Abstract
Objectives
The aim of this study was to summarize the available evidence on the prevalence of stress, burnout, anxiety and depression among healthcare providers in the Gulf Cooperation Council (GCC) countries (KSA, Bahrain, Kuwait, Oman, Qatar, and the United Arab Emirates) during the COVID-19 pandemic.
Methods
We searched PubMed, PsycINFO, Scopus, and Google scholar for related studies published between January 2020 and April 2021 and conducted a systematic review and meta-analysis.
Results
Of the 1815 identified studies, 29 met the inclusion criteria, and 19 studies were included in the meta-analysis. The pooled estimate of prevalence for moderate to severe anxiety as reported using GAD-7 was 34.57% (95% CI = 19.73%, 51.12%), that for moderate to severe depression using PHQ-9 was 53.12% (95% CI = 32.76%, 72.96%), and that for moderate to severe stress using the 10-item Perceived Stress Scales was 81.12% (95% CI = 72.15%, 88.70%). Meta-analysis was not performed for burnout due to the small number of identified studies and the different tools used; however, the highest prevalence was reported at 76% (95% CI = 64%, 85%). Overall, a positive trend was observed over time for moderate to severe anxiety and depression, p = 0.0059 and 0.0762, respectively. Of note, the heterogeneity was significant among the studies, and many studies were of poor quality.
Conclusion
The prevalence of mental health disorders during the current pandemic among healthcare workers in GCC countries is high. However, the results could be affected by the high heterogeneity and low quality studies.
Keywords: Anxiety, Arabian Gulf, COVID-19, Depression, Healthcare worker, Mental health
الملخص
أهداف البحث
تهدف هذه المراجعة إلى تلخيص الدراسات العلمية حول مدى انتشار الكرب، والاحتراق النفسي، والقلق، والاكتئاب بين مقدمي الرعاية الصحية في دول مجلس التعاون الخليجي (المملكة العربية السعودية، البحرين، الكويت، سلطنة عمان، قطر، الإمارات العربية المتحدة) خلال جائحة كوفيد-١٩.
طرق البحث
قمنا بالبحث في قواعد البيانات ببميد، سايك إنفو، سكوبس، وقوقل سكولار للتعرف على الدراسات ذات الصلة المنشورة في الفترة ما بين يناير ٢٠٢٠ إلى أبريل ٢٠٢١، وقمنا بعمل مراجعة منهجية وتحليل تلوي.
النتائج
تم العثور على ١٨١٥ ورقة في قواعد البيانات، من بينها ٢٩ دراسة استوفت معايير الاشتمال، ومنها ١٩ دراسة قمنا بتضمينها في التحليل التلوي. التقدير المجمع للقلق المتوسط إلى الشديد باستخدام مقياس "جاد-7" كان ٣٤.٥٧٪ (فترة الثقة: ١٩.٧٣٪ إلى ٥١.١٢٪)، بينما للاكتئاب المتوسط إلى الشديد باستخدام مقياس "استبانة صحة المريض-9" كان٥٣.٢١٪ (فترة الثقة: ٣٢.٧٦٪ إلى ٧٢.٩٦٪)، وللكرب باستخدام " مقياس إدراك الكرب-10" كان ٨١.١٢٪ (فترة الثقة: ٧٢.١٥٪ إلى ٨٨.٧٠٪).
أما بالنسبة للاحتراق النفسي، فلم يتم عمل التحليل التلوي لقلة الدراسات التي تم العثور عليها، غير أن أعلى نسبة بين الدراسات كانت ٪٧٦ (فترة الثقة: ٪٦٤ إلى ٪٨٥).
وبشكل عام، فقد لوحظ وجود اتجاه موجب مع تقدم الوقت للجائحة بالنسبة للقلق والاكتئاب المتوسطين إلى شديدي الدرجة. مع ملاحظة بأن هناك عدم تجانس عال بين الدراسات، وكثير من الدراسات كانت منخفضة الجودة.
الاستنتاجات
معدل انتشار الاضطرابات النفسية بين العاملين في الرعاية الصحية في دول مجلس التعاون الخليجي خلال الجائحة الحالية عال. على الرغم من ذلك، قد تتأثر النتائج بعدم التجانس العالي بين الدراسات وانخفاض جودتها.
الكلمات المفتاحية: القلق, الخليج العربي, كوفيد -19, الاكتئاب, ممارس صحي, الصحة النفسية
Introduction
Coronavirus disease (COVID-19) is an infectious disease that emerged in China in December 2019 and spread rapidly across the globe. The infection rate rose exponentially, forcing healthcare systems to operate beyond their capacity.1 Healthcare workers (HCWs) were among the “front-liners” to battle this pandemic while exposed to many stressors, such as high workload and the unexpected growing number of cases and deaths. Furthermore, there was a shortage of personal protective equipment, ventilators and intensive care unit (ICU) beds. In addition, many of HCWs faced social stigmatization and some isolated themselves in fear of transmitting the infection to their families.2,3
The countries of the Gulf Cooperation Council (GCC), the KSA, United Arab Emirates, Kuwait, Oman, Qatar and Bahrain,4 were no exception to the global pandemic, with the first case of COVID-19 identified on January 29, 2020.5 These countries, classified as high-income countries, are located in southwest Asia, along the Arabian Gulf, and have a total population of 56,905,993.6,7 In addition to geographical borders, they share common cultural, social, political and economic backgrounds, as well as language and religion.8 For containment of the emergent pandemic, several public health measures were implemented in GCC countries, including but not limited to travel bans, partial or complete lockdowns and the prohibition of mass gathering events.9 Despite these measures, the number of reported cases in GCC countries until January 2021 was as high as 20,759 per million compared to 13,135 per million worldwide.10 HCWs faced several challenges, such as high risk of infection and transmission of the infection to their families, high workload and increasing working hours.5
The objective of this review is to summarize the available evidence on the prevalence of stress, burnout, anxiety, and depression among HCWs in GCC countries during the COVID-19 pandemic. The synthesized knowledge can help evaluate the local situation and draw the attention of national health authorities and policymakers to the need to implement interventions to improve the mental health of HCWs in the current and similar future situations. Furthermore, it can provide baseline data for further research on the long-term effects of this pandemic on the mental health of HCWs in GCC countries.
Materials and Methods
Information sources
PubMed, PsycINFO, Scopus and Google scholar were searched for studies published between January 2020 and mid-April 2021. Additionally, the reference lists of the included studies were screened for relevant literature.
Search strategy
A population/outcome question was formulated. The following question was addressed; “in adult HCWs in the GCC countries, what was the prevalence of moderate to severe mental health problems, including anxiety, depression, stress, or burnout, during the period of the COVID-19 pandemic from 29 January 2020 to 15 April 2021, in any healthcare setting?” Multiple terms were categorized into population or outcome (Supplementary Table 1) and used in the search strategy. The search strategy for each database is presented in Supplementary Table 2. For Google Scholar, the search terms were modified to the most sensitive ones; only the first 49 pages were retrievable due to limitations associated with the search engine. This protocol was not registered.
Eligibility criteria
Studies were considered eligible for inclusion if they fulfilled the following criteria: 1) reported the prevalence of depression, anxiety, stress or burnout; 2) included HCWs regardless of the setting; 3) were conducted in one or more GCC countries; 4) the data collection process was conducted after the identification of the first confirmed case of COVID-19 GCC countries (i.e., January 30, 2020),5 and 5) outcome assessment (prevalence of mental health disorders) was performed using a valid tool. Studies for which the full text was not available, along with duplicate studies were excluded.
Selection process
All identified studies were imported to Covidence, a web-based software designed for systematic reviews (Veritas Health Innovation, Melbourne, Australia). First, the title and abstract of all studies were screened independently in a double-blind manner by two reviewers. Any conflict was resolved by discussion. Subsequently, the full text of the studies was reviewed, and the reason for exclusion of any study was recorded in the same software.
