Abstract
Left atrial (LA) structure and function in heart failure with reduced (HFrEF) versus preserved ejection fraction (HFpEF) is only established in small studies. Therefore, we conducted a systematic review of LA structure and function in order to find differences between patients with HFrEF and HFpEF. English literature on LA structure and function using echocardiography was reviewed to calculate pooled prevalence and weighted mean differences (WMD). A total of 61 studies, comprising 8806 patients with HFrEF and 9928 patients with HFpEF, were included. The pooled prevalence of atrial fibrillation (AF) was 34.4% versus 42.8% in the acute inpatient setting, and 20.1% versus 33.1% in the chronic outpatient setting when comparing between HFrEF and HFpEF. LA volume index (LAVi), LA reservoir global longitudinal strain (LAGLSR), and E/e’ was 59.7 versus 52.7 ml/m2, 9.0% versus 18.9%, and 18.5 versus 14.0 in the acute inpatient setting, and 48.3 versus 38.2 ml/m2, 12.8% versus 23.4%, and 16.9 versus 13.5 in the chronic outpatient setting when comparing HFrEF versus HFpEF, respectively. The relationship between LAVi and LAGLSR was significant in HFpEF, but not in HFrEF. Also, in those studies that directly compared patients with HFrEF versus HFpEF, those with HFrEF had worse LAGLSR [WMD = 16.3% (22.05,8.61); p < 0.001], and higher E/e’ [WMD = −0.40 (−0.56, −0.24); p < 0.05], while LAVi was comparable. When focusing on acute hospitalized patients, E/e’ was comparable between patients with HFrEF and HFpEF. Despite the higher burden of AF in HFpEF, patients with HFrEF had worse LA global function. Left atrial myopathy is not specifically related to HFpEF.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10741-021-10204-8.
Keywords: LA structure, Function, HFrEF, HFpEF
Introduction
The left atrium can be considered a transporting chamber that optimizes left ventricular (LV) filling [1]. Left atrial (LA) hypertension with subsequent pulmonary venous congestion is the hallmark of HF regardless of LV ejection fraction (LVEF) [2, 3]. More recently, the significant pathophysiological role of LA dysfunction in HF has gained increasing attention, particularly in HF with preserved EF (HFpEF) [3–5]. Over the past decades, the incidence of HFpEF has risen relative to HF with reduced ejection fraction (HFrEF), accounting now for approximately 50% of cases of HF [6, 7]. Studies have shown that atrial fibrillation (AF), diabetes, and obesity are risk factors for the development of HFpEF, whereas coronary artery disease (CAD) and myocardial infarction are more predisposed to the development of HFrEF [6, 7]. The close link between AF and HFpEF might be explained by intrinsic LA myopathy underlying both HFpEF and AF [8].
However, information regarding differences in LA structure and function between HFrEF and HFpEF, particularly LA functional information assessed by strain analysis, is scarce and not fully understood. Thus, we aimed to conduct a systematic review of LA structure and function assessed by echocardiography in patients with HFrEF versus HFpEF.
Methods
The systemic review and meta-analysis were conducted according to the Preferred Reporting items for Systemic Reviews and Meta-Analysis (PRISMA) statement [9]. The review protocol had been registered with PROSPERO (http://www.crd.york.ac.uk/PROSPERO).
Literature search strategy
We performed a systematic search in the MEDLINE and EMBASE database from inception through February 2021. Our search was restricted to studies in the English language. Additional studies were selected by reviewing and searching references of identified articles, which were not identified by the initial search. Search terms are mainly composed of the patient domain, including “heart failure,” “heart failure with preserved ejection fraction” and “heart failure with reduced ejection fraction,” and outcome domain as LA structure and function related terms, respectively. The detailed search strategy was described in the online supplementary Table S1.
Study selection
Studies were eligible if they were performed in a clearly defined group of patients with HFrEF or HFpEF or both. The study population had to have a clinical diagnosis of HF, based on signs and symptoms such as dyspnea, fatigue at rest or during exercise, or a previous HF hospitalization. At least one measure of LA structure and function assessed by echocardiography had to be reported. For HFrEF versus HFpEF categorization, the cutoff value of LVEF assessed by echocardiography had to be 45% or 50%. Elevated natriuretic peptides were recognized, but not mandatory for study inclusion. Two authors (XY.J, K.TH.T) independently screened the titles and abstracts of retrieved citations to identify potentially relevant studies. If abstracts were ambiguous, studies were reviewed at the full-text level. Citations were included when consensus between two authors was achieved.
Data extraction
For each included study, the following data of study participants were extracted: (1) baseline characteristics [i.e., publication year, the total number of study participants, the clinical setting of HF (i.e., inpatient vs outpatient setting), age, sex, body mass index (BMI), hypertension, ischemic heart disease (IHD), atrial fibrillation (AF), diabetes, and presence of more than moderate functional mitral regurgitation (MR)], (2) echocardiographic characteristics [i.e., LVEF, LV global longitudinal strain (GLS), the ratio of mitral valve peak velocity of early and late LV filling (E/A), mitral annulus e’ velocity (e’), E/e’ ratio, LA (reservoir, booster, conduit) GLS, software used for post-offline analysis]. When longitudinal studies reported cardiovascular outcomes (mortality and hospitalization), unadjusted and adjusted hazard ratio (HR) for the association between the LA-related parameter with outcomes were obtained. Follow-up time in months, outcome measure, and variables for which was adjusted were also obtained.
Quality assessment
To perform a quality assessment of included studies, the Newcastle–Ottawa scale adapted for observational studies [10] was used scoring each study on several items (i.e., selection process, comparability, and assessment of the outcome/exposure criterion). Moreover, the quality of the clinical trials was evaluated using the revised Cochrane risk-of-bias tool (RoB 2.0) [11], covering five domains (randomization, intervention, missing data, outcome measure, and reported results) of included studies.
Statistical analysis
Continuous variables were reported as mean ± standard deviation (SD), and categorical variables as percentage. When only medians and interquartile ranges were reported in the study, we translated those into means and SDs by an established formula based on previous recommendations [12].
The summary and pooled values of corresponding LA parameters were calculated by the weighted average based on the number of patients among included studies and depicted in forest plots for HFrEF and HFpEF, respectively. The prevalence of comorbidities for included studies was pooled by the weighted average according to the number of patients for HFrEF and HFpEF, respectively. Data on LA related echocardiographic parameters in both patients with HFrEF and HFpEF were pooled to derive weighted mean differences (WMDs) and 95% confidence intervals (CI). Linear regression and the mixed-effects meta-regression model were applied to investigate the relationship of LAGLSR with LAVi and LVGLS in patients with HFrEF and HFpEF, respectively. Random effects model with inverse variance weighting was performed using the Cochrane I2 statistic to account for heterogeneity across the studies. All statistical analyses were performed using RStudio version 1.1456.
Results
Study characteristics and quality assessment
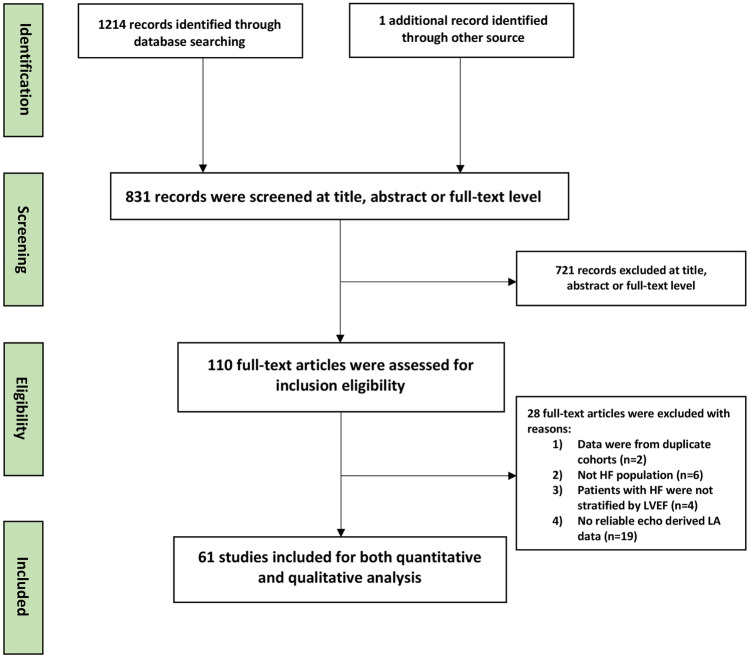
The search strategy and study selection are summarized in the PRISMA flowchart [9] (Fig. 1). Of 1114 studies identified, a total of 61 studies were selected for the final quantitative and qualitative analysis. The quality assessment of included studies is shown in the supplementary material online (Tables S2 and S3). Reasons for exclusions were described in the supplementary Table S4. Among 61 studies, 27 studies (including 8806 patients with HFrEF and 38 studies including 9928 patients with HFpEF) reported LA structural and functional parameters by echocardiography. Nine out of 61 studies included both patients with HFrEF (n = 1877) and HFpEF (n = 3085). Nine out of 61 studies included patients with HF from an acute inpatient setting (HFrEF, n = 2749; HFpEF, n = 3319), whereas fifty-two studies included patients with HF from a chronic stable outpatient setting (HFrEF, n = 6057; HFpEF, n = 6714). The pooled clinical and echocardiographic characteristics in patients with HFrEF versus HFpEF in the acute inpatient versus chronic outpatient setting were described separately in Table 1. Moreover, the details of clinical and echocardiographic characteristics of included studies are described in Tables 2 and 3.
Fig. 1.
PRISMA flowchart of process for literature search and study selection. HF, heart failure; LA, left atrial, LVEF, left ventricular ejection fraction
Table 1.
The pooled clinical and echocardiographic characteristics in patients with HFrEF versus HFpEF
| Acute inpatient setting | Chronic outpatient setting | |||
|---|---|---|---|---|
| HFrEF (n = 2749) | HFpEF (n = 3319) | HFrEF (n = 6057) | HFpEF (n = 6714) | |
| Age (years) | 69.0 | 73.0 | 60.8 | 67.3 |
| Sex (female, %) | 37.8% | 57.8% | 28.7% | 58.9% |
| Diabetes (%) | 36.6% | 37.1% | 28.2% | 33.2% |
| AF (%) | 34.4% | 42.8% | 20.1% | 33.1% |
| IHD (%) | 39.8% | 30.7% | 49.8% | 33.3% |
| BMI (kg/m2) | 25.2 | 25.6 | 27.5 | 29.8 |
| Presence of moderate to severe mitral regurgitation (%) | - | - | 27.2% | 12.0% |
| LVEF (%) | 25.6 | 60.1 | 27.9 | 61.8 |
| LVGLS (%) | −12.5 | −15.1 | −8.4 | −16.5 |
| MV e’(cm/s) | 4.7 | 6.6 | 6.5 | 7.5 |
| E/e’ | 18.5 | 14.0 | 16.9 | 13.5 |
| LAVi (ml/m2) | 59.7 | 52.7 | 48.3 | 38.2 |
| LAGLSR (%) | 9.0 | 18.9 | 12.8 | 23.4 |
| LAGLSB (%) | - | - | 7.7 | 13.9 |
| LAGLSC (%) | - | - | - | 15.8 |
HFrEF heart failure with reduced ejection fraction, HFpEF heart failure with preserved ejection fraction, AF atrial fibrillation, IHD ischemic heart disease, BMI body mass index, LVEF left ventricle ejection fraction, LVGLS left ventricle global longitudinal strain, MV e’ mitral annular early diastolic velocity by tissue doppler, E/e’ the ratio between early mitral inflow velocity and mitral annular early diastolic velocity, LAVi left atrial volume index, LAGLSR left atrial global longitudinal strain at reservoir phase, LAGLSB left atrial global longitudinal strain at booster phase, LAGLSC left atrial global longitudinal strain at conduit phase
Table 2.
