Abstract
Background
Resident training in emergency airway management is not well described. We quantified training and exposure to airway emergencies among graduating Otolaryngology-Head and Neck Surgery and Anesthesiology residents.
Methods
A national, web-based, survey of chief residents.
Results
The response rate was 52% (Otolaryngology) and 60% (Anesthesiology). More Otolaryngology residents rotated on Anesthesiology, than Anesthesia residents on Otolaryngology (33% vs. 8%). More Anesthesiology chiefs never performed an emergency surgical airway than Otolaryngology (92% vs. 18%). The most common self-rating of competency was “9”, with 82% overall self-rating "8" or higher (10= ”totally competent”).
Conclusions
Otolaryngology and Anesthesiology emergency airway management experience/training is heterogeneous and non-standardized. Many chief residents graduate with little exposure to airway emergencies, especially surgical airways. Resident confidence levels are high despite minimal experience. This high confidence–low experience dichotomy may reflect novice overconfidence and suggests the need for improved training methods.
Keywords: airway, emergency trachesotomy, training, medical education, survey
INTRODUCTION
In-hospital airway emergencies are complex events that involve the interplay of the patient, healthcare personnel, training, skill, equipment, and systems management issues under time pressure. These situations present a clinical challenge for otolaryngologists, who are often called to the bedside when other physicians are unable to secure an airway. Problems that can result from airway emergencies include permanent and serious injury and death. They also create challenges for health care organizations, including increased length of hospital stay, cost, liability, and implications for quality of care. For example, respiratory difficulties are the most common source of malpractice claims for Anesthesiology1 and airway issues play a role in 30% of all anesthesia-related deaths.2 Furthermore, a self-reporting system found 10% of intensive care unit (ICU) adverse events were airway-related; half of these were judged to be preventable.3
In the Otolaryngology-Head and Neck Surgery literature there is little written regarding training in this area. In contrast, this topic is covered in greater depth in the Anesthesiology and Critical Care,4 and Emergency Medicine5 literature, albeit from different perspectives.6 Although evaluation and management of the airway is integral to Otolaryngology, it is so integrated into practice that it is often not specifically codified. In the traditional apprenticeship model, it is often assumed that there is ample exposure to airway management during a five year Otolaryngology residency.
With changing AGCME residency requirements that core competencies of training be quantified and measured, we wondered how emergency airway management is currently taught to Otolaryngology and Anesthesiology residents. We sought to determine existing methods of emergency airway management training, quantify the residents’ experiences and assess their confidence in this clinical sphere. We hypothesized that different training methods and clinical experiences in Otolaryngology and Anesthesiology affect residents’ confidence, and we expected that their experiences would correlate directly with their self-assessed competence in managing emergency airways.
MATERIALS & METHODS
Survey Methodology
We used an anonymous web-based survey system7 to query chief residents in all Otolaryngology and Anesthesiology training programs in the U.S. We contacted the office of residency program directors and requested e-mail addresses for their chief residents. E-mails were sent directly to these residents inviting them to take the survey. Subjects could opt out and receive no further communication from us. Non-responders were re-contacted at two-week intervals up to a total of three times. The survey software anonymously tracked and separated respondents, non-responders, and those who opted out. We calculated response rates as the percentage of surveys sent out that were returned.
Survey questions concerned formal training, participation in actual airway emergencies, and self-assessment of training experiences and competence in handling airway emergencies (Appendix A, available online). The following definition of an “airway emergency” was provided in the survey for reference: “An ‘Airway Emergency’ is defined as a ‘cannot intubate, cannot ventilate’ situation OR a situation where multiple attempts to secure the airway have failed and it is becoming difficult to maintain oxygenation and ventilation.” Approval from the Institutional Review Board was obtained via waiver.
Statistical Analysis
Survey data was analyzed using SPSS software (SPSS, Inc., Chicago, IL). Responses from Otolaryngology and Anesthesiology residents were analyzed separately and compared with each other to determine differences between the specialties. Questions regarding the number of actual airway emergencies and surgical airways performed gave the respondents a range from which to choose (ie: “1–2,” “3–5,” etc; see Appendix A). Therefore, numerical data on airway emergency participation and surgical airway performance is presented as the median of reported ranges. Continuous variables were assessed using the Student’s t-test, and binary variables were compared with the Chi-square test. We used ordered logistic regression analysis to find significant correlations between a respondent’s answer to each question and that person’s self-rating of competence. Self-ratings are reported as mean +/− SEM. A p-value less than 0.05 was considered significant.
