Key Points
Question
What is the 30-day acute risk of venous thromboembolism (VTE) among ambulatory patients with COVID-19, and what are the clinical and genetic risk factors predisposing them to developing post–COVID-19 VTE?
Findings
In this retrospective cohort study of 18 818 outpatients with COVID-19 and 93 179 propensity score–matched noninfected participants, a higher VTE incidence was observed in the former (hazard ratio, 21.42); however, this risk was considerably attenuated among the fully vaccinated, after breakthrough infection. Older age, male sex, obesity, no vaccination or partial vaccination, and inherited thrombophilia were independent risk factors for COVID-19–associated VTE.
Meaning
The results of this study suggest that ambulatory patients with COVID-19, either vaccinated or not, present a clinically relevant increased risk of incident VTE during the acute phase, with the risk pronounced by factors of older age, male sex, obesity, incomplete vaccination, and factor V Leiden thrombophilia.
Abstract
Importance
The risk of venous thromboembolism (VTE) in ambulatory COVID-19 is controversial. In addition, the association of vaccination with COVID-19–related VTE and relevant clinical and genetic risk factors remain to be elucidated.
Objective
To quantify the association between ambulatory COVID-19 and short-term risk of VTE, study the potential protective role of vaccination, and investigate clinical and genetic risk factors for post–COVID-19 VTE.
Design, Setting, and Participants
This population-based cohort study of patients with COVID-19 from UK Biobank included participants with SARS-CoV-2 infection that was confirmed by a positive polymerase chain test reaction result between March 1, 2020, and September 3, 2021, who were then propensity score matched to COVID-19–naive people during the same period. Participants with a history of VTE who used antithrombotic drugs (1 year before index dates) or tested positive in hospital were excluded.
Exposures
First infection with SARS-CoV-2, age, sex, ethnicity, socioeconomic status, obesity, vaccination status, and inherited thrombophilia.
Main Outcomes and Measures
The primary outcome was a composite VTE, including deep vein thrombosis or pulmonary embolism, which occurred 30 days after the infection. Hazard ratios (HRs) with 95% CIs were calculated using cause-specific Cox models.
Results
In 18 818 outpatients with COVID-19 (10 580 women [56.2%]; mean [SD] age, 64.3 [8.0] years) and 93 179 matched uninfected participants (52 177 women [56.0%]; mean [SD] age, 64.3 [7.9] years), the infection was associated with an increased risk of VTE in 30 days (incidence rate of 50.99 and 2.37 per 1000 person-years for infected and uninfected people, respectively; HR, 21.42; 95% CI, 12.63-36.31). However, risk was substantially attenuated among the fully vaccinated (HR, 5.95; 95% CI, 1.82-19.5; interaction P = .02). In patients with COVID-19, older age, male sex, and obesity were independently associated with higher risk, with adjusted HRs of 1.87 (95% CI, 1.50-2.33) per 10 years, 1.69 (95% CI, 1.30-2.19), and 1.83 (95% CI, 1.28-2.61), respectively. Further, inherited thrombophilia was associated with an HR of 2.05 (95% CI, 1.15-3.66) for post–COVID-19 VTE.
Conclusions and Relevance
In this population-based cohort study of patients with COVID-19, ambulatory COVID-19 was associated with a substantially increased risk of incident VTE, but this risk was greatly reduced in fully vaccinated people with breakthrough infection. Older age, male sex, and obesity were clinical risk factors for post–COVID-19 VTE; factor V Leiden thrombophilia was additionally associated with double the risk, comparable with the risk of 10-year aging. These findings may reinforce the need for vaccination, inform VTE risk stratification, and call for targeted VTE prophylaxis strategies for unvaccinated outpatients with COVID-19.
This cohort study examines the association between ambulatory COVID-19 and risk of venous thromboembolism.
Introduction
Numerous hospital-based studies and case series have demonstrated a high risk of venous thromboembolism (VTE) in patients with severe COVID-19. A recent meta-analysis reported a pooled VTE rate of 14.7% and 23.2% among those admitted to the hospital and intensive care units, respectively.1 Additionally, emerging randomized clinical trials2,3,4 have shown the benefit-risk of anticoagulation for patients with COVID-19 at different stages of the disease, and clinical societies have recommended initiating routine antithrombotic therapy during hospital admission.5
In contrast, fewer clinical interventions have been implemented to prevent VTE among ambulatory patients with SARS-CoV-2 infection, partially because of conflicting findings on the association between the infection and VTE occurrence, with cohort studies showing no elevated risk6 but self-controlled case series studies consistently showing a substantial increase of short-term risk.7,8,9 Also, mixed evidence of benefit from oral anticoagulation complicated clinical decisions for ambulatory COVID-19.10 Given the ongoing global rollout of vaccines, relaxation of public health restrictions, and the widespread highly transmissible Omicron variant, the absolute number of milder COVID-19 cases treated in ambulatory settings continues to rise worldwide.11,12 These collectively suggest that prophylaxis, including timing and dosing regimens, requires further refinement, particularly in the outpatient setting.2,3,4,13,14 Moreover,15 a lack of insight into the association of clinical, socioeconomic, and genetic risk factors with infection-related VTE persists. This study aimed to (1) quantify the magnitude of short-term VTE risk associated with SARS-CoV-2 infection identified in ambulatory settings and (2) investigate the clinical and genetic risk factors for VTE after SARS-CoV-2 infection.
