Abstract
Objectives:
Develop an approach for identifying Medicare beneficiaries residing in US assisted living (AL) communities in CY2018.
Design:
We employed the following data sources: national directory of licensed ALs, file of US addresses and their associated 9-digit ZIP codes (ZIP+4), Medicare Enrollment Data Base (EDB), Master Beneficiary Summary File (MBSF), and the Minimum Data Set (MDS).
Setting & Participants:
A total of 412,723 Medicare beneficiaries who lived in ZIP+4 codes associated with an AL were identified as residents. About 28% of the 16,682 ALs in which these beneficiaries resided were smaller communities (<25 beds).
Methods:
For each AL we identified ZIP+4 codes associated with its address. Using this ZIP+4 file, we searched through the Medicare EDB to identify beneficiaries who lived in each ZIP+4 code. MBSF and the MDS were used to exclude beneficiaries who died prior to 2018 and those whose AL and nursing home stays overlapped. We identified three cohorts of Medicare beneficiaries: 1) residents of a specific AL (one AL address per ZIP+4); 2) most likely AL residents; and 3) not likely AL residents. Comparisons across these cohorts were used to examine construct validity of our approach. Additional comparisons were made to AL residents based on the National Survey of Long-Term Care Providers (NSLTCP) and to FFS Medicare community-dwelling and long-stay nursing home residents.
Results:
The cohorts of beneficiaries identified as AL residents exhibited good construct validity. AL residents also showed similarity in demographic characteristics to the 2018 sample from the NSLTCP, and as expected were different from FFS community and nursing home beneficiaries.
Conclusion & Implications:
We developed a methodology for identifying Medicare beneficiaries who reside in ALs. As this residential setting continues to grow, future studies will need effective approaches for identifying AL residents in order to evaluate the quality of care they receive.
Keywords: assisted living, Medicare, methodology, ZIP+4 codes
Brief summary:
We present a new methodology for identifying Medicare Beneficiaries who reside in Assisted Living communities, and examine it’s sensitivity and specificity using national administrative data.
INTRODUCTION
Assisted Living (AL) communities, which provide congregate residential, board, supervision and social support services, and also coordinate personal care and some health-related services,1 have evolved over the past four decades to serve an increasingly varied and frail resident population. By various accounts, ALs serve upwards of 800,000 individuals, most of whom are older, Medicare eligible, experience multiple chronic conditions as well as physical and cognitive impairment.2–3 Because of the way ALs have evolved and remained regulated largely only at the state level,4 there is no central depository of data that can be used to systematically identify Medicare beneficiaries residing in ALs, to assess the quality of care they receive or to examine their health outcomes. Consequently, large scale national studies of this population and the quality of care provided in ALs have been limited.
In 2018 Thomas and colleagues pioneered a methodology that used national administrative data to identify Medicare beneficiaries residing in larger ALs (=>25 beds).5 The development of this methodology opened new opportunities for researchers to answer questions that previously remained not satisfactorily examined, due to the need for primary data collection and small samples this typically necessitates.6,7–9
While our original aim was to replicate this methodology to examine hereto unexplored questions about the AL population, we have been able to develop an alternative approach, which we believe may have several advantages: it is cheaper; allows for the identification of AL residents in small as well as larger communities; and may be more precise in identifying residents. Thus, the purpose of this study was to: 1) describe the development of this alternative approach; 2) examine the characteristics of AL residents identified through this method; and 3) compare the characteristics of thus identified AL residents to: a) a nationally representative sample of individuals in residential care communities, as reported in the 2018 National Study of Long Term Care Providers (NSLTCP), and b) to the CY2017 long-stay residents of US nursing homes and those who were community-dwelling Medicare beneficiaries.
METHODS
Creating AL Directory
ALs are certified and regulated at the state level. States vary significantly with regards to which aspects of AL operations are regulated, which state agencies are responsible for these regulations, and the regulatory stringency.4,10,11 Different terms and license categories are used to identify ALs both within and across states. For example, California licenses residential care facilities for the elderly. In Wisconsin, licensure terms for ALs include community-based residential facilities, residential care apartment complexes, and adult family homes. Georgia licenses AL communities and personal care homes. We used the regulatory reviews conducted by the National Center for Assisted Living (NCAL) for CY2019, as the primary source for identifying AL licensure categories in each state.12 Because we were interested primarily in identifying communities serving older Medicare beneficiaries, we excluded adult foster care homes. Most such homes are authorized under Medicaid AL waivers, do not typically accept private-pay residents, and are variously defined across states. These homes may differ from the more typical ALs in a number of ways, among them focusing on adults with disabilities, limiting the number of residents to no more than 6, and having care providers live in the same residence.13
AL directories were obtained from state Department of Health websites or directly from states upon request to appropriate agencies. Web pages were also scraped for additional information, such as bed/unit size or a physical address, when necessary. For each state, we created a list of ALs containing their physical address and the number of beds/units; the latter was not always available in two states (Connecticut and Michigan) because these states license home health agencies that provide services not the brick and mortar residences. After checking and deleting duplicates sharing the same AL name and exact address within each state, we concatenated the state lists to create a single national directory containing 34,514 communities (Figure 1).
