ABSTRACT
The aim of this study was to assess injury patterns and risk factors of the acetabular labrum and associated cartilage in patients with femoroacetabular impingement (FAI) versus dysplasia. We retrospectively reviewed 137 patients diagnosed with labral tears and FAI or dysplasia (74 or 63 cases, respectively) through an arthroscopic procedure. Labral and concomitant cartilage injuries were evaluated. Demographics and radiological variables [lateral center-edge angle (LCEA), anterior center-edge angle, acetabular index (AI), acetabular version and alpha angle] were evaluated as risk factors for labral and cartilage injuries. Detachment of acetabular cartilage with intact labro-cartilaginous junction was the most common in dysplasia, whereas cartilage delamination from the labro-cartilaginous junction was more common in FAI (P < 0.001). A higher body mass index was significantly associated with delamination injury in FAI (odds ratio 1.226; 95% CI 1.043–1.441; P = 0.013). A significant correlation was evident between detachment injury and a larger AI in dysplasia (odds ratio 1.127; 95% CI 1.000–1.270; P = 0.049). In addition, symptom duration was positively correlated with the extent of labral tearing in FAI (P = 0.013), whereas the smaller LCEA was correlated with the larger extent of labral tearing in dysplasia (P = 0.044). FAI and dysplasia patients exhibited different labral and cartilage injury patterns. Increased body mass index was correlated with delamination injury in FAI, whereas an increased AI was associated with detachment injury in dysplasia. Greater tearing was associated with a longer symptom duration in FAI, and a decreased LCEA was a risk factor for the extent of tearing in dysplasia.
Level of evidence
Level III. Case–control study.
INTRODUCTION
The hip labrum is of vital importance for maintaining joint stability [1]. Labral tears, which were initially reported in 1953 [2], are frequently diagnosed due to advances in imaging techniques [3, 4]. Recently, labral tearing has been recognized as a feature of various diseases rather than as an independent diagnostic entity. Because the base of the labrum abuts the acetabular cartilage, cartilaginous injury is prognostic of labral tearing. For example, Imam et al. [5] demonstrated that repeated femoroacetabular impingement (FAI) could trigger labral and chondral lesions, potentially causing hip osteoarthritis (OA), and Amanatullah et al. [6] observed that untreated FAI could progress to early OA due to cartilage injury.
Of various hip diseases, FAI [7] and dysplasia [8] are the two most common causes of labral tearing and associated cartilaginous injuries. The labral tear patterns of both diseases have been investigated [9–11]. However, most studies have employed only diagnostic imaging, and direct, confirmatory arthroscopic observations are lacking. Moreover, only a few studies have investigated the labral tear patterns and cartilage injuries to identify relevant risk factors in FAI and dysplasia patients [12, 13].
Accordingly, the purpose of this study was to analyze labral tears and adjacent cartilage injury patterns of patients with hip FAI and dysplasia using arthroscopy (via the joint capsule) during osteotomies and to investigate the association between labral and cartilaginous injuries and clinical characteristics, including radiological findings. We hypothesized that FAI and dysplasia would exhibit different labral and cartilage injury patterns, and some patient demographics or radiologic parameters might be risk factors for cartilage injury and tear extent.
MATERIALS AND METHODS
This study was approved by our institutional review board (Kyung Hee University Hospital, KHUH 2020-07-016), and informed consent was obtained from all patients.
Patient selection and methods
We retrospectively reviewed the data of patients diagnosed with hip FAI or dysplasia at our institution between January 2012 and February 2019. Among the patients with FAI or dysplasia, those with labral tears observed arthroscopically during surgery were included in this study. The surgical indication was persistent hip pain despite conservative treatment (non-steroidal anti-inflammatory medication and physical therapy) for at least 3 months.
For FAI, cases of reproducible groin pain due to abnormal contact during the normal range of motion and positive anterior impingement pain were included [6, 14], and these cases were classified into cam, pincer and mixed types. The cam-type FAI was diagnosed based on an alpha angle ≥50°, and the alpha angle was measured in the preoperative frog-leg view and magnetic resonance arthrography or radial oblique view on magnetic resonance imaging. The pincer type was diagnosed based on a lateral center-edge angle (LCEA) ≥40° or crossover sign, and the mixed type was defined as the presence of the features of both cam and pincer types [4, 15]. Dysplasia was diagnosed based on an evident LCEA and anterior center-edge angle (ACEA) <20° on plain anteroposterior (AP) and false-profile radiographs [14]. In addition, in the case of cam-type FAI, patients with or without borderline dysplasia were classified, and differences in cartilage injury patterns according to concomitant borderline dysplasia were analyzed. Borderline dysplasia was defined by an LCEA of ≥20° and < 25° [16].