Clinical characteristics of included studies
| Author/year | Study design | Study setting | Heart failure phenotype examined | LVEF cutoff | Number of patients (n) | Age (years) | Female sex (%) | Atrial fibrillation (%) | Diabetes mellitus (%) | Hypertension (%) | Ischemic heart disease (%) | BMI (kg/m2) | Moderate to severe mitral regurgitation | LA structure and functional parameters measured |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hoshida et al. [27] | Prospective multi-center observational study | CHF, inpatient setting | HFpEF | ≥ 50% | 105 | 78.5 ± 10.2 | 53.3% | 41% | 88% | 24.3 ± 5.0 | LAVi, E/e' | |||
| Harada et al. [28] | Prospective single-center cohort study | AHF, compensatory inpatient setting | HFpEF | ≥ 45% | 92 | 73.0 ± 12.8 | 59% | 47% | 27% | 72% | 34% | 22.3 ± 3.6 | LAVi, E/e', e' | |
| Hwang et al. [29] | Prospective multi-center observational study | AHF, multi-center, inpatient setting | HFpEF | ≥ 50% | 1105 | 76.0 ± 9.6 | 60.6% | 32.9% | 32.4% | 64.3% | 29.3% | 23.9 ± 3.7 | LAVi, E/e' LA reservoir strain | |
| Shah et al. [30] | Retrospective cohort study | CHF, inpatient setting | HFrEF | ≤ 40% | 67 | 49.5 ± 11.4 | 34.3% | 9% | 64.2% | 35.8% | 31.8 ± 7.0 | LAVi, E/e' | ||
| HFrEF | ≤ 40% | 69 | 57.5 ± 15.3 | 24.6% | 8.7% | 60.9% | 36.2% | 31.1 ± 7.3 | LAVi, E/e' | |||||
| Tanaka et al. [31] | Retrospective cohort study | CHF, outpatient setting | HFrEF | ≤ 45% | 205 | 59 ± 17 | 31% | 14% | 27% | 19% | 32% | LAVi, E/e' | ||
| Castrichini et al. [32] | Prospective single-center cohort study | CHF, outpatient setting | HFrEF | < 40% | 77 | 65 ± 11 | 12.1% | 37.7% | 45.5% | 54.5% | 40.3% | 32% | LAVi, E/e', LA reservoir strain | |
| Valentim et al. [33] | Prospective single-center cohort study | CHF, outpatient setting | HFrEF | < 40% | 42 | 58.6 ± 11.1 | 17.1% | 40% | 31.4% | 42.9% | 28.1 ± 3.8 | LAVi, E/e' | ||
| Kurzawski et al. [34] | Retrospective single-center cohort | CHF, inpatient and outpatient settings | HFrEF | < 25% | 63 | 61.9 ± 10.9 | 4.8% | 33.3% | 54% | 52.4% | 26.2 ± 4.5 | LAVi, E/e', LA reservoir strain | ||
| Park et al. [16] | Retrospective cohort study | AHF, multi-center, inpatient setting | HFpEF | ≥ 50% | 1191 | 73.4 ± 13.3 | 60.3% | 35% | 31% | 62% | 27.4% | 23.8 ± 4.1 | LAVi, E/e', LA reservoir strain, e' | |
| HFrEF | < 40% | 2036 | 68.4 ± 14.1 | 38.3% | 24.9% | 36.3% | 54.2% | 34.4% | 23.1 ± 4.3 | |||||
| Deferm et al. [35] | Prospective single-center cohort study | ADHF (Acute decompensated HF), inpatient setting | HFrEF | ≤ 40% | 31 | 64 ± 15 | 22.6% | 32.3% | 29% | 48.4% | 48.4% | 28.1 ± 6.0 | 51.6% | LAVi, E/e' LA reservoir strain |
| Shah et al. [36] | Randomized, multi-center double-blind placebo controlled trial | CHF, multi-centers (752 sites in 43 countries), inpatients and outpatient settings | HFpEF (PARAGON-HF trial-ECHO study | ≥ 45% | 1097 | 74 ± 8 | 53% | 35% | 40% | 94% | 30% | 29.9 ± 4.9 | 12% | LAVi, E/e', E/A, e' |
| Reddy et al. [14] | Prospective single-center cohort study | CHF, single-center, outpatient setting | HFpEF | ≥ 50% | 238 | 68 ± 10 | 62% | 17% | 29% | 90% | 32% | 32.9 ± 7.1 | LAVi, LA Reservoir, conduit and contractile strain | |
| Modin et al. [18] | Retrospective single-center cohort study | CHF, outpatient setting | HFrEF | ≤ 45% | 818 | 66.4 ± 11.4 | 26.6% | 15.3% | 11.4% | 41.2% | 55.9% | 26.4 ± 4.8 | 9% | LAVi, E/e', E/A, e' |
| Shintani et al. [37] | Retrospective single-center cross-sectional study | AHF, inpatient setting | HFpEF | ≥ 50% | 127 | 80.6 ± 8.1 | 50% | 52% | 41% | 67% | 23.2 ± 3.7 | LAVi | ||
| HFrEF | < 40% | 617 | 75.0 ± 11.1 | 33% | 48% | 37% | 71% | 22.5 ± 3.7 | ||||||
| Wu et al. [38] | Prospective single-center cohort study | CHF, inpatient setting | HFpEF | ≥ 50% | 163 | 61.1 ± 15.3 | 61% | 30.1% | 60.1% | 3.5% | 25.9 ± 4.2 | LAVi, E/e', E/A, e' | ||
| HFrEF | < 40% | 34 | 54.5 ± 15.4 | 18% | 17.6% | 44.1% | 44.1% | 25.2 ± 4.7 | ||||||
| Telles et al. [39] | Prospective single-center cohort study | CHF, inpatient setting | HFpEF | ≥ 50% | 49 | 69.4 ± 8.0 | 71.4% | 26.5% | 14% | 67% | 14% | 30.2 ± 5.0 | LAVi, E/e', LA reservoir strain, conduit, e', E/A | |
| Sobirin et al. [40] | A single-center, unblind, randomized, controlled clinical trial | CHF, outpatient setting | HFpEF | > 50% | 30 | 62 ± 8 | 50% | 73.3% | LAVi, E/e' | |||||
| Lundberg et al. [41] | Prospective single-center cohort study | CHF, inpatient setting | HFpEF | ≥ 50% | 92 | 73.0 ± 8.8 | 62% | 48% | 19% | 69% | 3% | 26.6 ± 5.2 | LAVi, E/e', LA reservoir strain, e', E/A | |
| HFrEF | < 50% | 72 | 56.3 ± 12.6 | 21% | 46% | 18% | 58% | 26% | 27.3 ± 5.2 | |||||
| Saikhan et al. [42] | Prospective single-center cohort study | CHF, outpatient setting | HFpEF | ≥ 50% | 110 | 63 ± 11 | 38.1% | excluded | 48.1% | 82.7% | 60% | 27.8 ± 5.4 | LAVi, LA Reservoir, conduit and contractile strain | |
| Burns [43] | Prospective single-center cohort study | CHF, outpatient setting | HFpEF with anemia | ≥ 50% | 224 | 65 ± 12 | 56% | 26% | 37% | 79% | 50% | 32 ± 10 | LAVi, E/e', e' | |
| HFpEF without anemia | ≥ 50% | 195 | 63 ± 13 | 69% | 27% | 28% | 75% | 46% | 33 ± 9 | |||||
| Obokata et al. [44] | Prospective single-center cohort study | CHF, inpatient and outpatient settings | HFpEF | ≥ 50% | 271 | 71 ± 9 | 56% | 42% | 33% | 84% | 57% | 32 ± 7 | LAVi, E/e', e' | |
| Nagy et al. [45] | Subset of prospective, observational, multi-center study | CHF, inpatient setting | HFpEF | ≥ 45% | 86 | 72 ± 10 | 51% | 60% | 33% | 79% | 15% | 30 ± 5 | LAVi, E/e', LA reservoir strain, e, E/A ratio' | |
| Carluccio et al. [19] | Prospective single-center cohort study | CHF, outpatient setting | HFrEF | ≤ 40% | 405 | 65.2 ± 12.3 | 24% | 26% | 38% | 26.6 ± 4.1 | LAVi, E/e', LA reservoir strain, e, E/A ratio' | |||
| Malagoli et al. [46] | Prospective single-center cohort | CHF, outpatient setting | HFrEF | < 40% | 286 | 67 ± 11 | 19% | 64% | LAVi, LA Reservoir strain | |||||
| Eroglu et al. [47] | Retrospective cohort | CHF, outpatient setting | HFrEF | < 50% | 59 | 57 ± 13 | 23% | 84% | LAVi, E/e', E/A, e' | |||||
| Almeida et al. [48] | Retrospective case–control study | AHF, inpatient setting | HFpEF | ≥ 50% | 65 | 55% | 47.7% | 80% | 33.8% | LAVi, E/e' | ||||
| HFrEF | < 40% | 65 | 43.1% | 70.8% | 44.6% | |||||||||
| Liu et al. [49] | Prospective single-center study | CHF, inpatient setting | HFpEF | ≥ 50% | 55 | 61 ± 13 | 54.5% | 43% | 93% | 33% | LAVi, E/e', LA reservoir strain, e', E/A | |||
| Shah et al. [50] | Prospective multinational multi-center observational study | CHF, outpatient setting | HFpEF | ≥ 40% | 51 | 72.4 ± 9.0 | 63% | 35% | 25% | 92% | 16% | 32.5 ± 10.7 | LAVi, E/e', LA reservoir strain | |
| CHF, outpatient setting | HFpEF | ≥ 40% | 151 | 74.7 ± 8.7 | 52% | 58% | 30% | 81% | 21% | 29.0 ± 8.5 | LAVi, E/e', LA reservoir strain | |||
| Xu et al. [51] | Retrospective, single-center cohort | CHF, inpatient setting | HFrEF | < 40% | 28 | 38 ± 14 | 18% | 20.6 ± 3.2 | 57.1% | |||||
| CHF, inpatient setting | HFrEF | < 40% | 17 | 42 ± 10 | 41% | 22.5 ± 5.2 | 17.6% | |||||||
| Saha et al. [52] | Retrospective, single-center cohort | CHF, outpatient setting | HFrEF | < 40% | 49 | 72 ± 13 | 42% | 8% | 12% | 68% | E/e', LA reservoir strain | |||
