Abstract
Objectives
We sought to assess if a state-wide lockdown implemented due to COVID-19 was associated with increased odds of being a potentially avoidable transfer (PAT).
Methods
We conducted a retrospective observational analysis using hospital administrative data of interfacility ED-to-ED transfers to a single, quaternary care adult ED after “Safer at Home” orders were issued March 23rd, 2020 in [Blinded for submission]. Using the PAT classification to identify transfers rapidly discharged from the ED or hospital and may not require in-person care, we used a multivariable logistic regression model to examine the association of the lockdown order with odds of a transfer being a PAT. We compared the period January 1, 2018 to March 23, 2020 with March 24, 2020 to September 30, 2020, adjusting for seasonality, patient, and situational factors.
Results
There were 20,978 ED-to-ED transfers from during this period that were eligible and 4806 (23%) that met PAT criteria. While the first month post-lockdown saw a decrease in PATs (28%), this was not sustained. In the multivariable model there was a significant seasonal effect; May through September had the highest number of transfers as well as PATs. After adjusting for seasonality, the lockdown was not associated with PATs (adjusted odds ratio [aOR] 0.99, 95% CI 0.2, 5.2) and PATs decreased over time.
Conclusions
We did not find an effect of the COVID-19 lockdown on PATs though there was a considerable seasonal effect and an overall downward trend in PATs over time.
Keywords: Transfers, ED, COVID-19, Telehealth
Abbreviations: CI, Confidence Interval; PAT, potentially avoidable transfer
1. Introduction
Emergent interfacility transfers occur as a means to access specialty care but can be disruptive to patients, families, and staff [1]. There is wide variability in the practices of transferring facilities. The Agency for Healthcare Research and Quality's (AHRQ) HCUPNet, estimates that in 2016 there were nearly 2.3 million ED transfers and the number of transfers has nearly doubled since 2006 [2]. While transfers enable patients to access specialty care that otherwise might not be available to them, they are also associated with increased length of stay, costs, and inpatient mortality, even after adjusting for patient characteristics and mortality risk [3]. They also can result in a significant disruption into ED workflows and operations [1,4].
Prior work from [Blinded] and others demonstrated nearly 1-in-4, may be “potentially avoidable” because they are rapidly discharged from the ED or the hospital (if admitted) [[4], [5], [6]]. Called “potentially avoidable transfers” (PATs), such transfers are defined as either discharged from the ED, or admitted for <24 h without a specialty procedure. Such transfers may be amenable to alternative means of care (e.g., telehealth), obviating the need for physical transfer and easing the burden on already crowded EDs [7]. A systematic review of telehealth for neurosurgical patients, focused specifically on neurotrauma and emergent neurological conditions, suggested that the use of telemedicine in emergent settings facilitated safe and feasible methods of increasing access to neurosurgical care [8].
The COVID-19 pandemic substantially impacted U.S. healthcare. Some studies found a nearly 42% reduction in ED visits when comparing volumes early in the pandemic to the same time period a year earlier [9,10].
While prior work demonstrated reduced emergency transfer volume for patients with acute stroke and trauma during the pandemic, the broader impact on general ED-to-ED interfacility transfers, specifically in the US, is not known [[11], [12], [13]]. Further, cognitive psychology suggests that stress may adversely affect decision-making [14]. Lower workload is associated with improved decision-making when prescribing opioids and admitting [15,16]. Locally, during the pandemic we identified that ED stroke activations were more likely to be diagnosed with acute ischemic stroke. Thus, we sought to examine the COVID-19 pandemic as a system stressor rather than disease-focused and to examine all interfacility ED-to-ED transfers during this pandemic period. We hypothesized that the proportion of transfers meeting the PAT definition would be reduced given the lower ED volumes and overall stress imposed on external EDs.
2. Methods
We conducted a retrospective observational analysis using hospital electronic administrative data of all interfacility transfers to a single quaternary care facility's ED – [Blinded for manuscript submission]. XXX is a major receiving center in [Region]–the region's only Level 1 trauma center with a catchment of approximately 65,000 mile2. To examine broader trends in interfacility transfers, we included transfers that occurred between January 1, 2018 and September 30, 2020. Time periods prior to January 2018 were excluded as a new electronic health record was implemented during this time, replacing the software previously used by our facility.
