ABSTRACT
The purpose of this study is to evaluate the predictive value of preoperative diagnostic intra-articular injections with formal provocative post-injection functional testing on patient-reported outcomes (PROs) following hip arthroscopy. Patients aged 14–40 with suspected labral pathology and/or femoroacetabular impingement were prospectively enrolled. Patients received a diagnostic intra-articular anesthetic injection then completed a battery of provocative physical function (PF) tests and were asked to rate the percentage of pain improvement. Patients completed PRO surveys preoperatively and up to 2 years postoperatively. PROs were compared between positive and negative injection response groups. Ninety-six patients received a diagnostic injection with provocative functional testing and subsequently underwent hip arthroscopy, 74 reported a positive injection response (≥75% improvement) and 22 reported a negative injection response (<75% improvement). The average postoperative follow-up was 12 months. Both groups experienced significant improvement in PROs postoperatively. A positive injection response was associated with greater improvements in hip outcome score, Non-Arthritic Hip Score, Patient-Reported Outcomes Measurement Information System (PROMIS) pain interference and PROMIS PF at final follow-up compared to a negative injection response. Similar improvements in modified Harris Hip Score, Visual Analog Scale hip pain and PROMIS depression were experienced between groups. These results indicate that diagnostic intra-articular hip anesthetic injection with provocative functional testing may be a valuable predictor of pain and PF following hip arthroscopy. However, patients with negative injection responses still experienced significant clinical improvement in their postoperative outcomes. As such, a negative injection response should not preclude patients from being surgical candidates, but their outcomes may be less predictable.
INTRODUCTION
Hip arthroscopy is increasingly utilized to address intra-articular hip dysfunction, with reports of successful long-term outcomes [1, 2]. Prior to surgical intervention, confidence that intra-articular structures are responsible for pain generation is essential. Multiple sources can contribute to hip pain, which can make an accurate diagnosis a challenge. Improved imaging has allowed for a better understanding of intra-articular pathology; however, this is unable to differentiate between symptomatic and asymptomatic abnormalities [3]. Sometimes an individual’s pain is a product of dynamic motion and not reproducible upon routine clinical exam, further limiting the ability to isolate the pain source. In addition, some athletes may only experience pain with specific provocative maneuvers or higher-level exertion, which can be difficult to reproduce in an examination room with limited space and resources.
Pursuing surgical intervention without confirmation of the pain generator may lead to unnecessary procedures and unrealistic expectations. Diagnostic injections may be helpful when trying to isolate the primary source of hip pain [4–6]. Previous studies dispute the correlation between injection results and surgical outcomes [7–9]. However, studies are limited by variable methodology and assessment of injection response. In addition, taking patients through known provocative functional activities immediately following injection may provide further valuable prognostic information for patients that experience pain with dynamic movements or more strenuous activity.
The purpose of this study is to prospectively evaluate if diagnostic intra-articular anesthetic hip injection with formal provocative post-injection functional testing is predictive of patient-reported outcomes (PROs) following hip arthroscopy. We hypothesize that the relative effectiveness of a diagnostic intra-articular hip injection used in conjunction with a provocative exercise challenge will be predictive of outcomes following arthroscopic hip surgery. Furthermore, we anticipate in cases where a diagnostic injection does not provide symptomatic relief, surgical intervention is less likely to provide improvement in pain and functional outcomes.
MATERIALS AND METHODS
Patient population
This study was approved by our institutional review board. Patients aged 14–40 years with hip pain/dysfunction suspected to be caused by labral pathology and/or femoroacetabular impingement (FAI), who were undergoing a diagnostic intra-articular hip injection and considering arthroscopic intervention were eligible for inclusion. Patients were prospectively enrolled from June 2015 to December 2017. Patients were excluded if they previously underwent surgery on the affected hip, were unable to complete the functional tasks required for testing, had a contraindication to the injection, were undergoing arthroscopic hip surgery as a staged procedure prior to open hip preservation surgery, were not surgical candidates or had significant degenerative changes in the involved hip (Tonnis grade ≥3). Patients that did not ultimately undergo hip arthroscopy or did not complete at least 4 months of postoperative follow-up were subsequently excluded from the analysis.
