Abstract
Introduction
Less-than-optimum positioning of femoral and tibial components and improper soft tissue tension, with abnormal loads and reduced range of motion, may cause lower patient satisfaction rates. To reduce surgeon-related variables during TKA, technology-assisted TKA was introduced, including computer navigation and robotic-assisted surgery (RATKA). Although several studies show promising short- and long-term functional and radiological outcomes of RATKA, there are still concerns related to its absolute superiority over conventional TKA.
Methods
This review aims to provide an updated insight into the most recent articles reporting on outcomes (functional, radiological, and complications) of RATKA through a systematic search of major databases. A comprehensive English literature search was performed by both authors through four databases (Embase, PubMed, Web of Science, and Scopus). The full text of the final eligible studies was evaluated for inclusion, resulting in 13 studies that are included in this review.
Results
There were 2112 knees in the 13 studies, with a follow-up ranging from three months to 13 years; only three were randomized controlled trials (RCTs), and nine directly compared the results of RATKA with CTKA technique. Seven studies reported the operative time ranging from 76.8 to 156 min; six reported a longer operative time with RATKA. Length of hospital stay (LOS) was reported in six studies which ranged from 0.48 to 2.1 days; in four studies the LOS was shorter with RATKA. In seven of the nine studies comparing RATKA with CTKA, no difference in functional outcomes was found. Four out of six studies reported that the overall alignment had mechanical alignment within ±3° of neutral alignment in all RATKA patients with an HKA ranging from −0.3 to 1.8°. Only one study reported better radiological outcomes in the RATKA group. In six comparative studies, no difference was found in the incidence of complications between RATKA and CTKA.
Conclusion
Although robotic-assisted total knee arthroplasty is a promising technology that provides better component alignment and superior early functional outcomes, the justification for its widespread adoption needs more robust evidence through well-designed and better long-term studies demonstrating superior, predictable, and durable clinical results compared to conventional total knee arthroplasty techniques.
Keywords: Total knee arthroplasty, Total knee replacement, Robotic-assisted, Robot, Outcomes
1. Introduction
Despite the considerable annual increase in the number of total knee arthroplasty (TKA) procedures being performed worldwide and improvements in implant designs and perioperative care, patient satisfaction rates remain lower than expected; this is attributed partly to less-than-optimum positioning of femoral and tibial components and improper soft tissue tension, with abnormal loads and reduced range of motion (ROM).1, 2, 3, 4
Aiming to reduce surgeon-related variables during TKA, technology-assisted TKA was introduced, including computer navigation and robotic-assisted surgery. It was hoped that these technologies would help more accurate implant positioning, alignment, ligament balancing, and preservation of the soft-tissue envelope, thereby leading to improved outcomes and better longevity.5, 6, 7
Robotic-assisted TKA (RATKA) entails detailed planning intra-operatively or through preoperative three-dimensional CT scans, which are then analyzed by specialized software to convert them into virtual intraoperative navigation; this eventually restricts bony cuts to the preoperative plan and prevents excessive, unnecessary cuts through the haptic feedback, which eventually improves components alignment.8,9
Although several studies show promising short- and long-term functional and radiological outcomes of RATKA, there are still concerns related to its absolute superiority compared to conventional TKA (CTKA) to justify the additional costs and radiation exposure.10,11 This review aims to provide an updated insight into the most recent articles reporting on outcomes (functional, radiological, and complications) of RATKA through a systematic search of major databases.
2. Methods
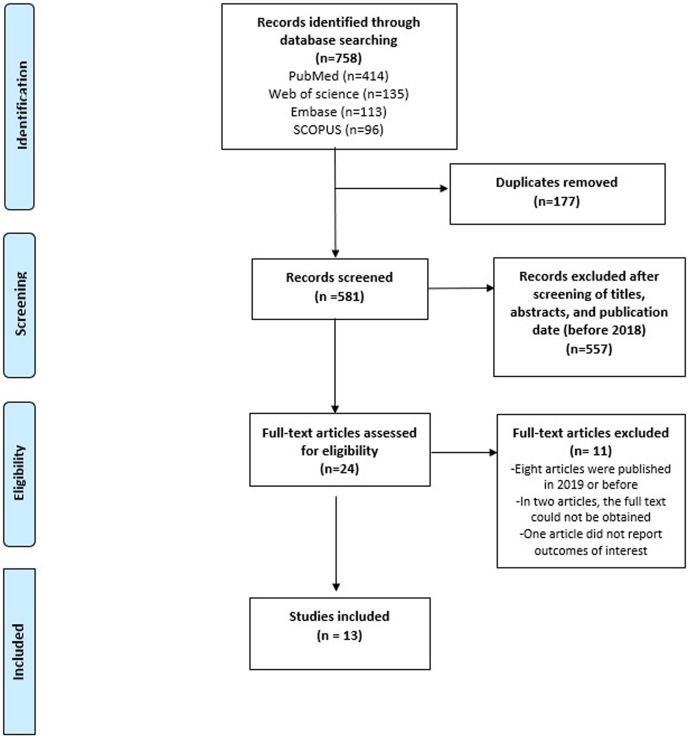
A systematic search on RATKA in adult patients following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.12 The inclusion criteria were English language original studies reporting on the use of RATKA where the following data were presented: patient-reported outcomes (PROMs), functional outcomes, radiological outcomes, and incidence of complications. Studies investigating other procedures such as unicompartmental knee arthroplasty (UKA), cadaveric studies, outcomes of interest, cost analysis studies, other types of publications (reviews, editorials, case reports), and studies not published in the English language were excluded. A comprehensive English literature search was performed by both authors through four databases (Embase, PubMed, Web of Science, and Scopus) till February 28, 2022, using various combinations of the terms “total knee arthroplasty,” “total knee replacement,” “robotic,” and “robotic-assisted.” After downloading the results to Endnote 20, duplicates were excluded, followed by screening the title and abstracts for eligibility. The full text of the final eligible studies was evaluated for inclusion, resulting in 13 studies13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 which are included in the formulation of this review (Fig. 1). To keep the current review as updated as possible, the included studies are considered the most recent ones (published in 2020 and after) discussing RATKA and including one study published in 2019 which was not included in previous recent reviews.10,11
Fig. 1.