Exclusion criteria were as follows: dysplasia patients with cam morphology (alpha angle ≥50°), deformities that could cause secondary FAI or dysplasia, history of trauma or hip surgery, preoperative plain radiographic findings of OA (Tonnis grade 2 or greater) or lack of medical or arthroscopic data. We arthroscopically examined only dysplasia patients for whom manual traction sufficed when opening the hip joint capsule. Dysplasia patients for whom arthroscopic images were unavailable were also excluded (Fig. 1).
Fig. 1.

Flow diagram of patient selection.
Throughout the study period, 311 patients underwent surgery with an arthroscopic examination (FAI, 95; dysplasia, 216). The surgical indication was persistent hip pain despite conservative treatment (non-steroidal anti-inflammatory medication and physical therapy) for at least 3 months. After applying the inclusion and exclusion criteria, 137 patients were included for the final analysis (FAI, 74; dysplasia, 63).
Preoperative radiographic evaluation
All radiologic parameters were measured by one corresponding author. All FAI patients were preoperatively assessed in terms of the LCEA, acetabular index (AI), acetabular version and alpha angle via magnetic resonance arthrography and plain pelvic AP radiography. For patients with dysplasia, the LCEA and ACEA were measured on pelvic AP and false-profile plain radiographs, respectively.
According to the method proposed by Clohisy et al., standard pelvic AP radiographs were taken in the supine position with 15° internal rotation of the lower limbs. Frog-leg radiographs were taken in the supine position, with the affected knee abducted by 30° and the hip abducted by 45°. False-profile radiographs were taken in the standing position with the hip joint on the affected side placed on the cassette, pelvis rotated by 65° and foot on the affected side placed parallel with the cassette [17].
Intraoperative arthroscopic findings
We examined the extent of labral hypertrophy, fibrillation and bruising associated with labral tears in both groups. Labral hypertrophy was defined as width > 4 mm [18]. Some cases exhibited acetabular or femoral head fissuring (or both), which were attributable to sustained shear stress on the acetabulum [19] due to chronic anterolateral migration of the femoral head associated with the characteristic instability of hip dysplasia. Such cases were compared with FAI cases. Finally, we compared the labral tear patterns and adjacent cartilage injuries between both groups.
Cartilage injury was evaluated by detachment or delamination, respectively. Cartilage detachment was defined as the separation of entire damaged acetabular cartilage from the central acetabulum with intact labro-cartilaginous junction. Cartilage delamination was defined as the development of a delaminated cartilage flap from the labro-cartilaginous junction.
Based on the study by Tamura et al. [20], the tear extent was divided into a total of 24 planes using a clock face system relative to the acetabular dome. Tear extent was defined as the total angles of the planes that showed labral tears in arthroscopic findings.
Operative techniques
All operations were performed by the senior author using standardized procedures. Dysplasia patients underwent transtrochanteric periacetabular rotational osteotomy in the lateral position. Dry arthroscopic examinations were performed after exposure of the joint capsule (before osteotomy) to confirm the location and pattern of the labral tear. An assistant performed manual traction, and transtrochanteric periacetabular osrotational osteotomy was performed under arthroscopic guidance. FAI patients underwent arthroscopic surgery supine on a traction table. The torn labrum was debrided or repaired depending on the status of the residual tissue. Femoral or acetabular bony procedures were administered if indicated.
Statistical analysis
An independent t-test was used to compare patient demographics and the extent of tearing between the FAI and dysplasia groups. One-way ANOVA test was used to compare radiologic parameters between each FAI type and dysplasia. Chi-squared test was employed to compare intraoperative arthroscopic findings (hypertrophy, fibrillation, bruising and location of fissuring) between the two groups. Multinomial logistic regression analysis was used to identify correlations between radiological parameters and patient demographics. Linear regression analyses were performed to determine the correlations between radiological parameters, demographics and the extent of tearing. The level of statistical significance was set at 0.05, with associated 95% confidence intervals (CIs). SPSS ver. 21.0 (IBM, Chicago, IL, USA) was used for all statistical analyses. Post hoc power calculation (alpha error: 0.05, 1-beta error: 0.95) was performed using G*Power (version 3.1.9.7). The interobserver reliability of the radiologic parameters was determined with intra-class correlation coefficients (ICCs).