RESULTS
Response and Demographics
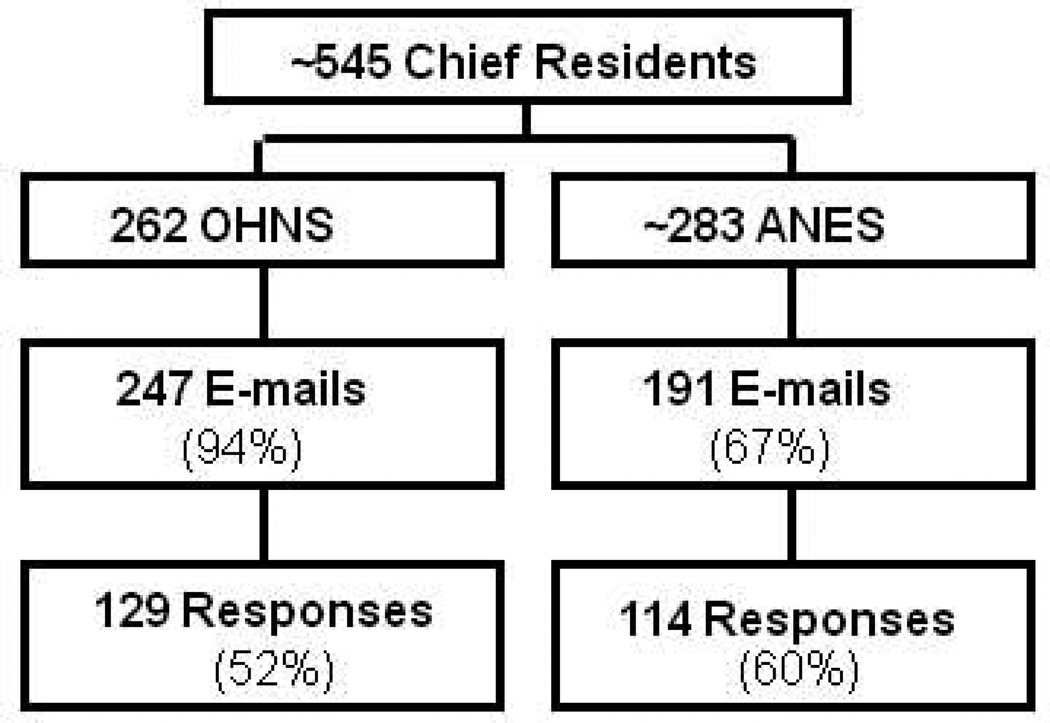
There are approximately 545 chief residents in the U.S. in Otolaryngology and Anesthesiology (Figure 1). We obtained e-mail addresses for 94% (247/262) of the Otolaryngology chiefs, and 67% (191/283) of the Anesthesiology chiefs. Some programs refused to disclose contact information for privacy reasons or department policy. 52% (129/247) of Otolaryngology chiefs and 60% (114/191) of Anesthesiology chiefs contacted completed the survey. Because demographic information was obtained from completed, anonymous surveys only, we cannot determine whether non-responders differed from respondents.
Figure 1.
Response rates of Otolaryngology and Anesthesiology chief residents
Training
Table 1 presents the list of training methods surveyed, percentage of residents responding “yes” to the prompts, and the relative significance of the difference between specialties. As expected, there were significant and substantial differences in training methods between Otolaryngology and Anesthesiology. Anesthesiology programs were more likely to require airway workshops, while Otolaryngology residents more frequently cited unsupervised management of airway emergencies as part of their training.
Table 1.
Training Methods
| OHNS % (n) | ANES % (n) | p-value | |
|---|---|---|---|
| Attendance at an airway workshop is required in my program | 27.1 (35) | 57.9 (66) | <0.001 |
| I attended an airway workshop | 30.2 (39) | 69.3 (79) | <0.001 |
| My training in airway emergencies included… | |||
| Selected readings | 65.1 (84) | 84.2 (96) | 0.001 |
| Use of emergency or secondary techniques and equipment for routine intubations | 58.1 (75) | 90.4 (103) | <0.001 |
| Mannequins | 22.5 (29) | 67.5 (77) | <0.001 |
| Full scale computerized patient simulator | 7.0 (9) | 44.7 (51) | <0.001 |
| Virtual reality tools | 2.3 (3) | 15.8 (18) | <0.001 |
| Animal labs | 12.4 (16) | 7.9 (9) | NS |
| Cadaver labs | 10.9 (14) | 12.3 (14) | NS |
| Lectures | 84.5 (109) | 93.0 (106) | <0.05 |
| Videos | 13.2 (17) | 38.6 (44) | <0.001 |
| Supervised management of actual emergencies | 77.5 (100) | 83.3 (95) | NS |
| Unsupervised management of actual emergencies | 76.7 (99) | 60.5 (69) | <0.05 |
| Routine diagnostic fiberoptic laryngoscopy in the clinical setting | 90.7 (117) | 70.2 (80) | <0.001 |
| Operative rigid direct laryngoscopy/bronochoscopy for diagnosis, biopsy or management of disease | 95.4 (123) | 20.2 (23) | <0.001 |
33% (43/129) of Otolaryngology chiefs rotated on Anesthesiology compared with only 8% (9/114) of Anesthesiology chiefs who rotated on Otolaryngology (p<0.001). It should be noted that the Otolaryngology chiefs who responded to this survey started their residency before an Anesthesiology rotation became a mandatory component of all Otolaryngology programs in 2004.