Flow diagram showing the study search and selection method.
3. Results
3.1. Demographics and operative characteristics
For this review, we included 13 of the most recent studies (Table 1) reporting results of adopting RATKA, with a total of 2112 knees (range 26–724 TKA per study). Most of the patients were females (61%). Follow-up ranged from three months to 13 years; all studies reported a short-term follow-up except two studies, which reported their results at a long-term mean follow-up of eight and 13 years, respectively.24,25
Table 1.
Basic characteristics of the included studies.
| No. | Author/year | Country | Study | Level of evidence | Sample size (RATKAs) | Sex |
Age (years) | Follow up | BMI (kg/m2) | LOS (days) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||||
| 1 | Richards et al., 2022 (CR) | USA | Retrospective Cohort (Single surgeon) | LOE Ⅲ | 107 | 18 (16.8%) | 89 (83.2%) | 65 ± 10.3 | 16.4 ± 5.6 Months | 30.5 ± 5.5 | 1.7 ± 1.2 |
| Richards et al., 2022 (PS) | USA | Retrospective Cohort (Single surgeon) | LOE Ⅲ | 107 | 56 (52.3%) | 51 (47.7%) | 66.7 ± 9.6 | 19.2 ± 6.3 Months | 32.9 ± 6.2 | 1.5 ± 0.8 | |
| 2 | Z. Li et al., 2022 | China | RCT (multicenter) | LOE Ⅰ | 73 | 13 (17.8%) | 60 (82.2%) | 68 ± 8 (30–86) | 3 Months | 26.9 ± 3.26 (20–38.5) | NR |
| 3 | C. Li et al., 2022 | China | prospective cohort (Single surgeon) | LOE Ⅱ | 26 | 9 (34.6%) | 17 (65.4%) | 66.4 (50–76) | 3 Months | NR | NR |
| 4 | Smith et al., 2021 | USA | retrospective cohort (Single surgeon) | LOE Ⅲ | 120 | 48 (40%) | 72 (60%) | 68 (40–86) | 17 (Min:12) Months | 31.2 (18–47) | 2.1 |
| 5 | Shaw et al., 2021 | USA | prospective cohort | LOE Ⅱ | 260 | 84 (32.33%) | 176 (67.7%) | 67.2 (41–91) | NR | 32.4 (16.2–48.3) | 1.04 (0–5) |
| 6 | Samuel et al., 2021 | USA | retrospective cohort | LOE Ⅲ | 85 | 38 (44.7%) | 47 (55.3%) | 63.3 ± 8.8 | Min 12 Months | 31.7 ± 5.9 | 0.48 ± 0.59 |
| 7 | Nickel et al., 2021 | USA | prospective case series | LOE Ⅳ | 105 | NR | 62.4 ± 8.5 | NR | 30.6 ± 6.1 | NR | |
| 8 | Mitchell et al., 2021 | USA | retrospective cohort (Single surgeon) | LOE Ⅲ | 148 | 72 (48.6%) | 76 (51.4%) | 65.9 ± 8.2 | Min 12 Months | 30.6 ± 5.3 | 1.18 |
| 9 | Marchand et al., 2021 | USA | retrospective cohort (Single surgeon) | LOE Ⅲ | 80 | 51 (64%) | 29 (36%) | 67 ± 8 (46–84) | Min 24 Months | 31 ± 7 | NR |
| 10 | Held et al., 2021 | USA | retrospective cohort (Single surgeon) | LOE Ⅲ | 111 | 37 (33%) | 74 (67%) | 70 | Min 24 Months | 30.1 | 2 |
| 11 | Blum et al., 2021 | USA | prospective case series (Single surgeon) | LOE Ⅳ | 106 | NR | 69.6 ± 8.3 | Min 24 Months | 29.8 ± 4.1 | NR | |
| 12 | Kim et al., 2020 | South Korea | RCT (Single surgeon) | LOE Ⅰ | 724 | 132 (18.2%) | 542 (81.8%) | 60 ± 7 (49–65) | 13 (10–15) years | 28 ± 9 (26–36) | NR |
| 13 | Yeo et al., 2019 (KA) | South Korea | RCT (Single surgeon) | LOE Ⅰ | 30 | 5 (16.7%) | 25 (83.3%) | 72 ± 5.5 | Min 8 years | 26.1 ± 5 | NR |
| Yeo et al., 2019 (MA) | South Korea | RCT (Single surgeon) | LOE Ⅰ | 30 | 3 (10%) | 27 (90%) | 74 ± 5.2 | Min 8 years | 26.9 ± 2.1 | NR | |
Data presented as mean ± SD (range) whenever possible. RATKA: robotic assisted total knee arthroplasty, BMI: body mass index, LOS: length of hospital stay, CR: cruciate retaining, PS: posterior stabilized, RCT: randomized controlled trial, NR: not reported, Min: minimum, KA: kinematic alignment, MA: mechanical alignment.