RESULTS
Demographic data and mean radiologic parameters of enrolled patients are summarized in Tables I and II. Symptom duration was defined as the time from the first onset of pain to immediately before surgery.
Table I.
Demographic characteristics
| FAI | Dysplasia | P-values | |
|---|---|---|---|
| Number of cases | 74 | 63 | – |
| Age (years), mean ± SD | 36.4 ± 14.0 | 34.7 ± 11.6 | 0.235 |
| Sex (n), male/female | 35/39 | 3/60 | <0.001 |
| Side (n), right/left | 37/37 | 34/29 | 0.883 |
| BMI (kg/m2) | 23.3 ± 3.9 | 22.0 ± 3.1 | 0.131 |
| Symptom duration (months) | 21.1 ± 23.7 | 15.2 ± 17.6 | 0.107 |
Table II.
Preoperative radiologic parameters
| FAI (n = 74) | |||||
|---|---|---|---|---|---|
| Cam (n = 55) | Pincer (n = 6) | Mixed (n = 13) | Dysplasia (n = 63) | P-values | |
| LCEA | 25.6° ± 3.6° | 42.1° ± 1.4° | 41.4° ± 3.8° | 8.6° ± 7.1° | < 0.001 |
| ACEA | – | – | – | 10.0° ± 6.9° | – |
| AI | 8.0° ± 3.9° | 4.7° ± 4.0° | 5.5° ± 4.8° | 19.7° ± 6.4° | < 0.001 |
| Acetabular anteversion | 18.1° ± 5.5° | 12.4° ± 3.4° | 13.0° ± 7.0° | – | < 0.001 |
| Alpha angle | 57.6° ± 6.4° | 46.1° ± 2.7° | 62.9° ± 4.6° | – | < 0.001 |
FAI, femoroacetabular impingement; LCEA, lateral center-edge angle; ACEA, anterior center-edge angle; AI, acetabular index.
The ICCs of radiologic parameters between the independent observers was 0.943 (95% CI, 0.887–0.972, P < 0.001) for LCEA, 0.905 (95% CI, 0.761–0.963, P < 0.001) for ACEA, 0.933 (95% CI, 0.860–0.968, P < 0.001) for AI, 0.897 (95% CI, 0.775–0.953, P < 0.001) for acetabular version and 0.945 (95% CI, 0.879–0.975, P < 0.001) for alpha angle, showing good-to-excellent concordance.
Dysplasia patients showed a significantly greater extent of tears than FAI patients (82.9 ± 50.9° versus 52.3 ± 28.4°, P < 0.001). There were no differences in tear extent according to FAI type (P = 0.569).
Characteristics of labral tears and location of fissures
Labral hypertrophy was more common in dysplasia cases than in FAI cases (P = 0.002). However, bruises were more common in FAI cases than in dysplasia cases (P = 0.003; Table III).
Table III.
Comparison of the labral tear characteristics and fissuring between patients with FAI and dysplasia
| FAI (n = 74) | Dysplasia (n = 63) | P-values | |
|---|---|---|---|
| Characteristics | |||
| Hypertrophy | 25 (33.8%) | 38 (60.3%) | 0.002 |
| Fibrillation | 14 (18.9%) | 12 (19.0%) | 0.608 |
| Bruising | 39 (52.7%) | 14 (22.2%) | 0.003 |
| Fissures | |||
| Acetabuluma | 11 (14.9%) | 34 (54.0%) | |
| Both acetabulum and the femoral headb | 9 (12.2%) | 17 (27.0%) | < 0.001 |
| None | 54 (72.9%) | 12 (19.0%) | |
FAI, femoroacetabular impingement.
Acetabulum, superomedial side.
Femoral head, superolateral side.