Data collection process and data items
A template for data extraction was designed in Covidence software and the following items were extracted: 1) journal, study title and author name; 2) country in which the study was conducted; 3) study aim; 4) study design; 5) start and end dates of data collection; 6) inclusion and exclusion criteria; 7) sampling technique and recruitment methods; 8) total number of participants; 9) measurement tool for the study outcomes; 10) cutoff points for the outcomes; 11) reported the prevalence of depression, anxiety, stress and/or burnout in general and/or in each category (mild, moderate, severe, or as specified in each study report); 12) average score (mean or median) for the abovementioned mental health disorders, and 13) associated risk factors for each studied outcome.
Risk of bias assessment
Each study was assessed using the modified Newcastle-Ottawa Scale (NOS) for the quality assessment of cross-sectional studies. This tool has three domains: selection, comparability and outcome, and seven question items. The tool uses a star system ranging from 0 to 10, with the highest being the best.11 Based on the final score, studies are classified as being of unsatisfactory (1–4), satisfactory (5–6), good (7–8) or very good (9–10) quality.
In addition, the Joanna Briggs Institute (JBI) checklist for prevalence studies was also used.12 This checklist has nine item questions with three possible answers (yes, no or unclear); 1 point is given for each “yes” answer, and 0 for “no” or “unclear.” The maximum final score is 9 points, with higher scores indicating higher-quality studies.
Synthesis methods
The extracted data for each study were presented in a table to facilitate comparison, and narrative synthesis was used to summarize the distribution of the studied mental health disorders. R software (version 4.1.2) (Vienna, Austria) with meta (version 5.2-0) and metaphor (version 3.4-0) packages was used for the meta-analysis, meta-regression and related plots. Due to differences between populations, analyses were performed using the random effects model. Double-arcsine transformation was used to stabilize the variance. Studies that reported data collection time were included in meta-regression. Mid-time point was considered in the model construction. Heterogeneity was assessed using the I2 statistic and Cochran's Q test.
Reporting bias assessment
Funnel plots were generated and Eggar's test was performed to assess publication bias.
Results
Study selection
The literature search identified a total of 2162 studies. An additional four studies were identified from the reference lists of the included studies. After removing duplicates, 1815 studies were screened at the title and abstract level, of which 90 studies were included for full-text screening and assessment against the eligibility criteria. Finally, 29 studies were included for analysis (Figure 1).
Figure 1.
PRISMA flow diagram.
Study characteristics
The characteristics of the included studies are presented in Table 1. The majority of the studies were conducted in the KSA (18 studies),13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 six in Oman,31, 32, 33, 34, 35, 36 two in Kuwait37,38 and one study in Bahrain.39 The remaining two included studies were conducted in multiple countries, including KSA.40,41 The sample sizes ranged from 47 to 4,920.28,30
Table 1.
Characteristics of the included studies.
| Study | Country | Sampling technique | Sample size | Response rate | Population | Related outcomes | NOS quality | JBI score |
|---|---|---|---|---|---|---|---|---|
| Abu-Snieneh et al. (2020)13 | KSA | Convenience sampling | 1265 | – | Nurses | Anxiety and depression | Good | 5 |
| Alahmadi et al. (2020)14 | KSA | – | 108 | 59% | Ophthalmology residents | Depression | Unsatisfactory | 4 |
| AlAmmari et al. (2021)23 | KSA | Purposive sampling | 720 | – | HCWs | Anxiety and depression | Satisfactory | 4 |
| Alamri et al. (2020)24 | KSA | – | 542 (HCWs only) | – | General population (including HCWs) | Anxiety, depression, and stress | Unsatisfactory | 5 |
| Alanazi et al. (2020)25 | KSA | – | 3557 | – | HCWs | Burnout | Satisfactory | 5 |
| AlAteeq et al. (2020)26 | KSA | Convenience sampling | 502 | – | HCWs | Anxiety and depression | Satisfactory | 4 |
| Aldarmasi et al. (2021)27 | KSA | – | 377 | – | HCWs | Stress | Unsatisfactory | 4 |
| Alenazi et al. (2020)28 | KSA | Convenience sampling | 4920 | 3.4% | HCWs | Anxiety | Good | 6 |
| AlMahyijari et al. (2020)31 | Oman | – | 150 | – | Nurses and physicians | Anxiety | Unsatisfactory | 4 |
| AlMaqbali et al. (2021)32 | Oman | – | 1130 | – | Nurses | Anxiety, depression, and stress | Unsatisfactory | 6 |
| Almater et al. (2020)29 | KSA | – | 107 | 30.6% | Ophthalmologists | Anxiety, depression, and stress | Unsatisfactory | 4 |
| Almubark et al. (2020)30 | KSA | – | 47 | – | Nurses in ICU and ED | Burnout | Unsatisfactory | 4 |
| Alsairafi et al. (2021)37 | Kuwait | Convenience sampling | 559 (HCWs only) | – | HCWs and health students | Anxiety and depression | Good | 5 |
| Alsaywid et al. (2020)15 | KSA | – | 1528 | 10.7% | Residents and fellows | Anxiety and depression | Satisfactory | 5 |
| Alshekaili et al. (2020)33 | Oman | Random sampling | 1139 | – | HCWs | Anxiety, depression, and stress | Unsatisfactory | 7 |
| Alsulimani et al. (2021)16 | KSA | – | 646 | – | HCWs | Burnout | Unsatisfactory | 6 |
| Alzaid et al. (2020)17 | KSA | – | 441 | 96.7% | HCWs | Anxiety | Very Good | 6 |
| Arafa et al. (2020)40 | KSA and Egypt | Snowball sampling | 151 (KSA only) | – | HCWs | Anxiety, depression, and stress | Satisfactory | 3 |
| Badahdah et al. (2020)34 | Oman | Convenience sampling | 509 | – | Physicians and nurses | Anxiety and Stress | Unsatisfactory | 3 |
| Balay-Odao et al. (2021)18 | KSA | Convenience sampling | 281 | – | Nurses | Anxiety, depression, and stress | Satisfactory | 5 |
| Burhamah et al. (2020)38 | Kuwait | – | 282 (HCWs only) | – | General population (including HCWs) | Anxiety and depression | Satisfactory | 3 |
| Cravero et al. (2020)41 | International (including KSA) | Snowball sampling | 76 (KSA only) | – | Residents and fellows | Burnout | Satisfactory | 5 |
| Jahan et al. (2021)35 | Oman | – | 327 | – | Physicians and nurses in PHCs | Anxiety, depression, and stress | Unsatisfactory | 4 |
| Jahrami et al. (2020)39 | Bahrain | Purposive/convenience sampling | 257 | 94% | HCWs (working directly with patients) | Stress | Satisfactory | 5 |
| Joseph et al. (2020)19 | KSA | – | 110 (HCWs only) | – | General population (including HCWs) | Anxiety, depression, and stress | Satisfactory | 6 |
| Khamis et al. (2020)36 | Oman | – | 402 | – | Female physicians and nurses | Anxiety and stress | Unsatisfactory | 5 |
| Shalaby et al. (2021)20 | KSA | Snowball sampling | 1182 | – | HCWs in tertiary hospitals | Anxiety and depression | Satisfactory | 3 |
| Surrati et al. (2020)21 | KSA | – | 118 | – | HCWs | Anxiety, depression, and stress | Unsatisfactory | 5 |
| Temsah et al. (2020)22 | KSA | Convenience sampling | 582 | 71.8% | HCWs | Anxiety | Satisfactory | 4 |
Abbreviations: KSA, Kingdom of Saudi Arabia; NOS, Newcastle-Ottawa Scale; JBI, Joanna Briggs Institute.
