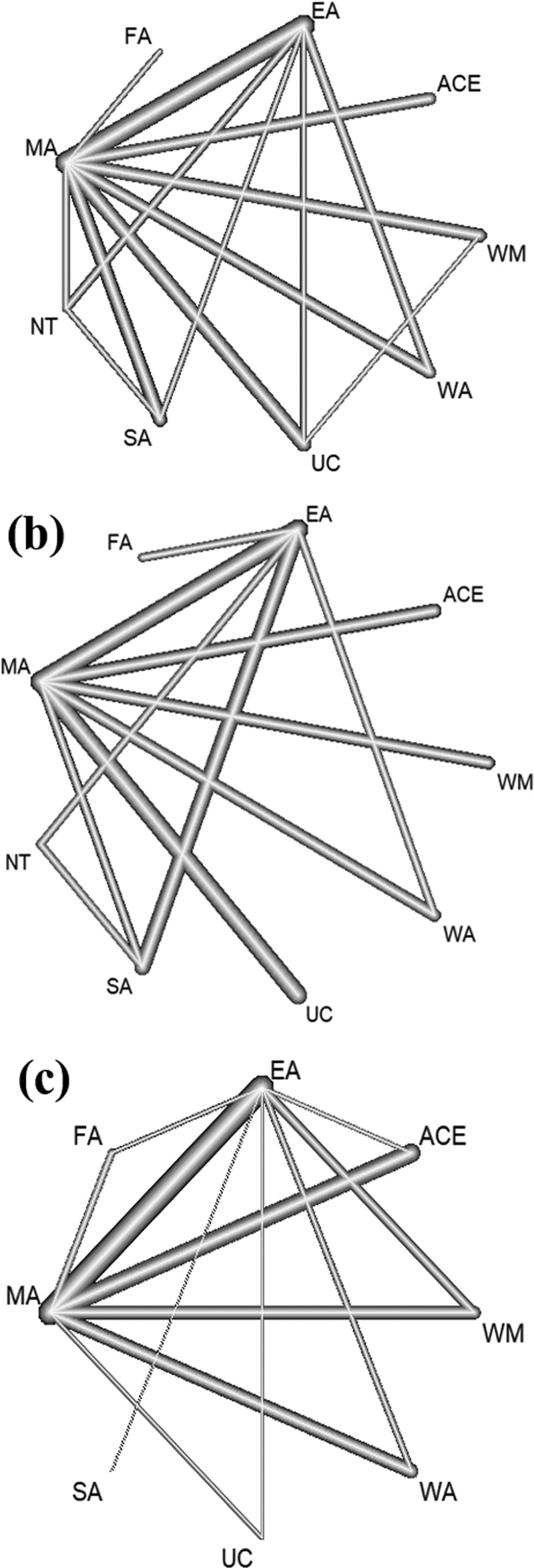
3.5.1. Network plot for different interventions.
In the network plot, the thickness of an edge represents the number of studies comparing 2 given interventions. Forty-two studies covering 9 interventions and 3158 participants with neck pain were included in the network meta-analysis for pain intensity (Fig. 4A). Pain-related disability was reported in 21 studies covering 9 interventions and 1581 participants (Fig. 4B), and the efficacy rate was reported in 40 studies covering 8 interventions and 3512 participants (Fig. 4C).
Figure 4.
Network plots for pain intensity (A), pain-related disability (B), and efficacy rate (C). ACE = acupoint catgut embedding, EA = electroacupuncture, FA = fire acupuncture, MA = manual acupuncture, NT = no treatment, SA = sham acupuncture, UC = usual care, WA = warm acupuncture, WM = Western medicine.
3.5.2. Evaluation of statistical inconsistency.
The results of the consistency tests for pain intensity, pain-related disability, and the efficacy rate did not show statistically significant heterogeneity (P = .6848, .2138, and .7169, respectively, and thus > 0.05 for all); therefore the consistency model was selected. All local inconsistency tests were performed with net-split analysis. The net-split analyses for pain intensity, pain-related disability, and the efficacy rate yielded P values > .05, indicating that there was no significant difference between direct and indirect effect estimates for any of the intervention comparisons.
3.5.3. Pain intensity.
A league table was established to compare effectiveness in relieving pain intensity among 9 interventions (Table 5). FA, WA, ACE, and EA more effectively lowered pain intensity than SA or UC, and MA was only more effective than SA (last row and third-to-last rows of Table 5, respectively). FA, WA, ACE, and EA significantly reduced pain intensity compared with NT (second-to-last row of Table 5). FA, WA, and EA had significantly better effects in reducing pain intensity compared with MA (fourth-to-last row of Table 5).
Table 5.
Network meta-analysis comparisons of effectiveness for reducing pain intensity.
| Fire acupuncture | ||||||||
|---|---|---|---|---|---|---|---|---|
| –0.70 (–2.43, 1.04) | Warm acupuncture | |||||||
| –1.07 (–2.88, 0.74) | –0.37 (–1.42, 0.67) | Acupoint catgut embedding | ||||||
| –1.16 (–2.83, 0.51) | –0.47 (–1.14, 0.20) | –0.09 (–1.02, 0.83) | Electroacupuncture | |||||
| –1.70 (–3.47, 0.07) | –1.00 (–1.98, –0.02) | –0.63 (–1.72, 0.47) | –0.53 (–1.38, 0.32) | Western medicine | ||||
| –1.76 (–3.37, –0.14) | –1.06 (–1.71, –0.41) | –0.69 (–1.50, 0.13) | –0.59 (–1.03, –0.15) | –0.06 (–0.79, 0.67) | Manual acupuncture | |||
| –2.34 (–4.07, –0.60) | –1.64 (–2.54, –0.74) | –1.27 (–2.31, –0.23) | –1.17 (–1.91, –0.43) | –0.64 (–1.56, 0.28) | –0.58 (–1.22, 0.06) | Usual care | ||
| –2.53 (–4.39, –0.66) | –1.83 (–2.93, –0.72) | –1.46 (–2.70, –0.22) | –1.36 (–2.32, –0.41) | –0.83 (–2.02, 0.36) | –0.77 (–1.71, 0.17) | –0.19 (–1.31, 0.94) | No treatment | |
| –2.62 (–4.37, –0.87) | –1.92 (–2.86, –0.99) | –1.55 (–2.62, –0.48) | –1.46 (–2.23, –0.68) | –0.92 (–1.93, 0.08) | –0.86 (–1.55, –0.17) | –0.28 (–1.22, 0.65) | –0.09 (–1.16, 0.98) | Sham acupuncture |
Bold and indicate that SMD < 0.00 is statistically significant.
