Abstract
Introduction:
There is currently no consensus as to the comparative complication profiles of mini-plate (MP) and reconstruction bar (RB) osseous fixation in fibula flap mandibular reconstruction. The aim of this study is to compare complication rates associated with the use of MP versus RB fixation for vascularized fibula free flap (FFF) reconstruction of oncologic mandibular defects in an effort to better guide hardware utilization and preoperative virtual surgical planning methods.
Methods:
A systematic review and meta-analysis was performed according to PRISMA guidelines. PubMed, EMBASE, and Cochrane Library databases were queried to identify studies related to FFF-based mandibular reconstruction with either MP or RB fixation. Primary endpoints of interest were plate complications, wound infection, malunion or nonunion, and total flap loss. Complication rates were calculated as weighted proportions and compared via Fisher exact testing.
Results
Sixteen studies met inclusion criteria, which examined 1,513 patients. Only 3 studies directly compared MP fixation to RB fixation. MP fixation was used in 828 (54.7%) cases and RB fixation in 685 (45.3%). MP fixation demonstrated greater rates of plate-related complications (32.5% versus 18.8%, p < 0.01, respectively), fistula formation (15.8% versus 4.7%, p=0.04), total flap loss (9.4% versus 4.7%, p=0.02), partial flap loss (20.6% versus 6.1%, p<0.01), and re-operation for vascular compromise (13.3% versus 4.0%, p<0.01). Rates of infection, mal-union/non-union, and wound dehiscence were similar across both groups.
Conclusion:
Our results suggest that MP use may be associated with higher rates of plate related complications. Though limited by outcome reporting heterogeneity, this review can serve as a template for future investigations evaluating the safety profiles of MP and RB fixation in head and neck surgery.
Keywords: Fibular Free Flap, Mini-plate, Reconstruction Bar, Osseous Fixation, Meta-analysis
Introduction
The operative management of malignant or benign head and neck lesions often results in segmental defects of the mandible.1 Mastication, swallowing and speech are key functions that may become impaired as a result of loss of motor innervation, interruption of mandibular continuity, or muscle/tendon disruption. Without subsequent reconstruction of the mandible, patients may also experience considerable aesthetic and psychosocial sequelae, contributing to diminished health-related quality of life (QOL).2–5 Free tissue transfer remains the gold standard for mandibular reconstruction following oncologic resections, with the fibula free flap (FFF) widely considered the workhorse. Its success can be attributed to its long vascular pedicle, adequate vessel diameter, ample length of bone available for harvest, a dual blood supply (periosteal and endosteal) enabling multiple osteotomies, and a thin pliable skin paddle.6–9 Osseous fixation in fibula free flap-based mandibular reconstruction primarily relies on the use of either mini-plates (MP), which confer stability at the junction of the osteotomy or reconstruction bars (RB), which span the entire length of the defect.10 With these fixation options, osteocutaneous free tissue transfer has become an efficient and reliable criterion standard for the correction of segmental mandibular defects.
The benefit of using a rigid RB is the ability to conform the shape to that of the native mandible, thereby more precisely recreating the gonial angle and improving flap-mandible contact following fibular inset.11 The rapid and reliable restoration of mandibular form has rendered reconstruction bar fixation relatively commonplace for mandibular reconstruction. However, post-operative complications and decreasing flap bone density remain salient disadvantages of rigid RB fixation.12,13 These complications include both flap related outcomes9,14 such as surgical site infection, osteonecrosis, and flap loss, and plate related outcomes such as exposure, fracture, and hardware infection.7,8,15 Historically, the use of semi-rigid MP osteosynthesis was the preferred fixation method at our center and others, given the ease of fixation due to the ability to precisely contour the smaller and more malleable plates to individual mandibular segments and the ease of removal in the event of plate infection or exposure.16 With the advent of milled and prefabricated plates, this preference has waned, though the recent ability to prefabricate mini-plates may create a resurgence of this fixation method moving forward.
Despite the growing literature investigating the use of RB and MP fixation, there is currently no consensus as to the comparative safety profiles of these fixation techniques. Direct comparison of patient outcomes between fixation types is necessary to help further guide operative management for patients with segmental mandibular defects scheduled to undergo FFF-based reconstruction. The aim of this systematic review and meta-analysis is to compare complication rates associated with the use of MP versus RB fixation in vascularized FFF oncologic reconstruction of mandibular defects in an effort to better guide hardware utilization and preoperative virtual surgical planning.
Methods
Search Strategy and Eligibility Criteria
A systematic review and meta-analysis was performed according to PRISMA guidelines.17 Comprehensive literature search of PubMed/MEDLINE, Embase, and Cochrane databases pertaining to fibula free flap-based mandibular reconstruction with mini-plate and/or reconstruction bar fixation was conducted in January 2020. Databases were queried based on subject headings (MeSH, Emtree terms) and/or keywords in Title, Abstract and Keyword fields (Supplemental Figure 1). To avoid exclusion of articles with complications reported only in full text, outcome-related terms were not included in the query. The search strategies focused instead on components related to mandibular reconstruction with surgical plates and/or FFF. Boolean Operators “OR” and “AND” were used to combine the terms and search strategy components. Searches were limited to English in PubMed and Embase databases. Publications identified through the database search were manually queried by title and abstract. Full-text articles were screened for eligibility based on the inclusion/exclusion criteria and the resulting articles were chosen for the systematic review and analysis. Moreover, we queried the references in each of the articles included in our study; however, we were unable to identify additional studies that met inclusion criteria.
