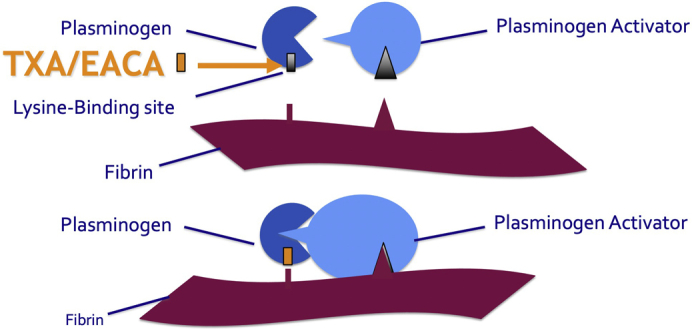
Antifibrinolytic action of aminocaproic acid and tranexamic acid.
Central Message.
The study confirms that the effectiveness of the lysine analogs, tranexamic acid and epsilon-aminocaproic acid, in reducing bleeding and transfusion is comparable in adults undergoing cardiac surgery.
See Article page 114.
In this issue of the JTCVS Open, Broadwin and colleagues1 retrospective analyzed 66 patients who underwent cardiac surgery with cardiopulmonary bypass (CPB) and received either tranexamic acid (TXA) or epsilon-aminocaproic acid (EACA). The authors report comparable transfusion rate and chest tube drainage output. The study was not powered or designed to compare the safety of the 2 drugs.
EACA inhibits binding of plasmin to fibrin by occupying the lysine-binding sites of the proenzyme plasminogen.2 TXA acts like EACA but is 10 times more potent on a molar basis. The number and quality of studies that assessed the effectiveness and safety of TXA outweighs those on EACA.3 In a large study of 4662 patient undergoing coronary artery surgery, TXA was associated with a lower risk of bleeding than the placebo, without a greater risk of death or thrombotic complications within 30 days after surgery.4 TXA did not affect death or severe disability through to 1 year after surgery.5
To date, the number of studies comparing TXA and EACA is sparse. Although the BART (Blood Conservation Using Antifibrinolytics in a Randomized Trial) study mainly compared aprotinin with each of the lysine analogs, no clinically relevant difference was reported between the 2 drugs.6 In 2014, Falana and Patel7 performed a single-center retrospective study of 120 patients who underwent cardiovascular surgery with or without CPB and received at least 1 dose of TXA or EACA. The authors concluded that there were no differences in the efficacy and safety of TXA and EACA. In a randomized, double-blinded trial, Leff and colleagues8 compared the effectiveness of EACA and TXA in reducing blood loss and transfusion requirements in 114 patients undergoing cardiac surgery with CPB. The authors did not report any statistically significant difference between groups when analyzing chest tube drainage. However, they found a significant difference in the administration of any blood product transfusion intraoperatively to 24 hours postoperatively, with less transfusion in patients receiving EACA compared with TXA (25% vs 44.8%, respectively; P = .027).
One of the concerns associated with the administration of lysine analogs has been the dose-dependent increase in the risk of clinical seizures.4,9 In their study, Martin and colleagues10 reported a significant lower new onset of clinical seizures in patients treated with EACA compared with TXA (3.3% vs 7.6%, P = .019). In another study by Makhija and colleagues,11 the authors also reported a tendency for greater incidence of seizure with TXA. Clinical safety and efficacy data for EACA are limited, and some authors have reported an increased risk for postoperative renal dysfunction after EACA administration.10,11
In summary, EACA could be considered as a cost-effective alternative to TXA for the prevention of bleeding and transfusion in cardiac surgical patients. However, EACA and TXA have only been compared in small retrospective studies, and safety concerns have been raised for EACA. Further large prospective studies comparing EACA and TXA would therefore be needed before EACA could be considered a safe alternative to the well-studied TXA.
Footnotes
Disclosures: The author reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Broadwin M., Grant P.E., Robich M.P., Palmeri M.L., Lucas F.L., Rappold J., et al. Comparison of intraoperative tranexamic acid and epsilon-aminocaproic acid in cardiopulmonary bypass patients. J Thorac Cardiovasc Surg Open. 2020;3:114–125. doi: 10.1016/j.xjon.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mannucci P.M., Levi M. Prevention and treatment of major blood loss. N Engl J Med. 2007;356:2301–2311. doi: 10.1056/NEJMra067742. [DOI] [PubMed] [Google Scholar]
- 3.Henry D.A., Carless P.A., Moxey A.J., O'Connell D., Stokes B.J., Fergusson D.A., et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2011:CD001886. doi: 10.1002/14651858.CD001886.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Myles P.S., Smith J.A., Forbes A., Silbert B., Jayarajah M., Painter T., et al. Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017;376:136–148. doi: 10.1056/NEJMoa1606424. [DOI] [PubMed] [Google Scholar]
- 5.Myles P.S., Smith J.A., Kasza J., Silbert B., Jayarajah M., Painter T., et al. Tranexamic acid in coronary artery surgery: one-year results of the Aspirin and Tranexamic Acid for Coronary Artery Surgery (ATACAS) trial. J Thorac Cardiovasc Surg. 2019;157:644–652.e9. doi: 10.1016/j.jtcvs.2018.09.113. [DOI] [PubMed] [Google Scholar]
- 6.Fergusson D.A., Hébert P.C., Mazer C.D., Fremes S., MacAdams C., Murkin J.M., et al. A comparison of aprotinin and lysine analogues in high-risk cardiac surgery. N Engl J Med. 2008;358:2319–2331. doi: 10.1056/NEJMoa0802395. [DOI] [PubMed] [Google Scholar]
- 7.Falana O., Patel G. Efficacy and safety of tranexamic acid versus ε-aminocaproic acid in cardiovascular surgery. Ann Pharmacother. 2014;48:1563–1569. doi: 10.1177/1060028014549558. [DOI] [PubMed] [Google Scholar]
- 8.Leff J., Rhee A., Nair S., Lazar D., Sathyanarayana S.K., Shore-Lesserson L. A randomized, double-blinded trial comparing the effectiveness of tranexamic acid and epsilon-aminocaproic acid in reducing bleeding and transfusion in cardiac surgery. Ann Card Anaesth. 2019;22:265–272. doi: 10.4103/aca.ACA_137_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lecker I., Wang D.-S., Romaschin A.D., Peterson M., Mazer C.D., Orser B.A. Tranexamic acid concentrations associated with human seizures inhibit glycine receptors. J Clin Invest. 2012;122:4654–4666. doi: 10.1172/JCI63375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin K., Knorr J., Breuer T., Gertler R., Macguill M., Lange R., et al. Seizures after open heart surgery: comparison of ε-aminocaproic acid and tranexamic acid. J Cardiothorac Vasc Anesth. 2011;25:20–25. doi: 10.1053/j.jvca.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Makhija N., Sarupria A., Kumar Choudhary S., Das S., Lakshmy R., Kiran U. Comparison of epsilon aminocaproic acid and tranexamic acid in thoracic aortic surgery: clinical efficacy and safety. J Cardiothorac Vasc Anesth. 2013;27:1201–1207. doi: 10.1053/j.jvca.2013.04.003. [DOI] [PubMed] [Google Scholar]