Methods
We included UK Biobank (UKBB) participants from England who were alive on March 1, 2020. All participants provided written informed consent at the UKBB cohort recruitment. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines and received ethical approval from the UKBB ethics advisory committee.
Data Sources and Study Cohorts
We obtained data from UK Biobank comprising multiple linked sources, including baseline surveys conducted between 2006 and 2010, individual genetic data, primary care electronic medical records, hospital inpatient data from Hospital Episode Statistics, diagnostic COVID-19 test data from the Public Health England's Second Generation Surveillance System,16 and death records from the national death registry (Office of National Statistics).
We curated an infected cohort by enrolling individuals with positive polymerase chain reaction SARS-CoV-2 test results that were confirmed between March 1, 2020, and September 30, 2021. Participants who were never tested or only had negative test results were classified into the noninfected cohort. The index date was the date of the first positive specimen sample for the infected cohort. A random date that followed the same calendar period distribution of the index date as the infected individuals was assigned to the noninfected individuals. Participants with a history of VTE or who used oral anticoagulants and antiplatelet drugs 1 year before the index dates were excluded. Additionally, we excluded those in the infected cohort who were already hospitalized at the time of testing positive for COVID-19. Any information after the index date was not used for the cohort exclusion (eFigure 1 in the Supplement).
Inherited Thrombophilia
Information on genotyping and imputation procedures in UK Biobank has been detailed in previous studies.17 Briefly, genome-wide single-nucleotide polymorphisms (SNPs) were genotyped using 2 closely related purpose-designed arrays (the UK BiLEVE Axiom array and UK Biobank Axiom array). We defined inherited thrombophilia carriers as having any of 2 risk SNP variants in factor V Leiden (rs6025) or prothrombin G20210A (rs1799963). We also defined a positive genetic control exposure by calculating a 297-SNPs polygenic risk score (PRS) for VTE that did not include these 2 variants18 (eMethods in the Supplement).
Covariates
We prespecified a list of covariates for adjustment based on clinicians’ knowledge, including demographic characteristics (age, sex, self-reported race and ethnicity grouped into other racial and ethnic categories that included Asian or Asian British, Black or Black British, Chinese, and unspecific/unknown ethnicity or White, given that approximately 90% of the UKBB participants were White), socioeconomic status measured by the Index of Multiple Deprivation (a continuous summary deprivation measurement used in England containing 7 aspects in crime, education, employment, health, housing, income, and living environment),19 body mass index (BMI), medications for chronic illness prescribed within 1 year before the index date, and trauma-related diagnosis and all comorbidities included in the Charlson Comorbidity Index (Table 1).20 The orthopedic surge, number of hospital admissions during the past year (proxy of health care utilization), and vaccination status (not or partially vaccinated vs fully vaccinated) were also studied.
Table 1. Baseline Characteristics of Participants Stratified by the SARS-CoV-2 Infection Status Before and After Matchinga.
| Characteristic | Unmatched cohorts | Matched cohorts | ||||
|---|---|---|---|---|---|---|
| Uninfected | Infected | SMDb | Uninfected | Infected | SMDb | |
| No. | 317 943 | 18 847 | NA | 93 179 | 18 818 | NA |
| Age, mean (SD) | 67.96 (8.03) | 64.32 (8.03) | 0.453 | 64.31 (7.92) | 64.33 (8.03) | 0.002 |
| Sex, No. (%) | ||||||
| Female | 185 897 (58.5) | 10 600 (56.2) | 0.045 | 52 177 (56.0) | 10 580 (56.2) | 0.005 |
| Male | 132 046 (41.5) | 8247 (43.8) | 0.045 | 41 002 (44.0) | 8238 (43.8) | 0.005 |
| Race and ethnicity, No. (%) | ||||||
| White | 297 595 (93.6) | 16 590 (88.0) | 0.194 | 83 261 (89.4) | 16 588 (88.1) | 0.038 |
| Multiracial/unknownc | 20 348 (6.4) | 2257 (12.0) | 0.194 | 9918 (10.6) | 2230 (11.9) | 0.038 |
| Index of multiple deprivation, mean (SD) | 17.03 (13.51) | 19.87 (14.68) | 0.201 | 19.41 (14.92) | 19.83 (14.65) | 0.028 |
| Body mass index, mean (SD)d | 27.04 (4.61) | 27.65 (4.83) | 0.130 | 27.58 (4.99) | 27.64 (4.81) | 0.014 |
| Vaccination status, No. (%) | ||||||
| Not or partially vaccinated | 195 574 (61.5) | 11 156 (59.2) | 0.047 | 55 183 (59.2) | 11 135 (59.2) | 0.001 |
| Fully vaccinated | 122 369 (38.5) | 7691 (40.8) | 0.047 | 37 996 (40.8) | 7683 (40.8) | 0.001 |
| Recent medications, No. (%) | ||||||
| Lipid-lowering drugs | 87 164 (27.4) | 4634 (24.6) | 0.064 | 22 507 (24.2) | 4627 (24.6) | 0.010 |