With regards to the outcomes of interest, nine studies assessed the prevalence of anxiety, depression and stress,18,19,21,24,29,32,33,35,40 seven assessed anxiety and depression,13,15,20,23,26,37,38 two assessed anxiety and stress,34,36 four assessed anxiety only,17,22,28,31 four assessed burnout,16,25,30,41 two assessed stress,27,39 and one study reported the prevalence of depression only.14
Risk of bias assessment
Based on NOS scores, the quality of the included studies ranged from unsatisfactory to very good with the majority of studies being rated as unsatisfactory. The mean score based on the JBI assessment tool was 4.6 (Table 1).
Meta-analysis results
Prevalence of anxiety
Of the 29 included studies, 22 reported the prevalence of anxiety (Table 2).13,15,17, 18, 19, 20, 21, 22, 23, 24,26,28,29,31, 32, 33, 34, 35, 36, 37, 38,40 In general, regardless of the tool and cutoff points, the reported prevalence of moderate to severe anxiety ranged from 11% (22) to 81% (20).
Table 2.
Prevalence of anxiety.
| Study | Country | Population | Sample size | Period of data collection | Instrument | Prevalence |
|---|---|---|---|---|---|---|
| Abu-Snieneh et al. (2020)13 | KSA | Nurses | 1265 | End of April 2020. Middle of June 2020 | GAD-7 | Mild: 31.2% Moderate: 9.7% Severe: 8.8% Moderate to severe: 18.5% |
| AlAmmari et al. (2021)23 | KSA | HCWs | 720 | 27 April 2020–4 May 2020 | GAD-7 | Mild: 28.47% Moderate: 12.77% Severe: 8.33% Moderate to severe: 21.1% |
| Alamri et al. (2020)24 | KSA | General population (including HCWs) | 542 (HCWs only) | 10 May 2020–16 May 2020 | DASS-21 | 20.1% (cut-off 21) |
| AlAteeq et al. (2020)26 | KSA | HCWs | 502 | March 2020 | GAD-7 | Mild: 25.1% Moderate: 11% Severe: 15.3% Moderate to severe: 26.3% |
| Alenazi et al. (2020)28 | KSA | HCWs | 4920 | 15 May 2020–18 May 2020 | Dispositional cancer worry scale | Low: 31.5% Medium: 36.1% High: 32.3% Medium to high: 68.3% |
| AlMahyijari et al. (2020)31 | Oman | Nurses and physicians | 150 | – | GAD-7 | 28.67% |
| AlMaqbali et al. (2021)32 | Oman | Nurses | 1130 | 7 August 2020–17 August 2020 | HADS | 44.2% |
| Almater et al. (2020)29 | KSA | Ophthalmologists | 107 | 28 March 2020–4 April 2020 | GAD-7 | Mild: 25.2% Moderate: 15.9% Severe: 5.6% Moderate to severe: 21.5% |
| Alsairafi et al. (2021)37 | Kuwait | HCWs and health students | 559 (HCWs only) | May 2020–July 2020 | GAD-7 | Mild: 19.5% Moderate: 43.1% Severe: 37.4% Moderate to severe: 80.5% |
| Alsaywid et al. (2020)15 | KSA | Residents and fellows | 1528 | – | GAD-7 | Mild: 26.7% Moderate: 24.5% Severe: 35.6% Moderate to severe: 60.1% |
| Alshekaili et al. (2020)33 | Oman | HCWs | 1139 | 8 April 2020–17 April 2020 | DASS-21 | 34.1% |
| Alzaid et al. (2020)17 | KSA | HCWs | 441 | GAD-7 | Mild: 27% Moderate: 13.2% Severe: 7.9% Moderate to severe: 21.1% |
|
| Arafa et al. (2020)40 | KSA and Egypt | HCWs | 151 (KSA only) | 14 April 2020–24 April 2020 | DASS-21 | Mild to moderate: 26.5% Severe to very severe: 15.2% Mild to very severe: 41.7% |
| Badahdah et al. (2020)34 | Oman | Physicians and nurses | 509 | 1st two weeks of April 2020 | GAD-7 | Mild: 38.7% Moderate: 17.7% Severe: 8.3% Moderate to severe: 26% |
| Balay-Odao et al. (2021)18 | KSA | nurses | 281 | April 2020–June 2020 | DASS-21 | Mild: 6.8% Moderate: 37.4% Severe: 12.1% Extremely severe: 7.5% Mild to extremely severe: 57% |
| Burhamah et al. (2020)38 | Kuwait | General population (including HCWs) | 282 (HCWs only) | 25 May 2020–30 May 2020 | GAD-7 | 34% |
| Jahan et al. (2021)35 | Oman | Physicians and nurses in PHCs | 327 | – | DASS-21 | Mild: 13.4% Moderate: 27.1% Severe: 10.3% Extremely severe: 10.9% Mild to extremely severe: 61.7% |
| Joseph et al. (2020)19 | KSA | General population (including HCWs) | 110 (HCWs only) | 12 April 2020–10 May 2020 | PHQ-4 | Moderate to severe (combined anxiety–depression): 20% |
| Khamis et al. (2020)36 | Oman | Female physicians and nurses | 402 | April 2020 (first 2 weeks) | GAD-7 | Mild: 39.6% Moderate: 18.9% Severe: 8.9% Moderate to severe: 27.8% |
| Shalaby et al. (2021)20 | KSA | HCWs in tertiary hospitals | 1182 | 1 June 2020–31 July 2020 | GAD-7 | Moderate: 9% Moderately severe: 48% Severe: 33% Moderately severe–severe: 81% |
| Surrati et al. (2020)21 | KSA | HCWs | 118 | April 2020 | HADS | Borderline: 21.2% Abnormal: 35.6% Total: 56.8% |
| Temsah et al. (2020)22 | KSA | HCWs | 582 | 5 February 2020–16 February 2020 | GAD-7 | Mild: 20.8% Moderate: 8.1% Severe: 2.9% Moderate to severe: 11% |
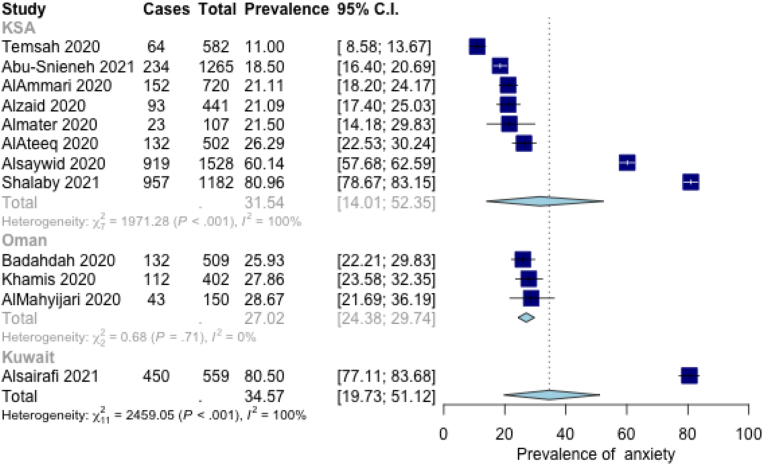
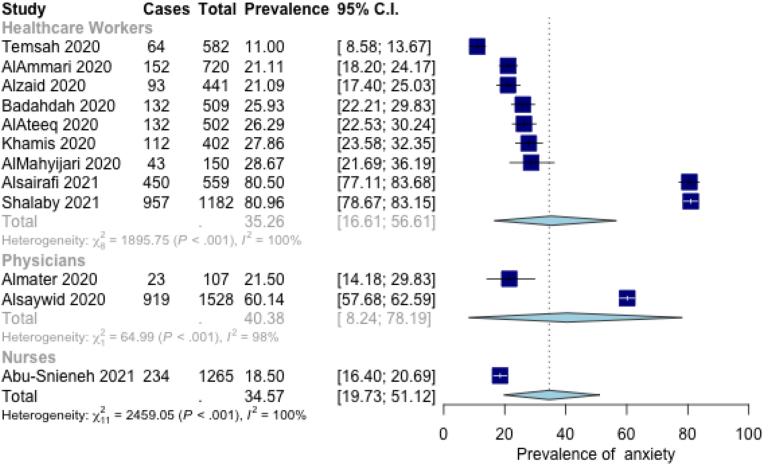
The pooled estimate of moderate to severe anxiety as reported using GAD-7 was 34.57% (95% CI = 19.73%, 51.12%). By country, it was 31.54% (95% CI = 14.01%, 52.35%), 27.02% (95% CI = 24.38%, 29.74%), for KSA and Oman, respectively, with one study from Kuwait reporting prevalence of 80.50% (95% CI = 77.11%, 83.68%) (Figure 2). Moreover, subgroup analysis by population for studies on all HCWs showed a pooled prevalence of 35.26% (95% CI = 16.61%, 56.61%), while for physicians it was 40.38% (95% CI = 8.24%, 78.19), and for nurses it was reported by a single study at 18.50% (95% CI = 16.40%, 20.69%)13 (Figure 3). The removal of studies with unsatisfactory quality did not improve heterogeneity.
