Abstract
Background: The Universal Health Coverage (UHC) is a very important and effective policy in the health system of countries worldwide. Using the experiences and learning from the best practices of successful countries in the UHC can be very helpful. Therefore, the aim of the present study is to provide a scoping review of successful global interventions and practices in achieving UHC.
Methods: This is a scoping review study that has been conducted using the Arkesy and O'Malley framework. To gather information, Embase, PubMed, The Cochrane Library, Scopus, Scientific Information Database, and MagIran were searched using relevant keywords from 2000 to 2019. Studies about different reforms in health systems and case studies, which have examined successful interventions and reforms on the path to UHC, were included. Articles and abstracts presented at conferences and congresses were excluded. Framework Analysis was also used to analyze the data.
Results: Out of 4257 articles, 57 finally included in the study. The results showed that of the 40 countries that had successful interventions, most were Asian. The interventions were financial protection (40 interventions that were categorized into 14 items), service coverage (31 interventions categorized into 7 items), population coverage (36 interventions categorized into 9 items), and quality (18 interventions categorized into 7 items), respectively. Also, the positive results of interventions on the way to achieving UHC were financial protection (14 interventions), service coverage (7 interventions), population coverage (9 interventions), and quality (7 interventions), respectively.
Conclusion: This study provides a comprehensive and clear view of successful interventions in achieving the UHC. Therefore, with consideration to lessons learned from successful interventions, policymakers can design appropriate interventions for their country.
Keywords: Universal Health Coverage, Health Care Reform, Financing, Services Coverage, Quality, Scoping Review
What is “already known” in this topic
The UHC approach has been highly considered by countries in the last two decades, and these countries have taken many steps with success or failure in the road of achieving UHC. Accordingly, reviewing and learning from the successful interventions of other countries and learning from these experiences in the field of UHC can be very useful.
What this article adds
This study provides the comprehensive and clear view of successful interventions performed in most countries at different income levels, which seek to achieve the UHC. Reporting these successful interventions can be a model and guide for other countries to avoid the costs and recurring mistakes.
Introduction
The UHC has been introduced by the World Health Organization (WHO) as a viable approach and a way for countries to access equitable health services and ultimately a healthy community (1, 2). The UHC can be accepted as a very important and effective policy in the health system of countries, which can improve the quality of people's lives to an acceptable level by providing equitable quality health services to all people everywhere without any financial pressure (3-11). Thus, achieving UHC can have a significant impact on health promotion, easier access to health care for those in need, and improved public health, especially for the poor (12, 13).
Given the importance of achieving UHC for high- and middle-income countries, the number of countries trying to achieve this has increased in the last 2 decades (14, 15). In addition, nowadays, countries by increasing their knowledge and awareness of strategies and applying the experiences of successful countries as well as acquiring the necessary capabilities to meet their urgent needs, are trying to take the path of achieving UHC (16-18). Like other high-income countries that have achieved UHC, low- and middle-income countries, with taking into account the structure and resources that they have on the path to UHC undertake measures, such as mobilizing resources, fulfilling the political commitments necessary to implement health-related policies, and implementing effective reforms and interventions in macronational policies (1, 19-21). The UHC can be one of the most challenging political processes that require the support of various stakeholders, including health system policymakers (4). Although all countries pursue the same goal of achieving UHC, the path and duration of achieving this goal depend on the structure and resources of the countries as well as the specific effective factors of each country (4).
Given the specific circumstances of each country, there is no uniform way of achieving UHC, and countries act based on their structural strengths and weaknesses. (4, 22-24). To achieve UHC, countries need to identify their strategic issue. For example, in the field of stewardship, financing, resources generation, and service provision, each country based on its health system needs, identifies effective factors, such as prioritizing health system reforms according to its own factors, such as prioritizing health system reforms (25), considering organizational structure and its capacity (26-28), having national and political commitment (29-32), economic growth (33-35), financial protection (36-39), health insurance coverage (15, 34, 40), prevention of catastrophic costs (41, 42), reduction of out-of-pocket payments (41, 43-49), health insurance prepayment (40, 50-53), national policies for human resources training (25-27) and geographical distribution of services (54-57), and given its weaknesses or strengths in these functions, to reform and strengthen its health system on the path to UHC.
On the path to UHC, it is crucial to consider the functions of the health system and reform these functions based on the specific circumstances of the countries. In this regard, using the experiences of other countries and learning from the best practices in successful countries in the field of UHC can be highly useful. The definition of the best practices in this study is to paying attention to the experiences and successful interventions of countries’ health systems in the achievement of UHC.Therefore, the purpose of the present study was to review the successful global interventions and practices to achieve UHC in the form of a scoping review.
- Identify successful financial protection interventions, reforms, and practices in achieving UHC
- Identify interventions, improvements, and successful service coverage practices in achieving UHC
- Identify successful population coverage interventions, reforms, and practices in achieving UHC
- Identify successful interventions, reforms, and practices in the quality of health services in achieving UHC
Methods
This was is a scoping review study conducted in 2019 based on the book "A Systematic Review to Support Evidence-Based Medicine" (58).
Information Sources
Required information was searched in the Embase, PubMed, the Cochrane Library, Scopus, Scientific Information Database, and MagIran from January 2000 until the end of January 2019. The keywords of Universal health coverage, Universal health care coverage, Universal health care coverage, Universal coverage, UHC, Strength,* Transform,* interventions, improve,* program,* innovations, initiative, Financing, "Service delivery", Stewardship, and "Resource generation" were used in the search. Some specialized journals, Google Scholar, and the references of included articles were reviewed manually. The databases of the European Association for Gray Literature Exploitation and the Health Care Management Information Consortium as well as the WHO and World Bank sites were also searched (Table 1).
Table 1. Complete Search Strategy for PubMed Databases.
| Set | Strategy | Results |
|---|---|---|
| #1 | (((("universal health care coverage") OR "universal healthcare coverage"[Title/Abstract]) OR "universal health coverage"[Title/Abstract]) OR "universal coverage"[Title/Abstract]) OR "UHC"[Title/Abstract] Filters: Publication date from 2000/01/01 to 2019/1/31; English | 3735 |
| #2 | (Strength [TIAB] OR Strengthes [ TIAB] OR Transfor [TIAB] OR Transfores [TIAB] OR intervention [TIAB] OR interventions [TIAB] OR improve [TIAB] OR improvement [TIAB] OR programm [TIAB] OR programmes [TIAB] OR initiative [TIAB] OR initiatives [TIAB] OR innovation [TIAB] OR innovations [TIAB] OR Financing [TIAB] OR Financings [TIAB] OR "Service delivery" [TIAB] OR Stewardship [TIAB] OR "Resource generation" [TIAB]) Filters: Publication date from 2000/01/01 to 2019/1/31; English | 1958401 |
| #3 | #1 AND #2 | 1666* |
| * Filters activated: Publication date from 2000/01/01 to 2019/1/31, English. | ||
Eligibility Criteria
Inclusion criteria: All observational (descriptive studies about different reforms in health systems) and intervention studies, especially case studies, which have examined successful interventions and reforms of countries on the path to UHC and published between 2000 and 2019, were included in the study.
Exclusion Criteria: Articles and abstracts presented at conferences and congresses as well as studies that did not report successful interventions were excluded.
Review Process:
In this study, the Arkesy and O'Malley frameworks for scoping review were used. This framework is the first methodological framework for conducting scoping review research published in 2005 (59). The framework consists of 6 steps: (1) identification of the research question; (2) identification of relevant studies, (3) study selection; (4) Data charting; (5) data analysis and reporting the results; and (6) consultation exercise. The study also used the (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) PRISMA framework to report the results (60, 61).
The study process was such that initially the titles of all articles were reviewed and articles that were incompatible with the aims of the study were excluded. Subsequently, abstracts and full-texts of the articles were studied, respectively, and studies that did not meet the inclusion criteria and had poor correlation with study aims were identified and excluded. Data were extracted according to a researcher-made data extraction form, and entered into the designed table. At first, as a pilot for data extraction form, the data of 5 papers were extracted and the deficiencies of the original form were eliminated. The whole process of systematic review was performed by 2 researchers independently and disputes were referred to a third researcher.
Given that it was necessary to study the full-text of the included studies to extract data, this was done by the research team in 2 stages. However, in the third and fourth stages of the Arkesy and O'Malley frameworks, after the initial extraction of the data from the selected studies, the research team reexamined the data in 2 sessions carefully and, finally, the studies were rescreened by the research team to include precisely relevant and high-quality studies. Endnote X9 software was also used to organize study titles and abstracts as well as identify duplicates.
Data Analysis
The framework analysis was used to analyze the data, which is a hierarchical approach used to classify and organize data based on key themes, concepts, and emerging classes. Data were extracted by 2 researchers and entered in to data extraction table. The steps for analyzing and coding the data were (1) familiarity with the text of articles (immersion in article results); (2) identifying and extracting primary themes (identifying and extracting more articles relevant to primary themes); (3) placing articles in determined themes, (4) reviewing and completing the results of each theme with the use of results of the articles and ensuring the reliability of the themes and the results extracted in each theme (in cases of disagreement between the 2 coders, the dispute was referred to the third researcher). Textual data were analyzed manually and categorized into dimensions of UHC (financial protection, population coverage, service coverage, and quality) using the framework analysis method (62, 63). In case of disagreement between researchers, the study was reviewed by a third person who was an expert, and with the authors' consensus, the proper function was selected.
Results
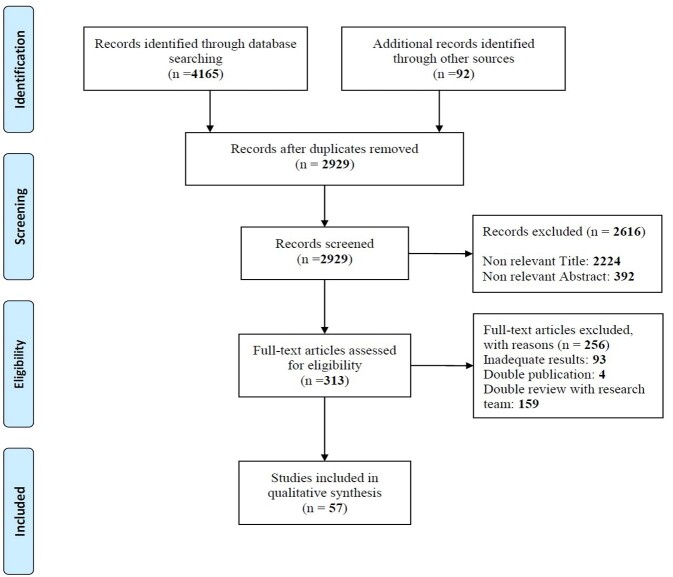
Of the 4257 articles found, 1328 were excluded as duplicate papers and 2616 were excluded in title and abstract reviews. Also, of the 313 articles entered the full-text review phase, 256 were excluded because of lack of appropriate information and lack of reporting of the required information as well as rescreening of the full-text. Finally, 57 articles were included in the study (Fig. 1).
Fig. 1.
Flow diagram of the searches and Inclusion process.
The results of included studies are summarized in supplementary file1 (Appendix 1).
Country of Study
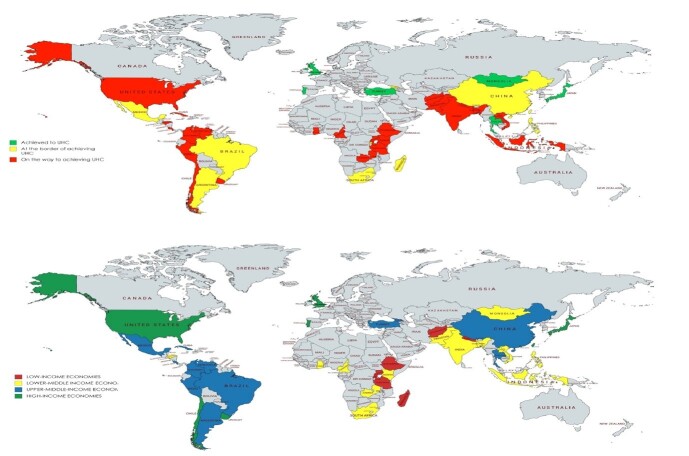
Studies published on successful interventions to achieve UHC were conducted in 40 countries. Most studies were in Asia, with 14 countries, and the least in European countries with 4 studies. Most studies were conducted in Thailand (6 studies), China (6 studies), Mexico (6 studies), and Brazil (6 studies). Among these countries, 5 achieved to UHC, 11 were at the border of achieving, and others were on the path to UHC. Also, according to the latest World Bank classification in 2019-2020 (64), 9 studies were conducted in low-income countries (LICs), 13 in lower-middle income countries (LMIC), 18 in upper-middle income countries (UMIC) and 9 studies in High-Income Countries (HIC), and 8 in more than 1 country (Fig. 2).
Fig. 2.
Countries’ successful interventions on the path to UHC with different condition and suc-cessful interventions in achieving UHC in countries based on the World Bank’s latest classification.
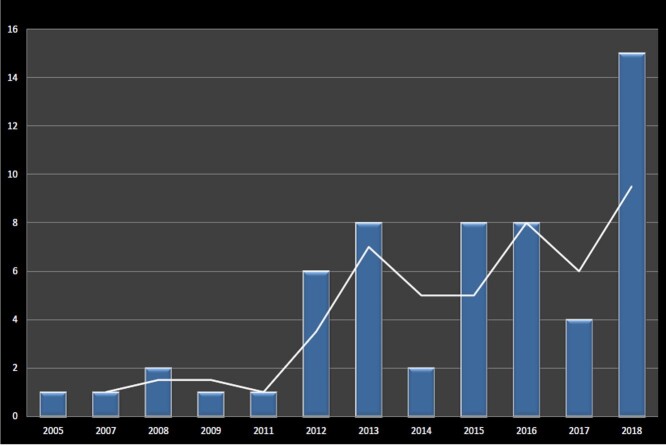
Trend of Publications Year
The time trend of the studies’ publication shows that most of the studies, except for 2, were published after the announcement of UHC as a global, international health policy for all countries by the WHO in 2008, and most of studies (n = 15 studies) were published in 2018 (Fig. 3).
Fig. 3.