Nine (69%) studies were published from the USA, two (15.5%) from China, and two (15.5%) from South Korea. Only three were randomized controlled trials (RCTs)14,24,25; the remaining were cohort and case series studies. Nine studies compared the results of RATKA with CTKA technique,14, 15, 16, 17, 18,20, 21, 22,24 one study compared RATKA in a group using cruciate retaining (CR) implants with another group using posterior stabilized (PS) implants,13 while in another study, the authors compared kinematic alignment (KA) with mechanical alignment (MA) during RATKA.25 All studies, except for one,15 reported the brand of robot used, and Mako CT-based robot was the most commonly used (seven studies).13,16, 17, 18, 19, 20, 21 Various implants were used, both cemented and cementless, and PS and CR (Table 2).
Table 2.
Operative details of the included studies.
| No. | Author/year | Operative time (Minutes) |
Machine used | Implant | ||
|---|---|---|---|---|---|---|
| RATKA | CTKA | P value | ||||
| 1 | Richards et al., 2022 (CR) | 91.8 ± 20.3 | MAKO, Stryker, Mahwah, NJ | Triathlon (CR), Stryker, Mahwah, NJ | ||
| Richards et al., 2022 (PS) | 91 ± 16.8 | MAKO, Stryker, Mahwah, NJ | Triathlon (PS), Stryker, Mahwah, NJ | |||
| 2 | Z. Li et al., 2022 | 126 (105–180) | HURWA, BEIJING HURWA-ROBOT Technology Co. Ltd | Legion system (Smith & Nephew, London, UK) | ||
| 3 | C. Li et al., 2022 | 126.0 (105–180) | 75.2 (50–90) | <0.0001 | NR | ADVANCE designs (MicroPort Orthopedics Inc., China) |
| 4 | Smith et al., 2021 | 96 | 86 | <0.01 | MAKO, Stryker, Mahwah, NJ | Triathlon (PS), Stryker, Mahwah, NJ (110 cementless, 10 cemented) |
| 5 | Shaw et al., 2021 | 76.8 | 87.2 | <0.001 | MAKO, Stryker, Kalamazoo, MI | (Cemented and cementless implants) |
| 6 | Samuel et al., 2021 | 113 | 105 | <0.001 | MAKO, Stryker, Kalamazoo, MI | Stryker implants (Stryker Corp.) |
| 7 | Nickel et al., 2021 | NR | MAKO, Stryker, Mahwah, NJ | NR | ||
| 8 | Mitchell et al., 2021 | NR | MAKO, Stryker, Mahwah, NJ | Triathlon (CR), Stryker, Mahwah, NJ | ||
| 9 | Marchand et al., 2021 | NR | MAKO, Stryker, Mahwah, NJ | Triathlon, cementless (CR), Stryker, Mahwah, NJ | ||
| 10 | Held et al., 2021 | 123 | 107 | <0.001 | NAVIO imageless surgical system; Smith & Nephew, Memphis TN | Journey II BCS; Smith & Nephew, Memphis TN |
| 11 | Blum et al., 2021 | NR | The OMNIBotics Robotic-Assisted Total Knee System. | OMNI Apex Ultra-Congruent system (Corin USA, Raynham, MA) | ||
| 12 | Kim et al. 2020 | 97 (81–123) | 69 (56–81) | <0.001 | ROBODOC system (Integrated Surgical Systems Inc, Davis, CA, USA) | A Duracon (PS) (Stryker Orthopedics, Mahwah, NJ, USA) |
| 13 | Yeo et al., 2019 (KA) | NR | ROBODOC system (Integrated Surgical System, Davis, CA, USA). | NexGen, (CR) prosthesis (Zimmer, Warsaw, IN, USA) | ||
| Yeo et al., 2019 (MA) | NR | ROBODOC system (Integrated Surgical System, Davis, CA, USA). | NexGen, (CR) prosthesis (Zimmer, Warsaw, IN, USA) | |||
Data presented as mean ± SD (range) whenever possible. RATKA: robotic assisted total knee arthroplasty, CTKA: conventional total knee arthroplasty, CR: cruciate retaining, PS: posterior stabilized, RCT: randomized controlled trial.
Seven studies reported the operative time, which ranged from 76.8 to 156 min.13,14,16, 17, 18,22,24 Six of seven comparative studies reported that the operative time for RATKA was longer than that for CTKA technique.13,14,16,18,22,24 In one study in which the authors reported a shorter operative time in the RATKA group,17 most of the implants used were cementless, whereas cemented implants were mainly used in the CTKA group. Furthermore, the length of hospital stay (LOS) was reported in six studies which ranged from 0.48 to 2.1 days.13,16, 17, 18,20,22 In five studies comparing RATKA vs. CTKA, four found LOS was less in RATKA patients compared to CTKA patients,13,16, 17, 18,20 and in one study, the authors found no difference.22
Regarding outcomes (Table 3), all studies reported various functional outcomes (PROMs and knee ROM), seven reported the radiological outcomes, and eight reported the complication rates.
Table 3.
