Abstract
Purpose
Postoperative recovery is a complex process with physiologic, functional, and psychologic dimensions. Postoperative quality of recovery is considered as a crucial outcome following surgery and anesthesia. The objective of this study was to assess and compare the quality of postoperative recovery and health status before and after surgery, in patients undergoing elective surgery.
Methods
This observational, prospective study was conducted on patients proposed for elective surgery. Evaluation of postoperative recovery was performed using the Postoperative Quality of Recovery Scale and health status was assessed by applying the EuroQol assessing problems in five dimensions: mobility, personal care, usual activities, pain/discomfort, and anxiety/depression, and the World Health Organization Disability Assessment Schedule 2.0. Poor quality of recovery was defined as recovery in fewer than two domains at postoperative Day 1 in the Postoperative Quality of Recovery Scale.
Results
Before surgery (D0), patients with poor quality of recovery had median Visual Analog Scale scores in EuroQol similar to those of patients without poor quality of recovery, but they had more problems in the mobility, usual activities, pain/discomfort, and anxiety/depression dimensions. At 3 months after surgery, patients with poor quality of recovery had median Visual Analog Scale scores in EuroQol similar to those of patients without poor quality of recovery, but they maintained more problems in the pain/discomfort dimension. Patients with poor quality of recovery scored significantly higher on the World Health Organization Disability Assessment Schedule 2.0 scale at baseline, although the results were similar at 3 months.
Conclusions
Patients with poor quality of recovery had the worst health status at D0. Evaluation at 3 months indicated similar rates of problems in EuroQol (except for pain/discomfort) and World Health Organization Disability Assessment Schedule 2.0 scores were similar.
Keywords: Postoperative recovery, Poor quality of recovery, Health status, WHODAS, EQ-5D
Resumo
Objetivo
A recuperação pós-operatória é um processo complexo com dimensões fisiológicas, funcionais e psicológicas. A qualidade da recuperação pós-operatória é considerada um resultado crucial após cirurgia e anestesia. O objetivo deste estudo foi avaliar e comparar a qualidade da recuperação pós-operatória e o estado de saúde antes e depois da cirurgia em pacientes submetidos à cirurgia eletiva.
Métodos
Este estudo observacional prospectivo foi feito com pacientes agendados para cirurgia eletiva. A avaliação da recuperação pós-operatória foi feita usando a Escala de Qualidade da Recuperação Pós-operatória (Postoperative Quality of Recovery Scale) e o estado de saúde foi avaliado com a aplicação do EuroQol, que analisa problemas em cinco dimensões (mobilidade, cuidados pessoais, atividades habituais, dor/desconforto e ansiedade/depressão) e a ferramenta para medida de incapacidade desenvolvida pela Organização Mundial da Saúde (World Health Organization Disability Assessment Schedule 2.0). Má qualidade de recuperação foi definida como uma recuperação em menos de dois domínios da Escala de Qualidade da Recuperação Pós-operatória no primeiro dia (D1) de pós-operatório.
Resultados
Antes da cirurgia (D0), os pacientes com má qualidade de recuperação apresentaram escores medianos na escala visual analógica semelhantes aos dos pacientes sem má qualidade de recuperação, mas apresentaram mais problemas nas dimensões mobilidade, atividades habituais, dor/desconforto e ansiedade/depressão. No terceiro mês após a cirurgia, os pacientes com má qualidade de recuperação apresentaram escores na escala visual analógica medianos no EuroQol semelhantes aos dos pacientes sem má qualidade de recuperação, mas apresentaram mais problemas na dimensão dor/desconforto. Os escores World Health Organization Disability Assessment Schedule 2.0 dos pacientes com má qualidade de recuperação foram significativamente maiores no início do estudo, embora os resultados tenham sido semelhantes no terceiro mês.
Conclusões
Os pacientes com má qualidade de recuperação apresentaram o pior estado de saúde no D0. A avaliação no terceiro mês indicou taxas semelhantes de problemas no EuroQol (exceto dor/desconforto) e escores semelhantes no World Health Organization Disability Assessment Schedule 2.0.