The time trend of interventional studies' publication on the path to UHC
Interventions According to the Dimensions of UHC
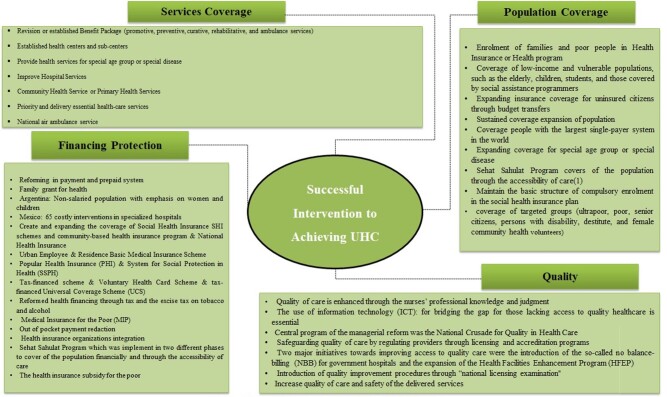
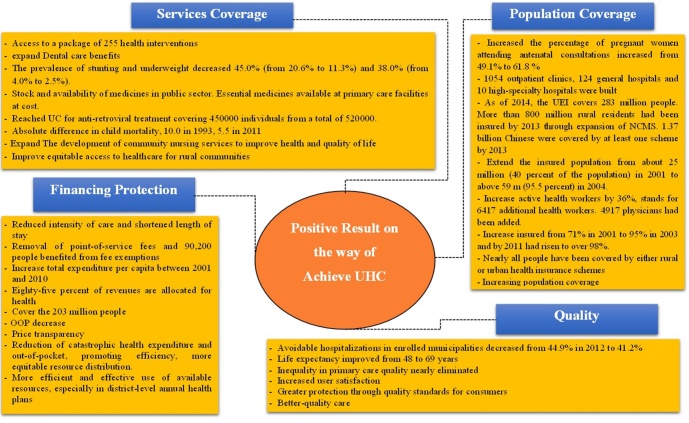
According to the type of interventions in each of the UHC dimension, interventions were categorized into different parts as follows: financial protection (40 interventions categorized into 14 items), service coverage (31 interventions categorized into 7 items), population coverage (36 interventions categorized into 9 items), and quality (18 interventions categorized into 7 items). The most and the least interventions were financial protection and quality, respectively (Fig. 4).
Fig. 4.
Successful interventions in achieving UHC in countries
Successful Results of Interventions
According to the type of successful results gained from interventions in countries in each of the UHC dimension, results were categorized into different items as follows: financial protection (n = 14 items), service coverage (n = 7 items), population coverage (n = 9 items), and quality (n = 7 items) (Fig. 5).
Fig. 5.
Achieving positive results on the way to achieving UHC
Discussion
Out of 4257 articles found, finally 57 were included in the study. These articles examined successful interventions in 40 countries on the path to UHC. Most studies were conducted in Asia and the least in Europe.
Results were categorized into different items: financial protection (n = 14 items), service coverage (n = 7 items), population coverage (n = 9 items), and quality (n = 7 items). Most of the interventions were done in LMICs. The results show that most of the interventions in the field of service coverage are targeted specific groups, such as children, adolescents, women, and as specific patients.
The results of the reviewing the time trend of study publication revealed that most studies (except for 2) were published after announcing the UHC as a national and international policy for countries by the WHO in 2008 (3, 65). Also, the time trend of articles publication indicates the importance and great attention of countries to international health-related policies. Considering the many efforts being made in this area, again the high importance of this issue and its repeated mention by the WHO and the commitment of countries to achieve UHC by 2030, demonstrates the feasibility of conducting interventional studies and publication of very important and modeling articles for other countries. Therefore, published articles in this field need to address the performed intervention in more detail so that other countries do not make repeated and costly mistakes when using model countries' experiences (3, 6, 66, 67).
Most of the interventions were done in LMICs and UMICs. Few studies were conducted in high or LICs. One of the possible reasons could be that the HICs are fully achieved UHC and need for no major interventions. In LICs, also, the low interventions could be due to their low income and their inability to finance the structural and basic interventions and to develop major infrastructure. However, evidence suggests that LICs have also taken substantial measures and successful interventions to achieve UHC, given the importance of health and its impact on their economies and sustainable development. However, valuable interventions in countries, such as Nepal (68, 69), Uganda (70, 71), Rwanda (72), Tanzania (56, 73), Ethiopia (74), Afghanistan (75), and Madagascar, (76) have been conducted and positive results have been reported. In addition to published studies in this area, it should be noted that many successful interventions may have taken place before the announcement of this global policy in 2008, which has not been published with the aim of UHC, and these studies are likely to be lost.
Each country, taking into account its own needs and specific circumstances, undertakes specific interventions to achieve UHC. Considering the economic conditions of countries, the results of the present study show that most of the interventions have been performed in the field of financing or financial protection functions. Thus, most interventions in these countries have focused on the insurance system and targeted the poor people or specific groups of society (69, 72, 77-81).
Also, one of the issues that mostly reformed by countries is the payment and premium systems (76, 82-84). Similarly, a study by Elio Borgonovi and Emilia Compagni (2013) indicates that social, economic, and political sustainability are key drivers of health interventions and reforms in achieving UHC (85). Also, in many studies, social health insurance (SHI) (86), premium (50, 51, 87), cost containment (88), national health insurance system (89-91), tax revenue (92, 93), risk-pooling mechanisms (4, 92) and strategic purchasing (94) are crucial factors in the financial protection function of achieving UHC, such that positive reform interventions in these areas can draw countries one step closer to achieving their original goal.
That is why financing function or the financial protec tion dimension and interventions in them can be considered as an essential component of achieving UHC. The results of the study showed that successful interventions in the countries under study have positive results such as reduction in the intensity of care and a decrease in length of hospital stay (82, 95), elimination of costs of services that cause overuse of health services (76), allocating a large percentage of income to health (79), reducing out-of-pocket payments (96), and so on.
The results show that most of the interventions in the field of service coverage are targeted specific groups, such as children, adolescents, women, and specific patients, which could be due to the high vulnerability of women and children under 5 years old and the financial inability of these groups in LMICs. Also, designing dedicated and fully customized service packages can be much more efficient and effective than comprehensive service packages designed for the population of a country without considering the specific needs of different groups. With regard to specific diseases, special conditions, such as chronicity, being erodible, and cost consuming, can lead to catastrophic expenditure; for this reason, people with specific illnesses are covered by free services. Interventions in service coverage show that most interventions are in areas such as modifying or creating service packages based on people's needs at all levels of service provision or for different age groups and specific diseases, and also implementing fundamental interventions in primary health care or community-based health care. Interventions in this area have been in line with the findings of studies that have identified service packages as a major and very effective factor in achieving UHC (15, 88, 97-100).
The study showed that most of the interventions in the field of population coverage were related to the coverage expansion in specific groups or diseases (69, 73, 76, 79, 80, 101-106). Countries are also trying to cover poor households and individuals by implementing mandatory or voluntary insurance programs to cover more population (15, 79, 81, 107, 108). Thailand, for example, with the aim of covering its population considering socioeconomic conditions, by implementing a 30 Bahat health plan, could increase its insured population from 40% to 95% within 4 years, which is also considered one of the most successful interventions in this field (109). China has also been able to cover its entire population by implementing urban and rural health insurance plans (77, 78).
Studying the results of interventions in different countries showed that most of the interventions targeted financial protection and most of the published results also were in this area. This could be due to the importance of financing and reimbursement in the health system and financial protection of citizens against illness, as interventions in this area can reflect an early impact and can be better monitored and evaluated. However, results from the quality dimension are less reported. One of the reasons may be that interventions in this field are new and, on the other hand, the long-term impact of quality improvement interventions can be effective in publishing less studies in this area. Delays in the considering of the quality of health services by the WHO as the fourth dimension could also be another reason for the low publication of quality interventions and their effects on UHC.
The results of the present study show that quality interventions with 18 cases had the least report. However, studies on UHC have identified the quality of care and regulatory mechanisms for quality as one of the most influential factors in achieving UHC (36, 55, 110-112). One of the reasons for low interventions in this dimension could be the overemphasis of countries on the quantity of services provided and coverage of the majority of the population. It can also be attributed to the late introduction of this dimension and its recognition as the hidden dimension of UHC. While implementing programs related to other dimensions of public health coverage, countries need to take into account the quality and its monitoring, so that the interventions can be more efficient and effective. However, given the importance of quality in health, countries have taken important interventions, such as training and using experienced nurses (103), using information technology to reduce medical errors and filling the gap in access to health services (113), maintaining quality of service by licensing qualified individuals and hospitals accreditation (16, 114), and improving patient safety (34). However, the results of interventions in the quality dimension indicate maintaining and enhancing the quality of health care for service receivers through the implementation of quality standards and increasing users' satisfaction with services and eliminating the inequality in accessing quality health services in some countries (84, 115, 116).
One of the limitations of this study was the use of only English and Farsi languages to search and collect studies and documentation based on the authors' familiarity with these 2 languages. However, reports and documentation of successful interventions in countries may have been published and documented in other languages than have not been reviewed in this study. It should be noted that the present study examined only successful interventions that had good and significant results for countries. The reader should note that also some countries on the path to achieving UHC have had unsuccessful and costly interventions that can be used as a model to learn from failures and that only focusing on successful patterns cannot be effective.
Conclusion
Despite the issues raised in achieving UHC and necessity of interventions in the dimensions of UHC, and in light of the results, it should be made clear that in addition to providing the countries with the appropriate technical conditions on this path, the financial resources and political commitment of officials in all disciplines are essential, as the continuity and sustainability of this policy will achieve UHC. The results show that each country, depending on their particular economic, social and political circumstances have selected appropriate intervention mechanisms and tools for achieving UHC and have intervened. Each country has also been able to achieve significant progress in this area by identifying its weaknesses and prioritizing the most important ones for intervention, have achieved remarkable success in this regard, and have taken a step forward. Therefore, lessons learned from successful interventions in these countries can be highly efficient and effective through localizing and combining with target country' features.
Implications for Research and Policy
The present study provides a comprehensive and clear view of successful interventions performed in most countries at different income levels that seek to achieve UHC, and summarizing and reporting these successful interventions can be a model and guide for other countries to avoid the costs and mistakes. The results showed that countries have paid little attention to the quality of services. Therefore, more attention is needed to design and implement comprehensive interventions and policies to improve the quality of services in achieving UHC. Valid interventions with strong methodology and the use of control groups are recommended for future studies. Specific methodological evaluation of interventions is also recommended for future studies.
Conflict of Interests
The authors declare that they have no competing interests.
Acknowledgment
We are grateful to the experts for their contribution, time, and invaluable comments. Also, we are very grateful to Iran University of Medical Sciences for providing financing support.
Appendix 1.
Characterized of studies included and summarized in the study.
| Author & Year | Country | Dimensions | Health System Function | Innovations / Intervention | Result |
|---|---|---|---|---|---|
| Chan, W. Y, et al, 2017 (1) | China & Hong Kong |
Services Coverage
Population Coverage Quality |
Stewardship
Services Delivery |
- The Central government of China established CHS centers and subcenters in place in every neighborhood within a 15-minute walking distance to ensure close-to-home primary care.
- Community Nursing Services CHN is improving health care accessibility in China; and the scope of CHN service places much focus on promoting public health - The government provides financial support on the basic public health (BPH) service package, which is determined by the number of citizens using CHN centers’ services. The BPH services are broad and comprehensive, including (a) to establish health profiles and medical records; (b) to provide health education; (c) disease prevention and vaccination; (d) to provide health management for the elderly, pregnant women, children and citizens with hypertension, diabetes or serious mental illness; (e) to control infectious diseases and public health emergencies and (f) to monitor public health. |
- Quality of care is also enhanced because the nurses’ professional knowledge and judgment ensure that the patients are properly assessed, served, and most importantly, referred to the other health care professionals for appropriate care.
- Community-based nursing services present a great opportunity for nurses to enhance their contributions to Universal Health Coverage. - The development of community nursing services has expanded the scope of nursing services to those in need of, not just hospital-level nursing care, but more holistic care to improve health and quality of life. |
| Cheng, S. H. et al, 2012 (2) | Taiwan | Financial Protection | Financing |
- Review of impacts of implementation diagnosis-related group (DRG) payments on health care provider's behavior under a universal coverage system in Taiwan.
- Reforming of payment system |
-The DRG-based payment resulted in reduced intensity of care and shortened length of stay. |
| de Andrade, L. O. et al, 2015 (3) |
Brazil
Chile Colombia Cuba |
Financial Protection
Population Coverage Quality |
Stewardship
Financing Services Delivery |
- Brazil: The conditional cash transfer (family grant) was established in 2003 to ensure access to social rights for health care to provider social rights for health care.
- The program unified several existing programs (School Grant, Food Grant, Food Card, and Gas Grant) and in 2011 became part of the broader government strategy Plan (Plan Brazil without Misery) to raise population income and welfare. The Plan Brazil without Misery targets Brazilian households with per person incomes of less than R$70 (about US$30). The program has three axes: productive, second; access to public services and third, income transfers. - Chile: (Chile Grows with You) is a system of protection for early childhood development, with a mission to monitor, protect, and uphold the rights of all children and their families by providing programs and services, which enable special support for the poorest households that account for most vulnerable families. - Colombia: (From birth to Forever) is the National Strategy for Comprehensive Care in Early Childhood in Colombia. The strategy aims to unify the efforts of the public and private sectors, civil society organizations, and international cooperation to improve the experience and outcomes of early childhood in Colombia. The strategy a community nursery program that provided nutrition and child care for children from poor households. The strategy focuses on strengthening primary health care, including through participatory and social mobilization approaches, with the local authorities playing an important part in supporting progress towards universal health coverage and wider sustainable development objectives. - Cuba: Cuba’s Dengue Prevention Program and Eradication is a comprehensive set of intersectoral interventions aimed at elimination and control of Aedes aegypti mosquito through environmental sanitation, hygiene, and collective household actions. Underpinned by legislation, the program includes the local government, the Ministry of Public Health, community associations, family doctors, water resources management, the antimosquito brigade, and several civil society organizations. - The Dengue Prevention Programme’s grounding at the primary healthcare level, with implementation leadership provided by provincial and municipal governments and participatory approaches to create local level needs assessment and action plans, offers important lessons for intersectoral action for universal health coverage, and sustainable development. |
- Brazil: The Bolsa Família program (family grant) in Brazil is widely regarded as a success. It has lifted millions of people out of poverty, supported people with the greatest unmet need to access health services and has contributed to progressive realization of universal health coverage.
- Between 2002 and 2011, the percentage of pregnant women (in the target population) attending seven or more antenatal consultations increased from49.1% to 61.8%. Inter sectoral action through Bolsa Família has also contributed to improvements in health and action on social determinants. Integration of health and education policies in Bolsa Família expanded access for the poorest groups in Brazil and in 2003–13, contributed to substantial increases in immunization and reduced child mal nutrition, and in 2004–09 to reductions in under-5 mortalities. - Chile: The evidence so far suggests positive effects in reducing child poverty and increasing access to educational opportunities and health. - Colombia: the strategy is a platform to enhance coverage and quality of health care. - Cuba: The program has led to a reduction of dengue infections and improved environmental management for vector control. |
| Edward, A. et al, 2015 (4) | Afghanistan |
Services Coverage
Population Coverage |
Stewardship
Resources Generation Services Delivery |
- Innovative strategies of paired male and female Community Health Workforce CHWs, institution of a special cadre of community health supervisors, and community health councils were introduced as systems strengthening mechanisms.
