This cross-sectional study uses Centers for Disease Control and Prevention data to estimate cases of COVID-19 among people experiencing homelessness at US state and local levels and to compare the incidence rates with those in the general population.
Key Points
Question
How many cases of COVID-19 in the US have occurred among people experiencing homelessness?
Findings
In this cross-sectional study of 64 US jurisdictional health departments, 26 349 cases of COVID-19 among people experiencing homelessness were reported at the state level and 20 487 at the local level. The annual incidence rate of COVID-19 was lower among people experiencing homelessness than in the general population at state and local levels.
Meaning
The findings suggest that incorporating housing and homelessness status in infectious disease surveillance may improve understanding of the burden of infectious diseases among disproportionately affected groups and aid public health decision-making.
Abstract
Importance
A lack of timely and high-quality data is an ongoing challenge for public health responses to COVID-19 among people experiencing homelessness (PEH). Little is known about the total number of cases of COVID-19 among PEH.
Objective
To estimate the number of COVID-19 cases among PEH and compare the incidence rate among PEH with that in the general population.
Design, Setting, and Participants
This cross-sectional study used data from a survey distributed by the Centers for Disease Control and Prevention to all US state, district, and territorial health departments that requested aggregated COVID-19 data among PEH from January 1, 2020, to September 30, 2021. Jurisdictions were encouraged to share the survey with local health departments.
Main Outcomes and Measures
The primary study outcome was the number of cases of COVID-19 identified among PEH. COVID-19 cases and incidence rates among PEH were compared with those in the general population in the same geographic areas.
Results
Participants included a population-based sample of all 64 US jurisdictional health departments. Overall, 25 states, districts, and territories completed the survey, among which 18 states (72.0%) and 27 localities reported COVID-19 data among PEH. A total of 26 349 cases of COVID-19 among PEH were reported at the state level and 20 487 at the local level. The annual incidence rate of COVID-19 among PEH at the state level was 567.9 per 10 000 person-years (95% CI, 560.5-575.4 per 10 000 person-years) compared with 715.0 per 10 000 person-years (95% CI, 714.5-715.5 per 10 000 person-years) in the general population. At the local level, the incidence rate of COVID-19 among PEH was 799.2 per 10 000 person-years (95% CI, 765.5-834.0 per 10 000 person-years) vs 812.5 per 10 000 person-years (95% CI, 810.7-814.3 per 10 000 person-years) in the general population.
Conclusions and Relevance
These results provide an estimate of COVID-19 incidence rates among PEH in multiple US jurisdictions; however, a national estimate and the extent of under- or overestimation remain unknown. The findings suggest that opportunities exist for incorporating housing and homelessness status in infectious disease reporting to inform public health decision-making.
Introduction
In the US, more than half a million people experience homelessness on any given night.1 Compared with the general population, people experiencing homelessness (PEH) have a higher burden of infectious diseases, behavioral health diagnoses, and chronic health conditions.2,3,4,5 SARS-CoV-2, the virus that causes COVID-19, is highly transmissible, especially in congregate settings, such as homeless shelters, where there may be crowding and frequent client turnover.6,7,8 Between March and September 2020, numerous COVID-19 outbreaks were reported at homeless shelters, but little is known about cases of COVID-19 among PEH in general.9,10,11,12,13 Given the infectious disease risks for PEH, it is critical to better understand the true burden of COVID-19 in this population to inform prevention recommendations and provision of care.14
The purpose of this study was to gather information from state, territorial, district, county, city, and other local jurisdictions to estimate the number of COVID-19 cases that have occurred among PEH. This study also aimed to compare the incidence rate of COVID-19 among PEH with that in the general population in the jurisdictions collecting these data.
Methods
Design, Setting, and Participants
This cross-sectional study was conducted in November 2021. The Centers for Disease Control and Prevention sent state health departments a link to a standardized REDCap survey requesting deidentified and aggregated COVID-19 data among PEH. State health departments were encouraged to share the survey with county and local health departments within their state. Survey questions captured the name and level of the jurisdiction (state, territory, district, county, city, or other); point of contact information for follow-up questions; how the jurisdiction defined homelessness in data collection, including duration of homelessness; the data sources the jurisdiction used to identify or verify housing or homelessness status among COVID-19 cases; the total number of cases of COVID-19 among PEH in their jurisdiction from January 1, 2020, through September 30, 2021; and when available, the proportion of COVID-19 cases among PEH by race and ethnicity and by sex. Responses from states, territories, and districts were grouped and are presented as state- and district-level results, and responses from counties, cities, and other local health agencies were grouped and are presented as local-level results. This research was reviewed by the Centers for Disease Control and Prevention and was conducted consistently with applicable federal law and Centers for Disease Control and Prevention policy (45 CFR §46, 21 CFR §56, 42 USC §241(d), 5 USC §552a, 44 USC §3501, et seq). Written informed consent was obtained from participants at the beginning of the survey. Data are presented descriptively following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.25
Public Data Sources and Measurement of Homelessness
We obtained COVID-19 case data for the general population in the same jurisdictions and during the same time frame as available data on PEH from USAFacts, which aggregates data from the Centers for Disease Control and Prevention and state health departments.15 Population size for the respective jurisdictions was obtained from the US Census Bureau.16 Publicly available data from the US Department of Housing and Urban Development (HUD) 2020 Point-in-Time (PIT) count served as the population estimates for PEH to calculate the COVID-19 incidence per 10 000 PEH in a subsample of the participating jurisdictions.1 The PIT count estimates the number of individuals and families experiencing homelessness during any given night in January of each year and includes counting the number of people living unsheltered (outdoors or in a car, tent, or other place not meant for human habitation) as well as the number of individuals accessing services at emergency homeless shelters or enrolled in transitional housing programs.17
Method for Estimating COVID-19 Incidence Rate Among PEH
Because not all responding jurisdictions collected COVID-19 case data among PEH for the same duration and they used varying definitions of homelessness, we limited the number of jurisdictions used to estimate an incidence rate. Jurisdictions that collected data with at least 1 of the following components in their definition were included in the estimates: person stayed in a homeless shelter, person accessed other homeless services, person slept outside in a place not meant for human habitation, person stayed in transitional housing, person was described as experiencing homelessness in medical records, or person described themselves as experiencing homelessness (such as in a case interview). Jurisdictions that included people staying with friends (“couch surfing”), people staying in permanent supportive housing, and people in hotels or motels were excluded from incidence rate estimates regardless of any other definitions included because their definition of homelessness included experiences not included in HUD’s PIT count, which could lead to an overestimate.
