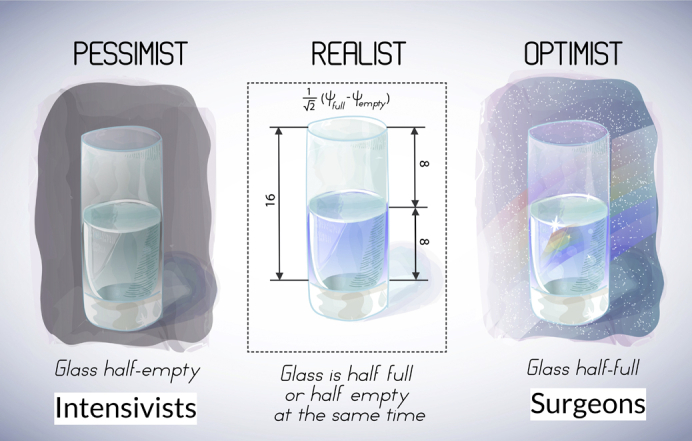
Three interpretations of a glass half full/empty.
Central Message.
Optimal postoperative thoracic intensive care can only be provided by a joint effort of thoracic surgeons and intensivists.
See Article page 281.
There is nothing that generates more emotion (and potential conflict) for patients, families, and physicians alike than the care of critically ill thoracic surgical patients.1 While the vast majority of patients undergoing anatomic lung resection do extremely well, it is inevitable that a small fraction of patients will develop postoperative complications (respiratory, in particular) requiring a stay in the intensive care unit. Typically, these patients preoperatively have recognized marginal lung function, undergo lung resection further reducing their respiratory reserve, and develop postoperative complications like retained secretions or respiratory infection that produce life-threatening problems.
In this retrospective, multicenter cohort study from the United Kingdom, Shelley and colleagues2 attempt to identify risk factors for “unplanned” critical care admission in exactly this group of patients. Nearly one half (16/34) of all Association of Cardiothoracic Anaesthesia and Critical Care centers participated, reviewing 11,208 patients over a 2-year time period (2013-2014) and identifying 253 patients (2.3%) who required unplanned critical care unit admission. The only variables noted independently to predict survival were, not surprisingly, right ventricular dysfunction and the need for both mechanical ventilation and renal-replacement therapy. Overall, the model had an extremely poor predictive value of critical care mortality—no better than a coin flip (area under the curve, 0.64; 95% confidence interval, 0.56-0.72).
Although no novel or major findings were identified, the study is remarkable for what is not present—a surgical perspective. Amazingly, intensivists conceived, planned, and interpreted the entire study that examines thoracic surgical outcomes of patients without the input of a single thoracic surgeon or author! This reflects the increasing duality of thoracic intensive care, which currently is conducted by almost 2 independent physician groups with differing and sometimes conflicting goals. On one side, intensivists focus on high intensive care unit resource use and a mortality of 89 of 253 (35.2%) and seek to predict poor outcomes based on postoperative factors to select appropriate “goals of care” limiting futile resource use—the “glass is half empty” mentality (Figure 1). On the other side, thoracic surgeons who preoperatively establish relationships with patients and their families pursue aggressive management of complications to fulfill these expectations both on the part of the patients/families as well as the surgeons themselves, concentrating on overall success, ie, outstanding overall mortality of 0.8% (89/11, 208). This is the “glass is half full” mentality. Further, thoracic surgeons increasingly are faced with outcome measures, such as “failure to rescue,” which directly conflict with intensivist efforts to limit “futile” resource use.3, 4, 5 This leads not only to conflicts within the treatment “team” that compromise patient care and confuses patients and families but significantly diminishes the satisfaction of all involved, including intensivists and thoracic surgeons.
Figure 1.
Thoracic surgeons often interpret postoperative problems as a glass half full whereas intensivists consider similar problems as a glass half empty. The reality is more in between, and both surgeons and intensivists should strive to better understand different viewpoints.
The optimal strategy, of course, is to identify high-risk patients preoperatively, preferably when they can be targeted for additional perioperative measures or advised to seek alternative therapies rather than surgery. Thoracic surgeons and intensivists must work together in a mutual respectful way. Intensivists must recognize the extensive intensive care experience of thoracic surgeons, and thoracic surgeons must recognize the broad training and experience that the intensivists bring to the table. Only together will both sides provide optimal care.
Footnotes
Disclosures: The author reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Paul Olson T.J., Brasel K.J., Redmann A.J., Alexander G.C., Schwarze M.L. Surgeon-reported conflict with intensivists about postoperative goals of care. JAMA Surg. 2013;148:29–35. doi: 10.1001/jamasurgery.2013.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shelley B.G., McCall P.J., Glass A., Orzechowska I., Klein A.A. Outcome following unplanned critical care admission after lung resection. J Thorac Cardiovasc Surg Open. 2022;9:281–290. doi: 10.1016/j.xjon.2022.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurlansky P.A., O'Brien S.M., Vassileva C.M., Lobdell K.W., Edwards F.H., Jacobs J.P., et al. Failure to rescue: a new Society of Thoracic Surgeons quality metric for cardiac surgery. Ann Thorac Surg. July 6, 2021 doi: 10.1016/j.athoracsur.2021.06.025. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Farjah F., Backhus L., Cheng A., Englum B., Kim S., Saha-Chaudhuri P., et al. Failure to rescue and pulmonary resection for lung cancer. J Thorac Cardiovasc Surg. 2015;149:1365–1371. doi: 10.1016/j.jtcvs.2015.01.063. discussion 1371-3.e3. [DOI] [PubMed] [Google Scholar]
- 5.Farjah F. Failure-to-rescue in thoracic surgery. Thorac Surg Clin. 2017;27:257–266. doi: 10.1016/j.thorsurg.2017.03.005. [DOI] [PubMed] [Google Scholar]