Assessment of Resident Competence
We asked residents how their competence in emergency airway management was assessed (Table 2). A variety of assessment measures were listed, but the majority of residents from both specialties selected “attestation” by an attending physician stating their competence in this area. Anesthesiology chiefs more frequently reported the use of additional assessment tools, including performance on mannequins, patients or cadavers (p<0.001) and simulation of an airway emergency (p<0.001).
Table 2.
How is competence assessed?
| OHNS % (n) | ANES % (n) | p-value | |
|---|---|---|---|
| Attending physician(s) attest that you are competent to take the boards and practice | 86.8 (112) | 76.3 (87) | <0.05 |
| Log books demonstrating your experience in specific emergency airway techniques | 42.6 (55) | 32.4 (37) | NS |
| Written exam in emergency airway management | 10.1 (13) | 20.2 (23) | <0.05 |
| Oral exam in emergency airway management | 12.4 (16) | 23.7 (27) | <0.05 |
| Observed demonstration of acceptable techniques on mannequins, patients or cadavers | 20.2 (26) | 46.5 (53) | <0.001 |
| Completion of an observed simulated airway emergency experience | 5.4 (7) | 20.2 (23) | <0.001 |
| Virtual reality or other computer-based simulation | 3.1 (4) | 3.5 (4) | NS |
| I don't know | 14.7 (19) | 13.2 (15) | NS |
Call schedules
Because differences in call structure may help to explain variations in experience and confidence, subjects were queried about their schedules. Otolaryngology and Anesthesiology residents reported different approaches to on-call coverage in their programs. All surveyed Anesthesiology chiefs reported that Anesthesiology resident coverage for airway emergencies is in-house 24 hours a day. Only 28.8% (37/129) of Otolaryngology respondents came from programs where around-the-clock in-house coverage is required (data not shown). The burden of overnight coverage falls more heavily on the junior Otolaryngology residents. (Table 3)
Table 3.
During what years of specialty training (after internship) did you take in-house call?
| % In-House (n) | |||
|---|---|---|---|
| OHNS | ANES | p-value | |
| 1st Year | 56.0 (72) | 98.2 (112) | <0.001 |
| 2nd Year | 44.4 (57) | 99.1 (113) | <0.001 |
| 3rd Year | 26.6 (34) | 99.1 (113) | <0.001 |
| 4th Year | 9.9 (13) | 96.8 (110) | <0.001 |
Clinical Exposure
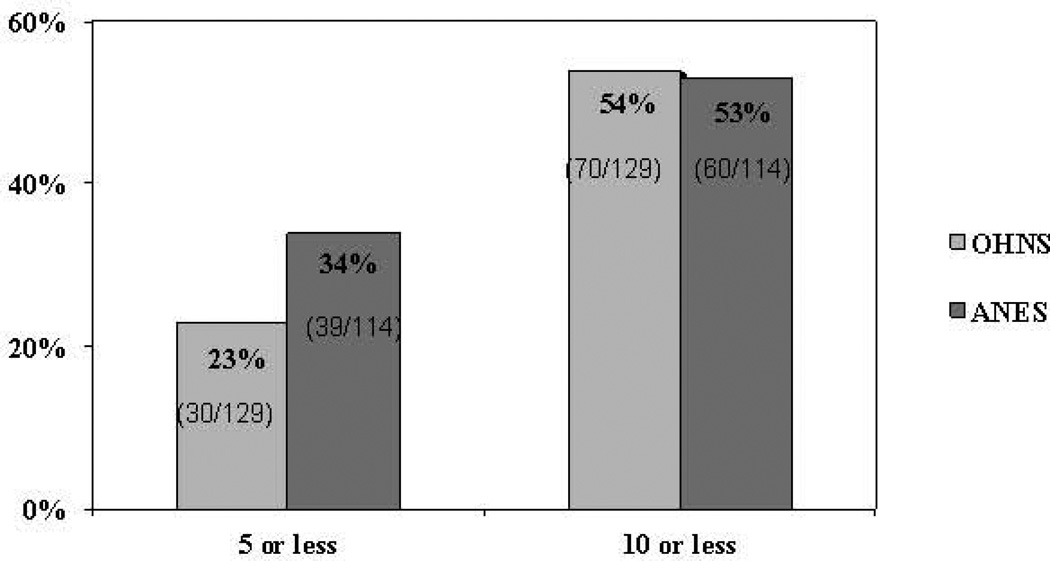
The median range of airway emergencies that both Otolaryngology and Anesthesiology chiefs participated in during their residencies (ie: involved in any capacity) was “6–10.” 54% (70/129) of Otolaryngology chiefs and 53% (60/114) of Anesthesiology chiefs had participated in 10 or fewer airway emergencies, and 23% (30/129) of Otolaryngology and 34% (39/114) of Anesthesiology chiefs had participated in 5 or less. (Figure 2)
Figure 2.
How many airway emergencies have you personally participated in (ie: you were present during the emergency and involved in any capacity) during your residency? Otolaryngology median range = 6–10; Anesthesiology median range = 6–10. % answering yes on Y axis.