Palavras-chave: Recuperação pós-operatória, Má qualidade da recuperação, Estado de saúde, WHODAS, EQ-5D
Introduction
Postoperative recovery is a complex and multidimensional process that requires a holistic view of the resumption of capacities and homoeostasis after an event.1, 2 It is described as a multidimensional process of returning to normal, based on comparison with pre-illness standards in multiple domains, including physical, physiological, psychological, social, and economic aspects.3, 4, 5 For evaluating recovery, traditionally, major focus has been placed on physical signs, and the patients’ status is judged immediately after their arrival in the recovery room and every hour thereafter, until their discharge.6 Pain, nausea, emotional and psychological distress, and complications of surgery are the core indicators of poor recovery.2 Although these measures are of great interest to clinicians, they do not consider the patients’ notion of recovery, which includes not only the absence of symptoms, but also the return of their ability to perform activities to the same level as that before the surgery.4
Korttila7 described three fundamental overlapping phases of recovery: an early phase, defined as the period before discharge from the Post Anesthesia Care Unit (PACU) which is evaluated with the Postoperative Quality Recovery Scale (PQRS), which assesses physiologic and biologic outcomes;1, 4, 5, 7, 8 an intermediate phase comprising the period between admittance to the surgical ward and discharge from hospital, more effectively evaluated with instruments that consider symptoms as well as activities of daily living, such as the Quality of Recovery scale (QoR);1, 4, 5, 7, 8 and late phase, which extends after hospital discharge until the return to usual function and activities where functional status and health-related quality of life may be evaluated with quality of life scores and measurement of daily activities such as the 6 minute walk test, Community Health Activities Model Program for Seniors, Short Form Six Dimensions (SF-6D), or EuroQol Five Dimensions (EQ-5D).1, 4, 5, 7, 8
In this study, the PQRS, World Health Organization Disability Assessment Schedule (WHODAS), and EQ-5D were used to assess the participants’ quality of recovery and health status.
In a 2010 study, Royse et al.9 demonstrated that the PQRS can track recovery in multiple domains and over multiple time periods; moreover, the authors reported that it was a brief, feasible, and valid test for many types of surgery.9 The WHODAS has also proved an accurate and reliable measure of postoperative disability and is highly responsive to change, despite occurrence of an expected floor effect.10 The EQ-5D obtains evidence of inferior validity when used as a measure of postoperative recovery when compared to the SF-6D in the context of elective colorectal surgery, which may be due to its lower descriptive ability.11
Because incomplete postoperative recovery is predictive of long-term adverse outcomes, the early and accurate identification of these patients facilitates timely interventions to prevent such adverse outcomes.3 Therefore, the aim of this study was to assess and compare the quality of postoperative recovery and health status before and after surgery in patients proposed for elective surgery.
Materials and methods
The present study was conducted at Centro Hospitalar de São João (CHSJ), which is a tertiary, academic hospital situated in Porto, Portugal. It serves as a reference center for a vast area in the northern Portugal, and currently has 1105 beds distributed across several medical and surgical specialties.
Ethical approval for this study (Ethics Reference n° 209/2015) was provided by the Ethics Committee for Health of Centro Hospitalar de São João and the Faculty of Medicine, University of Porto, Porto, Portugal on July 21st, 2015.
After being approved by the institutional ethics committee, an observational, prospective study was conducted in the Post Anesthesia Care Unit (PACU), including patients proposed for elective surgery. Inclusion criteria were as follows: patients older than 18 years; those undergoing non-cardiac, non-obstetric, and non-neurological surgery; and those being admitted to the PACU between June and August of 2015. Exclusion criteria were as follows: patients’ refusal, inability to provide informed consent, and undergoing regional anesthesia. All participants provided written informed consent.
Patients were evaluated up to 14 days before surgery by the investigators, who collected perioperative data and applied the PQRS, EQ-5D, and WHODAS 2.0.