Data Extraction
Data were extracted manually by two independent evaluators (NS and KA) and input into a standard data collection template in Microsoft Excel. The following variables were collected: age at surgery, patient sex, history of smoking, diabetes mellitus, prior head and neck surgery, indication for mandibular reconstruction (malignant lesion versus benign lesion versus osteoradionecrosis), and radiation therapy (adjuvant versus neoadjuvant). Primary endpoints of interest included plate-related complications, wound infection, mal-union or non-union, total flap loss, partial flap loss, wound dehiscence, fistula formation, and re-operation for vascular compromise. Whereas minor complications are routinely defined as those post-operative sequelae that require conservative management and major complications are those outcomes that necessitate procedural or operative intervention, the variability in reporting did not allow for appropriate stratification of post-operative outcome severity. Of note, operative take-back for major complications other than arterial insufficiency or venous thrombosis were not routinely or consistently recorded, thereby rendering re-operation data extraction difficult. As such, re-operation or revision indication was limited to vascular compromise.
Statistical Analysis
Data were analyzed using the Cochrane RevMan Version 5.3 (Cochrane Collaboration, Copenhagen) and IBM SPSS Version 25 (IBM Corp., Armonk, N.Y.) statistical suites. Images were generated using the JASP statistical suite (JASP Group, Amsterdam) and Meta-Analyst software (Brown University, Providence, R.I.). Statistical significance was defined as a p value < 0.05. All p values and 95% confidence intervals (CI) were 2-sided. Because only 3 studies directly compared mini-plates to reconstruction bars, patient demographics and complication rates were calculated as weighted means/proportions and compared via Fisher exact testing. Only those outcomes that were reported in ≥3 studies were included in the analysis.
A meta-analysis comparing total flap loss and plate-related complication rates was conducted, as these variables were recorded in at least 3 studies that directly compared outcomes between mini-plate and reconstruction bar cohorts. These outcomes were weighted according to the inverse proportion of variance in each study, yielding weighted mean odds ratio (OR) and 95% confidence intervals for each study. Heterogeneity of effect size among studies was evaluated using χ2 testing (with p < 0.05 indicating heterogenous effects). Homogenous datasets were analyzed using fixed-effects modeling, whereas heterogenous variables were compared using random-effects modeling.
Results
Study Characteristics
The initial database search resulted in 4606 publications, with 2895 studies manually queried by title and abstract for articles focused on post-operative outcomes following FFF mandibular reconstruction with MP and/or RB fixation after removal of duplicates (Figure 1). Forty full-text articles were screened for eligibility against our inclusion/exclusion criteria (Table 1). Sixteen studies18–31 met inclusion criteria for this systematic review and meta-analysis (Table 2), with 1437 total patients having undergone FFF-based mandibular reconstruction with either MP or RB fixation. The mean age of patients presenting was 48.1 years (range, 12.9 – 66.4). The majority of patients were male (n = 845, 64.0%). Almost half of the patients had undergone prior head and neck surgery. With regard to medical comorbidities, 58.3% of patients were active or former smokers, and 5.7% had diabetes mellitus. The most common indication for mandibular resection was malignancy (43.2%), followed by benign head and neck lesions (29.5%) and osteoradionecrosis (10.1%). Notably, rates of adjuvant radiation therapy (31.8%) outnumbered rates of neoadjuvant radiation therapy (27.6%) in the malignancy cohort.
Figure 1.
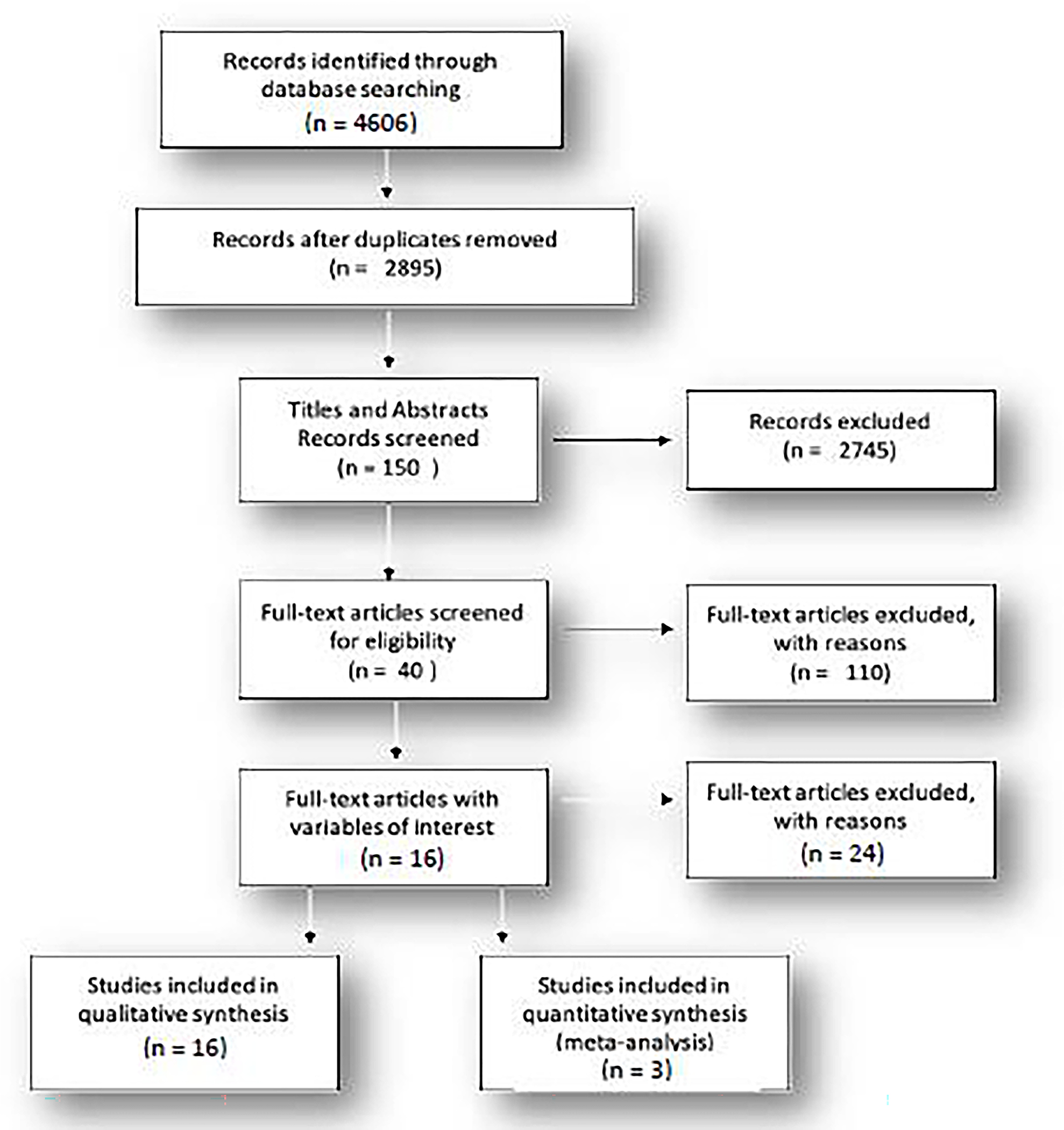
Meta-analysis data was collected following the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria |
|
|
| Mandibular reconstruction with fibula free flap and plate fixation (mini-plate or reconstruction bar) |
| Immediate reconstruction or delayed reconstruction |
|
|
| Exclusion Criteria |
|
|
| Single case reports |
| Surgical technique reports |
| Cadaver studies |
| Literary reviews without original data |
| Abstracts |
| Sample size < 10 FFF reconstructions |
| Use of non-fibula osteocutaneous free flaps (radial, iliac crest, scapular, etc.) |
| Language other than English |
FFF, fibula free flap
Table 2.