Figure 2.
Prevalence of moderate to severe anxiety by country (GAD-7).
Figure 3.
Prevalence of moderate to severe anxiety by population (GAD-7).
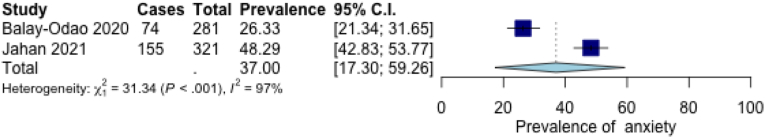
For DASS-21, the pooled estimate was 37.00% (95% CI = 17.30%, 59.26%) with high heterogeneity (p < 0.001, I2 = 97%) (Figure 4).
Figure 4.
Prevalence of moderate to severe anxiety (DASS-21).
Two studies used the Hospital Anxiety and Depression Scale (HADS); the prevalence of anxiety was reported at 56.8% and 44.2% in KSA and Oman, respectively.21,32
Prevalence of depression
A total of 17 studies reported the prevalence of depression13, 14, 15,18, 19, 20, 21,23,24,26,29,32,33,35,37,38,40 (Table 3). The prevalence of depression among all included studies ranged from 23% (23) to 95.9% (37).
Table 3.
Prevalence of depression.
| Study | Country | Population | Sample size | Period of data collection | Instrument | Prevalence |
|---|---|---|---|---|---|---|
| Abu-Snieneh et al. (2020)13 | KSA | Nurses | 1265 | End of April 2020–middle of June 2020 | PHQ-9 | Mild: 33.6% Moderate: 14.5% Severe: 11.4% Moderate to severe: 25.9% |
| Alahmadi et al. (2020)14 | KSA | ophthalmology residents | 142 (PHQ-9: 108) | 7 July 2020–14 July 2020 | PHQ-9 | Mild: 33.1% Moderate: 26.1% Severe: 11.3% Moderate to severe: 37.4% |
| AlAmmari et al. (2021)23 | KSA | HCWs | 720 | 27 April 2020–4 May 2020 | PHQ-9 | Mild: 26.1% Moderate: 13% Moderately severe: 7.91% Severe: 2.08% Moderate to severe: 22.99% |
| Alamri et al. (2020)24 | KSA | General population (including HCWs) | 542 (HCWs only) | 10 May 2020–16 May 2020 | DASS-21 | 32.7% (cut-off: 21) |
| AlAteeq et al. (2020)26 | KSA | HCWs | 502 | March 2020 | PHQ-9 | Mild: 24.9% Moderate: 14.5% Moderately severe: 10% Severe: 5.8% Moderate to severe: 30.3% |
| AlMaqbali et al. (2021)32 | Oman | Nurses | 1130 | 7 August 2020–17 August 2020 | HADS | 38.5% |
| Almater et al. (2020)29 | KSA | Ophthalmologists | 107 | 28 March 2020–4 April 2020 | PHQ-9 | Mild: 21.5% Moderate: 17.8% Moderately severe: 7.5% Severe: 3.7% Moderate to severe: 29% |
| Alsairafi et al. (2021)37 | Kuwait | HCWs and health students | 559 (HCWs only) | May 2020–July 2020 | PHQ-9 | Mild: 4.1% Moderate: 32.2% Moderately severe: 35.6% Severe: 28.1% Moderate to severe: 95.9% |
| Alsaywid et al. (2020)15 | KSA | Residents and fellows | 1528 | – | PHQ-9 | Mild: 23.4% Moderate: 24.4% Moderately severe: 22.3% Severe: 19.9% Moderate to severe: 66.6% |
| Alshekaili et al. (2020)33 | Oman | HCWs | 1139 | 8 April 2020–17 April 2020 | DASS-21 | 32.3% |
| Arafa et al. (2020)40 | KSA and Egypt | HCWs | 151 (KSA only) | 14 April 2020–24 April 2020 | DASS-21 | Mild to moderate: 37.1% Severe to very severe: 14.6% Total: 51.7% |
| Balay-Odao et al. (2021)18 | KSA | Nurses | 281 | April 2020–June 2020 | DASS-21 | Mild: 19.6% Severe: 23.5% Extremely severe: 5.7% Mild to extremely severe: 48.8% |
| Burhamah et al. (2020)38 | Kuwait | General population (including HCWs) | 282 (HCWs only) | 25 May 2020–30 May 2020 | PHQ-9 | 63.8% |
| Jahan et al. (2021)35 | Oman | Physicians and nurses in PHCs | 327 | – | DASS-21 | Mild: 14% Moderate: 21.5% Severe: 4.4% Extremely severe: 2.2% Mild to extremely severe: 42.1% |
| Joseph et al. (2020)19 | KSA | General population (including HCWs) | 110 (HCWs only) | 12 April 2020–10 May 2020 | PHQ-4 | Moderate to severe combined anxiety/depression: 20% |
| Shalaby et al. (2021)20 | KSA | HCWs in tertiary hospitals | 1182 | 1 June 2020–31 July 2020 | PHQ-9 | Mild: 4% Moderate: 14% Moderately severe: 30% Severe: 52% Moderately severe to severe: 82% (cut-off: 11) |
| Surrati et al. (2020)21 | KSA | HCWs | 118 | April 2020 | HADS | Borderline: 21.2% Abnormal: 27.9% Total: 49.1% |
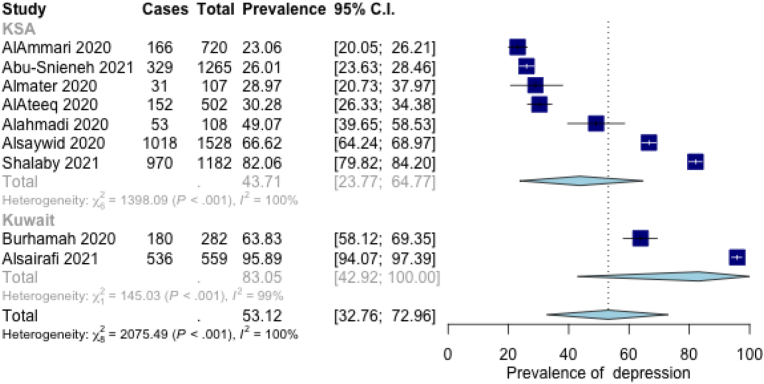
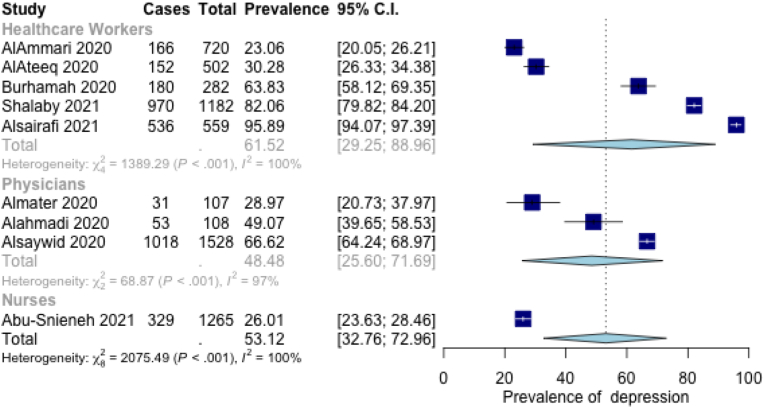
Using PHQ-9, studies in Kuwait showed a higher prevalence at 83.05% (95% CI = 42.92%,100%) as compared to KSA 43.71% (95% CI = 23.77%, 64.77%) (Figure 5). On the other hand, studies involving healthcare workers in general showed a higher prevalence at 61.52% (95% CI = 29.25%, 88.96%) than physicians alone at 48.48% (95% CI = 25.60%, 71.69%) (Figure 6). In both cases, high levels of heterogeneity were observed (p < 0.001, I2 = 100%). Overall, moderate to severe depression, as detected by PHQ-9, was pooled at 53.12% (95% CI = 32.76, 72.96). The pooling estimate from satisfactory to very good quality studies did not change the heterogeneity.