Statistical Analysis
For jurisdictions that only reported assessing whether a person stayed in a homeless shelter, only the sheltered PIT count was included for the population estimate. Otherwise, the total number of PEH identified in the PIT count was used for the denominator. Free text responses were reviewed to identify whether jurisdictions only selecting “other” for the definition of homelessness should be included in incidence calculations. OpenEpi, version 3.01, was used to calculate incidence rates and 95% CIs.18
Results
State and District Level Results
Participants included a population-based sample of all 64 US jurisdictional health departments. At the state, territory, and district level, 25 jurisdictions completed the survey, of which 18 (72.0%; 17 states and the District of Columbia) indicated that they collected COVID-19 data among PEH. The District of Columbia and the states that collected data on PEH represent 50.6% of all PEH in the US, indicating that a large number of PEH in the US were not represented in these data.1 From January 1, 2020, to November 15, 2021, 17 states and the District of Columbia reported a total of 26 349 cases of COVID-19 among PEH (Table 1). Ten states were included in COVID-19 incidence rate calculations (Table 2). The annual state-level incidence rate of COVID-19 among PEH was 567.9 per 10 000 person-years (95% CI, 560.5-575.4 per 10 000 person-years). The annual incidence rate of COVID-19 in the general population in these same jurisdictions was 715.0 per 10 000 person-years (95% CI, 714.5-715.5 per 10 000 person-years).
Table 1. Cases of COVID-19 Among PEH and in the General Population in States and Districts Collecting COVID-19 Data Among PEH From January 2020 to November 2021.
| Jurisdiction | First date of available data | End date of available data | Duration of data availability, mo. | PEH | General population | ||
|---|---|---|---|---|---|---|---|
| COVID-19 cases, No. | Estimated No.a | COVID-19 cases, No.b | Estimated No.c | ||||
| Alaska | Mar 1, 2020 | Sep 30, 2021 | 19.0 | 1026 | 2888 | 108 604 | 731 545 |
| Arkansas | Apr 1, 2020 | Nov 15, 2021 | 19.5 | 584 | 2556 | 517 193 | 3 017 804 |
| California | Jan 27, 2020 | Sep 30, 2021 | 20.1 | 14 903 | 139 209 | 4 496 246 | 39 512 223 |
| Colorado | Jan 1, 2021 | Sep 30, 2021 | 9.0 | 2364 | 14 667 | 337 281 | 5 758 736 |
| Delaware | Feb 21, 2020 | Sep 30, 2021 | 19.3 | 345 | 1825 | 132 963 | 973 764 |
| District of Columbia | Apr 1, 2021 | Sep 30, 2021 | 6.0 | 583 | 22 351 | 16 497 | 705 749 |
| Hawaii | Apr 15, 2021 | Sep 30, 2021 | 5.5 | 94 | 6390 | 48 226 | 1 415 872 |
| Illinois | Jan 1, 2020 | Oct 28, 2021 | 21.9 | 1536 | 24 587 | 1 693 045 | 12 671 821 |
| Maine | Jan 1, 2020 | Sep 30, 2021 | 21.0 | 252 | 4531 | 89 989 | 1 344 212 |
| Minnesota | Apr 5, 2020 | Sep 30, 2021 | 17.8 | 1134 | 22 745 | 710 231 | 5 639 632 |
| Mississippi | Aug 11, 2020 | Sep 29, 2021 | 13.6 | 529 | 2684 | 419 647 | 2 976 149 |
| Montana | Jan 1, 2020 | Sep 30, 2021 | 21.0 | 551 | 2249 | 151 033 | 1 068 778 |
| Oregon | Jan 26, 2020 | Sep 30, 2021 | 20.1 | 550 | 17 210 | 330 055 | 4 217 737 |
| Pennsylvania | Mar 24, 2020 | Sep 30, 2021 | 18.2 | 393 | 8244d | 1 429 296 | 12 801 989 |
| Rhode Island | Mar 1, 2020 | Sep 30, 2021 | 19.0 | 359 | 3119 | 172 361 | 1 059 361 |
| South Dakota | Sep 1, 2020 | Sep 30, 2021 | 13.0 | 20 | 1724 | 131 040 | 884 659 |
| Tennessee | Apr 6, 2021 | Nov 14, 2021 | 7.3 | 339 | 10 519 | 478 774 | 6 829 174 |
| Utah | Jan 1, 2020 | Sep 30, 2021 | 21.0 | 787 | 6478 | 508 494 | 3 205 958 |
| Total | NA | NA | NA | 26 349 | 293 976 | 11 770 950 | 103 566 385 |
Abbreviations: NA, not applicable; PEH, people experiencing homelessness.