The Portuguese version of the PQRS was applied at baseline (up to 14 days before surgery) and 15 (T15) and 40 (T40) minutes and 1 (D1) and 3 (D3) days after surgery, with evaluation of general recovery in several domains. Recovery was defined as a return to baseline values or better for all questions within each domain; all domains were assessed both together and individually.9
Poor Quality of Recovery (PQR) was defined as recovery in fewer than two domains at postoperative D1 in the PQRS and was considered our primary outcome was PQR at D1 using the PQRS.
Preoperative health status was assessed using the EQ-5D and WHODAS 2.0 12 item version at baseline (up to 14 days before surgery, D0) and 3 months after surgery (M3).
EuroQoL 5D (EQ-5D) evaluating Health Related Quality of Life in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression12; According to EQ-5D, mobility, day-to-day activities, self-care problems, anxiety and pain were categorized independently for the presence of problems.
The World Health Organization Disability Assessment Schedule 2.0 (WHODAS) measures disability. The 12 item WHODAS was scored attributing numerical values to each item on a 5 point Likert scale: none = 0; mild = 1; moderate = 2; severe = 3; and extreme = 4. The total score (between 0 and 48) was then divided by 48 and multiplied by 100 to convert it to a percentage of the maximum disability score. We considered a score of greater than or equal to 25% to indicate disability.13
Statistical analysis
A required sample size of 161 participants with a confidence level of 95% and a confidence interval of 5% was calculated assuming a PQR rate of 12% in our study population. In the experimental time-frame, our sample size was expected to exceed this figure.
Descriptive analysis of variables was used to summarize the data. Ordinal and continuous data without normal distribution, based on the Kolmogorov-Smirnov test for normality of the underlying population, are presented as the median and interquartile range. The Mann–Whitney U-test, Chi-square, or Fisher's exact test were used for comparisons. Differences were considered statistically significant when p < 0.05. The data were analyzed using the Statistical Package for the Social Sciences version 19.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Of 206 patients observed, 182 were included and 24 patients were excluded from the study: eight could not perform the preoperative assessment, four were admitted to a surgical intensive care unit, four were unable to provide informed consent, and one refused to participate. In the remaining seven patients, postoperative evaluation could not be completed.
Table 1 shows the participants’ characteristics regarding the site of surgery.
Table 1.
Characterization of the surgery site.
| Surgery | Absolut frequency (n = 182) |
|---|---|
| Gynaecologic | 32 |
| Head and neck | 13 |
| Gastrointestinal | 82 |
| Urologic | 10 |
| Breast | 32 |
| Plastic and reconstructive | 13 |
At D1, six patients (3%) showed return to baseline values or better on the full PQRS, 26 patients (14%) showed return to baseline values or better in four domains, one-hundred one patients (55%) showed return to baseline values or better in three domains and on-hundred 58 (87%) showed return to baseline values or better in two domains; 24 patients (13%) recovered in fewer than two domains and were considered PQR patients.
Patients with PQR had a less frequently full recovery at any PQRS domain at D1 as compared to patients without PQR (Table 2).
Table 2.
The percentage of patients showing recovery by domains at day 1 in the Post-operative Quality Recovery Scale.
| Domain | PQR (n = 24) 13.2% |
Without PQR (n = 158) 86.8% |
p |
|---|---|---|---|
| Physiological | 5 (21) | 95 (60) | <0.001a |
| Cognitive | 0 (0) | 44 (28) | 0.001b |
| Emotive | 0 (0) | 90 (57) | <0.001b |
| Nociceptive | 15 (63) | 146 (92) | <0.001a |
| Activities of daily living | 1 (4) | 73 (46) | <0.001b |
PQR, poor quality of recovery.
Chi-square test.
Fisher's exact test
Table 3 lists patients’ characteristics regarding age, sex, American Society of Anesthesiologists14 physical status, Body Mass Index (BMI), duration of anesthesia, duration of PACU stay, and duration of hospital stay. The results of PQRS questionnaire at D1 revealed that 24 of 182 patients admitted to the PACU were considered to have PQR (13.2%). No differences were observed in the majority of the studied pre-admission patient characteristics, namely age, sex, ASA physical status, and BMI, between patients with and without PQR. There were no significant group-wise differences in duration of anesthesia or duration of PACU stay, however, duration of hospital stay was significantly higher in the PQR patients (6.5 days vs. 5 days, p = 0.049).