Figure 5.
Prevalence of moderate to severe depression by country (PHQ-9).
Figure 6.
Prevalence of moderate to severe depression by population (PHQ-9).
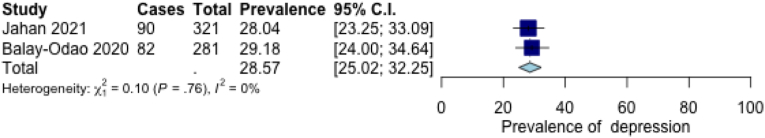
Moderate to severe depression, as reported by two studies using DASS-21, was pooled at 28.57% (95% CI = 25.02%, 32.25%) (Figure 7).
Figure 7.
Prevalence of moderate to severe depression (DASS-21).
Prevalence of stress
As shown in Table 4, 13 studies investigated the prevalence of stress among HCWs.18,19,21,24,27,29,32, 33, 34, 35, 36,39,40 The highest prevalence was in KSA at 90%27 while the lowest was 17.7% among nurses in KSA.18
Table 4.
Prevalence of stress.
| Study | Country | Population | Sample size | Period of data collection | Instrument | Prevalence |
|---|---|---|---|---|---|---|
| Alamri et al. (2020)24 | KSA | General population (including HCWs) | 542 (HCWs only) | 10 May 2020–16 May 2020 | DASS-21 | 22.1% |
| Aldarmasi et al. (2021)27 | KSA | HCWs | 377 | November 2020–January 2021 | PSS-10 | Low: 10% Moderate: 82% High: 8% Moderate to high: 90% |
| AlMaqbali et al. (2021)32 | Oman | Nurses | 1130 | 7 August 2020–17 August 2020 | PSS-10 | 75.6% |
| Almater et al. (2020)29 | KSA | Ophthalmologists | 107 | 28 March 2020–4 April 2020 | PSS-10 | Low: 28% Moderate: 68.2% High: 3.7% Moderate to high: 71.9% |
| Alshekaili et al. (2020)33 | Oman | HCWs | 1139 | 8 April 2020–17 April 2020 | DASS-21 | 23.8% |
| Arafa et al. (2020)40 | KSA and Egypt | HCWs | 151 (KSA only) | 14 April 2020–24 April 2020 | DASS-21 | Mild to moderate: 22.5% Severe to very severe: 12.6% Mild to very severe: 35.1% |
| Badahdah et al. (2020)34 | Oman | physicians and nurses | 509 | 1st two weeks of April 2020 | PSS-10 | Low stress: 43.6% High stress: 56.4% |
| Balay-Odao et al. (2021)18 | KSA | nurses | 281 | April 2020–June 2020 | DASS-21 | Mild: 5.7% Moderate: 8.5% Severe: 2.8% Extremely severe: 0.7% Mild to extremely severe: 17.7% |
| Jahan et al. (2021)35 | Oman | Physicians and nurses in PHCs | 327 | – | DASS-21 | Mild: 14.3% Moderate: 7.2% Severe: 4.4% Extremely severe: 0.9% Mild to extremely severe: 26.8% |
| Jahrami et al. (2020)39 | Bahrain | HCWs | 257 | April 2020 | PSS-10 | Low: 15.9% Moderate: 66.9% High: 17.1% Moderate to severe: 84% |
| Joseph et al. (2020)19 | KSA | General population (including HCWs) | 110 (HCWs only) | 12 April 2020–10 May 2020 | IES-6 | 68% |
| Khamis et al. (2020)36 | Oman | Female physicians and nurses | 402 | April 2020 (first 2 weeks) | PSS-10 | Low: 46.5% High: 53.5% |
| Surrati et al. (2020)21 | KSA | HCWs | 118 | April 2020 | PSS-4 | Low: 24.5% Moderate: 72.8% Severe: 2.6% Moderate to severe: 33.8% |
The pooled estimate of moderate to severe stress using the PSS-10 was 81.12% (95% CI = 72.15%, 88.70) with high levels of heterogeneity (p < 0.001, I2 = 94%) (Figure 8). Subgroup analysis was not performed due to the low number of studies in each group. The removal of low-quality studies resulted in only two studies to pool.
Figure 8.
Prevalence of moderate to severe stress (PSS-10).
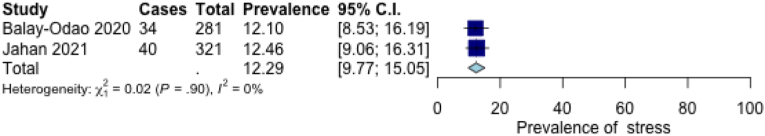
For two of the studies that used the DASS-21, we found a lower estimate of 12.29% (95% CI = 9.77%, 15.05%) (Figure 9). However, due to the large difference between the two groups, these were not pooled together.
Figure 9.
Prevalence of moderate to severe stress (DASS-21).
Other tools included the 6-item Impact of Event Scale; the prevalence for this tool was reported at 68%,19 and the 4-item PSS (PSS-4), with a prevalence reported at 33.8%.21
Prevalence of burnout
Our search identified four studies that assessed the prevalence of burnout among HCWs in GCC countries16,25,30,41 (Table 5). Each of these used a different tool for assessment: the Maslach Burnout Inventory,25 Maslach Burnout Inventory-Human Services Survey,30 Copenhagen Burnout Inventory,16 and the Single-item Measures of Emotional Exhaustion and Depersonalization.41 The highest prevalence (76%) was reported in an international study that included Saudi medical trainees.41 Due to the small number of identified studies and the use of different tools with different classifications, meta-analysis was not performed.
Table 5.