Population estimates of PEH are from the 2020 Point-in-Time estimates reported by the US Department of Housing and Urban Development.1
Cases of COVID-19 in the general population were accessed from USAFacts.15
Population estimates for the entire state are from the US Census Bureau.16
Pennsylvania reported only assessing cases of COVID-19 among PEH who stayed in homeless shelters. The Point-in-Time count includes only people staying in homeless shelters, not the total number of PEH.
Table 2. Incidence Rate of COVID-19 Among PEH and in the General Population in Jurisdictions That Collected Data for 12 or More Months and Defined Homelessness Similar to the US Department of Housing and Urban Development Definition From January 2020 to November 2021.
| Jurisdiction | Duration of follow-up, y | PEH | General population | ||||
|---|---|---|---|---|---|---|---|
| COVID-19 cases, No. | Estimated No.a | Incidence rate, per 10 000 person years (95% CI) | COVID-19 cases, No.b | Estimated No.c | Incidence rate, per 10 000 person-years (95% CI) | ||
| State level | |||||||
| California | 1.68 | 14 903 | 139 209 | 637.2 (627.1-647.5) | 4 496 246 | 39 512 223 | 677.3 (676.7-678.0) |
| Colorado | 0.75 | 2364 | 14 667 | 2149.0 (2064.0-2237.0) | 337 281 | 5 758 736 | 780.9 (778.3-783.6) |
| Hawaii | 0.46 | 94 | 6390 | 319.8 (259.9-389.6) | 48 226 | 1 415 872 | 740.5 (733.9-747.1) |
| Illinois | 1.83 | 1536 | 24 587 | 341.4 (324.6-358.8) | 1 693 045 | 12 671 821 | 730.1 (729.0-731.2) |
| Maine | 1.75 | 252 | 4531 | 317.8 (280.4-358.9) | 89 989 | 1 344 212 | 382.5 (380.0-385.0) |
| Minnesota | 1.48 | 1134 | 22 745 | 336.9 (317.7-356.9) | 710 231 | 5 639 632 | 850.9 (848.9-852.9) |
| Oregon | 1.68 | 550 | 17 210 | 190.2 (174.8-206.6) | 330 055 | 4 217 737 | 465.8 (464.2-467.4) |
| Pennsylvania | 1.52 | 393 | 8244d | 313.6 (283.7-345.8) | 1 429 296 | 12 801 989 | 734.5 (733.3-735.7) |
| Tennessee | 0.61 | 339 | 10 519 | 528.3 (474.3-586.9) | 478 774 | 6 829 174 | 1149.3 (1146.0-1153.0) |
| Utah | 1.75 | 787 | 6478 | 694.2 (647.0-744.0) | 508 494 | 3 205 958 | 906.3 (903.8-908.8) |
| Total | 13.51 | 22 352 | 254 580 | 567.9 (560.5-575.4)e | 10 121 637 | 93 397 354 | 715.0 (714.5-715.5)e |
| Local level | |||||||
| Chicago, Illinois (Cook County) | 1.54 | 682 | 14 433 | 306.8 (284.5-330.5) | 619 536 | 5 150 233 | 781.1 (779.2-783.1) |
| Lexington-Fayette County, Kentucky | 1.43 | 240 | 1162 | 1444.3 (1270.0-1636.0) | 48 953 | 323 152 | 1059.3 (1050.6-1069.2) |
| San Luis Obispo County, California | 1.19 | 71 | 228d | 2616.8 (2059.0-3281.0) | 26 199 | 283 111 | 777.6 (768.3-787.1) |
| Stanislaus County, California | 1.28 | 1098 | 1566 | 5477.7 (5161.0-5809.0) | 71 888 | 550 660 | 1671.0 (1659.0-1683.0) |
| Total | 5.44 | 2091 | 17 389 | 799.2 (765.5-834.0)e | 766 576 | 6 307 156 | 812.5 (810.7-814.3)e |
Abbreviation: PEH, people experiencing homelessness.
Population estimates of PEH are from the 2020 Point-in-Time estimates reported by the US Department of Housing and Urban Development.1
Cases of COVID-19 in the general population were accessed from USAFacts.15
Population estimates for the entire jurisdiction are from the US Census Bureau.16
Pennsylvania and San Luis Obispo County, California, reported only assessing cases among PEH who stayed in homeless shelters. The Point-in-Time count includes only people staying in homeless shelters, not the total number of PEH.
The total incidence rate was calculated using the total number of cases divided by the sum of person-time contributed by all included jurisdictions.