The P score denotes the probability that 1 intervention is more effective than the others.[20] The network meta-analysis for pain intensity demonstrated the following ranking of P scores for the interventions: FA (P = .9397), WA (P = .8582), ACE (P = .7176), EA (P = .6845), WM (P = .4562), MA (P = .4260), UC (P = .1861), NT (P = .1368), and SA (P = .0947).
3.5.4. Pain-related disability.
For pain-related disability, the network meta-analysis involved data from 21 RCTs covering 9 interventions (Table 6). The results showed that FA, EA, and WA were more effective in lowering pain-related disability compared to UC (last row of Table 6). EA more effectively reduced disability compared to MA (second-to-last row of Table 6).
Table 6.
Network meta-analysis comparisons of effectiveness for reducing pain-related disability.
| Fire acupuncture | ||||||||
|---|---|---|---|---|---|---|---|---|
| –0.60 (–2.22, 1.02) | Electroacupuncture | |||||||
| –0.76 (–2.68, 1.16) | –0.16 (–1.19, 0.88) | Warm acupuncture | ||||||
| –1.14 (–3.26, 0.97) | –0.54 (–1.91, 0.83) | –0.38 (–1.91, 1.14) | Western medicine | |||||
| –1.35 (–3.43, 0.72) | –0.75 (–2.05, 0.55) | –0.59 (–2.05, 0.87) | –0.21 (–1.83, 1.41) | Acupoint catgut embedding | ||||
| –1.35 (–3.16, 0.47) | –0.75 (–1.57, 0.07) | –0.59 (–1.85, 0.67) | –0.20 (–1.72, 1.31) | 0.00 (–1.45, 1.46) | Sham acupuncture | |||
| –1.52 (–3.73, 0.69) | –0.91 (–2.42, 0.59) | –0.76 (–2.56, 1.05) | –0.37 (–2.38, 1.63) | –0.16 (–2.12, 1.79) | –0.17 (–1.67, 1.33) | No treatment | ||
| –1.68 (–3.44, 0.07) | –1.08 (–1.76, –0.40) | –0.92 (–1.88, 0.04) | –0.54 (–1.73, 0.65) | –0.33 (–1.44, 0.78) | –0.33 (–1.28, 0.61) | –0.17 (–1.78, 1.45) | Manual acupuncture | |
| –2.10 (–4.04, –0.16) | –1.49 (–2.56, –0.43) | –1.34 (–2.60, –0.07) | –0.95 (–2.40, 0.49) | –0.74 (–2.13, 0.64) | –0.75 (–2.00, 0.51) | –0.58 (–2.39, 1.23) | –0.41 (–1.24, 0.41) | Usual care |
Bold and indicate that SMD < 0.00 is statistically significant.
The network meta-analysis for pain-related disability showed the following ranking of P scores for the interventions: FA (P = .8867), EA (P = .7933), WA (P = .7050), WM (P = .5295), ACE (P = .4350), SA (P = .4263), NT (P = .3666), MA (P = .2535), and UC (P = .1042).
3.5.5. Efficacy rate.
Twelve RCTs covering 8 interventions reported on the efficacy rate (Table 7). FA, WA, ACE, and EA were significantly more effective compared to UC, WM, and MA alone (second-, third-, and fourth-to-last rows of Table 7, respectively). FA had a higher efficacy rate than EA or ACE (second and third rows of Table 7, respectively).
Table 7.
Network meta-analysis comparisons of efficacy rate.
| Fire acupuncture | |||||||
|---|---|---|---|---|---|---|---|
| 1.13 (0.99, 1.28) | Warm acupuncture | ||||||
| 1.16 (1.02, 1.31) | 1.03 (0.94, 1.12) | Acupoint catgut embedding | |||||
| 1.18 (1.05, 1.32) | 1.05 (0.97, 1.13) | 1.02 (0.95, 1.09) | Electroacupuncture | ||||
| 1.30 (1.16, 1.45) | 1.16 (1.08, 1.24) | 1.12 (1.06, 1.19) | 1.10 (1.06, 1.15) | Manual acupuncture | |||
| 1.37 (1.20, 1.55) | 1.21 (1.10, 1.33) | 1.18 (1.08, 1.29) | 1.16 (1.08, 1.24) | 1.05 (0.98, 1.12) | Western medicine | ||
| 1.43 (1.18, 1.73) | 1.27 (1.07, 1.51) | 1.23 (1.04, 1.46) | 1.21 (1.03, 1.42) | 1.10 (0.94, 1.29) | 1.04 (0.88, 1.24) | Usual care | |
| 1.72 (0.93, 3.20) | 1.53 (0.83, 2.83) | 1.49 (0.80, 2.75) | 1.46 (0.79, 2.69) | 1.32 (0.72, 2.44) | 1.26 (0.68, 2.33) | 1.21 (0.64, 2.27) | Sham acupuncture |
Bold and indicate that RR > 1.00 is statistically significant.
The network meta-analysis for efficacy rate demonstrated the following ranking of P scores for the interventions: FA (P = .9864), WA (P = .7951), ACE (P = .6961), EA (P = .6128), MA (P = .3725), WM (P = .2205), UC (P = .1678), and SA (P = .1489).
