Abstract
Background:
According to the 2019 Global Burden of Disease (GBD) report, India contributes to an estimated 12.9% of global asthma cases (34.3 million) but a disproportionate 42.3% of all global asthma deaths. Also, asthma causes 4.83 million disability-adjusted life years (DALYs) annually in India, four times more than China, which ranks second.
Hypothesis:
We hypothesised that this disproportionate increase in asthma deaths and suffering in India could be due to the under-use of inhaled corticosteroids.
Methods:
Using the estimated number of asthma cases in each state and union territory in India (34.3 million) from the 2019 GBD data, we calculated the expected sales of inhaled corticosteroids (ICS) for asthmatics in India. We assumed that 10% of asthmatics have mild intermitted disease and thus need only 4 units of ICS pMDI per year. The remaining 90% should ideally use 12 units of ICS pMDI or equivalent DPI. We also assumed that 30% of ICS sales in India would be accounted for by the 38 million COPD patients. State-wise actual sales of ICS in India were obtained from IQVIA.
Results:
The total amount of ICS sales in India for asthma obtained from IQVIA was 26.4 million versus the 384.16 million expected sales, which is only 6.8% of the required estimated sales. Moreover, when we correlated state-wise actual sales of ICS in India versus asthma mortality and DALYs (per 100,000 population), we found a significant negative correlation (R = −0.56; P < 0.001 for asthma deaths and R = −0.61; P < 0.001 for asthma DALYs).
Impact and Future Direction:
Policy-makers, health care providers, public health researchers, asthma sufferers and the people at large need to take cognizance of our findings and undertake appropriate measures, such as creating awareness and ensuring availability and regular use of ICS by asthmatics in India.
Keywords: Asthma, inhaled corticosteroids, underuse
BACKGROUND
The 2019 Global Burden of Disease (GBD) report revealed some alarming observations about asthma in India. India has the largest number of asthmatics in the world (34.3 million), having just overtaken the USA. While deaths due to asthma in most developed countries have declined steadily, the deaths due to asthma in India increased by 33% from 1990 (149,454 to 198,798). India now contributes to an alarming 42.4% of all global asthma deaths, although it accounts for only 12.9% of the global asthma cases. Moreover, India ranks number one in the world for disability-adjusted life years (DALYs) due to asthma (5.83 million), four times above China (1.41 million), which ranks second. These shocking figures of asthma suffering and deaths in India is a serious wakeup call for policy-makers, healthcare providers, researchers, pharmacists and the people at large and demands for an urgent need to understand the reasons behind this and address these on a war footing level.
In 2015, the Asthma Insights and Management (AIM) survey highlighted the poor state of affairs about asthma management in India.[1,2] This global survey examined asthma management related issues in the USA, Canada, four countries in Europe, five countries in Latin America and nine countries in the Asia-Pacific region, including India, and reported that among the 20 countries studied, asthmatics from India had the most number of bothersome day-time and night-time symptoms, had the poorest quality of life and the most number of absenteeism’s from school or work. None of the 400 randomly selected asthmatics from the eight cities and towns in India had well-controlled asthma when evaluated objectively. Less than one third of the asthmatics in India reported the use of inhalers for asthma treatment; 50% reported the use of oral medications for asthma control, and oral corticosteroids were used by 89% of the asthmatics in the previous 1 year. Prescription audit studies from Delhi,[3] Kolkata[4] and Gorakhpur[5] showed that less than one third of the asthmatics were prescribed inhaled medications, and among these, only a small proportion received inhaled steroids on a regular basis. Most patients in India received only reliever medications, be it inhaled short-acting beta-agonists or oral beta-agonists and theophyllines.
With the understanding that asthma is an inflammatory disease of the airways, the introduction of anti-inflammatory inhaled corticosteroids in the 1990s revolutionised its treatment.[6] Either alone or in combination with long-acting beta-agonists, inhaled corticosteroids have been shown to significantly improve symptoms and quality of life and reduce asthma exacerbations, need for hospitalisation and asthma deaths.[7,8] Countries where ICS is used regularly have shown a steady decline in death rates and DALYs due to asthma.[9,10,11] In Saskatechewan, Suissa et al.[9] showed that use of more than six canisters of ICS per year (out of 12) was associated with a 50% reduction in asthma deaths. These observations enhanced the appreciation of the pivotal role for ICS in reducing’ with ‘These observations highlight the pivotal role for ICS in reducing asthma suffering and deaths. More recently, the use of inhaled corticosteroids has been shown to be beneficial and necessary even in subjects with mild intermittent asthma,[12] and this has now been included in the latest Global Initiative for Asthma (GINA) guidelines.[13]
Hypothesis: We hypothesised that the increased suffering and deaths associated with asthma in India may be due to the under-use of inhaled corticosteroids. We aimed to investigate this by studying the correlation between the national sales of ICS in India versus asthma mortality and DALYs across different states and union territories in India.
