Abstract
Objectives
To examine the prevalence of mental health symptoms among medical interns working for the first time as physicians in a large tertiary hospital in Israel during the 1st COVID year.
Methods
All interns who worked for at least 2 months during the 1st COVID year (March 2020–February 2021) at the Tel-Aviv Sourasky Medical Center (TASMC), a large tertiary general hospital in Israel were approached simultaneously during April–May 2021, and were requested to fill in an online survey. In each questionnaire, the interns were asked to refer to the worst time they endured the symptoms described. Included were all medical. Depression and anxiety symptoms, post-traumatic stress symptoms and Burnout measures were evaluated using validated questionnaires. Depressive/anxiety symptoms were defined as primary end measures. We assessed the association between depression and anxiety symptoms, and demographic, post-traumatic and burnout measures.
Results
145 out of 188 interns completed the study (77% overall response rate). The mean age was 30.36 ± 2.97. Almost half the interns (47%) reported depression/anxiety symptoms. The high depression/anxiety group was characterized by a lower mean age (29.87 ± 2.93 vs. 30.92 ± 2.91, p = 0.041), higher post-traumatic symptoms (15.62 ± 13.32 vs. 3.63 ± 5.59, p < 0.0001) and higher scores in 2/3 burnout subscales - emotional exhaustion (5.09 ± 1.29 vs. 3.61 ± 1.38, p = 0.000001) and depersonalization (3.83 ± 1.71 vs. 2.94 ± 1.46, p = 0.002). 11.4% of interns in the full sample reported they used cannabis or alcohol as “self-medication”.
Conclusions
medical interns serving for their first year as physicians during the COVID pandemic, developed mental symptoms in alarming numbers. The findings point to a crucial need to implement active interventions to protect these doctors, so that they can safely embark on their medical careers, specifically in times of global health crises.
1. Introduction
Studying mental-health related effects of the coronavirus pandemic (COVID-19) on frontline physicians worldwide is a growing focus of attention [[1], [2], [3], [4], [5], [6], [7]]. Previous studies have provided preliminary evidence that healthcare workers during the pandemic are at increased rate of developing depressive and anxiety symptoms [1,5,8]. Medical interns, introduced for the first time as workers of healthcare systems, are in a unique position during the pandemic: serving many times as frontline caregivers while contemplating the future of their medical career.
In Israel, the internship year is a transitional phase between medical studies, and practical medical work [9]. Interns are assigned to hospitals across the country, where they are required to rotate between departments of general internal medicine, emergency medicine, surgery, pediatrics and more, upon the completion of their medical studies and prior to receiving their medical license. In the special circumstances of the “1st COVID year” (March 2020 through February 2021), many of them were thrust to the midst of a global crisis caused by the pandemic. These harsh circumstances placed this well -defined group of early-career physicians in a susceptible state, potentially prone to develop mental health issues such as work-related burnout, anxiety, and depression. Moreover, during their internship, these soon-to-be residents are expected to explore and choose a medical field to specialize in, competing for limited resident physician positions. Although some studies examined mental effects of treating COVID-19 patients on early-career physicians (residents) [5,10,11], to the best of our knowledge, no previous studies focused on the specific population of interns.
We sought to examine differences in the development of depression and anxiety symptoms, our main outcome measure, among a group of medical interns in a large tertiary hospital in Israel during the 1st COVID year – and the relationship between these symptoms and other mental-health related measures such as use of cannabis or alcohol, development of post-traumatic stress symptoms, burnout measures and more.
2. Materials and methods
2.1. Participants
Included in the study were all medical interns who worked at the Tel-Aviv Sourasky Medical Center (TASMC) for at least 2 months during the 1st COVID year, at the time beginning from March 2020 till end of February 2021 (the first confirmed COVID-19 patient was diagnosed in Israel at the end of February 2020, with restrictions and lockdowns imposed from March 2020). All interns were approached during April–May 2021 and asked to fill in an on-line survey containing demographic details and mental health questionnaires. There were no exclusion criteria. By completing the survey, participants provided informed consent to participate in the study. The study was approved by the institutional review board of the TASMC.
