Multidisciplinary team to treat injection drug use–related endocarditis.
Central Message.
Successful treatment of patients with injection drug use–related endocarditis requires multidisciplinary collaboration to simultaneously treat endocarditis and addiction.
See Commentary on page 321.
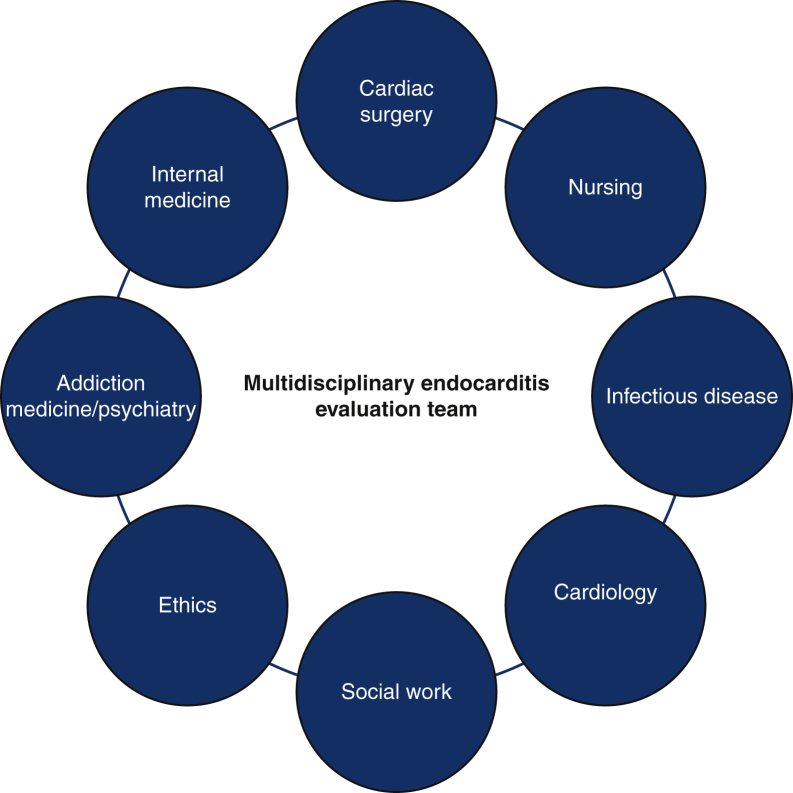
The opioid epidemic in the United States is accompanied by the increasing incidence of injection drug use–related infective endocarditis (IDU-IE).1,2 Cardiac surgeons are increasingly faced with this complex patient population, with one-third of valve operations for endocarditis related to drug use.1,3 The technical challenges of operative management are compounded by the complexities surrounding the decision to offer the operation to patients with IDU-IE. Because the risk and consequence of substance use relapse in the absence of addiction treatment after the operation are substantial,4 surgeons must work closely with a multidisciplinary team that comprises not only cardiology, internal medicine, and infectious disease, but also addiction medicine or addiction psychiatry, social work, nursing, and sometimes ethics experts to develop careful and comprehensive treatment strategies for patients (Figure 1). Ensuring that IDU-IE patients receive multidisciplinary care is important, because the treatment that patients with addiction receive is often less than those recommended in guidelines.5 Surgical and nonsurgical treatment options for drug-related infective endocarditis (IE) continues to evolve, including less invasive approaches such as the use of aspiration catheter systems, the potential safety of postoperative oral rather than intravenous (I.V.) antibiotic treatment, and a multimodal approach to addiction treatment. In this Expert Opinion article, we explore the frontiers in the management of IDU-IE patients relevant to cardiac surgeons.
Figure 1.
Multidisciplinary team to treat injection drug use–related endocarditis.