Prevalence of burnout.
| Study | Country | Population | Sample size | Period of data collection | Instrument | Prevalence |
|---|---|---|---|---|---|---|
| Alanazi et al. (2020)25 | KSA | HCWs (all categories) | 3557 | 5 October 2020–12 October 2020 | MBI | Low: EE burnout: 47% Depersonalization burnout: 50% Low personal achievement burnout: 42.9% High: EE burnout: 38.5% Depersonalization burnout: 31.2% Low personal achievement burnout: 33.6% |
| Almubark et al. (2020)30 | KSA | Nurses in ICU and ED | 47 | – | MBI-HSS | Low: 59% Moderate: 30% High: 11% |
| Alsulimani et al. (2021)16 | KSA | HCWs | 646 | June 2020–August 2020 | CBI (work-related part) | 75.1% (95% CI 0.71–0.78) |
| Cravero et al. (2020)41 | International (including KSA) | Residents and fellows | 76 (KSA only) | 20 April 2020–11 May 2020 | Single item measures of emotional exhaustion and depersonalization | 76% |
Meta regression
Prevalence of anxiety
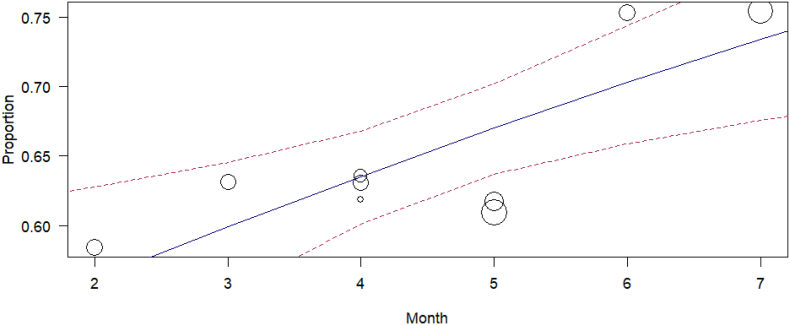
Meta-regression of moderate to severe anxiety using the GAD-7 scale on month of the study revealed positive trend over time with high significance (p = 0.0059) (Figure 10). Neither population nor country of the study were significant when considered as additional moderators.
Figure 10.
Meta-regression of moderate to severe anxiety (GAD-7) on month of study, 2020.
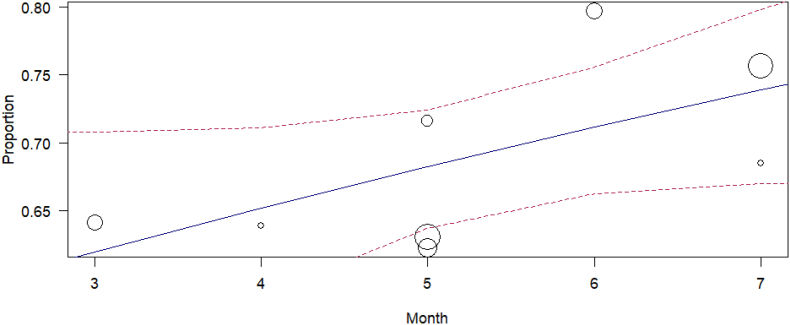
Prevalence of depression
Meta-regression of moderate to severe depression using the PHQ-9 scale on month of the study also revealed a positive trend over time but with borderline significance (p = 0.0762) (Figure 11). As with the anxiety model, neither population nor country of the study were significant when added as moderators.
Figure 11.
Meta-regression of moderate to severe depression (PHQ-9) on month of study, 2020.
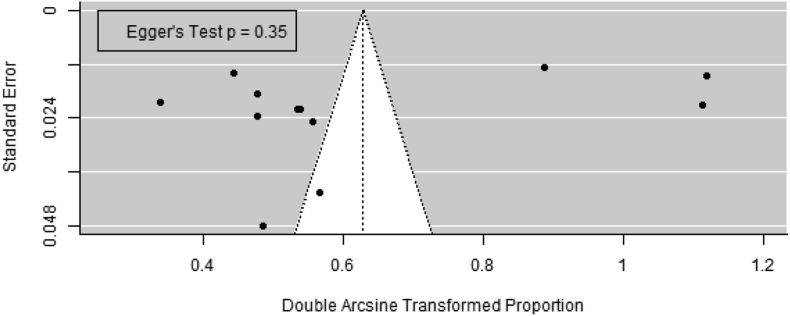
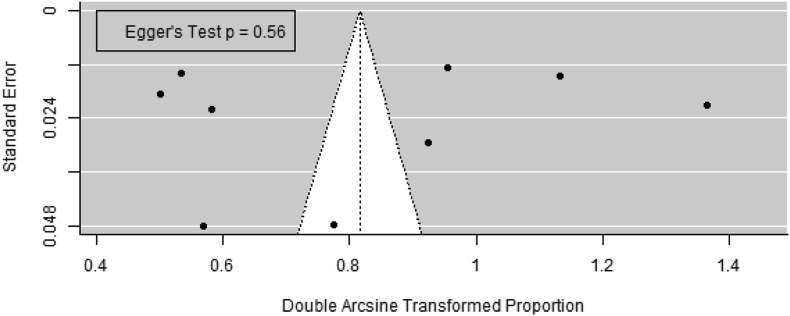
Publication bias
Publication bias was assessed using funnel plots of transformed proportions against standard error. Only GAD-7 for anxiety and PHQ-9 for depression categories with ∼10 studies were assessed.
Despite of the visually apparent unbalanced distributions, the unweighted regression test was not significant for any of the outcomes of interest (moderate to severe anxiety using GAD-7: p = 0.35; and moderate to severe depression using PHQ-9: p = 0.56) (Figure 12, Figure 13).
Figure 12.
Funnel plot for moderate to severe anxiety (GAD-7).
Figure 13.
Funnel plot for moderate to severe depression (PHQ-9).
Discussion
The results of this systematic review and meta-analysis indicate a high prevalence of mental health disorders among HCWs in GCC countries during the COVID-19 pandemic. However, there was marked heterogeneity among the studies; this was most likely due to differences in time, population and settings between the studies. This finding also suggests that better-quality studies are needed in the future.
In the present analysis, all four of the evaluated mental health outcomes (i.e., anxiety, depression, stress, and burnout) showed a wide prevalence range. This could be explained by several factors, such as the time of data collection. For instance, the lowest reported prevalence of anxiety was in a study conducted in February 2020 in KSA before the appearance of the first case in the country.22 Another possible explanation is that different tools and different cutoff points were used to report the prevalence. For example, the lowest prevalence rates of stress using the PSS-10 were reported in two studies that used cutoff points of 25 (36) and 24 (34); these represented the mean scores of the participants. These cutoff points are higher than that used in other studies14 meaning that some of the participants that could be classified as having stress in other studies were not classified as such in these two studies, thus resulting in an underestimated proportion. Different tools may also result in different prevalence rates.42 Furthermore, the differences in the target population and settings may play an important role. Some studies targeted nurses and those working on the frontline. In addition, in many of the studies, the majority of participants were of female gender. These factors were found to be associated with higher rates of mental health disorders during the COVID-19 pandemic.15,17,18,23,26,28,32,40 This high level of heterogeneity between included studies, along with the low number (n < 10) of studies in each category, may have contributed to the discrepancy between non-significant Egger's test results and unbalanced funnel plots.
In comparison to other global systematic reviews conducted between December 2019 and October 2020, our results indicated higher prevalence rates.43, 44, 45, 46 For example, Salari et al. reported the prevalence of anxiety, depression and stress at 25.8% (95% CI: 20.5%, 31.9%), 24.3% (95% CI: 18.2, 31.6%) and 45% (95% CI: 24.3%, 67.5%), respectively.45 A recent systematic review on the prevalence of mental health disorders among the general population in KSA during the pandemic reported lower rates than those found in our study. The reported rates were 20% (95% CI: 16%, 24%), 30% (95% CI: 22%, 38%) and 29% (95% CI: 11%, 47%) for anxiety, depression, and stress, respectively.47 This discordance between previously reported data and the present findings could be due to the different search time frame.
The positive time trend for the proportion of anxiety and depression aligns with the increased impact of the pandemic GCC populations over time. This further validates the results of this review.