Demographics and background characteristics: all participants completed a demographic questionnaire, including items on age, sex, marital status, and parenthood. They were further asked to specify the number of months spent in internship, the number of months spent in COVID-19 wards, prior experience as a physician-assistant (working alongside a resident physician, usually during medical school, to acquire clinical experience), preferred specialty for residency (both pre and post internship) and unexpected changes in their internship program due to the COVID-19 pandemic. COVID-19 exposure items included whether the intern or any of his/her family members contracted COVID-19 during the internship, and the number of quarantine episodes imposed on the intern due to exposure to COVID-19 infected patients, colleagues, or family members, during the internship.
2.2. Mental health measures
Depressive and anxiety symptoms were defined as the primary end measures and evaluated by the Hebrew version of the Hospital Anxiety and Depression Scale (HADS) [[12], [13], [14]], a widely used measure of depression and anxiety. We chose this unified measure as it is well validated, short to administer and combines depressive and anxious symptoms, a combination we postulated will characterize the clinical presentation. The HADS is comprised of 14 items, seven of which assess depressive symptoms (HADS-D) and seven assess anxiety symptoms (HADS-A). Each item is scored from 0 to 3, thus providing a total score ranging from 0 to 21 for each domain screened. A comprehensive review of studies employing The HADS questionnaire concluded that a cut-off of 8+ is optimal in terms of balance between sensitivity and specificity as a screening instrument, for both the HADS-A and HADS-D [15,16].
Participants were further asked to report current psychological treatment, prior & current psychopharmacological treatment, need for mental health treatment during the internship, and whether they felt they had to use cannabis or alcohol during the COVID year to get through the difficulties they encountered.
Post-traumatic symptoms: we used the Hebrew version of the PTSD checklist - PCL-5 self-report measure [17,18] - designed according to the PTSD criteria in the Diagnostic and Statistical Manual of Mental Disorders 5th ed. (DSM-5) [19]. The PCL-5 is one of the most validated and widely used self-report measures of post-traumatic stress disorder (PTSD) [17,20,21] and was recently used to assess post-traumatic symptoms among healthcare workers in the COVID-19 pandemic [22]. It is comprised of 20 items corresponding to the various PTSD diagnostic criteria. Responses indicate severity of each symptom in a 0 to 4 scale. Item scores are summed to yield a measure of PTSD overall symptom severity. A total of 32 and above is considered as the threshold for possible PTSD in the PCL-5, corresponding to a score of 44 in the previous version of the questionnaire [21,23].
Burnout: we used the Hebrew version of the Maslach Burnout Inventory (MBI) [24,25], the most widely used measure of burnout symptoms. The MBI consists of 16 items classified into three scales, averaged separately: emotional exhaustion (EE, measured by 5 items), depersonalization (DP, measured by 5 items), and personal accomplishment (PA, measured by 6 items). Items are scored on a 7-point scale ranging from 1 (never) to 7 (always). Calculations of Cronbach's alpha for subscales yielded values of 0.882 for EE, 0.855 for DP, and 0.738 for PA.
For all mental health questionnaires (HADS, PCL-5, MBI), the interns were asked to refer to the worst time they endured during the 1st COVID year, associated with their experience as physicians in COVID wards. We chose to define the time frame as such taking into consideration that mental symptoms do not necessarily appear in proximity to the trigger and in many cases their onset is somewhat delayed.
2.3. Statistical analysis
Continuous variables are displayed as means (standard deviation, SD). Categorical variables are displayed as numbers (%) of participants within each group or category. Groups were compared using a student's t-test for normally distributed continuous variables and a Chi-squared test for categorical variables. Fisher's exact test was performed for low frequencies (n < 5). No interpolations were performed to replace missing data. All reported tests were 2-sided, and a P value <0.05 was considered significant. SPSS/WIN (version 27.0, SPSS, Chicago, IL, USA) was used for all statistical analyses.
3. Results
188 medical interns worked for at least 2 months during the 1st COVID year at the TASMC, and all were approached during May 2021 (at a time when COVID-19 cases were relatively low in Israel, between the 3rd and 4th waves of the pandemic), by both text messages and a personal phone call by the research team leader (O.T.) to enhance adherence. 145 interns completed the study (at least partially), reflecting an overall response rate of 77%. Their data were available for analysis.