Outcomes of the included studies.
| No. | Study | PROMs |
ROM |
Radiological |
Complications | Revisions | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RATKA | CTKA | P-value | RATKA | CTKA | P-value | RATKA | CTKA | P-value | ||||
| 1 | Richards et al., 2022(CR) | KSS function: 84.1 ± 14.2 KSS knee: 92.2 ± 9.1 WOMAC: 86.7 ± 13.2 FJS: 65.4 ± 28.9 KOOS-JR: 83 ± 16.9 Satisfaction: 93.1 |
NR | NR | −2 superficial infection (managed conservatively) −10 stiffness (managed by MUA) |
Total 3: 1 instability, 1 for persistent stiffness, 1 periprosthetic fracture |
||||||
| Richards et al., 2022(PS) | KSS function: 84.3 ± 16.5 KSS knee: 89.9 ± 11.4 WOMAC: 84.6 ± 19.9 FJS: 66.3 ± 28 KOOS-JR: 83.5 ± 18 Satisfaction: 94.7 |
NR | NR | −2 superficial infection (managed conservatively) −10 stiffness (managed by MUA) |
Total 3: all were for instability | |||||||
| 2 | Z. Li et al., 2022 | KSS function: 58.2 ± 18.19 KSS knee: 70 ± 7.31 WOMAC: 80.6 ± 46.5 SF 36: 61.19 ± 19.9 HSS score: 80.1 ± 12.461 |
54.7 ± 19.52 67.8 ± 10.06 72.1 ± 44.40 63.05 ± 19.021 79.45 ± 11.52 |
0.3942 0.1107 0.2559 0.4511 0.9862 |
114.5 ± 18.41 (60–135) (Measured at 12 weeks) |
111.6 ± 18.75 (75–140) | 0.2877 | HKA: 1.8 ± 1.6 varus (0.15–7.75) | 3 ± 2.7 varus (0.2–15.15) | 0.0207 | NR | NR |
| 3 | C. Li et al., 2022 | KSS knee: 92.3 (64–99) WOMAC: 8.9 (4–22) (Measured at 90 days) |
91.8 (66–98) 8.9 (4–22) |
0.8308 0.9552 |
106 (70–120) (Measured at 90 days) |
103.5 (80–120) | 0.3613 | 21 (80.8%) patients were within ±3° | 15 (57.7%) patients were within ±3° | 0.1318 | NR | NR |
| 4 | Smith et al., 2021 | KSS function: 80 KSS knee: 85 Satisfaction 94% |
73 82 84% |
0.005 0.046 0.036 |
119 | 116 | 0.02 | NR | −9: Stiffness, all underwent MUA, 6 needed arthroscopic lysis. −2: non-fatal PE |
0 | ||
| 5 | Shaw et al., 2021 | KOOS-JR: 71.72 PROMIS: -MH:54.84 -PH: 49.43 (Measured at 8 months) |
72.08 51.64 48.62 |
0.727 0.010 0.471 |
NR | NR | NR | NR | ||||
| 6 | Samuel et al., 2021 | KOOS -pain: 42.7 ± 19.7 -PS: 26.2 ± 17.1 -KRQoL: 50.6 ± 21.9 VR-12 -MCS: 0.03 ± 9.80 -PCS: 17.8 ± 9.25 (Measured at 12 months, as differences from baseline (scaled)) |
42.2 ± 18.5 26.8 ± 16.5 47.1 ± 26.2 0.03 (9.80) 17.8 (9.25) |
0.836 0.796 0.283 0.127 0.711 |
117.8 ± 10.2 (Measured at 90 days) | 120.3 ± 9.9 | 0.043 | NR | −2 superficial infection −2 stiffness −1 DVT |
0 | ||
| 7 | Nickel et al., 2021 | KOOS-JR: 89.6 LEAS: 11.9 NPRS: 0.7 (Measured at 24 months) |
NR | HKA: 0.97 ± 1.79 (−2.4 to 3) (Measured at 12 months) |
−5 stiffness (managed by MUA) −1 patellar clunk required arthroscopy |
0 | ||||||
| 8 | Mitchell et al., 2021 | KOOS-JR: 75.8 ± 12.5 VR-12 -MCS: 55.9 ± 9.0, -PCS: 42.9 ± 9.7 UCLA: 6.1 ± 1.7 |
72.2 ± 13.7 55.4 ± 9.2 41.6 ± 10.6 5.6 ± 2.3 |
0.072 0.668 0.336 0.059 |
NR | NR | NR | 0 | ||||
| 9 | Marchand et al., 2021 | r-WOMAC -pain: 1 ± 2 (0–10) -Physical function: 2 ± 3 (0–14) -Total: 4 ± 5 (0–24) (Measured at 24 months) |
2 ± 3 (0–9) 4 ± 5 (0–28) 6 ± 7 (0–28) |
0.024 0.009 0.009 |
NR | Tibial alignment in the coronal plane was within 3° of varus and valgus in all cases | NR | −2 Stiffness: (one underwent MUA, one underwent 2 arthroscopies then poly exchange at 24 months) −1 DVT −1 PE −1 posterolateral mechanical catching underwent arthroscopic synovectomy at 13 months |
0 | |||
| 10 | Held et al., 2021 | KSS function: 75 WOMAC: -Function:87.30, -Stiffness:82.26, -Pain:90.48 SF 12: -M:44.83 -P:48.57 |
76.04 81.90 76.09 87.10 45.33 47.11 |
0.820 0.182 0.232 0.327 0.713 0.220 |
123 | 120 | 0.37 | NR | −2 Periprosthetic fracture: (one distal femoral fracture due to a fall required surgical intervention and one unicortical tibial fracture at pin site, treated conservatively) −1 aseptic loosening (stable loose lines and not revised) −10 superficial infection (3 were at pin site, treated conservatively) −2 Deep infection: treated by DAIR −1 stiffness -1 patellar tendon rupture |
NR | ||
| 11 | Blum et al., 2021 | KOOS (Measured at 24 months) -pain 46.3 ± 15.0 -Symptoms 40.3 ± 15.7 -ADL: 42.9 ± 15.4 -KRQoL 57.2 ± 18.9 -Sports and Rec: 45.2 ± 27.2 Satisfaction 100% |
139 ± 4 (Measured immediate postoperatively) | HKA: 0.8 ± 1.1 (Measured immediate postoperatively) | −2 Stiffness: managed by MUA | NR | ||||||
| 12 | Kim et al., 2020 | KSS knee: 93 ± 5 WOMAC: 18 ± 14 points UCLA: 7 points |
92 ± 6 19 ± 15 7 points |
0.321 0.981 1.000 |
125 ± 6 | 128 ± 7° | 0.321 | −86% were within ±3° of neutral mechanical alignment. -Anatomical TF angle:2 ± 2 (0–6) of valgus -TIBIA: 90 ± 1 (87–94) -FEMUR: 98 ± 2 (94–102) |
- 74% - 3 ± 3 (0–8) valgus −89 ± 6 2 (86–92) −97 ± 2 (91–101) |
−0.035 −0.897 −0.721 −0.953 |
−15 knees had aseptic loosening of the femoral and/or tibial component (the authors did not report if they were revised or not). −4 Superficial infection |
NR |
| 13 | Yeo et al., 2019(KA) | KSS function 90.1 ± 10.5 KSS (pain) 47.5 ± 5.6 WOMAC19.3 ± 1.9 HSS score 93.2 ± 8 |