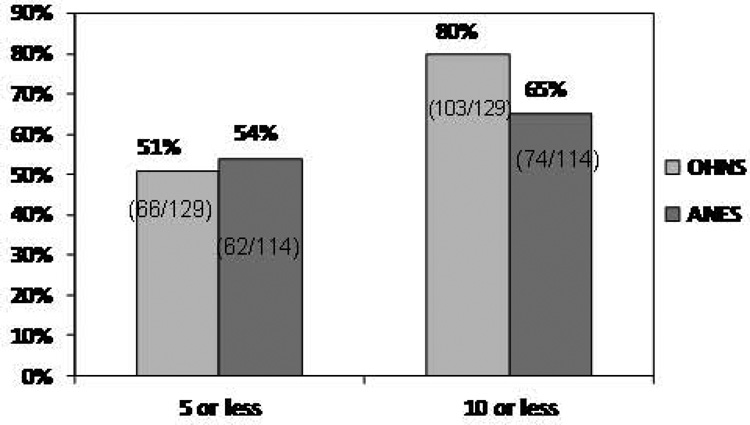
The median range of airway emergencies that both Otolaryngology and Anesthesiology chiefs personally managed (i.e., charged with securing the airway) was ”3–5.” 80% (103/129) of Otolaryngology chiefs and 65% (74/184) of Anesthesiology chiefs had personally managed 10 or fewer airway emergencies, and 51% (66/129) of Otolaryngology and 54% (62/114) of Anesthesiology chiefs had personally managed 5 or less. (Figure 3)
Figure 3.
How many airway emergencies have you personally managed (you were the resident charged with securing the airway) during your residency? Otolaryngology median range = 3–5; Anesthesiology median range = 3–5. % answering yes on Y axis.
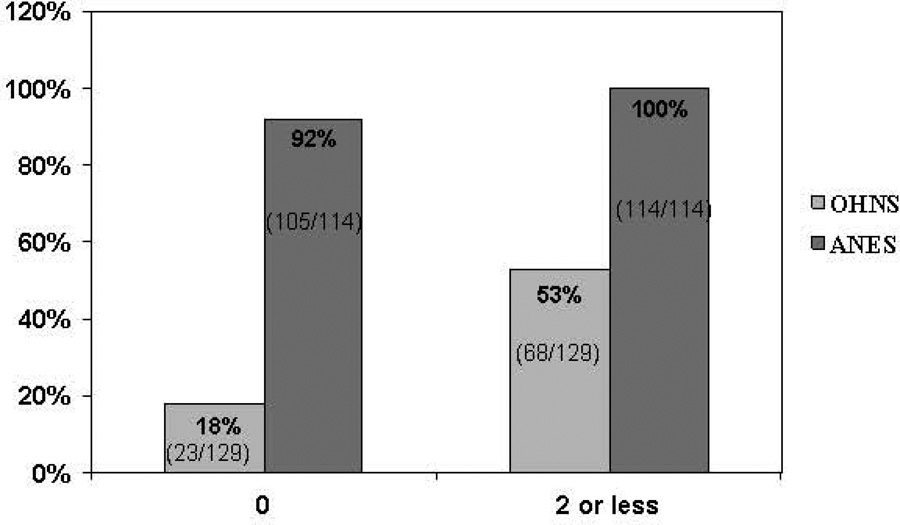
Surgical experience
The median range of emergency surgical airways (ie: tracheostomy or cricothyrotomy) performed by Otolaryngology chiefs was ”1–2,” whereas the median number for Anesthesiology chiefs was “0” (P<0.001). 18% (23/129) of Otolaryngology chiefs reported never performing an emergency surgical airway, and 53% (68/129) have performed no more than 2. Among Anesthesiology respondents, 92% (105/114) have never performed an emergency surgical airway, and no Anesthesiology chief has done more than 2 (Figure 4).
Figure 4.
How many emergency surgical airways (tracheostomy or cricothyrotomy) have you personally performed during your residency? Otolaryngology median range = 1–2; Anesthesiology median range = 0. % answering yes on Y axis.
Self-reported Confidence
Resident confidence also varied by specialty. When asked if they felt their clinical experience during residency training had given them the opportunity to manage an adequate number of airway emergencies, 90% (116/129) of Otolaryngology chiefs responded yes compared to 80% (91/114) of Anesthesiology chiefs (p=0.04).