3.1. Demographic, internship, mental-health, and COVID-19 exposure-related characteristics
Most interns were females (51.7%), single (50.4%), and had no children (80%). The mean age was 30.36 ± 2.97. The mean time spent in the internship before completion of the survey was 6.17 ± 3.91 months, of which 1.85 ± 1.33 months were spent working in COVID-19 dedicated wards (although the interns were continuously treating COVID patients even on months not working in COVID-19 only wards, e.g., in general ER shifts). More than half (50.5%) of the interns had prior experience as physician assistants (working alongside a resident physician during medical school, to acquire clinical experience). Regarding mental health-related history, 11.7% of interns were treated with psychotherapy during the survey and 5.5% were treated with psychopharmacological agents. 10.4% felt they needed to use cannabis or alcohol to “get through” the hardships of treating COVID-19 patients amid the pandemic. 5% were ill with COVID-19 themselves, and 12.4% had an ill close family member. 20.7% of the interns experienced 1 quarantine during internship, while 10.3% experienced 2 or more. Most interns (65.5%) experienced last-minute changes in their internship program, and these changes were reported to have a moderate to severe effect on the intern's mental state in 30.4% of responders. 19.4% of the interns reported that the experience in the COVID-19 wards contributed, at least moderately, to a change in their choice of residency (from the time prior to their internship).
3.2. Depression and anxiety, post-traumatic and burnout symptoms
The mean HADS score was 6.84 (SD = 4.62) for the HADS-A and 4.84 (3.79) for the HADS-D. 41% of interns scored higher than the threshold for anxiety and 23.3% scored higher than the threshold for depression. The correlation between the HADS-A and HADS-D score was 0.61 (p < 0.0001), in accordance with previous evidence in the literature, which reported correlations ranging from 0.4 to 0.75 [15]. Higher depression score was significantly correlated with a greater chance of changing residency choice (r = 0.39, p < 0.0001) and this was also the case for anxiety (r = 0.32, p < 0.001). Regarding post-traumatic symptoms, the mean total PCL-5 score was 9.06 (11.48), with subscale means of 1.47 (2.47), 0.70 (1.53), 3.44 (4.62) and 3.57 (4.41) for intrusion, avoidance, negative changes in mood and cognition and arousal and reactivity, respectively. 11 (9.6%) interns scored above the threshold for possible PTSD. The mean MBI scores, measuring burnout symptoms, were 4.3 (1.54), 3.36 (1.63) and 5.44 (0.99) for the emotional exhaustion, depersonalization, and personal accomplishment scales, respectively. More time spent in COVID-19 specific wards was associated with increased emotional exhaustion, with an MBI-EE mean of 4.47 (1.26) for interns working >1 month in COVID-19 specific wards vs. 3.82 (1.55) for those working 1 month only (p = 0.035).
3.3. Group comparison: low vs. high depression/anxiety
Using the screening cut-offs previously mentioned for the HADS-D, HADS-A or both, we divided the sample to a high depression/anxiety symptom group and a low depression/anxiety symptom group. For this analysis, full data were available for 134 participants. The high depressed/anxious group included 63 participants (47%). We compared these groups in demographic, internship-related and mental health-related measures.
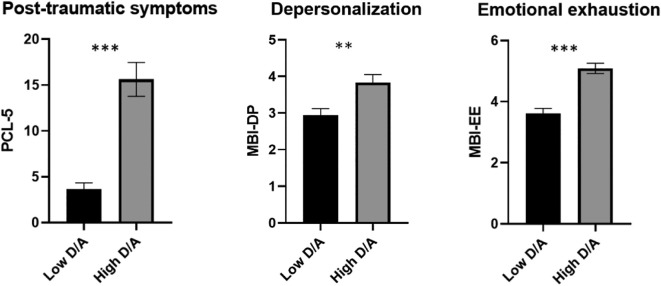
The mean age in the high depression/anxiety group was significantly lower compared with the mean age in the low depression/anxiety group (29.87 ± 2.93 vs. 30.92 ± 2.91, p = 0.041). Prior experience as physician assistant was not found to differ between groups. COVID-19 illness during internship was rare and was more common in the high depression/anxiety group (9.8% vs. 1.5% in the low depression/anxiety group), although this difference did not reach statistical significance (p = 0.053). More interns in the high depression/anxiety group were currently in psychological treatment (19% vs. 5.6%, p = 0.03), and more interns in this group felt they needed mental health treatment following their time treating COVID-19 patients during the pandemic, compared with the low depression/anxiety group (36.5% vs. 8.5%, p = 0.000083). Full data are detailed in Table 1 . (See Fig. 1.)