Table 3.
Pre-admission patients’ characteristics and outcomes.
| PQR (n = 24) 13.2% |
Without PQR (n = 158) 86.8% |
p | |
|---|---|---|---|
| Age (years) median (IQR) | 63 (47–70) | 56 (54–64) | 0.081b |
| Sex, n (%) | 0.399a | ||
| Female | 14 (58.3%) | 106 (67.1%) | |
| Male | 1 0 (41.7%) | 52 (32.9%) | |
| ASA, n (%) | 0.432a | ||
| I | 2 (8.3) | 19 (12.0) | |
| II | 15 (62.5) | 113 (71.5) | |
| III | 7 (29.2) | 25 (15.8) | |
| IV | – | 1 (0.6) | |
| BMI, median (IQR) | 25.8 (24.4–30.8) | 26.9 (23.5–30.5) | 0.736b |
| Duration of anesthesia (min), median (IQR) | 148.0 (120.0–193.0) | 144.5 (110.0–180.0) | 0.437b |
| Duration of PACU stay (min), median (IQR) | 127.5 (90.8–341.3) | 120.0 (92.3–158.5) | 0.607b |
| Duration of hospital stay (days), median (IQR) | 6.5 (3.0–14.0) | 5.0 (3.0–7.0) | 0.049b |
PQR, poor quality of recovery; ASA, American Society of Anesthesiologists; BMI, Body Mass Index; PACU, Post Anesthesia Care Unit; min, minutes.
Chi-square test.
Mann–Whitney U-test.
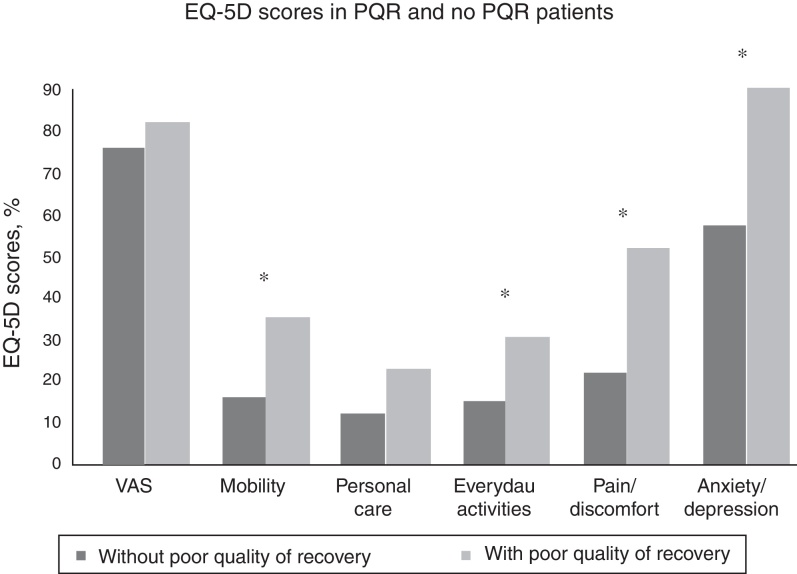
Fig. 1 displays the distribution of several endpoints from the EQ-5D scale between the patients with and without PQR at D0. At D0, patients with PQR had median Visual Analog Scale (VAS) scores for EQ-5D similar to those of patients without PQR (73 vs. 80, p = 0.314), but they had more problems in the mobility (33% vs. 14%, p = 0.017), usual activities (29% vs. 13%, p = 0.045), pain/discomfort (50% vs. 20%, p = 0.002), and anxiety/depression (88% vs. 55%, p = 0.002) domains.
Figure 1.
EQ-5D scores at baseline (D0) in patients with and without PQR; (PQR, poor quality of recovery; VAS, visual analogical scale; *p ≤ 0.05).