STUDY METHODS
We obtained state-wise sales of inhaled corticosteroids (via both pressurised metered-dose inhalers and dry-powder inhalers) across India from the IQVIA database, and asthma mortality and DALYs were obtained from the Global Burden of Disease 2019 data set.
IQVIA, a merger of Intercontinental Marketing Services (IMS) Health and Quintiles, is one of the largest data science organisations in the pharmaceutical industry. They provide data related to pharmaceutical sales, prescriptions, prescribers and patient-level information, which can be used to analyse further to draw insights. We used data from IQVIA to source the monthly sales of inhaled corticosteroids (either singly or in combination with beta-agonists) both in the pMDI as well as DPI forms for all states and union territories in India. One canister of pMDI containing ICS (either alone or with beta-agonist) has 120 doses, which if taken twice a day lasts for a month. One-unit sale of ICS pMDI, therefore, lasts for 1 month. The single-dose DPIs are sold in boxes of 30 capsules that last 15 days; therefore, two bottles of unit-dose ICS DPIs are required for a month’s supply. Very few multi-dose DPIs are used in India (<1%). Therefore, we considered two bottles of unit-dose DPIs as equivalent to one unit of ICS. For 1 year, each asthma patient is expected to use either 12 units of pMDI or 24 units of single-dose DPI. We obtained monthly unit sales data for the last 1 year (2019–2020) from all states and union territories in India.
The data on deaths and DALYs for asthma for every state in India were obtained from the Global Burden of Disease (GBD) website, which is an open-source data site (https://vizhub.healthdata.org/gbd-compare/india). On the dashboard of the GBD-India website, by using the advanced settings, DALYs and death rates were obtained for all age groups and both genders for all states and UTs in India with the cause entered as asthma. The GBD-India dashboard gives an option to download the state-wise data. On selecting the required parameters of deaths, DALYs, gender and age groups, the data were downloaded from the GBD website in an excel format for further analysis.
Data analysis
Asthma severity is divided into mild intermittent, mild persistent, moderate and severe. ICS use is recommended for all severities; however, in mild intermittent disease, the use of ICS is recommended only on a when-required basis. In all other severities, regular use of ICS is recommended with or without a combination with long-acting beta-agonists. We assumed that in India, 10% of the asthmatics have mild intermittent disease and would use up to 4 units of ICS containing pMDIs per year or 8 units of single-dose DPIs; the remaining 90% of asthmatics should ideally need to use 12 units of ICS pMDIs or 14 units of single-dose DPIs per year.
Therefore, 10% of 34.3 million, that is, 3.43 million × 4 = 13.72 million units plus 90% of 34.3 million, that is, 30.87 million × 12 units a year = 370.44 million units of ICS would be required. In an ideal state, 13.72 + 370.44 = 384.16 million units of ICS should be sold every year in India for the 34.3 million asthmatics.
RESULTS
Data collected from IQVIA showed that the total sales of ICS-containing drugs (both pMDI and DPI for all brands in India) in all states and union territories for 1 year was 39.61 million units.
If we assume that all ICS units that are sold in India are used only by asthmatics, then 39.61/384.16 × 100 = 10.3% is the use of ICS by asthmatics in India (best-case scenario). However, ICS is also prescribed for COPD patients. There are an estimated 38 million COPD patients in India (GBD 2019 data). If we assume that 1/3rd of the ICS units sold in India (i.e. 13.2 million units) are also used by patients of COPD, then only 26.4 million units would be used by asthmatics, which reduces the proportion of ICS use in asthma to 6.8% (26.4 million/384.16 million). The total use of ICS by asthmatics in India is likely to be between 6.8% and 10.3%. This suggests that there is over 90% of under-use of ICS by asthmatic patients in India.