| Abohammar et al. [53] | Prospective single-center observational study | AHF, inpatient setting | HFpEF | > 50% | 114 | 59 ± 8 | 55% | 64% | 64% | 16% | 27 ± 3 | LAVi, E/e' | ||
| Modin et al. [54] | Retrospective single-center cohort | CHF, outpatient setting | HFrEF | < 45% | 151 | 70.5 ± 9.2 | 21.2% | 9.2% | 43% | 26.7 ± 5.1 | LAVi, E/e' | |||
| Batalli [55] | Prospective single-center cohort | CHF | HFpEF | NA | 55 | 63.0 ± 6.8 | Excluded | 59% | 41% | 29 ± 4 | E/e' | |||
| HFrEF | NA | 56 | 62 ± 12 | Excluded | 38% | 45% | 28.0 ± 3.6 | |||||||
| Sugimoto et al. [56] | Prospective single-center study | CHF, outpatient setting | HFpEF | > 50% | 20 | 72.6 ± 10.3 | 60% | 42% | 74% | 10% | 28.3 ± 5.0 | LAVi, E/e', LA reservoir strain, E/A | ||
| HFrEF | < 40% | 49 | 63.1 ± 12.9 | 31% | 35% | 63% | 52% | 26.7 ± 4.5 | ||||||
| Hage et al. [57] | Subset of prospective observational multicenter study | AHF, inpatient setting | HFpEF | > 45% | 86 | 72.3 ± 8.9 | 51% | 57% | 31% | 79% | 34% | 28.8 ± 5.9 | LAVi, E/e' | |
| Sargento et al. [58] | Prospective single-center observational study | CHF, outpatient setting | HFrEF | < 40% | 203 | 67.8 ± 12.5 | 26.6% | 26.1% | 32% | 88.7% | 39.4% | 27.2 ± 4.4 | LAVi | |
| Aung et al. [59] | Prospective two center study | CHF | HFpEF | ≥ 50% | 38 | 65.2 ± 5.7 | 50% | 13.2% | 60.5% | 47.4% | 28.1 ± 2.0 | LAVi, E/e', LA reservoir strain, contractile, e' | ||
| Hung [60] | Prospective single-center cohort study | CHF, outpatient setting | HFpEF | ≥ 50% | 58 | 64.3 ± 12.4 | 53.4% | 32.8% | 74.1% | 27.2 ± 3.7 | E/e', LA reservoir strain, e', E/A | |||
| Freed et al. [61] | Prospective single-center cohort study | CHF, outpatient setting | HFpEF | ≥ 50% | 308 | 65 ± 13 | 64% | 26% | 30% | 75% | 50% | 31.5 ± 8.6 | 14% | LAVi, LA Reservoir, conduit and contractile strain, E/e', E/A |
| Unger et al. [62] | Prospective single-center cohort | CHF, outpatient setting | HFpEF without CKD | > 50% | 154 | 60.9 ± 12.3 | 62% | 22% | 21% | 68% | 46% | 31.8 ± 8.7 | LAVi, E/e', LA reservoir, conduit and booster strain | |
| HFpEF with CKD | > 50% | 145 | 69.3 ± 12.1 | 66% | 30% | 39% | 83% | 52% | 31.5 ± 8.4 | LAVi, E/e', LA reservoir, conduit and booster strain | ||||
| Georgievska-Ismail et al. [63] | Prospective single-center, cross-sectional study | CHF, outpatient setting | HFpEF | > 50% | 108 | 63.2 ± 8.9 | 60.2% | 98.1% | 18.5% | 29.9 ± 3.8 | ||||
| Melenovsky et al. [17] | Retrospective single-center cohort study | CHF, outpatient setting | HFpEF | ≥ 50% | 101 | 71 ± 10 | 58% | 42% | 47% | 93% | 44% | 34.0 ± 8.6 | LAVi,e' | |
| HFrEF | < 50% | 97 | 61 ± 13 | 20% | 26% | 41% | 56% | 46% | 31.0 ± 6.9 | |||||
| Gracia et al. [64] | Prospective single-center cohort study | CHF, outpatient setting | HFpEF | ≥ 50% | 28 | 60 ± 2 | 40% | 90% | LAVi, E/e', E/A, e' | |||||
| Hasselberg et al. [65] | Prospective single-center Cross-sectional study | CHF, inpatient setting | HFpEF | ≥ 50% | 37 | 58 ± 11 | 32.4% | 14% | 41% | 60% | 26 ± 4 | LAVi, E/e', E/A, e' | ||
| Sanchis et al. [15] | Prospective single-center cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 63 | 76 ± 8 | 71.4% | 39.7% | 23.8% | 85.7% | 30 ± 5 | LAVI, E/e', LA reservoir strain | ||
| Shah et al. [66] | International, multicenter, randomized, double blind placebo-controlled trial (with an echo substudy) | CHF, multi-center (270 sites in 6 countries) | HFpEF (TOPCAT-ECHO) | ≥ 45% | 935 | 69.9 ± 9.7 | 49% | 38% | 40% | 91% | 60% | 32.6 ± 7.5 | LAVi, E/e', LA reservoir, contractile strain, E/A, e' | |
| Santos et al. [67] | Echo substudy multicenter, international, randomized, double blind placebo-controlled trial | CHF, multi-centers (65 centers in 13 countries) | HFpEF (PARAMOUNT trial) | ≥ 45% | 135 | 70 ± 9 | 61% | 23% | 35% | 92% | 22% | 29.6 ± 5.7 | LAVi, LA Reservoir, conduit and contractile strain, E/e', E/A | |
| HFrEF | < 40% | 32 | 74 ± 12 | 37.5% | 50% | 43.8% | 78.1% | |||||||
| Donal et al. [68] | Prospective, multi-center international observational study | AHF inpatient setting | HFpEF | ≥ 45% | 539 | 77 ± 19 | 56% | 30% | 78% | 43.5% | 29 ± 6 | LAVi, E/e', E/A, e' | ||
| Burke et al. [69] | Prospective single-center cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 419 | 65 ± 13 | 62% | 26% | 33% | 77% | 48% | 33 ± 9 | 14% | LAVi, E/e', e' |
| Motoki et al. [70] | Prospective single-center cohort | CHF, outpatient setting | HFrEF | ≤ 35% | 108 | 57 ± 15 | 23% | excluded | 27% | 51% | 45% | LAVi, E/e', LA reservoir strain, contractile, e' | ||
| Obokata et al. [71] | Prospective single-center cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 40 | 77 ± 13 | 65% | 35% | 88% | 22 ± 5 | LA reservoir strain, E/e', e', E/A | |||
| Carluccio et al. [72] | Prospective single-center observational study | CHF, outpatient setting | HFrEF | < 45% | 747 | 68 ± 12 | 22% | 16% | 22% | 48% | 26 ± 4 | 32% | LAVi, E/e' | |
| Gupta et al. [73] | Prospective on-going multi-comunities cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 85 | 61.6 ± 6.9 | 85% | 42% | 85% | 13% | 32.6 ± 5.9 | 0% | E/A | |
| HFrEF | < 50% | 31 | 60.9 ± 8.0 | 65% | 68% | 84% | 32% | 33.7 ± 9.6 | 10% | |||||
| Oh et al. [23] | International randomized trial | CHF, international (122 sites in 26 countries) | HFrEF | ≤ 35% | 2006 | 60.9 ± 9.5 | 13.6% | 5% | 37% | 60% | 99% | 24% | LAVi, E/e', E/A, e' | |
| Zile et al. [74] | Echo-cohort of placebo-controlled double-blind multi-center international parallel study | CHF, inpatient and outpatient settings | HFpEF (I-PRESERVE-Echo cohort) | ≥ 45% | 745 | 72 ± 7 | 62% | 26% | 25% | 92% | 33% | 30 ± 5 | E/e', LA area, e' | |
| Tan et al. [75] | Prospective single-center cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 50 | 72 ± 8 | 70% | excluded | 30% | 100% | 18% | 31 ± 5 | LAVi | |
| Jaubert et al. [76] | Prospective single-center cohort | CHF, inpatient setting | HFpEF | ≥ 45% | 59 | 64 ± 12 | 37% | 36% | 58% | 49% | 27 ± 5 | LAVi, E/e', e' | ||
| Hinderliter et al. [77] | Prospective cohort | CHF, outpatient setting | HFrEF | ≤ 40% | 211 | 57 ± 12 | 31% | 19% | 44% | 77% | 43% | 31.2 ± 7.2 | LAVi | |
| Donal et al. [78] | Prospective multi-center cohort | CHF, outpatient setting | HFrEF | < 35% | 75 | 59 ± 11 | 82.7% | 34.7% | LAVi | |||||
| Jasic-Szpak et al. [79] | Prospective single-center cohort | CHF, outpatient setting | HFpEF without AF | ≥ 50% | 131 | 63.7 ± 8.0 | 73% | 0 | 37% | 89% | - | 29.4 ± 4.1 | - | LAVi, LA Reservoir, conduit and contractile strain, E/e', E/A |
| Prospective single-center cohort | CHF, outpatient setting | HFpEF with AF | ≥ 50% | 39 | 67.4 ± 8.9 | 72% | 100% | 49% | 97% | - | 30.4 ± 4.3 | - | ||
| CarluccioE [80] | Prospective single-center cohort | CHF, outpatient setting | HFpEF | ≥ 50% | 46 | 75 ± 8 | 52% | - | 35% | 91% | - | LAVi, E/e', E/A |
ADHF acute decompensated heart failure, AHF acute heart failure, CHF chronic heart failure, CKD chronic kidney disease, HFpEF heart failure with preserved ejection fraction, HFrEF heart failure with reduced ejection fraction, LA left atrial, LAVi left atrial volume index, e’ mitral annular early diastolic velocity by tissue doppler, E/A the ratio between early and late mitral inflow velocity by doppler, E/e’ the ratio between early mitral inflow velocity and mitral annular early diastolic velocity
Table 3.