Study Characteristics
| Characteristic | No. Studies (%) |
|---|---|
|
| |
| Total | 16 |
| Study Design | |
| Retrospective Cohort | 14 (87.5) |
| Case Control | 1 (6.3) |
| Case Series | 1 (6.3) |
| Fixation Type | |
| Mini-Plate | 6 (37.5) |
| Reconstruction Bar | 7 (43.8) |
| Both | 3 (18.8) |
| National | 4 (25.0) |
| International | 12 (75.0) |
Post-Operative Outcomes
The most common complication following FFF-based mandibular reconstruction was plate-related exposure or fracture (n = 286, 26.8%) followed by wound dehiscence (14.0%), malunion/non-union (11.7%), and fistula formation (8.6%). Infection (6.8%), partial flap loss (7.7%), and total flap loss (6.0%) occurred at similar rates (Table 3). Re-operations performed for vascular compromise, either arterial insufficiency or venous thrombosis, occurred in nearly 6.5% of cases.
Table 3.
Overview of Post-Operative Complications
| Complication | Total | No. Studies |
|---|---|---|
|
| ||
| Infection | 54 (6.8) | 8 |
| Fistula | 14 (8.6) | 5 |
| Mal-Union/Non-Union | 28 (11.7) | 4 |
| Wound Dehiscence | 7 (14.0) | 2 |
| Total Flap Loss | 48 (6.0) | 12 |
| Partial Flap Loss | 23 (7.7) | 5 |
| Re-operation for Vascular Compromise | 24 (6.5) | 7 |
| Plate-Related Complication | 286 (26.8) | 10 |
Mini-Plate versus Reconstruction Bar
With regard to fixation type, 786 patients underwent FFF mandibular reconstruction with mini-plate (MP) fixation, whereas the remaining 651 underwent reconstruction bar (RB) fixation. Patients in the RB cohort demonstrated significantly higher rates of previous head and neck surgery, and reconstruction for malignant tumors and osteoradionecrosis (Table 4). In addition, these patients were more likely to receive adjuvant radiation therapy when compared to their MP counterparts. Patient groups were otherwise well-matched with respect to age, sex, and smoking history.
Table 4.
Patient Characteristics by Fixation Type
| Characteristic | Mini-Plate (%) | No. Studies | Reconstruction Bar (%) | No. Studies | p |
|---|---|---|---|---|---|
|
| |||||
| No. Patients | 828 | 10 | 685 | 11 | |
| Mean Age (Range), year | 46.3 (8.2 – 68.8) | 6 | 49.4 (15.4 – 73.2) | 8 | |
| Patient Sex | |||||
| Male | 435 (62.1) | 8 | 410 (66.1) | 9 | 0.136 |
| Female | 265 (37.9) | 8 | 210 (33.9) | 9 | 0.136 |
| Smoking | 39 (52.7) | 4 | 94 (61.0) | 3 | 0.253 |
| Diabetes | 2 (5.7) | 2 | NR | NR | - |
| Prior Head and Neck Reconstruction | 13 (14.6) | 3 | 140 (64.5) | 3 | < 0.001* |
| Indications for Mandibular Resection | |||||
| Malignancy | 249 (33.6) | 7 | 309 (47.5) | 10 | < 0.001* |
| Benign Lesion | 246 (33.2) | 7 | 190 (29.2) | 10 | < 0.001* |
| ORN | 10 (1.4) | 7 | 139 (21.4) | 10 | < 0.001* |
| Other | 235 (31.8) | 7 | 12 (1.9) | 10 | < 0.001* |
| Radiation | |||||
| Adjuvant | 10 (16.4) | 3 | 46 (40.0) | 3 | < 0.001* |
| Neoadjuvant | 4 (30.8) | 1 | 17 (27.0) | 2 | 0.745 |
NR, not reported; ORN, osteoradionecrosis
Statistically significant (p < 0.05)
Note, percentages for each variable were calculated with a denominator that represents the sum of patients within the corresponding number of studies, not necessarily the total number of patients in reconstruction bar or mini-plate cohorts.