3.6. Safety
Overall, 24 RCTs including 1852 patients reported on the safety of interventions, as shown in Table 1. Thirteen RCTs showed no adverse events[26,30,38,43,45,53,62,64,68,69,71,72,76]; the 11 studies in which adverse events were observed included the interventions of MA, SA, WM, EA, ACE, and WA. Acupuncture most frequently caused minor subcutaneous bleeding or bruises at the acupuncture point. Soreness and discomfort at acupuncture points, sweating, low blood pressure, headache, dizziness, and chest pain were also reported. For WM, subcutaneous bruises were reported after injection.[42] These intervention-related adverse reactions were not serious and resolved without treatment.
3.7. Publication bias and sensitivity analysis
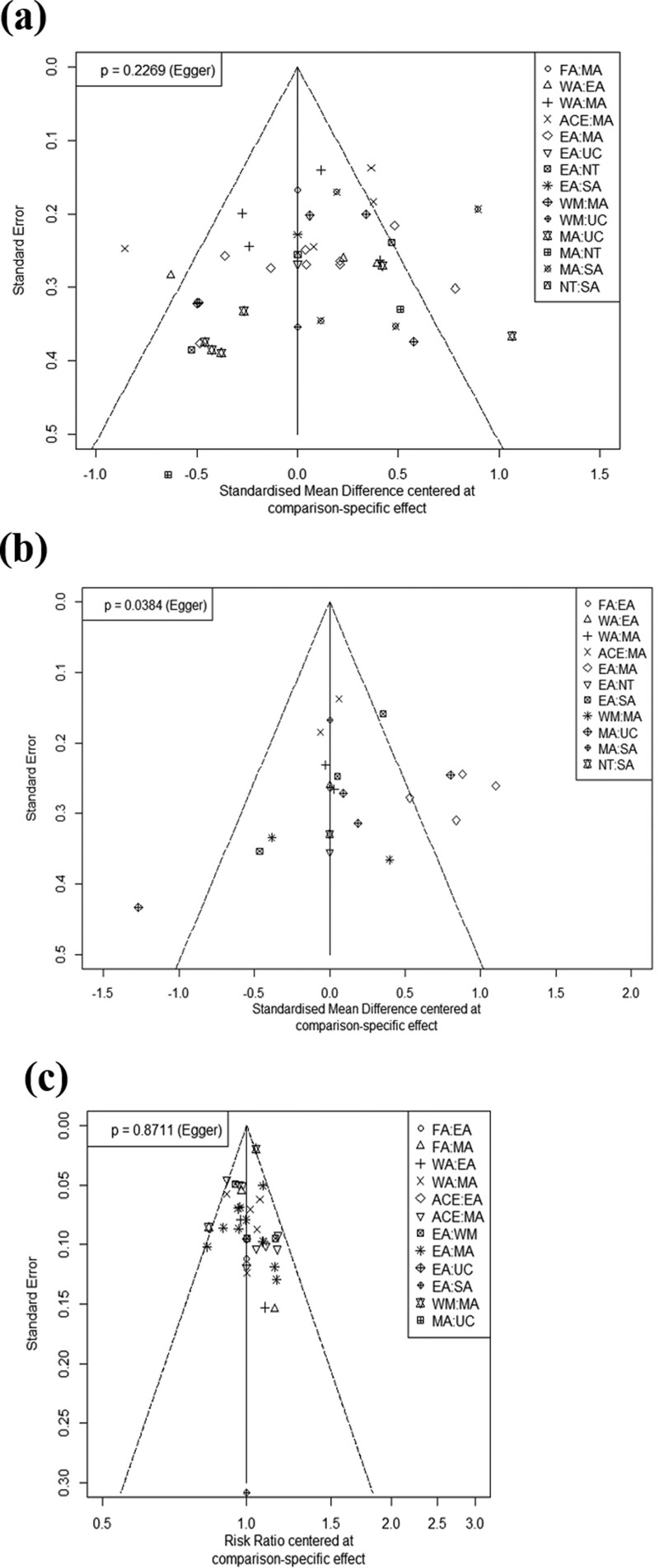
Funnel plots and the P value for the Egger test were used to visually inspect and assess the symmetry of network meta-analyses (Fig. 5). The funnel plot for the pain-related disability network was visually asymmetrical and the P value for its Egger test was < 0.05 (P = .0384), indicating the presence of potential publication bias. While the funnel plot and P value of the Egger test (P = .2269) demonstrated no strong evidence of publication bias across pain intensity, it revealed a scattered distribution that may be related to the obvious heterogeneity between studies.
Figure 5.
Funnel plots for the network meta-analysis of pain intensity (A), pain-related disability (B), and efficacy rate (C). ACE = acupoint catgut embedding, EA = electroacupuncture, FA = fire acupuncture, MA = manual acupuncture, NT = no treatment, SA = sham acupuncture, UC = usual care, WA = warm acupuncture, WM = Western medicine.
We conducted a sensitivity analysis by excluding 3 studies[31,42,43] that had 3 high-risk bias in risk of bias tool or had a very small-sample size (number per group < 10). This did not change the P-score ranking: FA had the highest P-score for reducing pain intensity (P = .9305), followed by WA (P = .8491), ACE (P = .6983), EA (P = .6697), WM (P = .5091), MA (P = .3984), UC (P = .1892), NT (P = .1716), and SA (P = .0841).
3.8. GRADE assessment
The GRADE approach was used to evaluate study limitations, inconsistency, indirectness, imprecision, and publication bias. Overall, the certainty of the evidence for pain intensity, pain-related disability, and efficacy rate was “very low,” “very low,” and “low,” respectively. This reflected that most of the included studies had high risk of bias and serious imprecisions (see Appendix S2–S4, Supplemental Digital Content, http://links.lww.com/MD/G898, which show details on the GRADE assessment for all pairwise comparisons).