Our timeframe for analysis included the period before and after Safer-at-Home orders were issued by the XXX Health Department on March 23, 2020, restricting the movement and activities of people in XXX to reduce the spread of COVID-19 [17]. We used the time leading up to the issuance of the Safer-at-Home order to establish the baseline in transfer patterns and trends. These orders ran through the end of the study period when the mandate officially expired and a majority of surrounding counties re-opened (not including the county of the receiving hospital). For reference, Lockdown for all counties in the state continued until April 30th when 89/95 counties re-opened with advancement plans. COVID-19 daily new cases in the state over the lockdown remained low at an average of 271 per day [18].
Our primary outcome was an ED-to-ED interfacility transfer that met the PAT definition; either discharged from the ED or an inpatient/observation length of stay <24 h without a specialty procedure [4,6]. Our key independent variable was the time period, classified as before the COVID-19 Stay-at-Home order versus after the order. We constructed a multivariable logistic regression model to examine whether this lockdown period was associated with increased odds of transfers being a PAT [5]. Covariates included seasonality, duration of time since start of the study, patient factors and facility characteristics. Patient factors included demographics (age, sex, insurance, race), situational (arrival during the week, arrival during non-business hours, mode of arrival, acuity at arrival) and clinical diagnostic group as determined by AHRQ's Clinical Classification Software (CCS) [2]. Facility characteristics included transferring hospital type (urban versus rural).
Our objective was to assess if transfers during the lockdown had higher odds of being a PAT. We sought to examine COVID-19 as a system stressor (one which dramatically affected ED volumes) and how this decline in patients affected PATs. To ensure preservation of all observations we applied a single value imputation using the mode for all independent variables as necessary. Since all patients are eligible for Medicare at age 65, we planned to include an interaction term between age and insurance status. We sought to obtain 6 months of data after the shutdown to capture immediate trends. This timeframe was used as a common timeframe to evaluate the sustainability of an intervention. Electronic data abstraction was conducted by a study team member who was aware of the intended study outcomes but did not conduct the analyses.
3. Results
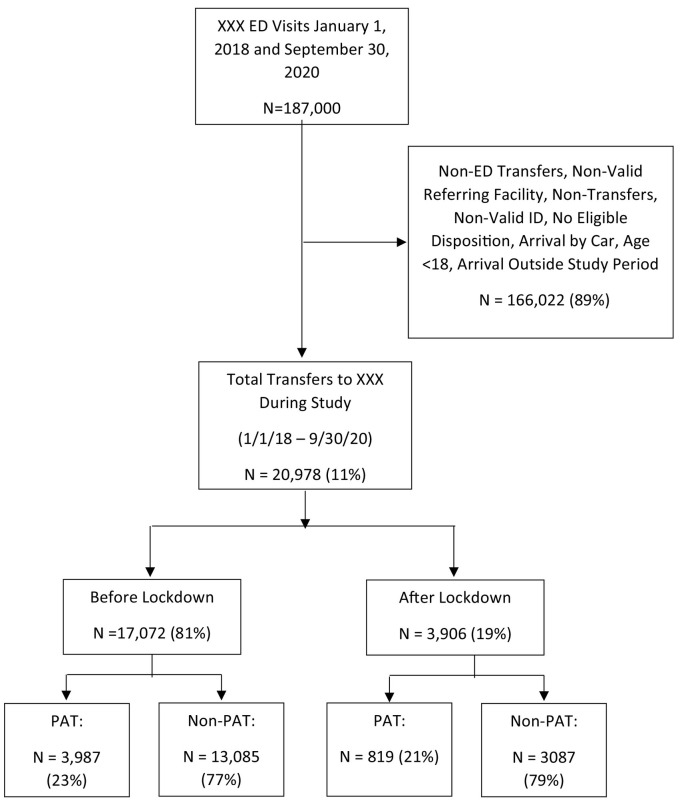
From the original review of our EHR in January 1, 2018 through September 30, 2020, we identified 187,000 ED visits. After applying our inclusion/exclusion criteria, we identified 20,978 transfers during our study period that met eligibility criteria. Among these, 3906 (18.6%) occurred after the Safer-at-Home order. A CONSORT diagram of our study population can be seen in Fig. 1 .
Fig. 1.
CONSORT Diagram of patient cohort definition.