Echocardiographic characteristics of included studies
| Author/year | HF phenotype | Number of patients (n) | LAVi | LAGLSR (%) | LAGLSB (%) | LAGLSC (%) | E/e' | MV E/A | Mitral annulus e' | LVEF | LVGLS | Software for Speckle tracking analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hoshida et al. [27] | HFpEF | 105 | 47.6 ± 24.2 | 14.4 ± 5.7 | 60.9 ± 6.9 | |||||||
| Harada et al. [28] | HFpEF | 92 | 54.6 ± 26,7 | 17.7 ± 7.3 | 5.2 ± 1.7 | 57.8 ± 9.4 | −13.9 ± 4.4 | EchoPAC | ||||
| Hwang et al. [29] | HFpEF | 1105 | 49.9(34.5–69.8) | 18.6 ± 11.6 | 15.1 ± 7.1 | 0.9 ± 0.5 | 5.6 ± 2.5 | 59.3 ± 6.6 | −15.1 ± 5.0 | TomTec | ||
| Park et al. [16] | HFpEF | 1191 | 63 ± 48.8 | 19.1 ± 11.6 | 16.9 ± 9.2 | 5.9 ± 2.4 | 59.1 ± 5.9 | TomTec | ||||
| Sobirin et al. [40] | HFpEF | 30 | 33.0 ± 8.0 | 18.6 ± 3.4 | 1.09 ± 0.5 | 6.0 ± 1.6 | 56.0 ± 7.0 | |||||
| Shah et al. [36] | HFpEF | 1097 | 38.9 ± 15.5 | 12.6 ± 5.7 | 1.33 ± 0.73 | 7.9 ± 2.5 | 58.6 ± 9.8 | |||||
| Reddy et al. [14] | HFpEF | 238 | 32 ± 15 | 29 ± 16 | 18 ± 10 | 16 ± 9 | 14 ± 6 | −15 ± 3 | Syngo | |||
| Shintani et al. [37] | HFpEF | 127 | 66.0 ± 27.4 | |||||||||
| Wu et al. [38] | HFpEF | 163 | 37.1 ± 8.1 | 16.5 ± 2.4 | 0.7 ± 0.1 | 68.0 ± 9.0 | ||||||
| Telles et al. [39] | HFpEF | 49 | 41.5 ± 15.2 | 24.3 ± 9.6 | 16.1 ± 5.9 | 12.9 ± 5.7 | 1.4 ± 0.6 | 9.4 ± 2.4 | 62.6 ± 6.1 | −18.7 ± 2.3 | TomTec | |
| Lundberg et al. [41] | HFpEF | 92 | 43.0 ± 14.0 | 12.3 ± 8.0 | 13.4 ± 6.6 | 1.4 ± 0.9 | 8.5 ± 3.2 | 60.7 ± 5.9 | −17.3 ± 4.4 | EchoPAC | ||
| Shah et al. [50] | HFpEF-absent CMD | 51 | 36.5 ± 11 | 19.8 ± 8.3 | 12.4 ± 4.7 | 1.2 ± 0.9 | 8.1 ± 2.4 | 60.9 ± 6.4 | −17 ± 3.5 | TomTec | ||
| HFpEF-present CMD | 151 | 39.3 ± 13.4 | 15.0 ± 7.7 | 13.5 ± 6.2 | 1.5 ± 0.9 | 8.9 ± 5.9 | 58.5 ± 8.1 | −15.7 ± 3.5 | TomTec | |||
| Abohammar et al. [53] | HFpEF | 114 | 47.0 ± 7.0 | 12.2 ± 2.0 | 1.6 ± 0.7 | 7.0 ± 3.0 | 61.0 ± 3.0 | −13.5 ± 1.5 | EchoPAC | |||
| Saikhan et al. [42] | HFpEF | 110 | 38.8 ± 12.7 | 26.2 ± 1.9 | 13.1 ± 4.4 | 13 ± 1.1 | 11.7 ± 4.5 | 0.9 ± 0.3 | 7.1 ± 2.1 | 64.9 ± 7.7 | EchoPAC | |
| Burns et al. [43] | HFpEF-Anemia | 224 | 36.6 ± 15.8 | 16.1 ± 8.8 | 1.5 ± 0.8 | 9.6 ± 3.8 | 61.0 ± 7.0 | |||||
| HFpEF-No Anemia | 195 | 31.3 ± 11.9 | 14.0 ± 7.3 | 1.2 ± 0.6 | 7.1 ± 2.7 | 61.0 ± 6.0 | ||||||
| Obokata et al. [44] | HFpEF | 271 | 44 ± 15 | 16 ± 8 | 6.6 ± 2 | 62 ± 7 | ||||||
| Nagy et al. [45] | HFpEF | 86 | 44 ± 16 | 13.3 ± 11.0 | 12.6 ± 6 | 1.8 ± 1.4 | 7.9 ± 2.2 | 62.5 ± 7.0 | −15.3 ± 3.6 | TomTec | ||
| Almeida et al. [48] | HFpEF | 65 | 48.0 ± 19.4 | 16.0 ± 8.1 | 58.0 ± 5.9 | −14.0 ± 3.7 | EchoPAC | |||||
| Liu et al. [49] | HFpEF | 55 | 37.5 ± 8.3 | 20.4 ± 7.4 | 10.8 ± 4.2 | 12.8 ± 5.8 | 1.09 ± 0.73 | 7.7 ± 2.4 | 59.5 ± 6.5 | EchoPAC | ||
| Batalli et al. [55] | HFpEF | 55 | 9.4 ± 4.7 | 0.8 ± 0.3 | 6.7 ± 2.6 | 59.6 ± 8.7 | Philips iE33 | |||||
| Sugimoto et al. [56] | HFpEF | 20 | 52.0 ± 24.0 | 14.7 ± 7.4 | 20.0 ± 8.0 | 1.3 ± 0.9 | 56.0 ± 11.0 | EchoPAC | ||||
| Hage et al. [57] | HFpEF | 86 | 44.4 ± 11.6 | 11.0 ± 4.2 | 1.5 ± 1.1 | 8.3 ± 2.2 | 63.3 ± 7.4 | |||||
| Freed et al. [61] | HFpEF | 308 | 34.4 ± 13.7 | 36.2 ± 14.9 | 18.3 ± 7.7 | 19.8 ± 8.5 | 15.0 ± 8.1 | 1.3 ± 0.7 | 7.0 ± 2.7 | 61.0 ± 6.4 | − 7.5 ± 4.1 | TomTec |
| Aung et al. [59] | HFpEF | 38 | 43.7 ± 9.4 | 17.0 ± 4.1 | 11.0 ± 2.4 | 11.6 ± 1.8 | 0.7 ± 0.2 | 5.6 ± 1.5 | 62.9 ± 4.2 | EchoPAC | ||
| Hunget al. [60] | HFpEF | 58 | 28.2 ± 6.4 | 16.3 ± 6.3 | 5.9 ± 1.9 | 62.1 ± 6.3 | −15.7 ± 1.8 | EchoPAC | ||||
| Unger et al. [62] | HFpEF-no CKD | 154 | 32.5 ± 12.0 | 36.7 ± 16.3 | 19.1 ± 8.3 | 19.6 ± 8.9 | 11.8 ± 7.7 | 1.3 ± 0.7 | 10.1 ± 4.1 | 61.5 ± 6.3 | −18.2 ± 4.0 | TomTec |
| HFpEF-CKD | 145 | 36.5 ± 15.4 | 28.8 ± 14.9 | 15.9 ± 7.9 | 15.4 ± 7.2 | 14.8 ± 7.6 | 1.4 ± 0.7 | 8.5 ± 3.4 | 60.9 ± 6.6 | −16.8 ± 4.1 | TomTec | |
| Shah et al. [66] | HFpEF | 935 | 28.0 ± 10.3 | 10.9 ± 4.7 | 1.09 ± 0.53 | 7.6 ± 3.1 | 60.0 ± 6.4 | |||||
| Melenovsky et al. [17] | HFpEF | 101 | 41.0 ± 12.0 | 7.7 ± 2.2 | 62.0 ± 5.9 | |||||||
| Hasselberg et al. [65] | HFpEF | 37 | 45.0 ± 22.0 | 11.0 ± 5.0 | 1.5 ± 1.1 | 7.1 ± 2.0 | 62.0 ± 7.0 | −17.5 ± 3.2 | EchoPAC | |||
| Gracia et al. [64] | HFpEF | 28 | 32.6 ± 12.0 | 12.3 ± 3.6 | 1.0 ± 2.0 | 6.6 ± 1.4 | 65.0 ± 8.0 | |||||
| Sanchis et al. [15] | HFpEF | 63 | 58.9 ± 23.3 | 8.9 ± 4.9 | 11.3 ± 5.5 | 60.0 ± 5.0 | −16 ± 3.7 | EchoPAC | ||||
| Santos et al. [67] | HFpEF | 135 | 33.4 ± 11.5 | 24.6 ± 0.6 | 13.7 ± 8.6 | 1.2 ± 0.7 | 6.6 ± 2.4 | 59.0 ± 7.0 | −15 ± 3.4 | TomTec | ||
| Donal et al. [68] | HFpEF | 539 | 49.4 ± 17.8 | 12.9 ± 6.1 | 1.8 ± 1.3 | 7.9 ± 2.6 | 62.0 ± 7.0 | −19.0 ± 5.0 | ||||
| Burker et al. [69] | HFpEF | 419 | 34.2 ± 14.3 | 13.3 ± 7.9 | 9.3 ± 3.9 | 61.0 ± 7.0 | ||||||
| Obokata et al. [71] | HFpEF | 40 | 22.7 ± 6.6 | 12.3 ± 5.9 | 19.8 ± 6.8 | 0.8 ± 0.3 | 3.3 ± 1.1 | 60 ± 13.3 | −12.8 ± 3.5 | EchoPAC | ||
| Gupta et al. [73] | HFpEF | 85 | 1.0 ± 0.2 | |||||||||
| Zile et al. [74] | HFpEF | 746 | 10.0 ± 4.5 | 1.1 ± 0.7 | 9.1 ± 3.4 | 64.0 ± 9.0 | ||||||
| Tan et al. [75] | HFpEF | 50 | 30.4 ± 9.2 | 62.0 ± 9.0 | EchoPAC | |||||||
| Jaubert et al. [76] | HFpEF | 59 | 30.7 ± 12.6 | 6.7 ± 2.7 | 10.8 ± 2.3 | |||||||
| Shah et al. [30] | HFrEF(recovered) | 67 | 38.1 ± 12.5 | 22.4 ± 10.3 | 1.8 ± 1.0 | 26.4 ± 5.8 | ||||||
| HFrEF (non-recovered) | 69 | 47.1 ± 11.7 | 21.7 ± 8.8 | 2.0 ± 1.4 | 25.1 ± 7.1 | |||||||
| Tanaka et al. [31] | HFrEF | 205 | 51.0 ± 20.0 | 14.3 ± 7.3 | 31.0 ± 8.0 | −7.6 ± 2.0 | Tomtec | |||||
| Castrichini et al. [32] | HFrEF | 77 | 57.0 ± 26.0 | 10.3 ± 6.9 | 16.7 ± 9.0 | 28.0 ± 6.0 | −3 ± 4.0 | Tomtec | ||||
| Valentim et al. [33] | HFrEF | 42 | 51.5 ± 22.6 | 13.6 ± 4.5 | 29.3 ± 6.4 | −7.0 ± 2.6 | ||||||
| Deferm et al. [35] | HFrEF | 31 | 69.0 ± 26.0 | 6.4 ± 2.2 | 16.8 ± 6.6 | 2.6 ± 0.7 | 20.0 ± 12.0 | −7.3 ± 3.5 | Tomtec | |||
| Park et al. [16] | HFrEF | 2036 | 58.1 ± 28.8 | 11.7 ± 8.1 | 20.5 ± 11.9 | 4.7 ± 1.9 | 27.6 ± 7.3 | Tomtec | ||||
| Kurzawski et al. [34] | HFrEF | 63 | 62.1 ± 13.3 | 8.9 ± 2.0 | 24.2 ± 8.4 | 2.4 ± 1.1 | 19.2 ± 4.1 | EchoPAC | ||||
| Modin et al. [18] | HFrEF | 818 | 30.9 ± 13.8 | 12.2 ± 5.2 | 1.13 ± 0.67 | 6.9 ± 2.5 | 27.8 ± 9.1 | −9.7 ± 3.3 | EchoPAC | |||
| Shintani et al. [37] | HFrEF | 617 | 67 ± 24.4 | |||||||||
| Wu et al. [38] | HFrEF | 34 | 38.4 ± 6.5 | 19.5 ± 7.7 | 1.28 ± 0.16 | 30 ± 9 | ||||||
| Lundberg et al. [41] | HFrEF | 72 | 57.7 ± 18.5 | 7.7 ± 4.2 | 16.8 ± 9.0 | 2.8 ± 1.6 | 7.8 ± 2.9 | 28.3 ± 14.8 | −7.2 ± 3.7 | EchoPAC | ||
| Malagoli et al. [46] | HFrEF | 286 | 46.2 ± 18.2 | 19.4 ± 9.4 | 31.6 ± 6.3 | |||||||
| Carluccio et al. [19] | HFrEF | 405 | 52.6 ± 18.6 | 15.8 ± 7.0 | 14.3 ± 5.2 | 1.4 ± 1.2 | 5.4 ± 1.8 | 30.0 ± 7.4 | −8.3 ± 2.9 | EchoPAC | ||
| Eroglu et al. [47] | HFrEF | 59 | 42.7 ± 22.1 | 17.0 ± 6.0 | 1.7 ± 1.7 | 5.3 ± 1.3 | 33.3 ± 10.4 | −9.7 ± 4.4 | Philips QLAB | |||
| Almeida et al. [48] | HFrEF | 65 | 46.7 ± 13.3 | 17.7 ± 5.2 | 27.7 ± 11.9 | −7.7 ± 2.2 | EchoPAC | |||||
| Xu et al. [51] | HFrEF-event | 28 | 71.0 ± 22.0 | 19.3 ± 10.7 | 2.7 ± 0.8 | 17.0 ± 5.4 | ||||||
| HFrEF-event-free | 17 | 57.0 ± 16.0 | 20.5 ± 11.1 | 2.1 ± 1.2 | 19.0 ± 5.6 | |||||||
| Saha et al. [52] | HFrEF | 49 | 11 ± 6 | 15 ± 10 | 31 ± 8 | –7 ± 3 | EchoPAC | |||||
| Modin et al. [54] | HFrEF | 151 | 42.1 ± 19.0 | 11.9 ± 5.3 | 8.6 ± 2.6 | 26.2 ± 9.4 | −10.1 ± 3.6 | EchoPAC | ||||
| Batalli et al. [55] | HFrEF | 56 | 13.5 ± 6.4 | 1.3 ± 0.9 | 5.3 ± 2.2 | 35 ± 7.5 | ||||||
| Sugimoto et al. [56] | HFrEF | 49 | 55.0 ± 29.0 | 15.1 ± 10.1 | 24.0 ± 13.0 | 1.5 ± 1.1 | 31.0 ± 8.0 | EchoPAC | ||||
| Sargento et al. [58] | HFrEF | 203 | 42.3 ± 18.3 | 1.4 ± 1.0 | 28.2 ± 8.4 | −8.7 ± 3.3 | EchoPAC | |||||
| Melenovsky et al. [17] | HFrEF | 97 | 50.0 ± 17.0 | 6.2 ± 2.1 | 24 ± 9.7 | |||||||
| Sanchis et al. [15] | HFrEF | 32 | 57.8 ± 20.8 | 6.5 ± 5.4 | 11.6 ± 7.6 | 34.0 ± 10.0 | −9.5 ± 4.5 | |||||