Comparing complications following MP fixation to RB fixation, Fischer exact testing of weighted proportions demonstrated significantly higher rates of fistula formation (15.8% versus 4.7%, p = 0.04), total flap loss (9.4% versus 4.7%, p = 0.02), partial flap loss (20.6% versus 6.1%, p < 0.01), plate-related complications (32.5% versus 18.8%, p < 0.01), and re-operation for vascular indications (13.3% versus 4.0%, p<0.01) (Table 5). Rates of infection, malunion/non-union, and wound dehiscence were similar across both groups. Only 3 studies directly compared RB to MP fixation (Table 6).
Table 5.
Post-Operative Complications by Fixation Type
| Complication | Mini-Plate (%) | No. Studies | Reconstruction Bar (%) | No. Studies | p |
|---|---|---|---|---|---|
|
| |||||
| Infection | 42 (6.8) | 4 | 12 (6.7) | 5 | 0.863 |
| Fistula | 9 (15.8) | 3 | 5 (4.7) | 3 | 0.036* |
| Mal-Union/Non-Union | 15 (11.0) | 3 | 13 (12.6) | 3 | 0.690 |
| Wound Dehiscence | 7 (18.4) | 2 | 0 (0.0) | 1 | 0.174 |
| Total Flap Loss | 21 (9.4) | 7 | 27 (4.7) | 8 | 0.019* |
| Partial Flap Loss | 7 (20.6) | 2 | 16 (6.1) | 3 | < 0.001* |
| Re-operation for Vascular | 13 (13.3) | 4 | 11 (4.0) | 3 | < 0.001* |
| Compromise | |||||
| Plate-Related Complication | 241 (32.5) | 6 | 61 (18.8) | 7 | < 0.001* |
Statistically significant (p < 0.05)
Table 6.
Complication Rates in Comparative Studies (Mini-Plate versus Reconstruction Bar)
| Study | Year | Fixation | No. Patients | Infection (%) | Fistula (%) | Non-Union/Mal-Union (%) | Wound Dehiscence (%) | Total Flap Loss (%) | Partial Flap Loss (%) | Plate-Related Complications (%) |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Al-Bustani | 2016 | Mini-Plate | 13 | 0 (0.0) | 1 (7.7) | NR | 2 (15.4) | 1 (7.7) | NR | 4 (30.8) |
| Reconstruction Bar | 12 | 1 (8.3) | 0 (0.0) | NR | 0 (0.0) | 1 (8.3) | NR | 0 (0.0) | ||
| Kim | 2015 | Mini-Plate | 26 | NR | NR | 4 (15.4) | NR | 7 (26.9) | NR | 11 (42.3) |
| Reconstruction Bar | 21 | NR | NR | 4 (19.0) | NR | 5 (23.8) | NR | 7 (33.3) | ||
| Robey | 2008 | Mini-Plate | 86 | NR | NR | 8 (9.3) | NR | 9 (10.4) | NR | 16 (18.6) |
| Reconstruction Bar | 31 | NR | NR | 2 (6.5) | NR | 5 (16.1) | NR | 3 (9.7) | ||
NR, not reported
Plate-Related Complications
Rates of plate exposure or fracture in either MP or RB fixation following FFF-based mandibular reconstruction were investigated in 3 studies.27,30,32 We observed significant heterogeneity among study results (p < 0.01). Importantly, random-effects modeling demonstrated no significant difference in odds of plate-related complication between the two groups (OR 2.02, 95% CI 0.87 – 4.71, p = 0.10). However, we observed a trend toward significance, suggesting that mini-plate fixation may confer a higher risk of plate exposure or hardware fracture when compared to reconstruction bar fixation following fibula free flap reconstruction of the mandible (Figure 1). No differences in odd ratios were observed during sensitivity analysis.
Total Flap Loss
Three studies27,30,32 reported incidence of total flap loss between MP (17 of 125) and RB (11 of 64) cohorts, with homogeneity of result observed across studies (p = 0.76). Fixed-effects modeling demonstrated similar odds of total flap loss among MP and RB cohorts (OR 0.82, 95% CI 0.35–1.91). Sensitivity analysis demonstrated no difference in odds ratio with stepwise exclusion of studies (Table 7). Funnel plot was not constructed given limitation in the number of available comparative studies.
Table 7.
P-values for Sensitivity Analysis (Mini-Plate versus Reconstruction Bar)
| Study | Plate-Related Complication | Total Flap Loss |
|---|---|---|
|
| ||
| Al-Bustani, et al. 2016 | 0.219 | 0.648 |
| Kim, et al. 2015 | 0.102 | 0.431 |
| Robey, et al. 2008 | 0.309 | 0.844 |
Discussion
The use of the fibula free flap for mandibular reconstruction was first described by Hidalgo in 1989, and subsequently popularized by Wei and Zlotolow in the early 1990s.25,33–36 It has since become the most common vascularized bone flap for the reconstruction of segmental mandibular defects. Fibula bone segments require the use of either mini-plate or reconstruction bar fixation to confer stability at the osteotomy sites, both of which have unique advantages and disadvantages. Despite the availability of studies demonstrating the benefits of various fixation types, few directly compare safety profiles between MP and RB based reconstructions.27 In this systematic review and meta-analysis, we aimed to directly compare the complication profiles of MP and RB mediated fixation for FFF-based mandibular reconstruction.
Our review examined 16 studies that evaluated outcomes following FFF-based reconstruction of the mandible with MP and or RB and revealed significant differences in rates of hardware-related complications between the two fixation methods, with MP fixation conferring higher risk of plate exposure and plate fracture. Some authors have advocated for the use of MP fixation for osteocutaneous flap reconstruction of the mandible to avoid plate-related complications.37 In theory, a RB that spans the entire length of the vascularized bone flap is more likely to experience plate exposure when compared to MP, given the additional surface area of hardware requiring soft tissue coverage. Day et al. reported that the rate of plate exposure following RB fixation following vascularized bone flap-based mandibular reconstruction approached nearly 20% in their patient cohort.7 However, the results of our study suggest that MP fixation may be associated with higher rates of hardware-related complications following FFF reconstruction.