| RAS inhibitors | 57 832 (18.2) | 3296 (17.5) | 0.018 | 16 035 (17.2) | 3292 (17.5) | 0.008 |
| Other antihypertensives | 25 961 (8.2) | 1367 (7.3) | 0.034 | 6750 (7.2) | 1363 (7.2) | 0.001 |
| Proton pump inhibitors | 78 080 (24.6) | 5263 (27.9) | 0.077 | 25 371 (27.2) | 5246 (27.9) | 0.015 |
| Diabetes medicines | 16 108 (5.1) | 1112 (5.9) | 0.037 | 5238 (5.6) | 1106 (5.9) | 0.011 |
| Antidepressants | 43 310 (13.6) | 3188 (16.9) | 0.092 | 15 483 (16.6) | 3178 (16.9) | 0.007 |
| Systemic glucocorticoids | 14 237 (4.5) | 972 (5.2) | 0.032 | 4623 (5.0) | 969 (5.1) | 0.009 |
| Immunosuppressants | 3541 (1.1) | 203 (1.1) | 0.004 | 938 (1.0) | 203 (1.1) | 0.007 |
| Antineoplastic agents | 178 (0.1) | 14 (0.1) | 0.007 | 66 (0.1) | 14 (0.1) | 0.001 |
| Recent orthopedic surgery, No. (%) | 6018 (1.9) | 371 (2.0) | 0.006 | 1844 (2.0) | 371 (2.0) | 0.001 |
| Recent hospital admissions, mean (SD) | 0.29 (1.48) | 0.31 (1.95) | 0.014 | 0.30 (1.61) | 0.31 (1.95) | 0.011 |
| Coexisting conditions, No. (%) | ||||||
| Fracture | 57 539 (18.1) | 3415 (18.1) | 0.001 | 16 850 (18.1) | 3414 (18.1) | 0.002 |
| Fall | 24 063 (7.6) | 1381 (7.3) | 0.009 | 6721 (7.2) | 1374 (7.3) | 0.003 |
| Cancer | 31 271 (9.8) | 1476 (7.8) | 0.071 | 7175 (7.7) | 1474 (7.8) | 0.005 |
| Malignant cancer | 1119 (0.4) | 63 (0.3) | 0.003 | 297 (0.3) | 63 (0.3) | 0.003 |
| Diabetes (uncomplicated) | 23 250 (7.3) | 1496 (7.9) | 0.024 | 7203 (7.7) | 1490 (7.9) | 0.007 |
| Diabetes (end-organ damage) | 6714 (2.1) | 415 (2.2) | 0.006 | 2004 (2.2) | 415 (2.2) | 0.004 |
| Congestive heart failure | 1666 (0.5) | 89 (0.5) | 0.007 | 445 (0.5) | 89 (0.5) | 0.001 |
| Myocardial infarction | 658 (0.2) | 34 (0.2) | 0.006 | 161 (0.2) | 34 (0.2) | 0.002 |
| Cerebrovascular disease | 2500 (0.8) | 138 (0.7) | 0.006 | 655 (0.7) | 138 (0.7) | 0.004 |
| Peripheral vascular disease | 1379 (0.4) | 49 (0.3) | 0.030 | 213 (0.2) | 49 (0.3) | 0.006 |
| Liver disease (mild) | 1506 (0.5) | 81 (0.4) | 0.007 | 401 (0.4) | 80 (0.4) | 0.001 |
| Liver disease (moderate to severe) | 607 (0.2) | 46 (0.2) | 0.011 | 231 (0.2) | 46 (0.2) | 0.001 |
| COPD | 49 834 (15.7) | 3309 (17.6) | 0.051 | 16 182 (17.4) | 3302 (17.5) | 0.005 |
| Chronic kidney disease | 12 847 (4.0) | 691 (3.7) | 0.019 | 3367 (3.6) | 690 (3.7) | 0.003 |
| Peptic ulcer | 6256 (2.0) | 419 (2.2) | 0.018 | 2039 (2.2) | 414 (2.2) | 0.001 |
| Rheumatoid arthritis | 8363 (2.6) | 511 (2.7) | 0.005 | 2412 (2.6) | 510 (2.7) | 0.008 |
| Dementia | 1902 (0.6) | 205 (1.1) | 0.054 | 998 (1.1) | 202 (1.1) | 0.001 |
| Hemiplegia | 242 (0.1) | 15 (0.1) | 0.001 | 83 (0.1) | 15 (0.1) | 0.003 |
| AIDS | 309 (0.1) | 17 (0.1) | 0.002 | 76 (0.1) | 17 (0.1) | 0.003 |
Abbreviations: AIDS, acquired immune deficiency syndrome; COPD, chronic obstructive pulmonary disease; NA, not applicable; SMD, standardized mean difference.
The look-back window of covariates for recent medications, orthopedic surgery, and hospital admissions was past 1 year before the index date and for coexisting conditions was any time before the index date. Age, index of multiple deprivation, body mass index, and recent hospital admissions were included as the continuous and other covariates as binary in logistic regression model for the generation of propensity score.
Value ≤0.10 is considered good balance.
Includes Asian or Asian British, Black or Black British, Chinese, and unspecific/unknown ethnicity.
Calculated as weight in kilograms divided by height in meters squared.
Outcomes
Incident VTE, comprising either deep vein thrombosis or pulmonary embolism, was identified using International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes based on hospital records. Eligible participants were followed up for up to 30 days after the index date, given that VTE occurring after 30 days was much less likely to be associated with SARS-CoV-2 infection.
Statistical Analyses
We used propensity score (PS) matching to minimize confounding in studying the association between SARS-CoV-2 infection and VTE. We fitted multivariable logistic regression models to estimate PS as the probability of infection based on all predefined covariates. We then matched infected with noninfected individuals with a ratio of 1:5 based on PS values, with a caliper width of up to 0.2 standard deviations of the logit of the PS, with exact matching on index dates.21,22 We assessed the covariate balance between the cohorts before and after matching using absolute standardized mean differences (SMDs) and specified an SMD greater than 0.1 as relevant imbalances.23 Cause-specific Cox survival models were applied to estimate the hazard ratio (HR) for VTE according to exposure, for which death was considered a competing risk.24 The overall HR and that in subgroups by prior vaccination status were provided. The multiplicative interaction effect between the infection and vaccination status was tested statistically on the probability scale.