In patients with dysplasia, acetabular (superomedial) fissures were the most common presentations [34 cases (54%)]; 17 cases (27%) exhibited both acetabular (superomedial) and femoral head (superolateral) fissures (Fig. 2a and b). Fifty-four FAI patients (72.9%) exhibited no fissures; a significant between-group difference in fissure cases was thus evident (P < 0.001; Table III). In the 20 FAI patients who presented fissures, the cam-type was the most common (total, 13; acetabulum, 8; both, 5), followed by the mixed type (total, 5; acetabulum, 1; both, 4) and pincer type (total, 2; acetabulum, 2; both, 0).
Fig. 2.
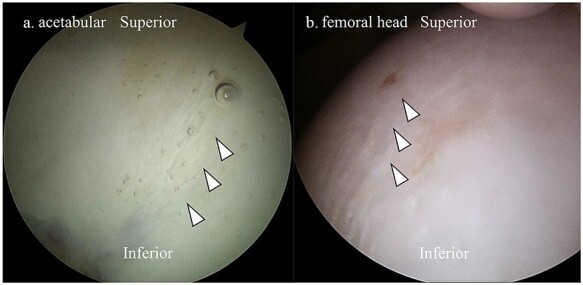
(a) Intraoperative arthroscopic findings from a 19-year-old male patient with dysplasia showing a fissure (arrowheads) in the superomedial side of the acetabulum. (b) Intraoperative arthroscopic findings from a 48-year-old female patient showing a fissure (arrowheads) in the acetabulum and superolateral side of the femoral head.
Characteristics of adjacent cartilage injuries
Cartilage injuries differed significantly between the two groups (P < 0.001; Fig. 3a and b; Table IV). Dysplasia showed the most cartilage detachment, while FAI showed the most cartilage delamination, with a statistically significant difference (P < 0.001). We performed a post hoc power analysis using the characteristics of cartilage injury, which demonstrated a statistically significant difference and was considered the most important value in this study. The effect size was 0.463 and at alpha = 0.05, the power of this study was 0.99. Among the cam-type FAI cases, 78.2% (70.9% delamination and 7.3% detachment) had cartilage injury and there were no significant differences in the characteristics of cartilage injury with (n = 26, 80.8% delamination and 3.8% detachment) or without (n = 29, 62.1% delamination and 10.3% detachment) borderline dysplasia (P = 0.350); among the pincer types, 83.3% (66.7% delamination and 16.6% detachment) had cartilage injury; among the mixed types, 84.6% (69.2% delamination and 15.4% detachment) had cartilage injury. There were no statistically significant differences in the characteristics of cartilage injury among various FAI types (P = 0.764).
Fig. 3.

(a) Intraoperative arthroscopic findings from a 25-year-old female patient with dysplasia showing cartilage detachment (arrowheads) and intact chondrolabral junction (arrow). (b) Intraoperative arthroscopic findings from a 54-year-old female patient with FAI showing cartilage delamination (arrowheads).
Table IV.
Characteristics of adjacent cartilage injury in patients with FAI and dysplasia
| Characteristics |
FAI (n = 74)
Cam/pincer/mixed |
Dysplasia (n = 63) | P-values |
|---|---|---|---|
| Cartilage detachment | 7 4 (57.1%)/1 (14.3%)/2 (28.6%) |
24 (38.1%) | |
| Cartilage delamination | 52 39 (75.0%)/4 (7.7%)/9 (17.3%) |
16 (25.4%) | < 0.001 |
| Intact | 15 12 (80.0%)/1 (6.7%)/2 (13.3%) |
23 (36.5%) |
FAI, femoroacetabular impingement.
Risk factors for cartilage injury
Logistic regression analysis showed that a higher body mass index (BMI) was associated with a higher rate of cartilage delamination in FAI patients [odds ratio (OR) 1.226; 95% CI, 1.043–1.441; P = 0.013). In patients with dysplasia, a higher AI was associated with cartilage detachment (OR 1.127; 95% CI, 1.000–1.270; P = 0.049); although statistical significance was not attained, BMI tended to be associated with cartilage delamination (P = 0.056; Table V).
Table V.