Fifteen of the 18 states or districts collecting data among PEH (83.3%) also reported breakdown of cases by race and ethnicity (Table 3). Of the 23 339 cases among PEH at the state and district level with race and ethnicity data, 504 (2.2%) were in American Indian or Alaska Native PEH, 483 (2.1%) in Asian PEH, 4976 (21.3%) in Black PEH, 311 (1.3%) in Native Hawaiian or Pacific Islander PEH, 8087 (34.7%) in White PEH, and 8978 (38.5%) in PEH who reported other race and ethnicity (multiple races and ethnicities or race and ethnicity not already listed). Information on cases among PEH by sex was provided by 16 of the 18 states or districts (88.9%) (Table 3). Of the 25 421 cases with sex information at the state or district level, 12 012 (47.3%) were identified in females. The full gender breakdown of the sample, including nonbinary, agender, gender fluid, or other identity, is not available.
Table 3. Cases of COVID-19 Among PEH by Race and Ethnicity and Sex at the State, County, City, or Other Local Level From January 2020 to November 2021.
| No. (%)a | ||
|---|---|---|
| States or districts | Local jurisdictions | |
| Race and ethnicity b | ||
| Jurisdictions reporting data | 15/18 (83.3) | 20/25 (80.0) |
| COVID-19 cases | ||
| Total | 23 339 (100) | 15 911 (100) |
| American Indian or Alaska Native | 504 (2.2) | 347 (2.2) |
| Asian | 483 (2.1) | 393 (2.5) |
| Black | 4976 (21.3) | 4783 (30.1) |
| Native Hawaiian or Pacific Islander | 311 (1.3) | 179 (1.1) |
| White | 8087 (34.7) | 6844 (43.0) |
| Otherc | 8978 (38.5) | 3365 (21.1) |
| Sex d | ||
| Jurisdictions reporting data | 16/18 (88.9) | 21/25 (84.0) |
| COVID-19 cases | ||
| Total | 25 421 (100) | 18 830 (100) |
| Femalee | 12 012 (47.3) | 6211 (33.0) |
Abbreviation: PEH, people experiencing homelessness.
Data were limited to only jurisdictions that collected COVID-19 data among PEH.
Jurisdictions were asked what percentage of cases among PEH were in each race and ethnicity group. The number of cases by group was calculated using the percentage multiplied by the total number of cases among PEH reported by that jurisdiction.
Other includes people who identified as more than 1 race and ethnicity or who identifed as a race and ethnicity not otherwise listed.
Jurisdictions were asked what percentage of cases among PEH were in each sex. The number of cases by sex was calculated using the percentage multiplied by the total number of cases among PEH reported by that jurisdiction.
Only the number (percentage) of females was reported. The full gender breakdown for jurisdictions, including nonbinary, agender, gender fluid, or other identity, is not available.
The most common components of the definition of homelessness used by the 18 states and districts collecting COVID-19 data among PEH included person stayed in homeless shelter (13 [72.2%]) and person described themselves as experiencing homelessness (13 [72.2%]) (Figure). Sixteen of the 18 states or districts collecting these data (88.9%) considered a person to be experiencing homelessness at the time of the positive COVID-19 test result, and 2 states or districts (11.1%) considered a person to be experiencing homelessness after different durations (1 for at least 12 months and 1 for at least 24 months).
Figure. Definitions of Homelessness or Housing Status in State and Local Jurisdictions Collecting COVID-19 Data Among People Experiencing Homelessness, January 2020 to November 2021.
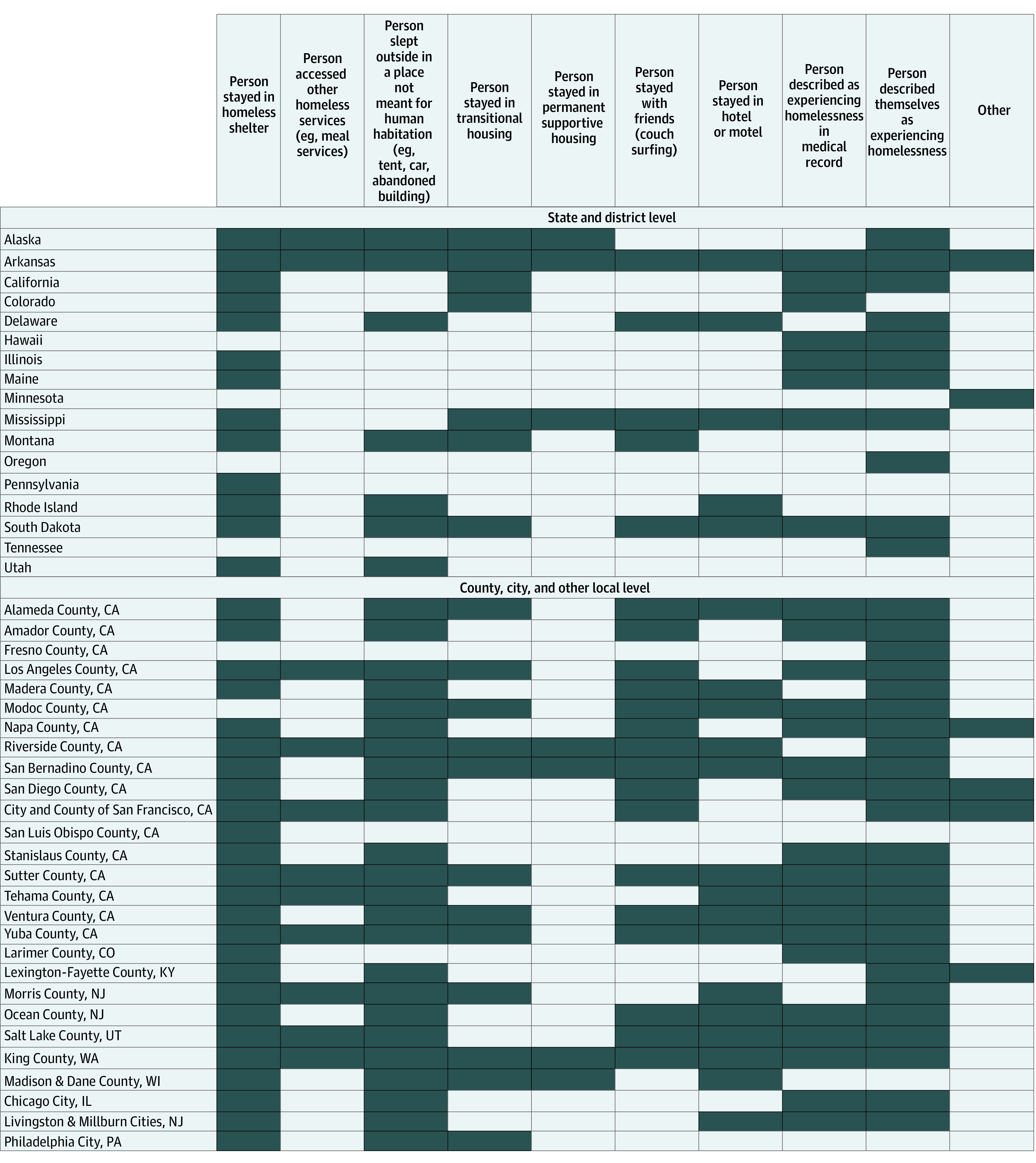
Shaded cells indicate factors that the jurisdiction reported using for homelessness in data collection. The District of Columbia collected data among people experiencing homelessness but did not answer how it defined homelessness in data collection.