Diagnostic injection and provocative functional testing
All diagnostic injections were performed by the senior surgeon. A total of 5 cc of 1% lidocaine was injected into the intra-articular space of the affected hip under ultrasound guidance. Following the diagnostic injection (within 30 min), a battery of provocative functional tests was administered by a certified athletic trainer or physical therapist trained in the testing procedure. The testing protocol was developed to simulate the dynamic movements that commonly exacerbate symptoms in this population based upon the investigators’ clinical experience. Provocative testing consisted of five functional tasks, with a 2-min break between each (Fig. 1). After completion of all five tests, patients were taken through any self-reported provocative activities that were not yet performed during the previous functional tests (kicking a soccer ball, dance high kicks, splits, squats, etc.). Immediately after completion of provocative testing, patients were asked to indicate their perceived percentage of symptom improvement compared to pre-injection, with 0% indicating no pain relief and 100% indicating complete resolution of pain.
Fig. 1.
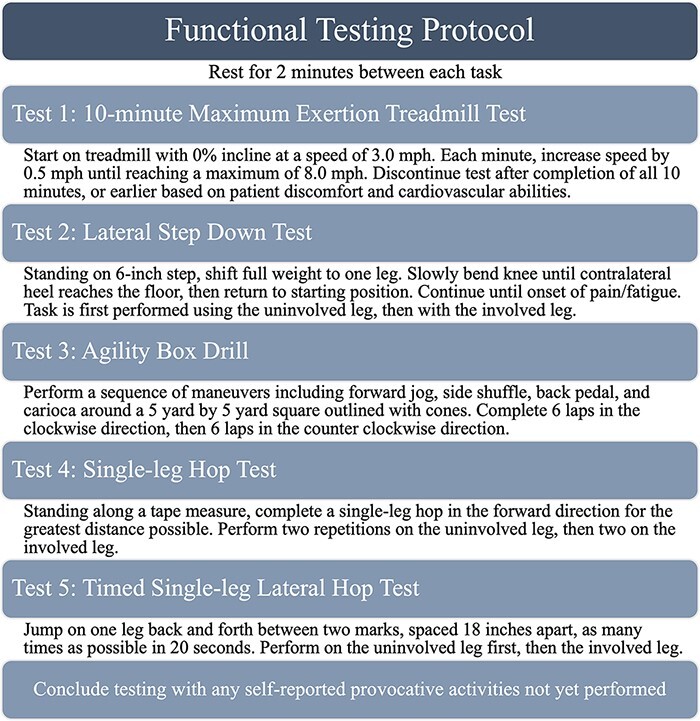
Provocative functional post-injection testing protocol.
Surgical intervention
The results obtained from the diagnostic injection and provocative testing were used quantitatively to inform subsequent discussions between the surgeon and patient about next treatment steps. A specific threshold for a positive or negative response was not utilized while counseling patients on surgical outcomes. The decision to proceed with hip arthroscopy in each case was based upon that patient’s preferences and a combination of imaging findings, physical examination and the clinical judgment of the treating surgeon. All surgeries were performed by a single fellowship-trained hip surgeon. Arthroscopy was performed with the patient in the supine position using the anterolateral peritrochanteric, modified mid-anterior and distal accessory anterolateral portals. Diagnostic arthroscopy was completed and pathology was addressed via chondroplasty, labral debridement/repair, acetabuloplasty, femoroplasty and iliopsoas lengthening, as appropriate.
Clinical outcomes assessment
Baseline characteristics were recorded for each patient including age, sex, body mass index and smoking status. Hip morphology (normal, FAI or borderline dysplasia) was assessed by the senior surgeon based upon preoperative radiographs. PRO surveys were administered preoperatively and at all postoperative appointments, including 2-week, 6-week, 4-month, 1-year and 2-year follow-up visits. Patients completed several surveys including the modified Harris Hip Score (mHHS), hip outcome score (HOS) including the activities of daily living (ADL) and sports-specific (SS) subsets, Non-Arthritic Hip Score (NAHS), Visual Analog Scale (VAS) hip pain score and Patient-Reported Outcomes Measurement Information System (PROMIS) pain interference (PI), physical function (PF) and depression domains. Achievement of the minimum clinically important difference (MCID) and patient acceptable symptom state (PASS) at final follow-up was assessed for each patient using values available in the literature. MCID cutoffs used for improvement in mHHS, HOS-ADL and HOS-SS at final follow-up compared to preoperative scores were 8, 5 and 6, respectively [10]. PASS threshold scores used for mHHS, HOS-ADL and HOS-SS were 74, 87 and 75, respectively [11]. MCID values used for VAS hip pain, PROMIS PI and PROMIS PF were 14.8, 10.9 and 5.1, respectively [12, 13].