4. Discussion
Numerous studies have assessed the efficacy and safety of acupuncture for treating neck pain, but the literature has lacked a direct comparison of RCTs between different acupuncture methods. This has limited the ability of clinicians to choose the best treatment from empirical information. Here, we used the network meta-analysis method to compare and rank different types of acupuncture for their ability to reduce pain intensity and pain-related disability, as well as their efficacy rate for treatment of neck pain.
In this SR and network meta-analysis, we combined direct and indirect evidence from 65 studies covering 5266 participants with neck pain. We compared the effectiveness of different acupuncture options by assessing pain intensity, pain-related disability, and the efficacy rate. Our network meta-analyses showed that FA, WA, ACE, and EA were more effective in relieving neck pain intensity compared to UC and SA; MA reduced pain intensity more than SA alone; and FA, WA, and EA reduced pain intensity more than MA. In terms of reducing pain-related disability, FA, EA, and WA were more effective than UC, and EA was superior to MA. In terms of the efficacy rate, FA, EA, ACE, and EA outperformed MA, WM, and UC; and FA was more effective than ACE and EA. Consequently, in terms of the efficacy rate and the ability to reduce overall symptoms, FA, EA, and WA were more effective than UC; and EA was more effective than MA.
In our 3 network meta-analyses, FA, WA, ACE, and EA generally had high rankings; there was no significant difference between them, probably due to the small number of direct comparisons. Among them, FA was considered to be the best performing option in terms of symptom relief and efficacy rate of neck pain treatment. Several studies[89,90] have suggested that FA can trigger the rapid absorption of inflammatory factors (e.g., interleukin [IL]-1, IL-6, IL-1β, and tumor necrosis factor-α) in the diseased area through the surrounding lymphoid tissue and may control the central nervous system. This could account for the ability of FA to reduce neck-pain intensity and neck-pain-related disability.
Since the number of the included studies performed FA, WA, or ACE was <10, and these studies were assessed as being of low quality due to the presence of several bias risks, the effect size of each intervention was overestimated comparing with direct comparisons. Nevertheless, the differences in the relative effects between interventions were acceptable, and the estimated effect size should not be taken, as it was in interpreting the results of this study.
While MA was effective in reducing pain intensity compared to SA, it was ranked lower than SA for decreasing pain-related disability and was not significantly different in terms of the efficacy rate. These results contradict several previous reviews.[13,14,91] Unlike the previous reviews; however, we included only SA designed with nonpenetrating acupuncture, resulting in insufficient direct comparison of SA and other acupuncture. Several types of SA were excluded in this study, such as the use of penetrating needles at locations away from true acupuncture points and the superficial insertion of needles. One review on the impact of SA in patients with pain found that the shallow insertion of needles at nonacupuncture points could have therapeutic activity for pain, albeit less effective than that obtained by deep insertion at a correct location.[92] MacPherson et al suggested that there was no significant difference between shallow and deep needling when considering changes in fMRI.[93] In addition, since shallow penetrating acupuncture (e.g., that with an intradermal needle) is already used as a treatment method, noninvasive SA was recently recommended as a sham control in RCT.[92,94]
While 24 of the 65 included studies reported on the safety of interventions, there was no report of safety related to FA and only 1 study related to ACE, which ranked high in our network meta-analyses. FA is used to treat lateral epicondylitis,[95] knee osteoarthritis,[96] and ankle sprain,[97] and may cause pain, burns, and skin rash due to a red-hot needle. There were few reports of adverse events to the FA in the previous studies,[95–97] and Yeon et al[98] reported that after FA, local third-degree burns were observed in the muscle and skin layers without any scarring, and the residual products present after FA did not exert toxicity, but rather increased cell growth. ACE has been used for the treatment of musculoskeletal pain, obesity, and facial palsy in Korea, China, and Taiwan.[99] One review[100] on the safety of ACE reported that the most common adverse events were induration, bleeding, fever, redness, and swelling, all of which disappeared without special treatment. Furthermore, the incidence of serious adverse events was 0.1%, which had no clear causal relationship with ACE. The evidence suggests that FA and ACE are safe treatment methods, but it is difficult to draw a clear conclusion on safety due to the small number of studies included. Thus, the safety of FA and ACE should be carefully assessed in further trials.
The present study has the following limitations. First, because of poor reporting, most of the included RCTs were considered to have an unclear risk of bias in their allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. In addition, the sequences of 9 studies were randomly ordered based on the date of admission or visit, resulting in high risks of selection bias. Overall, the certainty of evidence obtained in our network meta-analyses was very low, largely because most of the included studies had considerable risks for bias and imprecision. Thus, further high-quality and larger-scale studies are needed. Second, it was difficult to assess the long-term effects of the interventions, as the studies varied in their follow-up periods. Third, we observed publication bias in our network meta-analysis of pain-related disability. Fourth, factors such as the selection of acupuncture points and variances in treatment methods (e.g., the numbers, frequencies, durations, and/or intervals of treatments) contributed to the high heterogeneity of our analyses. Despite these limitations, this study is the first network meta-analysis of RCTs to evaluate and rank the comparative effectiveness of various interventions for treating neck pain. More precisely designed, generated, and published RCTs are highly recommended.
5. Conclusion
The findings of our network meta-analyses indicate that FA, WA, ACE, and EA were more effective in relieving pain intensity and had higher efficacy rates than the other interventions (UC, SA, NT). We also show that FA, EA, and WA were more effective than MA in pain intensity mitigation and the efficacy rate, and that EA reduced pain-related disability more effectively than MA. Overall, FA was found to be the best acupuncture method to reduce pain and disability index scores, while showing a high efficacy rate. However, higher-quality head-to-head trials comparing acupuncture therapies for treating neck pain are needed to confirm this conclusion. The findings of this review should be interpreted with caution given the low certainty of the evidence included in the 3 network meta-analyses.