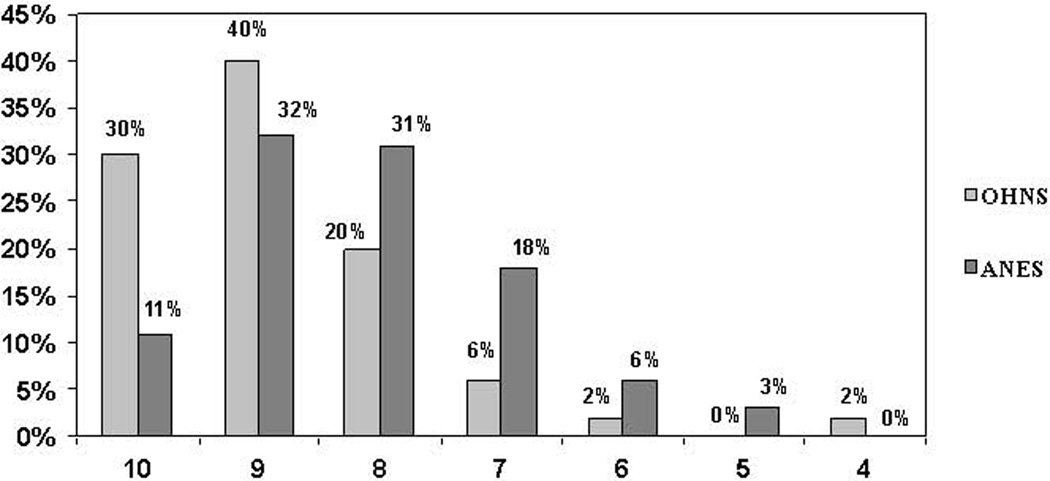
Chief residents in both specialties gave themselves high ratings for competence in managing airway emergencies. On a scale of 1 to 10 (10 = “totally competent,” 1 = “not competent at all”), the most common self-rating for both specialties was “9.” The mean self-rating for Otolaryngology chiefs was 8.9 +/− 0.10, compared with 8.1 +/− 0.11 for Anesthesiology (p<0.001). 70% (90/129) of Otolaryngology chiefs rated themselves “9” or “10,” and 90% (116/129) self-rated “8” or higher. Among Anesthesiology chiefs, 43% (49/114) rated themselves “9” or ”10,” and 74% (84/114) responded “8” or higher (Figure 5).
Figure 5.
On a scale of 1 to 10, how would you rate your competency to handle an airway emergency? 10=totally competent; 1=not competent at all. Otolaryngology mean = 8.9; Anesthesiology mean = 8.1. % answering yes on Y axis.
We identified factors of resident training and experience that correlated with a higher self-rating of competence. Interestingly, respondents who reported they had not managed an adequate number of airway emergencies rated themselves higher than those who felt their exposure was adequate (p<0.001) (Table 4); of all surveyed factors, this response had the strongest correlation with a high self-rating for both specialties. Participating in a greater number of airway emergencies also correlated with a higher self-rating (p≤0.001) (Table 5). For Otolaryngology chiefs, rotating on an Anesthesiology service during residency was significantly correlated to a higher self-rating (p=0.02). Similarly, there was a trend towards higher self-rating among Anesthesiology chiefs who rotated on an Otolaryngology service, but this was not statistically significant (p=0.064). A summary of the training and experiences with the strongest correlation to higher self-ratings of competence is presented in Tables 4 and 5.
Table 4.
Factors that Are Inversely Correlated with High Self-Rating of Competency
| Factor | OHNS | ANES |
|---|---|---|
| p-value | ||
| Managed an adequate number of airway emergencies | 0.001 | 0.001 |
| Full scale computerized patient simulator | 0.026 | 0.430 |
| Virtual reality tools | 0.022 | 0.811 |
Table 5.
Factors that Are Positively Correlated with High Self-Rating of Competency
| Factor | OHNS | ANES |
|---|---|---|
| p-value | ||
| Rotation on an otolaryngology service during your residency | 0.064 | |
| Rotation on an anesthesiology service during residency | 0.019 | |
| Number of actual airway emergencies (present and involved in any capacity) | 0.0001 | 0.001 |
| Number of actual airway emergencies personally managed (responsible for securing the airway) | 0.001 | 0.001 |
| Supervised management of actual emergencies | 0.017 | 0.002 |
| Unsupervised management of actual emergencies | 0.045 | 0.001 |
DISCUSSION
Airway emergencies are life-threatening and represent significant clinical challenges. Unfortunately, there is no consensus definition of “airway emergency.” The American Society of Anesthesiologists defines a “difficult airway” as “the clinical situation in which a conventionally trained anesthesiologist experiences difficulty with face mask ventilation of the upper airway, difficulty with tracheal intubation, or both.”8 There is no similar definition in Otolaryngology. In our study, we focused on the emergency situation in which otolaryngologists may be called to intervene and therefore used a specific definition (see above). Though our definition does not address subacute situations or the use of adjunctive airway techniques (supraglottic masks or blind intubation devices), it conveys the critical nature of airway emergencies in which the patient’s condition is quickly deteriorating despite best efforts to secure an airway.
Our data show significant and substantial differences in training structures in airway management for residents in Anesthesiology and Otolaryngology. Coupled with varying exposure to and management responsibility for life-threatening airway events these findings help validate limitations of traditional apprenticeship training approaches. Despite these differences, we could not detect a difference in exposure and frequency of actual airway emergencies between the specialties. Emergency surgical airways were performed rarely by residents of either specialty. Residents in their final year of training in both specialties still rated their exposure as adequate, and their competence as high.