Table 1.
group comparison of demographics, internship characteristics and mental health outcomes between low and high depression/anxiety groups.
| Characteristic | Total N = 134 | Low depression/anxiety group N = 71 (53%) | High depression/anxiety group N = 63 (47%) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age, years (SD) | 30.43 (2.95) | 30.92 (2.91) | 29.87 (2.93) | 0.041 |
| Female, n (%) | 66 (49.3%) | 32 (45%) | 34 (54%) | 0.56 |
| Married/in a relationship, n (%) | 52 (45.6%) | 25 (35.2%) | 27 (42.9%) | 0.59 |
| Number of children, n (%) | 28 (20.9%) | 17 (23.9%) | 11 (17.5%) | 0.36 |
| Internship-related characteristics | ||||
| Accumulated time in internship, months (SD) | 6.94 (3.55) | 6.79 (3.36) | 7.11 (3.77) | 0.60 |
| Time in COVID-19 specific wards, months (SD) | 1.93 (1.31) | 1.78 (1.31) | 2.09 (1.31) | 0.17 |
| Prior experience as physician assistant, n (%) | 48 (51.6%) | 28 (54.9%) | 20 (47.6%) | 0.48 |
| COVID-19 illness during internship, n (%) | 7 (5.5%) | 1 (1.5%) | 6 (9.8%) | 0.053 |
| Family member COVID-19 illness during internship, n (%) | 18 (13.4%) | 7 (9.9%) | 11 (17.5%) | 0.19 |
| Changes in internship program due to the pandemic, n (%) | 90 (67.2%) | 46 (64.8%) | 44 (69.8%) | 0.53 |
| Mental health-related characteristics | ||||
| Previous history of psychiatric drug treatment, n (%) | 6 (4.7%) | 2 (2.9%) | 4 (6.8%) | 0.42 |
| Current psychiatric drug treatment, n (%) | 8 (6%) | 2 (2.8%) | 6 (9.5%) | 0.147 |
| Current psychological treatment, n (%) | 16 (11.9%) | 4 (5.6%) | 12 (19%) | 0.03 |
| Felt they needed mental health treatment, n (%) | 29 (21.6%) | 6 (8.5%) | 23 (36.5%) | 0.000083 |
| Used cannabis/alcohol as self-medication, n (%) | 15 (11.3%) | 5 (7%) | 10 (16.1%) | 0.098 |
| Post-traumatic symptoms (PCL-5) | ||||
| Intrusion | 1.54 (2.02) | 0.43 (0.97) | 2.65 (3.08) | 0.000007 |
| Avoidance | 0.76 (1.27) | 0.13 (0.56) | 1.38 (1.98) | 0.000045 |
| Negative alterations in cognition and mood | 3.72 (4.03) | 1.49 (2.79) | 5.94 (5.27) | 0.000001 |
| Arousal and reactivity | 3.8 (3.67) | 1.64 (2.09) | 5.96 (5.25) | 0.000001 |
| Total score | 9.09 (11.53) | 3.63 (5.59) | 15.62 (13.32) | 0.000001 |
| Burnout symptoms (MBI) | ||||
| Emotional exhaustion | 4.32 (1.52) | 3.61 (1.38) | 5.09 (1.29) | 0.000001 |
| Depersonalization | 3.37 (1.64) | 2.94 (1.46) | 3.83 (1.71) | 0.002 |
| Personal accomplishment | 5.46 (0.99) | 5.54 (0.88) | 5.36 (1.09) | 0.30 |
Fig. 1.
Group comparison of post-traumatic and burnout symptoms between low and high depression/anxiety groups. PCL-5 = PTSD checklist-5. D/A = Depression/Anxiety. ** = p < 0.01. *** = p < 0.001.
Regarding mental-health measures, the high depression/anxiety group showed significantly higher post-traumatic stress symptoms, measured by the PCL-5 (15.62 ± 13.32 vs. 3.63 ± 5.59, p < 0.0001). This difference was found in all four PTSD clusters - intrusion, avoidance, negative alterations in cognition and mood, and arousal and reactivity (see Table 1). When comparing groups of above-threshold depression only (6%), above-threshold anxiety only (23.9%), or above-threshold in both measures (17.2%), having only high anxiety was associated with a higher PCL score compared with having only high depression (9.37 vs. 2.79, respectively), and having both high anxiety and high depression was associated with the highest PCL score (24.29, F(3,110) = 28.77, p < 0.0001, Bonferroni-corrected for multiple comparisons).