Logistic regression for cartilage injury in patients with FAI and dysplasia
| FAI |
Detachment
P-values |
OR
(95% CI) |
Delamination
P-values |
OR
(95% CI) |
|---|---|---|---|---|
| Typea | ||||
| Cam (ref. mixed) | 0.341 | 0.333 (0.035, 3.205) |
0.701 | 0.722 (0.137, 3.205) |
| Pincer (ref. mixed) | 1.000 | 1.000 (0.034, 29.807) |
0.931 | 0.889 (0.061, 12.885) |
| Radiological factors | ||||
| LCEA | 0.394 | 1.048 (0.941, 1.169) |
0.770 | 0.989 (0.919, 1.065) |
| AI | 0.818 | 0.974 (0.785, 1.209) |
0.814 | 1.017 (0.885, 1.169) |
| Acetabular version | 0.563 | 1.053 (0.884, 1.254) |
0.471 | 1.040 (0.935, 1.156) |
| Alpha angle | 0.859 | 0.988 (0.870, 1.123) |
0.841 | 1.008 (0.929, 1.094) |
| Demographic factors | ||||
| BMI | 0.346 | 1.116 (0.888, 1.402) |
0.013 | 1.226 (1.043, 1.441) |
| Age | 0.079 | 1.067 (0.992, 1.147) |
0.669 | 1.009 (0.967, 1.053) |
| Symptom duration | 0.499 | 0.987 (0.951, 1.025) |
0.173 | 0.985 (0.963, 1.007) |
| Sex | 0.181 | 0.267 (0.038, 1.852) |
0.348 | 0.571 (0.178, 1.838) |
| Side | 0.648 | 1.524 (0.250, 9.295) |
0.624 | 1.333 (0.422, 4.218) |
| Dysplasia | ||||
| Radiological factors | ||||
| LCEA | 0.234 | 0.947 (0.866, 1.036) |
0.868 | 0.991 (0.894, 1.100) |
| ACEA | 0.431 | 0.964 (0.880, 1.056) |
0.959 | 0.997 (0.898, 1.107) |
| AI | 0.049 | 1.127 (1.000, 1.270) |
0.071 | 1.104 (0.992, 1.229) |
| Demographic factors | ||||
| BMI | 0.111 | 1.195 (0.960, 1.487) |
0.056 | 1.259 (0.994, 1.593) |
| Age | 0.105 | 1.044 (0.991, 1.101) |
0.499 | 1.020 (0.963, 1.081) |
| Symptom duration | 0.437 | 1.014 (0.979, 1.051) |
0.261 | 0.999 (0.984, 1.061) |
| Side | 0.465 | 0.651 (0.206, 2.057) |
0.709 | 1.282 (0.348, 4.730) |
FAI, femoroacetabular impingement; OR, odds ratio; CI, confidence interval; LCEA, lateral center-edge angle; ACEA, anterior center-edge angle; AI, acetabular index; BMI, body mass index.
Cam, pincer and mixed, as revealed by multinomial logistic regression.
Bold P-values indicate statistical significance (P < 0.05).
Risk factors for the extent of tearing in FAI and dysplasia patients
In patients with FAI, symptom duration was a significant risk factor for tear extent (P = 0.020), and a higher BMI tended to be associated with increased tearing (P = 0.059; Table VI). In patients with dysplasia, linear regression analyses revealed that decreased LCEA was a significant risk factor for tear extent (P = 0.044), and increased AI tended to be associated with increasing tearing (P = 0.072; Table VII).
Table VI.
Linear regression analysis of clinical and demographic variables associated with tear extent in patients with FAI
| FAI | Beta | P-values | 95% CI |
|---|---|---|---|
| Typea | |||
| Cam (ref. mixed) | −9.16 | 0.376 | (−29.44, 11.12) |
| Pincer (ref. mixed) | 1.25 | 0.939 | (−30.57, 33.07) |
| Radiological factors | |||
| LCEA | 0.58 | 0.251 | (−0.42, 1.57) |
| AI | −0.80 | 0.393 | (−2.67, 1.06) |
| Acetabular version | −0.42 | 0.577 | (−1.90, 1.07) |
| Alpha angle | 0.32 | 0.557 | (−0.77, 1.42) |
| Demographic factors | |||
| BMI | 1.88 | 0.059 | (−0.08, 3.84) |
| Age | 0.06 | 0.843 | (−0.51, 0.62) |
| Symptom duration | 0.38 | 0.020 | (0.06, 0.69) |
| Sex | −2.40 | 0.759 | (−17.92, 13.12) |
| Side | −8.61 | 0.269 | (−24.00, 6.79) |
FAI, femoroacetabular impingement; LCEA, lateral center-edge angle; AI, acetabular index; BMI, body mass index.
Cam, pincer and mixed, as revealed by the generalized linear model.