Survey research presents limitations, including selection bias, recall bias, response rates and survey design.9 In this study, our goal was to contact every chief resident in Otolaryngology and Anesthesiology in the U.S. to represent all training programs, minimize selection bias and increase power. There is no single source for this information and selection bias in survey research is multifactorial. We approximated the total number of Otolaryngology and Anesthesiology chief residents in the U.S., but the exact number varies by year due to unfilled program positions, changes in the number of residents for which a program is approved, and for Anesthesiology, due to variations in the number of chief residents selected from each graduating class.
Several programs in Otolaryngology and many more in Anesthesiology refused to divulge contact information for their chief residents, citing privacy concerns. As a result, we were only able to contact 94% of Otolaryngology residents. Anesthesiology programs select only a few of a given class to be chiefs each year and criteria vary by program and by year. Some programs refused to divulge even how many chief residents they had. Based on the program sizes obtained from the Accreditation Council for Graduate Medical Education (ACGME) and data from the programs that did reveal the number of their chief residents, we estimated that there were 283 Anesthesiology chief residents in the study year. We obtained e-mail addresses for 67% of them. Of those residents contacted, 52% of the Otolaryngology chiefs and 60% of the Anesthesiology chiefs completed the survey. A study of response rates to e-mail surveys shows that since the initiation of such surveys in 1986, response rates have been trending downwards year-by-year.10 Compared with the 31 academic surveys studied, our response rate compares favorably (range: 19% to 61%).10 Although low response rates increase the likelihood of bias in the data, there is no agreement on an acceptable response rate, below which the respondents’ representativeness of the target population is compromised; it can range from 50 to 75%.11 Despite the response rates, our survey still provides the only detailed national data on resident training, hands-on practice and confidence in emergency airway management. We acknowledge that these barriers may cause our results to not completely represent the experience of residents in these fields.
Another factor that may affect our results is the different structure of Otolaryngology and Anesthesiology residency programs. All Otolaryngology residents are required to complete a “chief year” (the last year of training), while most Anesthesiology programs select a few from their graduating class to be chief residents. Thus, while our survey targeted essentially all Otolaryngology residents in their final year of training, we invited a small fraction of all of the Anesthesiology residents graduating in 2007 to take the survey. One assumes that higher performing Anesthesiology residents are selected to be chiefs. This methodology may skew the Anesthesiology results towards higher levels of competence and skill as assessed by their faculty. Inherent differences in training structure between the specialties training related to size (larger classes of anesthesia residents requiring more structure teaching and evaluation) and cultural differences (early adoption of new airway technologies, innovation in simulation, standardized assessment, quality improvement, etc., that are prevalent in anesthesia). Lastly, differences in call schedule (in house for Anesthesia versus home call for Otolaryngology) may be reflected in our results.
Airway emergencies are low incidence high risk situations, marked by time pressure and resource management challenges. It is apparent that, for Otolaryngology programs, junior residents take a disproportionate amount of in-house overnight call when compared with their seniors. This places junior residents at increased risk for experience with airway emergencies when senior residents and attending physicians are not readily available to assist or educate. Not only do unsupervised residents miss out on important educational opportunities, but they may also put their patients at an increased risk for complications.12 Finding ways to optimize resident supervision during airway emergencies may improve both resident training and patient outcomes.
Over half of all chief residents of both specialties reported being involved in any capacity at fewer than 10 airway emergencies, and over half reported having personally managed fewer than 5 over the course of their training. This implies that throughout their training, residents have limited opportunities to participate in an airway emergency to practice not only technical skills but leadership, team and incident management skills. The number of emergency surgical airways is even more striking, with over half of Otolaryngology residents performing two or less and almost all of Anesthesiology residents never performing one. Situations that call for an emergency surgical airway often require the intervention of otolaryngologists or other surgeons, but our survey suggests that the opportunity to perform such a procedure is severely limited during training. One study demonstrated that even in a highly controlled and simplified environment, 96% of participants needed at least five attempts on a mannequin in order to perform a cricothyrotomy correctly in 40 seconds or less.13 The limited exposure during residency is perhaps a consequence of an overall decline in the performance of surgical airways, a phenomenon that should compel program directors to reconsider how its trainees will gain the necessary experience before graduation.14 It is not known whether the incidence of airway emergencies is rising or falling, or whether outcomes are changing Further epidemiologic research on this topic may shed light on these questions, especially with the current emphasis on safety, quality, and outcomes in healthcare.
Perhaps the most compelling result of this survey is the dichotomy between low levels of experience and high levels of confidence and self-assessed competence. This suggests that either residents are truly competent or they are overconfident. In the first case, one concludes that airway emergency training is adequate and that residents are heading into practice with high levels of skill in dealing with this critical clinical situation. Clinical experience and prior study,15,16 however, reveal that airway management problems remain a source of preventable morbidity and mortality, with improved training as one potential remedy.17 18 19 Generally, the main focus of medical education has been focused on technical and clinical skills than situation management. In the second case, one supposes that residents are graduating full of confidence, but with their inexperience, they do not have the competence that they think they have. Several studies in different domains of proficiency have compared self-assessed competence with competence assessed by an expert observer.20 Most studies we found show a weak to moderate correlation between self-assessment and independently-judged skill.21 22 One additional factor that may explain the paradox is that institutions where interdisciplinary teamwork in airway management is strong (and consequently trainees are surrounded by outstanding support) may have fewer emergencies but still generate high skill and confidence in their residents.