County-, City-, and Other Local-Level Results
At the county, city, or other local level, 27 of 39 jurisdictions that completed the survey (69.2%) reported collecting COVID-19 data among PEH. Two pairs of jurisdictions were each combined into a single jurisdiction because they are grouped together in the HUD PIT count, leaving a final sample of 25 local jurisdictions. From January 1, 2020, to November 16, 2021, there were 20 487 cases of COVID-19 reported among PEH at the county, city, or other local level (Table 4). Four localities met the criteria for inclusion in COVID-19 incidence rate calculations (using a definition for homelessness that is consistent with HUD PIT counts) (Table 2). Across these 4 localities, the annual incidence rate of COVID-19 among PEH was 799.2 per 10 000 person-years (95% CI, 765.5-834.0 per 10 000 person-years). The annual incidence rate of COVID-19 in the general population in these same jurisdictions was 812.5 per 10 000 person-years (95% CI, 810.7-814.3 per 10 000 person-years).
Table 4. Cases of COVID-19 Among PEH and in the General Population in Counties, Cities, and Other Localities Collecting COVID-19 Data Among PEH From January 2020 to November 2021.
| Jurisdiction | First date of available data | End date of available data | Duration of data availability, mo | PEH | General population | ||
|---|---|---|---|---|---|---|---|
| COVID-19 cases, No. | Estimated No.a | COVID-19 cases, No.b | Estimated No.c | ||||
| California | |||||||
| Alameda County | Apr 1, 2020 | Sep 30, 2021 | 18.0 | 993 | 5853 | 114 512 | 1 671 329 |
| Amador County | Jun 12, 2020 | Sep 30, 2021 | 15.6 | 20 | 307 | 5094 | 39 752 |
| City and County of San Francisco | Mar 20, 2021 | Sep 30, 2021 | 6.3 | 939 | 13 389 | 15 554 | 881 549 |
| Fresno and Madera Countiesd | Dec 12, 2020 | Sep 30, 2021 | 9.6 | 64 | 2871 | 69 414 | 1 156 428 |
| Los Angeles County | Feb 7, 2020 | Sep 30, 2021 | 19.8 | 9489 | 46 668 | 1 394 823 | 10 039 107 |
| Modoc County | Jul 31, 2020 | Nov 16, 2021 | 15.5 | 1 | 792 | 535 | 8841 |
| Napa County | Jul 17, 2020 | Sep 30, 2021 | 14.4 | 62 | 253 | 11 602 | 137 744 |
| Riverside County | Mar 21, 2020 | Sep 30, 2021 | 18.3 | 725 | 2347 | 346 819 | 2 470 546 |
| San Bernardino County | Mar 11, 2020 | Sep 30, 2021 | 18.6 | 158 | 4427 | 341 118 | 2 180 085 |
| San Diego County | Jan 1, 2020 | Sep 30, 2021 | 21.0 | 1442 | 10 360 | 356 454 | 3 338 330 |
| San Luis Obispo Countye | Jul 22, 2020 | Sep 30, 2021 | 14.3 | 71 | 228e | 26 199 | 283 111 |
| Stanislaus County | Jun 17, 2020 | Sep 30, 2021 | 15.4 | 1098 | 1566 | 71 888 | 550 660 |
| Sutter and Yuba Countiesd | Sep 2, 2020 | Sep 30, 2021 | 12.9 | 82 | 417 | 18 187 | 175 639 |
| Tehama County | Jul 24, 2021 | Sep 23, 2021 | 2.0 | 53 | 273 | 2013 | 65 084 |
| Ventura County | Mar 21, 2020 | Sep 1, 2021 | 17.3 | 120 | 1845 | 94 717 | 846 006 |
| Colorado | |||||||
| Larimer County | Jan 1, 2020 | Sep 30, 2021 | 21.0 | 167 | 1180 | 35 270 | 356 899 |
| Illinois | |||||||
| Chicagof | Mar 14, 2020 | Sep 30, 2021 | 18.5 | 682 | 14 433 | 619 536 | 5 150 233 |
| Kentucky | |||||||
| Lexington-Fayette County | Apr 24, 2020 | Sep 30, 2021 | 17.2 | 240 | 1162 | 48 953 | 323 152 |
| New Jersey | |||||||
| Livingston and Millburng | Apr 30, 2021 | Nov 15, 2021 | 6.5 | 2 | 3429 | 94 174 | 798 975 |
| Morris County | Apr 16, 2020 | Nov 3, 2021 | 18.6 | 50 | 583 | 54 862 | 491 845 |
| Ocean County | Dec 26, 2020 | Sep 30, 2021 | 9.1 | 15 | 621 | 59 328 | 607 186 |
| Pennsylvania | |||||||