As seen in Table 1 , our study population was more likely to be white males over 65 and have Medicare as their primary insurer. Patients were most likely to arrive during non-business hours via ground ambulance. Among PATs, transfers were younger (median age of 46, interquartile range [IQR] 31.5, 61.8) years compared with non-PATs (58.7 years, [IQR] 43.3, 70.8) and were more likely to be uninsured (20.2% vs. 9%). Among transferred patients, the three most common diagnostic groups were for injury codes and these transfers accounted for a higher proportion of PATs vs. non-PATs (49% vs. 31%). In the 7 months post-lockdown, there was an overall downward trend in the number of PATs. However, this trend was a continuation of the period between 2018 and 2020. Additionally, over these three years, the top five referring facilities (by number of transfers) consistently maintained PAT rates between 27% and 32% – higher than the median.
Table 1.
Patient Characteristics from Interfacility Transfers by Potentially Avoidable Transfer (PAT) status.
| Variable | Overall |
Before Lockdown |
After Lockdown |
Difference (95% CI) | |
|---|---|---|---|---|---|
| N = 20,978 | N = 17,072 | N = 3906 | |||
| PAT (%) | Non-PAT | 16,172 (77.1) | 13,085 (76.6) | 3087 (79.0) | −0.02 (−0.04, −0.01)b |
| PAT | 4806 (22.9) | 3987 (23.4) | 819 (21.0) | 0.02 (0.01, 0.04)b |
|
| Age (median [IQR]) | 56.3 [39.7, 69.2] |
56.4 [39.9, 69.5] | 55.9 [39.1, 68.2] | 0.95 (0.27, 1.63)a |
|
| Sex (%) | Male | 11,844 (56.5) | 9553 (56.0) | 2291 (58.7) | −0.03 ( −0.04, −0.01)b |
| Female | 9134 (43.5) | 7519 (44.0) | 1615 (41.3) | 0.03 (0.01, 0.04)b |
|
| Race Group (%) | White | 17,285 (82.4) | 14,130 (82.8) | 3155 (80.8) | 0.02 (0.01, 0.03)b |
| African American | 2727 (13.0) | 2222 (13.0) | 505 (12.9) | 0 (−0.01, 0.01)b |
|
| Other | 966 (4.6) | 720 (4.2) | 246 (6.3) | −0.02 (−0.03, −0.01)b |
|
| Point of Origin (%) | Hospital (Acute Care Facility) | 17,227 (82.1) | 13,649 (79.9) | 3578 (91.6) | −0.12 (−0.13, −0.11)b |
| Non-Healthcare Facility | 3751 (17.9) | 3423 (20.1) | 328 (8.4) | 0.12 (0.11, 0.13)b |
|
| Insurance Coverage (%) | Insured | 18,558 (88.5) | 15,190 (89.0) | 3368 (86.2) | 0.03 (0.02, 0.04)b |
| Uninsured | 2420 (11.5) | 1882 (11.0) | 538 (13.8) | −0.03 (−0.04, −0.02)b |
|
| Mode of Transport (%) | Ambulance | 17,608 (83.9) | 14,409 (84.4) | 3199 (81.9) | 0.03 (0.01, 0.04)b |
| Medical Flight | 2657 (12.7) | 2079 (12.2) | 578 (14.8) | −0.03 (−0.04, −0.01)b |
|
| Other | 606 (2.9) | 535 (3.1) | 71 (1.8) | 0.01 (0.01, 0.02)b |
|
| NA | 107 (0.5) | 49 (0.3) | 58 (1.5) | ||
| Patient Stability (%) | Systolic BP ≥ 90 mmHg | 13,474 (64.2) | 13,474 (78.9) | 0 (0.0) | 0.79 (0.78, 0.8)b |