To study clinical risk factors, we fitted multivariable Cox models of 30-day VTE in the ambulatory COVID-19 cohort, including age, sex, race and ethnicity, socioeconomic status, obesity (BMI less than vs equal or more than 30), vaccination status, cancer, fall, fracture, and the number of comorbidities. For the analysis of the association of inherited thrombophilia with post–COVID-19 VTE, we adjusted Cox models for age, sex, and genetic ancestry (quantified by the first 3 principal components), assuming that genetic variants were independent of all other baseline characteristics.
We performed a sensitivity analysis repeating the modeling of clinical risk factors with VTE in the uninfected cohort, in which no association was expected between vaccination and COVID-19–unrelated VTE. We also introduced a positive exposure control (PRS for VTE) and a negative outcome (arterial thromboembolism) experiment to detect residual confounding and potential unresolved bias for the exposure of inherited thrombophilia.25
All statistical tests were 2-sided, for which a P = .05 or a 95% CI that did not cross 1 were considered statistically significant for the primary analyses. All analyses and data visualizations were conducted using R, version 4.1.2 (R Foundation). Genetic data management and quality controls were performed using Plink 1.9.26
Results
Baseline Characteristics
Out of 407 311 UKBB participants, 26 210 (6.4%) had SARS-CoV-2 infection between March 1, 2020, and September 30, 2021. After applying exclusion criteria, 21 724 of 26 210 (83.0%) infected and 317 943 of 380 398 (83.5%) noninfected individuals were eligible for analyses (eFigure 1 in the Supplement). For all infections, 2877 (13.2%) and 18 847 (86.8%) were tested in hospital and outpatient settings, respectively. Only the latter were included for subsequent analyses.
Baseline characteristics by infection status and incident VTE outcome are summarized in Table 1 and eTable 1 in the Supplement. Before matching, ambulatory participants with COVID-19 were younger than those without infection (mean [SD] age, 64.32 [8.03] vs 67.96 [8.03]), more likely male (8247 [43.8%] vs 132 046 [41.5%]), of a racial and ethnic minority group (2257 [12.0%] vs 20 348 [6.4%]), experienced greater socioeconomic deprivation, and had obesity. After 1:5 PS matching, 18 818 patients with COVID-19 were matched to 93 179 uninfected counterparts (98.6% of COVID-19 with 5 matches). All covariates became balanced (eg, mean [SD] age of 64.31 [7.92] years and 44.0% male in the COVID-19 group vs mean [SD] age of 64.33 [8.03] years and 43.8% male in controls). In addition, index dates and calendar periods were accurately aligned between the cohorts, as depicted in eFigure 2 in the Supplement.
Association of SARS-CoV-2 Infection With Incident VTE
Figure 1 depicts the cumulative incidence of VTE according to infection status, showing an early separation of the matched cohorts, with continued divergence over time. A total of 73 and 17 VTE events were seen within 30 days among the ambulatory patients with COVID-19 and matched uninfected individuals, which corresponded to incidence rates of 50.99 and 2.37 per 1000 person-years, respectively. Survival analyses (Table 2) suggested that the infection was associated with a substantial increase in VTE risk (HR, 21.42; 95% CI, 12.63-36.31). The observed risk was more pronounced in the unvaccinated patients (HR, 27.94; 95% CI, 15.11-51.65) and significantly mitigated in those fully vaccinated (HR, 5.95; 95% CI, 1.82-19.51; interaction P = .02).
Figure 1. Cumulative Incidence Curves of Venous Thromboembolism Within 30 Days Overall and in Subgroups by Vaccination Status.