| Philadelphiah | Mar 20, 2020 | Sep 29, 2021 | 18.3 | 316 | 10 310 | 174 108 | 1 584 064 |
| Utah | |||||||
| Salt Lake County | Mar 19, 2020 | Nov 15, 2021 | 19.9 | 1144 | 4769 | 204 118 | 1 160 437 |
| Washington | |||||||
| King County | Mar 11, 2020 | Sep 30, 2021 | 18.6 | 2392 | 14 739 | 151 277 | 2 252 782 |
| Wisconsin | |||||||
| Madison and Dane Counties | Apr 4, 2021 | Sep 30, 2021 | 5.9 | 162 | 2204 | 10 723 | 546 695 |
| Total | NA | NA | NA | 20 487 | 145 026 | 4 321 278 | 37 116 479 |
Abbreviations: NA, not applicable; PEH, people experiencing homelessness.
Population estimates of PEH are from the 2020 Point-in-Time estimates reported by the US Department of Housing and Urban Development.1
Cases of COVID-19 in the general population were accessed from USAFacts.15
Population estimates for the entire locality are from the US Census Bureau.16
These counties are reported in the same geographic area for population estimates of PEH; thus, they are grouped and presented together.
San Luis Obispo County, California, reported only assessing cases among PEH who stayed in homeless shelters. The Point-in-Time count includes only people staying in homeless shelters, not the total number of PEH.
The general population case counts and population size for Chicago, Illinois, are for all of Cook County.
The general population case counts and population size for Livingston and Millburn, New Jersey, are for all of Essex County.
The general population case counts and population size for Philadelphia, Pennsylvania, are for all of Philadelphia County.
Twenty of the 25 counties, cities, or other local jurisdictions reporting COVID-19 data among PEH (80.0%) provided race and ethnicity data for cases in this population (Table 3). Of the 15 911 COVID-19 cases among PEH at the county, city, or local level with race and ethnicity data, 347 (2.2%) were in American Indian or Alaska Native PEH, 393 (2.5%) in Asian PEH, 4783 (30.1%) in Black PEH, 179 (1.1%) in Native Hawaiian or Pacific Islander PEH, 6844 (43%) in White PEH, and 3365 (21.1%) in PEH who identified as other race and ethnicity. Twenty-one of the 25 counties, cities, or other local jurisdictions (84.0%) reported the percentage of COVID-19 cases among PEH who were female sex (Table 3). Of the 18 830 cases reported by sex at the local level, 6211 (33.0%) were identified in females. The full gender breakdown of the sample is not available.
The most common components of the definition of homelessness used by the 25 counties, cities, or localities were person stayed in a homeless shelter (25 [100%]), person described themselves as experiencing homelessness (24 [96.0%]), and person slept outside in a place not meant for human habitation (eg, tent, car, abandoned building) (24 [96.0%]) (Figure). Only 1 county, city, or local jurisdiction considered a person to be experiencing homelessness at a duration other than at the time of the positive COVID-19 test, which was experiencing homelessness for at least 1 month.
Data Sources to Assess Housing or Homelessness Status
Most jurisdictions used multiple data sources to verify a person’s homelessness or housing status. The jurisdictions’ most common data collection method was case investigations or interviews conducted in any modality (eg, in person, by electronic text survey, or by telephone). Reviews of medical records were also used as supplemental information before or after a case investigation or interview and to identify hospitalizations. Many jurisdictions reported that they did not have a process for data matching between the Homeless Management Information System and health data systems.