Figure 1:
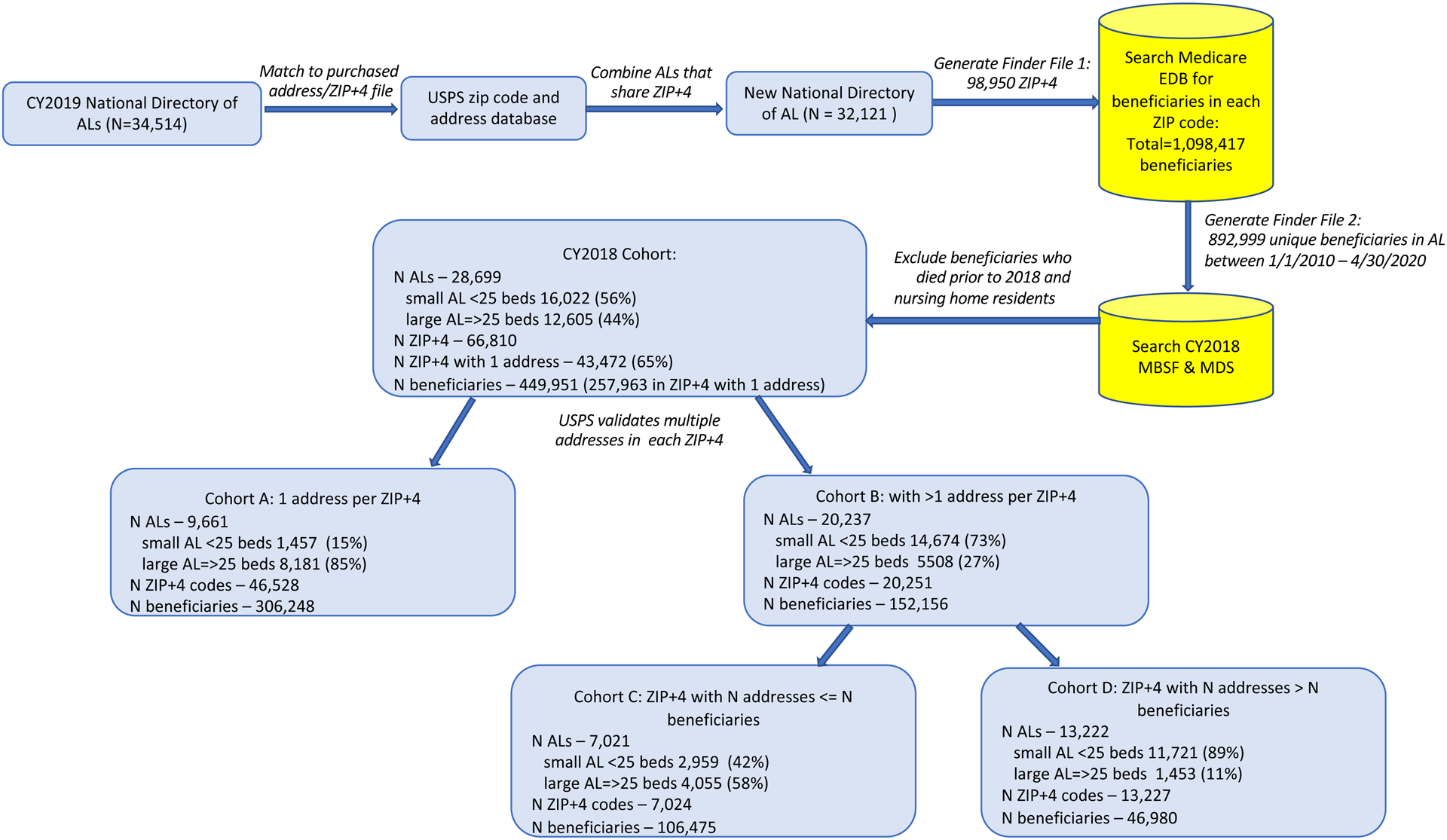
Flow Chart for Identifying AL Communities and Their Medicare Beneficiary Residents
Note:
“Cohort A: 1 address per ZIP+4” = ZIP+4 code cover only one physical address known to be AL. This cohort includes Medicare beneficiaries who are definitely residents of a specific AL community.
“Cohort B: >1 address per ZIP+4” = ZIP+4 code covers more than 1 physical address, with some known to be AL address and others not. This cohort includes Medicare beneficiaries who very likely to be AL residents as well as those who are not.
“Cohort C: ZIP+4 with N addresses <=N beneficiaries” = subset of Cohort B, in which more than one AL shares ZIP+4 codes and the number of Medicare beneficiaries exceeds the number of associated addresses. This cohort includes beneficiaries who very likely reside in ALs, but it is not possible to identify their specific AL of residence.
“Cohort D: ZIP+4 with N addresses > N beneficiaries” = subset of Cohort B, in which the number of addresses exceeds the number of Medicare beneficiaries. For these beneficiaries, it is not possible to distinguish between those who are residents of AL versus their Medicare eligible neighbors.
We then purchased, from a commercial provider, a CY2019 file of 9-digit ZIP codes (ZIP+4) and their associated addresses for all of the US. This allowed us to identify multiple ZIP+4 codes associated with an AL, which is common for larger communities. We identified about 4,500 mostly smaller (usually fewer than 10 beds) ALs sharing a ZIP+4. Many also shared a name (suggesting the same operating entity) and were located on the same street but with a different dwelling number. Recognizing that we would not be able to assign Medicare beneficiaries to their specific AL of residence, and yet not wanting to delete them entirely from our database, we treated these ALs as one (adding their bed counts), effectively reducing the number of ALs to 32,121. Merging this AL directory, based on its street addresses, with the ZIP+4 file, produced a list of 98,950 ZIP+4 codes. The process for identifying Medicare beneficiaries residing in ALs consisted of several steps, as shown in Figure 1, and described below.