The limitations of the present study are as follows. First, due to the nature of our cross-sectional design, it remains unclear as to whether the evaluated mental health outcomes were pre-existent; thus, a causal relationship between the high prevalence of mental health disorders and the pandemic cannot be established. Several studies that were conducted in healthcare settings before the pandemic reported high prevalence rates among the participants. For example, Alshardi and Farahat (2019) found that 40% of medical residents in Jeddah, KSA reported moderate to severe depression.48 A study among ICU nurses in KSA reported a prevalence of 88% for moderate to severe stress.49 Another study in the United Arab Emirates showed that 70% of medical residents experienced burnout.50 However, to the best of our knowledge, this is the first study to review the mental health of HCWs with focus on the GCC region. Other outcomes, such as sleep disturbance, were also found to have a high prevalence, but they were not included in this review. Furthermore, to ensure homogeneity in the study population, healthcare students were not included.
Another limitation of this study is the quality of the analyzed studies, although two quality assessment tools were used to avoid bias. The most common weakness point was the representativeness of the samples. In many studies, sampling was performed by the convenience sampling technique; this may have affected the generalizability of the results. In addition, all studies used self-reported questionnaires for the investigated outcomes; however, as explained by some authors, this was due to the restrictions employed during that period, such as social distancing.16
A further limitation is that, in some studies, there was unequal representation of genders, with the majority of participants being female; this may simply be due to the fact that the majority of HCWs are females, as reported by Alshekaili et al.33 Moreover, most of the included studies were conducted in KSA, followed by Oman; no studies were conducted in Qatar or the United Arab Emirates. Consequently, generalizing the results to these countries should be taken cautiously.
Furthermore, due to high publication rates during the pandemic,51 there could be studies that were not included in our review. For example, a study that was published after our search timeframe, conducted from April 2020 to June 2020, included a total of 554 HCWs from all over the KSA and reported a prevalence of 52% for depression.52
Finally, an important limitation is that all studies were based on screening tools. Many of these tools can provide dimensional but not categorical classification. For example, the DASS and GAD-7 can detect different anxiety disorders including panic disorder, social anxiety and generalized anxiety disorder.53,54 Therefore, specifying an outcome depending only on these tools could be difficult.
Conclusion
This study found a high prevalence of mental health disorders including anxiety, depression, and stress among HCWs in GCC countries during the pandemic which increased over time; however, it also points to the need for higher-quality studies with better sampling methods. Moreover, future studies should focus on studying the developing trends as new factors are evolving, such as the development of effective vaccines and the emergence of new variants. More importantly, particular focus should be paid on developing effective measures to reduce the burden of these mental health disorders among HCWs.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Not applicable.
Authors contributions
RA developed the search strategy, performed the search, screened the articles, reviewed full text articles, extracted data, assessed the risk of bias, and wrote the initial and final drafts. AA contributed to the search strategy, screened the articles, designed and performed the meta-analysis, reviewed the initial and final drafts, and provided supervision. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
We would like to acknowledge Naike Wang for his comprehensive publication on meta-analysis of proportions in R which informed our work.55 Also, we owe thanks to the reviewers who had invaluable input into the text. Finally, we would like to acknowledge Elsevier Language Editing Services for editing and reviewing this paper for English language.
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtumed.2022.07.014.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Traylor A.M., Tannenbaum S.I., Thomas E.J., Salas E. Helping healthcare teams save lives during COVID-19: insights and countermeasures from team science. Am Psychol. 2021;76:1–13. doi: 10.1037/amp0000750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Hage W., Hingray C., Lemogne C., Yrondi A., Brunault P., Bienvenu T., et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks? Encephale. 2020;46:S73–S80. doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Secretariat General of the Gulf Cooperation Council . 2021. About GCC – Member states.https://www.gcc-sg.org/en-us/AboutGCC/MemberStates/Pages/Home.aspx [Google Scholar]
- 5.GCC Statistical Center . 2021. COVID 19 in GCC countries.https://www.gccstat.org/en/statistic/publications/covid-19 [Google Scholar]
- 6.GCC Statistical Center . 2021. Atlas of GCC statistics.https://www.gccstat.org/en/statistic/publications/atlas-of-gcc-statistics [Google Scholar]
- 7.GCC Statistical Center . 2020. Population.https://www.gccstat.org/en/statistic/statistics/population [Google Scholar]
- 8.Secretariat General of the Gulf Cooperation Council . 2021. About GCC – objectives.http://gcc-sg.org/en-us/AboutGCC/Pages/StartingPointsAndGoals.asp [Google Scholar]
- 9.Gulf Health Council . 2020. The GCC countries face COVID-19.http://www.ghc.sa/ar-sa/Documents/The GCC Countries Face COVID-19.pdf [Google Scholar]
- 10.GCC Statistical Center . 2021. A year of COVID-19 in GCC.https://www.gccstat.org/images/gccstat/docman/publications/A year of COVID-19 in GCC.pdf [Google Scholar]
- 11.Herzog R., Álvarez-Pasquin M.J., Díaz C., Del Barrio J.L., Estrada J.M., Gil Á. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Joanna Briggs Institute . 2017. Critical appraisal tools for use in JBI systematic reviews - checklist for prevalence studies.https://jbi.global/critical-appraisal-tools [Google Scholar]
- 13.Abu-Snieneh H.M. Psychological factors associated with the spread of Coronavirus disease 2019 (COVID-19) among nurses working in health sectors in KSA. Perspect Psychiatr Care. 2021;57:1399–1408. doi: 10.1111/ppc.12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alahmadi A.S., Alhatlan H.M., Bin Helayel H., Khandekar R., Al Habash A., Al-Shahwan S. Residents' perceived impact of COVID-19 on Saudi ophthalmology training programs-a survey. Clin Ophthalmol. 2020;14:3755–3761. doi: 10.2147/OPTH.S283073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Ammari M., Sultana K., Thomas A., Al Swaidan L., Al Harthi N. Mental health outcomes amongst health care workers during COVID 19 pandemic in KSA. Front Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.619540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alamri H.S., Algarni A., Shehata S.F., Al Bshabshe A., Alshehri N.N., ALAsiri A.M., et al. Prevalence of depression, anxiety, and stress among the general population in KSA during Covid-19 pandemic. Int J Environ Res Public Health. 2020;17:9183. doi: 10.3390/ijerph17249183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alanazi K.H., bin Saleh G.M., AlEidi S.M., AlHarbi M.A., Hathout H.M. Prevalence and risk factors of burnout among healthcare professionals during COVID-19 pandemic - KSA. Am J Public Health Res. 2021;9:18–27. doi: 10.12691/ajphr-9-1-3. [DOI] [Google Scholar]
- 18.AlAteeq D.A., Aljhani S., Althiyabi I., Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in KSA. J Infect Public Health. 2020;13:1432–1437. doi: 10.1016/j.jiph.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aldarmasi M.A., Alghamdi A.H. Factors influencing stress perception among healthcare workers during the coronavirus pandemic: a multi-centric cross-sectional study. Int J Med Res Health Sci. 2021;10:142–149. [Google Scholar]
