INTRODUCTION:
Despite targeted public health efforts, rates of hypertension remain persistently high, and the prevalence of hypertension control, low in the United States (US). Recently, US death rates attributed to hypertension as the underlying cause of death have increased, and marked race-sex disparities persist.1 However, hypertension is infrequently listed as an underlying cause of death; more commonly it contributes to death through cardiovascular diseases (CVD), such as ischemic heart disease (IHD), heart failure (HF), and cerebrovascular disease (CBD).2 To inform public health strategies around hypertension, we leveraged the multiple cause of death files from the CDC to comprehensively quantify trends in the burden of hypertension-related CVD deaths.
METHODS
This study utilized the CDC WONDER dataset, which includes all death certificates filed in the US.3 We included decedents ≥25 years with any mention of hypertension (International Classification of Diseases, Tenth Revision [ICD-10]: I10-I15 listed as the underlying or a contributing cause of death) and underlying cause of death listed as CVD (I00–99) between 2000–2018. Hypertension-related CVD deaths were also stratified by leading CVD subtypes: 1) IHD (I20–25) as underlying cause of death; 2) HF (ICD-10: I50) as underlying cause of death or any mention (consistent with mortality reporting recommendations for HF); and 3) CBD (I60–69) as underlying cause of death. Race-sex-specific analyses were performed for black and white decedents. We did not stratify by ethnicity given concern for misclassification in reporting.
Age-adjusted mortality rates (AAMR) per 100,000 population for all hypertension-related CVD deaths and for each CVD subtype (hypertension-related IHD, HF, and CBD) were calculated using the 2000 US standard population.3 Joinpoint software (Version 4.7.0.0) using serial permutation testing identified trend inflections in AAMR for hypertension-related CVD deaths in the overall population.4 Average annual percentage change (AAPC [%], 95% CI) for linear AAMR trends between these standardized inflection points and the full analysis period were calculated for all specified subgroups. Using the method from Boyle and Parkin we calculated rate ratios (95% CI) of the AAMR in blacks compared with whites. Statistical significance was indicated at two-sided p<0.05.
RESULTS
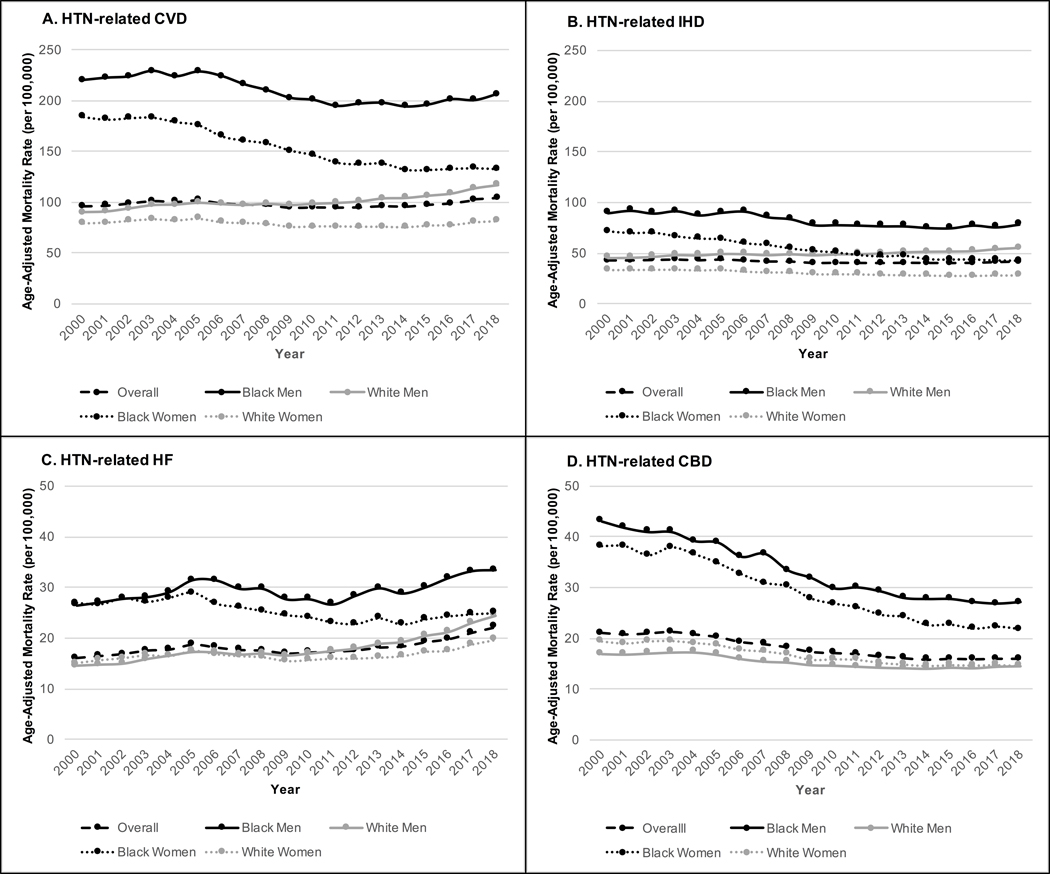
Between 2000–2018, total hypertension-related CVD deaths increased from 171,259 to 270,839 and overall AAMR for hypertension-related CVD increased by +0.5%/year (95% CI: +0.1, +0.8), on average. We identified a triphasic trend pattern with two inflection points (2003, 2012): the overall AAMR increased between 2000–2003, decreased between 2003–2012 and increased again between 2012–2018 (FIGURE). Across CVD subtypes, the AAMR for hypertension-related: 1) IHD deaths declined −1.5%/y (−1.8, −1.1), 2) HF deaths increased +1.8%/y (+1.4, +2.3), and 3) CBD deaths remained stable −0.1%/year (−0.4, +0.2) between 2000–2018.