Interns in the high depression/anxiety group also showed significantly higher scores in two of the three burnout subscales - emotional exhaustion (5.09 ± 1.29 vs. 3.61 ± 1.38, p = 0.000001) and depersonalization (3.83 ± 1.71 vs. 2.94 ± 1.46, p = 0.002), but the sense of personal accomplishment did not differ between groups. When comparing groups of above-threshold depression only, above-threshold anxiety only, or above-threshold in both measures, having both high anxiety and high depression was associated with the highest score in both these burnout measures ((F(14.77, p < 0.0001) for emotional exhaustion, (F(3,123) = 4.23, p < 0.001) for depersonalization), and was the only group significantly different from not having high depression or anxiety at all, when Bonferroni-correcting for multiple-comparisons). This pattern of results was not found for the personal accomplishment measure.
4. Discussion
In this study we report that medical interns who began working as physicians during the 1st year of the COVID pandemic in a large tertiary hospital in Israel, developed mental symptoms in considerable numbers. More specifically, we identified a considerable group of interns (almost half of the sample in the current study) who reported anxiety and depressive symptoms associated with their frontline work as health care providers during the pandemic. Similar findings were reported in previous disease outbreaks (e.g., the SARS epidemic in 2003 [[26], [27], [28]]) and are also emerging in growing numbers in the current COVID-19 pandemic [[29], [30], [31]], showing that frontline workers have a significantly higher risk of developing anxiety, depression, insomnia, and overall psychological problems compared with non-frontline workers [32]. Nevertheless, previous studies did not focus on medical interns but on healthcare workers in general.
Medical residency is stressful even in “plague-free” times [[33], [34], [35]], and a previous meta-analysis found that 20–40% of residents reported anxiety and depressive symptoms [36]. Furthermore, these symptoms were found to be associated with worse social skills, possibly limiting the ability of affected doctors to provide empathic patient care [[37], [38], [39]]. The fact that these symptoms were even more prevalent in the current study among the physicians at their earliest career stage, i.e., interns, and considering that internship is considered less demanding in terms of workload than residency, is notable.
In the current study, interns with high depression and/or anxiety symptoms were slightly, yet significantly younger than interns who reported fewer symptoms, possibly reflecting a protective role of age (and maturity). Interns in the high depression/anxiety group were more prone to report a need for mental health treatment, emphasizing the crucial and urgent need to facilitate mental health treatment for physicians, a population that tends to avoid mental care due to the stigma and fear of harming their medical career [40]. A significant proportion of doctors from the whole sample (10.4%) reported a need to use substances (cannabis and/or alcohol) as self-medication to get through the hardships of working in COVID-19 wards, with no significant difference between the high and low depression/anxiety groups. This too is a distressing finding. The survey was anonymous, yet the real number of substance users is probably higher than reported [41,42]. Possibly, many of these physicians felt a need to use cannabis or alcohol as self-medication to face their stressful tasks.
Interns who reacted with high depression/anxiety reported significantly more post-traumatic symptoms, and this was evident in all PTSD clusters (intrusion, avoidance, negative alterations in cognition and mood, arousal, and reactivity). Moreover, having both high anxiety and high depression was associated with more a higher PTSD measure score, compared with having either anxiety or depression, but not both. In a recent systematic review of PTSD symptoms among healthcare workers during the COVID-19 pandemic, low work experience, heavy workload and lack of training, all factors which characterize medical interns [43,44], were found to be predictors of PTSD symptoms as a psychological sequela [45]. This strengthens the need, also reflected in the current findings, for special interventions aimed at protecting these interns from harmful consequences of their work.
The high depression/anxiety group reported significantly more burnout symptoms in two domains - depersonalization and emotional exhaustion. Moreover, having both high anxiety and high depression was associated with a higher depersonalization and emotional exhaustion score. These findings are not surprising as exhaustion, a key component of burnout, is a symptom of depression as well, and there is debate about how separate these conditions are [46]. Nevertheless, these are noteworthy findings especially when appearing in such an early phase of these physicians' careers. Increased burnout rates among physicians are a well-known finding [[47], [48], [49]], and have already been described as “simmering for years” and coming to a “boil” even before the pandemic, with an estimated economical cost of billions in the United States alone [50]. Since the outbreak of the pandemic, increased burnout symptoms have been reported in all healthcare workers, but especially in frontline physicians, such as intensive care physicians [51]. Interns and resident physicians may be particularly vulnerable, the latter already shown to suffer from increased burnout during the pandemic [5,10,11].