Recent advances in the construct of RBs may contribute to the difference in plate-related complications observed between the two cohorts. The newer generations of RB tend to have smaller profiles, with better biocompatibility, thereby mitigating some of the previously described post-operative sequelae.38 In addition, the introduction of locking technology to replace screw-based fixation has minimized pressure necrosis of the vascularized bone flap, resulting in decreased stress on the fixation hardware and fewer plate complications.39 Furthermore, the use of CAD/CAM technology has significantly reduced discrepancies in contour between the fixation plate and fibula free flap, thereby minimizing aberrant vectors of tension that may contribute to hardware failure.40–42 This has, in turn, reduced operating time and improved cosmesis by enabling preoperative virtual reconstruction of the jaw with pre-bent or prefabricated RB. Conversely, given the size of MPs, their location along the margin of the flap-mandible junction, and the degrees of freedom conferred by semi-rigid fixation, it is reasonable to speculate that stress distributed over a smaller surface area with continued mastication could contribute to the higher rates of plate fracture observed in the MP cohort. It is also possible that pre-fabrication of MPs along the contour of the reconstructed mandible using CAD/CAM technology could minimize angular deviation, thereby decreasing risk of plate fracture.43 Further studies are necessary to elucidate the role of CAD/CAM technology in MP fixation for fibula free flap reconstruction of the mandible.
This study revealed a greater incidence of flap-related complications in patients having undergone MP fixation, particularly with regard to partial/total flap loss, fistula formation, and vascular compromise requiring operative take-back. Contrary to prior reports, the results of our review suggest that patients who undergo MP fixation of FFF for mandibular reconstruction may be more susceptible to flap loss. We believe that the more recent studies included in our review benefited from improvements in design of modern RBs. Furthermore, it is critical to consider that flap loss likely may not occur due to complications arising from the presence of a foreign body, but rather, is more often associated with underlying patient comorbidities, oncologic management and, especially, technical error associated with microvascular free tissue transfer. Previous studies have demonstrated an association of flap failure with diabetes mellitus and smoking, secondary to impaired microcirculation.44,45 Our study population demonstrated comparable rates of smoking between fixation types, but data with regard to diabetes mellitus remained largely incomplete. In addition, post-operative complications, such as surgical site infection, can contribute to flap failure due to local inflammation and tissue edema that may interfere with the vascular supply of the free flap. Therefore, evaluation of patient outcome based on fixation type should include appropriate consideration of baseline patient morbidity to avoid confounding and improve the generalizability of results.
The deleterious effects of radiotherapy following free flap reconstruction of the mandible have been extensively reported within the literature. Vascular fibrosis and direct cytotoxicity conferred by radiation therapy can minimize tissue regeneration capacity along the wound bed.46 Therefore, patients who undergo head and neck irradiation are more susceptible to wound breakdown than their non-irradiated counterparts. Radiation therapy has been associated with the development of osteoradionecrosis of the vascularized bone flap, secondary to tissue hypoxia that occurs due to microcirculatory occlusion following radiation-induced inflammation and obliterative endarteritis.47 In their study, Robey et al. demonstrated that MP fixation of FFF for mandibular reconstruction may be protective against the development of osteoradionecrosis.30 This is likely due to the decreased surgical manipulation of irradiated bone segments for MP fixation when compared to RB placement.
Importantly, the timing of radiation may also influence rates of post-operative complication following mandibular reconstruction. Adjuvant radiotherapy results in direct damage to soft tissue coverage of the fibula free flap, thereby accentuating the potential for local wound breakdown and, subsequently, plate exposure. Neoadjuvant head and neck irradiation, conversely, results in damage to the native oral mucosa, but spares the skin paddle and vascularized bony segment of the fibula free flap, thereby reducing the risk of flap-related wound complications. Removal of irradiated tissue at the time of surgery and subsequent replacement with viable, non-irradiated tissue may also improve the local wound healing milieu, minimizing local breakdown or infection. The preponderance of adjuvant radiation therapy in our patient population may be a central driver of post-operative outcomes. However, the results of our analysis suggest that MP fixation may be associated with higher rates of wound complication, including fistula formation, despite higher rates of neoadjuvant radiation therapy. It is possible that the semi-rigid fixation conferred by MP allows for repeated micro-movement of the osteotomy site, resulting in loosening of the plate and predisposing toward fistula formation. Radiation therapy has long been regarded as an independent risk factor for fistula formation secondary to poor wound healing.48 As such, future investigations are necessary to better elucidate the role and timing of head and neck irradiation in the formation of wound-related complications for patients undergoing MP or RB fixation of osteocutaneous free flaps.
The main limitation of this review is the paucity of studies directly comparing post-operative complication rates between MP and RB fixation for FFF-based mandibular reconstruction. Those studies that are available focus more broadly on vascularized bone flaps, which may limit generalizability, as differences in flap type can confound analysis of post-operative complication rates. As such, we relied on the comparison of weighted means/proportions to identify differences in outcome between the two fixation types. In addition, heterogeneity in the reporting of complications rendered pooled analysis difficult, thereby limiting the generalizability of our results. No distinctions were made with regard to plate manufacture or thickness of RB, as most studies simply reported plate type (MP versus RB). We also could not account for the evolution of hardware over time. Early experiences with RB more likely included bulky plates, bent by the surgeon, which may confer greater rates of post-operative complication than the current pre-fabricated models based on CAD/CAM technology. This technology not only shortens the duration of operation but also provides for a better fit of the RB to the fibular free flap. Additionally, the interventions used were unlikely to have been performed by a single surgeon, thus rendering comparison among different publications challenging. As such, it may be difficult to effectively assess results from manuscripts published early in the decade to those published more recently. Moreover, differences in surgical technique, pre-operative planning, and post-surgical management cannot be controlled for statistically and, thus, may disproportionately skew the data. This work further highlights the challenge in comparing heterogenous populations from varying institutions with bias in management that may result in differing complication rates. Additionally, this heterogeneity in data precludes our ability to classify outcomes according to standard Clavien-Dindo classifications. However, we anticipate that the large total population size is sufficient to mitigate some of these confounding effects.