| Motoki et al. [70] | HFrEF | 108 | 42.0 ± 15.0 | 14.5 ± 8.2 | 7.7 ± 5.7 | 20.0 ± 12.0 | 1.7 ± 1.4 | 7.2 ± 4.5 | 25.0 ± 6.0 | Syngo | ||
| Carluccio et al. [72] | HFrEF | 747 | 43.9 ± 18.8 | 14.7 ± 8.0 | 1.77 ± 1.56 | 6.7 ± 2.8 | 29.0 ± 7.0 | |||||
| Gupta et al. [73] | HFrEF | 31 | 0.8 ± 0.3 | |||||||||
| Oh et al. [23] | HFrEF | 2006 | 41.9 ± 15.2 | 17.6 ± 9.6 | 1.3 ± 1.1 | 6.0 ± 3.0 | 28.9 ± 8.3 | |||||
| Hinderliter et al. [77] | HFrEF | 211 | 49 ± 23 | 32 ± 11 | ||||||||
| Donal et al. [78] | HFrEF | 75 | 43.4 ± 20.8 | |||||||||
| Jasic-Szpak et al. [79] | HFpEF without AF | 131 | 33.6 ± 9.3 | 29.0 ± 7.4 | 14.5 ± 4.0 | 14.4 ± 6.0 | 11.0 ± 2.8 | 0.87 ± 0.29 | 5.9 ± 1.2 | 72.7 ± 8.5 | −18.6 ± 3.1 | EchoPAC |
| HFpEF with AF | 39 | 39.9 ± 8.1 | 23.1 ± 6.5 | 10.9 ± 3.7 | 12.3 ± 4.9 | 13.6 ± 5.3 | 1.21 ± 0.78 | 5.5 ± 1.3 | 71.6 ± 8.5 | −17.5 ± 3.8 | ||
| CarluccioE [80] | HFpEF | 46 | 43.3 ± 16.9 | 16.7 ± 6.8 | 1.53 ± 0.87 | 5.9 ± 1.5 | 60 ± 6 | −15.4 ± 3.5 | EchoPAC |
HFpEF heart failure with preserved ejection fraction, HFrEF heart failure with reduced ejection fraction, HF heart failure, CMD coronary microvascular dysfunction, CKD chronic kidney dysfunction, GLS global longitudinal strain, LVGLS left ventricle global longitudinal strain, LVEF left ventricle ejection fraction, LA left atrial, LAVi left atrial volume index, LAGLSR left atrial global longitudinal strain at reservoir phase, LAGLSB left atrial global longitudinal strain at booster phase, LAGLSC left atrial global longitudinal strain at conduit phase, e’ mitral annular early diastolic velocity by tissue doppler, MV E/A the ratio between early and late mitral inflow velocity by doppler, E/e’ the ratio between early mitral inflow velocity and mitral annular early diastolic velocity
As compared to patients with HFrEF, patients with HFpEF appeared to be older, women, and had more often hypertension, AF and diabetes irrespective of inpatient or outpatient clinical setting (Table 1). The prevalence of IHD was 39.8% versus 30.7% in the acute inpatient setting and 49.8% versus 33.3% in the chronic outpatient setting when comparing patients with HFrEF versus HFpEF. Patients with HFrEF were more likely to be present with functional MR (27.2%) as compared to patients with HFpEF (12.0%) in the chronic ambulant setting of the study. The pooled mean value of BMI was 25.2 versus 25.6 kg/m2 in the acute inpatient setting and 27.5 versus 29.8 kg/m2 in the chronic outpatient in patients with HFrEF versus HFpEF. As expected by definition, patients with HFpEF had better LV systolic function as compared to patients with HFrEF with higher pooled LVEF and pooled absolute values of LVGLS irrespective of clinical setting of the study either acute inpatient or chronic outpatient (Table 1). Patients with HFpEF appeared to have higher pooled e’ (6.6 versus 7.5 cm/s in the acute inpatient versus chronic outpatient setting) than patients with HFrEF (4.7 versus 6.5 cm/s in the acute inpatient versus chronic outpatient setting). Conversely, the HFrEF group was characterized by higher E/e’ (18.5 versus 16.9 in the acute inpatient versus chronic outpatient setting) as compared to patients with HFpEF (14.0 versus 13.5 the acute inpatient versus chronic outpatient setting) irrespective of clinical setting of the study, indicating higher LV filling pressure in HFrEF.
LA size and pressure estimated by LAVi and E/e’
Twenty-nine studies reported LAVi in patients with HFrEF (n = 8726), and thirty-eight studies reported LAVi in patients with HFpEF (n = 9049). The pooled mean value of LAVi was 59.7 versus 48.3 ml/m2 in the acute inpatient versus chronic outpatient setting for patients with HFrEF, and 52.7 versus 38.2 ml/m2 in the acute inpatient versus chronic outpatient setting for patients with HFpEF. Eight out of 41 included studies reported LAVi in both patients with HFrEF (n = 3002) and HFpEF (n = 1822). In these eight studies, LAVi was comparable between patients with HFrEF and HFpEF [pooled mean LAVi, 42.7 versus 37.6 ml/m2; weighed mean difference [WMD] = −0.2 (−0.48, 0.07); p = 0.15; I2 = 89.8%]. Three out of these eight studies enrolled both patients with HFrEF (n = 2718) and HFpEF (n = 1383) in the acute hospitalized setting, where the remaining studies included patients with both HF phenotypes in the chronic stable setting (HFrEF, n = 284; HFpEF, n = 439). In both acute inpatient [pooled mean LAVi, 54.8 versus 52.6 ml/m2 in HFrEF versus HFpEF; WMD = −0.2 (−0.48, 0.07); p = 0.13; I2 = 89.8%] and outpatient setting [pooled mean LAVi, 42.7 versus 36.9 ml/m2 in HFrEF versus HFpEF; WMD = −0.2 (−0.48, 0.07); p = 0.153; I2 = 89.8%], the LAVi was comparable between patient with HFrEF and HFpEF, although the difference between HFrEF and HFpEF patients appeared to be more narrowed in acute inpatient HF settings. Seven out of 41 included studies reported E/e’ in both patients with HFrEF and HFpEF (HFrEF, n = 2344; HFpEF, n = 1649). In these studies, E/e’ was significantly higher in patients with HFrEF as compared to patients with HFpEF [15.9 versus 13.4 in HFrEF versus HFpEF; WMD = −0.40 (−0.56, −0.24); p < 0.05, I2 = 77.6%]. However, in the acute inpatient setting, E/e’ was comparable between patients with HFrEF and HFpEF [17.7 versus 14.0 in HFrEF versus HFpEF; WMD = −0.40 (−0.56, −0.24); p = 0.15, I2 = 77.6%], whereas E/e’ was significantly higher in patients with HFrEF as compared to patients with HFpEF in chronic HF setting [15.3 versus 13.3 in HFrEF versus HFpEF; WMD = − 0.40 (−0.56, −0.24); p < 0.05, I2 = 77.6%].
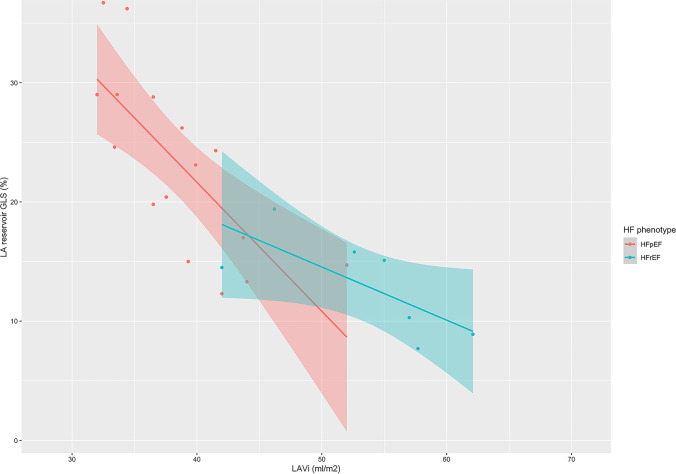
LA function estimated by LA reservoir, booster, and conduit GLS
Ten studies reported LA reservoir GLS (LAGLSR) in patients with HFrEF (n = 3176), and seventeen studies reported LAGLSR in patients with HFpEF (n = 4196). The pooled mean value of LAGLSR was 9.0 versus 12.8% in the acute inpatient versus chronic outpatient setting for patients with HFrEF, and 18.9 versus 23.4% in the acute inpatient versus chronic outpatient setting for HFpEF patients. Four out of 61 studies in the chronic outpatient setting reported LAGLSR in both patients with HFpEF (n = 1877) and HFrEF (n = 3058). LAGLSR was worse in patients with HFrEF as compared to patients with HFpEF [8.5% versus 23.6%; WMD = 16.3% (22.05, 8.61); p < 0.001, I2 = 77.6%]. Besides, the relationship between LAVi and LAGLSR (Fig. 2) was significant in HFpEF (estimated coefficient −1.08, p = 0.009, R2 = 0.525), but not in HFrEF (estimated coefficient −0.44, p = 0.06, R2 = 0.447). On the other hand, the relationship between LAGLS with LVGLS was not significant in neither HFpEF (estimated coefficient 1.35, p = 0.30, R2 = 0.01) nor HFrEF (estimated coefficient 2.81, p = 0.41, R2 = 0.006). Two studies reported LA booster GLS (LAGLSB) in patients with HFrEF (n = 140), and ten studies reported LAGLSB in patients with HFpEF (n = 1320). The pooled mean value of LAGLSB was 7.7% versus 13.9% between patients with HFrEF and HFpEF in the chronic ambulant clinical setting. None of the included studies reported the LAGLSB in both patients with HFpEF and HFrEF. Five studies reported LA conduit GLS (LAGLSC) in patients with HFpEF (n = 1173) in the chronic ambulant clinical setting, and the pooled mean value LAGLSC was 15.8% in patients with HFpEF. No included studies reported LAGLSC in patients with HFrEF. Given the very limited number of studies comparing LA booster and conduit function in patients with HFrEF versus HFpEF, it is hard to determine how these two LA phasic function differ in patients with HFrEF versus HFpEF. Lastly, the details of prognostic information for each LA parameter and the adjusted covariates from included studies were summarized in supplementary online (Tables S5 and S6).
