Abstract
Introduction:
Social prescribing (SP) aims to provide targeted psychosocial support and close the gap between medical and non-medical services. This review assesses the effectiveness of community-based SP interventions.
Methods:
We performed a systematic review and qualitative synthesis of interventional studies of community referral interventions focused on facilitating psychosocial support. We considered health-related endpoints, other patient reported outcomes, or health care utilization. Six databases, grey literature, and additional trials registers were searched. Results were screened in a two-step process, followed by data extraction, each by two independent reviewers. If data permitted such, effect sizes were calculated. Risk of bias was assessed with the EPHPP and the Cochrane RoB2 tools.
Results:
We identified 68 reports from 53 different projects, three were controlled studies. Uncontrolled studies with shorter time frames frequently reported positive effects. This could largely not be seen in controlled settings and for longer follow-up periods. Designs, populations, and outcomes evaluated were heterogeneous with high risk of bias for most studies.
Discussion and conclusion:
Current evidence suggests positive effects of SP on a variety of relevant endpoints. Due to quality deficits in the available studies, scope for conclusions concerning clinical relevance and sustainability is limited. Further methodologically rigorous controlled trials are needed.
Keywords: social prescribing, community referral intervention, systematic review, integrated care
Abstract
Einleitung:
Social prescribing (SP) soll gezielte psychosoziale Unterstützung ermöglichen und die Lücke zwischen medizinischen und nicht-medizinischen Angeboten schließen. Diese Übersichtsarbeit untersucht die Wirksamkeit von gemeindebasierten SP-Interventionen.
Methoden:
Es erfolgte eine systematische Übersichtsarbeit und qualitative Synthese von Interventionsstudien zu gemeindebasierten Überweisungs-Interventionen, die auf eine Förderung psychosozialer Unterstützung abzielen. Es wurden gesundheitsrelevante Endpunkte, andere patientenberichtete Outcomes, sowie die Inanspruchnahme von Gesundheitsleistungen berücksichtigt. Die Suche erfolgte in sechs Datenbanken, grauer Literatur, sowie zusätzlich in Studienregistern. Die Ergebnisse wurden in einem zweistufigen Prozess gesichtet, gefolgt von der Datenextraktion. Beide Schritte erfolgten durch zwei unabhängige Reviewer. Bei ausreichend verfügbaren Daten wurden Effektstärken errechnet. Das Verzerrungspotenzial wurde mit den EPHPP und Cochrane RoB2 Instrumenten bewertet.
Ergebnisse:
Es wurden 68 Berichte aus 53 unterschiedlichen Projekten identifiziert, darunter waren drei kontrollierte Studien. Nicht-kontrollierte Studien mit kürzeren Betrachtungszeiträumen berichteten häufig positive Effekte. In kontrollierten Settings und über längere Beobachtungszeiten konnte dies überwiegend nicht gezeigt werden. Betrachtete Designs, Populationen und Endpunkte waren heterogen, das Verzerrungspotential in den meisten Studien hoch.
Diskussion und Schlussfolgerungen:
Die derzeitige Evidenz legt positive Effekte von SP auf eine Reihe relevanter Endpunkte nahe. Aufgrund von Qualitätsdefiziten in den verfügbaren Studien können die klinische Relevanz und die Langfristigkeit der Effekte nur eingeschränkt beurteilt werden. Zusätzliche methodisch hochwertige Studien sind erforderlich.
Introduction
Psychosocial problems play a major role in primary care [1] and have a considerable impact on manifestation and course of mental and somatic conditions [2,3,4]. Psychosocial issues typically seen in primary care include loneliness and restrictions in social participation of elderly multi-morbid patients, problems in the family and at work, as well as financial difficulties [1]. Psychosocial problems are also associated with considerable economic costs, e.g. caused by sick leave and long-term absence from work [5, 6].
While General Practitioners (GPs) can target only few problems during their consultations [7], there is an extensive range of social care and counseling in many countries. Consequently, there may frequently be no formalized connections between psychosocial counseling services and primary care [8]. Depending on local circumstances, the diversity of offers in the non-medical sector may confuse providers. For an individual, choosing the right contact point might be challenging.
Social prescribing (SP) is an innovative and promising approach for providing vulnerable groups with psychosocial support and bridge the gap between medical and psychosocial services [9]. It equips GPs with a non-medical referral option which can accompany existing treatments to improve health and well-being. SP is usually implemented by involving a “link worker” to whom patients with psychosocial problems are referred (= issued a “social prescription”). The link worker identifies non-medical problems and initiates subsequent contact with appropriate local services [10]. The SP concept combines two key forms of integrated care: horizontal integration with its focus on multidisciplinary support, as well as people-centered integration aimed at empowerment and self-management [11].
SP has been implemented in pilot trials, especially in the United Kingdom (UK), and published evaluations have demonstrated improvement with respect to relevant outcomes, such as quality of life, anxiety and depression [12,13,14,15], reduction in healthcare utilization [16,17,18] and workload reduction for primary care physicians [19], as well as earlier return to work [15]. Nevertheless, the methodological spectrum and manner of reporting are heterogeneous, ranging from formally publicized randomized controlled trials [20] to non-peer-reviewed before-and-after studies. Previous systematic reviews have either focused on specific outcomes [21] or were limited to studies in the UK [22,23], thus leaving important questions unanswered.
Therefore, this systematic review aims to assess the effectiveness of SP for facilitating psychosocial support with an international focus.
Methods
Protocol
The protocol was published a priori in the PROSPERO registry (registration number: CRD42020182562 [24]). The protocol development was supervised by an independent advisory board including experts from primary care and public health as well as patient representatives.
Eligibility criteria
The target population consisted of adults with an actual or assumed need for psychosocial support or counseling. Interventions were eligible if they consisted of a community referral intervention aimed at psychosocial support or counseling and if the referral was initiated by an outpatient medical provider (primary care providers, other physicians, nurses, outpatient clinics etc.). In this context, referrals to a facilitator, coordinator or institution assessing needs and initiating appropriate measures were considered pertinent. We included controlled trials as well as uncontrolled studies with a before-and-after design. We considered all health-related endpoints and surrogate parameters, any other patient reported outcomes, as well as any measures of health care utilization. Measurements needed to be assessed at least at two different time points and/or in two different groups with no limit to the length of follow-up.
Information sources and search strategy
We searched the following electronic bibliographic databases: MEDLINE, Embase, SocIndex, Social Care Online, CINAHL, and the Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials). We conducted a search on ClinicalTrials.gov and the International Clinical Trials Registry Platform (ICTRP). We did not apply constraints concerning language or country of origin. The time frame was limited to studies published since 2000, as SP as a concept was established in the late 90s and early 2000s [25,26] with evaluation methods and general rigor of study conduct in health services research concurrently advancing [27]. Supplementary search strategies included analysis of bibliographies of studies and reviews identified by the electronic search (citation tracking), as well as an internet search with defined keywords for identification of “grey literature”. Such resources beyond formal scientific publishing were also retrieved from pertinent information repositories: Open Grey, Grey Literature Report and Grey Guide Repository. All search algorithms used can be found in the supplement (Appendix 1). The initial search was conducted on May 5th 2020, an update search was performed on February 1st 2021.
Study selection and data extraction
After removal of duplicates, we performed a two-step screening process to select studies meeting inclusion criteria. Firstly, two reviewers independently assessed all titles and abstracts. Secondly, two reviewers independently assessed all eligible full texts. In both steps, disagreement was resolved through discussion, and where necessary by consulting a third researcher. A standardized data extraction sheet was developed and piloted. Two reviewers extracted data independently. Discrepancies were resolved by discussion. Zotero [28] was used for collecting and de-duplicating publications and Covidence [29] for selecting studies and extracting data.
Risk of bias
We used the Effective Public Health Practice Project’s Quality Assessment Tool for Quantitative Studies (EPHPP) for study-level quality appraisal [30,31]. Additionally, we assessed the quality of randomized controlled trials with the Cochrane Risk of Bias tool for randomized trials (RoB 2) [32]. Two reviewers assessed risk of bias independently. Risk of bias was visualized using the robvis package [33].