Conclusion
This systematic review and meta-analysis compares post-operative complication rates following mandibular reconstruction with FFF based on fixation technique. Our results suggest that MP use may be associated with higher rates of plate related complications and fistula formation. Whereas our analysis is limited by heterogeneity in outcome reporting, this study can serve as a template for future investigations evaluating the safety profiles of RB and MP in head and neck surgery. Additionally and as prefabricated miniplates become widely available, these data can be used to aid surgeon decision-making for the type of plate fixation in virtual surgical planning for operative management of segmental mandibular defects.
Supplementary Material
Supplemental Figure 1. Search strategy terms.
Figure 2.
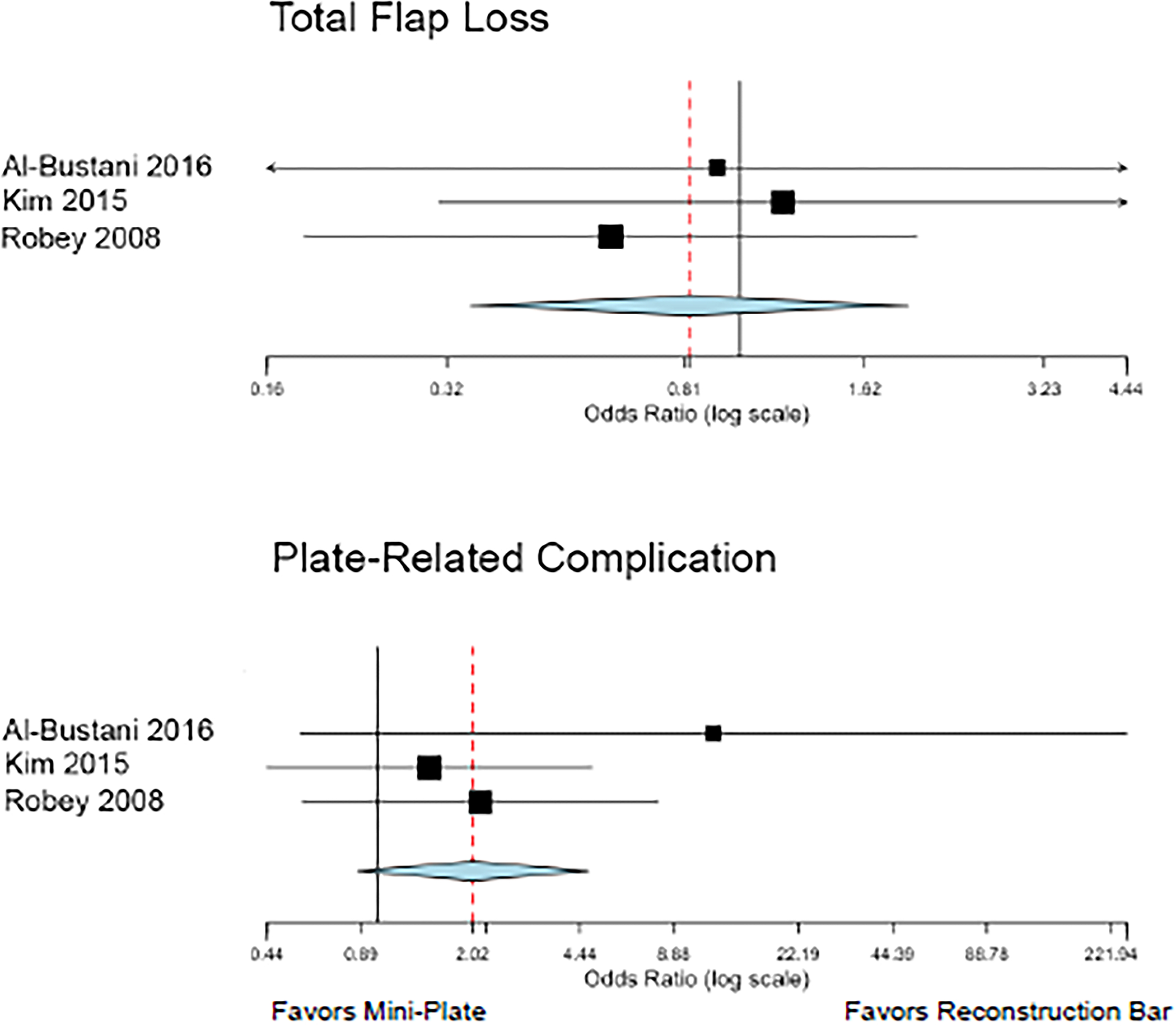
Forest plot depicting odds of total flap loss and plate-related complications between mini-plate and reconstruction bar fixation cohorts following fibula free flap-based mandibular reconstruction. No significant difference in odds of post-operative complications were observed between cohorts. However, there was a trend toward significance for plate-related complications, suggesting that mini-plate fixation may confer a higher risk of hardware fracture or plate exposure when compared to reconstruction bar fixation.
Footnotes
Conflicts of Interest
None Declared.