Evolving Burden of Injection Drug Use–Related Endocarditis in the United States
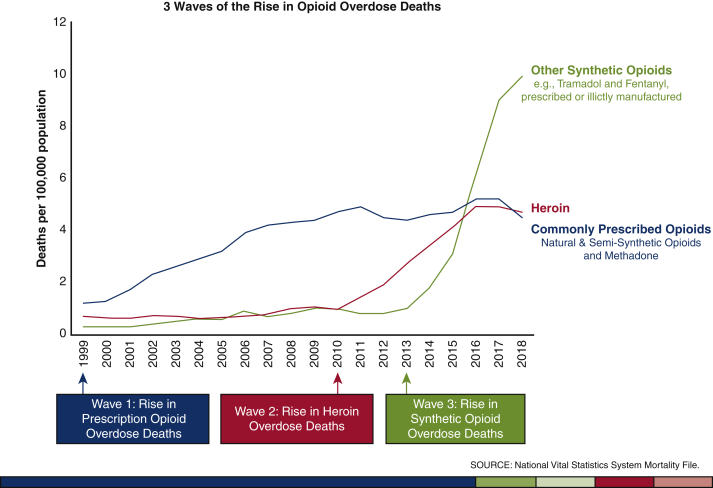
Understanding the evolving burden of IDU-IE allows us to appreciate the challenges unique to the current wave of the US opioid epidemic. The current opioid epidemic in the United States is among the worst in the world, with approximately 130 deaths from an opioid overdose each day.6 Other countries, especially Canada and European countries, also suffer from an increase in opioid prescriptions per patient for the past 15 years,7,8 although fortunately this has not translated into the magnitude of epidemic seen in the United States. Three waves of U.S. opioid epidemics have occurred, starting in the 1990s, 2010, and 2013, with each having distinct patient characteristics and substance of choice (Figure 2).9 The latest wave is characterized by predominant occurrence in urban settings,10 affecting an increasing proportion of young patients with approximately 30% of death related to overdose occurring in those younger than 25 years old. This is also a socioeconomically disadvantaged population with a history of incarceration in 58% of cases and with 22% with a history of homelessness.11 Geographically, East South Central and South Atlantic regions bear the heaviest disease burden.3 Such shifting demographic characteristics of patients affected by the opioid epidemic in turn changed the population with IDU-IE with whom surgeons are faced.
Figure 2.
United States overdose deaths involving opioids. Deaths per 100,0000 population according to year. Reproduced with permission from the Centers for Disease Control and Prevention.9
Operative Indications and Considerations for Injection Drug Use–Related Endocarditis
Guidelines have variably defined operative indications for endocarditis in the setting of injection drug use. The decision to offer operation revolves around the complexity of simultaneously treating 2 diseases: endocarditis and addiction. Additionally, in considering the chronic relapsing nature of addiction and risk of reinfection related to recurrent drug use, the traditional framework of perioperative and long-term survival to define the benefit of operation might not readily apply in forming recommendations as they do in other cardiovascular diseases. Perhaps as a result, American and European guidelines differ in their recommendations. For example, the 2015 European Society of Cardiology (ESC) guideline generally discourages right-sided valve operation for endocarditis related to injection drug use outside of conservative criteria,12 whereas the 2014 American Heart Association/American College of Cardiology guideline does not recommend indications specific to IDU-IE13; in contrast, The American Association for Thoracic Surgery guideline recommends applying the same operative indication for non–IDU-IE, taking addiction into account.14 Multidisciplinary discussion, including the patient and the family, should be a default process. We agree with the ESC recommendation that operations should be considered for those with right heart failure related to tricuspid regurgitation, persistent infection due to fastidious organisms, and large (>20 mm) tricuspid vegetations with a high pulmonary embolic burden.
There are less extensive operative and procedural approaches to tricuspid endocarditis, although with undefined long-term outcomes. These include the use of an aspiration catheter system,15 and tricuspid valvectomy,16 in which the tricuspid valve is excised without replacement with a prosthetic valve. Although the perioperative risk tends to be lower with these approaches that do not result in a complete replacement of the valve with a shorter or no cardiopulmonary bypass run, rigorous follow-up data are lacking. An aspiration catheter system might result in incomplete removal of infected tissue and valvectomy might have adverse effects on the right ventricular and liver function related to severe tricuspid regurgitation. Therefore, these approaches should not be a routine treatment option at this juncture. The less invasive nature of aspiration catheter systems might offer a salvage treatment to carefully selected patients with high embolic burden who cannot undergo operative removal of the infected tissue.