Author contributions
Conceptualization: Hyo-Rim Jo, Eun-Ji Noh, Se-Hee Oh; Data curation: Su-Ji Choi: Formal analysis: Eun-Ji Noh, Seung-Ug Hong; Funding acquisition: Eun-Jung Kim; Methodology: Hyo-Rim Jo, Eun-Ji Noh, Se-Hee Oh; Project administration: Dong-Il Kim, Seung-Ug Hong; Supervision: Eun-Jung Kim; Writing–original draft: Hyo-Rim Jo; Writing–review&editing: Seong-Kyeong Choi, Won-Suk Sung, Eun-Jung Kim.
Supplementary Material
Abbreviations:
- 95% CI =
- 95% confidence interval
- ACE =
- acupoint catgut embedding
- EA =
- electroacupuncture
- FA =
- fire acupuncture
- GRADE =
- Grading of Recommendations Assessment, Development and Evaluation
- IL =
- interleukin
- MA =
- manual acupuncture
- NDI =
- Neck Disability Index
- NPQ =
- Neck Pain Questionnaire
- NRS =
- Numeric Rating Scale
- NT =
- no treatment
- PRISMA =
- Preferred Reporting Items for Systematic Reviews and Meta-analyses
- RCT =
- randomized controlled trial
- RR =
- relative risk
- SA =
- sham acupuncture
- SMD =
- standardized mean difference
- SR =
- systematic review
- SUCRA =
- cumulative ranking under the surface curve
- UC =
- usual care
- VAS =
- Visual Analog Scale
- WA =
- warm acupuncture
- WM =
- western medicine
How to cite this article: Jo H-R, Noh E-J, Oh S-H, Choi S-K, Sung W-S, Choi S-J, Kim D-I, Hong S-U, Kim E-J. Comparative effectiveness of different acupuncture therapies for neck pain. Medicine 2022;101:33(e29656).
Data and material from this trial are available upon reasonable request and approval by the corresponding author.
The authors have no funding and conflicts of interest to disclose.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number HI19C0142, HF20C0210).
Supplemental Digital Content is available for this article.
Contributor Information
Hyo-Rim Jo, Email: sunny4396@hanmail.net.
Eun-Ji Noh, Email: wldmssh@naver.com.
Se-Hee Oh, Email: sherlene1207@naver.com.
Seong-Kyeong Choi, Email: stomatok13@naver.com.
Won-Suk Sung, Email: 1984sws@hanmail.net.
Su-Ji Choi, Email: stomatok13@naver.com.
Dong-Il Kim, Email: hanijjung@naver.com.
Seung-Ug Hong, Email: heenthsu@dumc.or.kr.
References
- [1].Guzman J, Hurwitz EL, Carroll LJ, et al. A new conceptual model of neck pain: linking onset, course, and care: the bone and joint decade 2000-2010 task force on neck pain and its associated disorders. Spine. 2008;33:S14–23. [DOI] [PubMed] [Google Scholar]
- [2].Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2017;47:A1–A83. [Google Scholar]
- [3].Wang WT, Olson SL, Campbell AH, et al. Effectiveness of physical therapy for patients with neck pain: an individualized approach using a clinical decision-making algorithm. Am J Phys Med Rehabil. 2003;82:203–18. [DOI] [PubMed] [Google Scholar]
- [4].Peloso P, Gross A, Haines T, et al. Cervical Overview Group. Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev. 2007;CD0000319. [DOI] [PubMed] [Google Scholar]
- [5].Childress MA, Becker BA. Nonoperative management of cervical radiculopathy. Am Fam Physician. 2016;93:746–54. [PubMed] [Google Scholar]
- [6].White AP, Arnold PM, Norvell DC, et al. Pharmacologic management of chronic low back pain: synthesis of the evidence. Spine. 2011;36:S131–43. [DOI] [PubMed] [Google Scholar]
- [7].Chu HR, Hu J, Sun K, et al. Clinical practice guidelines of acupuncture-moxibustion for cervical spondylotic radiculopathy. World J Acupunct Moxibust. 2017;27:3–11. [Google Scholar]
- [8].Kjaer P, Kongsted A, Hartvigsen J, et al. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur Spine J. 2017;26:2242–57. [DOI] [PubMed] [Google Scholar]
- [9].Nahn RL, Barnes PM, Stussman BA. Expenditures on complementary health approaches: United States, 2012. Natl Health Stat Rep. 2016;95:1–11. [PubMed] [Google Scholar]
- [10].Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- [11].Lee YJ, Kim MR, Lee EJ, et al. An evidence-based approach for the development of a clinical practice guideline for the treatment of neck pain using traditional Korean medicine. Eur J Integr Med. 2021;44:e101337. [Google Scholar]
- [12].Seo SY, Lee KB, Shin JS, et al. Effectiveness of acupuncture and electroacupuncture for chronic neck pain: a systematic review and meta-analysis. Am J Chin Med. 2017;45:1573–95. [DOI] [PubMed] [Google Scholar]
- [13].Trinh KV, Graham N, Gross AR, et al. Acupuncture for neck disorders. Cochrane Database Syst Rev. 2006;CD004870. [DOI] [PubMed] [Google Scholar]
- [14].Yuan QL, Guo TM, Liu L, et al. Traditional Chinese medicine for neck pain and low back pain: a systematic review and meta-analysis. PLoS One. 2015;10:e0117146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fu LM, Li JT, Wu WS. Randomized controlled trials of acupuncture for neck pain: systematic review and meta-analysis. J Altern Complement Med. 2009;15:133–45. [DOI] [PubMed] [Google Scholar]
- [16].Seide SE, Jensen K, Kieser M. A comparison of Bayesian and frequentist methods in random-effects network meta-analysis of binary data. Res Synth Methods. 2020;11:363–78. [DOI] [PubMed] [Google Scholar]
- [17].Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jo HR, Noh EJ, Oh SH. The effectiveness of different acupuncture therapies for neck pain: A protocol for systematic review and/or network meta-analysis. Medicine. 2021;100:e25379e25379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Salanti G, Del Giovane C, Chaimani A, et al. Evaluating the quality of evidence from a network meta-analysis. PLoS One. 2014;9:e99682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011;64:1303–10. [DOI] [PubMed] [Google Scholar]