- CHW: The deployment of volunteer CHWs by the Ministry of Public Health implemented in 2003, to improve equitable access to healthcare for rural communities. One male and one female CHW were selected and trained for each village health post, serving up to 150 households. The CHW job description included treatment of childhood diseases, provision of contraceptives, health promotion, and demand-creation for preventive and maternal health services at the supporting health facility. |
- Formative assessments evidenced that CHWs were highly valued as they provided equitable, accessible and affordable 24h care.
- Improve equitable access to healthcare for rural communities |
| Frenk, J and Gomez-Dantes, O. 2018 (5) | Latin America |
Services Coverage
Population Coverage Financial Protection |
Stewardship
Services Delivery Financing |
- Argentina: Plan name: Plan Nacer -2003 -Non-salaried population with emphasis on women and children-Maternal and child services provided in ambulatory facilities with gradual expansion to surgical services for congenital heart diseases
- Chile: Plan name: Plan de Acceso Universal a Garant IAS Explıcitas (AUGE) 2005, all the population- 80 interventions that cover around 60% of the national burden of disease. - Colombia: Plan name: Plan Obligatorio de Salud (POS) 1993- All the population- Comprehensive health packages that includes essentials and costly interventions - Honduras: Plan name: Plan de Beneficios en Salud (PBS) 2003- Poor, rural population with emphasis on women and Children-Maternal and child ambulatory services, with emphasis in health promotion and preventive interventions. - Mexico: Plans name: Catalogo Universal de Servicios Esenciales de Salud (CAUSES). Fondo de Protecci_on contra Gastos Catastroficos (FPGC). Seguro, 2003 -Non-salaried population- 280 essential interventions provided by ambulatory facilities and general hospitals (CAUSES) and 65 costly interventions provided in specialized hospitals (FPGC). - Peru: Plan name: Plan Esencial de Aseguramiento en Salud or PEAS, 2009 -All the population- 140 essential interventions with emphasis on maternal and child care |
- These programs were the initial reforms in these countries to achieve public health coverage, which hoped to achieve public health coverage because of the progress and positive effects of implementing these reforms in these countries. To achieve this important goal, these countries need experts to implement innovative reforms tailored to the needs of the country. |
| Frenk, J. et al, 2009 (6) | Mexico |
Services Coverage
Financial Protection Population Coverage |
Stewardship
Financing Resources Generation |
- In 2003, the Mexican Congress approved a reform establishing the System of Social Protection in Health, whereby public funding for health is being increased by one percent of the 2003 gross domestic product over seven years to guarantee universal health insurance.
- In the System of Social Protection in Health, funds are allocated into four components: (i) stewardship, information, research and development; (ii) community health services; (iii) non-catastrophic, personal health services; and (iv) high-cost personal health services. - The Seguro Popular is the insurance instrument devised to finance these services under the reform. For financing purposes, personal health services derive from two sources: a package of essential interventions provided in outpatient settings and general hospitals and financed through a fund for personal health services, and a package of highcost, specialized interventions financed through the Fondo de Protección contra Gastos Catastróficos Fund for Protection against Catastrophic Expenditures. - The Seguro Popular will offer coverage to all Mexicans not protected by any other public insurance scheme: the self-employed, those who are out of the labour market and those in the informal sector of the economy. - The Seguro Popular is financed, first, through a social contribution from the federal government. Second, since there is no employer, financial coresponsibility is established between the federal and state governments to generate the so-called federal and state solidarity contributions. The third contribution comes from families and is tied to income, as in the case of social security institutions. |
- In a phase of seven years, this will provide access to formal social insurance, to the 45 million Mexicans who had been excluded from it in the past.
- The new Seguro Popular scheme guarantees access to a package of 255 health interventions targeting more than 90% of the causes leading to service demand in public outpatient units and general hospitals, and a package of 18 costly interventions. - The population with social protection in health increased 20% between 2003 and 2007. - Expenditure for health increased from 4.8% of the GDP in 1990 to 5.6% in 2000 and to 6.5% in 2006. - Public health expenditure as a percentage of total health expenditure increased from 43.8% in 2002 to 46.4% in 2006. - The budget of the MoH increased 72.5% in real terms between 2000 and 2006. - The proportion of the MoH health budget devoted to investment increased from 3.8% in 2000 to 9.1% in 2006, and because of this, the MoH was able to construct 751 outpatient clinics and 104 hospitals, including high-specialty hospitals in the poorest states, between 2001 and 2006. In the public sector as a whole, 1054 outpatient clinics, 124 general hospitals and 10 high-specialty hospitals were built in the same period. |
| Garchitorena, A. et al, 2017 (7) | Madagascar |
Services Coverage
Financial Protection Population Coverage |
Stewardship
Services Delivery Financing |
- A national policy for universal health coverage was signed in December 2015, focused primarily on developing a national health insurance system that pools contributions from taxes, external donor grants, and other sources, to create a prepaid system that reduces fees at the point of service.
- Since 2014 two pilot programs to remove access barriers by providing primary health care services free of charge were implemented in a rural district of Madagascar. - Intervention 1: - The conditions of the Vatovavy-Fitovinany region prompted the World Bank to include it in a project for Emergency Support to Critical Education, Health, and Nutrition Services, implemented in five regions in extreme need across Madagascar. The health component of this project aimed to increase access to health care by providing an essential package of services at no cost for children under age five and pregnant women. The program was implemented in Ifanadiana at all thirteen major health centers but did not cover the districts six other health centers, which were classified as basic health centers. The essential services covered prevention of and treatment for a wide range of conditions. The program was initiated in Ifanadiana in February 2014 and was carried out by local nongovernmental organizations through a voucher system. Every woman attending the health center for antenatal, delivery, or postnatal care (first six weeks) or escorting a child under age five with any illness received a voucher from a program agent. After consultation at the health center, the patient could preset her voucher at the center’s dispensary to receive free medicines prescribed by the center’s Ministry of Health staff. - Intervention 2: - In early 2014 Madagascar’s Ministry of Health also partnered with a nongovernmental organization, PIVOT, to create a model health district for the country based on the WHO’s framework of six building blocks of health system strengthening. Ifanadiana was chosen as the place to test the model health district interventions. This program’s first phase focused primarily on the catchment area of four major health centers, representing approximately one-third of Ifanadiana’s population. In these health centers, supply-side initiatives such as infrastructure renovations and support for different clinical programs have been progressively implemented over the first two years. The most discrete policy change implemented in this area was a program to eliminate point-of-service payments for all patients seeking care at the four targeted health centers. This program, covered costs of forty essential medicines and twenty medical supplies Some additional health system strengthening activities span the entire district, such as hiring medical and non-medical staff at health centers to comply with Ministry of Health policies, training medical staff to improve quality of care, and establishing a referral ambulance network to facilitate access to secondary care. |
- The two programs’ removal of point-of-service fees was associated with health care utilization increases of nearly two-thirds for all patients, more than half for children under age five, and more than 25 percent over two years in maternity consultations.
- Baseline outpatient utilization rates were higher at major health centers than at basic health centers for all patients (relative change: 1.60) and for children under age five (RC: 1.44) but not for maternity care. Each additional health care provider presents in the health center in-creased utilization (RC: 1.09). - The direct costs of the two reimbursement programs were low. In the period from the beginning of each program until December 2015, 90,200 people benefited from fee exemptions in Ifanadiana health centers, with an average cost of US$0.60 per patient. |
| Suneela Garg, 2018 (8) | India |
Services Coverage
Quality |
Stewardship
Services Delivery Resources Generation Financing |
- From medical coverage to achieving holistic health: A paradigm shifts from provision of essential to quality health care at the primary care level. These wellness centers will provide comprehensive healthcare for the management of non-communicable diseases with lifestyle modifications, maternal and child care, adolescent health, nutritional and health education, promotion of menstrual hygiene, and free essential drugs and diagnostic services. Basic dental, ENT and ophthalmology services will also be provided at these centers.
- Primary healthcare with focus on systems beyond medicine: There is a renewed governmental focus on hygiene sanitation, housing, clean indoor air by provision of clean fuels, and expansion of immunization service and coverage. All these initiatives that influence the health of the poor, vulnerable, and under-served population have achieved excellent success in their respective domains. - Focus on protecting maternal health: The Maternal Death Surveillance Response program is geared toward reducing maternal mortality and near misses by improving quality of maternal death reporting with the appropriate capacity building. It involves tracking and identifying the cause of every maternal death at both the facility and the community level and using the information generated for health system strengthening and capacity building for precluding future instances. - Promoting gender equity: There is a welcome and sustained focus on ending female feticide, improving child sex ratio and education of the girl child through the campaign of the government of India called (Save the girl child – Educate the girl child). Promoting menstrual hygiene by the distribution of free of cost menstrual pads, prevention and control of anemia by the distribution of weekly iron‑folic acid tablets in schools, construction of toilets in all schools, scholarships for girls from vulnerable sections of society. - The use of information technology (ICT): for bridging the gap for those lacking access to quality healthcare and reaching the unreached is essential. The various ICT application in healthcare being explored in India include telemedicine, vaccine and drug inventory control and storage, training of health workers, disseminating health education, promotion of behavior change, drug adherence in tuberculosis (TB). - Promotion of generic medicines and cheaper implants to significantly lower out‑of‑pocket costs: The Affordable Medicines and Reliable Implants for Treatment schemes reflect prioritization toward amelioration of routine treatment costs for patients lacking insurance coverage for their outpatient expenses. Strict quality control measures and ubiquitous drug availability and affordability through promotion of entrepreneurial opportunities are the key program drivers. - Public–private partnerships (PPP): Collaborative efforts between private and public sector for improving health service delivery, expansion of coverage, and last mile service delivery have found significant traction in the past two decades. Furthermore, utilizing PPP in critical national health programs such as TB to improve drug adherence and cure rates in patients reaching private sector has received growing impetus. - Strengthening of national programs in TB and HIV‑AIDS |
- The advancement of UHC in India shows a steady evolution.
- Sustainable development regarding universal access to good education, sanitation, clean energy, safe environmental and sound infrastructure which are essential for realizing and maintaining a state of good health is in a state of acceleration. |
| He, A. J and Wu, S. 2017 (9) | China |
Financial Protection
Population Coverage |
Stewardship
Financing |
- The landmark health reform plan announced in 2009. In this health reform expanding the coverage of SHI schemes stands out as one of the five strategic objectives. An additional US$125 billion equivalent to 53 % of the coun-try’s total health expenditures in 2009 has been spent in the first phase of the reform from 2009 to 2011.
- Urban Employee Basic Medical Insurance Scheme (UEI): Launched in 1998 after successful pilots in two cities, the Urban Employee Basic Medical Insurance Scheme (UEI) is the first initiative to fulfill the government’s com-mitment to universal coverage. All urban employees are required to join, by paying 2 % of their payroll income, which is matched by an employer’s contribution of 6 %. The UEI is administered by human resources and social security bureaus at the city level, which have a certain degree of discretion in setting the rate of contribution, deductibles, copayments, reimbursement ceilings, and the methods of collecting premiums as well as paying pro-viders. Upper-level social security authorities exert oversight on the operation of local schemes. - New Cooperative Medical Scheme (NCMS) in 2003: As a voluntary insurance program, the NCMS is pooled at the county level and administered by local health bureaus, with vertical supervision from the central and provincial health authorities. The scheme is funded by enrollees’ premiums (about 20 %) and generous subsidies from both central and local governments (about 80 %). In order to avoid adverse selection, enrolment is required at the household level. - Urban Resident Basic Medical Insurance Scheme (URI): Introduced in 2007, URI aims to insure students, children, and other unemployed urban residents, who were not previously protected by the UEI. Like the NCMS, the URI was designed as a voluntary program, and requires enrollment at the household level to reduce adverse selection. Similar to the arrangements of the NCMS, the URI is also financed by both individual contribution and govern-ment subsidies, at a 30–70 split. The actual rates of premiums and subsidies largely depend on individuals’ eco-nomic situations and the financial capacity of the local government. Local governments are given autonomy in designing their schemes, and therefore, benefit packages vary across localities. |
- As of 2014, the UEI covers 283 million people.
- With consideration to strong political commitment and administrative mobilization, the NCMS has expanded dramatically in coverage, despite its voluntary nature. More than 800 million rural resi-dents had been insured by 2013. - All SHI schemes have expanded significantly in the past decade: 1.37 billion Chinese were covered by at least one scheme by 2013, an achievement largely attributable to the strong political will of the central leadership, generous government subsidies, and the high mobilization capacity of the country’s admin-istrative machinery. - In parallel with the marked increase in outpatient visits, hospital admissions more than doubled between 2003 and 2011; the effect was most signifi-cant in rural areas. - ** In other words, the reform has not yet made significant progress towards its professed goal of providing affordable care. - ** Moreover, the structural fragmentation of the SHI system has undermined both equity and efficiency of risk pooling; reforms are necessary. - *** Significant disparities exist across the three schemes as well as different regions. As the most generous scheme, the UEI has wider coverage and offers higher benefits than URI and NCMS, thanks to its greater financing capacity. The average UEI premium is ten times higher than those of other schemes. |
| Hongoro, C. et al, 2018 (10) | Uganda | Population Coverage | Stewardship |
- A project entitled “Supporting Policy Engagement for Evidence-based Decisions (SPEED) for Universal Health Coverage (UHC) in Uganda” was launched by the School of Public Health at Makerere University (MakSPH) in 2015. The overall objective of SPEED Project is to strengthen capacity for policy analysis, implementation moni-toring and analysis of impact and thereby contribute to accelerating progress towards UHC in Uganda. The SPEED project seeks to conduct 3 barometer surveys over its 5-year life span (2015–2020).
- Policy Implementation Barometer (PIB) survey which is a mechanism to reveal gaps in policy implementation and thereby provide feedback to the decision makers about the implementation of a selected set of policy programmes for UHC. PIB is proposed as a mechanism to provide feedback to the decision makers about the implementation of a selected set of policy programmes at various implementation levels (macro, meso and micro level). The main objective is to establish the extent of implementation of malaria, family planning and emergency obstetric care policies in Uganda and use these results to support stakeholder engagements for corrective action - The specific objectives of the PIB study are (1) To assess the perceived appropriateness of policy programs im-plemented to address identified policy problems, (2) To assess, using priority parameters, the extent to which the prerequisites for implementation are established, (3) To determine the enablers and constraints to implementation of the selected policies , (4) To compare on-line and face-to-face administration of the PIB questionnaire among target respondents and (5) To document stakeholder responses to PIB findings with regards to policy implementa-tion, awareness and actions. - The main objective is to establish the extent of implementation of malaria, family planning and emergency obstet-ric care policies in Uganda and use these results to support stakeholder engagements for corrective action. |
- UHC objectives for Uganda by ensuring that the selected policy cases for the barometer are relevant to the UHC agenda and government priorities. Ap-plication of an accountability framework such as a policy implementation barometer will foster a sense of responsibility amongst implementers and upstream monitoring will therefore become more effective and hopefully the impact will improve.