Statistical analysis
Statistical analysis was performed using Stata/SE for Windows (StataCorp LP, College Station, TX, USA). Patients were split into two groups based on their perceived response to the injection. A positive response to injection was defined as ≥75% improvement in pain after injection and a negative response was defined as <75% pain relief. Baseline patient characteristics were compared between groups using independent t-tests and chi-squared analyses for continuous and categorical variables, respectively. Paired t-tests were used to determine improvement in PROs between preoperative and postoperative timepoints within each group. Postoperative improvement in PROs was compared between positive and negative response cohorts using independent t-tests. Differences in rates of MCID and PASS achievement at final follow-up were assessed between groups using chi-squared analysis. A P-value of <0.05 was used to determine statistical significance.
RESULTS
A total of 145 patients were prospectively enrolled between 2015 and 2017. Of these, 26 patients elected not to proceed with surgery after the diagnostic injection (10 positive responses and 16 negative responses) and 15 patients withdrew from the study. Additional reasons for exclusion were insufficient postoperative follow-up (n = 5) or incomplete data (n = 3). As such, 96 patients were included in the analysis, 74 (77.1%) with a positive response to injection and 22 (22.9%) with a negative injection response. The average improvement in pain after diagnostic injection among all patients was 81.4% ± 21.7%. The average length of postoperative follow-up was 12 months ± 6 months. Baseline characteristics, including age, sex, body mass index, smoking status and hip morphology, were similar between positive and negative response groups (P > 0.05; Table I).
Table I.
Baseline characteristics by the response to diagnostic injectiona
|
Negative response
(N = 22) |
Positive response
(N = 74) |
P-value b | |
|---|---|---|---|
| Age (Mean ± SD, years) | 21.6 ± 7.1 | 23.3 ± 7.1 | 0.319 |
| Sex (n) | 0.642 | ||
| Female | 63.6% (14) | 68.9% (51) | |
| Male | 36.4% (8) | 31.1% (23) | |
| Body mass index (n) | 0.573 | ||
| Non-obese (<30 kg/m2) | 86.4% (19) | 90.5% (67) | |
| Obese (≥30 kg/m2) | 13.6% (3) | 9.5% (7) | |
| Smoking status (n) | 0.337 | ||
| Non-smoker | 100.0% (22) | 96.0% (71) | |
| Smoker | 0.0% (0) | 4.0% (3) | |
| Hip morphology (n) | 0.994 | ||
| Normal | 9.1% (2) | 9.5% (7) | |
| FAI | 86.4% (19) | 86.5% (64) | |
| Borderline dysplasia | 4.5% (1) | 4.0% (3) |
SD = Standard deviation; FAI = femoroacetabular impingement.
Boldface indicates statistical significance.
P-values calculated using independent t-tests and chi-squared analyses for continuous and categorical variables, respectively.
Patients in both positive and negative response groups experienced an early worsening in mHHS, NAHS and HOS-ADL scores at 2 weeks followed by significant improvements at 4 months and 1 year compared to preoperative values (P < 0.05; Fig. 2). The positive response group reported significantly improved HOS-SS scores at 4 months and 1 year, whereas the negative response group did not. Patients with a positive injection response experienced significantly better improvements in HOS-ADL, HOS-SS and NAHS at 4 months and at final follow-up compared to patients with a negative injection response (P < 0.05 for all). No differences were seen between groups at 2-week and 6-week timepoints, or for mHHS at any timepoint. Table II details the associations between injection response and postoperative improvements in hip-specific PROs.