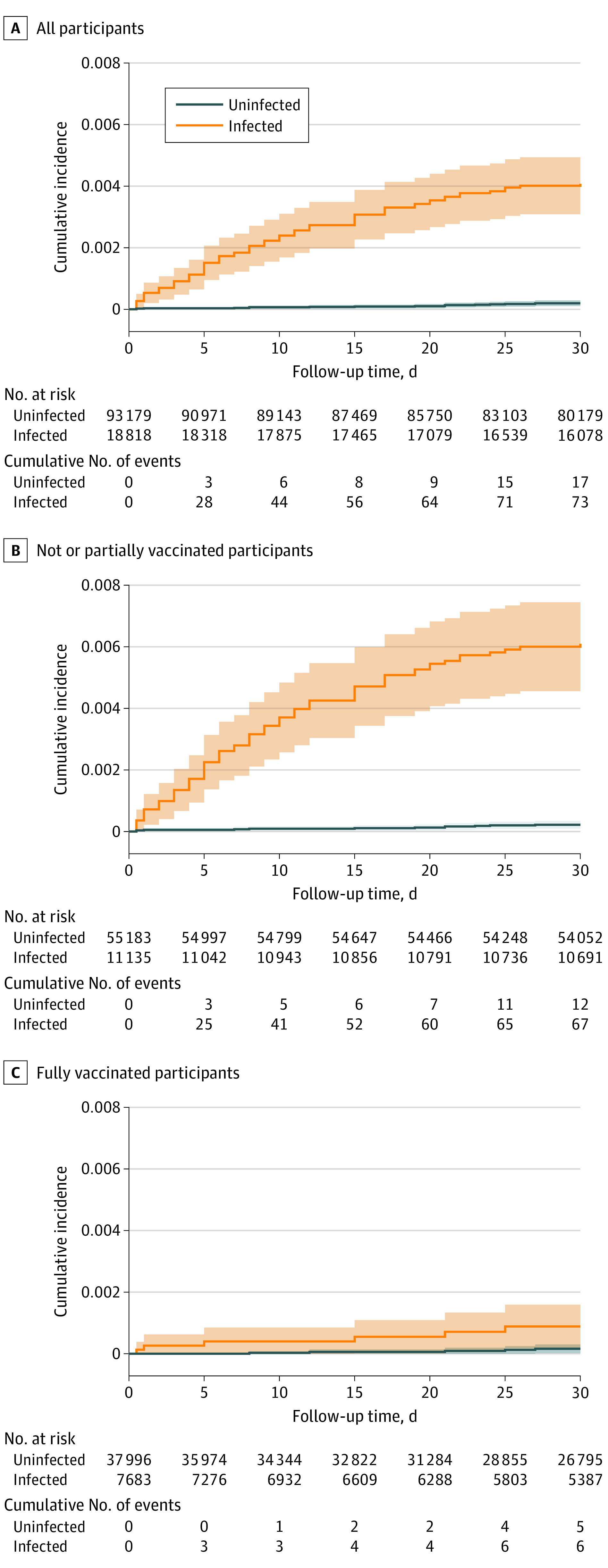
Table 2. Associations Between Ambulatory COVID-19 and Venous Thromboembolism Overall and in Subgroups by Vaccination Status.
| Characteristic | Uninfected | Infected | Hazard ratio (95% CI) | P value for interaction | ||||
|---|---|---|---|---|---|---|---|---|
| No. of people | No. of events | Incidence per 1000 patient-y | No. of people | No. of events | Incidence per 1000 patient-y | |||
| Overall | 93 179 | 17 | 2.37 | 18 818 | 73 | 50.99 | 21.42 (12.63-36.31) | NA |
| Subgroups | ||||||||
| Not or partially vaccinateda | 55 183 | 12 | 2.67 | 11 135 | 67 | 74.96 | 27.94 (15.11-51.65) | .02 |
| Fully vaccinated | 37 996 | 5 | 1.87 | 7683 | 6 | 11.15 | 5.95 (1.82-19.51) | |
Abbreviation: NA, not applicable.
A total of 92.2% of people were not vaccinated, and 7.8% were partially vaccinated.
Clinical Determinants of Post–COVID-19 VTE
The associations between sociodemographic and clinical factors (including vaccination status) and the risk of post–COVID-19 VTE are shown in Figure 2. Older participants had a higher risk, with an approximate doubling of risk per each 10-year increase in age (adjusted HR, 1.87; 95% CI, 1.50-2.33). Men were at higher risk than women (adjusted HR, 1.69; 95% CI, 1.30-2.19), and people with obesity at a higher risk than non-obese (adjusted HR, 1.83; 95% CI, 1.28-2.61). These associations were similarly seen for COVID-19–unrelated VTE in direction and magnitude (eTable 2 in the Supplement).
Figure 2. Hazard Ratio of Clinical Risk Factors for Venous Thromboembolism (VTE) Among Patients With COVID-19.
Covariates included in the single multivariable Cox regression model were age, sex, race and ethnicity, socioeconomic status, obesity, vaccination status, cancer, fall, fracture, and number of comorbidities. The estimate of hazard ratios for other VTE was calculated among the uninfected group, which was predefined as a negative control outcome analysis. BMI indicates body mass index (calculated as weight in kilograms divided by height in meters squared); IMD, index of multiple deprivation.
Additionally, no or partial vaccination was associated with evident higher risk of COVID-19–related VTE (adjusted HR, 5.50; 95% CI, 3.00-10.08). A sensitivity analysis demonstrated no association between vaccination status and COVID-19–unrelated VTE among the uninfected participants, with an HR equal to 1.07 (95% CI, 0.80-1.42) (Figure 2; eTable 2 in the Supplement).
Inherited Thrombophilia and Post–COVID-19 VTE
Among 21 055 infected participants with complete genetic data, 1287 (6.11%) had inherited thrombophilia, with 909 (4.32%) and 392 (1.86%) carrying risk variant/s of factor V Leiden and prothrombin G20210A, respectively (Table 3). The frequency of these genetic variations in the infected cohort was like that in the overall UKBB cohort and consistent with reports from previous literature (eTable 3 in the Supplement). No differences in any of the measured covariates (except for race and ethnicity), including sociodemographic characteristics, medications, or comorbidities, were observed when comparing those with vs without inherited thrombophilia (eTable 4 in the Supplement).
Table 3. Association of Inherited Thrombophilia With Venous and Arterial Thromboembolism Among Patients With COVID-19a.
| Exposure | Primary outcome, venous thromboembolism | Negative outcome, arterial thromboembolism | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||
| Inherited thrombophiliab | 1.82 (1.02-3.23) | 2.05 (1.15-3.66) | .01 | 0.94 (0.51-1.73) | 0.98 (0.53-1.80) | .95 |
| Factor V Leiden | 1.97 (1.03-3.76) | 2.17 (1.13-4.15) | .02 | 0.97 (0.48-1.98) | 0.99 (0.49-2.01) | .97 |
| Prothrombin G20210Ac | 1.31 (0.42-4.11) | 1.52 (0.48-4.79) | .45 | 0.84 (0.27-2.62) | 0.91 (0.29-2.84) | .86 |
| Positive control | ||||||
| Continuous PRSd | 1.29 (1.08-1.54) | 1.34 (1.11-1.60) | <.001 | NC | NC | NC |
| Categorical PRSe | 1.39 (0.73-2.66) | 1.54 (0.80-2.95) | .20 | NC | NC | NC |
Abbreviations: HR, hazard ratio; NC, not calculated; PRS, polygenic risk score.