The current study is unique in several aspects. We focused on medical interns whose first encounter with actual medical work was at the height of the COVID-19 pandemic and thus the formation of their professional identity was significantly affected by special circumstances. In Israel, internship is not a part of residency but an earlier training stage in which the intern rotates between wards.It is expected that by the end of the internship year, the interns will reach a decision regarding their desired medical residency and find a suitable position – adding stress to an already stressful situation. Accordingly, previous studies did point to an increase in depressive symptoms during the internship year [52]. Yet, this effect may be enhanced if the internship program is unexpectedly changed, as was the case in 65% of the interns in the current sample, and indeed >30% of them indicated that these changes affected their mental state to at least a moderate degree.
As opposed to many on-line survey studies which reflect participation bias, in the current study we made a special effort to reach every intern who worked during the COVID-19 pandemic in the Tel-Aviv Sourasky medical center, and indeed were able to recruit most of them (~75%). This may contribute to minimize participation bias and hence to strengthen the external validity of the findings.
The current study, however, has several limitations. First, we did not compare interns from the COVID-19 pandemic with interns who worked before the pandemic erupted. Such a comparison would have helped examine the unique contribution of the pandemic, above and beyond standard mental effects associated with medical internship and may be the focus of future studies. While we did collect and report data on past psychotropic use and past psychotherapy use, one could hypothesize an impact of prior military service, if present, particularly combat exposure. In addition, we acknowledge the fact that the interns were not asked to report their immediate status but rather recall the worst time during the 1st COVID year. Nevertheless, the survey was completed in proximity to the end of this year and thus we think the findings are reliable. The current study design also cannot prove a temporal relationship between mental-health measures; for example, we cannot conclude that anxiety and/or depression preceded post-traumatic symptoms. Nevertheless, given the fact that post-traumatic symptoms usually develop after the traumatic event (in this case, working in COVID-19 wards), there is at least some support for such a hypothesis. A recent study comparing mental health physiological parameters among physicians treating COVID-19 patients compared with non-COVID-19 patients concluded that early mental health intervention may prevent anxiety and depression symptoms to evolve into post-traumatic symptoms in susceptible physicians [53]. Lastly, as the sample included only Israeli physicians, the findings may not be generalizable to other countries, although health care systems worldwide have faced common challenges amid the COVID pandemic.
In summary, the results highlight an urgent problem: early-career physicians are sent to demanding wards, where an alarming number of them become anxious, depressed, post-traumatic and burnt out during their first year of clinical work. Healthcare systems worldwide share an essential common interest – to preserve and protect this future generation of doctors and help them thrive amid the hardships they encounter. Thus, it is crucial that health organizations implement active interventions to protect these doctors, so that they can safely embark on their medical careers with professional support that may help prevent mental health problems and enhance their ability to provide professional and compassionate care.
Author statement
R.S and O.T conceptualized the research. R.S and O.T conducted the investigation and acquired the data. R.S analyzed the data. R.S and O.T wrote the manuscript. Y.A, A.A and G.F contributed to supervising, reviewing and editing the manuscript.