- Policies succeed or fail for a variety of reasons and this study seeks to unpack the drivers and bottle-necks in the implementation of specific policies towards UHC in Uganda that is malaria, family planning and emergency obstetric care. These are transnational priority health areas affecting most countries in the sub-region. |
| Hughes D and Lee-thongdee S, 2007 (11) | Thailand | Population Coverage |
Stewardship
Services Delivery |
- The 30 Baht Scheme: is a new public health insurance scheme that provides treatments within a defined benefit package to registered members for a copayment of 30 baht. The 30 Baht Scheme filled the coverage gap left by the existing public health insurance schemes (US$0.80; 0.64 euro; and £0.43) per chargeable episode.
- All members register with a contracting unit and receive a gold card entitling them to care in their home area. Elderly people, children, and poor people receive a special version of the registration card and pay no fee. Drugs prescribed are limited to those on a national list, some high-cost or chronic disease treatments are sub-ject to cost ceilings, and there was initially no entitlement to antiretroviral thera-py or hemodialysis (although these were later brought within the scheme). Treat-ment outside the area of registration is limited to accident and emergency care. Finance for the scheme comes mainly from public revenues paid to local contract-ing units on the basis of population. |
- The 30 Baht Scheme extended the insured population from about twenty-five million (40 percent of the population) in 2001 to above fifty-nine million (95.5 percent) in 2004.
- Although basic coverage was achieved remarkably quick-ly, the 30 baht project required a transformation of the resource allocation system. |
| Kingue, S, et al, 2013 (12) | Cameroon | Population Coverage |
Stewardship
Resources Generation Financing |
- The Cameroonian government developed an HRH emergency plan for the years 2006 to 2008.
- The main strategy for reducing HRH problems in Cameroon is therefore to capital-ize on the existing potential – primarily by improving the coordination and effec-tiveness of the key stakeholders' current efforts to improve the health system. - Between 2007 and 2010, Cameroonian HRH received increased financial support from external sponsors. Over this period, the International Monetary Fund and the World Bank – via the Heavily Indebted Poor Country initiative – and the French government – via the Contrat de Désendettement et de Développement – together contributed about 7359 million African Financial Community (CFA) francs to-wards the salaries of health workers in Cameroon. - The HRH emergency plan for 2006–2008 did not solve the maldistribution of HRH in Cameroon, where health care is concentrated in urban areas; the low allo-cation of financial resources for HRH, or the absence of an accreditation system for HRH training. External resources were therefore mobilized to develop new approaches to address these challenges. The mobilization process started in 2007, with a 2-day conference on HRH organized by the Global Health Workforce Alli-ance. This conference resulted in the Douala Plan of Action.4 In 2010 – with fi-nancial support from the World Health Organization (WHO), the Global Health Workforce Alliance, the French Development Agency and the European Union – Cameroon's Ministry of Public Health formally adopted and implemented a “country coordination and facilitation” process. The aims were to clarify the main challenges to effective HRH in Cameroon and to subsequently create an integrated, participatory and comprehensive HRH-development strategy – for the years 2011–2015 – that would address these challenges. |
- the Cameroonian government in response to the HRH crisis, Implementation of this plan led to the recruitment of 5400 health workers, the opening of new training schools for health workers, the revision of the training curricula for paramedical staff, and a simplification of the process that contract or temporary workers need to follow to become permanent employees in the public sector.
-Between 2007 and 2009, the number of active health workers in Cameroon increased by 36% (Implementation of the HRH emergency plan resulted in the recruitment of 6417 additional health workers between 2007 and 2009.), Such recruitment increased the number of active health workers in the country from 11 528 in 2005 to 15 720 in 2009 – a 36% increase. Lessons: -In the improvement of HRH, strong leadership is needed to ensure effective coordination and communication be-tween the many different stakeholders. A national process of coordination and facilitation can produce a consensus-based view of the main HRH challenges. Once these chal-lenges have been identified, the stakeholders can plan appropriate interventions that are coordinated, evidence-based and coherent. |
| Felicia Marie Knaul and Julio Frenk, 2005, (13) | Mexico |
Finance protection
Population Coverage Services Coverage |
Stewardship
Financing Services Delivery |
- System for Social Protection in Health (SSPH):
- The reform was passed into law in April 2003, and the new insurance scheme, called the System for Social Protection in Health (SSPH), went into operation January 2004 with the goal of achieving universal coverage by 2010. The Popular Health Insurance (PHI) is the operational program of the new system. The affiliation process runs from 2004 to 2010, so that 14.3 percent of the approximately eleven million families that make up the uninsured population will be included each year. Preference must be given to families from the lowest income deciles. Reducing out-of-pocket payments tend to be inequitable, unjust, and inefficient a cause and a result of the imbalances discussed above is atarget of the reform. A new public insurance scheme (PHI) was devised to fi-nance personal health services. For funding purposes, personal health services are divided between an essential package of prima-ry- and secondary-level interventions in ambulatory settings and general hospitals, and a package of high-cost tertiary care fi-nanced through the Fund for Protection against Catastrophic Expenditures. - New system of social protection in health that will offer public insurance to all citizens. - The reform has four main objectives: (1) to generate a gradual, predictable, financially sustainable, and fiscally responsible mecha-nism to increase public spending in health so as to correct the existing disequilibria; (2) to stimulate greater allocational efficiency by protecting spending for public health interventions that are cost-effective but tend to be underfunded; (3) to protect families from excessive health spending by offering a collective mechanism that fairly manages the risks associated with paying for person-al health services; and (4) to transform the incentives in the system by moving from supply-side to demand-side subsidies to pro-mote quality, efficiency, and responsiveness to users. - The logic of the reform separates funding between personal and community health services by establishing a separate fund for the latter that is used exclusively to finance public health programs. - The package of essential services is covered by funds administered at the state level, because these services are associated with low risk, high-probability health events. |
- Through a new system of social protection in health that will offer public insurance to all citizens, the reform is expected to reduce cata-strophic and out-of-pocket spending while promoting efficiency, more equitable resource distribution, and better-quality care. |
| Knaul, F. M. et al, 2012, (14) | Mexico |
Finance protec-tion
Quality |
Stewardship
Financing Services Delivery |
- The 2003 reform established a system encompassing all three dimensions—risk, patient, and finance— embedded in the concept of social protection of health. Specifically, public health interventions, institutions and dedicated financing are providing protection against health risks; system-wide initiatives that enhance patient safety, effectiveness, and responsiveness are protecting the quali-ty of health care and Seguro Popular is continually expanding protection against the financial shocks of disease and disability.
- The financial reform was complemented with supply strengthening provisions, including hospital management reform, improved schemes for drug supply, outcome-oriented information systems, a master plan for long-run investment in health infrastructure, and technology assessment. - Innovations to promote protection for patients and against health risks: - Emphasis was also placed on public health through the following instruments: (1) a protected fund for community services; (2) a set of personal health promotion and disease prevention guides (similar to the traditional immunization certificates) with a gender and life course perspective; (3) a comprehensive reorganization of regulatory activities through a new public health agency—the Federal Commission for the Protection against Health Risks (COFEPRIS) charged with safety and efficacy approvals of new drugs and medical devices, food safety regulations, enforcement of environmental and occupational health standards, and control of mar-keting of hazardous substances such as alcohol and tobacco; and (4) major investments in public health to enhance security through epidemiological surveillance and improved preparedness to respond to emergencies, natural disasters, pandemics, and bioterrorism. - To reinforce patient protection, the central program of the managerial reform was the National Crusade for Quality in Health Care. The purpose of this program was to enhance patient safety, improve responsiveness, manage facility accreditation and provider certification, implement quality improvement initiatives, measure technical and interpersonal quality, and undertake performance benchmarking among states and other organizations. - Another important innovation was the creation of the National Center for Health Technology Excellence (CENETEC) in 2004. This Centre produces information and enables an evidence-based approach for investment and use of medical technologies, and coordinates the development of clinical practice guidelines. It has achieved international recognition and is a WHO collaborating center. - Innovations to promote financial protection: - Key to the financial innovations introduced by the SSPH is the separation of funding between personal health services and health-related public goods (including non-personal health services). The separation is designed to protect public health services, which tend to be at risk in reforms that expand insurance. Funds are aggregated over the population without access to social security and divided into four components: (1) stewardship, information, research, and development; (2) community health services; (3) essen-tial personal or clinical health services; and (4) high-cost, catastrophic health interventions. |
- Evidence shows significant progress in reduction of catastrophic health expenditure and impoverishing health expenditure. Catastrophic and impoverishing health-care payments from 1992 to 2010 show a long-run downward trend. In 2000, 3·1% of households had CHE and 3·3% had IHE. By 2010, the values had dropped to 2% for CHE and 0·8% for IHE.
- The differences between households with and without social security are decreasing. The differential share of out-of-pocket spending in house-hold income and CHE fell for all groups between 2004 and 2010, especially for families without so-cial security. IHE fell from 0·2% to 0·1% for households with social security, and from 2·1% to 1·6% for the rest of the population. - Seguro Popular is successfully closing the gaps in health financing across population groups the gap in the per capita allocation of public resources fell more than 70% be-tween 2004 and 2010. |
| Limwattanano et al, 2016 (15) | Thailand |
Finance protection
Population Coverage |
Financing
Stewardship Services Deliv-ery |
- Pre-reform:
- The single largest scheme was a non-contributory Medical Welfare Scheme that entitled the poor, children, the elderly (60+), the disabled and a few other groups to care in public facilities free of charge. This tax-financed scheme covered 32% of the population in 2001. The annual budget per enrollee was just 273 Baht (~$6.82) in 1998 (excluding salary costs). - The second largest programme prior to the reform was a Voluntary Health Card Scheme in which 21% of the population was enrolled in 2001. For 500 Baht ($12.50) per year, households could purchase a health card that entitled up to five house-hold members to free care at public facilities. The private contribution was supplemented by a 1000 Baht tax-financed gov-ernment subsidy. With over four enrollees per card on average, the budget was often insufficient to provide adequate care and, similar to the welfare scheme, there was substantial cross subsidization. - Active and retired government employees and their dependents were and continue to be covered by an entirely tax-financed scheme that provides completely free care at public health facilities. This Civil Servants Medical Benefit Scheme covered 8.5% of the population in 2001. Operating under an uncapped fee-for-service system with a generous benefit package, spending per capita was almost 2500 Baht ($62.50) per enrollee in 1998. - Post-reform: - All Thai citizens not covered by the two employment-based schemes were given entitlement to coverage by the newly instituted, tax-financed Universal Coverage Scheme (UCS) that replaced the welfare and voluntary enrollment schemes. Starting in April 2001 with its introduction in six pilot provinces, the scheme was expanded to cover 15 provinces in June 2001 and the remaining provinces by October of that year. - Beneficiaries of the UCS are entitled to inpatient treatment, ambulatory care and prescribed medicines at facilities within a local provider network. The benefit package is near comprehensive. Medicines can be prescribed from a restricted list con-taining a large proportion of generics. - On top of the coverage extension, the main ingredients of the supply side measures were: 1. a closed-end capitation-based budget; 2. gatekeeper control of access to specialist care; 3. prospective payment of hospitals for inpatient treatment; and, 4. a single public purchaser of care and medicines for UCS beneficiaries (from 2006). |
- Pre-reform:
- Ten years before the universal coverage reform in 2001, two-thirds of Thai citizens had no formal health insurance. Expansion of various public health insurance schemes cut this fraction to less than 30% just be-fore the reform. - The second largest programme prior to the reform was a Voluntary Health Card Scheme in which 21% of the population was enrolled in 2001. - Post-reform: - The percentage of the population covered by some form of health insurance jumped from 71% in 2001 to 95% in 2003, and by 2011 coverage had risen to over 98%. - In the post-reform period, such that real total expenditure per capita doubled be-tween 2001 and 2010, and public health expenditure per capita increased by almost 170%. Due to rapid economic growth, total health spending as a share of GDP in-creased by only 0.6 of a percentage point from 2001 to 2010. Household OOP spending held roughly constant in real terms and fell as a percentage of GDP. - The reform had the largest and most signifi-cant impact on household spending on ambulatory care, which was reduced by 38%, on average. |
| Long, S. K. 2008, (16) | Massachusetts USA | Population Coverage |
Stewardship
Financing Services Delivery |
- Massachusetts health reform includes expansions to the Medicaid program (called MassHealth), the creation of a new program that provides income-related subsidies for health insurance (the Commonwealth Care Health Insurance Program, or CommCare), the creation of a new purchasing arrangement (Commonwealth Choice, or CommChoice) via the new Com-monwealth Connector, health insurance market reforms, and requirements that both individuals and employers participate in the health insurance system.
- Key Components of the Massachusetts Health Reform: - Expansion of MassHealth (Medicaid) to children up to 300% of poverty - Expansion of MassHealth Insurance Partnership Program, which provides insurance subsidies and employer tax credits to workers in small firms to 300% of poverty. - Increase in enrollment caps for MassHealth programs for long-term unemployed adults (eligible up to 100% of poverty), disabled working adults (eligible at any income level), and people with HIV (eligible up to 200% of poverty). - Restoration of dental, vision, and other MassHealth benefits to adults. - Creation of new MassHealth wellness benefit/incentive program - Increase in hospital and physician rates under MassHealth. - Creation of CommCare, which provides subsidized insurance for adults up to 300% poverty who are not eligible for MassHealth and do not have access to employer coverage - Creation of Connector Authority, which provides purchasing vehicle for individuals without access to employer coverage and small employers (< 51 employees) via CommChoice. |
- Creation of new Young Adult products for up to 26-year-olds who do not have access to employer coverage
- Extend dependent coverage rules up to age 26 or two years after loss of IRS dependent status, whichever is earlier - Requirement that employers with 11+ employees offer access to Section 125 plan or face potential of a “free-rider sur-charge” if employees use substantial amounts of care through the Health Safety Net Trust Fund. - Requirement that employers must make a “fair and reasonable” contribution toward the cost of health insurance or pay a “fair share” assessment of $295 per employee. - Merger of nongroup and small-group markets - Requirement that all adults age 18 and older have health insurance if it is affordable (“individual mandate”). - Yet another goal of Massachusetts’ health care initiative is to improve access to affordable care both by expanding health insurance coverage and by raising the standard for what counts as insurance. - The uninsurance rate for adults ages 18–64 in Massachusetts dropped by almost half. As a result, in fall 2007, roughly one year after the state’s health reform initiative began; nearly 93 percent of nonelderly adults in the state were insured. - For adults with incomes below 300 percent of poverty (the target population for CommCare), the uninsurance rate dropped by nearly eleven percentage points as a result of health reform, down to about 13 percent in fall 2007. - Dental care benefits were expanded under MassHealth. - There were significant gains in access to care across the overall population under reform, with the gains concentrated among low-income adults. There were very few changes in access to care for higher-income adults, however, the changes that were ob-served suggest that there have been some improvements in access to care for that group as well. |
| Lu, C. et al, 2012 (17) | Rwanda |
Finance protection
Services Coverage |
Financing
Services Delivery Stewardship |
Mutuelles de sante´ (Mutuelles): is a community-based health insurance program established by the Government of Rwanda (GoR) as a key component of the national health strategy on providing universal health care and reaching the health Millen-nium Development Goals (MDGs).