Searching the Medicare Enrollment Data Base (EDB)
We submitted the file containing these ZIP+4 codes (i.e., finder file 1), to the designated CMS’ claims contractor. We received back a file containing 4,799,763 observations with 1,089,417 unique Medicare beneficiary identification numbers (BENE_ID) and over 2 million unique ZIP+4 codes. This file was derived from the Medicare enrollment data base (EDB), a record of beneficiaries’ enrollment information, entitlement, and changes of residence. EDB is based on information from the Social Security Administration (SSA) Master Beneficiary Record (MBR) and is updated daily. The file we received contained changes to the beneficiaries’ address of residence through 4/24/2020. For 3,422 ALs there were no matches to Medicare beneficiaries based on ZIP+4 in the EDB, and these ALs were excluded. The majority (74.7%) of these ALs had fewer than 25 beds.
We chose to subset the EDB file for beneficiaries who appeared to reside in ZIP+4 associated with AL addresses in our directory after 1/1/2010. This second finder file included 892,999 Medicare beneficiaries who had any record of AL residence between 1/1/2010 and 4/24/2020 (see Figure 1). Based on this file we received a cohort-specific Medicare Beneficiary Summary File (MBSF), and for purpose of excluding residents with an overlapping nursing home stay, we also used the national Minimum Data Set (MDS) containing nursing home assessments.
Identifying Medicare Beneficiaries Residing in Assisted Living
Step 1.
Using the MBSF, we identified and excluded Medicare beneficiaries who died prior to 2018. We then used the MDS to identify, and also exclude, beneficiaries whose nursing home stay overlapped with their AL stay. The resulting cohort included 449,951 Medicare beneficiaries who resided in one of the ZIP+4 associated with 28,699 ALs; 56% of the ALs were small (< 25 beds) and 44% were larger (=>25 beds). Information on bed size for 72 ALs was missing. Of these ZIP+4, 65% (N=43,472) had only 1 associated AL address, with a total of 257,963 Medicare residents.
Step 2.
An address within a ZIP+4 may be considered invalid if it does not exactly match to the US Postal Service (USPS) database. This commonly happens when an address is vacant or there is no physical structure or the address is new and as yet unregistered with the USPS. We requested the USPS to validate for us multiple addresses occurring within each ZIP+4. This increased the number of ZIP+4 codes with 1 AL address to 46,528, and the number of residents associated with a specific AL to 306,248. However, the number of ALs in which these Medicare beneficiaries resided dropped to 9,661, with only 15% being small (<25 beds) as the proportion of larger ALs (beds=>25) almost doubled to 85% (Figure 1, Cohort A).
Step 3.
The remaining 152,156 Medicare beneficiaries living in ZIP+4 with multiple validated addresses (Figure 1, Cohort B) may have included those still likely to be AL residents, as well as those who lived at a neighboring address within the same ZIP+4, but not in AL. [Please note that the total number of Medicare beneficiaries in Cohorts A and B does not add up to the number for the CY2018 Cohort because a small proportion of individuals move across ALs and/or zip codes, e.g., from an AL without memory care to one with.] In an attempt to identify AL residents in ZIP+4 with multiple addresses, we first compared the number of addresses to the number of Medicare beneficiaries in each ZIP+4. We assumed that if the number of Medicare beneficiaries identified within a ZIP+4 was greater than the number of associated addresses, there was a fair chance that these beneficiaries lived in AL. For example, if there were 5 validated addresses (including AL) and 16 Medicare beneficiaries, this suggested presence of a congregate living such as AL. We identified 7,024 ZIP+4 codes where the number of beneficiaries exceeded the number of associated addresses, accounting for 106,475 beneficiaries and 7,021 ALs, as shown in Cohort C (Figure 1). Many of the ALs in this cohort were small (42%) with larger ones accounting for 58%. Among the remaining beneficiaries (Cohort D, Figure 1) living in ZIP+4 in which the number of addresses exceeded the number of beneficiaries, it is not possible with any degree of certainty to distinguish those who may have lived in AL from their Medicare eligible but not AL residing neighbors. The computer code for creating these study cohorts will be provided by the authors, on request.
Construct Validity Testing
Medicare beneficiaries identified in Cohorts A and C (Figure 1) were respectively considered to be definitely and very likely AL residents. To test the extent to which these individuals were similar to or representative of what is known about AL residents, we made several comparisons. First, we compared the AL resident cohort, on selected characteristics (i.e., demographics and AL community size), to a nationally representative sample of individuals in residential care communities, obtained via the 2016 NSLTCP survey.14 Second, we compared the AL cohorts we identified as being AL residents to those who were not likely to represent that population (Cohort D). Because our approach to AL resident identification may perform differently for small and larger AL communities, we stratified our comparisons by AL size.
Third, we compared the AL resident cohort with the CY2017: a) long-stay nursing home residents; and b) community-dwelling Medicare beneficiaries, not in nursing homes and not residing in ZIP codes containing ALs, based on the national directory. Long-stay nursing home residents were defined as Medicare FFS beneficiaries who had a nursing home episode of 100 days or longer in 2017, following prior studies.15
MBSF was used to identify the residents’ characteristics such as their Medicare entitlement status and coverage, demographics, dual-eligibility for Medicaid (defined as enrolled in full Medicaid benefits for at least six months in CY2018), chronic conditions and other disabling conditions. Medicare beneficiaries with any Medicare Advantage (MA) plan coverage were excluded from these comparisons as the information on chronic conditions is not available for those without sufficient fee-for-service (FFS) coverage. We defined chronic conditions based on the first-ever occurrence date prior to 1/1/2018.