Synthesis of results
Findings were summarized descriptively. For purposes of judicious data analysis and reporting, outcomes had to be classified in thematic groups and prioritized based on the scope of available data. Thematic classification was based on the Common Outcomes Framework, focusing on the impact on the person and on the health and care system [34]. The six groups were: mental health, mental wellbeing, quality of life and general health, loneliness, self-efficacy, and health care utilization. Concerning length of follow-up for longitudinal outcome assessment, time frames were classified into short (0–3 months), intermediate (>3–6 months) and long term (>6 months). For continuous outcome parameters with sufficient information and data quality, we calculated standardized mean differences (SMD) as measures of effect size. We used test statistics or p values and degrees of freedom to approximate SMD using the effectsize package [35] in R [36]. When SMDs could be computed, visualization was performed with the meta package [37]. We refrained from calculating and presenting a pooled effect measure as to not exceed the body of evidence’s potential. Subgroup analyses were neither feasible.
Results
Study selection
We identified 4934 records and included 53 studies with 68 publications in our review. The study selection process is outlined in the revised PRISMA flow diagram (Figure 1) [38]. Appendix 2 provides a list of publications excluded in the full text screening stage, as well as reasons for exclusion.
Figure 1.
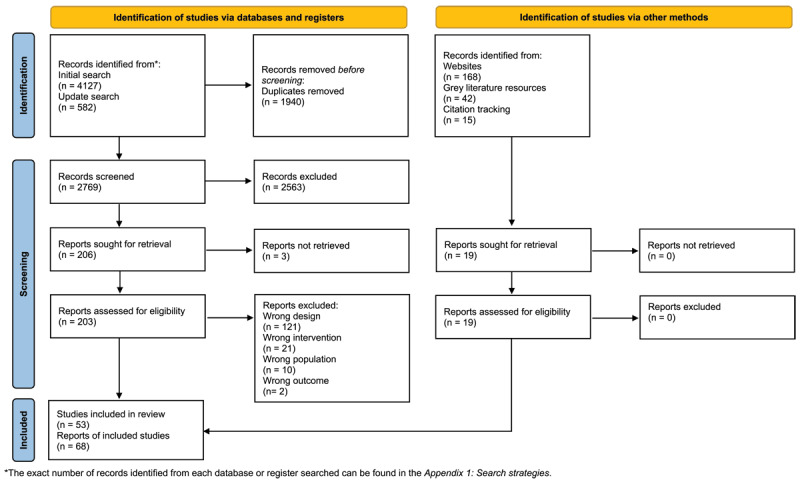
Revised PRISMA Flow diagram.
Note: The diagram shows the iterative steps of literature screening and selection. Numbers refer to the reports identified. For some interventional studies, more than one report was located. The bottommost box shows total numbers of included reports and underlying SP projects.
Study characteristics
All included studies were conducted in high-income countries, with 51 studies originating from the UK and two from Australia [15,39]. There were 50 uncontrolled studies with a before-and-after design [12,13,14,15,16,17,18,19,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91], one of these included a module with a controlled design for health care utilization outcomes [84]. Three studies included control groups: one randomized controlled trial [92], one quasi-experimental cluster randomized controlled trial [93], and one non-randomized controlled trial [94,95,96]. Fifteen evaluations were peer-reviewed before publishing, five were partly peer-reviewed (not all publications of the project were peer-reviewed) and 33 were not peer-reviewed. Most reports (n = 41, ~80%) had been published in the last five years, with about half of these dating back to the years 2019 and 2020 (n = 22). Fifteen SP evaluations focused on populations with special characteristics besides their existing psychosocial needs (Mental health issues: n = 6 [12,39,52,53,58,70,80,88], long-term conditions: n = 4 [49,50,51,54,57,60,61,97], geriatric age group: n = 2 [19,73], work-related injuries: n = 1 [15], high risk for cardiovascular disease: n = 1 [84] and sensory impairment: n = 1 [87]).The remaining studies had included unselected/mixed populations or did not provide detailed information about the target group. Sample sizes were highly heterogeneous, ranging from n = 12 [87] to n = 10643 [64]. All studies included into this review reported on a combined total number of n = 50237 patients (n = 41627 receiving SP, n = 8610 controls). One study did not report the total of recruited patients [77]. Only few publications described efforts of accounting for potential biases (Figures 2, 3, 4). Overall, the population across the field of included SP studies can be characterized as adult, of a wide age range, with a predominance of female participants (Appendix 3). Many studies included populations with high levels of social deprivation, unemployment, frequently living alone, and often afflicted with long-term conditions. Referral reasons reported were manifold, including social isolation, mental health issues, high primary care utilization, struggles with significant life changes, financial or housing problems, and conflicts at work or in the family, including e.g. special challenges of caregivers. The vast majority of studies was conducted in a primary care setting (Appendix 3). Some of the SP projects located the link worker directly in the primary care providers’ practices, while this function was situated in the community in most study setups. According to the concept proposed by Richard Kimberlee [98], SP programs can be delineated into different models based on the interventions’ components and how comprehensively they address the entirety of patients’ needs. Such have been labeled according to intensity as light, medium or holistic. Applying this concept, 30 programs in our study field could be described as holistic, 17 as medium and six as light evaluations. However, classification was difficult for some studies as to partially missing information, and a few programs comprising several alternative pathways (Appendix 3). Maximum length of observance of participants after baseline ranged between immediately after the end of intervention [12,15,42,61,69,77,78,82,83] and 18 months [16], but many studies did assess outcomes at more than one time point during follow-up. Regarding the small field of controlled studies, the non-randomized controlled trial reported by Carnes et al. [94,95,96] included two control groups. Assessment of differences in patient outcomes (e.g. quality of life) was based on comparison with a matched control group from six GP practices in the area, while another matched control group from the same GP practices was used for comparative evaluation of GP consultation rates. The control group in the randomized controlled trial by Grant et al. received routine GP care [20]. Mercer et al. [92,93] included randomly chosen patients from comparator practices located in the same area (Glasgow), which were additionally selected on basis of their catering to deprived patient populations. Comparator practices were not allocated a link worker. A detailed overview of all included evaluations can be found in the study characteristics table (Appendix 3).
Figure 2.
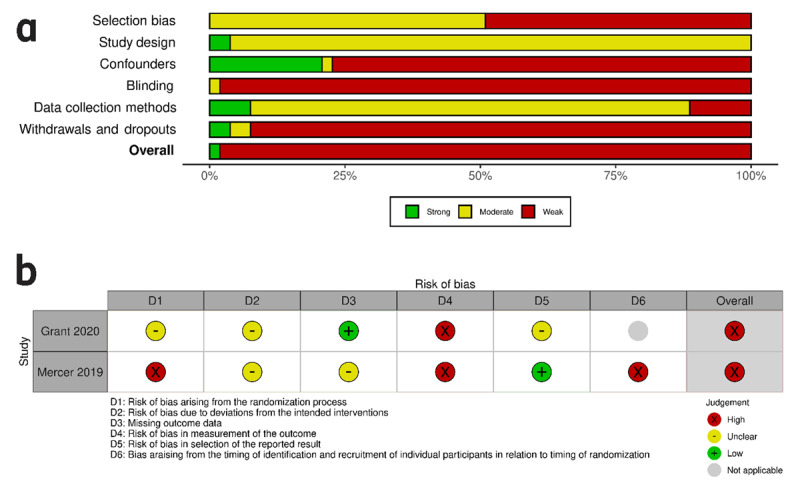
a: Risk of bias within studies: EPHPP for non-randomized studies, summary plot. b: Risk of bias within studies: RoB2 for randomized studies, traffic light plot.
Note: Figure 2a: Stacked bars in the summary plot represent percentages of studies with a corresponding rating for individual EPHPP domains and the overall quality judgment. Figure 2b: RoB 2 assessment for randomized studies only. Rows show individual domain and overall ratings for each study, visualized as traffic light symbols.
Figure 3.