Facing limited resources, the GoR has been implementing Mutuelles since 1999 to provide affordable basic services, espe-cially child and maternal care, to the uninsured population. A pilot program was implemented in three selected districts in 1999 and 2000. To standardize the main parameters of Mutuelles, such as the benefits package, enrollment fees, subsidization mechanisms, organizational structure, management systems, etc., the Mutuelles Health Insurance Policy was approved by the GoR at the end of 2004. Until it was fully implemented in 2006, there was variation and flexibility in scheme design across districts. In 2008, a law on the creation, organization, and management of Mutuelles was enacted, which further strengthened the strategy. Approximately 50 percent of Mutuelles’ funding was comprised of annual member premiums. The remaining half was ob-tained via transfers from other insurance funds, charitable organizations, NGOs, development partners, and the GoR. Providers are paid by Mutuelles directly, either through monthly capitation rates on a fee for-service basis, or performance-based payments. Mutuelles uses a policy of household subscription. Enrolled households are affiliated to designated health centers. With referrals from the health center, members may obtain hospital services covered by Mutuelles. To mitigate adverse selection, enrollees must wait one month to utilize covered services. |
To date, Rwanda is the only country in sub-Saharan Africa where more than 90% of the population is covered by community based health programs.
The evidence suggests that at the individual level, Mutuelles improved medical care utilization among the general population, under-five children, and women with child delivery. At the household level, Mutuelles protected households from catastrophic health spend-ing. At the provincial level, was existans a positive effect of Mutuelles coverage on child and maternal care coverage. At the national level, observed an increase in medical care coverage accompanied by a decrease in OOPS and percentage of households with catastrophic health spending. It seems plausible that the increase in medical care coverage contributed to major improvements in child mortality and maternal mortality during the same period. Currently, Rwanda is one of the few African countries that stand a chance of reaching the targets of health MDGs. *The positive results of the Mutuelles program in promoting medical care utilization and financial risk protection suggests that the community-based health insurance scheme can be an effective tool for achieving universal health coverage, together with other policy instruments. |
| Lu, J. F. R. and Chiang, T. L. 2018, (18) | Taiwan | Population Coverage Quality | Rescuers Generation |
Four key strategies adopted in the health service sector development Taiwan:
1) Enhancing public-private partnerships in developing medical resources with tax incentives and subsidies: Taiwan was able to exploit the economic resources to inculcate its health workforce and facilitate capacities building and has applied a combination of macro-controls and market forces to the health resource management at different levels of economic devel-opment. Once the economy started to boom, the government exerted efforts in engaging private investment and devise appro-priate policy to ameliorate distribution imbalance. Public-private partnership is one key to the success of service sector development, but the expansion of private sector cannot be left completely unregulated. 2) Ameliorating regional disparities in medical resource distribution through incentives and effective regulation: Taiwan’s government took multifaceted actions to successfully tackle the issues of supply shortage as well as maldistribution of physicians and hospital beds. Important throughout were the use of economic incentives, public-private partnerships, while government regulation also played a crucial role in stabilizing market supply and the geographic distribution of healthcare providers. 3) Safeguarding quality of care by regulating providers through licensing and accreditation programs. 4) Promoting an evidence-based policy-making process. The efforts exerted by the government, with the private sector partnerships, in AAAQ framework are described as below: Availability: Strengthen, plan and support the cultivation of health workforce through founding 4 public medical schools and subsidizing 8 private medical schools. Provide financial incentives (tax advantages and interest-free grants) to build up hospital capacities. Accessibility: Reduce inequality in workforce distribution through incentives (interest-free grants for hospital building projects in the non-metropolitan area and Group Practice Centers) and regulatory (constraints on the expansion of large private hospitals in resource-saturated metropolitan areas) approaches delineated in the Medical Care Network planning program. Acceptability: Reinforce the regulation of medical practices through 1975 New Physicians Act and 1986 Medical Care Act, which cracked down the practices of those who did not receive formal medical education and enforced the requirement of two-year resident training program and specialist licensing to meet public expectation. Quality: Safeguard hospital service quality, a nationwide all-hospital accreditation program was implemented in 1987. |
The key to its success in providing effective coverage to its 23 million populations was the readiness of the health service sector.
Taiwan’s experiences in service sector development manifest the importance of economics resources and political leadership. |
| Maluka, S. et al, 2018 (19) | Tanzania | Services Coverage |
Services Delivery
Stewardship |
Design and implementation of Service Agreement (SAs) between local governments and non-state providers) NSPs) for the provision of primary health care services.
In Tanzania, NSPs of health services include faith-based organizations (FBOs), non-governmental organizations (NGOs), private for-profit providers and informal providers. Faith-based providers, the most prominent group in terms of total infrastructure, number of staff, and geographic reach in Tanzania. The private not-for-profit sector of which the faith-based facilities make up the overwhelming majority is the second largest provider of health services in the country. The FBO sector owns 23.3% of health infrastructure, while the state owns 60%. However, 41.1% of hospitals are owned by FBOs while 40% are owned by the state, making faith-based NSPs the largest providers of hospital services in the country. Health sector funding in Tanzania comes from two main sources: central support financed by the government of Tanzania’s general tax revenue; and development partners’ (DPs) support. DPs provide pooled funding both through general budget support (GBS) and the Health Basket Fund (HBF), a form of sector budget support. Tanzania depends on a significant level of DP support to finance health care, while the share of funding from domestic taxes remains low. Governance of the health system occurs at multiple levels. The Ministry of Health, Community Development, Gender, Elderly and Children is mandated to provide overall stewardship of the health sector. In the 1990s, the introduction of the health sector reforms and the concept of partnerships between government and NSPs in health services delivery gained importance. The 1994 formulation of the health sector reforms highlighted the importance of the role of NSPs in health service delivery. In 2005, the government revised the 1992 agreements so that contracts could be signed at district level by the office of the District Executive Director (DED). In 2007 the government introduced the Primary Health Services Development Program (PHSDP), a major initiative to run from 2007 through 2017. This program also recognized the role of NSPs in expanding the coverage of health services. The Ministry of Health and Social Welfare developed a SA template to guide contractual arrangements between NSPs and the local government authorities. In 2009, Tanzania’s first public-private partnership (PPP) policy was developed to guide the institutionalization of these partnerships. The PPP Act followed in June 2010 and PPP Regulations were gazetted in June 2011. In all districts, the contractual arrangements mainly aimed at increasing access to MCH services. The central government had committed to provide free MCH services in all public health facilities. The specific services covered included antenatal care, delivery and postnatal care services and prevention of mother-to-child transmission of HIV. Two main problems were reported by the FBOs in relation to financing: overall shortages of funds and delays in the disbursement of funds. Shortages were caused by high demand for health services. |
Participation by NSPs leads to more efficient and effec-tive use of available resources, especially in district-level annual health plans.
Tanzania’s implementation of SAs in contracting-out delivery of primary health care services has already made significant contributions towards the country’s move-ment for universal health coverage. |
| Meng, Q. and Xu, L. 2014 (20) | China |
Services Coverage
Finance Protection Population Coverage |
Stewardship
Services Delivery Resources Generation Financing |
The reforms initiated in 2009 have focused on improving social health insurance schemes in both rural and urban areas, strengthening the primary health care system, supporting delivery of essential public health programs, removing drug markups from the financing of the primary health providers, and reforming the public hospital sector.
Prior to the reforms, China had begun expanding health insurance schemes for the rural population in 2003 and for urban unemployed individuals in 2007. Establishing prepayment systems has been a key strategy in China to provide people with financial protection. |
The population coverage of the three schemes from 2003 to 2011, with a rapid expansion from the mid-2000s. Between 2003 and 2008, the impoverishment rates de-creased by 0.9%.
Analysis of the progress towards UHC with selected indicators shows positive trends, especially in service coverage. In terms of financial protection, nearly all Chi-nese people have been covered by either rural or urban health insurance schemes. |
| Mills, A. et al, 2012, (21) | Ghana South Africa Tanzania | Population Coverage | Financing |
Ghana: Ghana began implementing a national health-insurance scheme (NHIS) in 2004, with elements covering both the formal and informal sectors. The NHIS covers people in the formal and informal sectors for a comprehensive range of outpatient and inpatient services at accredited public and private facilities.
Financing: Whereas formal-sector contributions are transferred from social security payroll deductions, people in the informal sector have to pay their district mutual health-insurance scheme between US$5 and $35 per person per year in accordance with their socioeconomic status. The National Health Insurance Act requires all Ghanaians to join the NHIS. Formal-sector workers automatically contribute to the NHIS through payroll deductions and benefit from it once they register and secure a membership card, but membership is effectively voluntary for people in the informal sector, since payment of their contributions cannot be enforced. South African: The South African Department of Health has recently released a Green Paper to introduce a national health insurance, which aims at achieving universal coverage. The Department of Health proposes a publicly funded system, which will purchase a comprehensive package of services from accred-ited public and private providers for all citizens. In the past decade, Tanzania has introduced mandatory health-insurance schemes for formal-sector employees, offering comprehensive health-care benefits to their members, the largest being the National Health Insurance Fund covering civil servants. The National Social Security Fund (for private formal-sector employees) has also introduced a Social Health Insurance Benefit. There is a voluntary insurance scheme, the Community Health Fund (CHF), for rural dwellers, with premiums of between $4·2 and $12·7‡ per household per year, off ering public primary care to the informal sector. A similar scheme was introduced recently for urban dwellers, termed Tiba kwa Kadi (TIKA). In view of the low level of coverage by insurance schemes, out-of-pocket payments remain a major share of health-care funding in Tanzania. Substantial attention is now being paid to expanding insurance coverage of the informal sector through the CHF and TIKA. Furthermore, management of the operation of CHF and TIKA has been assigned to the National Health Insurance Fund, which could open the way for greater integration across insurance schemes. |
Ghana: NHIS coverage was estimated to be about 60% of the population by 2009.
Participation by NSPs leads to more efficient and effec-tive use of available resources, especially in district-level annual health plans. Direct taxes were progressive in all three countries. Indirect taxes were regressive in South Africa but pro-gressive in Ghana and Tanzania. Out-of-pocket pay-ments were regressive and overall health-care financing was progressive in all three countries. Out-of-pocket payments were regressive in all three African countries we included, most notably in Tanzania and Ghana where out-of-pocket payments are still a large share of total health-care expenditure. One of the greatest challenges in all three countries is to change the distribution of health service benefits through addressing pervasive access constraints. |
| Nuñez, P. A. et al, 2016 (22) | Argentina |
Services Coverage
Population Coverage |
Plan Nacer: Faced with deteriorating health indicators, in October 2004 Argen-tina’s government implemented Plan Nacer to strengthen a fragmented national health system plagued by strong jurisdictional asymmetries. The program introduced innovative changes in the incentive framework of health care pro-viders to equitably increase the access and quality of prioritized health ser-vices for pregnant women and children younger than 5 years.
Programa Sumar: Program Programa Sumar was launched in 2013, expanding the strategy and extending health care coverage to 5.7 million children and adolescents (0–19 years) and 3.8 million women younger than 64 years. Both programs were implemented synergistically with the main conditional cash transfer programs. The enrollment of beneficiaries in the UHC programs is a requisite that increas-es development options of vulnerable families and promotes preventive health care, nutrition, and education. |
Plan Nacer and Programa Sumar achieved significant improvements in birth outcomes by reducing the risk of neonatal death and increasing birth weight and contrib-uted to a 22% reduction in infant mortality and a 10% reduction in maternal mortality between 2005 and 2012.
The prevalence of stunting and underweight decreased 45.0% (from 20.6% to 11.3%) and 38.0% (from 4.0% to 2.5%), respectively, with differences between rural versus urban areas, gender, regions, age, and seasons. Findings describe a substantial decrease in the preva-lence of stunting and underweight among children cov-ered by UHC programs in Argentina between 2005 and 2013. |
|
| Obermann, K. et al, 2018 (23) | Philippines |
Services Coverage
Finance Protection Quality Population Coverage |
Stewardship
Services Delivery Resources Generation Financing |
1969: Creation of Medicare, forerunner of PhilHealth; Coverage: about 20%......
In 1996, the Philippines introduced a program for poor households (the Sponsored Program), integrated in the National Health Insurance Program (NHIF). ‘Philippine Health Agenda 2017–2022’: The bill provides a massive jump forward in terms of UHC as it stipulates that all Filipinos are automatically enrolled in, and thus entitled to the benefits of, the National Health Security Program. The Bill covers a wide range of health care issues like governance, regulation, human resources, health service delivery and income retentionby hospitals, and a health information system. The Bill distinguishes between members in the formal group, who are obliged to pay a premium, and members in the non-formal group. All senior citizens are also mandatorily covered. PhilHealth is tasked with working on improving access to quality care and reducing out-of-pocket (OOP) expenses. Sin Tax 2011: Amidst a generally weak tax policy and dministration, the country reformed the excise tax on tobacco and alcohol, channeling most of its revenues to health. Within the first year, the Sin Tax raised more than 1.2 billion USD, allowing the enrol-ment of an additional 14 million families or roughly 45 million Filipinos into PhilHealth. Two major initiatives towards improving access to quality care were the introduction of the so-called no balance-billing (NBB) for government hospitals and the expansion of the Health Facilities Enhancement Program (HFEP) in 2011. The NBB is a policy response to the strategy of many hospitals charging patients on top of what PhilHealth reimburses for the specific condition and treatment. The NBB has now explicitly forbidden government-owned hospitals to charge patients anything over and above what PhilHealth reimburses for case rates, Z-benefits and primary benefits at all accredited government health care institutions. The HFEP, starting in 2007, is a nationwide program by the DOH that aims to improve the supply side and its budget has gone up from 0.86 million USD; 2007 to 0.54 billion USD; 2016, in part due to the allocations from the Sin Tax revenues. PhilHealth benefit package is broad and payment is mostly based on clinical inputs, not on diseases/conditions to be treated. In general, one can distinguish between an inpatient benefit package, an outpatient benefit package and special packages. Further-more, PhilHealth has added specific benefits for the Sponsored Program that are not available to other NHIP beneficiaries. There are explicit limits on coverage such as non-prescription drugs and devices, alcohol abuse or dependency treatment, cosmetic surgery, optometric services, fourth and subsequent normal obstetrical deliveries, and cost-ineffective procedures as being defined by the corporation. |
PhilHealth covers about 93 million of the 104 million Filipinos. Amongst the 11 million non-covered are the near-poor, non-registered formal sector workers, self-employed profession-als, and prison inmates.