125 ± 11.5 | HKA: 0.1 ± 2 TIBIA: 87.5 ± 1.7 FEMUR: 91.7 ± 1.9 |
NR | NR | ||||||
| Yeo et al., 2019 (MA) | KSS function 93 ± 9.1 KSS (pain) 47.2 ± 7.5 WOMAC20.4 ± 1.8 HSS score 94.8 5.5 |
129 ± 11.5 | HKA: − 0.3 ± 1.7 TIBIA: 90.1 ± 0.4 FEMUR: 89.5 ± 0.4 |
NR | NR | |||||||
PROMS: patient reported outcomes measures, ROM: range of motion, CR: cruciate retaining, PS: posterior stabilized, RATKA: robotic assisted total knee arthroplasty, CTKA: conventional total knee arthroplasty, KSS: knee society score, WOMAC: Western Ontario and McMaster Universities scoring systems, FJS: forgotten joint score, KOOS-JR: Knee Injury and Osteoarthritis Outcome Score for Joint Replacement, NR: not reported, MUA: manipulation under anesthesia, SF 36: short form, HSS: Hospital for Special Surgery, HKA: hip-knee-ankle mechanical angle, PE: pulmonary embolism, PROMIS: Patient-Reported Outcomes Measurement Information System, MH: mental health, PH: physical health, KRQoL: KOOS knee–related quality-of-life sub-score, LEAS: Lower Activity Extremity Score, NPRS: Numeric Pain Rating Scale, VR-12 MCS/PCS: Veterans RAND 12-Item Health Survey–Mental Component/Physical Component Scores, UCLA: University of California at Los Angeles Activity Score, r-WOMAC: reduced Western Ontario and McMaster Universities Osteoarthritis Index, SF-12 M and P: Short Form 12 Mental and Physical scores, DAIR: debridement, antibiotics and implant retention, KA: kinematic alignment, MA: mechanical alignment. N.B. the underlined complications were directly related to the robotic machine use.
3.2. Functional outcomes
Although various measures were used to evaluate the PROMs, all studies reported acceptable outcomes (Table 3). Patient satisfaction rates reported separately in three studies13,16,23 which were 93.1%, 94.7, 94%, and 100%, respectively. Of the nine studies comparing RATKA with CTKA, no difference at the last follow-up regarding functional outcomes between the two techniques was found in seven studies,14,15,17,18,20,22,24 while in two studies, the authors reported that RATKA achieved better functional outcomes compared to CTKA.16,21 Knee ROM was reported in six studies,14,15,18,23, 24, 25 ranging between 106 and 139° of flexion (Table 3).
3.3. Radiological outcomes
These were reported in seven studies (either overall mechanical limb alignment or individual component alignment in the coronal plane).14,15,19,21,23, 24, 25 Six studies reported on the overall alignment; in four studies, all RATKA patients had mechanical alignment within ± 3° of neutral alignment; and HKA ranged from −0.3 to 1.8°.14,19,23,25 In two studies, no exact values were reported; however, the mechanical alignment was within ± 3° of neutral alignment in 80.8 and 86% of the included patients, respectively.15,24 Two studies reported no difference in the radiological measurements between RATKA and CTKA,15,24 while in one study,14 the authors achieved better radiological outcomes in the RATKA group (Table 3).
3.4. Complications
Eight studies reported complications,13,16,18,19,21, 22, 23, 24 details of which are reported in (Table 3); however, the most common complication was stiffness which needed manipulation under anesthesia in most cases. Only one study reported two types of complications related to using the robotic machine22; the first was a superficial infection at the pin site, which was reported in three patients, and the second was a unicortical tibial fracture at a pin site in one patient; all were treated conservatively. In six comparative studies,16,18,20, 21, 22,24 the authors reported no difference in the incidence of complications between RATKA and CTKA.
4. Discussion
Although robotic-assisted surgery was introduced to knee arthroplasty surgery as early as 1980, aiming to provide accurate prosthesis alignment and decrease the malpositioning rates, it was not until the last decade that it began to gain popularity during total and partial knee arthroplasties.11,26
Several reports have supported the claims for adopting this new technology after proving its ability to drive proper component alignment, aid soft-tissue protection, and increase patient satisfaction.8,10,27,28 However, some concerns remain and are contentious, such as its cost-effectiveness, the learning curve, and most importantly, the long-term benefit of its usage.11,26,29
After a detailed analysis and review of the most recent publications on RATKA, we find that most of the studies have reported similar functional outcomes when comparing RATKA with CTKA; furthermore, radiological results and even complication rates were comparable. Most studies have reported short-term follow-ups, and the only included long-term follow-up RCT study by Kim et al.24 showed no difference between both techniques. In this review, we have not included studies evaluating the cost of this technology adoption or the learning curve.