- [23].Puhan MA, Schünemann HJ, Murad MH, et al. A grade working group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. [DOI] [PubMed] [Google Scholar]
- [24].Raeissadat SA, Rayegani SM, Sadeghi F, et al. Comparison of ozone and lidocaine injection efficacy vs dry needling in myofascial pain syndrome patients. J Pain Res. 2018;11:1273–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Tabatabaiee A, Ebrahimi-Takamjani I, Ahmadi A, et al. Comparison of pressure release, phonophoresis and dry needling in treatment of latent myofascial trigger point of upper Trapezius muscle. J Back Musculoskelet Rehabil. 2019;32:587–94. [DOI] [PubMed] [Google Scholar]
- [26].Nejati P, Mousavi R, Angoorani H. Acupuncture is as effective as exercise for improvement of chronic neck pain: a Randomized Clinical Trial. Shiraz E-Med J. 2021;22:e97497. [Google Scholar]
- [27].Ziaeifar M, Arab AM, Mosallanezhad Z, et al. Dry needling versus trigger point compression of the upper trapezius: a randomized clinical trial with two-week and three-month follow-up. J Man Manip Ther. 2019;27:152–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ziaeifar M, Arab AM, Nourbakhsh MR. Clinical effectiveness of dry needling immediately after application on myofascial trigger point in upper trapezius muscle. J Chiropr Med. 2016;15:252–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ziaeifar M, Arab AM, Karimi N, et al. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014;18:298–305. [DOI] [PubMed] [Google Scholar]
- [30].Arias-Buría JL, Monroy-Acevedo A, Fernández-de-Las-Peñas C, et al. Effects of dry needling of active trigger points in the scalene muscles in individuals with mechanical neck pain: a randomized clinical trial. Acupunct Med. 2020;38:380–7. [DOI] [PubMed] [Google Scholar]
- [31].Mejuto-Vázquez MJ, Salom-Moreno J, Ortega-Santiago R, et al. Short-term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44:252–60. [DOI] [PubMed] [Google Scholar]
- [32].Garcia-de-Miguel S, Pecos-Martin D, Larroca-Sanz T, et al. Short-term effects of pens versus dry needling in subjects with unilateral mechanical neck pain and active myofascial trigger points in levator scapulae muscle: a randomized controlled trial. J Clin Med 2020;9:1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Tekin L, Akarsu S, Durmuş O, et al. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol. 2013;32:309–15. [DOI] [PubMed] [Google Scholar]
- [34].Hayta E, Umdu NM. A randomized trial to study the comparison of trigger point dry needling versus kinesio taping technique in myofascial pain syndrome during a 3-month follow up. Int J Physiother. 2016;3:540–6. [Google Scholar]
- [35].Chou LW, Hsieh YL, Chen HS, et al. Remote therapeutic effectiveness of acupuncture in treating myofascial trigger point of the upper trapezius muscle. Am J Phys Med Rehabil. 2011;90:1036–49. [DOI] [PubMed] [Google Scholar]
- [36].Nabeta T, Kawakita K. Relief of chronic neck and shoulder pain by manual acupuncture to tender points—a sham-controlled randomized trial. Complement Ther Med. 2002;10:217–22. [DOI] [PubMed] [Google Scholar]
- [37].Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 2001;322:1574–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Cho JH, Nam DH, Kim KT, et al. Acupuncture with non-steroidal anti-inflammatory drugs (NSAIDs) versus acupuncture or NSAIDs alone for the treatment of chronic neck pain: an assessor-blinded randomised controlled pilot study. Acupunct Med. 2014;32:17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].De Meulemeester KE, Castelein B, Coppieters I, et al. Comparing trigger point dry needling and manual pressure technique for the management of myofascial neck/shoulder pain: a randomized clinical trial. J Manipulative Physiol Ther. 2017;40:11–20. [DOI] [PubMed] [Google Scholar]
- [40].Chen L, Deng H, Houle T, et al. A randomized trial to assess the immediate impact of acupuncture on quantitative sensory testing, pain, and functional status. Pain. 2019;160:2456–63. [DOI] [PubMed] [Google Scholar]
- [41].Ho LF, Lin ZX, Leung AWN, et al. Efficacy of abdominal acupuncture for neck pain: a randomized controlled trial. PLoS One. 2017;12:e0181360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Wang CM, Chen HW, Wang YW, et al. Therapeutic observation of acupuncture at myofascial trigger points for cervical spondylosis of vertebral artery type. Shanghai J Acupuncture Moxibustion. 2015;34:48–50. [Google Scholar]
- [43].Fu WB, Zhang HL, Zhu XP, et al. Randomized controlled study on picking therapy for treatment of cervical spondylosis. Chin Acupuncture Moxibustion. 2005;25:607–9. [PubMed] [Google Scholar]
- [44].Fu HL, Qu SS, Chen JQ, et al. A clinical randomized controlled study on the curative effect of abdominal acupuncture combined with Mckenzie therapy in the treatment of cervical spondylopathy. J Practical Med. 2013;29:650–2. [Google Scholar]
- [45].Cui QS. A contrastive study of EA and sham EA for neck pain of cervical spondylosis (Masters dissertation) . Guangdong Province, China: Guangzhou University of Chinese Medicine, 2016. [Google Scholar]
- [46].Feng X. Placebo effect of electrical acupuncture in chronic neck pain: a randomized clinical trial (Masters dissertation). Guangdong Province, China: Guangzhou University of Chinese Medicine, 2014. [Google Scholar]