Bold P-value indicates statistical significance (P < 0.05).
Table VII.
Linear regression analysis of clinical and demographic variables associated with tear extent in patients with dysplasia
| Dysplasia | Beta | P-values | 95% CI |
|---|---|---|---|
| Radiological factors | |||
| LCEA | −2.12 | 0.044 | (−4.19, −0.06) |
| ACEA | −1.77 | 0.101 | (−3.90, 0.36) |
| AI | 2.14 | 0.072 | (−0.20, 4.48) |
| Demographic factors | |||
| BMI | 2.85 | 0.233 | (−1.90, 7.60) |
| Age | 0.83 | 0.233 | (−0.55, 2.21) |
| Symptom duration | 0.12 | 0.770 | (−0.73, 0.98) |
| Sex | – | – | – |
| Side | 1.12 | 0.943 | (−30.01, 32.25) |
LCEA, lateral center-edge angle; ACEA, anterior center-edge angle; AI, acetabular index; BMI, body mass index.
Bold P-value indicates statistical significance (P < 0.05).
DISCUSSION
In this study, most FAI patients (70.3%) exhibited cartilage delamination of the labro-cartilaginous junction. Conversely, in dysplasia patients, cartilage detachment from the acetabulum and a torn labrum were the most common presentations (38.1%).
A few studies have examined labral morphologic characteristics in dysplasia and FAI patients. Sankar et al. [10] studied 553 hip labra of dysplasia patients and found that the most common abnormalities were degeneration and detachment. In a large multicenter study, Matsuda et al. [21] recruited a cohort of patients who underwent hip arthroscopy and compared labral lesions between those with and without dysplasia. However, those studies did not specify whether patients without dysplasia had FAI, and there was no detailed comparison of arthroscopic findings between patients with FAI and dysplasia. In our study, we performed arthroscopy and compared the clinical findings between FAI and dysplasia patients diagnosed preoperatively with imaging approaches. We were able to perform a more in-depth examination with arthroscopy, particularly in dysplasia cases, and the joint capsule was exposed prior to osteotomy. We found that labral hypertrophy was observed in 60.3% of dysplasia patients, a significantly greater proportion than that of FAI patients; the extent of labral tearing was also significantly greater in dysplasia patients, but bruising was significantly more common in FAI patients (52.7%). However, fibrillation did not differ between these two groups.
All subtypes of FAI are known to induce labral and chondral injuries due to the collision between the acetabular rim and the femoral head–neck junction [15, 22, 23], and the risk is higher in cam-type FAI than in pincer type [24]. Anderson et al. showed that cam-type FAI is more vulnerable to delamination due to the shear force inflicted by the non-spherical femoral head on the acetabular cartilage [22], and Alvarez et al. reported that the acetabular over-coverage zone and chondral delamination area are closely related in pincer-type FAI [23]. Similarly, we also observed that FAI patients usually had a cartilage delamination injury, and cam-type FAI (52.7%) had a higher prevalence than pincer type (5.4%) or mixed type (12.2%).
Dysplasia is known to cause cartilage injury via an inside-out mechanism involving an overload of shear force on the acetabular rim due to insufficient coverage of the acetabulum and anterolateral subluxation of the femoral head [15, 25, 26]. Kraeutler et al. [15] analyzed acetabular chondral injuries in FAI and dysplasia patients and found that outside-in cartilage flaps from the chondrolabral junction were mainly observed in FAI patients, while detached cartilages (inside-out flaps from the central acetabulum) with intact chondrolabral junctions were found principally in dysplasia patients [9]; however, not only patients with definite dysplasia (LCEA < 20°) but also those with borderline dysplasia were included in that study. Our study also reported a similar finding to Kraeutler et al. The patients with dysplasia more frequently had cartilage detachment injury from the central acetabulum with intact labro-cartilaginous junction. However, in the current study, we analyzed the patients with definite dysplasia.
Grace et al. [13] reported that higher-grade acetabular cartilage injuries was correlated with male patients, greater BMI and increasing alpha angle in patient with FAI. Similarly, we observed that an increased BMI was a significant risk factor for delaminated cartilage injuries in FAI patients, but sex was not. In addition, Fujii et al. [12] studied intra-articular lesions in dysplasia patients and concluded that cartilage degeneration became more severe as acetabular coverage decreased. Consistently, the current study found that a high AI was a significant risk factor for cartilage detachment, and delamination injuries tended to increase with an increased BMI in dysplasia patients.