Fig. 2.

Bar graphs depicting average preoperative and postoperative scores on hip-specific questionnaires including the mHHS (A), NAHS (B) and HOS-ADL (C) and SS (D) subsets for patients with a negative or positive response to injection. (*) indicates a significant difference compared to the preoperative score (P < 0.05).
Table II.
Response to injection association with hip questionnaires
|
Negative response
(N = 22) |
Positive response
(N = 74) |
P-value a b | |
|---|---|---|---|
| mHHS (mean ± SD) | |||
| Preoperative | 60.9 ± 15.2 | 59.9 ± 15.1 | 0.801 |
| 2 week Δ | −26.5 ± 20.4 | −22.2 ± 22.1 | 0.433 |
| 6 week Δ | 11.4 ± 16.3 | 11.9 ± 23.3 | 0.925 |
| 4 month Δ | 20.0 ± 20.0 | 26.5 ± 16.4 | 0.142 |
| Final Δ | 20.7 ± 22.4 | 27.8 ± 17.1 | 0.117 |
| HOS-ADLs (mean ± SD) | |||
| Preoperative | 68.9 ± 15.8 | 63.4 ± 18.1 | 0.197 |
| 2 week Δ | −29.5 ± 25.8 | −25.8 ± 20.8 | 0.502 |
| 6 week Δ | 2.8 ± 19.1 | 10.8 ± 24.4 | 0.178 |
| 4 month Δ | 14.7 ± 25.2 | 25.6 ± 19.1 | 0.039 |
| Final Δ | 16.4 ± 26.0 | 28.6 ± 17.9 | 0.014 |
| HOS-Sports (mean ± SD) | |||
| Preoperative | 56.3 ± 22.9 | 50.4 ± 21.9 | 0.276 |
| 2 week Δ | −39.0 ± 34.9 | −39.0 ± 28.3 | 1.000 |
| 6 week Δ | −23.1 ± 30.0 | −13.1 ± 37.0 | 0.267 |
| 4 month Δ | 5.7 ± 37.1 | 26.5 ± 30.2 | 0.011 |
| Final Δ | 15.2 ± 40.7 | 36.4 ± 23.9 | 0.003 |
| NAHS (mean ± SD) | |||
| Preoperative | 68.0 ± 18.1 | 64.0 ± 17.2 | 0.341 |
| 2 week Δ | −13.9 ± 18.7 | −14.6 ± 18.2 | 0.877 |
| 6 week Δ | 5.0 ± 17.1 | 8.4 ± 19.8 | 0.490 |
| 4 month Δ | 13.0 ± 23.2 | 23.9 ± 16.4 | 0.018 |
| Final Δ | 16.5 ± 21.5 | 26.5 ± 15.3 | 0.017 |
SD = Standard deviation; ADLs = activities of daily living; ∆ = postoperative score − preoperative score; NAHS = Non-Arthritic Hip Score; HOS = hip outcome score; mHHS = modified Harris Hip Score.
P-values calculated for each category using independent t-tests.
Boldface indicates statistical significance.
Patients in both groups experienced worsening in PROMIS PI and PF at 2 weeks, followed by significant improvements at 4 months and 1 year, and significant improvements in VAS hip pain at all postoperative timepoints compared to preoperative values (P < 0.05; Fig. 3). Patients with a positive response to injection experienced a small but significant improvement in PROMIS depression at 6 weeks, 4 months and 1 year, whereas patients with a negative response to injection only experienced this at 4 months. Table III compares postoperative improvements in PROMIS and VAS pain scores between groups. Positive response to injection was associated with greater improvements in PROMIS PI and PF at 4 months and final follow-up compared to a negative injection response (P < 0.05 for all). No differences in PROMIS depression or VAS hip pain were identified between groups at any timepoint.
Fig. 3.