References
- 1.Rumeysa E., Kurtulmus A., Arpacioglu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res [revista en Internet] 2020;290(1):1–5. doi: 10.1016/j.psychres.2020.113130. [acceso 19 de octubre de 2020]. 2020;(January) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abbasi J. Prioritizing physician mental health as COVID-19 marches on. JAMA - J Am Med Assoc. 2020;323(22):2235–2236. doi: 10.1001/jama.2020.5205. [DOI] [PubMed] [Google Scholar]
- 3.Galbraith N., Boyda D., McFeeters D., Hassan T. The mental health of doctors during the COVID-19 pandemic. BJPsych Bulletin. 2020:1–4. doi: 10.1192/bjb.2020.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dzau V.J., Kirch D.G., Nasca T.J. To care is human — collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378(4):312–314. doi: 10.1056/nejmp1715127. [DOI] [PubMed] [Google Scholar]
- 5.Kannampallil T.G., Goss C.W., Evanoff B.A., Strickland J.R., McAlister R.P., Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One. 2020;15(8 August):1–12. doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galbraith N., Boyda D., McFeeters D., Hassan T. The mental health of doctors during the COVID-19 pandemic. BJPsych Bulletin. 2021;45(2):93–97. doi: 10.1192/bjb.2020.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin K., Yang B.X., Luo D., et al. The mental health effects of COVID-19 on health care providers in China. Am J Psychiatry. 2020;177(7):635–636. doi: 10.1176/appi.ajp.2020.20040374. [DOI] [PubMed] [Google Scholar]
- 9.Reis S., Urkin J., Nave R., et al. Medical education in Israel 2016: five medical schools in a period of transition. Isr J Health Policy Res. 2016;5(1) doi: 10.1186/s13584-016-0104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Civantos A.M., Byrnes Y., Chang C., et al. Head and Neck. Vol 42. John Wiley and Sons Inc.; 2020. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study; pp. 1597–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khusid J.A., Weinstein C.S., Becerra A.Z., et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American National Survey. Int J Clin Pract. 2020;74(9) doi: 10.1111/ijcp.13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zigmond A.S., Snalth R.P. The hospital anxiety and depression scale. Acta psychiatr. Scand. [revista en internet] 2014 [acceso 28 de noviembre de 2019]; 64(5): 361-370. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 13.Xiao Y., Wang J., Chen S., et al. Psychological distress, burnout level and job satisfaction in emergency medicine: a cross-sectional study of physicians in China. EMA - Emerg Med Austral. 2014;26(6):538–542. doi: 10.1111/1742-6723.12315. [DOI] [PubMed] [Google Scholar]
- 14.Löwe B., Spitzer R.L., Gräfe K., et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78(2):131–140. doi: 10.1016/S0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 15.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 16.Hansson M., Chotai J., Nordstöm A., Bodlund O. Comparison of two self-rating scales to detect depression: HADS and PHQ-9. Br J Gen Pract. 2009;59(566):650–654. doi: 10.3399/bjgp09X454070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weathers F., Litz B.…DH Annual Convention of . 1993. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. researchgate.net. Accessed August 8, 2021. https://www.researchgate.net/profile/Frank-Weathers/publication/291448760_The_PTSD_Checklist_PCL_Reliability_validity_and_diagnostic_utility/links/57c7121208ae9d64047e9569/The-PTSD-Checklist-PCL-Reliability-validity-and-diagnostic-utility. [Google Scholar]
- 18.Marco C.A., Larkin G.L., Feeser V.R., Monti J.E., Vearrier L. Post-traumatic stress and stress disorders during the COVID-19 pandemic: survey of emergency physicians. J Am Coll Emerg Phys Open. 2020;1(6):1594–1601. doi: 10.1002/emp2.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Psychiatric Association . 5th ed. 2013. Diagnostic and statistical manual of mental disorders. [DOI] [Google Scholar]
- 20.Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. doi: 10.1002/JTS.22059. [DOI] [PubMed] [Google Scholar]
- 21.Wortmann J.H., Jordan A.H., Weathers F.W., et al. Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. 2016;28(11):1392–1403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]
- 22.Cheng P., Xu L.Z., Zheng W.H., et al. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J Affect Disord. 2020;277:368–374. doi: 10.1016/j.jad.2020.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoge C.W., Riviere L.A., Wilk J.E., Herrell R.K., Weathers F.W. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. Lancet Psychiatry. 2014;1(4):269–277. doi: 10.1016/S2215-0366(14)70235-4. [DOI] [PubMed] [Google Scholar]
- 24.Maslach C., Jackson S.E. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 25.Etzion D., Pines A. Sex and culture in burnout and coping among human service professionals: a social psychological perspective. J Cross Cult Psychol. 1986;17(2):191–209. doi: 10.1177/0022002186017002004. [DOI] [Google Scholar]