Risk factors for the extent of labral tearing have received little attention, and only a few studies have investigated the extent of labral tearing in dysplasia and FAI patients. Ross et al. [27] reported that patients with dysplasia and acetabular indices >15° exhibited larger labral tears, and an LCEA <15° tended to be associated with greater tearing, but statistical significance was not achieved; however, they did not analyze demographic factors as well as radiologic parameters. Another study showed that age, BMI and a history of developmental hip dislocation treatment were associated with the severity of labral tearing in dysplasia patients [], and a greater alpha angle was associated with tearing severity in FAI patients. In the present study, we observed that symptom duration was a significant risk factor for the extent of labral tearing in FAI patients and the extent of the tear tended to increase as the BMI increased. In addition, as mentioned above, a decreased LCEA was an independent risk factor for the extent of labral tearing, and the extent of the tear tended to increase as the AI increased, although statistical significance was not achieved.
This study has several limitations. First, compared with FAI, a large portion of patients with dysplasia were excluded in this study. Thus, there might be a selection bias. Second, as different arthroscopic procedures were performed in each group, it might have caused bias. Third, in subtypes of FAI, the number of pincer- and mixed-type cases was smaller than that of cam-type cases. Fourth, the ratio of male-to-female patients was not balanced, although sex is not a known confounder of labral tear features in patients with FAI or dysplasia. Fifth, the treatment methods and clinical outcomes based on the labral tear patterns were not assessed. However, especially in cases of dysplasia, only a few studies have directly observed the pattern of labral tear and cartilage injury, compared with FAI; therefore, this study would be meaningful.
CONCLUSIONS
FAI and dysplasia patients exhibited different cartilage injury patterns and labral tearing. In patients with FAI, prolonged duration of symptoms was associated with more extensive labral tears, and a higher BMI was associated with a higher incidence of delaminated cartilage injury. In patients with dysplasia, decreased acetabular coverage was associated with larger tears, and an increased AI was associated with increased cartilage detachment.
ACKNOWLEDGEMENT
None declared.
Contributor Information
Yoon-Je Cho, Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University Hospital, 23 Kyung Hee Dae-ro, Dongdaemoon-ku, Seoul 02447, Republic of Korea.
Kee-Hyung Rhyu, Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University Hospital, 23 Kyung Hee Dae-ro, Dongdaemoon-ku, Seoul 02447, Republic of Korea.
Young-Soo Chun, Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University Hospital at Gangdong, 892 Dongnam-ro, Gangdong-ku, Seoul 05278, Republic of Korea.
Myung-Seo Kim, Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University Hospital at Gangdong, 892 Dongnam-ro, Gangdong-ku, Seoul 05278, Republic of Korea.
DATA AVAILABILITY
The datasets generated and/or analysed during the current study are not publicly available due to reasons of sensitivity of human data, but are available from the corresponding author on reasonable request.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
REFERENCES
- 1. Seldes RM, Tan V, Hunt J. et al. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res 2001; 382: 232–40. [DOI] [PubMed] [Google Scholar]
- 2. Dameron TB Jr. Bucket-handle tear of acetabular labrum accompanying posterior dislocation of the hip. J Bone Joint Surg Am 1959; 41-A: 131–4. [PubMed] [Google Scholar]
- 3. Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res 2007; 455: 88–92. [DOI] [PubMed] [Google Scholar]
- 4. Su T, Chen GX, Yang L. Diagnosis and treatment of labral tear. Chin Med J (Engl) 2019; 132: 211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop 2011; 35: 1427–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Amanatullah DF, Antkowiak T, Pillay K. et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics 2015; 38: 185–99. [DOI] [PubMed] [Google Scholar]
- 7. Pennock AT, Bomar JD, Johnson KP. et al. Nonoperative management of femoroacetabular impingement: a prospective study. Am J Sports Med 2018; 46: 3415–22. [DOI] [PubMed] [Google Scholar]