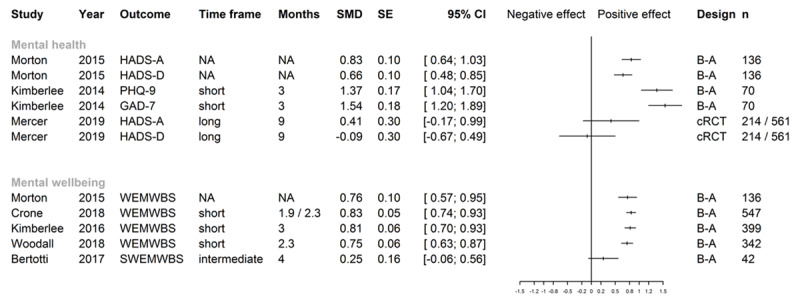
Effect sizes for mental health and mental wellbeing.
Note: HADS-A Hospital Anxiety and Depression Scale – Anxiety; HADS-D Hospital Anxiety and Depression Scale – Depression; PHQ-9 Patient Health Questionnaire-9; GAD-7 Generalized Anxiety Disorder Scale-7; WEMWBS Warwick Edinburgh Mental Wellbeing Scale; SWEMWBS Short Warwick Edinburgh Mental Wellbeing Scale; Time frame: short (0–3 months), intermediate (>3–6 months) and long term (>6 months); Follow-up time in months: in case of original study reporting follow-up in weeks, these were converted to 30-day months; Kimberlee 2016 [76]: follow-up time of 3 months was intended, but length unclear in half of cases; Woodall 2018 [90]: mean follow-up time; If different numbers of months are shown, follow-up length was different for sub-populations; NA not addressed in original report; B–A before-after study; cRCT cluster randomized controlled trial; n number of patients analyzed for outcome, numbers refer to intervention/control in case of controlled studies; SMD and SE rounded by software package to two digits, confidence intervals were calculated by R package “meta” [37] from SMD/SE values calculated by R package “effect size” [35]. For Mercer 2019 [92,93], effect sizes were taken from the original publication (adjusted SMD).
Figure 4.
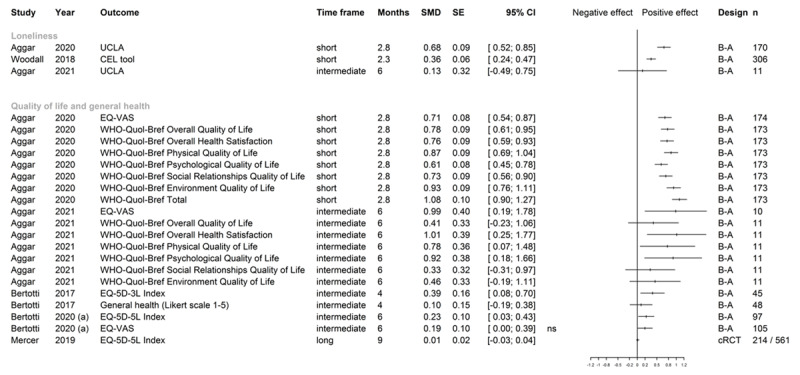
Effect sizes for loneliness, quality of life, and general health.
Note: UCLA University of California Los Angeles Loneliness Scale; CEL Campaign to End Loneliness ; EQ-VAS European Quality of Life Visual Analogue Scale; WHO-Quol-Bref, WHO Quality of Life short form; EQ-5D-3L/5L European Quality of Life 5 Dimensions 3 Level/5 Level; Time frame: short (0–3 months), intermediate (>3–6 months) and long term (>6 months); Follow-up time in months: in case of original study reporting follow-up in weeks, these were converted to 30-day months; B-A before-after study; cRCT cluster randomized controlled trial; n number of patients analyzed for outcome, numbers refer to intervention/control in case of controlled studies; SMD and SE rounded by software package to two digits, confidence intervals were calculated by R package “meta” [37] from SMD/SE values calculated by R package “effect size” [35]. In cases of 0.00 as a confidence interval bound, the graph shows whether the original study reported a significant (s) or non-significant (ns) result, as the plotting function only shows two digits. For Mercer 2019 [92,93], effect sizes were taken from the original publication (adjusted SMD).
Risk of bias within studies
Only one study met the criteria prerequisite for a “strong” rating with the EPHPP instrument [60]. All other studies were rated as “weak” (Figure 2a, Appendix 4). Overall, potential selection bias, lack of blinding, as well as high attrition rates (in combination with missing information on drop-out reasons) were the main causes for concern regarding risk of bias within studies. As to their randomized controlled designs, two project evaluations [20,92,93] could be additionally assessed with the revised RoB 2 tool (Figure 2b).
Results of individual studies
Mental health
The most frequent instrument of assessment was the Hospital Anxiety and Depression scale (HADS), while a few studies used the Generalized Anxiety Disorder Scale-7 (GAD-7) and/or the Patient Health Questionnaire-9 (PHQ-9). SMD for one controlled [92,93] and two uncontrolled studies [12,74,75] could be either computed or extracted (Figure 5). Positive effects were found in uncontrolled studies with shorter time frames, as indicated by the SMDs calculated for the Kimberlee et al. [76] and Morton et al. studies [12], as well as in several uncontrolled studies for which standardized effect sizes could not be computed [13,16,40,41,43,44,56,59,60,61,69,70,80,81,87,91]. This could not be equally shown for controlled settings and longer follow-up periods, as illustrated by the effect sizes for the study by Mercer et al. [92,93]. Grant et al. [20] showed significant improvement in anxiety symptoms (HADS-A) but not in depressive symptoms (HADS-D) versus controls in an intermediate time frame. Carnes et al. [94,95,96] could also not show any long-term group differences for either measure. Regarding further data on mental health outcomes, two uncontrolled studies [78,80] showed unclear improvements on the GAD-7 and PHQ-9 scales in unclear or short follow-up periods.
Figure 5.
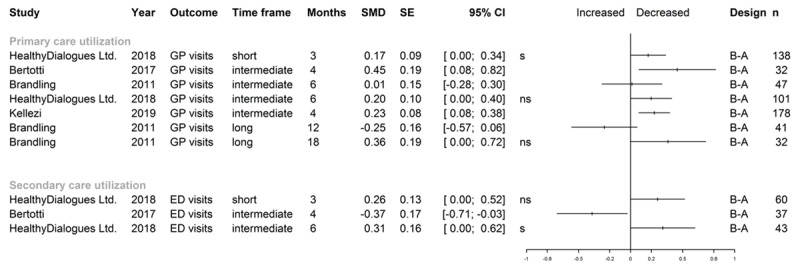
Effect sizes for health care utilization.
Note: GP general practitioner; ED emergency department; Time frame: short (0–3 months), intermediate (>3–6 months) and long term (>6 months); Follow-up time in months: in case of original study reporting follow-up in weeks, these were converted to 30-day months; B-A before-after study; n number of patients analyzed for outcome; SMD and SE rounded by software package to two digits, confidence intervals were calculated by R package “meta” [37] from SMD/SE values calculated by R package “effect size” [35]. In cases of 0.00 as a confidence interval bound, the graph shows whether the original study reported a significant (s) or non-significant (ns) result, as the plotting function only shows two digits.
Mental wellbeing
For mental wellbeing, the (Short) Warwick Edinburgh Mental Wellbeing Scale (SWEMWBS/WEMWBS) was the most frequently used outcome assessment tool. No controlled studies assessing mental wellbeing could be identified. SMDs could be computed for five uncontrolled studies [12,14,17,76,90] (Figure 3). Four evaluations showed large effects in a short follow-up period, and one evaluation with a small sample size showed no effect for SWEMWBS scores in an intermediate timeframe. This is accompanied by a number of uncontrolled studies with short or intermediate timeframes reporting improvements of mental wellbeing measures with altogether unclear clinical relevance [13,16,40,41,43,44,56,59,60,61,63,64,69,70,80,81,87,91].
Loneliness
Different scales were used to measure loneliness: University of California at Los Angeles (UCLA) Loneliness Scale, De Jong Gierveld Loneliness Scale, and Campaign to End Loneliness Tool. SMDs could be computed from three uncontrolled studies [15,39,90] (Figure 4). Two evaluations showed medium to large positive effects in a short or unknown follow-up period, one further evaluation showed no differences between pre and post in an intermediate time frame. We found eight further measures from six uncontrolled studies [13,43,70,71,72,79,84] with short to intermediate follow-up lengths, showing improvement with unclear clinical importance from pre to post intervention without information on the effect size.