| Systolic BP < 90 mmHg | 269 (1.3) | 269 (1.6) | 0 (0.0) | 0.02 (0.01, 0.02)b |
|
| Unknown | 7235 (34.5) | 3329 (19.5) | 3906 (100.0) | ||
| Transferring Hospital Type (%) | Urban | 10,644 (50.7) | 8736 (51.2) | 1908 (48.8) | 0.02 (0.01, 0.04)b |
| Rural | 10,334 (49.3) | 8336 (48.8) | 1998 (51.2) | −0.02 (−0.04, −0.01)b |
|
| Travel Distance (median [IQR]) | 59.0 [32.0, 95.0] |
59.0 [32.0, 93.0] | 65.0 [32.0, 101.0] | 0 (−4, 0)a |
|
| Business Hour (%) | Business Hours | 6049 (28.8) | 4982 (29.2) | 1067 (27.3) | 0.02 (0, 0.03)b |
| Non-Business Hours | 14,929 (71.2) | 12,090 (70.8) | 2839 (72.7) | −0.02 (−0.03, 0)b |
|
| Acuity, collapsed (%) | 1-Immediate | 526 (2.5) | 419 (2.5) | 107 (2.7) | 0 (−0.01, 0)b |
| 2-Emergent | 8577 (40.9) | 7053 (41.3) | 1524 (39.0) | 0.02 (0.01, 0.04)b |
|
| 3–5 Urgent to Non-Urgent | 11,784 (56.2) | 9526 (55.8) | 2258 (57.8) | 0.56 (0.55, 0.57)b |
|
| Unknown | 91 (0.4) | 74 (0.4) | 17 (0.4) | 0 (0,0)b |
|
| CCS Categories (%) | Symptoms, Not Classified | 1522 (7.3) | 1242 (7.3) | 280 (7.2) | 0 (−0.01, 0.01)b |
| Injury | 7307 (34.8) | 5778 (33.8) | 1529 (39.1) | −0.05 (−0.07, −0.04)b |
|
| Digestive | 2653 (12.6) | 2229 (13.1) | 424 (10.9) | 0.02 (0.01, 0.03)b |
|
| Circulatory | 2530 (12.1) | 2071 (12.1) | 459 (11.8) | 0 (−0.01, 0.02)b |
|
| Others | 4926 (23.5) | 4017 (23.5) | 909 (23.3) | 0 (−0.01, 0.02)b |
|
| ED Disposition Status (%) | Discharge | 3588 (17.1) | 2995 (17.5) | 593 (15.2) | 0.02 (0.01, 0.04)b |
| Admit | 17,051 (81.3) | 13,822 (81.0) | 3229 (82.7) | −0.02 (−0.03, 0)b |
|
| Other | 339 (1.6) | 255 (1.5) | 84 (2.2) | −0.01 (−0.01, 0)b |
|
| Specialty Procedure (%) | No | 15,234 (72.6) | 12,473 (73.1) | 2761 (70.7) | 0.02 (0.01, 0.04)b |
| Yes | 5744 (27.4) | 4599 (26.9) | 1145 (29.3) | −0.02 (−0.04, −0.01)b |
Wilcoxon.
Risk difference.
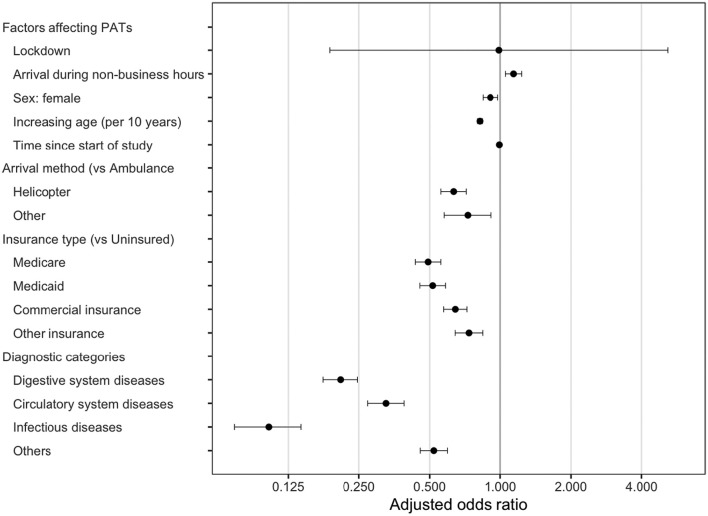
After accounting for seasonality in our multivariable analysis, the likelihood of a transfer being a PAT did not change after lockdown (adjusted odds ratio 1.0, 95%CI 0.2, 5.2). While the proportion of all PATs was decreasing prior to the lockdown, we did not see a change in the likelihood of being a PAT. The remainder of covariates are in a Forest Plot (Fig. 2 ). The following factors were associated with higher odds of being a PAT: lack of insurance (vs. commercial insurance) and arrival during non-business hours. The following factors were associated with lower odds of being a PAT: female sex, increasing age (for every 10 years), specific diagnostic codes (digestive, infectious, or circulatory conditions), and arrival by means other than ambulance (e.g., helicopter). Of note, there was no effect when we included an age by insurance interaction term to our model.