Correlation between ICS sales in different states and union territories in India versus state-wise asthma mortality and DALYs
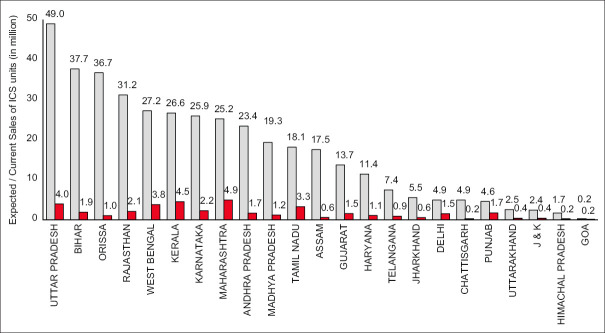
We examined the correlation between the unit sales of ICS containing inhalers in each state/union territory versus state-wise asthma deaths per 100,000 and found a strong negative correlation (R = –0.57; P < 0.006) [Figure 1]. States that had the highest sales of ICS containing inhalers had lower asthma death rates, and states that had low sales of ICS containing inhalers had higher asthma deaths.
Figure 1.
Correlation between state and union territory-wise unit sales of ICS (as proportion) versus asthma deaths per 100 K people in India
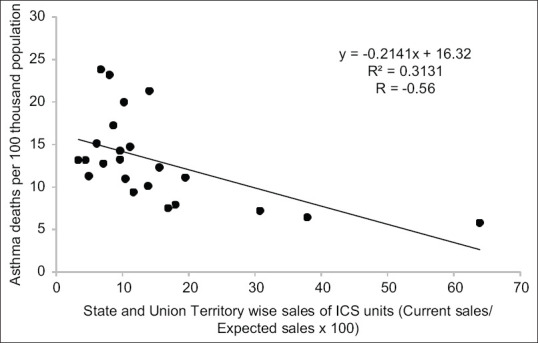
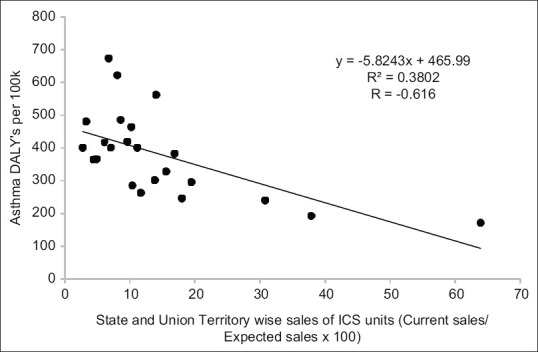
We found a similar but stronger negative correlation between state-wise ICS sales and state-wise DALYS per 100,000 in India (R = –0.616, P < 0.002) [Figure 2]. In Figure 3, we show the actual sales of ICS units versus ideal expected sales of ICS units for different states and union territories in India. States like Goa, Punjab and Maharashtra have relatively higher sales of ICS for the number of asthmatics in their states, while states like Odisha and Rajasthan have very low sales of ICS for their asthma population.
Figure 2.
Correlation between state and union territory-wise unit sales of ICS (as proportion) versus asthma DALYs per 100 K people in India
Figure 3.
Expected sales (grey bars) and current sales (red bars) of ICS units across different states and union territories in India based on estimated number of asthmatics in every state according to the 2019 GBD report
DISCUSSION
For the estimated 34.2 million asthmatics in India, the sale of ICS is less than 10% of what it should ideally be. To the best of our knowledge, this is the first study that has shown evidence for gross under-use of ICS for asthma treatment in India. Furthermore, we found a strong negative correlation between the sales of ICS in different states and union territories in India with asthma deaths and DALYs, suggesting that under-use of ICS in India may be contributing to asthma suffering and deaths. The observations made in our study likely explain why India contributes to 42.4% of all global asthma deaths. The findings of this study are an important message for healthcare providers, healthcare policy-makers, asthma patients, public health researchers and for the people at large and is a wake-up call to start mending things on a war-footing basis.
Under-use of ICS in India could be accounted for by various reasons.