The share of PhilHealth in total health expenditures is still only 14%, managing quality and cost of provid-ers remains insufficient, the benefit coverage does not reflect the coun-try’s burden of disease, and financial protection for PhilHealth members is low. Lowering OOP, increasing access and population coverage as the major achievement, and greater access to quality care Sin Tax: enrolment of an additional 14 million families or roughly 45 million Filipi-nos into PhilHealth. Also, Eighty-five percent of revenues are allocated for health, of which 80% are for achieving UHC. |
| Okech, T. C. and Lelegwe, S. L. 2015, (24) | Kenya |
Finance Protection
Population Coverage Services Coverage |
Stewardship
Services Delivery Financing |
The government of Kenya has over the years since independence in 1963 initiated policy reforms and strategies earmarked towards universal health coverage. Some of these are outlined in various policy documents including Kenya Health Policy Frame-work (KHPF 1994–2010), Health Sector Strategic Plans, Vision 2030 (operationalized through the medium term expenditure framework of 2008-2012), the Constitution 2010, and finally, the Health Bill of 2015. The Kenya government provides a legal framework for ensuring a health care delivery system that is driven by the people while brindging the gap on geographical access by providing for a devolved system of governance.
In Health Bill of 2015, the government has declared access to reproductive health and emergency medical treatment as a right by all persons. Other initiatives included progressive elimination of fees in public health facilities as part of the strategy of increase access to health care. In 1980’s the policy shift from purely government provided for care to cost sharing was followed by the 1993 institu-tional and structural reforms, and market orientation of the health services. The government in 1994 developed the Health Policy Framework and a five-year National Health Sector Strategic Plan (NHSSP) of 1999-2004 wherein targets and processes driving the health sector development, as well as healthcare service delivery were articulated. In the document, equitable allocation of government resources to reduce disparities in health status and increased cost-effectiveness and efficiency of resource allocation and use were emphasized. Other initaivies reiterated were enhanced regulato-ry role of the government in health care provision; creation of an enabling environment for increased private sector as well as community involvement in service provision and financing; and increase and diversify per capita financial flows to the health sector agin key ingredients necessary in achieveing universal coverage. In the country, a new Constitution was promulgated in 2010 which among other issues provides the necessary legal framework for ensuring a comprehensive and people driven health care delivery aimed at enhancing access to quality health care. Specifically, the Constitution introduced a devolved system of governance with two tier government System County and National government with the goal of enhancing utilization and geographical access to quality care by all Kenyansincluding the poor and other vulnera-ble groups. In 2013, the government announced the abolishion of user fees at primary health care facilities and introduced free maternal health care services in public health facilities. This was lauded as a positive towards enhancing access to quality care especially the poor and other vulnerable groups. National Health Insurance Fund: the government has identified and settled on NHIF as official vehicle for the successful imple-mentation of universal health coverage for the country (NHIF, 2015). The abolition of user fees at primary health care facilities and introduced free maternal health care services in public health facilities. National Health Insurance Fund The envisaged enhanced package includes in-patient, outpatient and maternity services, with the treatment protocols pegged on Kenya national treatment guidelines and the Kenya Essential Package for Health (KEPH). |
The increased attendance of publicly provided primary health care ser-vices by the poor and reduction of financial risks as a cause for not using services provide a basis to argue that policy reforms continue to generate positive health outcomes and that the country is headed towards the intended objective.
The country’s political leadership announced user fee removal policies for the public health sector out of the blue, without giving technocrats sufficient time to correctly design, prepare and implement the reform. Consequently, some national policies though considered politically sound, may fail to bring the expected. |
| Pokharel, R. and Silwal, P. R. 2018 (25) | Nepal |
Finance Protection
Population Coverage Services Coverage |
Services Delivery
Financing |
Free Health Care Policy (FHCP): The FHCP introduced in 2006 abolished user fees in public facilities below the district level. Under this policy, essential health‐care services are provided free of charge to all citizens at health post and primary health centers, and to the targeted groups (ultrapoor, poor, senior citizens, persons with disability, destitute, and female community health volunteers) at the district hospitals.
Safe motherhood policy (Ama program): The Ama program (also called Maternity Incentive Scheme implemented in 2007) provides a universal free delivery service and transportation allowance to women. The providers are paid retrospectively based on defined unit costs. SHI scheme: The Health Insurance Act was enacted on October 11, 2017 laying foundation for an autonomous entity—the National Health Insurance Board—to govern it and making the enrolment mandatory for every citizen both in formal and informal sector. The scheme's major source of revenue comes from contributions from the households (premium) plus complementary funding from the federal, provincial, and local government budget that is primarily targeted to subsidize the poor. The scheme provides partial to full subsidy to different categories of poor. Additionally, the health insurance fund can receive contributions from national and international organizations and foreign governments. The benefit package includes services beyond the existing free services being provided by the government. The benefit package includes promotive, preventive, curative, rehabilitative, and ambulance services within a defined ceiling of USD 500 per head per year per family with a few services excluded. These include plastic surgery, spectacles, and hearing devices beyond a cap price and artificial insemina-tion. 10 Other small‐scale social health protection schemes (viz, uterine prolapse treat-ment, subsidies for heart diseases, kidney disease, and cancer treatment) have also been introduced. |
- Reached population coverage of 5% in the implemented districts in just within a year of implementation.
- The development of the SHI scheme so far is encouraging. |
| Tang Sh, et al, 2012 (26) | China | Finance Protection |
Financing
Resources Gener-ation |
The paper introduces and discusses new initiatives and measures employed to control cost escalation of healthcare in China, including alternative provider payment methods, reforming drug procurement systems, and strengthening the application of standard clinical paths in treating patients at hospitals, and analyses the impacts of these initiatives and measures. Three cities in China (Shanghai, Shenzhen and Mudanjiang) have selected to look at what these cities have done in reforming their provider payment methods in order to tackle the rapid cost escalation of health care, among others. Several emerging initiatives of cost control targeting the supply side of healthcare markets in China and examine their effects have introduced. |
1-Using mixed provider payment methods:
All the three cities have used more than one provider payment method to pay for outpatient and inpatient services. One key message is that, except a few situations, all the three cities have tried to use alternative methods to FFS. The results show that either case-based payment, or using flat unit rate to pay for OP and IP services, or global budget, have produced positive impacts on cost control of health care in the three cities. 2- Separating revenue and expenditure system Under SRES, all the revenues, including incomes from service charges and drug sale, are paid into a special government account, while each service provider will be paid for by the county/district bureau of finance, according to agreed health budgets. The impacts of SRES initiative are on four aspects: 1) changes in health expenditure, 2) changes in quantity of services provided; 3) quality of care, and 4) perceptions of community health workers. The provision of public health interventions/ services has also been improved, as the initiative has a strong mandate to strengthen public health at the community level. 3- Reforming management of pharmaceutical distribution/ procurement systems In order to reduce the drug expenditure as percentage of total health expenditure and unnec-essary use of expensive drugs including antibiotics, the Government of China, with the support from WHO, has taken a series of actions to improve value for money. One major reform was to revise the list of national essential drugs since 2004. 4- Implementing standard clinical treatment path Clinical governance has been one of main challenges in reforming public hospitals in China. |
| Vragas.J.R, et al, 2013 (27) | Cost Rica |
Financial Protection
Population Coverage |
Stewardship
Financing Services Delivery |
This paper explores the implementation and sustenance of universal health coverage (UHC) in Costa Rica, discussing the development of a social security scheme that covered 5% of the population in 1940, to one that finances and provides compre-hensive healthcare to the whole population today. The scheme is financed by mandatory, tri-partite social insurance contribu-tions complemented by tax funding to cover the poor.
The analysis takes a historical perspective and explores the policy process including the key actors and their relative influence in decision-making. Data were collected using quali-tative research instruments, including a review of literature, institutional and other documents, and in-depth interviews with key informants. |
Key lessons to be learned are: 1. Population health was high on the political agenda in Costa Rica, in par-ticular before the 1980s when UHC was enacted and the transfer of hospitals to the social security institution took place. Opposition to UHC could therefore be contained through negotiation and implemented incrementally despite the absence of real consensus among the policy elite
2. Since the 1960s, the social security institution has been responsible for UHC in Costa Rica. This institution enjoys financial and managerial auton-omy relative to the general government, which has also facilitated the UHC policy implementation process. 3. UHC was simultaneously constructed on three pillars that reciprocally strengthened each other: increasing population coverage, increasing availa-bility of financial resources based on solidarity financing mechanisms, and increasing service coverage, ultimately offering comprehensive health ser-vices and the same benefits to every resident in the country particularly before the 1980s, the fruits of economic growth were structurally invested in health and other universal social policies, in particular education and sanita-tion. The social security institution became a flagship of Costa Rica’s na-tional development strategy which reinforced its political importance and contributed to its longer-term sustainability and that of UHC. |
| Zoidze. A, et al, 2013 (28) | Georgia |
Finance Protection
Services Coverage |
- Service Delivery
- Financial |
The present study focuses on the program “Medical Insurance for the Poor (MIP)” in Georgia. Under this program, the gov-ernment purchased coverage from private insurance companies for vulnerable households identified through a means testing system, targeting up to 23% of the total population. The benefit package included outpatient and inpatient services with no co-payments, but had only limited outpatient drug benefits. This paper presents the results of the study on the impact of MIP on access to health services and financial protection of the MIP-targeted and general population.
With a holistic case study design, the study employed a range of quantitative and qualitative methods. The methods included document review and secondary analy-sis of the data obtained through the nationwide household health expenditure and utilization surveys 2007–2010 using the difference-in-differences method. |
MIP had a positive impact in terms of reduced expenditure for inpatient services and total household health care costs, and there was a higher proba-bility of receiving free outpatient benefits among the MIP-insured. However, MIP insurance had almost no effect on health services utilization and the households’ expenditure on outpatient drugs, including for those with MIP insurance, due to limited drug benefits in the package and a low claims ratio. In summary, the extended MIP coverage and increased financial access pro-vided by the program, most likely due to the exclusion of outpatient drug coverage from the benefit package and possibly due to improper utilization management by private insurance companies, were not able to reverse ad-verse effects of economic slow-down and escalating health expenditure. MIP has only cushioned the negative impact for the poorest by decreasing the poor/rich gradient in the rates of catastrophic health expenditure MIP has contributed to an improvement in all three dimensions – population, service and cost coverage, and managed to improve financial protection of the bene-ficiaries that used health services against expenditure related to inpatient care. This, in turn, had a positive impact on financial access indicators for the poorest in the general population, but had limited or no overall effect on utilization of health services and financial protection for the general popula-tion as measured by the incidence of catastrophic health expenditure.
The study results also suggest that the sustained low utilization of health services, particularly primary health care services for the general population including MIP beneficiaries is mainly determined by the limited financial accessibility of outpatient pharmaceuticals. As a result, exclusion of an outpatient drug benefit from MIP benefit package during the first three years of implementation has detrimentally affected the potential impact of MIP on financial protection of the population. There are also indications that im-proper practices employed by the PICs – delayed enrolment and overly aggressive utilization management – may have also contributed to the low utilization at the initial stage of MIP implementation. Alternative approach-es to protecting households experiencing catastrophic health expenditure might need to be explored, most important of which may be the expansion of the MIP benefit package to cover a reasonable outpatient drug benefit that will include coverage of the leading causes of chronic illnesses such as hypertension and other cardiovascular diseases, bronchial asthma, gastroen-terology disorders, etc. Policies for the rationalization of unreasonably high pharmaceutical expenditure should also be pursued. |
| Soranz.D, et al, 2016 (29) |
Portugal
Brazil |
Finance Protection
Population Coverage Services Coverage |
-Stewardship
-Resource Generation -Service Delivery |
In October 2005, Portugal initiated an ambi¬tious PHC reform, based on the Primary Health Care Mission (MCSP), leading to a deep recon¬figuration of Pri-mary Healthcare in Portugal. In January 2006, MCSP published the “Priority Action Lines for the Development of Primary Health Care” in which it dissemi-nates its pro¬posed measures in eight areas of action and sets the way to develop-ing the reform. In the Portuguese reform, a set of strategic lines was elaborated and were clustered in the 2007-2009 strategic plan, namely: Axis I - quali¬ty and organizational change related to issues of leadership and independent manage-ment, im¬proved accessibility, with evaluation and moni¬toring and with the management of information and communication technologies. Axis II - clin¬ical governance and knowledge management addressed issues related to clinical governance, professional qualification and innovative and simplified care deliv-ery. Axis III – sustainability and development associated to issues related to accreditation of services, financial feasibility of primary healthcare and commu-nication with citizens and professionals Solutions pointed out by these Axes encom¬passed professional management, independence, teamwork, demand-oriented culture and pro¬fessional satisfaction and motivation. The chal¬lenges faced by health facility managers were to try to balance efficiency gains with effectiveness gains, manage resources rationally and have costs adequate to objectives, achieve health gains for the community, that is, by the performance of continued quality of service. “Model B” Family Health Facilities were espe-cially established for the development of innovative solutions pro¬posed by these Axes.
The city of Rio de Janeiro began its reform in April 2009, inspired by the Portu-guese Primary Healthcare Reform. Eight strategic axes10 were launched, with specific priorities for each year and recurring processes throughout the reform. Health facilities called “Family Clinics” were es¬tablished and “Model A” Mu-nicipal Health Cen¬ters transformed / physically refurbished to de¬velop the innovative solutions proposed by these Axes. As in Portugal, it was not enough to expand access without increasing primary health care’s resolution. Lisbon and Rio de Janeiro reforms aimed at improving the quality of health care, making them citizen-centered, accessible and efficient, always bearing in mind the need to improve the satisfaction of professionals and users. The modernization and reconfiguration of the Health Centers in both Lisbon and Rio de Ja¬neiro and the establishment of Family Clinics in the latter city were based on a set of principles: (i) community-oriented, with strategies adapted to local needs; (ii) organizational flexibility with self-organization and reduced organic strictness; (iii) leadership and teamwork, with establish¬ment of new competences and knowledge man¬agement; (iv) simplification of care, improving regulation with more trust in the citizen; (v) results-oriented management, with community impact assessment; (vi) contractualisation and evaluation, with definition of goals before the public administration13; (vii) independence and accountability; (viii) continuous improvement of quality as a way of acting. |
In the first half of 2015, 76.84% of users en¬rolled in the Lisbon and Tagus Valley region and 72.49% in the Al-garve region had a family doctor assigned to them. In Rio de Janeiro, in November 2016, it is estimated that 65% of Rio de Janeiro residents already had doctors working in Fam¬ ily Health Teams, except that most of them are un-dergoing a training process to obtain the title of special-ist. In the Lisbon Region, between 2009 and the end of 2015, 931 family doctors physi¬cians retired and 421 new ones joined the system, leading to a deficit of 510 doc-tors.