Discussion
This cross-sectional study collected the number of COVID-19 cases among PEH and estimated the incidence rate of COVID-19 in multiple jurisdictions. A total of 26 349 COVID-19 cases at the state and district level and 20 487 cases at the local level were reported among PEH. These findings highlight the need for data collection that uses similar definitions of homelessness across data sources. This study adds to the literature by identifying COVID-19 cases over time across multiple jurisdictions.
Considering the risks for other infectious diseases among PEH and the number of disease outbreaks identified in shelters, we expected that the incidence rates of COVID-19 among PEH would be higher than in the general population. The unexpected results found in this study may be explained by a few factors. One is that there could be underascertainment of homelessness among people with COVID-19. For example, community testing that did not collect information on housing status may have excluded some positive results among PEH, leading to underestimated incidence. In addition, because PEH are less likely to seek medical care in general,19 they may not have visited health care facilities if they had mild symptoms of COVID-19 and thus may not have been tested. One study in 202120 found that only 59% of individuals with COVID-19 were interviewed for case investigation. For jurisdictions relying on case investigation to determine homelessness status, this lack of interviews could create additional bias.20 In addition, data from the present study did not distinguish between sheltered and unsheltered homelessness. Previous data have shown that people experiencing unsheltered homelessness have a lower risk of COVID-19 than do people staying in shelters.21 Of note, the composition of PEH in the US is not representative of the general population. Compared with the general population, PEH are more likely to be male and older, and there is disproportionate representation of people who are Black or African American and American Indian or Alaska Native among PEH.1 The increased burden of COVID-19 among older adults and racial and ethnic minority individuals across the US is another reason our findings were unexpected.22,23
Despite these possible explanations for our findings, given the preventive measures put in place by shelters (eg, physical distancing, ventilation improvements, mask policies, and frequent testing), the results could represent a true balance of risk between PEH and the general population because of these interventions. Of importance, the responding jurisdictions may not be representative of jurisdictions that did not collect data among PEH. Data collection among PEH may indicate high capacity within the health department and could be linked with the ability to support homeless service sites in preventing COVID-19 transmission, or it could indicate that PEH were prioritized for data collection. Considering the data are incomplete and may be biased toward jurisdictions that were well resourced to prevent COVID-19 among PEH, these data should be interpreted with caution.
Limitations
This study has limitations. Because data could not be collected from all jurisdictions, the number of COVID-19 cases reported among PEH are not an estimate of national incidence. In addition, because of variability in the time frame of available data among PEH, definitions of homelessness, duration of homelessness to be considered homeless, and data sources used to verify housing or homelessness status, COVID-19 estimates could not be compared across jurisdictions. Furthermore, jurisdictions that use more inclusive definitions of homelessness may have different COVID-19 incidence rates than jurisdictions that use narrower definitions of homelessness, contributing to incomparable and possibly skewed estimates. We were not able to explore differences or changes in COVID-19 incidence among PEH during different seasons and in different climates, but it is possible that warmer climates and seasons may be associated with fewer cases of COVID-19 if PEH spend more time outdoors. At the county, city, or local level, COVID-19 incidence rates among PEH may also be affected owing to the reporting of population estimates of PEH from HUD. The number of PEH is reported by HUD at the continuum-of-care level, which does not always directly align with a specific city or county. In rural areas, multiple counties may be grouped together for the population estimate of PEH. Thus, these counties were combined during analysis, but this may have contributed to inaccuracies in incidence rates. There is also a large representation of local jurisdictions from California, and the study team could not control which state-level jurisdictions did or did not share the survey with their local health departments, both of which may bias the local-level results. The few localities used in the incidence calculations included 2 California counties with high rates of COVID-19, which may further bias the local estimates. Of note, there were discrepancies in the number of cases among PEH reported by state and local jurisdictions. For example, Salt Lake City, Utah, reported more cases among PEH than Utah reported for the state overall. This could be explained by differences in definitions for homelessness between Salt Lake City and Utah (Figure) because Salt Lake City had a broader definition of homelessness in data collection. In addition, there may have been variations in testing among PEH across jurisdictions. Some jurisdictional health departments facilitated testing only among people in shelters, and others may have also conducted outreach testing events to people experiencing unsheltered homelessness.
Conclusions
The results of this cross-sectional study include COVID-19 case counts among PEH in multiple jurisdictions, but a national-level estimate of COVID-19 incidence among PEH and the extent of underestimation or overestimation in these results remains unknown. Data on infection incidence rates during public health emergencies could be used to inform policy decisions and resource allocation to reduce the burden of infectious diseases among PEH. Possible opportunities for public health practice include integration of homeless service utilization data systems, such as the Homeless Management Information System, into health data systems.24 Integration of these data systems may alleviate burden on health departments in collecting housing or homelessness information during case investigations or interviews and would further support ongoing data modernization initiatives. In addition, health departments could consider creating public-facing dashboards or regularly posted reports with these data, which would allow for improved data sharing and informed decision-making at all levels of public health responses. Opportunities exist for incorporating housing and homelessness status in infectious disease reporting to inform public health actions.