This study was reviewed and approved by the University of Rochester institutional review board.
RESULTS
In Figure 2, we present a comparison of key demographic characteristics for the AL population of Medicare beneficiary residents we identified (Cohorts A and C) and the nationally representative NSLTCP sample of residential care facilities for 2018.14 The NSLTCP survey estimates for age, gender and race/ethnicity were very similar to the population parameters we obtained for cohorts A+C. For example, the NSLTCP reported 89% of sampled residential care community residents to have been white, 67% female, and 55% age 85 or older, compared to 90%, 66%, and 54%, respectively, in cohorts A+C.
Figure 2:
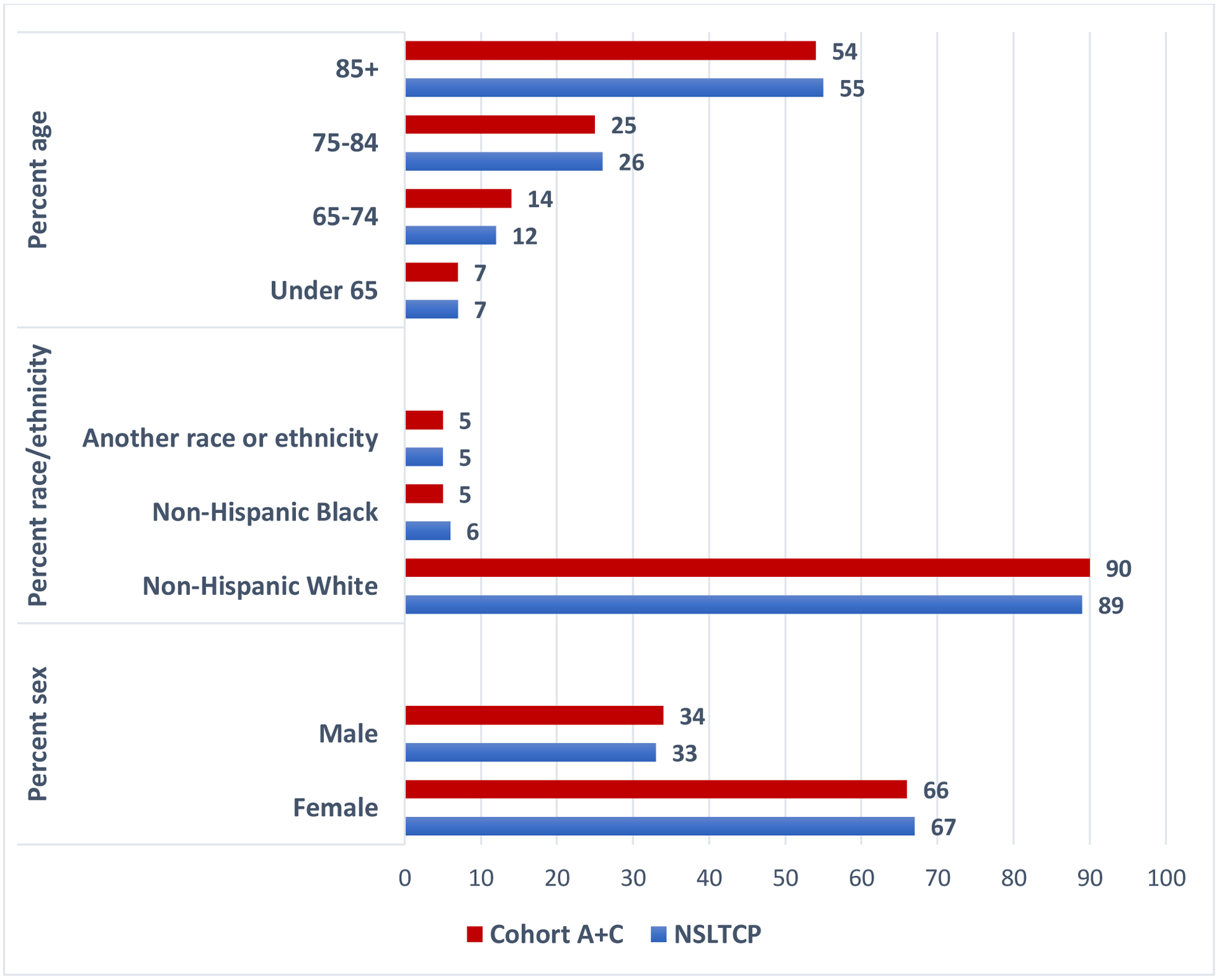
Comparison of Identified CY2018 Assisted Living Residents in Cohorts A+C to Residents in the 2018 National Survey of Long-Term Care Providers (NSLTCP)
Note: A+C= CY2018 Cohort of AL and their residents; NSLTCP=National Study of Long-term Care Providers.