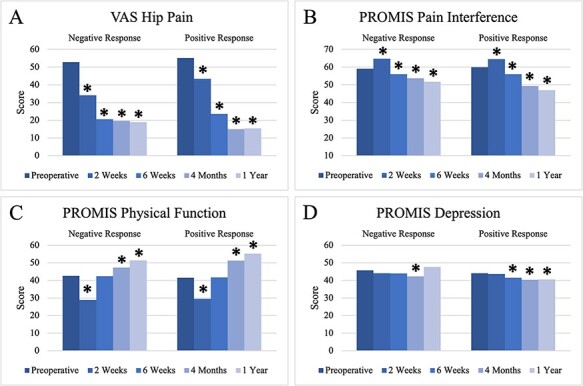
Bar graphs depicting average preoperative and postoperative scores on PRO surveys including the VAS for hip pain (A), PROMIS PI (B), PROMIS PF (C) and PROMIS depression (D) for patients with a negative or positive response to injection. (*) indicates a significant difference compared to the preoperative score (P < 0.05).
Table III.
Response to injection association with PRO
|
Negative response
(N = 22) |
Positive response
(N = 74) |
P-value a b | |
|---|---|---|---|
| VAS pain score (mean ± SD) | |||
| Preoperative | 52.8 ± 22.6 | 55.1 ± 25.3 | 0.702 |
| 2 week Δ | −16.5 ± 23.4 | −12.3 ± 27.7 | 0.537 |
| 6 week Δ | −33.1 ± 25.1 | −31.6 ± 33.1 | 0.856 |
| 4 month Δ | −33.8 ± 24.0 | −39.7 ± 28.5 | 0.398 |
| Final Δ | −33.2 ± 33.2 | −40.5 ± 28.6 | 0.314 |
| PROMIS PI (mean ± SD) | |||
| Preoperative | 59.1 ± 4.3 | 59.9 ± 6.2 | 0.583 |
| 2 week Δ | 5.9 ± 7.1 | 4.6 ± 7.6 | 0.494 |
| 6 week Δ | −3.3 ± 6.2 | −4.0 ± 8.4 | 0.715 |
| 4 month Δ | −5.2 ± 7.8 | −10.6 ± 8.9 | 0.015 |
| Final Δ | −7.5 ± 10.4 | −11.9 ± 8.4 | 0.045 |
| PROMIS PF (mean ± SD) | |||
| Preoperative | 42.6 ± 6.0 | 41.5 ± 5.7 | 0.416 |
| 2 week Δ | −14.4 ± 8.4 | −11.8 ± 7.4 | 0.179 |
| 6 week Δ | 0.1 ± 6.7 | 0.2 ± 7.7 | 0.939 |
| 4 month Δ | 4.1 ± 7.8 | 10.0 ± 10.6 | 0.023 |
| Final Δ | 7.8 ± 11.3 | 13.4 ± 10.7 | 0.037 |
| PROMIS depression (mean ± SD) | |||
| Preoperative | 45.7 ± 9.2 | 44.1 ± 10.1 | 0.518 |
| 2 week Δ | −1.1 ± 7.2 | −0.5 ± 7.5 | 0.724 |
| 6 week Δ | −2.2 ± 7.2 | −2.7 ± 7.1 | 0.773 |
| 4 month Δ | −3.7 ± 7.0 | −4.0 ± 7.9 | 0.884 |
| Final Δ | −0.9 ± 10.2 | −3.5 ± 8.9 | 0.248 |
SD = Standard deviation; VAS = Visual Analog Scale; PROMIS = Patient-Reported Outcomes Measurement Information System; ∆ = postoperative score − preoperative score; PI = pain interference; PF = physical function.
P-values calculated for each category using independent t-tests.
Boldface indicates statistical significance.
Rates of MCID and PASS achievement are compared between injection response groups in Table IV. Patients with a positive response were significantly more likely to reach MCID for HOS-ADLs (91.9% versus 72.7%, P = 0.017), HOS-SS (89.2% versus 68.2%, P = 0.017) and PROMIS PI (52.7% versus 27.3%, P = 0.036) compared to patients with a negative response. Positive response patients also achieved PASS for HOS-SS at a significantly higher rate than negative response patients (79.7% versus 54.6%, P = 0.018). Rates of MCID achievement for mHHS, VAS hip pain and PROMIS PF and rates of PASS achievement for mHHS and HOS-ADLs were similar between groups (P > 0.05).
Table IV.