Quality of life and general health
While most studies relied on different variations of the EQ-5D, two studies employed the WHO-Quol-Bref to measure quality of life [15,39]. For overall health, a general health Likert scale [17,94,95,96] and COOP/WONCA [20] were used. All three controlled studies and eleven uncontrolled before and after studies measured quality of life and general health at baseline and again at up to eight months after referral. SMDs for one controlled [92,93] and four uncontrolled studies [15,17,39,44,92,93] could be calculated or extracted (Figure 4). Positive effects were observed in a further number of uncontrolled studies [40,43,45,56,59,71,72,90]. This effect could not be shown in two controlled studies [92,93,94,95,96] for an intermediate timeframe. Grant et al. [20] indicated significant improvement in general health. This could not be seen in one uncontrolled [17] and one controlled study [94,95,96] for longer timeframes.
Self-efficacy
The Patient Activation Measure (PAM) and General Self-Efficacy Scale (GSE) were mainly used to report changes in self-efficacy [12,17,60,84]. We could compute the SMD for the GSE from Morton et al. [12], reporting a large positive effect in an unclear time frame (SMD = 0.85, 95% CI [0.65, 1.05]). Polley et al. and Elston et al. [60,84] reported clinically relevant increases in the PAM score, while Bertotti et al. [17] could not show any difference.
Health care utilization
Most frequent outcomes reported for health care resources use were longitudinal changes in utilization of primary care providers and emergency departments, reported as mean numbers of consultations for a period pre vs. post intervention/baseline. Results of studies for which effect sizes could be calculated (all were uncontrolled, Figure 5) suggest small to moderate effects in terms of reducing visits in primary or emergency hospital care. If longer time periods were observed, most pre-post studies permitting calculation of effect sizes did not show any significant changes in utilization.
Concerning primary care utilization, controlled studies painted a mixed picture. Carnes et al. [94,95,96] reported significant longitudinal consultation reductions for SP participants, while controls had significantly more visits in a pre-post comparison of annual utilization. In the study by Grant et al. [20], GP utilization in the post-randomization period was identical for intervention and control groups. Another study [84] including a health care utilization module with matched non-responder controls, showed a significant decline in the mean number of primary care visits in a three-month period for the intervention group, while there was no significant longitudinal change in controls. The cRCT by Mercer et al. [92,93] did only report GP utilization data at baseline. Regarding the considerable number of uncontrolled studies on primary care utilization for which data quality did not permit determination of effect sizes, reductions of unclear relevance were reported by many [40,43,56,62,69,70,74,75,76,85], but not all [66,68].
As to emergency department utilization trends in controlled studies, only the case-control study by Carnes et al. [94,95,96] reported relevant data, with a decline in visits in cases and an increase in controls for retrospective 3-month intervals from baseline and from the follow-up point at 8 months. Reported findings from a considerable number of pre-post studies likewise did not permit determination of effect sizes, and results were inconsistent, with pre-post reductions in visits registered by some [40,49,50,54,57,81,97], but not by others [43,55,60,79]. Extractable data was heterogeneous (means, percentages, absolute numbers), with measures of dispersion, confidence intervals, or tests of significance frequently missing (e.g. [55,56,76,77,81]).
Discussion
Summary of findings
In our systematic review, we found 68 reports from 53 different projects, with scarce evidence from controlled evaluations. Most frequently studied outcomes represent the domains of mental health and wellbeing, loneliness, quality of life, general health, self-efficacy, and health care utilization. Uncontrolled studies with shorter time frames showed mostly positive effects, while effects reported from studies with control groups or longer follow-up periods were smaller or inconsistent.
Evaluation of the evidence
The finding that controlled studies show positive effects less frequently calls for caution. SP effects could be non-specific consequences of being enrolled in a study, e.g. the feeling that someone cares. Regression towards the mean [99] might also be a problem because baseline values of certain outcomes (e.g. (S)WEMWBS) are quite low compared to the general public [40,76]. Effects seen could also be partially due to confounding, e.g. unknown concomitant interventions, as well as other sources of bias, e.g. selective dropout or social desirability [100].
As effect sizes could only be calculated for few studies and necessary information was often missing, clinical relevance of the evidence is difficult to judge. The results give reason to question sustainability, with longer-term studies tending to show smaller effects. The positive trends disappearing over time may be due to the complex problems of the target group: people referred to SP may have a plethora of problems related to e.g. low socioeconomic status, chronic illness or age. Temporarily alleviating one or two of the problems by counseling might be less beneficial in the long term, if the underlying destitute social situation remains [101,102].
Results in context
Our review is generally in line with preceding related works regarding the shortcomings of the available evidence and the need for further high-quality research, while providing the first evidence synthesis on SP quantifying effect sizes and applying methodologically rigorous standards of conduct and reporting. Two evidence syntheses by Bickerdike et al. [23] and Chatterjee et al. [103] have exclusively reviewed evidence from the NHS context, with studies from other settings not eligible for inclusion. Results of these works are presented narratively without attempts at comparative quantification of effects. In the Bickerdike review, 15 evaluations of SP programmes were included, primary outcomes were any measures of health and well-being or usage of health services. All included studies were rated as of high risk of bias, which corresponds to our assessment. Areas of methodological criticism encompassed lack of controls, missing data, and short follow-up, as well as non-standardized measuring instruments and unsatisfactory consideration of potential confounders. Authors consequently judged overall evidence as to the effectiveness of SP as inconclusive. Our findings also largely reflect the Chatterjee et al. review [103], which rated findings as overall positive while putting comparatively less emphasis on methodological shortcomings of the evidence. The risk of bias was only cursorily addressed in this review and not assessed systematically. Reinhardt et al. [21] have recently investigated the effectiveness of SP with loneliness as the outcome of interest, and collaterally addressed the impact on health care utilization. While not formally assessing risk of bias, authors stressed that available studies predominantly lacked control groups. They reported positive effects on loneliness-related score measures and health services usage reductions. Results were not synthesized quantitatively, and no effect sizes were reported. A further current systematic review by Portuguese researchers [104] published after the conclusion of our literature search included 13 studies on the effectiveness of SP. Most reports identified by this review are likewise represented in our literature pool, and authors judged evidence as weak, requiring further research. While our review project goes beyond this recent evidence synthesis regarding the scope of the literature search and the efforts to quantify effect sizes, conclusions essentially are in line with ours.
Strengths and limitations
For this systematic review, we employed a very comprehensive search strategy considering a wide range of bibliographic databases, performed citation tracking, as well as an extensive screening of the internet and of pertinent repositories for grey literature. By not relying exclusively on formally publicized evidence, this approach fits the special traits of SP research, which so far has been rather centered on pragmatic pilot intervention trials with ensuing report-style evaluations, and in this regard differs markedly from the rigorous conventions of conduct and reporting in clinical research. While the resulting body of literature is more challenging to synthesize and interpret, rejection of the evidence from non-controlled studies and non-peer-reviewed publications would have greatly narrowed the view on SP as it is practiced. Our international search focus also ensured that no evidence was missed on grounds of setting, even if results indicate that SP research is still overwhelmingly UK-centric. Lastly, our approach to compare evidence from different studies by calculation of effect sizes is novel in the field, with preceding reviews limited to mere descriptive summaries.
However, quantification was only possible for a minority of studies, and the necessity to refrain from meta-analysis is certainly a central limitation. While this would have been computationally feasible for the studies with SMD, it would certainly not have been scientifically permissible considering the heterogeneity of the study field. We found no comparative studies of different interventional approaches in the SP context aimed at identifying the most promising concept. As to the great heterogeneity and complexity, it was not possible to differentiate between specific SP models or components [97], although it would be plausible if some schemes would be more effective than others. Data did likewise not permit a substantiated distinction of different levels of intervention integration, with most studies for which effect sizes could be calculated classified as either medium or holistic. We also cannot tell whether other approaches (e.g. integration of social support services into primary care [100]), might be more promising than implementation of SP via a link worker. Neither were social prescribing schemes not involving outpatient medical providers considered in this review. Lastly, SP research is a rapidly evolving field, as indicated by the recentness of a major share of the publications included. Any literature review thus can only provide a snapshot and we may very well learn much more about SP effectiveness in the years to come.