In Portugal, some patients are still without a family doctor in the family health units, contrary to the principle underlying the establishment of this type of functional unit. This situation occurs predominantly in places with an increasing trend, particularly in the Family Health Units (USF), as a result of retirement or transfer to other func¬tional units without due replacement14. Measures introduced by the Portuguese Min¬istry of Health of the XIX Constitutional Gov¬ernment to respond to the shortage of medical professionals in the General and Family Medi¬cine career, namely (i) opening of proce-dures for the admission of professionals, (ii) recruitment of professionals (Iii) increase of normal working hours of the medical special career from 35 to 40 weekly hours, resulting in (iv) increasing the size of the list of registered users per physician from 1,550 to 1,900 users, and (v) incentives for geographic mobility have not been suffi-cient to achieve a more comprehensive coverage of pri-mary health care provision15. In 2016, in Rio de Janeiro, the lack of family doctors in the labor market or in places of ex¬treme violence occurred between 5 and 10% of the teams. In order to respond to this issue, plan¬ning was done in medical training so that, in 10 years, all team family physicians could have med-ical residency in family and community medi¬cine, by stipulating the following: (i) opening 220 annual resi-dency vacancies; (ii) requesting the Ministry of Health to deploy 101 Cuban family doctors to the most difficult areas; (iii) making workload for 20 or 40 hours flexible, as per the professional’s decision; (iv) keeping an average of 3,200 patients per team; (v) establishing a career plan with incentive for training; (vi) providing an incentive to geographic mobility; and (vii) investing heavily in the improvement of physical structures of the facilities and offices. |
| Somkotra.T, et al, 2008 (30) | Thailand | Finance Protection | - Financing |
This study aimed to measure the pattern of household out-of-pocket payments for health care and to exam-ine the financial catastrophe and impoverishment due to such payments during the transitional period (pre- and post-Universal Coverage policy implementation) in Thailand. This study used the nationally repre-sentative Socioeconomic Surveys in 2000 (pre-UC), 2002, and 2004 (post-UC), which contained data from 24747, 34758 and 34843 individual households, respectively.
Data were taken from the nationally representative household socioeconomic survey (SES) of Thailand in 2000, 2002 and 2004, which were conducted by the National Statistical Office (NSO). The SES2000 represented the pre-UC period in this study, and the SES2002 and SES2004 represented the post-UC period. The SES contained information on household income and consumption expenditures such as those for food and other goods and services, including out-of-pocket payments for health care. To achieve the purposes of this study, the total household consumption was adopted as one of the main measures of living standards. An equivalence scale was applied to household consumption to derive the household consumption per equivalent adult, which was then used to rank households into household quintiles. In addition, the non-food consumption, defined as total household consumption minus food consump-tion expenditure, was used as the alternative measure of living standards. Households. The methodology used in this study to measure the catastrophic payments for health care was based on the concept proposed by Wagstaff and van Doorslaer. We set various catastrophic thresholds to improve the robustness of the trends and findings as other previ-ous studies have. This study used 5%, 10% and 15% of total consumption and 20%, 25% and 30% of non-food consumption as the thresholds. |
Before the UC policy implementation, the ratio of out-of-pocket payments for health care as share of total household consumption between households in the richest quintile and the poorest was 1.4, but, after the UC policy implementation, the ratios increased.
The concentration indices of out-of-pocket payments for health care as share of household resources, either total household consumption or non-food consumption, are mostly positive. The rich households are more likely to spend for health care from their own re-sources than are the poor households. The trends of out of pocket payments for health care as share of the total household consumption or non-food consumption decline from pre-UC to post-UC, particular-ly among households that belong to the 1st and 2nd quintiles. Using the total household consumption and non-food consumption as the basis for defining the threshold to measure catastrophic payments for health care, the analysis shows a declining trend of the incidence of catastrophic payments for health care between the pre- and post-UC period. The concentration index of households that incurred catastrophic payments (CE) is also computed in order to shed light on whether the poor or rich households exceed-ed the threshold. Most of the CE are positive at various thresholds, indicating the greater tendencies for the rich households to incur catastrophic payments for health care. The concentration indices of the catastrophic overshoot (CO) generally display similar patterns as the concentration indices for households that incurred cata-strophic payments (CE). The COs are positive regardless of pre- or post-UC and, for all thresholds, indicating that large excess payments are concentrated among the rich households. Consequent-ly, the rank weighted gaps are smaller than the unweighted gaps, particularly in the post-UC period. The distribution of the incidence and intensity of catastrophic payments for health care against the threshold of 10% of total household consumption and 25% of non-food consumption across household quintiles in the urban and rural settings, respec-tively. Both thresholds of defining catastrophic payments for health care reveal similar patterns in terms of the incidence and intensity of catastrophic payments. The distribution of the incidence and intensity of catastrophic payments across quintiles reveal an increasing trend from the poorest to the richest. After the UC policy implementation, the incidence and intensity of catastrophic payments decrease particularly among the lower quintiles (Q1 and Q2). The pre-payment poverty headcount shows that the poverty headcount in Thailand has gradually decreased between 2000 and 2004. After subtracting the out-of-pocket payments for health care, the post-payment poverty headcount increased by 1.23% in pre-UC. Although the same pattern is observed in post-UC, the increases in both SES2002 and SES2004 are smaller as the post-payment poverty headcount increased by only 0.7% and 0.58%, respectively. The proportion of almost-poor households, defined as households whose total household consumption lies between 100% and 120% of their official poverty thresholds that become poor households after subtracting the out-of-pocket pay-ments for health care decrease from pre-UC to post-UC by 1.01% in 2000 to 0.62% and 0.49% in 2002 and 2004, respectively. After the UC policy implementation, the poverty impact of headcount decreased gradually in each region whether urban or rural area. The poverty gap and the normalized poverty gap also decrease. |
| Santoz,L.M.P, et al, 2016 (31) | Brazil |
Population Coverage
Services Coverage |
-Resource Generation |
The aim of this study was to evaluate the implementation of a program to provide primary care physicians for remote and deprived populations in Brazil.
The Mais Médicos (More Doctors) program was launched in July 2013 with public calls to recruit physicians for priority areas. Other strategies were to increase primary care infrastructure investments and to provide more places at medical schools. A quasi-experimental, before-and-after evaluation of the implementa-tion of the program has conducted in 1708 municipalities with populations living in extreme poverty and in remote border areas. We compared physician density, primary care coverage and avoidable hospitalizations in municipalities enrolled (n = 1450) and not enrolled (n = 258) in the program. Data extracted from health information systems and Ministry of Health publications were analyzed. |
By September 2015, 4917 physicians had been added to the 16 524 physicians already in place in municipalities with remote and deprived populations. The number of municipali-ties with ≥ 1.0 physician per 1000 inhabitants doubled from 163 in 2013 to 348 in 2015.
Primary care coverage in enrolled municipalities (based on 3000 inhabitants per primary care team) increased from 77.9% in 2012 to 86.3% in 2015. Avoidable hospitalizations in enrolled municipalities decreased from 44.9% in 2012 to 41.2% in 2015, but remained unchanged in control municipal-ities. We also documented higher infrastructure investments in enrolled municipalities and an increase in the number of medical school places over the study period. |
| Shibuya.k, et al, 2011. (32) | Japan |
Finance Protec-tion
Population Coverage |
-Stewardship
Finance Protection -Service Delivery |
Four major reforms have proposed to assure the sustainability and equity of Japan’s health ac-complishments in the past 50 years.
1. Implement a human-security value-based reform •Apply the notion of human security with increased pro activeness to Japans domestic policies. •Refine governmental health policies in medical education, system monitoring, and assessment from the people-center perspective. •Maintain the basic structure of compulsory enrolment in the social health insurance plan, based on the underlying value attached to equity in Japanese society. •Use good-quality research and scientific evidence to frame key choices in local, national, and global decision making. 2. Redefine the role of central and local governments •Transfer the authority and responsibility for improving the efficiency of allocation of Health-care resources and sustainability of funding to prefectural governments. •Consolidate fragmented agencies and institutions (eg, Japanese version of the Institute of Medi-cine, Centers for Disease Control and Prevention, and National Institutes of Health). •Reconstruct health systems in Tohoku area damaged by the Great East Japan. Earthquake as the test case for future reforms based on human security. 3. Improve the quality of health care •Build clinical databases to certify subspecialties to improve quality of physicians •Establish general practice as an official subspecialty for patient-center seamless care. •Monitor performances with mandatory reports for benchmarking •Enable functional differentiation and the establishment of referral networks in clinics and hospi-tals. 4. Commit to global health • Provide opportunities for domestic and global health experts to interact • Mobilise Japan’s accumulated knowledge, especially of the universal coverage, ageing and long-term care, and health and wellbeing for the past 50 years in the global health context. |
---- |
| Raj Adhikari (2018) (33) | Nepal | Services Cover-age | -Resource Generation | exploring availability, expiry, and stock-out duration of 17 key essential medicines at both pub-lic and private health facilities |
Stock of medicines and expired medicines in public sector:
1-Primary healthcare centers (PHCCs): 91.59 (stock)-0.89 % (expired). 2-Health posts (HPs): 96.42-3.04% 3-Sub Health posts (SHPs):98.2-2.55% |
| Ayub, A, et al. (2018) (34) | Pakistan |
Finance Protec-tion
Population Coverage |
Finance
-Service Delivery |
There is a plan named Sehat Sahulat Program (SSP) which was implemented in KP (name of a state in Pakistan) in two different phases in order to cover the 51% of the population financially and through the accessibility of care. The entire program covers all secondary and limited tertiary services. The maximum expenditure per family annually is 540000 Rs. Which is subsidized by a premium of 1549 Rs. |
Phase 1- covers 4 districts with a total fund of 13.4k $. It’s planned for 5 years and covers 21% of the poor poorest popu-lation.
Inpatient, maternity and all secondary services are covered ignoring the tertiary services. Phase 2- covers 26 districts with coverage of 51% of total poorest population. It’s planned for 2 years and is funded for 51.6k $. Treatment for diabetes complications, cancer treatment, treat-ing organ failure, admission for HCV&HBV complications, cardiovascular conditions like hypertension, emergencies and management of cerebrovascular are added up either. Tertiary services are covered to some extent. |
| Aantjes, C, et al. (2015) (35) | Zambia |
Finance Protection
Population Cover-age |
-Stewardship
Finance |
All three governments who had the power, stuck to the policy ensuring equitable care and reduction of the disparities.
There was integration between disease program in primary services and environmental health like water sanitation. Lower income due to economic stagnation has ended up in a deduction in health budget per capita. -Community-oriented palliative services were taken into action to cover up the gap produced by economic stagnation. -Donor funding formed 11% of the country’s health budget in 1995 and 38% in 2011. -Free anti-retroviral for HIV patients in hospitals -Under the Ouagadougou declaration, 650 health centers were estab-lished. -User fees were abolished for PHC in urban health facilities and prom-ulgated a new national health policy. -Increase in social welfare budget from a total of 30 to 40 million to 199 million (country’s currency)- also in 2011 the country reached a spend-ing of 15% on budget which was increased to 16% in 2014 Different authoritative and structural changes were implemented like decentralizing and transferring the power to domestic levels, integra-tions and alignments in duties and goals. |
- Also poor services are not recommended as an alternative to the high quali-ty services when there are equity considerations. Having a narrowed prioriti-zation can lead to inequity, so it is not suggested too.
- Has earmarked the total budget up to 75% in order to cover the district health which was disproportionally consumed within hospital before. - Zambia reached UC for anti-retroviral treatment in 2012 covering 450000 individuals from a total of 520000 due to decentralizing ART to PHC clin-ics. |
| Adams, A, et al. (2013) (36) | Bangladesh |
Population Cover-age
Service Coverage |
Financing
-Service Delivery |
Pro-poor and women-focused investments in health and social devel-opment such as the Expanded Program on Immunization, family plan-ning, female education subsidies, and women’s microcredit have con-tributed to some gains in different areas like child mortality, antenatal care, skilled birth attendant, complete immunization, modern family planning methods, oral rehydration therapy, acute respiratory infection treatment, composite coverage index also in total fertility rate. |
From 1993 to 2011,
1-there was absolute difference in child mortality by asset quintile for each group: infants (45 in 1993, 32 in 2011)- the children (51 in 1993, 9 in 2011)- the U5 (89 in 1993, 40 in 2011) 2-child mortality by gender for each group, shortfall inequality (the differ-ence between the expected and actual ratio): infants (45 in 1393, 32 in 2011)- the children (51 in 1993, 9 in 2011)- the U5 (89 in 1993, 40 in 2011) 3-The relative difference between economical quintile 5 (Q5) and quintile 1 (Q1) for each indices was (Q5:Q1): Antenatal care: 4.4 in 1993, 1.9 in 2011 Skilled birth attendant: 10.0 in 1993, 5.5 in 2011 Modern family planning methods: 1.5 in 1993, 1.2 in 2011 Oral rehydration therapy: 1.2 in 1993, 1.0 in 2011 Acute respiratory infection treatment: 2.2 in 1993, 1.2 in 2011 Composite coverage index: 1.7 in 1993, 1.3 in 2011 4- The difference in TFR in the all districts varies around 0.1 to 2.0, with a special concentration on the eastern districts. This show a dramatic im-provement in TFR due to higher levels of primary school attendance, child mortality, delivery assistance by skilled attendants, and access to an im-proved water source. |
| Agustina, R, et al. (2018) (37) | Indonesia |
Finance Protection
Population Cover-age Service Coverage |
-Stewardship
Financing -Service Delivery |
There are three main stages mentioned in the article:
From 1960 to 2001: a centralized health system was in Indonesia Decentralization of governance to 354 districts in 2001 and then to 514 ones. The UHC system introduced in 2014 concentrated on flexible and adaptive implementation features and quick evidenced-driven deci-sions based on changing needs. |
1- 2090 primary health centers were built. Life expectancy improved from 48 to 69 years and IMR decreased from 76 per 1000 to 23 per 1000 deaths. TFR decreased from 5.61 to 2.11 due to the first stage.