Ethical Approval
Not Required.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kumar BP, Venkatesh V, Kumar KA, Yadav BY, Mohan SR. Mandibular Reconstruction: Overview. J Maxillofac Oral Surg 2016; 15(4): 425–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Disa JJ, Cordeiro PG. Mandible reconstruction with microvascular surgery. Semin Surg Oncol 2000; 19(3): 226–34. [DOI] [PubMed] [Google Scholar]
- 3.Rogers SN. Quality of life perspectives in patients with oral cancer. Oral Oncol 2010; 46(6): 445–7. [DOI] [PubMed] [Google Scholar]
- 4.Rogers SN, Lowe D, Fisher SE, Brown JS, Vaughan ED. Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral Maxillofac Surg 2002; 40(1): 11–8. [DOI] [PubMed] [Google Scholar]
- 5.Van Cann EM, Dom M, Koole R, Merkx MA, Stoelinga PJ. Health related quality of life after mandibular resection for oral and oropharyngeal squamous cell carcinoma. Oral Oncol 2005; 41(7): 687–93. [DOI] [PubMed] [Google Scholar]
- 6.Blackwell KE. Unsurpassed reliability of free flaps for head and neck reconstruction. Arch Otolaryngol Head Neck Surg 1999; 125(3): 295–9. [DOI] [PubMed] [Google Scholar]
- 7.Day KE, Desmond R, Magnuson JS, Carroll WR, Rosenthal EL. Hardware removal after osseous free flap reconstruction. Otolaryngol Head Neck Surg 2014; 150(1): 40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsang GFZ, Zhang H, Yao C, et al. Hardware complications in oromandibular defects: Comparing scapular and fibular based free flap reconstructions. Oral Oncol 2017; 71: 163–8. [DOI] [PubMed] [Google Scholar]
- 9.Yao CM, Ziai H, Tsang G, et al. Surgical site infections following oral cavity cancer resection and reconstruction is a risk factor for plate exposure. J Otolaryngol Head Neck Surg 2017; 46(1): 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang ZL, Wang S, Sun CF, Xu ZF. Miniplates Versus Reconstruction Plates in Vascularized Osteocutaneous Flap Reconstruction of the Mandible. J Craniofac Surg 2019; 30(2): e119–e25. [DOI] [PubMed] [Google Scholar]
- 11.Seol GJ, Jeon EG, Lee JS, et al. Reconstruction plates used in the surgery for mandibular discontinuity defect. J Korean Assoc Oral Maxillofac Surg 2014; 40(6): 266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kennady MC, Tucker MR, Lester GE, Buckley MJ. Stress shielding effect of rigid internal fixation plates on mandibular bone grafts. A photon absorption densitometry and quantitative computerized tomographic evaluation. Int J Oral Maxillofac Surg 1989; 18(5): 307–10. [DOI] [PubMed] [Google Scholar]
- 13.Knott PD, Suh JD, Nabili V, et al. Evaluation of hardware-related complications in vascularized bone grafts with locking mandibular reconstruction plate fixation. Arch Otolaryngol Head Neck Surg 2007; 133(12): 1302–6. [DOI] [PubMed] [Google Scholar]
- 14.Herle P, Shukla L, Morrison WA, Shayan R. Preoperative radiation and free flap outcomes for head and neck reconstruction: a systematic review and meta-analysis. ANZ J Surg 2015; 85(3): 121–7. [DOI] [PubMed] [Google Scholar]
- 15.Poglio G, Grivetto F, Nicolotti M, Arcuri F, Benech A. Management of an exposed mandibular plate after fibula free flap with vacuum-assisted closure system. J Craniofac Surg 2011; 22(3): 905–8. [DOI] [PubMed] [Google Scholar]
- 16.van Gemert JTM, Abbink JH, van Es RJJ, Rosenberg A, Koole R, Van Cann EM. Early and late complications in the reconstructed mandible with free fibula flaps. J Surg Oncol 2018; 117(4): 773–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62(10): e1–34. [DOI] [PubMed] [Google Scholar]
- 18.Chaine A, Pitak-Arnnop P, Dhanuthai K, Ruhin-Poncet B, Bertrand JC, Bertolus C. A treatment algorithm for managing giant mandibular ameloblastoma: 5-year experiences in a Paris university hospital. Eur J Surg Oncol 2009; 35(9): 999–1005. [DOI] [PubMed] [Google Scholar]
- 19.Chaine A, Pitak-Arnnop P, Hivelin M, Dhanuthai K, Bertrand JC, Bertolus C. Postoperative complications of fibular free flaps in mandibular reconstruction: an analysis of 25 consecutive cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108(4): 488–95. [DOI] [PubMed] [Google Scholar]
- 20.Colletti G, Autelitano L, Rabbiosi D, et al. Technical refinements in mandibular reconstruction with free fibula flaps: outcome-oriented retrospective review of 99 cases. Acta Otorhinolaryngol Ital 2014; 34(5): 342–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Dean NR, Wax MK, Virgin FW, Magnuson JS, Carroll WR, Rosenthal EL. Free flap reconstruction of lateral mandibular defects: indications and outcomes. Otolaryngol Head Neck Surg 2012; 146(4): 547–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gazyakan E, Wu CW, Huang JJ, Engel H, Valerio IL, Cheng MH. Minimizing osteoradionecrosis after mandibular reconstruction and radiation in advanced head and neck cancer patients. J Surg Oncol 2016; 114(4): 399–404. [DOI] [PubMed] [Google Scholar]
- 23.Goil PP AN; Malhotra K; Chaudhary G Microvascular reconstruction with free fibula osteocutaneous flap in mandibular ameloblastomas—an institutional experience. Eur J Plast Surg 2018; 41: 15–20. [Google Scholar]
- 24.Han Z, Li J, Li H, Su M, Qin L. Single versus dual venous anastomoses of the free fibula osteocutaneous flap in mandibular reconstruction: a retrospective study. Microsurgery 2013; 33(8): 652–5. [DOI] [PubMed] [Google Scholar]