- 20.Alenazi T.H., BinDhim N.F., Alenazi M.H., Tamim H., Almagrabi R.S., Aljohani S.M., et al. Prevalence and predictors of anxiety among healthcare workers in KSA during the COVID-19 pandemic. J Infect Public Health. 2020;13:1645–1651. doi: 10.1016/j.jiph.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Almater A.I., Tobaigy M.F., Younis A.S., Alaqeel M.K., Abouammoh M.A. Effect of 2019 coronavirus pandemic on ophthalmologists practicing in KSA: a psychological health assessment. Middle East Afr J Ophthalmol. 2020;27:79–85. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almubark R., Almaleh Y., BinDhim N., Almedaini M., Almutairi A., Alqahtani S. Monitoring burnout in the intensive care unit and emergency department during the COVID-19 pandemic: the Saudi Arabian experience. Middle East J Nurs. 2020;14:12–21. doi: 10.5742/MEJN2020.93790. [DOI] [Google Scholar]
- 23.Alsaywid B., Housawi A., Lytras M., Halabi H., Abuzenada M., Alhaidar S.A., et al. Residents' training in COVID-19 pandemic times: an integrated survey of educational process, institutional support, anxiety and depression by the Saudi Commission for Health Specialties (SCFHS) Sustainability. 2020;12:10530. doi: 10.3390/su122410530. [DOI] [Google Scholar]
- 24.Alsulimani L.K., Farhat A.M., Borah R.A., AlKhalifah J.A., Alyaseen S.M., Alghamdi S.M., et al. Health care worker burnout during the COVID-19 pandemic: a cross-sectional survey study in KSA. Saudi Med J. 2021;42:306–314. doi: 10.15537/smj.2021.42.3.20200812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alzaid E.H., Alsaad S.S., Alshakhis N., Albagshi D., Albesher R., Aloqaili M. Prevalence of COVID-19-related anxiety among healthcare workers: a cross-sectional study. J Fam Med Prim Care. 2020;9:4904–4910. doi: 10.4103/jfmpc.jfmpc_674_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Balay-Odao E.M., Alquwez N., Inocian E.P., Alotaibi R.S. Hospital preparedness, resilience, and psychological burden among clinical nurses in addressing the COVID-19 crisis in Riyadh, KSA. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.573932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joseph R., Lucca J.M., Alshayban D., Alshehry Y.A. The immediate psychological response of the general population in KSA during COVID-19 pandemic: a cross-sectional study. J Infect Public Health. 2021;14:276–283. doi: 10.1016/j.jiph.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shalaby H.A., Baroom N., Obaid R.A., Raboe E. Factors associated with psychological outcomes of healthcare workers during the COVID-19 pandemic and its effects on quality of life. J Health Med Nurs. 2021;6:23–41. doi: 10.47604/jhmn.1259. [DOI] [Google Scholar]
- 29.Qasem Surrati A.M., Asad Mansuri F.M., Ayadh Alihabi A.A. Psychological impact of the COVID-19 pandemic on health care workers. J Taibah Univ Med Sci. 2020;15:536–543. doi: 10.1016/j.jtumed.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Temsah M.H., Al-Sohime F., Alamro N., Al-Eyadhy A., Al-Hasan K., Jamal A., et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. 2020;13:877–882. doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al Mahyijari N., Badahdah A., Khamis F. The psychological impacts of COVID-19: a study of frontline physicians and nurses in the Arab world. Ir J Psychol Med. 2020;38:186–191. doi: 10.1017/ipm.2020.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al Maqbali M., Al Khadhuri J. Psychological impact of the coronavirus 2019 (COVID-19) pandemic on nurses. Jpn J Nurs Sci. 2021 doi: 10.1111/jjns.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alshekaili M., Hassan W., Al Said N., Al Sulaimani F., Jayapal S.K., Al-Mawali A., et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Badahdah A., Khamis F., Al Mahyijari N., Al Balushi M., Al Hatmi H., Al Salmi I., et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry. 2021;67:90–95. doi: 10.1177/0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jahan F., Al Zadjali N.M.I., Siddiqui M., Al Moqbali S.A.M. Mental health status among health care workers in primary care exposed to COVID-19 pandemic in North Batinah, Oman. Eur J Mol Clin Med. 2021;8:1268–1280. [Google Scholar]
- 36.Khamis F., Al Mahyijari N., Al Lawati F., Badahdah A.M. The mental health of female physicians and nurses in Oman during the COVID-19 pandemic. Oman Med J. 2020;35 doi: 10.5001/omj.2020.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alsairafi Z., Naser A.Y., Alsaleh F.M., Awad A., Jalal Z. Mental health status of healthcare professionals and students of health sciences faculties in Kuwait during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:2203. doi: 10.3390/ijerph18042203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burhamah W., AlKhayyat A., Oroszlányová M., AlKenane A., Almansouri A., Behbehani M., et al. The psychological burden of the COVID-19 pandemic and associated lockdown measures: experience from 4000 participants. J Affect Disord. 2020;277:977–985. doi: 10.1016/j.jad.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jahrami H., BaHammam A.S., AlGahtani H., Ebrahim A., Faris M., AlEid K., et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25:503–511. doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arafa A., Mohammed Z., Mahmoud O., Elshazley M., Ewis A. Depressed, anxious, and stressed: what have healthcare workers on the frontlines in Egypt and KSA experienced during the COVID-19 pandemic? J Affect Disord. 2021;278:365–371. doi: 10.1016/j.jad.2020.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cravero A.L., Kim N.J., Feld L.D., Berry K., Rabiee A., Bazarbashi N., et al. Impact of exposure to patients with COVID-19 on residents and fellows: an international survey of 1420 trainees. Postgrad Med J. 2021;97:706–715. doi: 10.1136/postgradmedj-2020-138789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clover K., Lambert S.D., Oldmeadow C., Britton B., King M.T., Mitchell A.J., et al. Apples to apples? Comparison of the measurement properties of hospital anxiety and depression-anxiety subscale (HADS-A), depression, anxiety and stress scale-anxiety subscale (DASS-A), and generalised anxiety disorder (GAD-7) scale in an oncology setting using rasch analysis and diagnostic accuracy statistics. Curr Psychol. 2020 doi: 10.1007/s12144-020-00906-x. [DOI] [Google Scholar]
- 43.Sanghera J., Pattani N., Hashmi Y., Varley K.F., Cheruvu M.S., Bradley A., et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. 2020;62 doi: 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vizheh M., Qorbani M., Arzaghi S.M., Muhidin S., Javanmard Z., Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. 2020;19:1–12. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18:100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al Maqbali M., Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. 2021;141 doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alzahrani F., Alshahrani N.Z., Abu Sabah A., Zarbah A., Abu Sabah S., Mamun M.A. Prevalence and factors associated with mental health problems in Saudi general population during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. PsyCh J. 2022;11:18–29. doi: 10.1002/pchj.516. [DOI] [PubMed] [Google Scholar]
- 48.Alshardi A., Farahat F. Prevalence and predictors of depression among medical residents in Western KSA. J Clin Psychol Med Settings. 2020;27:746–752. doi: 10.1007/s10880-019-09667-7. [DOI] [PubMed] [Google Scholar]
- 49.Alharbi H., Alshehry A. Perceived stress and coping strategies among ICU nurses in government tertiary hospitals in KSA: a cross-sectional study. Ann Saudi Med. 2019;39:48–55. doi: 10.5144/0256-4947.2019.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Faizi N., Kazmi S. Universal health coverage - there is more to it than meets the eye. J Fam Med Prim Care. 2017;6:169–170. doi: 10.4103/jfmpc.jfmpc_13_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Putman M.S., Ruderman E.M., Niforatos J.D. Publication rate and journal review time of COVID-19-related research. Mayo Clin Proc. 2020;95:2290–2291. doi: 10.1016/j.mayocp.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.ALGhasab N.S., ALJadani A.H., ALMesned S.S., Hersi A.S. Depression among physicians and other medical employees involved in the COVID-19 outbreak: a cross-sectional study. Medicine (Baltimore) 2021;100 doi: 10.1097/MD.0000000000025290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tran T.D., Tran T., Fisher J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatr. 2013 Jan;13:24. doi: 10.1186/1471-244X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007 Mar;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 55.Wang N. 2018. How to conduct a meta-analysis of proportions in R: a comprehensive tutorial. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.