Conclusion
The evidence located suggests positive effects of SP on a variety of relevant endpoints. Due to prevalent quality deficits in the available studies, scope for conclusions concerning clinical relevance and sustainability is limited. In this context, evidence quality rather than quantity is the problem. SP seems to be a promising integrated care approach for psychosocial problems in the primary care setting. For the UK, NHS policymakers have decided to gradually roll out SP services nationwide [105], which has the potential to broaden the evidence base. Evaluating the effectiveness of complex interventions is a major challenge [106] and requires considerable effort and resources. Recent efforts to address these issues by special techniques, e.g. difference-in-differences analyses using secondary data, are commendable [107]. However, randomized controlled trials with long-term follow-up and efforts to minimize attrition would be the most desirable and valuable approach. In this context, the use of adaptive designs and pragmatic trials might facilitate conducting successful RCTs in the complex field of social prescribing. Additional possible approaches for enhancing feasibility of randomized designs could be e.g. randomization and evaluation of communities and/or practice sites instead of individual patients, or trials including waiting list or stepped wedge designs.
Additional Files
The additional files for this article can be found as follows:
Search strategies.
Studies excluded in full text screening.
Study characteristics table.
EPHPP: traffic light plot.
Acknowledgements
We would like to thank our scientific advisory board for their valuable contributions.
Funding Statement
This work was supported by a grant from the German Federal Ministry for Education and Research (BMBF), funding ref 01EL2027A and 01EL2027B. The project team was independent of the funding body. The BMBF did not actively participate during the conduct of the project. We acknowledge financial support from the Open Access Publication Fund of Charité – Universitätsmedizin Berlin and the German Research Foundation (DFG).
Reviewers
Two anonymous reviewers.
Funding Information
This work was supported by a grant from the German Federal Ministry for Education and Research (BMBF), funding ref 01EL2027A and 01EL2027B. The project team was independent of the funding body. The BMBF did not actively participate during the conduct of the project.
We acknowledge financial support from the Open Access Publication Fund of Charité – Universitätsmedizin Berlin and the German Research Foundation (DFG).
Competing Interests
The authors declare no competing interests.
Author Contributions
CH, WJH and FH developed the project idea and acquired third party funding. HN, KK and FH wrote the protocol with input from WJH. HN, KK, DK and FH performed the literature searches. HN and DK screened the identified literature, extracted data from the included studies and performed the risk of bias assessment with help from KK. HN and FH performed data analyses and visualization. HN and FH wrote the manuscript with input from all co-authors. All authors approved the final manuscript.
References
- 1.Zimmermann T, Mews C, Kloppe T, Tetzlaff B, Hadwiger M, Von dem Knesebeck O, et al. Social problems in primary health care – prevalence, responses, course of action, and the need for support from a general practitioners’ point of view. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen. 2018; 131: 81–89. DOI: 10.1016/j.zefq.2018.01.008 [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. PLOS Medicine. 2010; 7(7): e1000316. DOI: 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016; 102(13): 1009–1016. DOI: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lorant V, Croux C, Weich S, Deliège D, Mackenbach J, Ansseau M. Depression and socio-economic risk factors: 7-year longitudinal population study. The British Journal of Psychiatry. 2007; 190: 293–298. DOI: 10.1192/bjp.bp.105.020040 [DOI] [PubMed] [Google Scholar]
- 5.North FM, Syme SL, Feeney A, Shipley M, Marmot M. Psychosocial work environment and sickness absence among British civil servants: the Whitehall II study. American Journal of Public Health. 1996; 86(3): 332–340. DOI: 10.2105/AJPH.86.3.332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shiels C, Gabbay MB, Ford FM. Patient factors associated with duration of certified sickness absence and transition to long-term incapacity. The British Journal of General Practice. 2004; 54(499): 86–91. [PMC free article] [PubMed] [Google Scholar]
- 7.Zantinge EM, Verhaak PFM, Kerssens JJ, Bensing JM. The workload of GPs: consultations of patients with psychological and somatic problems compared. The British Journal of General Practice. 2005; 55(517): 609–614. DOI: 10.1093/fampra/cmh732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popay J, Kowarzik U, Mallinson S, Mackian S, Barker J. Social problems, primary care and pathways to help and support: addressing health inequalities at the individual level. Part II: lay perspectives. Journal of Epidemiology & Community Health. 2007; 61(11): 972–977. DOI: 10.1136/jech.2007.061945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roland M, Everington S, Marshall M. Social prescribing-transforming the relationship between physicians and their patients. New England Journal of Medicine. 2020; 383(2): 97–99. DOI: 10.1056/NEJMp1917060 [DOI] [PubMed] [Google Scholar]
- 10.Islam MM. Social Prescribing—An Effort to Apply a Common Knowledge: Impelling Forces and Challenges. Frontiers in Public Health. 2020; 8: 515469. DOI: 10.3389/fpubh.2020.515469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodwin N. Understanding Integrated Care. International Journal of Integrated Care. 2016; 16(4): 6. DOI: 10.5334/ijic.2530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morton L, Ferguson M, Baty F. Improving wellbeing and self-efficacy by social prescription. Public Health. 2015; 129(3): 286–289. DOI: 10.1016/j.puhe.2014.12.011 [DOI] [PubMed] [Google Scholar]
- 13.Brown C, Hammond J, Jones M, Kimberlee R, BAB Community Researchers. Community Webs Final Evaluation Report. Southmead Development Trust, Bristol CCG, Bristol City Council, Bristol Ageing Better, and the University of the West of England; 2018. http://bristolageingbetter.org.uk/userfiles/files/CR06%20-%20Community%20Webs%20Final%20Evaluation%20Report.pdf [Accessed 25th November 2021]. [Google Scholar]
- 14.Crone DM, Sumner RC, Baker CM, Loughren EA, Hughes S, James DVB. ‘Artlift’ arts-on-referral intervention in UK primary care: updated findings from an ongoing observational study. European Journal of Public Health. 2018; 28(3): 404–409. DOI: 10.1093/eurpub/cky021 [DOI] [PubMed] [Google Scholar]
- 15.Aggar C, Caruana T, Thomas T, Baker J. Social prescribing as an intervention for people with work-related injuries and psychosocial difficulties in Australia. Advances in Health and Behavior. 2020; 3(1): 101–111. DOI: 10.25082/AHB.2020.01.001 [DOI] [Google Scholar]
- 16.Brandling J, House W, Howitt D, Sansom A. New routes: Pilot research project of a new social prescribing service provided in Keynsham. Bristol: Mental Health Research and Development Unit; 2011. https://www.pdffiller.com/87706080--New-Routes-Pilot-Social-Prescribing-Service-Final-Report-190911doc-thecareforum- [Accessed 25th November 2021]. [Google Scholar]
- 17.Bertotti M, Frostick C, Tong J, Netuveli G. The Social Prescribing service in the London Borough of Waltham Forest: final evaluation report. Institute for Health and Human Development (University of East London); 2017. https://repository.uel.ac.uk/download/d3ec62380e7d5b7df0ed83dee6a6cbaca008a847e81c97ce10641635e6554ac7/737495/final%20report%20-%20SP%20in%20Waltham%20Forest%20.pdf [Accessed 25th November 2021]. [Google Scholar]
- 18.Healthy Dialogues Ltd. Evaluation of the East Merton Social Prescribing Pilot. 2018. https://secureservercdn.net/160.153.138.163/ahi.b5c.myftpupload.com/wp-content/uploads/2019/04/East-Merton-Social-Prescribing-Evaluation-Report-2018.pdf [Accessed 25th November 2021].