We discuss and summarize below additional recent studies which have reported upon various facets of RATKA. Emara et al.5 evaluated the early perioperative outcomes of technology-assisted (computer navigation and robotic-assisted) knee arthroplasty (including total and partial knee arthroplasty) by examining the US National Inpatient Sample between 2008 and 2018. In over 6.5 million procedures, the authors found that robotic-assisted procedures had a shorter LOS (2.0 ± 1.4 days versus 2.5 ± 1.8 days; p < 0.001) and fewer implant-related complications (including dislocation, periprosthetic fractures, wound problems and infection) compared to CTKA. They also found that in-hospital costs were lower for robotic-assisted procedures than for computer navigation. Their study showed an increasing trend of adopting robotic-assisted surgery over the ten-year study period (0.1% in 2008 versus 4.3% in 2018); they predicted that robotic-assisted surgery will represent 50% of all technology-assisted knee arthroplasty by 2030.5
This increasing trend of RATKA utilization was similarly echoed in a study by Naziri et al.,30 who found an increase of 500% between 2009 and 2013 among 27 hospitals in New York State, USA.
In an analysis of 22 studies comparing RATKA with CTKA, Agrawal et al.10 reported that RATKA resulted in better PROMs and radiological outcomes compared to CTKA. However, they mentioned that this superiority was unclear, and further analysis of complications and cost should be considered when interpreting the present data before the widespread adoption of this technology.
Jeon et al.7 retrospectively compared the long-term (mean follow up of 11 years) functional and radiological outcomes between 84 RATKAs and 79 CTKAs. They reported significantly longer tourniquet time in the RATKA group; however, there was no significant difference between both groups in terms of Knee Society scores (KSS), SF-36, and ROM. Although RATKA showed fewer outliers for mechanical alignment (measured as HKA angle) than the CTKA group, this did not reach statistical significance. Furthermore, no difference was found regarding complication and revision rates.
In a meta-analysis of 18 studies comparing the results of RATKA with CTKA, Onggo et al.31 reported the superiority of RATKA for radiological outcomes. While the functional outcomes and rate of overall complications were comparable between both techniques, the rate of periprosthetic infection was higher in two studies with RATKA.
In a meta-analysis evaluating seven studies (six were RCTs) comparing the results of ROBODOC image-based autonomous system with CTKA; Ren et al. 2,31 found that operative time was shorter with CTKA; but there were no differences in functional outcomes based on the Hospital for Special Surgery (HSS) scores and knee ROM; however, WOMAC and KSS scores were superior at six months postoperatively with RATKA. Furthermore, better postoperative lower limb alignment and more precise individual component positioning were observed with RATKA.
Song et al. randomized patients having simultaneous bilateral TKA into a RATKA group and a conventional TKA group. They reported more precision of mechanical axis restoration with RATKA; however, the coronal alignment of the femoral and tibial components was not different in both groups. Also, they reported no difference regarding functional outcomes or implant survivorship between both techniques.32 At 13 years of follow up, Cho et al.33 showed similar survivorship in RATKA vs. CTKA, despite the better overall mechanical limb alignment and individual component sagittal alignment with RATKA.
In a network metanalysis evaluating the role of new technologies (including robotics, computer navigation, and patient-specific cutting blocks) during TKA surgery vs. CTKA, Bouch'e et al.34 found that RATKA had the least outliers for postoperative mechanical alignment. The difference however, from other techniques was insignificant, with no difference in the functional outcomes at six, 12, and 24 months postoperatively (using KSS and WOMAC scores). They concluded that new technologies should be adopted cautiously until solid evidence proves their superiority over conventional manual techniques.
The cost-effectiveness of using robotic-assisted technology was not discussed in the studies in the current review. For the sake of completeness of this review, we discuss some recent papers that have shed light on this aspect. To compare the cost burden of RATKA to CTKA, Cool et al.35 carried out a case-controlled study including a propensity score matching. They demonstrated a significant decrease in the 90-day episode of care costs compared to CTKA; this was mainly attributed to the shorter length of stay and less 90-day acute postoperative services, even after accounting for the preoperative CT scan needed for planning the cost savings were up to US$ 2182. Another study36 reported a reduction in 90-day costs with RATKA vs. CTKA ($28,943 vs. $31,028; P = 0.05), owing to a decrease in LOS, 90-days readmission, and non-home discharge. Institutions may be less enthusiastic about adopting robotic technology due to the elevated initial startup costs to obtain a robotic system that could reach up to $1,000,000 and $545,000 in USA and Europe, respectively.26,37 Even after the justification of using robotic technology from a cost-effectiveness point of view, there is still a concern regarding exposing the patient to excess radiation while obtaining a preoperative CT scan, especially given that the risks do not seem to be mitigated by the enhanced benefit of RATKA over CTKA.11,37 Ponzio and Lonner found the mean effective radiation dose from preoperative CT scans required for planning of robotic-assisted UKA was 4.8 ± 3.0 mSv (millisieverts), which is equal to 48 chest x-rays; furthermore, a quarter of their patients required one or more further CT scans thus increasing the effective radiation dose to 103 mSv.38 This needs to be borne in mind given that patients are at an increased risk of radiation-induced cancers when exposed to doses between 10 and 100 mSv.39
Soft-tissue preservation is one of the suggested benefits of RATKA. A prospective comparative study by Kalyani et al.27 showed significantly less medial soft tissue injury and more precise femoral and tibial cuts with RATKA compared to CTKA. However, there are concerns related to the pins used to fix the tracking array, both as a source of postoperative pin tract infection and periprosthetic fracture (if placed in the diaphyseal instead of the metaphyseal segment).29 Chun et al. have reported a 5% incidence of patellar tendon disruption while using RATKA.40
The current review has some limitations; first, in order to keep the current review updated, we included the recently published studies and excluded some of the previously published work, which could have changed the results of the current review. Second, most of the included studies presented relatively short-term follow-ups. Last, we did not perform a thorough statistical analysis of the included studies.