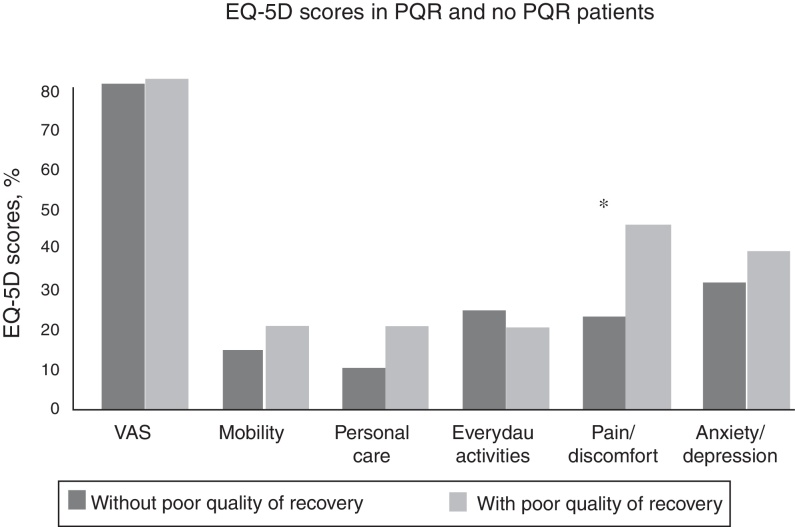
Fig. 2 presents the same endpoints as Fig. 1 measured at M3. At this point, the median VAS scores for EQ-5D were similar between patients with and without PQR (80 vs. 80, p = 0.945), but patients with PQR had more problems in the pain/discomfort domain (44% vs. 21%, p = 0.046).
Figure 2.
EQ-5D scores at 3 months (3M) in patients with and without PQR; (PQR, poor quality of recovery; VAS, visual analogical scale; *p ≤ 0.05).
According to the WHODAS results, 22 patients (12%) had disability at D0 and 13 patients (7%) had disability at M3. Patients with PQR scored significantly higher on the WHODAS at baseline (D0) (5.2 vs. 2.1, p = 0.015), indicating worse health status than that of patients without PQR (Table 4); and at M3, there were no differences between the groups (2.1 vs. 2.1, p = 0.964) (Table 5).
Table 4.
Preoperative health status assessed with WHODAS medium scores at baseline (up to 14 days before surgery) in patients with and without PQR.
| PQR (n = 24) | Without PQR (n = 158) | p | |
|---|---|---|---|
| WHODAS | 5.2 (4.2–13.0) | 2.1 (0–8.3) | 0.015a |
PQR, poor quality of recovery; WHODAS, World Health Organization Disability Assessment Schedule.
Mann–Whitney U-test.
Table 5.
Health status assessed with WHODAS medium scores at 3 months after surgery in patients with and without PQR.
| PQR (n = 16) | Without PQR (n = 124) | p | |
|---|---|---|---|
| WHODAS | 2.1 (0–4.2) | 2.1 (0–6.3) | 0.964a |
PQR, poor quality of recovery; WHODAS, World Health Organization Disability Assessment Schedule.
Mann–Whitney U-test.
Discussion
The major findings of this study were: 1) PQR was a frequent event; 2) Surgery had a great impact on quality of recovery in patients with PQR and such patients had lower rates of full recovery in all PQRS domains; 3) Patients with PQR had worse quality of life before surgery and 4) 3 months after surgery, the rates of problems in EQ-5D (except for pain/discomfort) and the WHODAS scores were similar.
To define PQR, we used a singular approach that involved recovery in PQRS domains at D1. In this study, the incidence of PQR in this study (13.2%) was in the range of values described in the current literature using other strategies.15, 16 Likewise, other studies have also reported higher PQR incidences, referring to populations selected using different methodologies, including post-cardiac17, 18 and post-neurological surgery patients.19 Recovery from anesthesia and surgery is sometimes complicated by residual sedation, pain, nausea, vomiting, and various other major and minor complaints, which can influence the occurrence of PQR.20
Complete recovery in all PQRS domains was significantly less frequent in patients with PQR, which was the expected result, since by definition PQR involved full recovery in only one or two dimensions. These results indicated that the recovery was not better in any of the considered dimensions of PQRS.