- 25.Hidalgo DA. Titanium miniplate fixation in free flap mandible reconstruction. Ann Plast Surg 1989; 23(6): 498–507. [DOI] [PubMed] [Google Scholar]
- 26.Iconomou TG, Zuker RM, Phillips JH. Mandibular reconstruction in children using the vascularized fibula. J Reconstr Microsurg 1999; 15(2): 83–90. [DOI] [PubMed] [Google Scholar]
- 27.Kim NK, Nam W, Kim HJ. Comparison of miniplates and biodegradable plates in reconstruction of the mandible with a fibular free flap. Br J Oral Maxillofac Surg 2015; 53(3): 223–9. [DOI] [PubMed] [Google Scholar]
- 28.Liu SP, Cai ZG, Zhang J, Zhang JG, Zhang Y. Stability and complications of miniplates for mandibular reconstruction with a fibular graft: outcomes for 544 patients. Br J Oral Maxillofac Surg 2016; 54(5): 496–500. [DOI] [PubMed] [Google Scholar]
- 29.Parise GK, Guebur MI, Ramos GHA, Groth AK, da Silva ABD, Sassi LM. Evaluation of complications and flap losses in mandibular reconstruction with microvascularized fibula flap. Oral Maxillofac Surg 2018; 22(3): 281–4. [DOI] [PubMed] [Google Scholar]
- 30.Robey AB, Spann ML, McAuliff TM, Meza JL, Hollins RR, Johnson PJ. Comparison of miniplates and reconstruction plates in fibular flap reconstruction of the mandible. Plast Reconstr Surg 2008; 122(6): 1733–8. [DOI] [PubMed] [Google Scholar]
- 31.Shen Y, Guo XH, Sun J, et al. Double-barrel vascularised fibula graft in mandibular reconstruction: a 10-year experience with an algorithm. J Plast Reconstr Aesthet Surg 2013; 66(3): 364–71. [DOI] [PubMed] [Google Scholar]
- 32.Al-Bustani S, Austin GK, Ambrose EC, Miller J, Hackman TG, Halvorson EG. Miniplates Versus Reconstruction Bars for Oncologic Free Fibula Flap Mandible Reconstruction. Ann Plast Surg 2016; 77(3): 314–7. [DOI] [PubMed] [Google Scholar]
- 33.Wei FC, Chen HC, Chuang CC, Noordhoff MS. Fibular osteoseptocutaneous flap: anatomic study and clinical application. Plast Reconstr Surg 1986; 78(2): 191–200. [DOI] [PubMed] [Google Scholar]
- 34.Wei FC, Seah CS, Tsai YC, Liu SJ, Tsai MS. Fibula osteoseptocutaneous flap for reconstruction of composite mandibular defects. Plast Reconstr Surg 1994; 93(2): 294–304; discussion 5–6. [PubMed] [Google Scholar]
- 35.Yadav PS, Ahmad QG, Shankhdhar VK, Nambi GI. There is no donor side specificity of fibula free flap for complex oromandibular reconstruction. Indian J Plast Surg 2010; 43(2): 177–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zlotolow IM, Huryn JM, Piro JD, Lenchewski E, Hidalgo DA. Osseointegrated implants and functional prosthetic rehabilitation in microvascular fibula free flap reconstructed mandibles. Am J Surg 1992; 164(6): 677–81. [DOI] [PubMed] [Google Scholar]
- 37.Kuhlefelt M, Laine P, Suominen-Taipale L, Ingman T, Lindqvist C, Thoren H. Risk factors contributing to symptomatic miniplate removal: a retrospective study of 153 bilateral sagittal split osteotomy patients. Int J Oral Maxillofac Surg 2010; 39(5): 430–5. [DOI] [PubMed] [Google Scholar]
- 38.Kawasaki G, Imayama N, Yoshitomi I, Furukawa K, Umeda M. Clinical Study of Reconstruction Plates Used in the Surgery for Mandibular Discontinuity Defect. In Vivo 2019; 33(1): 191–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Herford AS, Ellis E, 3rd. Use of a locking reconstruction bone plate/screw system for mandibular surgery. J Oral Maxillofac Surg 1998; 56(11): 1261–5. [DOI] [PubMed] [Google Scholar]
- 40.Rendenbach C, Sellenschloh K, Gerbig L, et al. CAD-CAM plates versus conventional fixation plates for primary mandibular reconstruction: A biomechanical in vitro analysis. J Craniomaxillofac Surg 2017; 45(11): 1878–83. [DOI] [PubMed] [Google Scholar]
- 41.Ciocca L, Mazzoni S, Fantini M, Persiani F, Marchetti C, Scotti R. CAD/CAM guided secondary mandibular reconstruction of a discontinuity defect after ablative cancer surgery. J Craniomaxillofac Surg 2012; 40(8): e511–5. [DOI] [PubMed] [Google Scholar]
- 42.Wilde F, Cornelius CP, Schramm A. Computer-Assisted Mandibular Reconstruction using a Patient-Specific Reconstruction Plate Fabricated with Computer-Aided Design and Manufacturing Techniques. Craniomaxillofac Trauma Reconstr 2014; 7(2): 158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lim SH, Kim MK, Kang SH. Precision of fibula positioning guide in mandibular reconstruction with a fibula graft. Head Face Med 2016; 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crippen MM, Patel N, Filimonov A, et al. Association of Smoking Tobacco With Complications in Head and Neck Microvascular Reconstructive Surgery. JAMA Facial Plast Surg 2019; 21(1): 20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou W, Zhang WB, Yu Y, et al. Risk factors for free flap failure: a retrospective analysis of 881 free flaps for head and neck defect reconstruction. Int J Oral Maxillofac Surg 2017; 46(8): 941–5. [DOI] [PubMed] [Google Scholar]
- 46.Haubner F, Ohmann E, Pohl F, Strutz J, Gassner HG. Wound healing after radiation therapy: review of the literature. Radiat Oncol 2012; 7: 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rathy R, Sunil S, Nivia M. Osteoradionecrosis of mandible: Case report with review of literature. Contemp Clin Dent 2013; 4(2): 251–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee EY, Kang JY, Kim KW, Choi KH, Yoon TY, Lee JY. Clinical Characteristics of Odontogenic Cutaneous Fistulas. Ann Dermatol 2016; 28(4): 417–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Search strategy terms.