- 19.Loftus AM, McCauley F, McCarron MO. Impact of social prescribing on general practice workload and polypharmacy. Public Health. 2017; 148: 96–101. DOI: 10.1016/j.puhe.2017.03.010 [DOI] [PubMed] [Google Scholar]
- 20.Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. British Medical Journal. 2000; 320(7232): 419–423. DOI: 10.1136/bmj.320.7232.419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reinhardt G, Vidovic D, Hammerton C. Understanding Loneliness: a Systematic Review of the Impact of Social Prescribing Initiatives on Loneliness. Perspectives in Public Health. 2021; 141(4): 204–213. DOI: 10.1177/1757913920967040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pescheny JV, Randhawa G, Pappas Y. The impact of social prescribing services on service users: a systematic review of the evidence. European Journal of Public Health. 2020; 30(4): 664–673. DOI: 10.1093/eurpub/ckz078 [DOI] [PubMed] [Google Scholar]
- 23.Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017; 7(4): e013384. DOI: 10.1136/bmjopen-2016-013384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holzinger F, Krüger K, Napierala H, Herrmann W. Social prescribing: systematic review of effectiveness of preventive psychosocial community referral interventions. PROSPERO; 2020. CRD42020182562. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020182562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis-Hall M. The Bromley by Bow Centre: harnessing the power of community. British Journal of General Practice. 2018; 68(672): 333. DOI: 10.3399/bjgp18X697733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. British Journal of General Practice. 2009; 59(563): 454–546. DOI: 10.3399/bjgp09X421085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department for Digital, Culture, Media and Sport. A connected society. A strategy for tackling loneliness: laying the foundations for change. London: Her Majesty’s Government; 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/748212/6.4882_DCMS_Loneliness_Strategy_web.pdf [Accessed 25th November 2021]. [Google Scholar]
- 28.Zotero [Software application]. Roy Rosenzweig Center for History and New Media. Washington, DC, USA: George Mason University; www.zotero.org. [Google Scholar]
- 29.Covidence [Software application]. Veritas Health Innovation, Melbourne, Australia; www.covidence.org. [Google Scholar]
- 30.Thomas BH, Ciliska D, Dobbins M, Micucci S. A Process for Systematically Reviewing the Literature: Providing the Research Evidence for Public Health Nursing Interventions. Worldviews on Evidence-Based Nursing. 2004; 1(3): 176–184. DOI: 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- 31.Deeks J, Dinnes J, D’Amico R, Sowden A, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technology Assessment. 2003; 7(27): 1–173. DOI: 10.3310/hta7270 [DOI] [PubMed] [Google Scholar]
- 32.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. British Medical Journal. 2019; 366: l4898. DOI: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 33.McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Research Synthesis Methods. 2021; 12(1): 55–61. DOI: 10.1002/jrsm.1411 [DOI] [PubMed] [Google Scholar]
- 34.NHS England. Social prescribing and community-based support: summary guide; 2020. https://www.england.nhs.uk/wp-content/uploads/2020/06/social-prescribing-summary-guide-updated-june-20.pdf [Accessed 25th November 2021].
- 35.Ben-Shachar MS, Lüdecke D, Makowski D. effectsize: Estimation of Effect Size Indices and Standardized Parameters. Journal of Open Source Software. 2020; 5(56): 2815. DOI: 10.21105/joss.02815 [DOI] [Google Scholar]
- 36.R: A language and environment for statistical computing Version 4.0.2 [Software application]. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- 37.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evidence-Based Mental Health. 2019; 22(4): 153–160. DOI: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. British Medical Journal. 2021; 372: n71. DOI: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aggar C, Thomas T, Gordon C, Bloomfield J, Baker J. Social Prescribing for Individuals Living with Mental Illness in an Australian Community Setting: A Pilot Study. Community Mental Health Journal. 2021; 57(1): 189–195. DOI: 10.1007/s10597-020-00631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Apteligen Ltd. Evaluation of Prevention Matters Buckinghamshire County Council Final Evaluation Report. Watford; 2015. http://docs.scie-socialcareonline.org.uk/fulltext/55826.pdf [Accessed 25th November 2021]. [Google Scholar]
- 41.Baines A. Rugby Social Prescribing Project ConnectWELL Harnessing community capacity to improve health and wellbeing Midterm Evaluation Report; 2015. https://docplayer.net/51921879-Rugby-social-prescribing-project-connectwell.html [Accessed 25th November 2021].
- 42.Baker C, Loughren EA, Ellis L, Crone D. Artlift Wiltshire Move On Groups Final Report. Cheltenham: University of Gloucestershire; 2017. https://artlift.org/wp-content/uploads/2019/02/2017-UoG-Artlift-Wiltshire-Move-on-Groups-Final-Report.pdf [Accessed 25th November 2021]. [Google Scholar]
- 43.Bertotti M, Frostick C, Temirov O. An evaluation of Social Prescribing in the London Borough of Redbridge: final evaluation report. Institute for Health and Human Development (University of East London); 2020. https://repository.uel.ac.uk/download/b166f8139440a6183a11e5756431965c13846b3c8716079c07ec309a5d258586/1290254/Final%20evaluation%20draft%20report%20Redbridge%20SP%20100920%20final.pdf [Accessed 13th October 2020]. [Google Scholar]
- 44.Bertotti M, Temirov MO, Lane W. Outcome and economic evaluation of City and Hackney Social Prescribing scheme. Institute for Health and Human Development (University of East London); 2020. https://repository.uel.ac.uk/item/887zw [Accessed 17th May 2021]. [Google Scholar]
- 45.Beynon P, Burdis G, Hoadley J, Jensen A, Beardmore A, Jones M, et al. Bristol Ageing Better Community Navigators Service: final evaluation report of a social prescribing initiative addressing loneliness and social isolation amongst older people. UWE Bristol; 2020. https://www.tnlcommunityfund.org.uk/media/insights/documents/Community-Navigators-Report2020-for-SCREEN.pdf?mtime=20201202121938&focal=none [Accessed 25th November 2021]. [Google Scholar]
- 46.Tower Hamlets CCG Network 6 – Bromley by Bow and Mile End East. Social Prescribing Service Bromley by Bow Centre Annual Report: April 2018 – March 2019; 2019. https://www.bbbc.org.uk/wp-content/uploads/2019/09/BBBC-Social-Prescribing-Annual-Report-April-2018-March-2019-FINAL.pdf [Accessed 25th November 2021].