Inadequate Medical Education/Training of doctors: An estimated 90,000 doctors train in modern medicine from government and private medical schools pass out each year in India. Most of them receive inadequate training in asthma diagnosis and management. Most government teaching hospitals in India do not have inhaled medications for the treatment of asthma, and almost all asthma patients in medical school-associated hospitals, especially the government-run teaching hospitals, are treated with tablets salbutamol and theophylline as the mainline treatment for asthma. Undergraduate students who are undergoing training in these hospitals believe that that is the correct treatment for asthma. Moreover, there is no emphasis on teaching how to use inhaler devices correctly in the undergraduate curriculum; therefore, more than 90% of undergraduate students do not know how to use inhaler devices correctly, and many of them even believe that inhalers are addictive. Even post-graduate students of Medicine, Respiratory Medicine and Paediatrics are not exposed to the correct use of inhaled steroids in asthma management as these drugs are not available in the pharmacy.[14] Lack of adequate training about asthma management and lack of availability of essential inhaled medications contribute in a major way to the under-use of ICS in asthma.
Healthcare Delivery in Public Hospitals: Around 20%–30% of patients in India, mostly those who belong to the lower socio-economic strata, visit public hospitals, where treatment is either free or substantially reduced. The remaining patients visit private doctors and have to pay out of their pocket for the consultancy and drugs. The public-run primary care clinics/hospitals do not have adequate diagnostic or therapeutic facilities for asthma. Most doctors lack the knowledge, skill set and confidence to diagnose and manage asthma and thus prescribe only oral medications for asthma because they are the only available asthma drugs. Although the WHO has recommended the need to have salbutamol, beclomethasone and budesonide inhalers as essential asthma medicines to be present in all public care facilities in all countries[15] and the Ministry of Health and Family Welfare, Government of India has also included these drugs in the essential drug list to be available in all public primary, secondary and tertiary care clinics/hospitals, in reality, they are not available in almost all public health centres.[16] Rajasthan was the only state that showed availability of inhaled salbutamol and beclomethasone in public health centres, but this was restricted to only the government hospital in Jaipur.[17]
Healthcare Delivery in Private Clinics/Hospitals: Out of the 1.5 million registered doctors in India, 0.8 million doctors are trained in Alternative Forms of Medicine (Ayurveda, Homeopathy, Siddhi, Naturopathy etc.). They are not taught the modern principles of medicine and are actively discouraged to use inhalers and steroids for asthma treatment because of the perceived addictive and side effects concerns. A proportion of doctors trained in alternative forms of medicine do practice modern medicine as well, but only a small minority of them use inhaled steroids in the management of asthma. They either receive this knowledge through attending conferences or are influenced by the medical representatives of various pharmaceutical companies who visit them. Those doctors who are trained in modern medicine lack adequate knowledge, skill set and confidence in diagnosing and treating asthma. Inhaled medications are prescribed in a small proportion of asthmatics, and an even smaller proportion get prescribed inhaled steroids. In a study from Delhi in 2008, 72% of GPs reported salbutamol as the preferred prevention for asthma, and inhaled medications was recommended by only 25% of GPs.[18] Generally, physicians focus more on treating acute episodes with bronchodilators, oral steroids and antibiotics and are not well versed with the standard asthma guidelines. Lack of knowledge and lack of confidence coupled with poor communication skills that are essential for counselling patients to start inhaled medications for asthma contribute to the under-use of ICS for asthma in the private care setting. Pulmonologists in recent times are well trained in the management of asthma, but not all of them prescribe ICS. Also, there are only 4000 pulmonologists in India serving a population of 1.2 billion population; therefore, most asthma patients in India are treated by primary care physicians (general practitioners and internists).
The community at large: Although the name asthma is known widely in the community, the underlying cause, diagnosis and management remain very poorly known. Many still consider asthma to be a contagious disease. Asthma carries a lot of social stigma and people do not want others to know that members of their family suffer from asthma. Apart from this, there are several myths and misbeliefs associated with the words ‘steroid’ and ‘inhaler’. Steroids are generally looked upon as drugs that have many side effects and thus need to be avoided. The word ‘inhaler’ is often linked with addiction, habit formation and very strong medicines and is therefore used only in the end stages of asthma, if at all.[19] Many asthmatics in India do not like to show the world that they are using inhalers. Most patients who get prescribed inhalers do not know how to use the device correctly, and among those who do, the majority do not use it correctly. Some patients who get prescribed the ICS and use them properly start noticing significant improvements in their symptoms and quality of life. They then stop the ICS believing that there is now no need to take the medicines. Poor adherence and compliance to use of ICS is another major challenge in the community setting. Cost of inhaler devices does not seem to be as big a problem for the vast majority of people because India has one of the cheapest and the largest variety of ICS inhalers in the world. Most asthma patients in India can afford inhalation therapy.