- 8. Kelly BT, Weiland DE, Schenker ML. et al. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy 2005; 21: 1496–504. [DOI] [PubMed] [Google Scholar]
- 9. Lee YK, Kim JM, Yoon BI. et al. Location and correlation of acetabular labral tears and paralabral cysts using magnetic resonance imaging or magnetic resonance arthrography in patients with femoroacetabular impingement. Arthroscopy 2019; 35: 809–15. [DOI] [PubMed] [Google Scholar]
- 10. Sankar WN, Beaulé PE, Clohisy JC. et al. Labral morphologic characteristics in patients with symptomatic acetabular dysplasia. Am J Sports Med 2015; 43: 2152–6. [DOI] [PubMed] [Google Scholar]
- 11. Tresch F, Dietrich TJ, Pfirrmann CWA. et al. Hip MRI: prevalence of articular cartilage defects and labral tears in asymptomatic volunteers. A comparison with a matched population of patients with femoroacetabular impingement. J Magn Reson Imaging 2017; 46: 440–51. [DOI] [PubMed] [Google Scholar]
- 12. Fujii M, Nakashima Y, Noguchi Y. et al. Factors associated with severity of intra-articular lesions in patients with severe hip dysplasia. Arthroscopy 2016; 32: 1581–9. [DOI] [PubMed] [Google Scholar]
- 13. Grace T, Samaan MA, Souza RB. et al. Correlation of patient symptoms with labral and articular cartilage damage in femoroacetabular impingement. Orthop J Sports Med 2018; 6: 2325967118778785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gala L, Clohisy JC, Beaulé PE. Hip dysplasia in the young adult. J Bone Joint Surg Am 2016; 98: 63–73. [DOI] [PubMed] [Google Scholar]
- 15. Kraeutler MJ, Goodrich JA, Fioravanti MJ. et al. The “outside-in” lesion of hip impingement and the “inside-out” lesion of hip dysplasia: two distinct patterns of acetabular chondral injury. Am J Sports Med 2019; 47: 2978–84. [DOI] [PubMed] [Google Scholar]
- 16. Kobayashi N, Inaba Y, Kubota S. et al. The distribution of impingement region in cam-type femoroacetabular impingement and borderline dysplasia of the hip with or without cam deformity: a computer simulation study. Arthroscopy 2017; 33: 329–34. [DOI] [PubMed] [Google Scholar]
- 17. Clohisy JC, Carlisle JC, Beaulé PE. et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 2008; 90: 47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nwachukwu BU, Gaudiani MA, Marsh NA. et al. Labral hypertrophy correlates with borderline hip dysplasia and microinstability in femoroacetabular impingement: a matched case-control analysis. Hip Int 2019; 29: 198–203. [DOI] [PubMed] [Google Scholar]
- 19. Leunig M, Podeszwa D, Beck M. et al. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res 2004; 418: 74–80. [DOI] [PubMed] [Google Scholar]
- 20. Tamura S, Nishii T, Takao M. et al. Differences in the locations and modes of labral tearing between dysplastic hips and those with femoroacetabular impingement. Bone Joint J 2013; 95-B: 1320–5. [DOI] [PubMed] [Google Scholar]
- 21. Matsuda DK, Wolff AB, Nho SJ. et al. Hip dysplasia: prevalence, associated findings, and procedures from large multicenter arthroscopy study group. Arthroscopy 2018; 34: 444–53. [DOI] [PubMed] [Google Scholar]
- 22. Anderson LA, Peters CL, Park BB. et al. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am 2009; 91: 305–13. [DOI] [PubMed] [Google Scholar]
- 23. Camacho-Alvarez D, Mardones-Peterman R. Femoroacetabular impingement: association between the over-coverage and acetabular cartilage delamination areas. Rev Esp Cir Ortop Traumatol 2013; 57: 111–6. [DOI] [PubMed] [Google Scholar]
- 24. Beaulé PE, Hynes K, Parker G. et al. Can the alpha angle assessment of cam impingement predict acetabular cartilage delamination? Clin Orthop Relat Res 2012; 470: 3361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kain MS, Novais EN, Vallim C. et al. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg Am 2011; 93: 57–61. [DOI] [PubMed] [Google Scholar]
- 26. Kraeutler MJ, Garabekyan T, Pascual-Garrido C. et al. Hip instability: a review of hip dysplasia and other contributing factors. Muscles Ligaments Tendons J 2016; 6: 343–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ross JR, Zaltz I, Nepple JJ. et al. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med 2011; 39: 72S–8S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to reasons of sensitivity of human data, but are available from the corresponding author on reasonable request.