Fig. 2.
Association of facility and patient characteristics with an ED-to-ED transfer meeting criteria for PAT. Adjusted odds ratios (95% CI) in this forest plot were generated from a single multivariable logistic regression model with each variable displayed included as an independent variable in the model. Factors falling to the RIGHT of the line are associated with increased odds, those falling to the left with decreased odds.
Regarding the seasonal effect where we might account for periods of time with an expected increase or decrease in transfers (e.g., trauma season), there was still a relative decreasing trend in the number of PATs. This is consistent with changes seen before and continuing after the period of interest (Fig. 3 ). Thus, as time went on, the odds of being a PAT decreased, despite the lockdown.
Fig. 3.
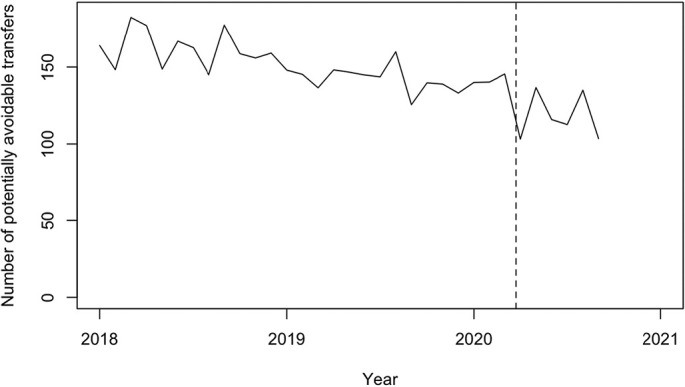
Seasonally adjusted number of PATs per month.
4. Discussion
When examining ED-to-ED interfacility transfers into [City], we found no difference in the likelihood of a transfer being a PATs pre- and post-COVID-19 lockdown. This work makes the following three important contributions: First, the likelihood of these transfers meeting the PAT criteria did not appear affected by the lockdown order, despite the significant declines in overall ED volume. Second, we identified an overall downward trend in PATs that began well before COVID-19. Third, we examine the broader emergency transfer trends in a large catchment area in the Southeast where we identified a significant impact of seasonality on transfer patterns; future work may be warranted to better understand the root cause of such seasonal fluctuations.
Our findings suggest that the issuance of a lockdown order in the [City], in the setting of broader reduction in ED volumes, did not substantially impact transfer patterns. We suspect that this can be partially explained by the relative brevity of adherence to the lockdown order. Further, the lockdown order was applicable to [City], but other counties either did not have such an order or allowed theirs to expire after only one month [19,20]. Of note, uninsured patients were much more likely to be PATs but Medicaid patients were the least likely to be PATs among insured individuals. Medicaid patients are likely to have more comorbidities [21], may be sicker, and therefore have lower odds of being a PAT.
While we use the PAT criteria to identify transfers potentially amenable to alternative forms of care, this definition does not address the appropriateness of these transfers. Events surrounding the transfers themselves, such as the availability of resources and patient and/or clinician preferences at the time of transfer, are unknown. The use of the PAT criteria facilitates the retrospective identification of transfers that may be amenable to other effective means of care (e.g., telehealth) [[22], [23], [24], [25], [26]].
Interestingly, we found that PATs appeared to be decreasing prior to the start of the COVID-19 pandemic and with significant seasonal effects. While we reasoned that the overall decline in ED volumes during the COVID-19 pandemic [9,27] may affect the availability of specialty consultation at referring sites, the decline in PATs began before COVID-19 and was not sustainably affected by the lockdown. We also see that season (i.e. summer months with increased trauma) did significantly affect PATs and that nearly 30% of all transfers and PATs in 2018–2020 occurred from 5 referring institutions, suggesting that telehealth could be targeted [22,25,26].