Data sources: The AL population data (Cohorts A+C) were based on all ALs with identified Medicare beneficiary residents in CY2018, based on the methodology reported by the authors. The NSLTCP estimates were derived from the 2018 biennial survey, reported in Caffrey, Sengupta, and Melekin, NCHS Data Brief, No. 404, September 2021 (reference no.14)
In Table 1, we compare the FFS Medicare beneficiaries who were identified as clearly being AL residents (Cohort A), those who very likely were (Cohort C), the combined A+C cohorts, and the beneficiaries among whom residence in AL was much less likely (Cohort D). We were able to identify 412,723 Medicare beneficiaries (both FFS and MA), 74% of whom may be linked to a specific AL community located in a ZIP+4 not being shared with other addresses (Cohort A). The remaining 26% very likely resided in AL, but we could not differentiate the specific AL of residence among the 2 or more ALs sharing the same ZIP+4 (Cohort C). Roughly 28% of ALs housing residents of combined Cohorts A and C were small (<25 beds), but that proportion dropped to 15% for residents of Cohort A, and increased to 42% for residents of Cohort C. This is consistent with the distribution of urban-rural location shown for these two cohorts, which was significantly more urban (86.2%) for Cohort A, compared to Cohort C (78.8%). Furthermore, consistent with the more rural location and with the higher proportion of small communities were the residents’ distributions of age, race-ethnicity, and dual status. Residents in Cohort A, compared to C, were older (mean age 84.5 vs. 77.5), more likely to be non-Hispanic white (93.1% vs. 81.2%) and much less likely to be dually eligible (13.6% vs. 45.0%). Despite these differences, beneficiaries in Cohorts A and C were similar with regard to most chronic conditions. For example, comparing Cohort A to C, we found similar prevalence of ADRD (41.2% vs. 49.8%), CHF (43.2% vs. 44.0%), diabetes (40.4% vs. 48.2%) and chronic kidney disease (47.6% vs. 48.5%). By contrast, beneficiaries in Cohort D, who reside largely outside of ALs, were substantially different on virtually all characteristics. This population was more urban (89.0%), younger (average age of 69.5), less non-Hispanic white (60.5%) and with lower prevalence of chronic conditions; 18.5% ADRD, 18.8% CHF, 29.8% diabetes, 26.7% chronic kidney disease.
Table 1:
Characteristics of FFS Medicare Beneficiaries by AL Residence Certainty
| Beneficiary Characteristics | Medicare FFS Beneficiaries Assigned to AL | Medicare FFS Beneficiaries Not Assigned to AL | |||
|---|---|---|---|---|---|
| Cohort A 1 address per zip9 | Cohort C Zip9 with N addresses<=N beneficiaries | Cohort A+C Combined | Cohort D Zip9 with N addresses> N beneficiaries | ||
| All residents (FFS+MA) | 306248 | 106475 | 412723 | 46980 | |
| FFS residents | 203185 | 70299 | 273484 | 28181 | |
| Pct. total (not in MA) | 66.3% | 66.0% | 66.2% | 60.0% | |
| Total number of ALs | 9661 | 7021 | 16682 | 13222 | |
| Pct. small AL | 15% | 42% | 28% | 89% | |
| Pct. large AL | 85% | 58% | 72% | 11% | |
| Urban-rural location | |||||
| Urban | 86.2% | 78.8% | 84.3% | 89.0% | |
| Large rural city/town | 7.9% | 10.9% | 8.7% | 5.9% | |
| Small or isolated rural town | 5.1% | 9.9% | 6.4% | 4.3% | |
| Missing | 0.7% | 0.4% | 0.6% | 0.8% | |
| Age- mean (SD) | 84.5 (9.69) | 77.5 (14.1) | 82.7 (11.4) | 69.5 (12.4) | |
| Pct. <65 | 3.7% | 15.2% | 6.6% | 17.9% | |
| 65–74 | 10.3% | 25.0% | 14.1% | 57.6% | |
| 75–84 | 26.6% | 21.9% | 25.4% | 12.7% | |
| 85–94 | 49.1% | 30.2% | 44.3% | 9.6% | |
| 95 and over | 10.2% | 7.7% | 9.6% | 2.2% | |
| Gender - female | 67.5% | 60.5% | 65.7% | 53.5% | |
| Race/Ethnicity | |||||
| Non-Hispanic White | 93.1% | 81.2% | 90.1% | 60.5% | |
| Non-Hispanic Black | 3.1% | 9.8% | 4.8% | 15.3% | |
| Hispanic | 1.6% | 5.0% | 2.5% | 10.8% | |
| Other | 2.2% | 4.0% | 2.6% | 13.3% | |
| Dual Eligibility | 13.6% | 45.0% | 21.7% | 23.0% | |
| Chronic Conditions | |||||
| ADRD | 41.2% | 49.8% | 43.4% | 18.5% | |
| COPD | 36.4% | 41.7% | 37.8% | 19.4% | |
| CHF | 43.2% | 44.0% | 43.4% | 18.8% | |
| DIABETES | 40.4% | 48.2% | 42.4% | 29.8% | |
| MOBILITY IMP | 10.0% | 13.7% | 10.9% | 6.3% | |
| CHRONIC KIDNEY | 47.6% | 48.5% | 47.8% | 26.7% | |
| ISCHEMIC HEART | 63.2% | 59.4% | 62.2% | 29.3% | |
| RHEUMATOID/OSTEO ARTH | 78.2% | 67.6% | 75.5% | 37.1% | |
| OBESITY | 23.2% | 28.5% | 24.5% | 20.1% | |
| PVD | 45.2% | 48.5% | 46.0% | 18.8% | |
| CATARACT | 85.2% | 69.0% | 81.0% | 35.0% | |
| GLAUCOMA | 34.4% | 26.7% | 32.4% | 14.2% | |
| OSTEOPOROSIS | 42.1% | 32.1% | 39.5% | 14.0% | |
| ANEMIA | 75.9% | 73.8% | 75.3% | 38.5% | |
| HYPERTENSION | 90.3% | 85.8% | 89.1% | 55.8% | |
| HYPOTENSION | 42.4% | 39.4% | 41.6% | 19.9% | |
| ATRIAL FIBRULATION | 29.0% | 22.1% | 27.2% | 8.7% | |
| DRUG ABUSE | 6.3% | 12.7% | 8.0% | 7.8% | |
| ASTHMA | 18.8% | 20.2% | 19.1% | 11.9% | |
| CANCER | 22.1% | 16.0% | 20.6% | 8.9% | |
| DEPRESSION | 54.6% | 64.2% | 57.1% | 33.3% | |
| HIP FRACTURE | 11.6% | 10.5% | 11.3% | 3.5% | |
| HYPERLIPIDEMIA | 86.6% | 79.2% | 84.7% | 52.2% | |
| STROKE | 28.9% | 27.8% | 28.6% | 11.8% | |
In Table 2, we present another comparison of AL Cohorts A+C with the CY2017 national sample of Medicare beneficiaries who were long-stay nursing home residents and those who resided in the community. As expected, AL residents were substantially older than the community dwellers (average age 82.7 vs. 70.6), but not when compared to nursing home residents (average age of 80.8). They were also more likely to be non-Hispanic white (90.1%) than either the community (77.2%) or the nursing home (78.3%) residents. The proportion of individuals with chronic conditions was also distributed as expected, with AL residents mostly showing lower prevalence than the nursing home residents, but higher compared to the community.