The choice of prosthetic valve is controversial in this patient group. In the general population, mechanical valve is preferred over bioprosthetic valve in young patients including the age range commonly represented in IDU-IE patients. However, mechanical valve requires strict adherence to a warfarin regimen and regular blood draws. Such an intensive regimen is often not compatible with the lifestyles of patients with IDU-IE. Considering that 5-year survival of patients with injection drug use is 62%, a substantial portion of the patients might not outlive the first bioprosthetic valve.17 Therefore, a bioprosthetic valve might be a reasonable option in this population despite their young age.
Ultimately, the decision to offer surgery should be on the basis of a multidisciplinary discussion between cardiac surgery, referring medical specialty, infectious disease, and addiction medicine or addiction psychiatry. The patient, family, and legal representatives (more commonly in European countries)18 should be involved in this process as well. Pertinent outcome-related data are: (1) reoperation for IDU-IE is associated with increased risk of perioperative mortality,19 (2) the leading cause of death within several years of valve operation for IDU-IE might be related to recurrent drug use,20 (3) untreated addiction has a poor prognosis, and (4) addiction treatment with and without pharmacologic means will substantially increase the chance of achieving sobriety and addiction recovery. Although data on outcomes specific to IDU-IE are evolving, clinical outcomes data alone are insufficient to guide satisfactory decision-making especially in the reoperative setting, because the treatment decision requires integration of multiple specialties and addiction treatment approaches.
Ethical Considerations in the Decision to Operate
DiMaio and colleagues21 have outlined a useful framework to navigate conflicting ethical principles of a decision to deny or offer reoperation, including balancing physicians' obligation to the patient (to treat those with medical needs) and the society (allocation of scarce resources). Arguments advocating that surgeons can refuse the operation includes the utilitarian view of maximizing the good of others by triaging resource away when poor outcomes are expected after the resource-intensive operation in patients with high risk of recurrent drug use. Arguments that surgeons cannot deny the operation include the view that physicians should not engage in the allocation of scarce health care resources, as coded in the American Medical Association's Code of Medical Ethics.22
In resource-rich countries such as the United States, surgeons might have the luxury of offering the operation for IDU-IE without immediate resource constraints. Such is often not the case for resource-poor countries23 and as the extreme situations in the COVID pandemic taught us, even extremely wealthy countries like the United States are vulnerable to situations that call for triaging immediate life support such as a mechanical ventilator.24 On a daily basis, cardiac surgeons engage themselves in the allocation of the donor heart, a scarce resource, even though the visceral weight of the decision is blunted by the nonhuman, algorithmic working of the organ allocation system. Therefore, a blanket statement that surgeons should not be involved in triaging health care resources does not reflect the reality of surgeons already playing the role. Additionally, we must be mindful that the decision to offer a resource-intensive operation to the patient is always accompanied by the indirect, downstream deprivation of resources from somewhere else, although it might not be perceptible within the narrow framework of individual patient–physician interaction. In this regard, surgeons must be mindful of the broader public health and health economics perspective.
Because of this highly contextualized and nuanced consideration, standardization of the practice might not be the goal. A national survey of cardiac surgeons revealed substantial variability in their willingness and policy in offering a second valve operation for patients with IDU-IE. Because the optimal process of reaching the decision occurs locally, it is important that surgeons and the multidisciplinary teams be familiar with the multitude of arguments for and against reoperation to allow for productive discussion and thorough considerations of conflicting principles to reach a collective decision.
Potential Safety of Postoperative Oral Antibiotics
With regard to the optimal antibiotic regimen in the postoperative phase of patients with IE, The American Association for Thoracic Surgery,14 American Heart Association,25 and ESC12 recommend I.V. antibiotic treatment for up to 6 weeks, with the possibility of adjusting regimen and duration depending on the causative organism and its sensitivity. The I.V. administration of antibiotics in patients with drug-related endocarditis is complicated for the maintenance of an indwelling catheter and possibility of the established I.V. access increasing the risk of recurrent drug use. To mitigate such risks, it is not uncommon for patients who have difficulty of being placed in rehabilitation facilities to be kept as inpatients for a prolonged period of time solely for the administration of I.V. antibiotics.