To set an informative positive exposure arm, we classified people into low and high polygenic risk groups according to their PRS value with a cutoff point at the 94th percentile. This threshold was chosen based on the proportion of inherited thrombophilia in the general UK Biobank population (approximately 6%).
Any risk variations in factor V Leiden and prothrombin G20210A.
Minimum detectable incidence rate ratio associated with the exposure of prothrombin G20210A is 3.58 less than the current sample size.
Per 1-SD increase of PRS.
Top 6% of PRS vs the lower.
Participants with inherited thrombophilia had a higher risk of VTE following SARS-CoV-2 infection than those without (adjusted HR, 2.05; 95% CI, 1.15-3.66). For each risk variant, the adjusted HR was 2.17 (95% CI, 1.13-4.15) for factor V Leiden carriers and 1.52 (95% CI, 0.48-4.79) for prothrombin G20210A carriers. Also, individuals with higher PRS values had greater VTE risk (adjusted HR per 1-SD increase of PRS, 1.33; 95% CI, 1.11-1.59) (Table 3). As expected, no associations were observed between inherited thrombophilia and the negative control outcome of arterial thromboembolism, with adjusted HRs ranging from 0.91 (95% CI, 0.29-2.84) to 0.99 (95% CI, 0.49-2.01).
Discussion
In this community-based cohort study of UKBB participants, including 26 210 with polymerase chain reaction–confirmed ambulatory COVID-19 cases and 380 398 matched contemporary noninfected controls, we found that SARS-CoV-2 infection was associated with an increased VTE risk within 30 days of a positive test (HR, 21.42). However, this risk was largely attenuated in the fully vaccinated participants who then experienced a breakthrough infection (HR, 5.95). Known clinical risk factors for VTE, including older age, male sex, and obesity, applied to post–COVID-19 VTE. Also, compared with the full vaccination, no or partial vaccination was associated with an increased risk of post–COVID-19 VTE. As expected, vaccination was not associated with VTE risk in the uninfected peers. Finally, factor V Leiden thrombophilia carriers had an additional double risk of post–COVID-19 VTE compared with noncarriers, which was equivalent to the excess risk associated with an increase of 10 years of age.
The study finding of a substantially higher incidence of VTE in ambulatory COVID-19 disagreed with a previous meta-analysis of 7 heterogeneous small COVID-19 cohorts, which had suggested that mild COVID-19 was not a risk factor for VTE, with a combined overall relative risk equal to 1.18 (95% CI, 0.79-1.77).6 However, the present study’s data align more with extensive self-controlled case series studies7,8,9 that better accounted for within-person confounding and consistently showed orders of magnitude increases in VTE risk after the infection (eg, more than 46-fold and 7-fold higher risk at 7-14 days for pulmonary embolism and deep vein thrombosis, respectively).7 Most recently, a large network cohort study in 5 European countries profiled that 90-day incidence of VTE ranged from 0.2% to 0.8% among any patients with COVID-19 and up to 4.5% for those hospitalized.27
Public interest and concerns have been placed predominantly on vaccine-related rare thromboembolic events,28 which have been associated with vaccine hesitancy and restrictions on their use.29 The present study found that the vaccination may offset SARS-CoV-2–induced VTE risk even if people get a breakthrough infection. This evident benefit should not be ignored in the ongoing global vaccination campaigns.
To our knowledge, for the first time, we showed that inherited thrombophilia was associated with a double risk of COVID-19–related VTE, echoing previous clinical findings of elevated factor V activity in patients with severe COVID-19.30,31,32 A relatively high proportion of congenital thrombophilia was detected in a small pilot study of 87 COVID-19 cases, but the minimal sample size precluded further robust inference.33
We analyzed linked data that combined extensive community SARS-CoV-2 testing, well-recorded vaccination status, ambulatory and hospital-based clinical outcomes, and large-scale genotyping data that were readily available for UKBB participants. The results of this analysis have potentially noteworthy implications. First, VTE risk management needs reevaluation for milder ambulatory COVID-19. With emerging evidence and guidelines focusing on VTE prophylaxis for hospitalized patients with COVID-19, further work is necessary to mitigate the risk in the community. The recent ACTIV-4B34 study demonstrated no benefit of use of aspirin or apixaban for VTE prevention among the general younger outpatients (median age, 54 years [IQR, 46-59]), largely because of a very low thrombotic event rate. The present study of older participants (mean age, 64 years) might inform ongoing35 or new trials that target the more elderly population, particularly those with the multiple risk factors identified in this study. Second, although the etiology of post–COVID-19 VTE is complex and multifaceted, this study’s findings elucidated the role of factor V and possibly prothrombin proteins as contributing factors. Third, although genetic testing of inherited thrombophilia for VTE prevention has been previously discussed in many clinical scenarios,36,37 this newly identified association with COVID-19–related VTE, comparable with a 10-year aging risk, supports the potential value of targeted genetic screening for thrombophilia in the infected older adults. Finally, the study data suggest the significant association of vaccination with minimizing the risk of COVID-19 VTE.