Although some studies have reported differences in the quality of recovery according to sex,21, 22, 23 our results were in agreement with reports suggesting that a patient's sex is not an independent influencing factor in the response to anesthesia and recovery after surgery.15, 16, 19, 24 To clarify this issue, Gornall et al.25 performed a systematic review in 2013, and reported that men had slightly higher QoR-40 scores than women, although the weighted mean differences were not constant across the studies. The discrepancies between studies were attributed to the effect of confounders because the comparison was made without adjusting for other factors that influence recovery, such as the patients’ age and extent of surgery, were not balanced when making this comparison25; on adjusting these confounding factors were balanced, a clear difference was observed between sexes, with poor overall quality of recovery in women.21
In addition to sex, age, ASA physical status, and BMI did not differ between patients with and without PQR. Some studies showed that age is not associated with quality of recovery15, 16; in contrast, other studies have reported a correlation between age and quality of recovery.23, 24
Some studies have reported that duration of surgery and/or duration of PACU stay are factors that affect PQR, although the relation of one or both varies greatly among studies.16, 19, 22, 24 Nevertheless, in the present study, a longer duration of anesthesia and/or a prolonged PACU stay were not positively correlated with a worse quality of recovery. This discrepancy may be have been due to differences in the definition of PQR, because of the lack of consensus on delineation of this variable.
A statistically significant correlation was observed between duration of hospital stay and quality of recovery, which is in agreement with the current reports that duration of hospital stay is an independent measure of quality of recovery; patients with PQR tended to have longer duration of hospital stay after surgery.14, 16, 19, 22, 23 In addition, duration of hospital stay is also often used as an indicator of discriminant construct validity for tests assessing quality of recovery.23 Collectively with these findings our results support the use of the PQRS as an accurate assessment tool to describe quality of recovery.
Both the EQ-5D and WHODAS are used to describe various health status parameters and are descriptors of health-related quality of life26, 27; therefore, in this study, we focused on combined health status and health-related quality of life. As a proof of concept, patients with PQR had a higher rate of health-related problems before surgery as measured using the EQ-5D, particularly in the domains of mobility, usual activities, pain/discomfort, and anxiety/depression; similarly, patients with worse health status, as indicated by higher WHODAS scores at baseline, tended to exhibit PQR more frequently than those with better health status. Therefore, a poor health status prior to surgery is associated with worse quality of recovery. These results can be explained in part by the fact that the same health conditions associated with higher EQ-5D and WHODAS scores also influence the patients’ ability to fully and quickly recover from surgery. This is consistent with the findings of Guimarães-Pereira et al.,15 that patients with poor quality of life before surgery exhibit PQR after surgery.
In general, 3 months after surgery, the rate of problems indicated by WHODAS and EQ-5D scores were similar in the PQR and non-PQR groups, which suggests that a worse quality of recovery does not rule out the outcome of better health-related quality of life at M3 and that recovery progresses through time. Nevertheless, these findings are contrary to those of Myles et al., who reported that poor-quality recovery can predict poor quality of life (measured using the 36 Item Short Form Health Survey) at M3 after cardiac surgery.18 Our findings contradict those of Guimarães-Pereira et al. in similar cohort, who, reported correlation between PQR and poor quality of life 3 months after surgery.15 Many factors may explain these apparent inconsistencies between studies: in the study of Myles et al., only cardiac surgery patients were considered under specific exclusion criteria, and other instruments were used to measure PQR and health status. Moreover, quality of recovery was evaluated 3 days after surgery, as opposed to D1 in our research. The study design adopted by Guimarães-Pereira et al. used a study design that was comparable to that of our study, with measurement of PQR measured in the first 24 h after surgery; however, they used QoR-40 as an assessment tool of recovery and health status, whereas, we used the PQRS for evaluating quality of recovery and the EQ-5D and WHODAS as measurement tools for health status. Notably, although quality of life is directly related to health-related quality of life, the two terms are not entirely overlapping because in general, quality of life generally comprises additional domains; hence comparative results between studies measuring these outcomes must be carefully interpreted.