5. Conclusion
Although robotic-assisted total knee arthroplasty is a promising technology that provides better component alignment and superior early functional outcomes, the justification for its widespread adoption needs more robust evidence through well-designed and better long-term studies demonstrating superior, predictable, and durable clinical results compared to conventional total knee arthroplasty techniques.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
Informed consent (patient/guardian)
Not applicable.
Institutional ethical committee approval (for all human studies)
Not applicable.
Authors' contribution
Both authors contributed equally to the design, research, and writing of the paper.
Declaration of competing interest
Arun Mullaji receives royalties from DePuy and Springer and institutional support from DePuy and Zimmer Biomet.
Acknowledgment
None.
Contributor Information
Arun B. Mullaji, Email: arunmullaji@gmail.com.
Ahmed A. Khalifa, Email: ahmed_adel0391@med.svu.edu.eg.
References
- 1.Kahlenberg C.A., Nwachukwu B.U., McLawhorn A.S., Cross M.B., Cornell C.N., Padgett D.E. Patient satisfaction after total knee replacement: a systematic review. HSS J. 2018;14(2):192–201. doi: 10.1007/s11420-018-9614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakano N., Shoman H., Olavarria F., Matsumoto T., Kuroda R., Khanduja V. Why are patients dissatisfied following a total knee replacement? A systematic review. Int Orthop. 2020;44(10):1971–2007. doi: 10.1007/s00264-020-04607-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bistolfi A., Giustra F., Bosco F., et al. Comparable results between crosslinked polyethylene and conventional ultra-high molecular weight polyethylene implanted in total knee arthroplasty: systematic review and meta-analysis of randomised clinical trials. Knee Surg Sports Traumatol Arthrosc. 2022 doi: 10.1007/s00167-022-06879-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mihalko W.M., Haider H., Kurtz S., Marcolongo M., Urish K. New materials for hip and knee joint replacement: what's hip and what's in kneed? J Orthop Res. 2020;38(7):1436–1444. doi: 10.1002/jor.24750. [DOI] [PubMed] [Google Scholar]
- 5.Emara A.K., Zhou G., Klika A.K., et al. Robotic-arm-assisted knee arthroplasty associated with favorable in-hospital metrics and exponentially rising adoption compared with manual knee arthroplasty. J Am Acad Orthop Surg. 2021;29(24):e1328–e1342. doi: 10.5435/JAAOS-D-21-00146. [DOI] [PubMed] [Google Scholar]
- 6.Panjwani T.R., Mullaji A., Doshi K., Thakur H. Comparison of functional outcomes of computer-assisted vs conventional total knee arthroplasty: a systematic review and meta-analysis of high-quality, prospective studies. J Arthroplasty. 2019;34(3):586–593. doi: 10.1016/j.arth.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 7.Jeon S.W., Kim K.I., Song S.J. Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty. 2019;34(8):1656–1661. doi: 10.1016/j.arth.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Khlopas A., Sodhi N., Hozack W.J., et al. Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg. 2020;33(7):685–690. doi: 10.1055/s-0039-1684014. [DOI] [PubMed] [Google Scholar]
- 9.Marchand R.C., Sodhi N., Anis H.K., et al. One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg. 2019;32(11):1063–1068. doi: 10.1055/s-0039-1683977. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal N., To K., McDonnell S., Khan W. Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2020;35(11):3393–3409 e2. doi: 10.1016/j.arth.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Onggo J.R., Onggo J.D., De Steiger R., Hau R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg. 2020;140(10):1533–1549. doi: 10.1007/s00402-020-03512-5. [DOI] [PubMed] [Google Scholar]
- 12.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richards J.A., Williams M.D., Gupta N.A., et al. No difference in PROMs between robotic-assisted CR versus PS total knee arthroplasty: a preliminary study. J Rob Surg. 2022 doi: 10.1007/s11701-021-01352-y. In press. [DOI] [PubMed] [Google Scholar]
- 14.Li Z., Chen X., Wang X., et al. HURWA robotic-assisted total knee arthroplasty improves component positioning and alignment - a prospective randomized and multicenter study. J Orthop Translat. 2022;33:31–40. doi: 10.1016/j.jot.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li C., Li T., Zhang Z., et al. Robotic-arm assisted versus conventional technique for total knee arthroplasty: early results of a prospective single centre study. Int Orthop. 2022 doi: 10.1007/s00264-022-05351-y. [DOI] [PubMed] [Google Scholar]
- 16.Smith A.F., Eccles C.J., Bhimani S.J., et al. Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg. 2021;34(7):730–738. doi: 10.1055/s-0039-1700837. [DOI] [PubMed] [Google Scholar]
- 17.Shaw J.H., Lindsay-Rivera K.G., Buckley P.J., Weir R.M., Banka T.R., Davis J.J. Minimal clinically important difference in robotic-assisted total knee arthroplasty versus standard manual total knee arthroplasty. J Arthroplasty. 2021;36(7S):S233–S241. doi: 10.1016/j.arth.2021.02.038. [DOI] [PubMed] [Google Scholar]
- 18.Samuel L.T., Karnuta J.M., Banerjee A., et al. Robotic arm-assisted versus manual total knee arthroplasty: a propensity score-matched analysis. J Knee Surg. 2021 doi: 10.1055/s-0041-1731323. [DOI] [PubMed] [Google Scholar]