5. Limitations
This is a retrospective observational design, and the use of the PAT criteria may not reflect the clinical complexity, patient preferences, or immediate availability of the resources involved in the decision-making at transfer. What may be classified as “potentially avoidable” may be an entirely appropriate decision within the context in which the transfer decision was made. However, this framework for looking at transfers has been used elsewhere [5] and provides an opportunity to evaluate what happens with transfers and where there may be opportunities for intervention given the disruptive and costly nature of transfers. In addition, we chose to use arrival emergency severity index (ESI) at the receiving facility as a surrogate of clinical severity and indicator of the severity seen by the receiving hospital. This is considered a limitation as we may have been seeing patients that were resuscitated at their index presentation and, while ultimately a PAT, were completely appropriate transfers. Additionally, this is a relatively limited sample of PATs, as evidenced by the wide confidence interval for lockdown in Fig. 2. A larger sample size would reduce the uncertainty and better define the association with PATs.
Last, this work was limited to a single quaternary care facility in the Southeast and may not reflect the patient population nor transfer practices and occurrence of COVID-19 mitigation efforts that happened in other regions, potentially limiting its generalizability.
6. Conclusions
The likelihood of being a PAT before and after a COVID-19 lockdown was unchanged. However, we identified significant seasonality in ED-to-ED interfacility transfers and a longitudinal reduction in PATs unrelated to the COVID-19 lockdown.
Note: “Seasonally adjusted” refers to the removal of patterns which repeat with a fixed period. The dashed line represents COVID-19 lockdown orders issued on March 23, 2020.
Financial support
Dr. Ward was supported VA ORH-10808 and I01HX003057, R34HL155400, and R21HL140382. REDCap was funded by UL1TR000445 from NCATS/NIH. Ms. Hennessy was also supported by the Vanderbilt Trans-Institutional Programs and a VICTR grant from CTSA (NCATS UL1 TR002243). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CRediT authorship contribution statement
Graham Van Schaik: Writing – review & editing, Writing – original draft, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Wesley H. Self: Writing – review & editing, Supervision, Resources, Methodology, Conceptualization. Cassandra Hennessy: Writing – review & editing, Validation, Methodology, Investigation, Formal analysis, Data curation. Michael J. Ward: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Declaration of Competing Interest
None.
References
- 1.McNaughton C., et al. Rural interfacility emergency department transfers: Framework and qualitative analysis. West J Emerg Med. Jul. 2020;21(4) doi: 10.5811/westjem.2020.3.46059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.HCUPnet HCUPnet. Oct. 30, 2021. https://hcupnetahrq.gov (accessed Oct. 30, 2021)
- 3.Sokol-Hessner L., White A.A., Davis K.F., Herzig S.J., Hohmann S.F. Interhospital transfer patients discharged by academic hospitalists and general internists: characteristics and outcomes: Interhospital transfer patients. J Hosp Med. Apr. 2016;11(4):245–250. doi: 10.1002/jhm.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohr N.M., Wu C., Ward M.J., McNaughton C.D., Richardson K., Kaboli P.J. Potentially avoidable Inter-Facility transfer from Veterans Health Administration emergency departments: A cohort study. BMC Health Serv Res. Feb. 2020;20(1) doi: 10.1186/s12913-020-4956-6. Art. no. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright M.K., Gong W., Hart K., Self W.H., Ward M.J. Association of insurance status with potentially avoidable transfers to an academic emergency department: A retrospective observational study. J Am Coll Emerg Phys Open. Apr. 2021;2(2) doi: 10.1002/emp2.12385. Art. no. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohr N.M., Harland K.K., Shane D.M., Miller S.L., Torner J.C. Potentially avoidable pediatric interfacility transfer is a costly burden for rural families: a cohort study. Acad Emerg Med. Aug. 2016;23(8):885–894. doi: 10.1111/acem.12972. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein S.L., et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med Off J Soc Acad Emerg Med. Jan. 2009;16(1) doi: 10.1111/j.1553-2712.2008.00295.x. Art. no. 1. [DOI] [PubMed] [Google Scholar]