FIGURE LEGEND. Trends in Age-Adjusted Mortality Rates (AAMR) per 100,000 of Hypertension-Related A) Cardiovascular Disease, B) Ischemic Heart Disease, C) Heart Failure, and D) Cerebrovascular Disease Deaths Overall and by Race-Sex Groups: 2000–2018.
The AAMR for is shown for the overall US population as well as for black and white men and women 2000–2018. HTN: hypertension; CVD: cardiovascular disease; IHD: ischemic heart disease; HF: heart failure; CBD: cerebrovascular disease.
In the earlier time periods, 2000–2012, the AAMR of hypertension-related CVD deaths (per 100,000) increased for white men (90.1 to 100.8) and decreased for white women (79.2 to 75.7), black men (220.1 to 197.0) and black women (184.1to 137.5). In the most recent period (2012–2018), AAMR accelerated for white men (100.8 to 117.2), reversed for white women (75.7 to 81.5) and black men (197.0 to 206.6), and decelerated for black women (137.5 to 132.7). Similar patterns were seen for other CVD subtypes (FIGURE). The rate-ratio of hypertension-related CVD AAMR in black compared with white men was 2.44 (2.38, 2.51) in 2000 and 1.76 (1.73, 1.80) in 2018. A similar black-white rate-ratio of hypertension-realted CVD AAMR was observed in women in both 2000 and 2018 (2.32 [2.28, 2.38] and 1.63 [1.60, 1.66], respectively).
DISCUSSION
Between 2000–2018, total annual hypertension-related CVD deaths and AAMR increased in the US. For each CVD subtype and race-sex group, death rates increased, stagnated or saw a deceleration of previously declining death rates in the most recent time period (2012–2018), undoing earlier progress. Although white men saw the greatest increase in hypertension-related CVD deaths between 2000–2018, disparities persisted with nearly 2-fold higher AAMR for hypertension-related CVD deaths in blacks compared with whites in 2018.
The 21st century has seen meaningful improvements in some aspects of cardiovascular health (e.g. declining rates of cigarette smoking) but this progress appears to have been offset by coincident increases in the number of individuals with obesity or diabetes, which may be adversely contributing to hypertension-related CVD mortality rates.5 Our analysis is limited by its reliance on ICD-10 codes and may be subject to misclassification. However, it provides the most robust and comprehensive estimates of hypertension-related national mortality rates available. Further, death certificates do not include individual-level data on control of hypertension and therefore, we are unable to differentiate those individuals with controlled vs. uncontrolled hypertension or the relative impact of hypertension control on death. Nonetheless, our results show a consistent worsening of national mortality rates for all hypertension-related CVD and race-sex subgroups between 2012–2018 and unacceptable persistent racial disparities in hypertension-related CVD mortality rates. Resources aimed at preventing and managing hypertension are urgently needed to reduce preventable deaths and reduce disparities.
Acknowledgements:
The funding sponsor did not contribute to design and conduct of the study, collection, management, analysis, or interpretation of the data or preparation, review, or approval of the manuscript. The authors take responsibility for decision to submit the manuscript for publication. Dr. Khan had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Sources of Funding:
Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number KL2TR001424 and the American Heart Association (#19TPA34890060) to SSK. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Leah Rethy was supported by a grant (2018–2019) from the Sarnoff Cardiovascular Research Foundation.
Footnotes
Disclosures: None
REFERENCES
- 1.Shah NS, Lloyd-Jones DM, O’Flaherty M, Capewell S, Kershaw KN, Carnethon M and Khan SS. Trends in Cardiometabolic Mortality in the United States, 1999–2017. Jama. 2019;322:780–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kung HC and Xu J. Hypertension-related Mortality in the United States, 2000–2013. NCHS data brief. 2015:1–8. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention National Center for Health Statistics. CDC WONDER: multiple cause of death 1999–2018,. [Google Scholar]
- 4.National Cancer Institute Division of Cancer Control and Population Sciences. Joinpoint regression program, version 4.7.0.0,. [Google Scholar]
- 5.Sidney S, Quesenberry CP Jr., Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, Go AS and Rana JS. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiol. 2016;1:594–9. [DOI] [PubMed] [Google Scholar]