One important caveat to our results is that we did not measure training in routine airway management, i.e., in the non-emergency setting. This would include daily intubations for Anesthesia residents, operative procedures such as direct laryngoscopy and elective tracheotomy for Otolaryngology residents, and flexible fiberoptic endoscopy for both groups. Certainly these practices are considered so integral and standard to approved training programs that currently the ACGME does not require either specialty to report numbers of the intubations performed. Otolaryngology residents do report flexible laryngoscopy (mean cases,(range): 25 [0–419]), diagnostic direct laryngoscopy (24.9 [0–419]) and tracheotomies (52.4[7–151]) (ACGME National Data Report, Otolaryngology Case Logs, 2010). We note that although CPT codes exist for emergency tracheotomy and cricothyrotomy, the ACGME currently does not collect these separately. Routine airway experiences certainly impact the trainee’s ability to perform in the emergency setting, especially regarding technical knowledge and skill. However, it must be noted that a number of factors are different in an airway emergency, including time pressure, site and equipment differences, lighting, need for quick and independent judgment, management of contingencies and team dynamics, psychological pressure, and potential absence of faculty supervision requiring different leadership and communication skills than those provided by routine situations.
If residents in Otolaryngology and Anesthesiology are graduating with little experience and unjustifiably high levels of confidence, the next steps would be to remedy the experience deficit and improve assessments of competence. Improving training in this clinical arena remains problematic for several reasons. Airway emergencies are unexpected with a wide variety of contextual challenges. Even if one could predict how many crises would occur in an institution in a given year, a resident’s exposure to the event is random: Is the resident in the hospital? On call? Covering the emergency pager? Or committed to an activity elsewhere? The restrictions imposed by the 80-hour work week reduce the chance that a resident will be available when an airway emergency arises. New ACGME requirements for trainee supervision under consideration may affect this clinical situation and many others. Additionally, attending faculty work to anticipate and prevent crises. During actual emergencies residents may not have the chance for hands-on practice or primary responsibility for event management.
In lieu of true clinical experience, novel educational strategies should be explored to provide training in airway crisis situations. The advent of realistic, computerized, advanced patient mannequins set up in realistic or actual health care settings provide a possible mechanism to provide trainees with vivid, life-like experiences.23 Interestingly, the use of virtual reality tools and full scale computerized patient simulators correlated inversely with self-assessed competence among Otolaryngology residents (Table 5). This could be due to a small sample size. Another reason may be that residents lacking the performance review and feedback offered by patient simulators are more likely to lack insight about their true level of competence. Data on specifics of training or quality of simulation exposure and feedback were not collected.
A systematic review of high-fidelity simulator technology and its application to medical learning demonstrated educational effectiveness and a role for simulators to complement bedside teaching.24 Cross-disciplinary training may also prove beneficial. For example, Anesthesiology residents may improve their airway skills by learning rigid laryngoscopy techniques practiced in Otolaryngology, or assisting the Otolaryngology service in routine tracheostomy placement. Conversely, Otolaryngology residents rotating in Anesthesiology may practice intubation via direct laryngoscopy or other techniques (laryngeal mask airway) to which they would otherwise have little or no exposure. Immersive interdisciplinary simulation with video feedback may also target improvement in complex problem solving, incident and resource management. Just as pilots train for rare, catastrophic, complex events for which even extensive routine experiences may not provide adequate preparation, physicians may benefit from analogous simulation training in airway emergency management in technical, clinical and incident management domains. Ultimately, this may improve outcomes for this difficult clinical situation.
CONCLUSIONS
Airway emergencies are a significant source of morbidity and mortality in the U.S. Many chief residents in Otolaryngology and Anesthesiology graduate with low levels of exposure to hands-on management of airway emergencies. Despite this, chief residents report high levels of confidence in their own ability to manage these events. Modern simulation curricula and technology may provide a useful training tool to address the low experience – high confidence dichotomy.
Supplementary Material
Acknowledgments
The authors would like to thank Ms. Jamie Phillips for her administrative assistance, and Dingcai Cao, Ph.D. in the Department of Health Studies for analytic support.
Funding
Drs. Andrews and Nocon were supported by the McHugh Otolaryngology Research Fund. Dr. Pinto was supported by an American Geriatrics Society/Dennis W. Jahnigen Scholars Award and the Institute for Translational Medicine [KL2 RR025000, UL1 RR024999] at The University of Chicago. This study was also supported by a grant from the Graduate Medical Education Committee and the Academy of Distinguished Medical Educators of the Pritzker School of Medicine of the University of Chicago and the Department of Surgery.
Footnotes
Other Disclosures
None
Ethical Approval
Approval from the Institutional Review Board was obtained.