Table 2:
Characteristics of FFS Medicare AL Residents Compared with Community-Dwelling and Long-Stay Nursing Home Residents
| AL Residents Cohorts A+C (CY2018) | Community-dwelling Residents (CY2017) | Long-stay Nursing Home Residents (CY2017) | ||
|---|---|---|---|---|
| Variables | N=273,484 | N=39,002,012 | N=957,660 | |
| Point Estimate | 95% CI | Point Estimate | Point Estimate | |
| Age - mean (SD) | 82.7 | [82.5, 82.9] | 70.6 (11.9) | 80.8 (12.3) |
| Pct. <65 | 6.6% | [6.3%, 7.0%] | 16.0% | 10.2% |
| 65–74 | 14.1% | [13.7%, 14.5%] | 50.0% | 17.9% |
| 75–84 | 25.4% | [25.1%, 25.7%] | 23.4% | 26.5% |
| 85–94 | 44.3% | [43.8%, 44.7%] | 9.3% | 35.1% |
| 95 and over | 9.6% | [9.4%, 9.8%] | 1.2% | 10.2% |
| Gender - female | 65.7% | [65.4%, 66.0%] | 52.8% | 65.8% |
| Race/ethnicity | ||||
| Non-Hispanic White | 90.1% | [89.7%, 90.5%] | 77.2% | 78.3% |
| Non-Hispanic Black | 4.8% | [4.5%, 5.1%] | 9.5% | 13.0% |
| Hispanic | 2.5% | [2.3%, 2.6%] | 7.0% | 5.4% |
| Other | 2.6% | [2.5%, 2.8%] | 6.3% | 3.3% |
| Dual Eligibility | 21.7% | [20.9%, 22.5%] | 11.1% | 68.8% |
| Chronic Conditions | ||||
| ADRD | 43.4% | [42.9%, 43.9%] | 7.4% | 74.0% |
| COPD | 37.8% | [37.4%, 38.2%] | 17.4% | 44.6% |
| CHF | 43.4% | [43.0%, 43.8%] | 15.6% | 55.6% |
| DIABETES | 42.4% | [42.0%, 42.9%] | 26.7% | 54.2% |
| MOBILITY IMP | 10.9% | [10.7%, 11.1%] | 3.0% | 23.1% |
| CHRONIC KIDNEY | 47.8% | [47.5%, 48.2%] | 21.1% | 55.4% |
| ISCHEMIC HEART | 62.2% | [61.8%, 62.6%] | 30.7% | 66.4% |
| RHEUMATOID/OSTEO ARTHRITIS | 75.5% | [75.1%, 75.8%] | 39.5% | 72.7% |
| OBESITY | 24.5% | [24.2%, 24.8%] | 17.7% | 27.1% |
| PVD | 46.0% | [45.5%, 46.5%] | 13.3% | 60.2% |
| CATARACT | 81.0% | [80.6%, 81.4%] | 42.5% | 75.9% |
| GLAUCOMA | 32.4% | [32.1%, 32.7%] | 15.3% | 26.9% |
| OSTEOPOROSIS | 39.5% | [39.2%, 39.9%] | 13.3% | 35.9% |
| ANEMIA | 75.3% | [75.0%, 75.7%] | 35.9% | 82.7% |
| HYPERTENSION | 89.1% | [88.9%, 89.3%] | 57.8% | 92.2% |
| HYPOTENSION | 41.6% | [41.3%, 41.9%] | 19.2% | 40.0% |
| ATRIAL FIBRULATION | 27.2% | [27.0%, 27.5%] | 9.3% | 26.1% |
| DRUG ABUSE | 8.0% | [7.8%, 8.2%] | 4.1% | 8.8% |
| ASTHMA | 19.1% | [18.9%, 19.3%] | 10.4% | 18.6% |
| CANCER | 20.6% | [20.4%, 20.8%] | 10.4% | 16.0% |
| DEPRESSION | 57.1% | [56.7%, 57.5%] | 25.1% | 72.5% |
| HIP FRACTURE | 11.3% | [11.1%, 11.5%] | 1.9% | 15.6% |
| HYPERLIPIDEMIA | 84.7% | [84.5%, 85.0%] | 55.8% | 80.3% |
| STROKE | 28.6% | [28.4%,28.9%] | 8.8% | 38.5% |
Note: 95% Confidence intervals (CI) were calculated using robust standard errors clustered at the AL level.