Fig. 2.
Meta-analytic scatterplot for the relationship between LAVi and LA reservoir GLS in patients with HFpEF versus HFrEF. HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; LAVi, left atrial volume index; LA, left atrial; GLS, global longitudinal strain
Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis assessing and comparing LA structural and functional echocardiographic parameters and their clinical relevance in patients with HFrEF versus HFpEF. It comprehensively summarized 61 studies, among which 27 studies with HFrEF patients (n = 8806) and 38 studies with HFpEF patients (n = 9928). Several important clinical findings emerged from the current study:
(1) LA volumes were comparable between patients with HFrEF and HFpEF; (2) LV filling pressures (estimated by E/e’) were comparable between patients with HFrEF and HFpEF in the acute inpatients setting, while in the chronic outpatient setting, LV filling pressures were higher in patients with HFrEF; (3) the LA reservoir GLS was profoundly lower in patients with HFrEF as compared to patients with HFpEF, despite the greater burden of AF in patients with HFpEF and clinical setting of the study (acute inpatient or chronic outpatient).
The left atrium is an easily expandable thin-walled structure that plays a crucial role in LV filling and optimizing cardiac output through interaction with both LV and pulmonary veins through the entire cardiac cycle [1]. It possesses three main functions, including mechanical, endocrine, and regulatory functions, which are closely intertwined and tightly coupled with one another [1]. Rapid development and application of 2D strain to the LA have enabled us to better understand the mechanical function of LA, which is composed of the reservoir, conduit, and booster functions based on the corresponding LA phase in the cardiac cycle [1]. Furthermore, a recent meta-analysis reported the normal values of each strain component, with LA reservoir, conduit, and booster GLS as 39%, 23%, and 17%, respectively [13]. Based on these reference values it can be concluded that pronounced LA dysfunction exists in both patients with HFpEF and HFrEF, further supporting the concept of LA myopathy. Most interestingly, it was recently described that LA reservoir GLS outperformed E/e’ and LAVi in the diagnosis of the HFpEF [14].
Several studies have compared LA structure and function using various imaging methods with mixed results in patients with HFrEF versus HFpEF, which was the starting point of our systematic review. For example, Sanchis et al. showed that LAVi and LA longitudinal strain were similar in new-onset outpatients with HFrEF versus HFpEF [15]. In contrast, LA dysfunction (using LAGLS) was worse in acute heart failure patients with HFrEF than HFpEF, but equally associated with survival [16]. Melenovsky et al. used LA ejection fraction (LAEF) and showed that LA dysfunction was associated with mortality only in patients with HFpEF despite worse LA function in patients with HFrEF [17]. In contrast, Modin et al. showed LAEF was independently associated with mortality in a larger sample of HFrEF patients [18], and Carluccio et al. showed that LA reservoir GLS was independently associated with survival in a cohort of patients with HFrEF [19]. Finally, a recent meta-analysis, pooling data of HFpEF studies, showed that LA reservoir strain was associated with prognosis in patients with HFpEF [5].
A change in LA structure and function is a complex, dynamic and heterogeneous process that may be different between phenotypes of HF. LA dysfunction and increase of LA pressure have long been considered as hallmarks of HFpEF, whereas HFrEF is generally considered as a left ventricular disease [3, 20, 21]. This might explain the discrepancy in the number of studies focusing on LA dysfunction in HFpEF versus HFrEF. However, despite a greater burden of AF in patients with HFpEF, our data found that LA function was worse in patients with HFrEF than patients with HFpEF. This might be related to the greater burden of moderate to severe functional MR in patients with HFrEF. HFrEF is more associated with an eccentric ventricular remodelling, resulting in tethering of the mitral leaflets [22, 23]. In our review, we showed that in HFpEF patients functional MR was less prevalent, but not negligible, and may be more the result of mitral annular dilation due to the high incidence of AF in this subgroup.
LA reservoir peak longitudinal strain, inherent to its nature as a strain, is dependent on its baseline length, with maximal elongation of the LA during LV systole, suggesting its high dependence on LV longitudinal strain as well [24]. Carluccio et al. showed that LA reservoir GLS was more strongly associated with LVGLS beyond LA volume and E/e’ in patients with HFrEF, supporting the significant contribution of LV systolic dysfunction to LA dysfunction in patients with HFrEF [19]. Comparatively, LA mechanical dysfunction in patients with HFpEF, particularly in the setting of AF, is usually not accompanied by substantial changes of LV systolic function, which suggests LA mechanical dysfunction to be disproportionate to LV systolic dysfunction in such patients [8]. Hence, a decrease of LV longitudinal function, as we show in patients with HFrEF, might impact LA reservoir function more in patients with HFrEF than HFpEF [17, 20], suggesting that the concept of LA myopathy is not only subject to HFpEF, but to HFrEF as well.
Despite worse LA global function in HFrEF than HFpEF, the prevalence of AF was higher in patients with HFpEF than HFrEF. AF and HFpEF share many convergent metabolic risk factors, including obesity that promote systematic inflammatory processes. Expansion of epicardial fat tissue may act as a local source of inflammation, amplifying ongoing systemic inflammatory processes [20]. LA dysfunction in HFpEF is likely associated with a series of inflammatory cascades resulting in coupled LA endocrine and regulatory dysfunctions. This is supported by data from Patel et al. who showed that LA reservoir strain was associated with biomarkers of neurohormonal activation [25]. However, the exact mechanism of how the LA mechanical, regulatory, and endocrine functions are coupled together, and particular which factor is the main driving component of LA dysfunction in both settings of HFpEF and HFrEF remains unknown.
Although the prognostic value of LA reservoir strain has been described in several studies that were included in our systematic review both in patients with HFpEF and HFrEF [16, 18, 19], future prognostic studies are warranted to investigate whether LA dysfunction in HFrEF and HFpEF are two distinct processes. A better understanding of different forms of LA dysfunction in HFrEF versus HFpEF may have important clinical implications. Given the distinct LA reservoir GLS in patients with HFrEF versus HFpEF, this measurement might serve as a potential marker to better phenotype patients with HF. For patients with HFpEF, a novel therapeutic intervention which specifically targets the LA by creating a shunt at the atrial level to offload LA pressure looks promising from preliminary data [26]. Given our finding of higher LA pressure and worse LAGLS in HFrEF, we might cautiously postulate a potential benefit of this novel device in patients with HFrEF as well.
Limitations
There are several limitations of the current systematic review. First, our review has the inherent limitation of selection and reporting bias, which was minimized by a thorough selection procedure and quality assessment. Secondly, we only focused on primary echocardiographic parameters assessing LA structures and function that have been widely recommended in guidelines. Other echocardiographic parameters such as LAEF and other LA-related parameters assessed by other imaging modalities were not included in the current review. Thirdly, we were not able to account for all differences in clinical characteristics due to a lack of individual-level data. For example, the definition (and thus the extent) of ischemic cardiomyopathy varies study by study, which hampers a thorough analysis of its (possibly) confounding role. Fourth, we were unable to report the weighted HR of comprehensive LA structural and functional parameters except for LA reservoir GLS due to the limited numbers of studies, different outcome measures, and lack of confounder adjustments. Last but not least, the details of averaging the RR interval for the strain measurement in the setting of AF were not addressed in most of the studies.
Conclusion
Although left atrial abnormalities have been proposed as a hallmark of HFpEF, we found that LA structure and function are worse in patients with HFrEF than HFpEF. Thus, the significant pathophysiological insight of intrinsic LA myopathy should be equally emphasized in both patients with HFrEF and patients with HFpEF.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Triposkiadis F, Pieske B, Butler J, Parissis J, Giamouzis G, Skoularigis J, Brutsaert D, Boudoulas H. Global left atrial failure in heart failure. Eur J Heart Fail. 2016;18:1307–1320. doi: 10.1002/ejhf.645. [DOI] [PubMed] [Google Scholar]
- 2.Bosch L, Lam CSP, Gong L, Chan SP, Sim D, Yeo D, Jaufeerally F, Leong KTG, Ong HY, Ng TP, Richards AM, Arslan F, Ling LH. Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail. 2017;19:1664–1671. doi: 10.1002/ejhf.873. [DOI] [PubMed] [Google Scholar]
- 3.Lam CSP, Voors AA, de Boer RA, Solomon SD, van Veldhuisen DJ. Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J. 2018;39:2780–2792. doi: 10.1093/eurheartj/ehy301. [DOI] [PubMed] [Google Scholar]
- 4.Patel RB, Shah SJ (2020) Therapeutic targeting of left atrial myopathy in atrial fibrillation and heart failure with preserved ejection fraction. JAMA Cardiol 5:497–499. 10.1001/jamacardio.2020.0136 [DOI] [PMC free article] [PubMed]
- 5.Khan MS, Memon MM, Murad MH, Vaduganathan M, Greene SJ, Hall M, Triposkiadis F, Lam CSP, Shah AM, Butler J, Shah SJ (2020) Left atrial function in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail 22:472–485. 10.1002/ejhf.1643 [DOI] [PubMed]
- 6.Simmonds SJ, Cuijpers I, Heymans S, Jones EAV (2020) Cellular and molecular differences between HFpEF and HFrEF: a step ahead in an improved pathological understanding. Cells 9:242. 10.3390/cells9010242 [DOI] [PMC free article] [PubMed]
- 7.Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14:591–602. 10.1038/nrcardio.2017.65 [DOI] [PubMed]
- 8.Packer M, Lam CSP, Lund LH, Redfield MM (2020) Interdependence of atrial fibrillation and heart failure with a preserved ejection fraction reflects a common underlying atrial and ventricular myopathy. Circulation 141:4–6. 10.1161/CIRCULATIONAHA.119.042996 [DOI] [PubMed]
- 9.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed]