In such circumstances, oral antibiotic treatment is an attractive alternative. A multicenter randomized trial showed noninferiority of oral antibiotic regimens in patients with left-sided IE with Streptococcus species, Enterococcus faecalis, Staphylococcus aureus, or coagulase-negative staphylococci.26 The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, or bacteremia relapse with the primary pathogen, which occurred in 9.0% in the oral group versus 12.1% in the I.V. group (odds ratio, 0.72; 95% CI, 0.37-1.36), with a between-group difference of 3.1 percentage points, which met the noninferiority criterion. The study expectedly showed a significantly shorter median length of hospital stay after randomization in the oral antibiotics arm compared with the I.V. antibiotics arm (3 vs 19 days; P < .001). It should be noted that patients with IDU-IE only comprised 1.3% (5/400) of the study participants. However, this should not be seen as the limitation toward generalizability of the results to the IDU-IE population, because most organisms isolated in IDU-IE is Staphylococcus species,2 which was well–represented in the trial.
Integrating Addiction Treatment in the Care of Patients With IDU-IE
In the past 15 years, there has been more than a 60% increase in the incidence of patients seeking hospitalization related to an opioid use disorder in parallel with increases of patients being treated for IDU-IE.2 Treatment models of patients with IDU-IE have historically focused on treating patients' symptoms but not their underlying disease of addiction leading to poor surgical and patient outcomes.27 Treating IDU-IE without addressing a patient's addiction often operates on the misunderstanding that addiction is a choice and patients can abstain through willpower alone. Advances in the neurobiology of addiction, however, elucidate that addiction is a chronic medical disease of the brain that impairs decision-making and continues despite harms, including serious health conditions like IDU-IE.28 Similar to other chronic diseases, addiction is treatable with evidence-based therapies and longitudinal care.29
Fifty-year experience of the specialty shows that there are highly effective treatments for opioid use disorder, the primary substance use disorder implicated in most cases of IDU-IE, and patients who receive these treatments have reduction of all-cause mortality, reduction of opioid use, improved retention in addiction and medical treatment, reduction in communicable disease risks, and reduced criminal activity.30 However, highly effective addiction treatment has remained largely siloed from most general medical care, including hospital settings. This is changing as specialty addiction medicine or addiction psychiatry consult services have started operating in hospital settings. Integrating addiction medicine/psychiatry consult services are compelling for several reasons: (1) most hospitalized patients with addiction desire treatment to be initiated in the hospital,31 and (2) addiction treatment provided in the hospital improves outcomes such as reduced opioid use, reduced hospital readmission rates, and increases retention in addiction and medical care.32 Specifically in patients with IDU-IE, receiving addiction treatment is associated with nearly a 70% lower risk of mortality.33
Multidisciplinary teams have emerged as an effective way to support clinical decision-making and complex care of patients hospitalized with IDU-IE. Hospital systems might create such teams modeled after “transplant selection committees” to formalize the process of evaluating operative candidacy and other complex treatment decisions. Such an approach can reduce the significant practice variation. One of the first models of which we are aware involves multidisciplinary input from addiction medicine, cardiology, cardiothoracic surgery, infectious disease, and social work at our center. The Multidisciplinary Endocarditis Evaluation Team at our center has shown feasibility, acceptability, and positive patient outcomes such as high antibiotic completion rate, retention in medical and addiction treatment, and reduction of 30-day hospital readmissions.