Disclaimer
None
Previous Presentations
Presented at the Annual Meeting of American Academy of Otolaryngology-Head and Neck Foundation, Washington, D.C., September 2007
REFERENCES
- 1.Peterson GN, Domino KB, Caplan RA. Management of the difficult airway: A closed claims analysis. Anesthesiology. 2005;103:33–39. doi: 10.1097/00000542-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Koppel JN, Reed AP. Formal instruction in difficult airway management: a survey of anesthesiology residency programs. Anesthesiology. 1995;83:1343–1346. doi: 10.1097/00000542-199512000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Needham DN, Thompson DA, Holzmueller CG. A system factors analysis of airway events from the intensive care unit safety reporting system (ICUSRS) Crit Care Med. 2004;32:2227–2233. doi: 10.1097/01.ccm.0000145230.52725.6c. [DOI] [PubMed] [Google Scholar]
- 4.Janssens M, Hartstein G. Management of difficult intubation. Eur J Anaesth. 2001;18:3–12. doi: 10.1046/j.0265-0215.2000.00777.x. [DOI] [PubMed] [Google Scholar]
- 5.Ollerton JE, Parr MJ, Harrison K. Potential cervical spine injury and difficult airway management for emergency intubation of trauma adults in the emergency department – a systematic review. Emerg Med J. 2006;23:3–11. doi: 10.1136/emj.2004.020552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graham CA. Emergency department airway management in the UK. J R Soc Med. 2005;98:107–110. doi: 10.1258/jrsm.98.3.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surveymonkey. Portland, OR: http://www.surveymonkey.com . [Google Scholar]
- 8.American Society of Anesthesiologists Task Force on Management of the Difficult Airway: Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiol. 2003;98:1269–1277. doi: 10.1097/00000542-200305000-00032. [DOI] [PubMed] [Google Scholar]
- 9.Kelley K, Clark B, Brown V. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- 10.Sheehan K. E-mail survey response rates: a review. Journal of Computer-Mediated Communication. 2001;6(2) [Online] Available: http://jcmc.indiana.edu/vol6/issue2/sheehan.html. [Google Scholar]
- 11.Coons SJ. Responses to survey research: transparency and representativeness are key. Clin Thera. 2007;29:466–468. doi: 10.1016/s0149-2918(07)80084-1. [DOI] [PubMed] [Google Scholar]
- 12.Boylan JF, Kavanagh BP. Emergency airway management: competence versus expertise? Anesthesiology. 2008;109:945–947. doi: 10.1097/ALN.0b013e31818e3f8f. [DOI] [PubMed] [Google Scholar]
- 13.Wong DT, Prabhu AJ, Coloma M, Imasogie N, Chung FF. What is the minimum required training for successful cricothyroidotomy? A study in mannequins. Anesthesiology. 2003;98:349–353. doi: 10.1097/00000542-200302000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Levitan RM. Myths and realities: the “difficult airway” and alternative airway devices in the emergency setting. Acad Emerg Med. 2001;8:829–832. doi: 10.1111/j.1553-2712.2001.tb00216.x. [DOI] [PubMed] [Google Scholar]
- 15.Clybourn PA. Early thoughts on ‘Why mothers die 2000–2002.’. Anesthesia. 2004;59:1155–1159. doi: 10.1111/j.1365-2044.2004.04060.x. [DOI] [PubMed] [Google Scholar]
- 16.Cheney FW. The American society of anesthesiologists closed claims project: what have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999;91:552–556. doi: 10.1097/00000542-199908000-00030. [DOI] [PubMed] [Google Scholar]
- 17.Dunn S, Connelly NR, Robbins L. Resident training in advanced airway management. J Clin Anesth. 2004;16:472–476. doi: 10.1016/j.jclinane.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Hapberg CA, Greger J, Chelly JE, Saad-Eddin HE. Instruction of airway management skills during anesthesiology residency training. J Clin Anesth. 2003;15:149–153. doi: 10.1016/s0952-8180(02)00503-2. [DOI] [PubMed] [Google Scholar]
- 19.Lavery GG, McCloskey BV. The difficult airway in adult critical care. Crit Care Med. 2008;36:2163–2173. doi: 10.1097/CCM.0b013e31817d7ae1. [DOI] [PubMed] [Google Scholar]
- 20.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296:1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- 21.Mandel LS, Goff BA, Lentz GM. Self-assessment of resident surgical skills: Is it feasible? Am J Ob Gyn. 2005;193:1817–1822. doi: 10.1016/j.ajog.2005.07.080. [DOI] [PubMed] [Google Scholar]
- 22.Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, Durbin DR. Assessing pediatric senior residents training in resuscitation: Fund of knowledge, technical skills and perception of confidence. Ped Emerg Care. 2000;16:73–76. doi: 10.1097/00006565-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Kory PD, Eisen LA, Adachi M, Ribaudo VA, Rosenthal ME, Mayo PH. Initial airway management skills of senior residents: simulation training compared with traditional training. Chest. 2007;132:1927–1931. doi: 10.1378/chest.07-1554. [DOI] [PubMed] [Google Scholar]
- 24.Issenberg SB, McGaghie WC, Petrusa ER. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27:10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.