- 10.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 11.Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernan MA, Hopewell S, Hrobjartsson A, Junqueira DR, Juni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed]
- 12.Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed]
- 13.Pathan F, D'Elia N, Nolan MT, Marwick TH, Negishi K (2017) Normal ranges of left atrial strain by speckle-tracking echocardiography: a systematic review and meta-analysis. J Am Soc Echocardiogr 30:59–70.e8. 10.1016/j.echo.2016.09.007 [DOI] [PubMed]
- 14.Reddy YNV, Obokata M, Egbe A, Yang JH, Pislaru S, Lin G, Carter R, Borlaug BA (2019) Left atrial strain and compliance in the diagnostic evaluation of heart failure with preserved ejection fraction. Eur J Heart Fail 21:891–900. 10.1002/ejhf.1464 [DOI] [PubMed]
- 15.Sanchis L, Gabrielli L, Andrea R, Falces C, Duchateau N, Perez-Villa F, Bijnens B, Sitges M (2015) Left atrial dysfunction relates to symptom onset in patients with heart failure and preserved left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging 16:62–67. 10.1093/ehjci/jeu165 [DOI] [PubMed]
- 16.Park JH, Hwang IC, Park JJ, Park JB, Cho GY. Prognostic power of left atrial strain in patients with acute heart failure. Eur Heart J Cardiovasc Imaging. 2020;2:210–219. doi: 10.1093/ehjci/jeaa013. [DOI] [PubMed] [Google Scholar]
- 17.Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail. 2015;8:295–303. doi: 10.1161/CIRCHEARTFAILURE.114.001667. [DOI] [PubMed] [Google Scholar]
- 18.Modin D, Sengelov M, Jorgensen PG, Olsen FJ, Bruun NE, Fritz-Hansen T, Andersen DM, Jensen JS, Biering-Sorensen T. Prognostic value of left atrial functional measures in heart failure with reduced ejection fraction. J Card Fail. 2019;25:87–96. doi: 10.1161/CIRCIMAGING.115.003754. [DOI] [PubMed] [Google Scholar]
- 19.Carluccio E, Biagioli P, Mengoni A, Francesca Cerasa M, Lauciello R, Zuchi C, Bardelli G, Alunni G, Coiro S, Gronda EG, Ambrosio G (2018) Left atrial reservoir function and outcome in heart failure with reduced ejection fraction. Circ Cardiovasc Imaging 11:11. 10.1161/CIRCIMAGING.118.007696 [DOI] [PubMed]
- 20.Packer M (2019) Drugs That ameliorate epicardial adipose tissue inflammation may have discordant effects in heart failure with a preserved ejection fraction as compared with a reduced ejection fraction. J Card Fail 25:986–1003. 10.1016/j.cardfail.2019.09.002 [DOI] [PubMed]
- 21.Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14:30–38. doi: 10.1038/nrcardio.2016.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deferm S, Bertrand PB, Verbrugge FH, Verhaert D, Rega F, Thomas JD, Vandervoort PM (2019) Atrial functional mitral regurgitation. JACC Review Topic of the Week. J Am Coll Cardiol 73:2465–2476. 10.1016/j.jacc.2019.02.061 [DOI] [PubMed]
- 23.Oh JK, Pellikka PA, Panza JA, Biernat J, Attisano T, Manahan BG, Wiste HJ, Lin G, Lee K, Miller FA, Jr, Stevens S, Sopko G, She L, Velazquez EJ, Investigators ST. Core lab analysis of baseline echocardiographic studies in the STICH trial and recommendation for use of echocardiography in future clinical trials. J Am Soc Echocardiogr. 2012;25:327–336. doi: 10.1016/j.echo.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ersboll M, Moller JE (2018) Left atrial function in heart failure with reduced ejection fraction. Circ Cardiovasc Imaging 11:e008427. 10.1161/CIRCIMAGING.118.008427 [DOI] [PubMed]
- 25.Patel RB, Alenezi F, Sun JL, Alhanti B, Vaduganathan M, Oh JK, Redfield MM, Butler J, Hernandez AF, Velazquez EJ, Shah SJ (2020) Biomarker profile of left atrial myopathy in heart failure with preserved ejection fraction: insights from the RELAX Trial. J Card Fail 26:270–275. 10.1016/j.cardfail.2019.12.001 [DOI] [PMC free article] [PubMed]
- 26.Kaye DM, Petrie MC, McKenzie S, Hasenfubeta G, Malek F, Post M, Doughty RN, Trochu JN, Gustafsson F, Lang I, Kolodziej A, Westenfeld R, Penicka M, Rosenberg M, Hausleiter J, Raake P, Jondeau G, Bergmann MW, Spelman T, Aytug H, Ponikowski P, Hayward C, investigators RL-Hs (2019) Impact of an interatrial shunt device on survival and heart failure hospitalization in patients with preserved ejection fraction. ESC Heart Fail 6:62–69. 10.1002/ehf2.12350 [DOI] [PMC free article] [PubMed]
- 27.Hoshida S, Watanabe T, Shinoda Y, Minamisaka T, Fukuoka H, Inui H, Ueno K, Yamada T, Uematsu M, Yasumura Y, Nakatani D, Suna S, Hikoso S, Higuchi Y, Sakata Y, Osaka CardioVascular Conference I (2020) Considerable scatter in the relationship between left atrial volume and pressure in heart failure with preserved left ventricular ejection fraction. Sci Rep 10:90. 10.1038/s41598-019-56581-x [DOI] [PMC free article] [PubMed]
- 28.Harada T, Sunaga H, Sorimachi H, Yoshida K, Kato T, Kurosawa K, Nagasaka T, Koitabashi N, Iso T, Kurabayashi M, Obokata M. Pathophysiological role of fatty acid-binding protein 4 in Asian patients with heart failure and preserved ejection fraction. ESC Heart Fail. 2020;7:4256–4266. doi: 10.1002/ehf2.13071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hwang IC, Cho GY, Choi HM, Yoon YE, Park JJ, Park JB, Park JH, Lee SP, Kim HK, Kim YJ. H2FPEF score reflects the left atrial strain and predicts prognosis in patients with heart failure with preserved ejection fraction. J Card Fail. 2021;27:198–207. doi: 10.1016/j.cardfail.2020.09.474. [DOI] [PubMed] [Google Scholar]
- 30.Shah MA, Soofi MA, Jafary Z, Alhomrani A, Alsmadi F, Wani TA, Bajwa IA (2020) Echocardiographic parameters associated with recovery in heart failure with reduced ejection fraction. Echocardiography 37:1574–1582.10.1111/echo.14859 [DOI] [PubMed]
- 31.Tanaka H, Tatsumi K, Matsuzoe H, Matsumoto K, Hirata KI (2020) Impact of diabetes mellitus on left ventricular longitudinal function of patients with non-ischemic dilated cardiomyopathy. Cardiovasc Diabetol 19:84.10.1186/s12933-020-01063-y [DOI] [PMC free article] [PubMed]
- 32.Castrichini M, Manca P, Nuzzi V, Barbati G, De Luca A, Korcova R, Stolfo D, Lenarda AD, Merlo M, Sinagra G. Sacubitril/valsartan induces global cardiac reverse remodeling in long-lasting heart failure with reduced ejection fraction: standard and advanced echocardiographic evidences. J Clin Med. 2020;9:906. doi: 10.3390/jcm9040906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Valentim Goncalves A, Galrinho A, Pereira-da-Silva T, Branco L, Rio P, Timoteo AT, Abreu J, Soares RM, Feliciano J, Moreira RI, Ferreira RC. Myocardial work improvement after sacubitril-valsartan therapy: a new echocardiographic parameter for a new treatment. J Cardiovasc Med (Hagerstown) 2020;21:223–230. doi: 10.2459/JCM.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 34.Kurzawski J, Janion-Sadowska A, Zandecki L, Piatek L, Koziel D, Sadowski M (2020) Global peak left atrial longitudinal strain assessed by transthoracic echocardiography is a good predictor of left atrial appendage thrombus in patients in sinus rhythm with heart failure and very low ejection fraction - an observational study. Cardiovasc Ultrasound 18:7. 10.1186/s12947-020-00188-0 [DOI] [PMC free article] [PubMed]
- 35.Deferm S, Martens P, Verbrugge FH, Bertrand PB, Dauw J, Verhaert D, Dupont M, Vandervoort PM, Mullens W (2020) LA mechanics in decompensated heart failure: insights from strain echocardiography with invasive hemodynamics. JACC Cardiovasc Imaging S1936–878X:31178–7. 10.1016/j.jcmg.2019.12.008 [DOI] [PubMed]
- 36.Shah AM, Cikes M, Prasad N, Li G, Getchevski S, Claggett B, Rizkala A, Lukashevich I, O'Meara E, Ryan JJ, Shah SJ, Mullens W, Zile MR, Lam CSP, McMurray JJV, Solomon SD, Investigators P-H (2019) Echocardiographic features of patients with heart failure and preserved left ventricular ejection fraction. J Am Coll Cardiol 74:2858–2873. 10.1016/j.jacc.2019.09.063 [DOI] [PubMed]
- 37.Shintani Y, Takahama H, Hamatani Y, Nishimura K, Kanzaki H, Kusano K, Noguchi T, Toyoda K, Yasuda S, Izumi C (2019) Ischemic stroke risk during post-discharge phases of heart failure: association of left ventricular concentric geometry. Heart Vessels 35:564–575. 10.1007/s00380-019-01522-x [DOI] [PubMed]
- 38.Wu CK, Lee JK, Hsu JC, Su MM, Wu YF, Lin TT, Lan CW, Hwang JJ, Lin LY (2020) Myocardial adipose deposition and the development of heart failure with preserved ejection fraction. Eur J Heart Fail 22:445–454. 10.1002/ejhf.1617 [DOI] [PubMed]
- 39.Telles F, Nanayakkara S, Evans S, Patel HC, Mariani JA, Vizi D, William J, Marwick TH, Kaye DM (2019) Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur J Heart Fail 21:495–505. 10.1002/ejhf.1399 [DOI] [PubMed]
- 40.Sobirin MA, Herry Y, Sofia SN, Uddin I, Rifqi S, Tsutsui H. Effects of coenzyme Q10 supplementation on diastolic function in patients with heart failure with preserved ejection fraction. Drug Discov Ther. 2019;13:38–46. doi: 10.5582/ddt.2019.01004. [DOI] [PubMed] [Google Scholar]
- 41.Lundberg A, Johnson J, Hage C, Bäck M, Merkely B, Venkateshvaran A, Lund LH, Nagy AI, Manouras A (2018) Left atrial strain improves estimation of filling pressures in heart failure: a simultaneous echocardiographic and invasive haemodynamic study. Clinical Res Cardiol 108:703–715. 10.1007/s00392-018-1399-8 [DOI] [PMC free article] [PubMed]
- 42.Al Saikhan L, Hughes AD, Chung WS, Alsharqi M, Nihoyannopoulos P. Left atrial function in heart failure with mid-range ejection fraction differs from that of heart failure with preserved ejection fraction: a 2D speckle-tracking echocardiographic study. Eur Heart J Cardiovasc Imaging. 2019;20:279–290. doi: 10.1093/ehjci/jey171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burns JA, Sanchez C, Beussink L, Daruwalla V, Freed BH, Selvaraj S, Shah SJ. Lack of association between anemia and intrinsic left ventricular diastolic function or cardiac mechanics in heart failure with preserved ejection fraction. Am J Cardiol. 2018;122:1359–1365. doi: 10.1016/j.amjcard.2018.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Obokata M, Reddy YNV, Melenovsky V, Pislaru S, Borlaug BA. Deterioration in right ventricular structure and function over time in patients with heart failure and preserved ejection fraction. Eur Heart J. 2019;40:689–697. doi: 10.1093/eurheartj/ehy809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagy AI, Hage C, Merkely B, Donal E, Daubert JC, Linde C, Lund LH, Manouras A. Left atrial rather than left ventricular impaired mechanics are associated with the pro-fibrotic ST2 marker and outcomes in heart failure with preserved ejection fraction. J Intern Med. 2018;283:380–391. doi: 10.1111/joim.12723. [DOI] [PubMed] [Google Scholar]
- 46.Malagoli A, Rossi L, Bursi F, Zanni A, Sticozzi C, Piepoli MF, Villani GQ (2019) Left atrial function predicts cardiovascular events in patients with chronic heart failure with reduced ejection fraction. J Am Soc Echocardiogr 32:248–256. 10.1016/j.echo.2018.08.012 [DOI] [PubMed]
- 47.Eroglu E, Kilicgedik A, Kahveci G, Bakal RB, Kirma C (2018) Red cell distribution width and its relationship with global longitudinal strain in patients with heart failure with reduced ejection fraction: a study using two-dimensional speckle tracking echocardiography. Kardiol Pol 76:580–585. 10.5603/KP.a2017.0256 [DOI] [PubMed]