- [47].Zhang SP, Chiu TT, Chiu SN. Long-term efficacy of electroacupuncture for chronic neck pain: a randomised controlled trial. Hong Kong Med J. 2013;19(Suppl 9):36–9. [PubMed] [Google Scholar]
- [48].Li JP. Electro-acupuncture treatment of cervical disease in clinical research. J Liaoning University Tradit Chin Med. 2008;10:124–5. [Google Scholar]
- [49].Yan SM. Observation on the short-term and long-term curative effect of electric acupuncture on 78 cases of cervical spondylotic radiculopathy. Fujian J Traditi Chin Med. 2006;37:35. [Google Scholar]
- [50].Diethelm P. Clinical study of acupuncture treatment of chronic recurrent nonspecific cervical disease with kinesio-taping (Doctoral thesis) . Shandong Province, China: Shandong University of Traditional Chinese Medicine, 2014. [Google Scholar]
- [51].Yang DD. Clinical observation on the changes of serum IL-6 in patients with cervical n spondylotic radiculopathy by short acupuncture combined with electroacupuncture (Masters dissertation) . Jiangsu Province, China: Nanjing University of Traditional Chinese Medicine, 2020. [Google Scholar]
- [52].Huang W, Jiang A. Effects on cervical spondylosis of neck type treated with Hegu needling and Shu needling techniques at the positive reaction points. Zhongguo Zhen Jiu 2018;38:1157–60. [DOI] [PubMed] [Google Scholar]
- [53].Chen YR. Clinical observation of the therapeutic effect of electro-acupuncture with abdominal acupuncture in treating cervical spondylosis of nerve root type (Masters dissertation). Guangdong Province, China: Guangzhou University of Chinese Medicine, 2016. [Google Scholar]
- [54].Chen GL. The Clinical efficacy observation on electroacupuncture at cervical jiaji points for neck type of cervical spondylosis (Masters dissertation). Heilongjiang Province, China: Heilongjiang University of Traditional Chinese Medicine, 2016. [Google Scholar]
- [55].Tian HZ, Sun ZR, Zhang QH. Observation of therapeutic effect on cervical Jiaji electroacupuncture treatment of nerve root type cervical spondylosis. J Emerg Traditi Chin Med. 2015;24:1050–2. [Google Scholar]
- [56].Chen L, Jiang W, Guan XF, et al. Clinical efficacy of Fangshi scalp acupuncture for treating cervical spondylotic. Shijie Zhong Yi Yao. 2015;10:1768–70. [Google Scholar]
- [57].Liu XF. Clinical observation of nerve root type cervical spondylosis treatment EA jiaji. Heilongjiang: Heilongjiang University of Chinese Medicine. 2014. [Google Scholar]
- [58].Jin DS. Clinical observation on treatment of cervical spondylotic radiculopathy by electro-acupuncture. Nanjing: Nanjing University of Chinese Medicine. 2013. [Google Scholar]
- [59].Zhang CP. Observation on therapeutic effect of electric nape acupuncture on cervical spondylopathy. Qiu Yi Wen Yao. 2011;9:530. [Google Scholar]
- [60].Yang XB, Ou YK, An JM. Electroacupuncture for 36 cases of nerve root cervical spondylopathy. Zhongyi Wai Zhi Za Zhi. 2011;21:30–1. [Google Scholar]
- [61].Ji BJ, Zhou ZQ, Huang MJ. The efficacy of different waveforms of electrical acupuncture on neck pain of cervical spondylosis. Baojian Yi Xue Yan Jiu Yu Shi Jian. 2015;12:39–43. [Google Scholar]
- [62].Wang WX. Clinical research on cervical spondylopathy and neck pain treating with electro-acupuncture, acupuncture. Guangzhou: Guangzhou University of Chinese Medicine, 2010. [Google Scholar]
- [63].Liu SL. Clinical study on treatment of cervical spondylosis of nerve-root type by electroacupuncture at jiaji point. Heilongjiang: Heilongjiang University of Chinese Medicine, 2010. [Google Scholar]
- [64].Lai RX. Clinical study of treating cervical spondylotic radiculopathy with electric needle acupuncture. Guangzhou: Guangzhou University of Chinese Medicine, 2010. [Google Scholar]
- [65].Yang YZ, Wang C. Evaluation of therapeutic effect of electroacupuncture on nerve root cervical spondylopathy. Zhong Yi Yao Xin Xi. 2009;26:69. [Google Scholar]
- [66].Ding ZG. Clinical research of electro-acupuncture of jiaji points on cervicalspondylotic radiculopathy. Nanjing: Nanjing University of Chinese Medicine. 2009. [Google Scholar]
- [67].Yu ZG. Clinical study on treatment of cervical spondylosis of nerve-root type by electroacupuncture at jiaji point. Heilongjiang: Heilongjiang University of Chinese Medicine. 2007. [Google Scholar]
- [68].Chen JB, Zheng JL, Wu XQ. Clinical study on treatment of cervical cervical spondylosis with warm needling at bamai jiaohui points. Shi Yong Zhong Yi Neike Za Zhi. 2020;34:76–9. [Google Scholar]
- [69].Ju D, Cheng WQ. Efficacy of silver needle with heat conduction therapy on cervical spondylotic radiculopathy. . Zhongyi Lin Chuang Yan Jiu. 2019;11:121–3. [Google Scholar]
- [70].Xu JF. Effects of warm acupuncture at jiaji points on nerve root type cervical spondylosis. . Zhong Yi Lin Chuang Yan Jiu. 2017;32:89–90. [Google Scholar]
- [71].Guo DD. Clinical Study on Cervicodynia of Cervical-type Cervical Spondylopathy with Electronic Wam needle. Guangzhou: Guangzhou University of Chinese Medicine. 2015. [Google Scholar]
- [72].Zhou JF, Li XW, Zhao JC, et al. Treatment of 30 patients with cervical spondylotic radiculopathy by acupuncture plus warming-needle. Shijie Zhen Jiu Za Zhi. 2014;24:24–8. [Google Scholar]
- [73].Lin ZX. Clinical study on electrothermal acupuncture treatment of cervical spondylopathy of nerve root type. Beijing: Beijing University of Chinese Medicine. 2012. [Google Scholar]