References
- 1.US Department of Housing and Urban Development . 2020 AHAR: Part 1—PIT estimates of homelessness in the US. Published March 2021. Accessed October 18, 2021. https://www.huduser.gov/portal/datasets/ahar/2020-ahar-part-1-pit-estimates-of-homelessness-in-the-us.html
- 2.Baggett TP, Liauw SS, Hwang SW. Cardiovascular disease and homelessness. J Am Coll Cardiol. 2018;71(22):2585-2597. doi: 10.1016/j.jacc.2018.02.077 [DOI] [PubMed] [Google Scholar]
- 3.Bartels SJ, Baggett TP, Freudenreich O, Bird BL. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatr Serv. 2020;71(10):1078-1081. doi: 10.1176/appi.ps.202000244 [DOI] [PubMed] [Google Scholar]
- 4.Kuhn R, Richards J, Roth S, Clair K. Homelessness and public health in Los Angeles. March 31, 2020. Accessed October 28, 2021. https://escholarship.org/uc/item/2gn3x56s
- 5.Snyder LD, Eisner MD. Obstructive lung disease among the urban homeless. Chest. 2004;125(5):1719-1725. doi: 10.1378/chest.125.5.1719 [DOI] [PubMed] [Google Scholar]
- 6.Ghinai I, Davis ES, Mayer S, et al. Risk factors for severe acute respiratory syndrome coronavirus 2 infection in homeless shelters in Chicago, Illinois—March-May, 2020. Open Forum Infect Dis. 2020;7(11):ofaa477. doi: 10.1093/ofid/ofaa477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers JH, Link AC, McCulloch D, et al. ; Seattle Flu Study Investigators . Characteristics of COVID-19 in homeless shelters: a community-based surveillance study. Ann Intern Med. 2021;174(1):42-49. doi: 10.7326/M20-3799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477. doi: 10.3201/eid2607.200282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020;323(21):2191-2192. doi: 10.1001/jama.2020.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imbert E, Kinley PM, Scarborough A, et al. Coronavirus disease 2019 outbreak in a San Francisco homeless shelter. Clin Infect Dis. 2021;73(2):324-327. doi: 10.1093/cid/ciaa1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohsenpour A, Bozorgmehr K, Rohleder S, Stratil J, Costa D. SARS-Cov-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: systematic review and meta-analysis. EClinicalMedicine. 2021;38:101032. doi: 10.1016/j.eclinm.2021.101032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mosites E, Parker EM, Clarke KEN, et al. ; COVID-19 Homelessness Team . Assessment of SARS-CoV-2 infection prevalence in homeless shelters—four US cities, March 27–April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):521-522. doi: 10.15585/mmwr.mm6917e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tobolowsky FA, Gonzales E, Self JL, et al. COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):523-526. doi: 10.15585/mmwr.mm6917e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mosites E, Harrison B, Montgomery MP, et al. Public health lessons learned in responding to COVID-19 among people experiencing homelessness in the United States. Public Health Rep. Published online April 29, 2022. doi: 10.1177/00333549221083643 [DOI] [PMC free article] [PubMed]
- 15.USAFacts . US COVID-19 cases and deaths by state. Accessed October 28, 2021. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map
- 16.US Census Bureau . County population totals: 2010-2019. Accessed October 18, 2021. https://www.census.gov/data/datasets/time-series/demo/popest/2010s-counties-total.html
- 17.US Department of Housing and Urban Development Exchange. HDX FAQs: FAQ ID 1818. Published December 2014. Accessed October 28, 2021. https://www.hudexchange.info/faqs/reporting-systems/homelessness-data-exchange-hdx/pit/pit-general/for-purposes-of-the-point-in-time-pit-count-who-does-hud-consider/#:~:text=HUD's%20PIT%20count%20is%20limited,the%20time%20of%20the%20count
- 18.Dean AG, Sullivan KM, Soe MM. OpenEpi: open source epidemiologic statistics for public health. Updated April 6, 2013. Accessed June 28, 2022. http://www.OpenEpi.com
- 19.Moore G, Gerdtz M, Manias E, Hepworth G, Dent A. Socio-demographic and clinical characteristics of re-presentation to an Australian inner-city emergency department: implications for service delivery. BMC Public Health. 2007;7:320. doi: 10.1186/1471-2458-7-320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lash RR, Moonan PK, Byers BL, et al. ; COVID-19 Contact Tracing Assessment Team . COVID-19 case investigation and contact tracing in the US, 2020. JAMA Netw Open. 2021;4(6):e2115850. doi: 10.1001/jamanetworkopen.2021.15850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon JC, Montgomery MP, Buff AM, et al. Coronavirus disease 2019 (COVID-19) prevalences among people experiencing homelessness and homelessness service staff during early community transmission in Atlanta, Georgia, April-May 2020. Clin Infect Dis. 2021;73(9):e2978-e2984. doi: 10.1093/cid/ciaa1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu HE, Ashe EM, Silverstein M, et al. Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an urban safety-net medical center—Boston, Massachusetts, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):864-869. doi: 10.15585/mmwr.mm6927a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess deaths associated with COVID-19, by age and race and ethnicity—United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1522-1527. doi: 10.15585/mmwr.mm6942e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Department of Housing and Urban Development Exchange . Homeless management information system. Accessed October 18, 2021. https://www.hudexchange.info/programs/hmis/
- 25.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]