In India, many patients simply visit a retail pharmacy and purchase medicines without any prescription. They rely on the advice of pharmacists to save on time and money for consulting a doctor. In a study in Chennai, when simulated clients with symptoms of mild persistent asthma visited retail pharmacists, they were given oral bronchodilators, antibiotics, methylxanthines and oral corticosteroids, but not inhaled steroids or bronchodilators.[20] This likely also reflects the prescription practices of physicians in their vicinity for the treatment of asthma. When poor patients visit a public facility, ICS medicines are not available, and if they visit a retail pharmacy, they are not given the essential medicines.
There is now ample evidence that the use of ICS in asthma reduces suffering, hospitalisation and deaths. In Singapore, as the sales of inhaled corticosteroids increased between 1994 and 2002, asthma deaths reduced by 52.4% among those aged 5–34 years and 56.7% among those aged 35–65 years. This was also accompanied by a significant decrease in asthma-related hospitalisations from 175.3/100,000 to 122.9/100,000.[21] In 2011, the Brazilian government made inhaled beclomethasone and salbutamol freely available through all the national states for patients diagnosed to have asthma and evaluated the impact of this on asthma-related hospitalisations and associated costs. It took around 2 years for the doctors and patients to start getting used to the availability and importance of these inhaled medications. After 3 years, admission rates decreased by 33.5% compared to the admission rates for the period before provision of free asthma medication. The Ministry of Health spent 7.7 million USD on procuring the asthma drugs but saved 25 million USD on hospitalisation costs.[22]
Impact and future direction
The WHO has categorised asthma as an important non-communicable disease, and according to the Sustainable Development Goals, the target is to reduce premature mortality by one-third by 2030.[23] With the growing evidence that increasing use of ICS reduces asthma deaths, it has been recommended that ICS needs to be brought under the essential components of Universal Health Coverage packages.[24] Access to rational treatment for asthma in India should be improved by establishing and disseminating national guidelines for asthma, the inclusion of asthma inhalation medicines in all state essential medicine list and pooled procurement of medicines, increasing awareness and education of all stake holders for asthma management and ensuring that asthma medicines are affordable for the population.[25] By creating awareness and ensuring that inhaled corticosteroids are made available to all asthmatics in India through public health measures, deaths due to asthma can be easily reduced by 50%.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Cipla Ltd. for sharing with us the IQVIA sales data of inhaled corticosteroids for the year 2019–2020 in India.
REFERENCES
- 1.Salvi SS, Apte KK, Dhar R, Shetty P, Faruqi RA, Thompson PJ, et al. Asthma insights and management in India:Lessons Learnt from the Asia Pacific - Asthma Insights and Management (AP-AIM) Study. J Assoc Physicians India. 2015;63:36–43. [PubMed] [Google Scholar]
- 2.Gold LS, Thompson P, Salvi S, Faruqi RA, Sullivan SD. Level of asthma control and health care utilization in Asia-Pacific countries. Respir Med. 2014;108:271–7. doi: 10.1016/j.rmed.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Kotwani A, Chhabra SK, Tayal V, Vijayan VK. Quality of asthma management in an urban community in Delhi, India. Indian J Med Res. 2012;135:184–92. [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattacharyya P, Paul R, Nag S, Bardhan S, Saha I, Ghosh M, et al. Treatment of asthma:Identification of the practice behavior and the deviation from the guideline recommendations. Lung India. 2010;27:141–4. doi: 10.4103/0970-2113.68315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pandey A, Tripathi P, Pandey RD. Prescription pattern in asthma therapy at Gorakhpur hospitals. Lung India. 2010;27:8–10. doi: 10.4103/0970-2113.59261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holgate ST. The inflammatory basis of asthma and its implications for drug treatment. Clin Exp Allergy. 1996;26((Suppl 4)):1–4. doi: 10.1111/j.1365-2222.1996.tb00660.x. [DOI] [PubMed] [Google Scholar]