- 8.Wright J., et al. A systematic review of telehealth for the delivery of emergent neurosurgical care. J Telemed Telecare. Jun. 2021;27(5):261–268. doi: 10.1177/1357633X211015548. [DOI] [PubMed] [Google Scholar]
- 9.Hartnett K.P. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–may 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.G. M. PhD, S. M. MAE MHSA, N. K. MS Pharm D., A. A. MS, and B. A. Z. MPH MD Hospital utilization during the pandemic: an update. Epic Health Res Network. Oct. 30, 2021 https://ehrn.org/articles/hospital-utilization-during-the-pandemic-an-update (accessed Oct. 30, 2021) [Google Scholar]
- 11.Nogueira R.G., et al. Global impact of COVID-19 on stroke care and IV thrombolysis. Neurology. Jun. 2021;96(23):e2824–e2838. doi: 10.1212/WNL.0000000000011885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelzl C.E., et al. COVID-19 and trauma: how social distancing orders altered the patient population using trauma services during the 2020 pandemic. Trauma Surg Acute Care Open. 2021;6(1) doi: 10.1136/tsaco-2020-000645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schopow N., et al. Central COVID-19 coordination centers in Germany: description, economic evaluation, and systematic review. JMIR Public Health Surveill. Nov. 2021;7(11):e33509. doi: 10.2196/33509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galván A., Rahdar A. The neurobiological effects of stress on adolescent decision making. Neuroscience. Sep. 2013;249:223–231. doi: 10.1016/j.neuroscience.2012.09.074. [DOI] [PubMed] [Google Scholar]
- 15.Gorski J.K., Batt R.J., Otles E., Shah M.N., Hamedani A.G., Patterson B.W. The impact of emergency department census on the decision to admit. Acad Emerg Med. Jan. 2017;24(1):13–21. doi: 10.1111/acem.13103. [DOI] [PubMed] [Google Scholar]
- 16.Ward M.J., Kc D., Jenkins C.A., Liu D., Padaki A., Pines J.M. Emergency department provider and facility variation in opioid prescriptions for discharged patients. Am J Emerg Med. May 2019;37(5):851–858. doi: 10.1016/j.ajem.2018.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Safer At Home Order « Nashville COVID-19 Response https://www.asafenashville.org/safer-at-home-order/ (accessed Feb. 05, 2022)
- 18.Downloadable Datasets https://www.tn.gov/health/cedep/ncov/data/downloadable-datasets.html (accessed Jun. 12, 2022)
- 19.Gov. Lee Issues Guidelines for Restaurants, Retail Stores to Reopen Early Next Week in 89 Counties https://www.tn.gov/governor/news/2020/4/24/gov--lee-issues-guidelines-for-restaurants--retail-stores-to-reopen-early-next-week-in-89-counties.html (accessed Feb. 06, 2022)
- 20.Epi Curves https://www.tn.gov/health/cedep/ncov/data/epi-curves.html (accessed Feb. 06, 2022)
- 21.Chapel J.M., Ritchey M.D., Zhang D., Wang G. Prevalence and medical costs of chronic diseases among adult medicaid beneficiaries. Am J Prev Med. Dec. 2017;53(6):S143–S154. doi: 10.1016/j.amepre.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joseph J., Kennedy M., Nathanson L., Wardlow L., Crowley C., Stuck A. Reducing emergency department transfers from skilled nursing facilities through an emergency physician telemedicine service. West J Emerg Med. Oct. 2020;21(6) doi: 10.5811/westjem.2020.7.46295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. Sep. 2015;2016(12) doi: 10.1002/14651858.CD002098.pub2. Art. no. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paik A.M., Granick M.S., Scott S. Plastic surgery telehealth consultation expedites emergency department treatment. J Telemed Telecare. Feb. 2017;23(2):321–327. doi: 10.1177/1357633X16639459. [DOI] [PubMed] [Google Scholar]
- 25.du Toit M., Malau-Aduli B., Vangaveti V., Sabesan S., Ray R.A. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: a systematic review. J Telemed Telecare. Jan. 2019;25(1):3–16. doi: 10.1177/1357633X17734239. [DOI] [PubMed] [Google Scholar]
- 26.Natafgi N., Shane D.M., Ullrich F., MacKinney A.C., Bell A., Ward M.M. Using tele-emergency to avoid patient transfers in rural emergency departments: an assessment of costs and benefits. J Telemed Telecare. Apr. 2018;24(3):193–201. doi: 10.1177/1357633X17696585. [DOI] [PubMed] [Google Scholar]
- 27.Lee S., Santarelli A., Choi H., Ashurst J. Impact of the COVID-19 pandemic on emergency department transfers to a higher level of care. West J Emerg Med. Jun. 2021;22(3) doi: 10.5811/westjem.2021.3.50907. Art. no. 3. [DOI] [PMC free article] [PubMed] [Google Scholar]