Even in the absence of a robust team, standardized screening for tobacco, alcohol, and drug use and evaluation for substance use disorder using evidence-based tools can identify patients who would benefit from a formal evaluation by addiction medicine or addiction psychiatry34 (Table 1). As a standard of practice, any patient with concerning opioid use should be further evaluated and if found to have opioid use disorder, offered treatments such as methadone or buprenorphine in the hospital setting. Tobacco use should also be addressed, and guideline-directed treatments offered. Postdischarge care must be arranged to address the chronic nature of addiction. Because of the high rate of mortality and morbidity from relapse to drug use in the setting of IDU-IE, long-term treatment with medications is essential. Surgeons are encouraged to collaborate with providers who can thoroughly evaluate patients for addiction, provide psychosocial support, and offer these treatments in the inpatient and outpatient setting.
Table 1.
Commonly used screening, risk assessment, and diagnostic tools for tobacco, alcohol, and other drugs
| Tool | Substance(s) included | Purpose of tool |
|---|---|---|
| SISQ-Alc35,36,∗ | Alcohol | Screen for unhealthy alcohol use |
| SISQ-Drug35,36,∗ | Prescription Drugs, other drugs | Screen for unhealthy drug use |
| TAPS37,∗ | Tobacco, alcohol, prescription drugs, other drugs | Risk assessment for unhealthy drug and alcohol use |
| DSM-5 | Any substance | Diagnose substance use disorder |
SISQ-Alc, Single-Item Screening Questions for Alcohol; SISQ-Drug, Single-Item Screening Questions for Drug Use; TAPS, Tobacco, Alcohol, Prescription Medication, and Other Substance Use; DSM-5, Diagnostic and Statistical Manual of Mental Disorders-Fifth Revision.
Screening and risk assessment tools that can be self-administered.
Conclusions
IDU-IE is a complex disease that often burdens those in socioeconomically disadvantaged groups of the society. Successful treatment requires simultaneous and thorough management of addiction and endocarditis. Standard valve replacement or valve repair techniques should be applied as in patients with non–IDU-IE. Less extensive operative approaches, such as valvectomy or catheter-based aspiration of vegetation, still lacks high-quality long-term data on their safety and efficacy. The decision to offer valve operation in this patient population requires multidisciplinary consideration of expected clinical benefit and the prospect of recovery from addiction under the recognition that health care resources are scarce. Increasing safety data on oral antibiotics might aid in successful completion of the required antibiotics course while reducing the hospital length of stay. Involvement of addiction medicine or addiction psychiatry service is essential to achieving the best possible outcomes.
Conflict of Interest Statement
Dr Mori has received funding support from the Yale Clinical and Translational Science Award, grant UL1TR001863, from the National Center for Advancing Translational Science, a component of the National Institutes of Health. Dr Geirsson has received a consulting fee for being a member of Medtronic Strategic Surgical Advisory Board. Medtronic produces valve products for valve replacement and repairs. Dr Weimer receive compensation as a consultant to this start up substance use treatment company with Path CCM, Inc. Dr Amabile reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Schranz A.J., Fleischauer A., Chu V.H., Wu L.T., Rosen D.L. Trends in drug use-associated infective endocarditis and heart valve surgery, 2007 to 2017: a study of statewide discharge data. Ann Intern Med. 2019;170:31–40. doi: 10.7326/M18-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mori M., Brown K.J., Bin Mahmood S.U., Geirsson A., Mangi A.A. Trends in infective endocarditis hospitalizations, characteristics, and valve operations in patients with opioid use disorders in the United States: 2005-2014. J Am Heart Assoc. 2020;9:e012465. doi: 10.1161/JAHA.119.012465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geirsson A., Schranz A., Jawitz O., Mori M., Feng L., Zwischenberger B.A., et al. The evolving burden of drug use associated infective endocarditis in the United States. Ann Thorac Surg. 2020;110:1185–1192. doi: 10.1016/j.athoracsur.2020.03.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Della Corte A., Di Mauro M., Actis Dato G., Barili F., Cugola D., Gelsomino S., et al. Surgery for prosthetic valve endocarditis: a retrospective study of a national registry. Eur J Cardiothorac Surg. 2017;52:105–111. doi: 10.1093/ejcts/ezx045. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal E.S., Karchmer A.W., Theisen-Toupal J., Castillo R.A., Rowley C.F. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med. 2016;129:481–485. doi: 10.1016/j.amjmed.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services What is the U.S. opioid epidemic? https://www.hhs.gov/opioids/about-the-epidemic/index.html Accessed November 13, 2020.