DISCUSSION
As the number of US adults age 65 or older continues to increase over the next 30 years, and their needs for long term services and supports also grow,16 residential preferences will continue to shift from nursing homes to less care intense settings such as AL.17 Contributing to this movement to community-based programs are state Medicaid policies aimed at rebalancing long-term services and supports (LTSS) from nursing homes to community-based residential care that includes ALs.18,19 These shifts in care preferences may be further accelerated in the wake of the COVID-19 pandemic that devastated nursing homes. Given these trends the importance of accurately capturing the size, characteristics, and service use of residential care population is clear, but the means for doing so have been limited largely to survey data.20 In 2018, Thomas and colleagues made a critical breakthrough in identifying residents of AL communities.5 Their method relied on a combination of place of service (POS) and residence indicators in the claims data, using the first 7 digits of a 9 digit ZIP code for Medicare beneficiaries identified in the claims to “validate 9-digit ZIP codes” of ALs, and then compiling a list of ZIP+4 codes of those who matched to the first 7 digits of an AL ZIP code.5 This highly innovative methodology, has already yielded a number of important national studies.
Building on this work, we developed an alternative approach for identifying AL residents, which we think has several important advantages, including being cheaper, capable of identifying residents of small ALs, and overall being more sensitive and specific in identifying AL residents. First, the method developed by Thomas et al., requires access to the home health outcome and assessment information set (OASIS) and to the Medicare Carrier file (physician/supplier Part B), as an initial step in identifying beneficiaries receiving services in AL, based on POS or residence codes. These datasets are expensive to obtain, particularly if they are not directly germane to the study aims. Our approach relies entirely on ZIP+4 and AL addresses and is therefore a cheaper alternative. Second, our method allows for finding Medicare beneficiaries residing in small (<25 beds) communities. These communities represent more than half of all ALs. Reports based on survey data have shown residents of small ALs to be younger, more likely to be minorities and dually eligible compared to the residents of larger ALs.14,21 It is, therefore, important that future studies focusing on AL quality, autonomy, person-centered care, and outcomes do not neglect to include these communities and their residents in analyses. Although our methodology has only been able to capture 28% of small ALs, our findings with regard to the characteristics of their residents are consistent with prior survey-based studies. Third, our findings suggest that the ZIP+4 methodology we developed is quite precise in two regards. It appears to have good construct validity in identifying residents within a specific AL community rather than only attributing Medicare beneficiaries to ALs in general. The differences we have shown between Cohorts A and C, point to the sensitivity of the approach. At the same time, the differences we were able to document between beneficiaries identified as AL residents and those who were not, point to the specificity of our method in distinguishing between AL and non-AL Medicare beneficiaries.
Several limitations should be noted. We relied solely on the chronic conditions segment of the MBSF to identify residents’ prevalence of conditions. For those who were enrolled in the MA plans chronic conditions are mostly missing and therefore we excluded these beneficiaries from our comparison analyses. As MA accounted for a large (over 30%) and growing proportion of older Medicare beneficiaries, this is a limitation not just of our study, but any studies that rely on the MBSF for this information. Furthermore, as the NSLTCP estimates suggest, there were more than 900,000 residents in residential care communities,14 yet we identified far fewer. Our study cohort is limited to Medicare beneficiaries whose EDB address corresponded to the ZIP+4 of an AL community. It may be that not all residents estimated via the NSLTCP were Medicare beneficiaries. It is also possible that some individuals who are AL residents do not report to Medicare (i.e., EDB) their actual physical address, but rather provide a mailing address of a family member responsible for financial/legal matters. The study cohort we identified is very close, in size, to the CY2014 sample based on the methodology developed by Thomas and colleagues,9 but it nevertheless is considerably smaller than the NSLTCP estimate and thus may not allow to generalize to all AL residents. Of the 16,682 ALs in which our identified Medicare beneficiaries resided, 28% were small (<25 beds). Thus, while we were able to identify Medicare beneficiaries residing in more than 1/4th of these ALs, beneficiaries residing in the majority of small ALs could not be attributed to a specific community. Finally, it may be worth noting that we employed ZIP codes from CY2019 but MBSF data from CY2018. ZIP codes do tend to change as new developments occur in an area. Thus, it is possible that not all 2019 ZIP codes may have corresponded to the 2018 AL address; this is more likely to affect non-urban areas and thus smaller ALs.
Conclusions and Implications
In conclusion, we developed an alternative methodology for identifying Medicare beneficiaries who reside in AL communities. Today, ALs encompass half of all long-term care beds, and extensively serve frail and impaired individuals. With Medicaid rebalancing of LTCSS increasingly funding AL as an alternative to nursing homes, the proportions of dual and minority residents in ALs are likely to grow. Given these changes, and the regulatory, financial, and workforce complexities increasingly affecting the residential care market,22 understanding how these factors influence care quality and outcomes, and to assess potential disparities in care, has become essential. Currently, there is no centralized, federally mandated data collection in ALs that would allow researchers to address such critical research and policy issues as, for example, whether disparities in care exist within and/or across ALs,23 is there a relationship between AL community size and residents’ health characteristics21 or with the state AL-specific regulatory stringency,4 or how post-acute care transitions and outcomes vary across communities.24 Thus, having alternative methodologies that allow researchers to more specifically identify AL residents, in small as well as in large communities, and to do so without the expense of obtaining claims data, other than that strictly needed to answer the questions of interest, should be of interest to researchers and policy makers in the AL arena.