Limitations
This study also had some limitations. Residual confounding cannot be ruled out in this observational study, although robust statistical approaches for causal inference were applied, including PS matching and knowledge-driven negative control analyses. Differential outcome ascertainment might also have contributed to the elevated risk to some extent, given that SARS-CoV-2 infection since the pandemic was strongly believed to be a risk factor for VTE, and clinicians were probably more intentionally looking for VTE in patients with COVID-19 than others requiring hospital care. Although participants with COVID-19 were from nonhospital settings, they were tested likely because of the presence of typical symptoms of COVID-19. The extent to which purely asymptomatic infection is associated with VTE risk warrants further investigation. Also, the VTE in this study appeared to be clinically relevant events that trigger ICD-10 coding. However, the diagnoses themselves did not necessarily reflect VTE status and severity (eg, asymptomatic, incidental, or symptomatic, which requires bespoke screening for VTE in patients with COVID-19). This study was performed among the antithrombotic use–naive population, and before the monoclonal antibody infusion or antivirals were approved for use; whether these treatments can mitigate ambulatory COVID-19–related VTE risk remains unclear. Moreover, the estimates from our analyses were an average and mixed short-term (30-day) effect of several SARS-CoV-2 strains from the original wild type to Delta,38 which should be cautiously extrapolated to ongoing or post–short-term periods and novel variants, such as Omicron. Finally, participants recruited in UKBB were not fully representative of the general population,39,40 and the data included in this study had very few participants who identified as Asian or Asian British, Black or Black British, or Chinese, which may limit the generalizability of the findings.
Conclusions
In this population-based cohort study of patients with COVID-19, ambulatory COVID-19 was associated with a substantial increase in excess VTE. This risk was much higher among unvaccinated individuals and increased with older age, in men, and in patients with obesity. Factor V Leiden thrombophilia further doubled VTE risk, comparable with a 10-year aging risk. These findings call for targeted prevention and tailored thromboprophylaxis strategies for post–COVID-19 VTE in outpatient settings and suggest an etiological role of inherited thrombophilia.
eFigure 1. Flow-chart for the study design and participants’ eligibility
eFigure 2. Distribution of infected and matched non-infected persons over the study period
eTable 1. Baseline characteristics of participants stratified by the VTE outcome during the follow-up period
eTable 2. Hazard ratio of clinical risk factors for venous thromboembolism amongs the infect and uninfected groups
eTable 3. Frequency of risk variants for inherited thrombophilia
eTable 4. Baseline characteristics amongst SARS-CoV-2 infected participants stratified by the inherited thrombophilia
eMethods.
References
- 1.Tan BK, Mainbourg S, Friggeri A, et al. Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis. Thorax. 2021;76(10):970-979. doi: 10.1136/thoraxjnl-2020-215383 [DOI] [PubMed] [Google Scholar]
- 2.Talasaz AH, Sadeghipour P, Kakavand H, et al. Recent randomized trials of antithrombotic therapy for patients with COVID-19: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(15):1903-1921. doi: 10.1016/j.jacc.2021.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spyropoulos AC, Goldin M, Giannis D, et al. ; HEP-COVID Investigators . Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized Patients with COVID-19: the HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181(12):1612-1620. doi: 10.1001/jamainternmed.2021.6203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortega-Paz L, Galli M, Capodanno D, et al. Safety and efficacy of different prophylactic anticoagulation dosing regimens in critically and non-critically ill patients with COVID-19: a systematic review and meta-analysis of randomized controlled trials. Eur Heart J Cardiovasc Pharmacother. Published online September 14, 2021. doi: 10.1093/ehjcvp/pvab070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institutes of Health . Antithrombotic therapy in patients with COVID-19. Accessed December 11, 2021. https://www.covid19treatmentguidelines.nih.gov/therapies/antithrombotic-therapy/
- 6.Mai V, Tan BK, Mainbourg S, et al. Venous thromboembolism in COVID-19 compared to non-COVID-19 cohorts: a systematic review with meta-analysis. Vascul Pharmacol. 2021;139:106882. doi: 10.1016/j.vph.2021.106882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katsoularis I, Fonseca-Rodríguez O, Farrington P, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377:e069590. doi: 10.1136/bmj-2021-069590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hippisley-Cox J, Patone M, Mei XW, et al. Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ. 2021;374:n1931. doi: 10.1136/bmj.n1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ho FK, Man KKC, Toshner M, et al. Thromboembolic risk in hospitalized and nonhospitalized COVID-19 patients: a self-controlled case series analysis of a nationwide cohort. Mayo Clin Proc. 2021;96(10):2587-2597. doi: 10.1016/j.mayocp.2021.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thilagar B, Beidoun M, Rhoades R, Kaatz S. COVID-19 and thrombosis: searching for evidence. Hematology Am Soc Hematol Educ Program. 2021;2021(1):621-627. doi: 10.1182/hematology.2021000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.European Centre for Disease Prevention and Control . Assessment of the further spread and potential impact of the SARS-CoV-2 Omicron variant of concern in the EU/EEA, 19th update. Accessed March 3, 2022. https://www.ecdc.europa.eu/en/publications-data/covid-19-omicron-risk-assessment-further-emergence-and-potential-impact
- 12.Iuliano AD, Brunkard JM, Boehmer TK, et al. Trends in disease severity and health care utilization during the early Omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):146-152. doi: 10.15585/mmwr.mm7104e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goligher EC, Bradbury CA, McVerry BJ, et al. ; REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators . Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N Engl J Med. 2021;385(9):777-789. doi: 10.1056/NEJMoa2103417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emert R, Shah P, Zampella JG. COVID-19 and hypercoagulability in the outpatient setting. Thromb Res. 2020;192:122-123. doi: 10.1016/j.thromres.2020.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiong X, Chi J, Gao Q. Prevalence and risk factors of thrombotic events on patients with COVID-19: a systematic review and meta-analysis. Thromb J. 2021;19(1):32. doi: 10.1186/s12959-021-00284-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong J, Rudkin JK, Allen N, et al. Dynamic linkage of COVID-19 test results between Public Health England’s Second Generation Surveillance System and UK Biobank. Microb Genom. 2020;6(7). doi: 10.1099/mgen.0.000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bycroft C, Freeman C, Petkova D, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562(7726):203-209. doi: 10.1038/s41586-018-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klarin D, Busenkell E, Judy R, et al. ; INVENT Consortium; Veterans Affairs’ Million Veteran Program . Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease. Nat Genet. 2019;51(11):1574-1579. doi: 10.1038/s41588-019-0519-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.GOV.UK. English indices of deprivation. GOV.UK. Updated December 13, 2012. https://www.gov.uk/government/collections/english-indices-of-deprivation. Accessed March 14, 2022.