- 48.Almeida P, Rodrigues J, Lourenco P, Maciel MJ, Bettencourt P. Left atrial volume index is critical for the diagnosis of heart failure with preserved ejection fraction. J Cardiovasc Med (Hagerstown) 2018;19:304–309. doi: 10.2459/JCM.0000000000000651. [DOI] [PubMed] [Google Scholar]
- 49.Liu S, Guan Z, Zheng X, Meng P, Wang Y, Li Y, Zhang Y, Yang J, Jia D, Ma C. Impaired left atrial systolic function and inter-atrial dyssynchrony may contribute to symptoms of heart failure with preserved left ventricular ejection fraction: A comprehensive assessment by echocardiography. Int J Cardiol. 2018;257:177–181. doi: 10.1016/j.ijcard.2017.12.042. [DOI] [PubMed] [Google Scholar]
- 50.Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, Beussink-Nelson L, Ljung Faxen U, Fermer ML, Broberg MA, Gan LM, Lund LH (2018) Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J 39:3439–3450. 10.1093/eurheartj/ehy531 [DOI] [PMC free article] [PubMed]
- 51.Xu B, Kawata T, Daimon M, Kimura K, Nakao T, Lee SC, Hirokawa M, Yoshinaga A, Watanabe M, Yatomi Y, Komuro I (2018) Prognostic value of a simple echocardiographic parameter, the right ventricular systolic to diastolic duration ratio, in patients with advanced heart failure with non-ischemic dilated cardiomyopathy. Int Heart J 59:968–975. 10.1536/ihj.17-475 [DOI] [PubMed]
- 52.Saha SK, Luo XX, Gopal AS, Govind SC, Fang F, Liu M, Zhang Q, Ma C, Dong M, Kiotsekoglou A, Yu CM. Incremental prognostic value of multichamber deformation imaging and renal function status to predict adverse outcome in heart failure with reduced ejection fraction. Echocardiography. 2018;35:450–458. doi: 10.1111/echo.13821. [DOI] [PubMed] [Google Scholar]
- 53.Abohammar S, ElSaidy MA, Fathalla D, Aldosarri M. Baseline characteristics of patients with heart failure and preserved ejection fraction at admission with acute heart failure in Saudi Arabia. Egypt Heart J. 2017;69:21–28. doi: 10.1016/j.ehj.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Modin D, Sengelov M, Jorgensen PG, Bruun NE, Olsen FJ, Dons M, Fritz Hansen T, Jensen JS, Biering-Sorensen T. Global longitudinal strain corrected by RR interval is a superior predictor of all-cause mortality in patients with systolic heart failure and atrial fibrillation. ESC Heart Fail. 2018;5:311–318. doi: 10.1002/ehf2.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Batalli A, Ibrahimi P, Bytyçi I, Ahmeti A, Haliti E, Elezi S, Henein MY, Bajraktari G (2017) Different determinants of exercise capacity in HFpEF compared to HFrEF. Cardiovascular Ultrasound 15:12. 10.1186/s12947-017-0103-x [DOI] [PMC free article] [PubMed]
- 56.Sugimoto T, Bandera F, Generati G, Alfonzetti E, Bussadori C, Guazzi M. Left atrial function dynamics during exercise in heart failure: pathophysiological implications on the right heart and exercise ventilation inefficiency. JACC Cardiovasc Imaging. 2017;10:1253–1264. doi: 10.1016/j.jcmg.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 57.Hage C, Michaelsson E, Linde C, Donal E, Daubert JC, Gan LM, Lund LH (2017) Inflammatory biomarkers predict heart failure severity and prognosis in patients with heart failure with preserved ejection fraction: a holistic proteomic approach. Circ Cardiovasc Genet 10(1). 10.1161/CIRCGENETICS.116.001633 [DOI] [PubMed]
- 58.Sargento L, Vicente Simoes A, Longo S, Lousada N, Palma Dos Reis R (2017) Left atrial function index predicts long-term survival in stable outpatients with systolic heart failure. Eur Heart J Cardiovasc Imaging 18:119–127. 10.1093/ehjci/jew196 [DOI] [PubMed]
- 59.Aung SM, Guler A, Guler Y, Huraibat A, Karabay CY, Akdemir I. Left atrial strain in heart failure with preserved ejection fraction. Herz. 2017;42:194–199. doi: 10.1007/s00059-016-4456-y. [DOI] [PubMed] [Google Scholar]
- 60.Hung CL, Yun CH, Lai YH, Sung KT, Bezerra HG, Kuo JY, Hou CJ, Chao TF, Bulwer BE, Yeh HI, Shih SC, Lin SJ, Cury RC (2016) An observational study of the association among interatrial adiposity by computed tomography measure, insulin resistance, and left atrial electromechanical disturbances in heart failure. Medicine (Baltimore) 95:e3912. 10.1097/MD.0000000000003912 [DOI] [PMC free article] [PubMed]
- 61.Freed BH, Daruwalla V, Cheng JY, Aguilar FG, Beussink L, Choi A, Klein DA, Dixon D, Baldridge A, Rasmussen-Torvik LJ, Maganti K, Shah SJ (2016) Prognostic utility and clinical significance of cardiac mechanics in heart failure with preserved ejection fraction: importance of left atrial strain. Circ Cardiovasc Imaging 9:e003754. 10.1161/CIRCIMAGING.115.003754 [DOI] [PMC free article] [PubMed]
- 62.Unger ED, Dubin RF, Deo R, Daruwalla V, Friedman JL, Medina C, Beussink L, Freed BH, Shah SJ (2016) Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail 18:103–112. 10.1002/ejhf.445 [DOI] [PMC free article] [PubMed]
- 63.Georgievska-Ismail L, Zafirovska P, Hristovski Z (2016) Evaluation of the role of left atrial strain using two-dimensional speckle tracking echocardiography in patients with diabetes mellitus and heart failure with preserved left ventricular ejection fraction. Diab Vasc Dis Res 13:384–394. 10.1177/1479164116655558 [DOI] [PubMed]
- 64.Garcia EL, Menezes MG, Stefani Cde M, Danzmann LC, Torres MA. Ergospirometry and echocardiography in early stage of heart failure with preserved ejection fraction and in healthy individuals. Arq Bras Cardiol. 2015;105:248–255. doi: 10.5935/abc.20150085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hasselberg NE, Haugaa KH, Sarvari SI, Gullestad L, Andreassen AK, Smiseth OA, Edvardsen T (2015) Left ventricular global longitudinal strain is associated with exercise capacity in failing hearts with preserved and reduced ejection fraction. Eur Heart J Cardiovasc Imaging 16:217–224. 10.1093/ehjci/jeu277 [DOI] [PMC free article] [PubMed]
- 66.Shah AM, Shah SJ, Anand IS, Sweitzer NK, O'Meara E, Heitner JF, Sopko G, Li G, Assmann SF, McKinlay SM, Pitt B, Pfeffer MA, Solomon SD, Investigators T. Cardiac structure and function in heart failure with preserved ejection fraction: baseline findings from the echocardiographic study of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist trial. Circ Heart Fail. 2014;7:104–115. doi: 10.1161/CIRCHEARTFAILURE.113.000887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Santos AB, Kraigher-Krainer E, Gupta DK, Claggett B, Zile MR, Pieske B, Voors AA, Lefkowitz M, Bransford T, Shi V, Packer M, McMurray JJ, Shah AM, Solomon SD, Investigators P. Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014;16:1096–1103. doi: 10.1002/ejhf.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Donal E, Lund LH, Oger E, Hage C, Persson H, Reynaud A, Ennezat PV, Bauer F, Sportouch-Dukhan C, Drouet E, Daubert JC, Linde C, KaRen I. Baseline characteristics of patients with heart failure and preserved ejection fraction included in the Karolinska Rennes (KaRen) study. Arch Cardiovasc Dis. 2014;107:112–121. doi: 10.1016/j.acvd.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 69.Burke MA, Katz DH, Beussink L, Selvaraj S, Gupta DK, Fox J, Chakrabarti S, Sauer AJ, Rich JD, Freed BH, Shah SJ. Prognostic importance of pathophysiologic markers in patients with heart failure and preserved ejection fraction. Circ Heart Fail. 2014;7:288–299. doi: 10.1161/CIRCHEARTFAILURE.113.000854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Motoki H, Borowski AG, Shrestha K, Troughton RW, Martin MG, Tang WH, Klein AL (2013) Impact of left ventricular diastolic function on left atrial mechanics in systolic heart failure. Am J Cardiol 112:821–826. 10.1016/j.amjcard.2013.05.007 [DOI] [PubMed]
- 71.Obokata M, Negishi K, Kurosawa K, Arima H, Tateno R, Ui G, Tange S, Arai M, Kurabayashi M. Incremental diagnostic value of la strain with leg lifts in heart failure with preserved ejection fraction. JACC Cardiovasc Imaging. 2013;6:749–758. doi: 10.1016/j.jcmg.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 72.Carluccio E, Dini FL, Biagioli P, Lauciello R, Simioniuc A, Zuchi C, Alunni G, Reboldi G, Marzilli M, Ambrosio G. The 'Echo Heart Failure Score': an echocardiographic risk prediction score of mortality in systolic heart failure. Eur J Heart Fail. 2013;15:868–876. doi: 10.1093/eurjhf/hft038. [DOI] [PubMed] [Google Scholar]
- 73.Gupta DK, Shah AM, Castagno D, Takeuchi M, Loehr LR, Fox ER, Butler KR, Mosley TH, Kitzman DW, Solomon SD. Heart failure with preserved ejection fraction in African Americans: The ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail. 2013;1:156–163. doi: 10.1016/j.jchf.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE, Investigators IP. Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation. 2011;124:2491–2501. doi: 10.1161/CIRCULATIONAHA.110.011031. [DOI] [PubMed] [Google Scholar]
- 75.Tan YT, Wenzelburger F, Lee E, Nightingale P, Heatlie G, Leyva F, Sanderson JE. Reduced left atrial function on exercise in patients with heart failure and normal ejection fraction. Heart. 2010;96:1017–1023. doi: 10.1136/hrt.2009.189118. [DOI] [PubMed] [Google Scholar]
- 76.Jaubert MP, Armero S, Bonello L, Nicoud A, Sbragia P, Paganelli F, Arques S. Predictors of B-type natriuretic peptide and left atrial volume index in patients with preserved left ventricular systolic function: an echocardiographic-catheterization study. Arch Cardiovasc Dis. 2010;103:3–9. doi: 10.1016/j.acvd.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 77.Hinderliter AL, Blumenthal JA, O'Conner C, Adams KF, Dupree CS, Waugh RA, Bensimhon D, Christenson RH, Sherwood A. Independent prognostic value of echocardiography and N-terminal pro-B-type natriuretic peptide in patients with heart failure. Am Heart J. 2008;156:1191–1195. doi: 10.1016/j.ahj.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Donal E, Raud-Raynier P, De Place C, Gervais R, Rosier A, Roulaud M, Ingels A, Carre F, Daubert JC, Denjean A. Resting echocardiographic assessments of left atrial function and filling pressure interest in the understanding of exercise capacity in patients with chronic congestive heart failure. J Am Soc Echocardiogr. 2008;21:703–710. doi: 10.1016/j.echo.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 79.Jasic-Szpak E, Marwick TH, Donal E, Przewlocka-Kosmala M, Huynh Q, Gozdzik A, Woznicka AK, Jankowska EA, Ponikowski P, Kosmala W. Prediction of AF in heart failure with preserved ejection fraction: incremental value of left atrial strain. JACC Cardiovasc Imaging. 2021;14(1):131–144. doi: 10.1016/j.jcmg.2020.07.040. [DOI] [PubMed] [Google Scholar]
- 80.Carluccio Erberto EE. Fibrosis assessment by integrated backscatter and its relationship with longitudinal deformation and diastolic function in heart failure with preserved ejection fraction. Int J Cardiovasc Imaging. 2016;32(7):1071–1080. doi: 10.1007/s10554-016-0881-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.