- 7.Curtis H.J., Croker R., Walker A.J., Richards G.C., Quinlan J., Goldacre B. Opioid prescribing trends and geographical variation in England, 1998-2018: a retrospective database study. Lancet Psychiatry. 2019;6:140–150. doi: 10.1016/S2215-0366(18)30471-1. [DOI] [PubMed] [Google Scholar]
- 8.Kalkman G.A., Kramers C., van Dongen R.T., van den Brink W., Schellekens A. Trends in use and misuse of opioids in The Netherlands: a retrospective, multi-source database study. Lancet Public Health. 2019;4:e498–e505. doi: 10.1016/S2468-2667(19)30128-8. [DOI] [PubMed] [Google Scholar]
- 9.CDC. Centers for Disease Control and Prevention Understanding the epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html Accessed November 13, 2020.
- 10.Soriano V. Why not an opioid epidemic in Europe like in the USA? AIDS Rev. 2019;21:234–235. [PubMed] [Google Scholar]
- 11.Degenhardt L., Peacock A., Colledge S., Leung J., Grebely J., Vickerman P., et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5:e1192–e1207. doi: 10.1016/S2214-109X(17)30375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Habib G., Lancellotti P., Antunes M.J., Bongiorni M.G., Casalta J.P., Del Zotti F., et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur Heart J. 2015;36:3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 13.Nishimura R.A., Otto C.M., Bonow R.O., Carabello B.A., Erwin J.P., III, Guyton R.A., et al. 2014 American Heart Association/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2438–2488. doi: 10.1016/j.jacc.2014.02.537. [DOI] [PubMed] [Google Scholar]
- 14.AATS Surgical Treatment of Infective Endocarditis Consensus Guidelines Writing Committee Chairs, Pettersson G.B., Coselli J.S., Writing Committee, Pettersson G.B., Coselli J.S., et al. 2016 the American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg. 2017;153:1241–1258.e29. doi: 10.1016/j.jtcvs.2016.09.093. [DOI] [PubMed] [Google Scholar]
- 15.Hosoba S., Mori M., Furtado A.D., Lattouf O.M. Extraction of right-sided vegetation with use of an aspiration catheter system. Innovations (Phila) 2015;10:357–359. doi: 10.1097/IMI.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 16.Protos A.N., Trivedi J.R., Whited W.M., Rogers M.P., Owolabi U., Grubb K.J., et al. Valvectomy versus replacement for the surgical treatment of tricuspid endocarditis. Ann Thorac Surg. 2018;106:664–669. doi: 10.1016/j.athoracsur.2018.04.051. [DOI] [PubMed] [Google Scholar]
- 17.Goodman-Meza D., Weiss R.E., Gamboa S., Gallegos A., Bui A.A.T., Goetz M.B., et al. Long term surgical outcomes for infective endocarditis in people who inject drugs: a systematic review and meta-analysis. BMC Infect Dis. 2019;19:918. doi: 10.1186/s12879-019-4558-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Druml C. Informed consent of incapable (ICU) patients in Europe: existing laws and the EU Directive. Curr Opin Crit Care. 2004;10:570–573. doi: 10.1097/01.ccx.0000144765.73540.89. [DOI] [PubMed] [Google Scholar]
- 19.Mori M., Bin Mahmood S.U., Schranz A.J., Sultan I., Axtell A.L., Sarsour N., et al. Risk of reoperative valve surgery for endocarditis associated with drug use. J Thorac Cardiovasc Surg. 2020;159:1262–1268.e2. doi: 10.1016/j.jtcvs.2019.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguemeni Tiako M.J., Mori M., Bin Mahmood S.U., Shioda K., Mangi A., Yun J., et al. Recidivism is the leading cause of death among intravenous drug users who underwent cardiac surgery for infective endocarditis. Semin Thorac Cardiovasc Surg. 2019;31:40–45. doi: 10.1053/j.semtcvs.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 21.DiMaio J.M., Salerno T.A., Bernstein R., Araujo K., Ricci M., Sade R.M. Ethical obligation of surgeons to noncompliant patients: can a surgeon refuse to operate on an intravenous drug-abusing patient with recurrent aortic valve prosthesis infection? Ann Thorac Surg. 2009;88:1–8. doi: 10.1016/j.athoracsur.2009.03.088. [DOI] [PubMed] [Google Scholar]
- 22.AMA Allocating limited health care resources. https://www.ama-assn.org/delivering-care/ethics/allocating-limited-health-care-resources Accessed November 2, 2020.