Acknowledgments:
Thank you to Dr. Kali Thomas and her group at Brown University for the many helpful discussions that have made this manuscript better.
The AHRQ funded our study but had no role in the design or preparation of the manuscript.
Funding source:
This work was supported by the Agency for Healthcare Research and Quality grant number R01HS026893
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose
REFERENCES
- 1.Wilson KB. Historical evolution of assisted living in the United States, 1979 to the present. The Gerontologist 2007;47 Spec No:8–22. [DOI] [PubMed] [Google Scholar]
- 2.Caffrey C, Harris-Kojetin L, Rome V, Sengupta M. Operating characteristics of residential care communities, by community bed size: United States, 2012. NCHS data brief 2014:1–8. [PubMed] [Google Scholar]
- 3.Caffrey C, Harris-Kojetin L, Sengupta M. Variation in Residential Care Community Resident Characteristics, by Size of Community: United States, 2014. NCHS data brief 2015:1–8. [PubMed] [Google Scholar]
- 4.Temkin-Greener H, Mao Y, Ladwig S, Cai X, Zimmerman S, Li Y. Variability and Potential Determinants of Assisted Living State Regulatory Stringency. J Am Med Dir Assoc 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas KS, Dosa D, Gozalo PL, et al. A Methodology to Identify a Cohort of Medicare Beneficiaries Residing in Large Assisted Living Facilities Using Administrative Data. Med Care 2018;56:e10–e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fabius CD, Thomas KS. Examining Black-White Disparities Among Medicare Beneficiaries in Assisted Living Settings in 2014. J Am Med Dir Assoc 2019;20:703–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas KS, Belanger E, Zhang W, Carder P. State Variability in Assisted Living Residents’ End-of-Life Care Trajectories. J Am Med Dir Assoc 2020;21:415–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hua C, Zhang W, Cornell P, Rahman M, Dosa D, Thomas K. Characterizing Emergency Department Use in Assisted Living. JAMDA 2020;July 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabius C, Cornell P, Zhang W, Thomas K. State Medicaid Financing and Access to Large Assisted Living Settings for Medicare-Medicaid Dual-Eligibles. Medical Care Research and Review 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carder P, O’Keeffe J, O’Keeffe C. Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition. 2015; Rockville, MD. [Google Scholar]
- 11.Smith L, Carder P, Bucy T, et al. Connecting policy to licensed assisted living communities, introducing health services regulatory analysis. Health Serv Res 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NCAL. National Center for Assisted Living. 2019 Assisted Living State Regulatory Review. 2019. https://www.ahcancal.org/Assisted-Living/Policy/Pages/state-regulations.aspx
- 13.Mollica RL, Simms-Kastelein K, Cheeks M, Baldwin C, Fernham J, al. e. Building Adult Foster Care: What States Can Do. Washington DC.: AARP; 2009. [Google Scholar]
- 14.Caffrey C, Sengupta M, Melekin A. Residential Care Community Resident Characteristics: United States, 2018. NCHS Data Brief No. 404, September 2021. [PubMed] [Google Scholar]
- 15.RTI. Research Triangle Institute. MDS 3.0 Quality Measures: User’s Manual 2016.
- 16.Thach NT, Wiener JM. An Overview of Long-Term Services and Supports and Medicaid: Final Report. . Waltham, MA: RTI International; 2018. [Google Scholar]
- 17.Cornell PY, Zhang W, Thomas KS. Changes in Long-Term Care Markets: Assisted Living Supply and the Prevalence of Low-Care Residents in Nursing Homes. J Am Med Dir Assoc 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grabowski DC, Stevenson DG, Cornell PY. Assisted Living Expansion and the Market for Nursing Home Care. Health Services Research 2012;47:2296–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silver BC, Grabowski DC, Gozalo PL, Dosa D, Thomas KS. Increasing Prevalence of Assisted Living as a Substitute for Private-Pay Long-Term Nursing Care. Health Serv Res 2018;53:4906–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zimmerman S, Guo W, Mao Y, Li Y, Temkin-Greener H. Health Care Needs in Assisted Living: Survey Data May Underestimate Chronic Conditions. JAMDA 2020;December 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khatutsky G, Ormond C, Wiener J, et al. Residential Care Communities and Their Residents in 2010: A National Portrait. Waltham, Mass.: Centers for Disease Control and Prevention. March 2016. https://stacks.cdc.gov/view/cdc/39062 [Google Scholar]
- 22.Zimmerman S, Carder P, Schwartz L, Silberback J, Temkin-Greener H, et al. The Imperative to Reimagine Assisted Living. JAMDA, 2021. Dec 31; S1525–8610(21)01055–0.doi: 10.1016/j.jamda.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Temkin-Greener H, Mao Y, McGarry B, Zimmerman S, Li Y. Healthcare Use and Outcomes in Assisted Living Communities: Race, Ethnicity, and Dual Eligibility. Medical Care Research and Review, October 8, 2021. doi: 10.1177/10775587211050189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Mao Y, McGarry B, Temkin-Greener H. Post-acute care transitions and outcomes among Medicare beneficiaries in assisted living communities. JAGS, Accepted for publication December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]