At M3, the EQ-5D values for pain/discomfort differed between groups, with PQR patients being more prone to adverse outcomes. This highlights the importance of adequate pain control to ensure better recovery. As supported by previous studies,15 our results indicated that patients with high risk for developing PQR can be identified prior to surgery through application of health-related quality of life measurement tools. The finding that patients with PQR had lower quality of life prior to surgery may facilitate earlier and more effective interventions to improve quality of recovery after surgery. Consequently, the application of health status scales before surgery could be important to optimum postoperative care of the patient.
Limitations of the study
This study has several limitations to this study. First, it was an observational study and the number of patients may be considered low due to high rate of dropout and losses caused by lack of information. Second, due to calculation of sample size in advance, our analyses may lack sufficient power to identify differences, especially for patients’ health status at the 3 months evaluation time-point. To prevent type II error, we estimated PQR rate of 12% at D1. To the best of our knowledge, this is the first study using PQRS to evaluate the incidence rate of PQR. In a study of patients undergoing cardiac surgery with high probability of PQR, Myles et al.17 showed a 20% rate of PQR at postoperative day 3 using another definition for PQR. To prevent type II error, we included a higher number of patients than the calculated value for the initial follow-up; however, the number of patients at 3 month follow-up was reduced; hence, the presence of type II error is possible.
Third, we did not study clinical variables, including comorbidities and medications that may have affected the results and patients’ quality of recovery and quality of life. Moreover, numerous definitions of PQR exist and the tools and timing of assessment greatly vary among studies. Thus, the different definitions of PQR may explain the differences between results of our study and those of previous studies.
Conclusions
Patients with PQR had the worst health status at D0 based on the rate of problems in the EQ-5D and WHODAS scores; whereas at M3 revealed that rates of problems in the EQ-5D (except for pain/discomfort) and WHODAS scores were similar.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Allvin R., Berg K., Idvall E., et al. Postoperative recovery: a concept analysis. J Adv Nurs. 2007;57:552–558. doi: 10.1111/j.1365-2648.2006.04156.x. [DOI] [PubMed] [Google Scholar]
- 2.Bowyer A., Jakobsson J., Ljungqvist O., et al. A review of the scope and measurement of postoperative quality of recovery. Anaesthesia. 2014;69:1266–1278. doi: 10.1111/anae.12730. [DOI] [PubMed] [Google Scholar]
- 3.Bowyer A., Royse C. The importance of postoperative quality of recovery: influences, assessment, and clinical and prognostic implications. Can J Anaesth. 2016;63:176–183. doi: 10.1007/s12630-015-0508-7. [DOI] [PubMed] [Google Scholar]
- 4.Lee L., Tran T., Mayo N.E., et al. What does it really mean to “recover” from an operation? Surgery. 2014;155:211–216. doi: 10.1016/j.surg.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Neville A., Lee L., Antonescu I., et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg. 2014;101:159–170. doi: 10.1002/bjs.9324. [DOI] [PubMed] [Google Scholar]
- 6.Aldrete J.A., Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–934. [PubMed] [Google Scholar]
- 7.Korttila K. Recovery from outpatient anaesthesia Factors affecting outcome. Anaesthesia. 1995;50(Suppl.):22–28. doi: 10.1111/j.1365-2044.1995.tb06186.x. [DOI] [PubMed] [Google Scholar]
- 8.Bowyer A.J., Royse C.F. Postoperative recovery and outcomes – what are we measuring and for whom? Anaesthesia. 2016;71(Suppl 1):72–77. doi: 10.1111/anae.13312. [DOI] [PubMed] [Google Scholar]
- 9.Royse C.F., Newman S., Chung F., et al. Development and feasibility of a scale to assess postoperative recovery: the post-operative quality recovery scale. Anesthesiology. 2010;113:892–905. doi: 10.1097/ALN.0b013e3181d960a9. [DOI] [PubMed] [Google Scholar]