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 21.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399-424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas L, Li F, Pencina M. Using propensity score methods to create target populations in observational clinical research. JAMA. 2020;323(5):466-467. doi: 10.1001/jama.2019.21558 [DOI] [PubMed] [Google Scholar]
- 23.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083-3107. doi: 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170(2):244-256. doi: 10.1093/aje/kwp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arnold BF, Ercumen A. Negative control outcomes: a tool to detect bias in randomized trials. JAMA. 2016;316(24):2597-2598. doi: 10.1001/jama.2016.17700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.PLINK . PLINK 1.90 beta. Accessed March 14, 2022. https://www.cog-genomics.org/plink/
- 27.Burn E, Duarte-Salles T, Fernandez-Bertolin S, et al. Venous or arterial thrombosis and deaths among COVID-19 cases: a European network cohort study. Lancet Infect Dis. 2022;0(0):S1473-3099(22)00223-7. doi: 10.1016/S1473-3099(22)00223-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cines DB, Bussel JB. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med. 2021;384(23):2254-2256. doi: 10.1056/NEJMe2106315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahase E. Covid-19: US suspends Johnson and Johnson vaccine rollout over blood clots. BMJ. 2021;373(970):n970. doi: 10.1136/bmj.n970 [DOI] [PubMed] [Google Scholar]
- 30.Stefely JA, Christensen BB, Gogakos T, et al. Marked factor V activity elevation in severe COVID-19 is associated with venous thromboembolism. Am J Hematol. 2020;95(12):1522-1530. doi: 10.1002/ajh.25979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Meijenfeldt FA, Havervall S, Adelmeijer J, et al. Elevated factor V activity and antigen levels in patients with Covid-19 are related to disease severity and 30-day mortality. Am J Hematol. 2021;96(4):E98-E100. doi: 10.1002/ajh.26085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Appenzeller F, Schmehl J, Gawaz M, Müller I. Extensive thromboembolism in a young male with asymptomatic COVID-19 infection and heterozygous factor V Leiden mutation. Hamostaseologie. 2021;41(5):400-402. doi: 10.1055/a-1554-6390 [DOI] [PubMed] [Google Scholar]
- 33.de la Morena-Barrio ME, Bravo-Pérez C, de la Morena-Barrio B, et al. A pilot study on the impact of congenital thrombophilia in COVID-19. Eur J Clin Invest. 2021;51(5):e13546. doi: 10.1111/eci.13546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Connors JM, Brooks MM, Sciurba FC, et al. ; ACTIV-4B Investigators . Effect of antithrombotic therapy on clinical outcomes in outpatients with clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial. JAMA. 2021;326(17):1703-1712. doi: 10.1001/jama.2021.17272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Capell WH, Barnathan ES, Piazza G, et al. Rationale and design for the study of rivaroxaban to reduce thrombotic events, hospitalization and death in outpatients with COVID-19: the PREVENT-HD study. Am Heart J. 2021;235:12-23. doi: 10.1016/j.ahj.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Connors JM. Thrombophilia testing and venous thrombosis. N Engl J Med. 2017;377(12):1177-1187. doi: 10.1056/NEJMra1700365 [DOI] [PubMed] [Google Scholar]
- 37.Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301(23):2472-2485. doi: 10.1001/jama.2009.853 [DOI] [PubMed] [Google Scholar]
- 38.GOV.UK . Investigation of SARS-CoV-2 variants: technical briefings. Accessed June 1, 2022. https://www.gov.uk/government/publications/investigation-of-sars-cov-2-variants-technical-briefings
- 39.Fry A, Littlejohns TJ, Sudlow C, et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186(9):1026-1034. doi: 10.1093/aje/kwx246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Flow-chart for the study design and participants’ eligibility
eFigure 2. Distribution of infected and matched non-infected persons over the study period
eTable 1. Baseline characteristics of participants stratified by the VTE outcome during the follow-up period
eTable 2. Hazard ratio of clinical risk factors for venous thromboembolism amongs the infect and uninfected groups
eTable 3. Frequency of risk variants for inherited thrombophilia
eTable 4. Baseline characteristics amongst SARS-CoV-2 infected participants stratified by the inherited thrombophilia
eMethods.