Clinically relevant outcome achievement at final follow-upa
|
Negative response
(N = 22) |
Positive response
(N = 74) |
P-value b | |
|---|---|---|---|
| mHHS | |||
| MCID (Δ8) | 77.3% (17) | 89.2% (66) | 0.152 |
| PASS (74) | 77.3% (17) | 78.4% (58) | 0.912 |
| HOS-ADLs | |||
| MCID (Δ5) | 72.7% (16) | 91.9% (68) | 0.017 |
| PASS (87) | 68.2% (15) | 79.7% (59) | 0.258 |
| HOS-sports | |||
| MCID (Δ6) | 68.2% (15) | 89.2% (66) | 0.017 |
| PASS (75) | 54.6% (12) | 79.7% (59) | 0.018 |
| VAS Pain Score | |||
| MCID (Δ14.8) | 68.2% (15) | 74.3% (55) | 0.569 |
| PROMIS PI | |||
| MCID (Δ10.9) | 27.3% (6) | 52.7% (39) | 0.036 |
| PROMIS PF | |||
| MCID (Δ5.1) | 59.1% (13) | 77.0% (57) | 0.096 |
MCID = minimum clinically important difference; PASS = patient acceptable symptom state; ADLs = activities of daily living; VAS = Visual Analog Scale; PROMIS = Patient-Reported Outcomes Measurement Information System; HOS = hip outcome score; PI = pain interference; PF = physical function.
Δ = difference between final follow-up score and preoperative score.
Boldface indicates statistical significance.
P-value was calculated for each category using chi-squared analysis.
DISCUSSION
This prospective study assessed the utility of diagnostic intra-articular lidocaine hip injections combined with provocative functional testing for predicting PROs following hip arthroscopy. The results of this study suggest that patients who report 75% pain improvement or more after diagnostic injection and functional testing experience superior postoperative outcomes after hip arthroscopy.
The results of the present study contrast with others in the literature. Krych et al. [8] reviewed 96 patients who underwent hip arthroscopy for labral pathology and received a preoperative injection. Injections were performed by radiologists under fluoroscopic or ultrasound guidance. The injection varied, although most patients received a combination of anesthetic and corticosteroid. Patients were grouped by the percentage of pain relief during the first 24 h after injection (>50% or ≤50% pain relief). The investigators reported no significant differences in postoperative mHHS, HOS-ADL or HOS-SS scores between injection response groups. The difference in results compared to the present study may in part be due to variations in methodology. In the current investigation, the injection was standardized with all procedures performed by a single provider and all patients receiving the same amount and type of anesthetic, without the addition of contrast or a corticosteroid. It has been the experience of the senior author that isolated anesthetic injections, without the dilutional effect of corticosteroid, contrast dye or other agent, maximizes the diagnostic value. This may have improved injection diagnostic accuracy and increased the reliability of injection responses relative to prior investigations. Of note, without the addition of a corticosteroid, the ability to provide a prolonged therapeutic response may be diminished. It may be useful to consider whether a diagnostic or therapeutic effect would be more important when choosing between an isolated anesthetic injection versus an anesthetic plus corticosteroid injection.
Additionally, the current results differ from an investigation by Ladd et al. [9]. They evaluated 93 hip arthroscopy patients who underwent a preoperative anesthetic injection and magnetic resonance arthrogram. Injections were performed by a radiologist under fluoroscopic guidance and contained a mixture of 1% lidocaine, 0.5% ropivacaine, saline and contrast dye. Immediately after injection, patients performed provocative maneuvers to elicit their typical symptoms. Patients were grouped by percent change in pain score before and after injection (60–100% = good/excellent, 30–59% = moderate, <30% = poor). Response to injection was not associated with surgical outcomes as determined by 1-year postoperative mHHS scores. While investigators utilized provocative maneuvers to assist in injection response assessment, this was done in a limited capacity and at the patient’s discretion in the fluoroscopy room. In contrast, the present study employed a unique provocative functional testing protocol, allowing for a more robust and standardized assessment that may enhance the diagnostic value. Sometimes, younger, more athletic populations require a higher level of physical exertion before the pain becomes appreciable. In some cases, miles of running or strenuous agility is necessary to unmask symptoms. Unless these testing conditions are reproduced, a diagnostic injection may produce equivocal results. Even if an athlete returns home and self-tests, these conditions are not standardized and the time taken to return home may limit the injection efficacy. The use of a functional testing protocol immediately following injection may better replicate the conditions that provoke symptoms, enhancing the diagnostic value for these populations. Further investigations may be useful to quantify the ability of this functional testing protocol to provoke symptoms and validate its utility in the assessment of post-injection pain relief.