- 23.Ahmed T., Safdar A. Ethical dilemma: should continuous intravenous drug use affect appropriate management in prosthetic valve endocarditis? Cureus. 2020;12:e8458. doi: 10.7759/cureus.8458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Truog R.D., Mitchell C., Daley G.Q. The toughest triage—allocating ventilators in a pandemic. N Engl J Med. 2020;382:1973–1975. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 25.Baddour L.M., Wilson W.R., Bayer A.S., Fowler V.G., Jr., Tleyjeh I.M., Rybak M.J., et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 26.Iversen K., Ihlemann N., Gill S.U., Madsen T., Elming H., Jensen K.T., et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380:415–424. doi: 10.1056/NEJMoa1808312. [DOI] [PubMed] [Google Scholar]
- 27.Serota D.P., Kraft C.S., Weimer M.B. Treating the symptom but not the underlying disease in infective endocarditis: a teachable moment. JAMA Intern Med. 2017;177:1026. doi: 10.1001/jamainternmed.2017.1489. [DOI] [PubMed] [Google Scholar]
- 28.Volkow N.D., Koob G.F., McLellan A.T. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374:363–371. doi: 10.1056/NEJMra1511480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ASAM. American Society of Addiction Medicine Definition of addiction. https://www.asam.org/Quality-Science/definition-of-addiction Accessed November 13, 2020.
- 30.Mattick R.P., Breen C., Kimber J., Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2:CD002207. doi: 10.1002/14651858.CD002207.pub4. [DOI] [PubMed] [Google Scholar]
- 31.Englander H., Weimer M., Solotaroff R., Nicolaidis C., Chan B., Velez C., et al. Planning and designing the improving addiction care team (IMPACT) for hospitalized adults with substance use disorder. J Hosp Med. 2017;12:339–342. doi: 10.12788/jhm.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weimer M., Morford K., Donroe J. Treatment of opioid use disorder in the acute hospital setting: a critical review of the literature (2014-2019) Curr Addict Rep. 2019;6:339–354. doi: 10.1007/s40429-019-00267-x. [DOI] [Google Scholar]
- 33.Rodger L., Glockler-Lauf S.D., Shojaei E., Sherazi A., Hallam B., Koivu S., et al. Clinical characteristics and factors associated with mortality in first-episode infective endocarditis among persons who inject drugs. JAMA Netw Open. 2018;1:e185220. doi: 10.1001/jamanetworkopen.2018.5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.New York State Department of Health Aids Institute Substance use screening and risk assessment in adults. https://www.hivguidelines.org/substance-use/su-screening Accessed November 13, 2020.
- 35.Smith P.C., Schmidt S.M., Allensworth-Davies D., Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24:783–788. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McNeely J., Cleland C.M., Strauss S.M., Palamar J.J., Rotrosen J., Saitz R. Validation of self-administered single-item screening questions (SISQs) for unhealthy alcohol and drug use in primary care patients. J Gen Intern Med. 2015;30:1757–1764. doi: 10.1007/s11606-015-3391-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McNeely J., Wu L.T., Subramaniam G., Sharma G., Cathers L.A., Svikis D., et al. Performance of the tobacco, alcohol, prescription medication, and other substance use (TAPS) tool for substance use screening in primary care patients. Ann Intern Med. 2016;165:690–699. doi: 10.7326/M16-0317. [DOI] [PMC free article] [PubMed] [Google Scholar]