- 19.Nickel B.T., Carroll K.M., Pearle A.D., et al. The accuracy and clinical success of robotic-assisted total knee arthroplasty. HSS J. 2021;17(3):261–266. doi: 10.1177/15563316211026307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell J., Wang J., Bukowski B., et al. Relative clinical outcomes comparing manual and robotic-assisted total knee arthroplasty at minimum 1-year follow-up. HSS J. 2021;17(3):267–273. doi: 10.1177/15563316211028568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marchand K.B., Moody R., Scholl L.Y., et al. Results of robotic-assisted versus manual total knee arthroplasty at 2-year follow-up. J Knee Surg. 2021 doi: 10.1055/s-0041-1731349. [DOI] [PubMed] [Google Scholar]
- 22.Held M.B., Gazgalis A., Neuwirth A.L., Shah R.P., Cooper H.J., Geller J.A. Imageless robotic-assisted total knee arthroplasty leads to similar 24-month WOMAC scores as compared to conventional total knee arthroplasty: a retrospective cohort study. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2021;7 doi: 10.1007/s00167-021-06599-4. [DOI] [PubMed] [Google Scholar]
- 23.Blum C.L., Lepkowsky E., Hussein A., Wakelin E.A., Plaskos C., Koenig J.A. Patient expectations and satisfaction in robotic-assisted total knee arthroplasty: a prospective two-year outcome study. Arch Orthop Trauma Surg. 2021;141(12):2155–2164. doi: 10.1007/s00402-021-04067-9. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y.H., Yoon S.H., Park J.W. Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized, controlled trial. Clin Orthop Relat Res. 2020;478(2):266–275. doi: 10.1097/CORR.0000000000000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yeo J.H., Seon J.K., Lee D.H., Song E.K. No difference in outcomes and gait analysis between mechanical and kinematic knee alignment methods using robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1142–1147. doi: 10.1007/s00167-018-5133-x. [DOI] [PubMed] [Google Scholar]
- 26.Lang J.E., Mannava S., Floyd A.J., et al. Robotic systems in orthopaedic surgery. J Bone Jt Surg Br. 2011;93(10):1296–1299. doi: 10.1302/0301-620X.93B10.27418. [DOI] [PubMed] [Google Scholar]
- 27.Kayani B., Konan S., Pietrzak J.R.T., Haddad F.S. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty. 2018;33(8):2496–2501. doi: 10.1016/j.arth.2018.03.042. [DOI] [PubMed] [Google Scholar]
- 28.Kayani B., Konan S., Huq S.S., Tahmassebi J., Haddad F.S. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1132–1141. doi: 10.1007/s00167-018-5138-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lonner J.H., Fillingham Y.A. Pros and cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty. 2018;33(7):2007–2013. doi: 10.1016/j.arth.2018.03.056. [DOI] [PubMed] [Google Scholar]
- 30.Naziri Q., Burekhovich S.A., Mixa P.J., et al. The trends in robotic-assisted knee arthroplasty: a statewide database study. J Orthop. 2019;16(3):298–301. doi: 10.1016/j.jor.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ren Y., Cao S., Wu J., Weng X., Feng B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med. 2019;95(1121):125–133. doi: 10.1136/postgradmedj-2018-136190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song E.K., Seon J.K., Park S.J., Jung W.B., Park H.W., Lee G.W. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1069–1076. doi: 10.1007/s00167-011-1400-9. [DOI] [PubMed] [Google Scholar]
- 33.Cho K.J., Seon J.K., Jang W.Y., Park C.G., Song E.K. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop. Jun 2019;43(6):1345–1354. doi: 10.1007/s00264-018-4231-1. [DOI] [PubMed] [Google Scholar]
- 34.Bouche P.A., Corsia S., Dechartres A., Resche-Rigon M., Nizard R. Are there differences in accuracy or outcomes scores among navigated, robotic, patient-specific instruments or standard cutting guides in TKA? A network meta-analysis. Clin Orthop Relat Res. 2020;478(9):2105–2116. doi: 10.1097/CORR.0000000000001324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cool C.L., Jacofsky D.J., Seeger K.A., Sodhi N., Mont M.A. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Effect Res. 2019;8(5):327–336. doi: 10.2217/cer-2018-0136. [DOI] [PubMed] [Google Scholar]
- 36.Koenig J., Plaskos C. Ninety-day costs and clinical results of robotic-assisted and conventional total knee arthroplasty. Br Editor Soc Bone Joint Surg. 2019:125. [Google Scholar]
- 37.Swank M.L., Alkire M., Conditt M., Lonner J.H. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthoped. 2009;38(2 Suppl):32–36. [PubMed] [Google Scholar]
- 38.Ponzio D.Y., Lonner J.H. Preoperative mapping in unicompartmental knee arthroplasty using computed tomography scans is associated with radiation exposure and carries high cost. J Arthroplasty. 2015;30(6):964–967. doi: 10.1016/j.arth.2014.10.039. [DOI] [PubMed] [Google Scholar]
- 39.Lin E.C. Radiation risk from medical imaging. Mayo Clin Proc. 2010;85(12):1142–1146. doi: 10.4065/mcp.2010.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chun Y.S., Kim K.I., Cho Y.J., Kim Y.H., Yoo M.C., Rhyu K.H. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty. 2011;26(4):621–625. doi: 10.1016/j.arth.2010.05.017. [DOI] [PubMed] [Google Scholar]