- 10.Shulman M.A., Myles P.S., Chan M.T., et al. Measurement of disability-free survival after surgery. Anesthesiology. 2015;122:524–536. doi: 10.1097/ALN.0000000000000586. [DOI] [PubMed] [Google Scholar]
- 11.Lee L., Mata J., Augustin B.R., et al. A comparison of the validity of two indirect utility instruments as measures of postoperative recovery. J Surg Res. 2014;190:79–86. doi: 10.1016/j.jss.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 12.van Agt H.M., Essink-Bot M.L., Krabbe P.F., et al. Test-retest reliability of health state valuations collected with the EuroQol questionnaire. Soc Sci Med. 1994;39:1537–1544. doi: 10.1016/0277-9536(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 13.Ustün T.B., Chatterji S., Kostanjsek N., et al. WHO/NIH Joint Project Developing the World Health Organization Disability Assessment Schedule 2.0. Bull World Health Organ. 2010;88:815–823. doi: 10.2471/BLT.09.067231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanaka Y., Wakita T., Fukuhara S., et al. Validation of the Japanese version of the quality of recovery score QoR-40. J Anesth. 2011;25:509–515. doi: 10.1007/s00540-011-1151-2. [DOI] [PubMed] [Google Scholar]
- 15.Guimarães-Pereira L., Costa M., Sousa G., et al. Quality of recovery after anaesthesia measured with QoR-40: a prospective observational study. Braz J Anesthesiol. 2016;66:369–375. doi: 10.1016/j.bjane.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Sá A.C., Sousa G., Santos A., et al. Quality of recovery after anesthesia: validation of the portuguese version of the ‘Quality of Recovery 15’ questionnaire. Acta Med Port. 2015;28:567–574. doi: 10.20344/amp.6129. [DOI] [PubMed] [Google Scholar]
- 17.Myles P.S., Viira D., Hunt J.O. Quality of life at three years after cardiac surgery: relationship with preoperative status and quality of recovery. Anaesth Intensive Care. 2006;34:176–183. doi: 10.1177/0310057X0603400220. [DOI] [PubMed] [Google Scholar]
- 18.Myles P.S., Hunt J.O., Fletcher H., et al. Relation between quality of recovery in hospital and quality of life at 3 months after cardiac surgery. Anesthesiology. 2001;95:862–867. doi: 10.1097/00000542-200110000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Leslie K., Troedel S., Irwin K., et al. Quality of recovery from anesthesia in neurosurgical patients. Anesthesiology. 2003;99:1158–1165. doi: 10.1097/00000542-200311000-00024. [DOI] [PubMed] [Google Scholar]
- 20.Myles P.S., Williams D.L., Hendrata M., et al. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84:6–10. doi: 10.1093/oxfordjournals.bja.a013383. [DOI] [PubMed] [Google Scholar]
- 21.Buchanan F.F., Myles P.S., Cicuttini F. Effect of patient sex on general anaesthesia and recovery. Br J Anaesth. 2011;106:832–839. doi: 10.1093/bja/aer094. [DOI] [PubMed] [Google Scholar]
- 22.Stark P.A., Myles P.S., Burke J.A. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology. 2013;118:1332–1340. doi: 10.1097/ALN.0b013e318289b84b. [DOI] [PubMed] [Google Scholar]
- 23.Myles P.S., Hunt J.O., Nightingale C.E., et al. Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesth Analg. 1999;88:83–90. doi: 10.1097/00000539-199901000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Stessel B., Fiddelers A.A., Joosten E.A., et al. Prevalence and predictors of quality of recovery at home after day surgery. Medicine (Baltimore) 2015;94:e1553. doi: 10.1097/MD.0000000000001553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gornall B.F., Myles P.S., Smith C.L., et al. Measurement of quality of recovery using the QoR-40: a quantitative systematic review. Br J Anaesth. 2013;111:161–169. doi: 10.1093/bja/aet014. [DOI] [PubMed] [Google Scholar]
- 26.Payakachat N., Ali M.M., Tilford J.M. Can The EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics. 2015;33:1137–1154. doi: 10.1007/s40273-015-0295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cieza A., Stucki G. Content comparison of health-related quality of life (HRQOL) instruments based on the international classification of functioning, disability and health (ICF) Qual Life Res. 2005;14:1225–1237. doi: 10.1007/s11136-004-4773-0. [DOI] [PubMed] [Google Scholar]