There is no universally accepted threshold for pain improvement that indicates a positive injection response. As such, variable cutoffs have been utilized among investigations that may contribute to discrepancies in their reported utility. A limited number of patients reported 0% improvement in the present study, suggesting that most will achieve some degree of pain relief and a generalized yes/no assessment may not provide enough detail. A 50% improvement threshold has been used previously but was felt to be too restrictive based upon our clinical experience and given the average improvement of 81.4%. As such, a higher cutoff value of 75% was deemed more appropriate. However, more work is needed to fully characterize a threshold for a positive response to injection.
Although their improvement was not as robust, patients with a negative response to injection still experienced good postoperative outcomes. Despite a negative response, patients reported significant improvements in nearly all PROs at 1 year and a majority achieved MCID/PASS thresholds at final follow-up. In addition, postoperative PROs for this group align with averages reported among general hip arthroscopy populations [14]. This suggests that failure to respond to injection does not necessarily indicate that hip arthroscopy will be unsuccessful. This is valuable information to the treating surgeon and rehabilitation team in establishing reasonable expectations prior to surgery as well as formulating customized perioperative care plans and rehabilitation strategies. While a negative injection response might suggest that intra-articular pathology is not the only pain source, it may still benefit from surgical intervention. Although hip arthroscopy may not fully address all pain sources in these patients, the improved hip mobility after correction of FAI may also indirectly alleviate some pain from extra-articular sources [15]. As such, while a negative injection response should be taken into consideration during treatment decision-making, it should not necessarily preclude patients from being hip arthroscopy candidates.
Limitations
This study has several limitations. First, all injections and surgeries were performed by the same surgeon at a single institution. This may limit the ability to generalize these results to wider patient populations. Second, there was a relatively limited sample size, particularly in the negative injection response group. This limited our ability to stratify patients by specific pathology or investigate various cutoff values for threshold optimization. In addition, this may have limited our statistical power to detect differences in some PROs. Third, an element of selection bias may be present in this study as patients with a negative injection response may have been less likely to undergo hip arthroscopy. In addition, there may have been some inherent bias in the negative response group as their expectations for surgery may have been lower, which may have influenced their perception of postoperative outcomes. Finally, poor compliance with survey completion at the 2-year postoperative follow-up prevented accurate data analysis for that timepoint. However, 2-year follow-up scores were incorporated in the final follow-up analyses when available. In addition, a minority of patients did not complete 1-year follow-up visits if they were doing well by 4–6 months and had no new concerns. While this occurred in similar proportions between groups, this may limit our results at the 1-year timepoint. Further investigation is needed to better understand the association between injection response and long-term postoperative outcomes.
CONCLUSIONS
Patients with a positive response to diagnostic injection (≥75% improvement) experienced greater improvement in PROs. These results indicate that diagnostic intra-articular hip anesthetic injection with provocative functional testing may be a valuable predictor of pain and PF following hip arthroscopy. However, patients with negative injection responses still experienced good postoperative outcomes. As such, a negative injection response should not preclude patients from being surgical candidates, but they should be advised that their outcomes may be less predictable.
ACKNOWLEDGEMENTS
The authors gratefully thank Kiah Mayo for her assistance with data collection and study coordination.
Contributor Information
Brittany E Haws, Department of Orthopaedics, University of Rochester Medical Center, 601 Elmwood Avenue, Box 665, Rochester, NY 14642, USA.
Chad G Condidorio, Department of Orthopaedics, University of Rochester Medical Center, 601 Elmwood Avenue, Box 665, Rochester, NY 14642, USA.
Kelly L Adler, Department of Orthopaedics, University of Rochester Medical Center, 601 Elmwood Avenue, Box 665, Rochester, NY 14642, USA.