- 47.Crone DM, O’Connell EE, Tyson PJ, Clark-Stone F, Opher S, James DVB. ‘Art Lift’ intervention to improve mental well-being: An observational study from UK general practice. International Journal of Mental Health Nursing. 2013; 22(3): 279–286. DOI: 10.1111/j.1447-0349.2012.00862.x [DOI] [PubMed] [Google Scholar]
- 48.Sumner RC, Crone DM, Baker C, Hughes S, Loughren EA, James DVB. Factors associated with attendance, engagement and wellbeing change in an arts on prescription intervention. Journal of Public Health. 2020; 42(1): e88–e95. DOI: 10.1093/pubmed/fdz032 [DOI] [PubMed] [Google Scholar]
- 49.Dayson C, Bashir N. The social and economic impact of the Rotherham Social Prescribing Pilot: Main evaluation report. CRESR, Sheffield Hallam University; 2014. https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/social-economic-impact-rotherham.pdf [Accessed 25th November 2021]. [Google Scholar]
- 50.Dayson C, Bashir N, Bennett E, Sanderson E. The Rotherham social prescribing service for people with long-term health conditions Summary report. CRESR, Sheffield Hallam University; 2016. https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/rotherham-social-prescribing-summary-report-2016_7_0.pdf [Accessed 25th November 2021]. [Google Scholar]
- 51.Dayson C, Bennett E. Evaluation of Doncaster Social Prescribing Service: Understanding outcomes and impact. CRESR, Sheffield Hallam University; 2016. http://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/eval-doncaster-social-prescribing-service.pdf [Accessed 25th November 2021]. [Google Scholar]
- 52.Dayson C, Bennett E. Evaluation of the Rotherham mental health social prescribing service 2015/16/-2016/17. CRESR, Sheffield Hallam University; 2017. http://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/eval-rotherham-health-social-prescribing-2015-2017.pdf [Accessed 25th November 2021]. [Google Scholar]
- 53.Dayson C, Bennett E. Evaluation of the Rotherham Mental Health Social Prescribing Pilot. CRESR Sheffield Hallam University; https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/eval-rotherham-mental-health-social-prescribing.pdf [Accessed 25th November 2021]. [Google Scholar]
- 54.Dayson C, Damm C. The Rotherham Social Prescribing Service for People with long-term conditions: evaluation update. CRESR, Sheffield Hallam University; 2017. http://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/rotherham-social-prescribing-evaluation-update.pdf [Accessed 25th November 2021]. [Google Scholar]
- 55.Dayson C, Damm C. Evaluation of the Rotherham social prescribing service for long term conditions: a review of data for 2016/17–2017/18. CRESR, Sheffield Hallam University; 2020. https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/eval-rotherham-social-prescribing-long-term-conditions-17-18.pdf [Accessed 25th November 2021]. [Google Scholar]
- 56.Dayson C, Leather D. Evaluation of Hale Community Connectors Social Prescribing Service 2017. CRESR, Sheffield Hallam University; 2018. http://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/eval-HALE-community-connectors-social-prescribing.pdf [Accessed 25th November 2021]. [Google Scholar]
- 57.Dayson C, Bashir N, Bennett E, Sanderson E. The Rotherham Social Prescribing Service for People with Long-Term Health Conditions: Annual Report. CRESR, Sheffield Hallam University; 2016. https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/rotherham-social-prescribing-annual-eval-report-2016_7.pdf [Accessed 25th November 2021]. [Google Scholar]
- 58.Dayson C, Bennett E. Key Findings from the Evaluation of the Rotherham Mental Health Social Prescribing Pilot. CRESR, Sheffield Hallam University; 2016. http://shura.shu.ac.uk/25785/1/eval-rotherham-mental-health-social-prescribing-key-findings.pdf [Accessed 25th November 2021]. [Google Scholar]
- 59.Dayson C, Leather D. Evaluation of HALE Community Connectors Social Prescribing Service 2018–19. CRESR, Sheffield Hallam University; 2020. http://shura.shu.ac.uk/25768/1/eval-HALE-comm-connectors-social-prescribing-service-2018-19.pdf [Accessed 25th November 2021]. [Google Scholar]
- 60.Elston J, Gradinger F, Asthana S, Lilley-Woolnough C, Wroe S, Harman H, et al. Does a social prescribing ‘holistic’ link-worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care use and costs? A 12-month before-and-after evaluation. Primary Health Care Research & Development. 2019; 20: e135. DOI: 10.1017/S1463423619000598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.ERS. Newcastle social prescribing project: Final report; 2013. http://phw.soutron.net/Library/Catalogues/Controls/Download.aspx?id=161 [Accessed 25th November 2021].
- 62.Ferguson K, Hogarth S. Social Prescribing in Tower Hamlets: Evaluation of Borough-wide Roll-out; 2018. https://www.stokeccg.nhs.uk/your-ccg/ns-publications/generic-publications/1331-tower-hamlets-social-prescribing-evaluation-final-full-report-03-2018/file [Accessed 25th November 2021].
- 63.Friedli L, Themessl-Huber M, Butchart M. Evaluation of Dundee Equally Well Sources of Support: Social Prescribing in Maryfield Evaluation Report Four; 2012. https://www.northstaffsccg.nhs.uk/your-ccg/ns-publications/generic-publications/1324-social-prescribing-evaluation-dundee/file [Accessed 25th November 2021].
- 64.Foster A, Thompson J, Holding E, Ariss S, Mukuria C, Jacques R, et al. Impact of social prescribing to address loneliness: A mixed methods evaluation of a national social prescribing programme. Health & Social Care in the Community. 2021; 29(5): 1439–1449. DOI: 10.1111/hsc.13200 [DOI] [PubMed] [Google Scholar]
- 65.Foster A, Akparibo R, Ariss S, Thompson J, Holding E, Mukuria C. Tackling loneliness and isolation: findings from the evaluation of our Connecting Communities service. London; 2019. https://www.sheffield.ac.uk/media/6027/download [Accessed 18th October 2021]. [Google Scholar]
- 66.Grayer J, Cape J, Orpwood L, Leibowitz J, Buszewicz M. Facilitating access to voluntary and community services for patients with psychosocial problems: a before-after evaluation. BMC Family Practice. 2008; 9(1): 27. DOI: 10.1186/1471-2296-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Holt NJ. Tracking momentary experience in the evaluation of arts-on-prescription services: using mood changes during art workshops to predict global wellbeing change. Perspectives in Public Health. 2020; 140(5): 270–276. DOI: 10.1177/1757913920913060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Howarth M, Griffiths A, da Silva A, Green R. Social prescribing: a ‘natural’ community-based solution. British Journal of Community Nursing. 2020; 25(6): 294–298. DOI: 10.12968/bjcn.2020.25.6.294 [DOI] [PubMed] [Google Scholar]
- 69.Jones C, Lynch M. Spice Time Credits Social Precribing Pilot Evaluation. Cardiff University & Bangor University; 2018. http://socialvalue.bangor.ac.uk/documents/SPICE%20Time%20Credits%20Social%20Prescribing%20Pilot%20Final%20Report.pdf [Accessed 25th November 2021]. [Google Scholar]
- 70.Jones C, Lynch M. Grow Well Social Prescribing Pilot Evaluation. Cardiff University & Bangor University; 2018. http://socialvalue.bangor.ac.uk/documents/Grow%20Well%20Social%20Prescribing%20Pilot%20Final%20Report.pdf [Accessed 25th November 2021]. [Google Scholar]
- 71.Kellezi B, Wakefield JRH, Stevenson C, McNamara N, Mair E, Bowe M, et al. The social cure of social prescribing: a mixed-methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ open. 2019; 9(11): e033137. DOI: 10.1136/bmjopen-2019-033137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wakefield JRH, Kellezi B, Stevenson C, McNamara N, Bowe M, Wilson I, et al. Social Prescribing as ‘Social Cure’: A longitudinal study of the health benefits of social connectedness within a Social Prescribing pathway. Journal of Health Psychology; 2020. DOI: 10.1177/1359105320944991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kensington & Chelsea Social Council. Self-Care Social Prescribing; 2018. https://socialvalueuk.org/wp-content/uploads/2018/04/KCSC-WLCCG-Self-Care-social-prescribing-SROI-2018_ENVOY.pdf [Accessed 25th November 2021].
- 74.Kimberlee R. What is the value of social prescribing? Advances in Social Sciences Research Journal. 2016; 3(3). DOI: 10.14738/assrj.33.1889 [DOI] [Google Scholar]
- 75.Kimberlee R, Ward R, Jones M, Powell J. Measuring the economic impact of the wellspring healthy living centre’s social prescribing wellbeing programme for low level mental health issues encountered by GP services. Faculty of Health and Life Sciences University of the West of England; 2014. http://www.wellspringhlc.org.uk/reports/POV_Final_Report_March_2014.pdf [Accessed 25th November 2021].
- 76.Kimberlee RH. Gloucestershire clinical commissioning group’s social prescribing service: Evaluation report. Faculty of Health and Life Sciences University of the West of England; 2016. https://uwe-repository.worktribe.com/output/905835 [Accessed 25th November 2021]. [Google Scholar]
- 77.Liles A, Darnton P. Social Prescribing in Wessex Understanding its impact and supporting spread; 2017. https://wessexahsn.org.uk/img/projects/Wessex%20Social%20Prescribing-1529938576.pdf [Accessed 25th November 2021].
- 78.Longwill A. Independent Evaluation of Hackney Well Family Service, Family Action; 2014. https://www.family-action.org.uk/content/uploads/2014/07/WellFamily-Evaluation-Executive-Summary.pdf [Accessed 25th November 2021].