- [74].Garov Y. The effectiveness and safety of electro-acupuncture and warm acupuncture for the treatment of cervical spondylotic radiculopathy. Nanjing: Nanjing University of Chinese Medicine. 2016. [Google Scholar]
- [75].Su CX, Lin F, Jiang ZL. Therapeutic observation of warm needling for neck-back myofascial pain syndrome. Shang Hai Zhen Jiu Za Zhi. 2015;34:1102–5. [Google Scholar]
- [76].Lin JS. Clinical observation on warm needle moxibustion for the treatment of the cervical spondylopathy. Guangzhou: Guangzhou University of Chinese Medicine. 2012. [Google Scholar]
- [77].Qui C, Zhang ZQ. Observation on curative effect of fire needle on nerve root cervical spondylopathy. Si Chuan Zhongyi. 2015;12:173–4. [Google Scholar]
- [78].Sun YJ, Wu YC, Zhang JF, et al. Therapeutic observation of LU’s heat-producing needling (Shao Shan Huo) for cervical spondylotic radiculopathy. Shang Hai Zhen Jiu Za Zhi. 2015;34:234–6. [Google Scholar]
- [79].Zhao MH. The study of fire-needle therapy on the cervical type cervical spondylosis. Guangzhou: Guangzhou University of Chinese Medicine. 2013. [Google Scholar]
- [80].Cheng SZ. Clinical observation on the treatment of nerve root cervical spondylopathy by catgut embedding at acupoints of five elements and eight diagrams (Hou Tian) at the umbilical. . Shi Yong Zhong Yi Yao Za Zhi. 2018;34:1114–5. [Google Scholar]
- [81].Qui C, Zhao CX, Wang TT, et al. Study on the clinical effect of catgut embedding at positive acupoints in the treatment of cervical spondylotic radiculopathy. Ha Bei Zhong Yi Yao Xue Bao. 2015;30:55–7. [Google Scholar]
- [82].Wang H, Sun WS, Wang YM, et al. Clinical observations on microinvasive thread embedding for the treatment of neck pain due to cercical spondylosis. Shang Hai Zhen Jiu Za Zhi. 2016;35:1494–6. [Google Scholar]
- [83].Li RQ, Wang BJ, Sun LX, et al. Observation on therapeutic effect of catgut embedding at acupoints on nerve root cervical spondylopathy. Xian Dai Zhong Xi Yi Jie He Za Zhi. 2015;24:3685–7. [Google Scholar]
- [84].Zhao Z, Zhao XX. Clinical research of catgut embedding and acupuncture treatment for cervical spondylosis. Zhong Yi Xue Bao. 2015;30:449. [Google Scholar]
- [85].Ding M, Jiang YQ, Feng H, et al. Therapeutic observation on micro-invasive thread-embedding therapy for cervical spondylosis of nerve root type. Shang Hai Zhen Jiu Za Zhi. 2012;31:900–1. [Google Scholar]
- [86].Feng H, Ding M, Jiang YQ, et al. Study on the efficacy and safety of minimally invasive thread embedding therapy in the treatment of nerve root cervical spondylopathy. Jiang Su Zhong Yi Yao. 2012;44:59–60. [Google Scholar]
- [87].Xian YD. Clinical research of cervical spondylotic radiculopathy with acupoint catgut embedding therapy. Guangzhou: Guangzhou University of Chinese Medicine. 2012. [Google Scholar]
- [88].Zou HH. Clinical research of cervical spondylotic radiculopathy with acupoint catgut embedding therapy. Guangzhou: Guangzhou University of Chinese Medicine. 2016. [Google Scholar]
- [89].Huang CJ, Huang YJ, Chen CY. The origin and development of fire. Chin Acupunctue Moxibustion. 2013;33:455–8. [PubMed] [Google Scholar]
- [90].Zhang XX, Wu ZH, Dong MX. Preliminary study on curing mechanism of fire needle therapy. Beijing J Trad Chin Med. 2007;2007:576–8. [Google Scholar]
- [91].Navarro-Santana MJ, Sanchez-Infante J, Fernández-de-Las-Peñas C, et al. effectiveness of dry needling for myofascial trigger points associated with neck pain symptoms: an updated systematic review and meta-analysis. J Clin Med. 2020;9:3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].MacPherson H, Vertosick E, Lewith G, et al. Influence of control group on effect size in trials of acupuncture for chronic pain: a secondary analysis of an individual patient data meta-analysis. PLoS One. 2014;9:e93739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].MacPherson H, Green G, Nevado A, et al. Brain imaging of acupuncture: comparing superficial with deep needling. Neurosci Lett. 2008;434:144–9. [DOI] [PubMed] [Google Scholar]
- [94].Jang JY, Kim SJ, Kim NS, et al. Review of analysis of sham acupuncture in acupuncture clinical trials. J Acupunct Res. 2011;28:29–38. [Google Scholar]
- [95].Wu SY, Lu CN, Chung CJ, et al. Therapeutic effects of acupuncture plus fire needle versus acupuncture alone in lateral epicondylitis: a randomized case-control pilot study. Medicine (Baltim). 2019;98:e15937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Ko HJ, Yoo JH, Shin JC. A systematic review and meta-analysis of fire needling treatment for knee osteoarthritis: focused on comparative studies with manual acupuncture treatment during recent five years. Korean J Acupuncture. 2019;36:104–14. [Google Scholar]
- [97].Ko HJ, Yoo JH, Kim MW, et al. Systematic review of fire needling or warm needling treatment for ankle sprain. Acupunct Res. 2020;37:19–27. [Google Scholar]
- [98].Yeon SH, Lee SB, Kwon OS, et al. The safety assessment of fire needling. Korean J Oriental Med. 2012;18:103–10. [Google Scholar]
- [99].Cho Y, Lee S, Kim J, et al. Thread embedding acupuncture for musculoskeletal pain: a systematic review and meta-analysis protocol. BMJ Open. 2018;8:e015461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Huang JJ, Liang JQ, Xu XK, et al. Safety of thread embedding acupuncture therapy: a systematic review. Chin J Integr Med. 2021;27:947–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.