- 7.Campbell MJ, Cogman GR, Holgate ST, Johnston SL. Age specific trends in asthma mortality in England and Wales, 1983-95:Results of an observational study. BMJ. 1997;314:1439–41. doi: 10.1136/bmj.314.7092.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Byrne P, Fabbri LM, Pavord ID, Papi A, Petruzzelli S, Lange P. Asthma progression and mortality:The role of inhaled corticosteroids. Eur Respir J. 2019;54:1900491. doi: 10.1183/13993003.00491-2019. doi:10.1183/13993003.00491-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343:332–6. doi: 10.1056/NEJM200008033430504. [DOI] [PubMed] [Google Scholar]
- 10.Suissa S, Ernst P. Use of anti-inflammatory therapy and asthma mortality in Japan. Eur Respir J. 2003;21:101–4. doi: 10.1183/09031936.03.00058503. [DOI] [PubMed] [Google Scholar]
- 11.Nunes de Melo M, Mendes Z, Martins P, Suissa S. Asthma mortality in Portugal:Impact of treatment with inhaled corticosteroids and leukotriene receptor antagonists. Treat Respir Med. 2006;5:143–7. doi: 10.2165/00151829-200605020-00007. [DOI] [PubMed] [Google Scholar]
- 12.Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Novel start study team, Controlled trial of budesonide-formoterol as needed for mild asthma. N Engl J Med. 2019;380:2020–30. doi: 10.1056/NEJMoa1901963. [DOI] [PubMed] [Google Scholar]
- 13.Muneswarao J, Hassali MA, Ibrahim B, Saini B, Ali IAH, Verma AK. It is time to change the way we manage mild asthma:An update in GINA. Respir Res. 2019;2019;20:183. doi: 10.1186/s12931-019-1159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kshatriya RM, Khara NV, Paliwal RP, Patel SN. Evaluation of proficiency in using different inhaler devices among intern doctors. J Family Med Prim Care. 2016;5:362–6. doi: 10.4103/2249-4863.192375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mace C, Bissell K, Bilo NE. Access to essential asthma medicines:The response of the asthma drug facility. Essential Medicines Monitor, WHO. 2011;5:1–4. [Google Scholar]
- 16.Kotwani A. Availability, price and affordability of asthma medicines in five Indian states. Int J Tuberc Lung Dis. 2009;13:574–9. [PubMed] [Google Scholar]
- 17.Kotwani A. Access to essential medicines and standard treatment for chronic diseases. Indian J Pharmacol. 2010;42:127–8. doi: 10.4103/0253-7613.66830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gautam VP, Shah A, Malhotra A, Dewanwala A, Taneja DK, Gupta VK, et al. General practitioners’ knowledge of childhood asthma in Delhi, India. Int J Tuberc Lung Dis. 2008;12:677–82. [PubMed] [Google Scholar]
- 19.Gupta SK, Sen Mazumdar K, Gupta S, Sen Mazumdar A, Gupta S. Patient education programme in bronchial asthma in India:Why, how, what and where to communicate?Indian J Chest Dis Allied Sci. 1998;40:117–24. [PubMed] [Google Scholar]
- 20.Van Sickle D. Management of asthma at private pharmacies in India. Int J Tuberc Lung Dis. 2006;10:1386–92. [PubMed] [Google Scholar]
- 21.Lim DL, Ma S, Wang XS, Cutter J, Chew SK, Lim TK, et al. Trends in sales of inhaled corticosteroids and asthma outcomes in Singapore. Thorax. 2006;61:362–3. doi: 10.1136/thx.2005.050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Comaru T, Pitrez PM, Friedrich FO, Silveira VD, Pinto LA. Free asthma medications reduces hospital admissions in Brazil (Free asthma drugs reduces hospitalizations in Brazil) Respir Med. 2016;121:21–5. doi: 10.1016/j.rmed.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Cao B, Bray F, Ilbawi A, Soerjomataram I. Effect on longevity of one-third reduction in premature mortality from non-communicable diseases by 2030:A global analysis of the Sustainable Development Goal health target. Lancet Glob Health. 2018:e1288–96. doi: 10.1016/S2214-109X(18)30411-X. doi:10.1016/S2214-109X(18)30411-X. [DOI] [PubMed] [Google Scholar]
- 24.Gaga M, Khaltaev N, Varghese C. Inhaled corticosteroids in asthma and the need for universal health coverage. Eur Respir J. 2019;54:1900963. doi: 10.1183/13993003.00963-2019. [DOI] [PubMed] [Google Scholar]
- 25.Kotwani A. Access to inhaled therapy in India:Availability, price and affordability of asthma medicines. Respiratory Drug Delivery Asia. 2014;1:55–66. [Google Scholar]