Brian D Giordano, Department of Orthopaedics, University of Rochester Medical Center, 601 Elmwood Avenue, Box 665, Rochester, NY 14642, USA.
Data availability
The data underlying this article will be made available upon reasonable request to the corresponding author.
Funding
No funds were received in support of this work.
Conflict of interest statement
B.D.G. has received royalties, consulting fees, speaking fees, and research support from Arthrex.
IRB approval
STUDY00000738.
REFERENCES
- 1. Bedi A, Chen N, Robertson W. et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy 2008; 24: 1135–45. [DOI] [PubMed] [Google Scholar]
- 2. Tejpal T, Shanmugaraj A, Kay J. et al. Historical analysis of the diagnosis and management of femoroacetabular impingement prior to the year 2000: a systematic review. J Hip Preserv Surg 2020; 7: 378–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gerhardt MB, Romero AA, Silvers HJ. et al. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med 2012; 40: 584–8. [DOI] [PubMed] [Google Scholar]
- 4. Yoong P, Guirguis R, Darrah R. et al. Evaluation of ultrasound-guided diagnostic local anaesthetic hip joint injection for osteoarthritis. Skeletal Radiol 2012; 41: 981–5. [DOI] [PubMed] [Google Scholar]
- 5. Kraeutler MJ, Garabekyan T, Fioravanti MJ. et al. Efficacy of a non-image-guided diagnostic hip injection in patients with clinical and radiographic evidence of intra-articular hip pathology. J Hip Preserv Surg 2018; 5: 220–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bray ED, Sherafati M, Cutts CL. et al. The young adult hip: extra-articular causes of hip pain and how to pick the winners. J Hip Preserv Surg 2015; 2: 51–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ayeni OR, Farrokhyar F, Crouch S. et al. Pre-operative intra-articular hip injection as a predictor of short-term outcome following arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2014; 22: 801–5. [DOI] [PubMed] [Google Scholar]
- 8. Krych AJ, Sousa PL, King AH. et al. Intra-articular diagnostic injection exhibits poor predictive value for outcome after hip arthroscopy. Arthroscopy 2016; 32: 1592–600. [DOI] [PubMed] [Google Scholar]
- 9. Ladd LM, Keene JS, Del Rio AM. et al. Correlation between hip arthroscopy outcomes and preoperative anesthetic hip joint injections, MR arthrogram imaging findings, and patient demographic characteristics. AJR Am J Roentgenol 2016; 207: 1062–9. [DOI] [PubMed] [Google Scholar]
- 10. Kemp JL, Collins NJ, Roos EM. et al. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 2013; 41: 2065–73. [DOI] [PubMed] [Google Scholar]
- 11. Chahal J, Van Thiel GS, Mather RC 3rd. et al. The patient acceptable symptomatic state for the modified Harris Hip Score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med 2015; 43: 1844–9. [DOI] [PubMed] [Google Scholar]
- 12. Kuhns BD, Reuter J, Lawton D. et al. Threshold values for success after hip arthroscopy using the patient-reported outcomes measurement information system assessment: determining the minimum clinically important difference and patient acceptable symptomatic state. Am J Sports Med 2020; 48: 3280–7. [DOI] [PubMed] [Google Scholar]
- 13. Beck EC, Nwachukwu BU, Kunze KN. et al. How can we define clinically important improvement in pain scores after hip arthroscopy for femoroacetabular impingement syndrome? Minimum 2-year follow-up study. Am J Sports Med 2019; 47: 3133–40. [DOI] [PubMed] [Google Scholar]
- 14. Levy DM, Kuhns BD, Chahal J. et al. Hip arthroscopy outcomes with respect to patient acceptable symptomatic state and minimal clinically important difference. Arthroscopy 2016; 32: 1877–86. [DOI] [PubMed] [Google Scholar]
- 15. Larson CM. Editorial commentary: ultrasound-guided injection with dynamic assessment could improve outcomes in atypical and revision hip arthroscopy patients: but today, few are trained to hear at such high frequencies. Arthroscopy 2021; 37: 136–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be made available upon reasonable request to the corresponding author.