- 26.Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020;274:405. doi: 10.1016/J.JAD.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maunder R.G. Was SARS a mental health catastrophe? Gen Hosp Psychiatry. 2009;31(4):316–317. doi: 10.1016/j.genhosppsych.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weilenmann S., Ernst J., Petry H., et al. Health care Workers’ mental health during the first weeks of the SARS-CoV-2 pandemic in Switzerland—a cross-sectional study. Front Psych. 2021;12 doi: 10.3389/fpsyt.2021.594340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carmassi C., Foghi C., Dell’Oste V., et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292 doi: 10.1016/J.PSYCHRES.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amin F., Sharif S., Saeed R., Durrani N., Jilani D. COVID-19 pandemic- knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatry. 2020;20(1) doi: 10.1186/s12888-020-02864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galbraith N., Boyda D., McFeeters D., Hassan T. The mental health of doctors during the COVID-19 pandemic. BJPsych Bulletin. 2021;45(2):93–97. doi: 10.1192/bjb.2020.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Que J., Shi L., Deng J., et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatry. 2020;33(3):1–12. doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peterlini M., Tibeârio I.F., Saadeh A., Pereira J.C., Martins M.A. 2022. Anxiety and depression in the ®rst year of medical residency training. [DOI] [PubMed] [Google Scholar]
- 34.Slavin S.J., Chibnall J.T. Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med. 2016;91(9):1194–1196. doi: 10.1097/ACM.0000000000001226. [DOI] [PubMed] [Google Scholar]
- 35.Collier V.U., Mccue J.D., Markus A., Smith L. Stress in medical residency: Status quo after a decade of reform? 2002. www.annals.org [DOI] [PubMed]
- 36.Pereira-Lima K., Loureiro S.R. Burnout, anxiety, depression, and social skills in medical residents. 2015;20(3):353–362. doi: 10.1080/13548506.2014.936889. [DOI] [PubMed] [Google Scholar]
- 37.Thirioux B., Birault F., Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7(MAY) doi: 10.3389/fpsyg.2016.00763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahrweiler F., Neumann M., Goldblatt H., Hahn E.G., Scheffer C. Vol 14. 2014. Determinants of Physician Empathy during Medical Education: Hypothetical Conclusions from an Exploratory Qualitative Survey of Practicing Physicians.http://www.biomedcentral.com/1472-6920/14/122http://www.biomedcentral.com/1472-6920/14/122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hojat M., Gonnella J.S., Nasca T.J., Mangione S., Vergare M., Magee M. Vol 159. 2002. Physician Empathy: Definition, Components, Measurement, and Relationship to Gender and Specialty. [DOI] [PubMed] [Google Scholar]
- 40.Gold K.J., Andrew L.B., Goldman E.B., Schwenk T.L. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51–57. doi: 10.1016/j.genhosppsych.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 41.Baldwin D., Blazer D. 2022. Prevalence of Substance Use Among US Physicians Related Papers Guidelines for t He Use of Cont Rolled Subst Ances in the Management of Chronic Pain Andrea Trescot Illicit and Nonmedical Drug Use Among Older Adults: A Review. [Google Scholar]
- 42.Montgomery A.J., Bradley C., Rochfort A., Panagopoulou E. A review of self-medication in physicians and medical students. Occup Med. 2011;61(7):490–497. doi: 10.1093/occmed/kqr098. [DOI] [PubMed] [Google Scholar]
- 43.West C.P., Shanafelt T.D., Kolars J.C. Quality of Life, Burnout, Educational Debt, and Medical Knowledge Among Internal Medicine Residents. www.jama.com [DOI] [PubMed]
- 44.Lin Y.H., Chen H.Y., Tsai S.L., Chang L.R., Chen P.C. A prospective study of the factors associated with life quality during medical internship. PLoS One. 2019;14(8) doi: 10.1371/journal.pone.0220608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.D’ettorre G., Ceccarelli G., Santinelli L., et al. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18(2):1–16. doi: 10.3390/ijerph18020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kachadourian L.K., Feder A., Murrough J.W., et al. Transdiagnostic psychiatric symptoms, burnout, and functioning in frontline health care workers responding to the COVID-19 pandemic. J Clin Psychiatry. 2021;82(3) doi: 10.4088/JCP.20M13766. [DOI] [PubMed] [Google Scholar]
- 47.Panagioti M., Panagopoulou E., Bower P., et al. Controlled interventions to reduce burnout in physicians a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 48.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians a systematic review. JAMA - J Am Med Assoc. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shanafelt T.D., Boone S., Tan L., et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 50.Hartzband P., Groopman J. Physician burnout, interrupted. 2020;382(26):2485–2487. doi: 10.1056/NEJMP2003149. [DOI] [PubMed] [Google Scholar]
- 51.Azoulay E., De Waele J., Ferrer R., et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10(1) doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sen S., Kranzler H.R., Krystal J.H., et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67(6):557–565. doi: 10.1001/archgenpsychiatry.2010.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dolev T., Zubedat S., Brand Z., et al. Physiological parameters of mental health predict the emergence of post-traumatic stress symptoms in physicians treating COVID-19 patients. Transl Psychiatry. 2021;11(1) doi: 10.1038/s41398-021-01299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]