- 79.Massie R, Ahmad N. An evaluation of Wolverhampton’s social prescribing service: a new route to wellbeing. Wolverhampton; 2019. https://issuu.com/universityofwolverhampton/docs/social_prescribing_evaluation_repor [Accessed 25th November 2021]. [Google Scholar]
- 80.Maund PR, Irvine KN, Reeves J, Strong E, Cromie R, Dallimer M, et al. Wetlands for Wellbeing: Piloting a Nature-Based Health Intervention for the Management of Anxiety and Depression. International Journal of Environmental Research and Public Health. 2019; 16(22). DOI: 10.3390/ijerph16224413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Palmer D, Wheeler J, Hendrix E, Sango PN, Hatzidimitriadou E. Social prescribing in Bexley: pilot evaluation report. Canterbury Christ Church University; 2017. https://mindinbexley.org.uk/wp-content/uploads/2020/01/Social-Prescribing-in-Bexley-Pilot-Evaluation-Report.pdf [Accessed 25th November 2021]. [Google Scholar]
- 82.Pescheny JV, Gunn LH, Pappas Y, Randhawa G. The impact of the Luton social prescribing programme on mental well-being: a quantitative before-and-after study. Journal of Public Health (Oxford). 2021; 43: e69–76. DOI: 10.1093/pubmed/fdz155 [DOI] [PubMed] [Google Scholar]
- 83.Pescheny JV. An evaluation of the implementation and practice of social prescribing. University of Bedfordshire; 2019. https://uobrep.openrepository.com/bitstream/handle/10547/623576/PESCHENY_repository%20version.pdf?sequence=1&isAllowed=y [Accessed 25th November 2021]. [Google Scholar]
- 84.Polley M, Seers H, Fixsen A. Evaluation Report of the Social Prescribing Demonstrator Site in Shropshire – Final Report. London: University of Westminster; 2019. https://www.researchgate.net/publication/339428473_Evaluation_Report_of_the_Social_Prescribing_Demonstrator_Site_in_Shropshire_-Final_Report [Accessed 25th November 2021]. [Google Scholar]
- 85.Smith B, Moran R, Smalley J. Social Prescribing end of project report. 2017. https://valonline.org.uk/wp-content/uploads/2019/04/WEB-version-social-prescribing-End-of-Project-.pdf [Accessed 25th November 2021].
- 86.Thomson LJ, Morse N, Elsden E, Chatterjee HJ. Art, nature and mental health: assessing the biopsychosocial effects of a ‘creative green prescription’ museum programme involving horticulture, artmaking and collections. Perspectives in Public Health. 2020; 140(5): 277–285. DOI: 10.1177/1757913920910443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vogelpoel N, Jarrold K. Social prescription and the role of participatory arts programmes for older people with sensory impairments. Journal of Integrated Care. 2014; 22(2): 39–50. DOI: 10.1108/JICA-01-2014-0002 [DOI] [Google Scholar]
- 88.Weld S, Kimberlee R, Biggs O, Blackburn K, Clifford Z, Jones M. For All Healthy Living Centre’s Healthy Connections Project. Final evaluation report and Social Return on Investment (SROI) Analysis; 2015. https://uwe-repository.worktribe.com/output/844999/for-all-healthy-living-centres-healthy-connections-project-final-evaluation-report-and-social-return-on-investment-sroi-analysis [Accessed 25th November 2021].
- 89.Wellbeing Enterprises CIC. ‘Ways to Wellbeing’ Social Prescribing Programme Social Impact Report 2019; 2019. https://www.wellbeingenterprises.org.uk/core/media/Ways-to-Wellbeing-2019-DIGITAL.pdf [Accessed 25th November 2021].
- 90.Woodall J, Trigwell J, Bunyan A-M, Raine G, Eaton V, Davis J, et al. Understanding the effectiveness and mechanisms of a social prescribing service: a mixed method analysis. BMC Health Services Research. 2018; 18(1): 604. DOI: 10.1186/s12913-018-3437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.York CVS. Ways to Wellbeing The impact of social prescribing in York; 2019. https://www.yorkcvs.org.uk/wp-content/uploads/2019/02/WTW_Evaluation_A4_FinalPDF-Electronic.pdf [Accessed 25th November 2021].
- 92.Mercer SW, Fitzpatrick B, Grant L, Chng NR, McConnachie A, Bakhshi A, et al. Effectiveness of Community-Links Practitioners in Areas of High Socioeconomic Deprivation. Annals of Family Medicine. 2019; 17(6): 518–525. DOI: 10.1370/afm.2429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mercer S, Wyke S, Fitzpatrick B, McConnachie A, O’Donnell K, Mackenzie M, et al. Evaluation of the Glasgow ‘Deep End’ Links Worker Programme. NHS Health Scotland; 2017. http://www.healthscotland.com/documents/29438.aspx [Accessed 17th May 2021].
- 94.City and Hackney Clinical Commissioning Group and, University of East London. Shine 2014 final report Social Prescribing: integrating GP and Community Assets for Health; 2015. https://www.health.org.uk/sites/default/files/City%20and%20Hackney%20CCG%20final%20report.pdf [Accessed 25th November 2021].
- 95.Carnes D, Sohanpal R, Matthur R, Homer K, Hull SA, Bertotti M, et al. City and Hackney Social Prescribing Service: Evaluation Report; 2015. https://www.researchgate.net/publication/286354138_City_and_Hackney_Social_Prescribing_Service_Evaluation_Report [Accessed 25th November 2021].
- 96.Carnes D, Sohanpal R, Frostick C, Hull S, Mathur R, Netuveli G, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Services Research. 2017; 17(1): 835. DOI: 10.1186/s12913-017-2778-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dayson C, Bashir N, Pearson S. From dependence to independence: emerging lessons from the Rotherham Social Prescribing Pilot. CRESR, Sheffield Hallam University; 2013. http://shura.shu.ac.uk/26799/1/rotherham-social-prescribing-summary.pdf [Accessed 25th November 2021]. [Google Scholar]
- 98.Kimberlee R. What is social prescribing? Advances in Social Sciences Research Journal. 2015; 2(1). DOI: 10.14738/assrj.21.808 [DOI] [Google Scholar]
- 99.Bland JM, Altman DG. Regression towards the mean. British Medical Journal. 1994; 308(6942): 1499. DOI: 10.1136/bmj.308.6942.1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Delgado-Rodríguez M, Llorca J. Bias. Journal of Epidemiology & Community Health. 2004; 58(8): 635–641. DOI: 10.1136/jech.2003.008466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, et al. Variation In Health Outcomes: The Role Of Spending On Social Services, Public Health, And Health Care, 2000–09. Health Affairs. 2016; 35(5): 760–768. DOI: 10.1377/hlthaff.2015.0814 [DOI] [PubMed] [Google Scholar]
- 102.Butler SM, Matthew DB, Cabello M. Re-balancing medical and social spending to promote health: Increasing state flexibility to improve health through housing. Center for Health Policy at Brookings and the USC Schaeffer Center for Health Policy & Economics; 2017. https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2017/02/15/re-balancing-medical-and-social-spending-to-promote-health-increasing-state-flexibility-to-improve-health-through-housing/ [Accessed 25th November 2021].
- 103.Chatterjee HJ, Camic PM, Lockyer B, Thomson LJ. Non-clinical community interventions: a systematised review of social prescribing schemes. Arts & Health. 2018; 10(2): 97–123. DOI: 10.1080/17533015.2017.1334002 [DOI] [Google Scholar]
- 104.Costa A, Sousa CJ, Seabra PRC, Virgolino A, Santos O, Lopes J, et al. Effectiveness of Social Prescribing Programs in the Primary Health-Care Context: A Systematic Literature Review. Sustainability. 2021; 13(5): 2731. DOI: 10.3390/su13052731 [DOI] [Google Scholar]
- 105.NHS ENGLAND. Universal personalised care: implementing the comprehensive model. London: NHS England; 2019. https://www.england.nhs.uk/wp-content/uploads/2019/01/universal-personalised-care.pdf [Google Scholar]
- 106.Goodwin N. Understanding and Evaluating the Implementation of Integrated Care: A ‘Three Pipe’ Problem. International Journal of Integrated Care. 16(4): 19. DOI: 10.5334/ijic.2609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wildman J, Wildman JM. Evaluation of a Community Health Worker Social Prescribing Program Among UK Patients With Type 2 Diabetes. JAMA Network Open. 2021; 4(9): e2126236. DOI: 10.1001/jamanetworkopen.2021.26236 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies.
Studies excluded in full text screening.
Study characteristics table.
EPHPP: traffic light plot.