2- Increase in health system heterogeneity and exacerbated equity gaps because of the second phase. 3- The largest single-payer system in the world and covers 203 million people. Entirely, from 2014 to 2017: Outpatients (million): 66.8 to 150.3 Health facilities: 18437 centers to 21763 Referral outpatients (millions): 21.3 to 64.4 Inpatients (million): 4.2 to 8.7 Health facilities (advanced medical treatment): 1681 to 2268 National health system insurance memberships (million): 133.42 to 187.98 Revenue from premium collection (in $2011 PPP billion): 10.08 to 17.72 Expenditure for health-care services (in $2011 PPP billion): 10.50 to 20.15 |
| Akashi, H, et al. (2015) (38) | Japan |
Population Coverage
Quality |
Stewardship
Resources Generation |
Four phases of HRH (human resources in health) development in Japan health system:
First, there was an absolute shortage in HR. Second, rapid production of low-educated HR whom experienced relaxed admission require-ments, shorter education periods, and increase in the numbers of educational facilities before introducing UHC Third, included introduction of quality improvement procedures through “national licensing examination". This was the stage that the system introduced UHC with improvements in health-related indicators. Forth, characterized by a predominance of formal health professionals. |
some health indicators improved such as the mortality rates for Pneumonia or tuberculosis. However, there was a debate whether the increases in the health workforce were responsible for these improvements? Since, streptomycin, chest X-rays, improved nutri-tion, etc. were introduced during that time, which contributed to a reduction in tuberculosis in Japan. |
| Akhnif, E, et al. (2018) (39) | Six African countries | ------- | Stewardship | To audit the ‘UHC systems’ to assess to what extent they function as “learning systems” toward UHC using an assessment tool specified for this purpose. All of the six countries scored their readiness between 4 to 5 which confirms the feasibility and relevance of adapting the learning organization framework to UHC Systems. |
Learnt lessons:
1. Participating the UHC actors in the evaluation process increase the chance of corrective collective actions in the follow-up of the assessment. 2. In Morocco, the creation of an inter-ministerial Steering commit-tee for UHC allowed a strategic positioning of the UHC agenda at the level of the government. 3. Burkina Faso shows that even low-income countries can build strong learning ecosystems |
| Alkenbrack, S, et al. (2013) (40) | Lao PDR |
Finance Protection
Population Coverage Quality |
Financing |
The prospects of expanding enrolment of CBHI (community-based health insurance) were examined using two distinct approaches.
In this study, household-level findings indicate that the better-off, individuals suffering an illness, and less risk-averse are most likely to enroll in insurance. Besides, poor quality of care obstructs the way to participate in such scheme. The main target group in CBHI is households that are self-employed or those who are active in the informal sector that are not covered by any of the other insurance organizations. Insurance membership is at the household level, and premiums vary depending on the city or village and the number of household members. Participation rates were about 2.5% to 3% of household income and were either monthly collected by the rural collector or paid to the fund manager at the district hospital. |
Increase coverage of poor people and self-employed or those who are active in the informal sector |
| Amaya, J, L, et al.(2016) (41) | Colombia | Finance Protection | Financing | The system classifies the population on a scale from 1 to 6 according to their economic wel-fare, determined based on access to public services, possession of durable goods, allocation of human capital, and current income. |
Lessons learnt:
People care much more about healthcare benefits and family coverage than health insurance costs. |
| Andrade, V,M, et al. (2018) (42) | Brazil |
Finance Protection
Population Coverage |
Financing
-Service Delivery |
Family Health Strategy is the primary healthcare program in Brazil,
11 indicators from different municipalities has been assembled and analyzed to recognize the pace of utilization and rate of expansion. The differentiating early and late adopter of the program were supply of doctor and population density. Sustained coverage expansion was considerably related to the population size and marginal benefits of the program and also doctor supply. The expansion of the utilization had no specific pattern and was completely heterogeneous in the state and municipal level. The economic development was not the main determinant of the uptake. |
Lessons learnt:
First, the funding mechanism is critical for program implementation, and must be accompanied by ways to support the supply of primary care physicians in low density areas. Second, in more developed and bigger areas the main challenge is lack of incentives to pursue universal coverage, especially due to the availability of private insurance. Third, population size is a crucial element to guarantee coverage sustainability over time. |
| Asaria, M, et al. (2016) (43) | England |
Finance Protection
Service Coverage Quality |
Financing
-Service Delivery |
In 2003 the UK Government made reducing health inequality a priority for the NHS in Eng-land, as part of a cross governmental strategy with explicit national targets for reducing health inequality by 2010.
Policy explanation: (1) major investments in primary care supply and quality from 2004, including the world’s largest primary care pay-for-performance program (2) targeted investment in primary care supply in under doctored areas of the country from 2008 (3) National guidance and support for effective primary care interventions for chronic condi-tions in disadvantaged adults from 2007 to 2014. |
From 2004/2005 to 2011/2012:
1- Socioeconomic inequalities in both primary care supply (PCS) relative to need and primary care quality (PCQ) decreased substan-tially in absolute and relative terms. 2-inequality in primary care supply eliminated and inequality in primary care quality nearly eliminated 3-PCS relative inequality -2% and PCQ relative inequality 1%: deprived to less-deprived areas 4-relative inequality for preventable hospitalization was 106% and for amenable mortality 57%: deprived to less-deprived areas |
| Asfaw, E, et al. (2014) (44) | Ethiopia |
Finance Protection
Quality |
-Service Delivery | This study aimed to measure patient satisfaction with task shifting of antiretroviral services in hospitals and health centers in four regions of Ethiopia. | -------- |
| Atun, R, et al. (2013) (45) | Turkey |
Finance Protection
Service Coverage Quality |
Financing
Stewardship Resources Generation -Service Delivery |
Turkey’s health transition plan. Includes:
- Contract-based employment introduced for healthcare personnel in rural and less developed regions. -changes to pricing and to value-added tax in pharmaceutical field -Patient Rights Directive introduced -Hospitals belonging to the Social Insurance Organization (146 hospitals) inte-grated with Ministry of Health hospitals. -Contract-based family medicine issued -Social Security Institution established as a single organization for financial pooling and purchasing -National air ambulance service -Cost-sharing in private hospitals for complex conditions -Mobile pharmacy services 2-Turkey’s 5 health insurance organizations integration |
Effects for item 1: enhance equity substantially- increased user satisfaction- better financial protection
Effects for item 2:increased the insurance coverage for poorest population from a 2.4-million-people population in 2003 to a 10.2-million –people one in 2013.Also, access and use of key maternal and child health services improved to help substantially reduce under-5, infant, and neonatal mortality, especially for socioeconomically disadvantaged households. |
| Atun, R, et al. (2015) (46) |
Argentina
Brazil Chile Colombia Costa Rica Mexico Peru Uruguay Venezuela |
Finance Protection
Service Coverage population Coverage Quality |
Stewardship
Resources Generation -Service Delivery Financing |
There were different reforms and programs which can be assessed through the following statements:
Health as a human right and citizens’ entitlement Regulation of health-care insurers and providers Expanding insurance coverage for uninsured citizens through budget transfers Comprehensive primary health care: the platform for universal health coverage |
Between 1990 to 2011 and through all 9 countries:
-A constant decrease in Under-5 mortality rate and infant mortality rate and a considerable decrease in maternal mortality rates. Also, there were constant increase in insurance and health coverage of the population. Quality of care and safety of the delivered services were boosted. |
| Aungkulanon, S, et al. (2016) (47) | Thailand | Service Coverage | -Service Delivery |
Thailand UHC program:
There was a significant decrease in overall mortality rate which was due to the reduction of inequality of HIV mortality in adults aged 15-44 years in the north region of Thailand. These improvements are followed by successful implementa-tion of HIV prevention program (vertical prevention from mother to child) and high coverage of universal access to antiretroviral treatment (ART) from HIV. The improvements in the benefits package were another influential factor contrib-uting to UHC. |
|
| Baine, O, S, et al.(2018) (48) | Uganda |
Finance Protection
Service Coverage Quality |
-Service Delivery
Financing |
Kisiizi Hospital Health Insurance scheme is an insurance program to improve access to health services, and provide a reliable source of funding and reduce bad debts to Kisiizi hospital through forming “Engozi Societies”
Results: -Compulsory insurance scheme memberships were posed on e-societies’ members - Kisiizi hospital health insurance scheme covered only health services obtained from Kisiizi hospital. - The scheme offered no exemption, credit and referral facilities - Premiums are paid inside the organized societies for members from savings and offered them loans |
-Membership increased from 330 in 1996 to 38,400 fami-lies in 2017
- The following scheme provided a stable source of funding and reduced bad debts to the hospital. |
| Ballart, X and Fuentes G, (2018) (49) | Uruguay |
Finance Protection
Service Coverage Quality |
-Service Delivery
Financing |
A reform in the health system with the aim of regaining the control of services provision by the state including:
- change in orientation from a system that was hospital centered, to a system that is oriented towards community health and preventive medicine based on the devel-opment of primary care - Creation of the National Health Fund and the National Health Insurance. - Formal workers and employers contribute to the National Health Fund based on their salary level. - Insured citizens have the option to change providers after being at least 3 years with one provider. - Uninsured citizens receive health services from the public provider |
People would rather take insurance services from private insurers and third parties than public sector, as the number of people covered in 2014 was 63 comparing to 2000 with a 47.5 percent.
Number of people insured by National Health Insurance increased from 0.5 million to 2.5 million. OOP was lower in Uruguay (16%) comparing to Brazil (25%1) and Mexico (44%) by 2014 Good for those health systems having difficulties with their quality of healthcare |
| Barasa, E, et al.(2018) (50) | Kenya |
Finance Protection
Population Coverage |
-Service Delivery
Financing |
Develops a summary measure of UHC for Kenya and track the country’s pro-gress between 2003 and 2013.
Financial reforms were in two main categories: 1-User fees: by 2013, user fees were completely abolished in health centers and dispensaries. A free maternity program was introduced that removed user fees for deliveries in all public facilities 2-Health insurance: National Health Insurance Fund was established. Then by 2015, the NHIF Act was amended to revise premiums upwards. The NHIF expanded its benefit package from inpatient only, to include outpatient ser-vices. |
Services coverage increased from 27.65% (27.13%–28.14%) in 2003 to 41.73%.
Financial risk protection reduced from 69.82% (69.11%–70.51%) in 2003 to 63.78% (63.55%–63.82%) in 2013. The weighted summary measure of UHC increased from 43.94% (95% CI 43.48% to 44.38%) in 2003 to 51.55% (95% CI 51.29% to 51.82%) in 2013. |
| Barasa, E, et al. (2018) (51) | Kenya |
Finance Protection
Population Coverage Service Coverage Quality |
Financing
Stewardship |
Policies Content:
(1) the introduction of the Civil Servants Scheme (CSS) (2) the introduction of a stepwise quality improvement system (3) the health insurance subsidy for the poor (HISP) (4) revision of monthly contribution rates and expansion of the benefit package (5) the upward revision of provider reimbursement rates |
There are improvements in several areas including equity, efficiency, feasibility, and sustainability:
-The number of Kenyans (principal members plus benefi-ciaries) enrolled in the NHIF increased from about 2.7 million in 2010 to 6.6 million in 2017. -administrative costs as a share of total revenues were reduced from 42% to 22% and the benefit payout ratio increased from 52% to 75% between 2010 in 2017. -though population coverage by the NHIF has increased, it remains considerably low at 14%. -Though the NHIF has doubled its revenue collection, this amounted to only 5% of Kenya’s total health ex-penditure. -Though the NHIF has reduced its administrative costs by half, at 22% the NHIF is still highly inefficient. |
| Barber, S, L, et al. (2013) (52) | China |
Finance Protection
Service Coverage Quality |
Financing
Stewardship Service Delivery |
1-Essential medicines lists issued at primary care centers.
2-Insurance reimbursement lists, which include the medicines on the EML, at higher reimbursement rates. 3-Centralized procurement and bidding platforms implemented in order to reduce the number of distributors and mark–ups in the distribution chain. 4-Setting and adjusting guiding retail prices for essential medicines. 5-Essential medicines are provided at cost (zero profit mark–up) at all govern-ment–run primary care facilities in urban and rural areas. 6-Quality, electronic bar codes required on pack ages for monitoring. Also, strengthened systems for adverse drug effects were established. 7-Rational medicines use, Clinical treatment guidelines and formularies of essential medicines formulated and issued, and prescription monitoring sys-tems put into place. |
-Essential medicines available at primary care facilities at cost.
-Prices for essential medicines have been reduced -Price transparency has been resulted. -Greater protection through quality standards for con-sumers. -Increased knowledge of rational medicines use |
| Bayarsaikhan, D, et al. (2015) (53) | Mongolia |
Finance Protection
Population Coverage |
Financing
Stewardship |
Mongolia introduced mandatory health insurance with a single national insur-ance pool. The Government chose to fully subsidize health insurance contribu-tions for low-income and vulnerable populations, such as the elderly, children, students, and those covered by social assistance programmers.
As the program developed the state separated financing from the provision of health services. The “Fee for service” for out-patient services and the “bed day” tariffs for in-patient care were adopted. To reduce the adverse economic incen-tives facing providers, prospective payments in form of a global budget were issued. Mongolia introduced case-based payments for in-patient services in 2006. |
By 2014, Mongolia almost reached 100% coverage. |
| Bredenkamp, C, et al. (2015) (54) |
China
Indonesia Philippines Thailand Vietnam |
Finance Protection
Population Coverage Service Coverage Quality |
Financing
Stewardship Service Delivery |
There are 3 main challenges that these countries each, address in a particular way. These challenges are:
1-Covering the informal sector. 2-Deciding which benefits to include in the package and how to update it. 3-Supply-side readiness: there are large variations and inequities in the supply-side readiness |
Thailand’s experience propose a much easier and quicker approach to achieve high levels of coverage among the informal sector that is to link coverage with citizenship or national residence, and to enroll the whole (as op-posed to only the poor) informal population using general government revenues.
Similarly, Thai’s health system provides a more comprehensive benefit package especially for poor which include high-cost medical treatments like kidney transplant. |
| Campbell, J, et al. (2013) (55) |
Ghana
Mexico Thailand Brazil |
Finance Protection
Service Coverage Quality |
Financing
Stewardship Service Delivery Resource Generation |
There are 4 dimensions of human resource for health (HRH) development which should be considered on the way to UHC,
Availability, Accessibility, Acceptability, Quality. Every country has experienced different processes and programs regarding each dimension in different sections of time: Ghana: 1) High Impact Rapid Delivery (HIRD) approach. 2)increase production of health workers focusing on mid-level health cadres (medical assistants, physician assistant, midwives etc.) 3) implement strategies for equitable distribution and retention of staff; implement comprehensive conditions of service for all health workers; improve and decentralize HRH management functions.4) Ministry of Health adopts its gender policy to reduce gender barriers in access to health care. 5) Improve performance management with corresponding rewards (incentives) and sanctions; improve human resource information systems, establishment of postgraduate medical college; strengthening regulatory bodies to promote effective legislation. Mexico: Establishment of National Commission for the Regulation of Trade in Human Resources in the Federal States (CNRCRHEF). Thailand: 1) One District, One Doctor (ODOD) Program 2) Special monthly allowance introduced for long services in district hospitals. 3) Special track for Muslim women in three southern provinces for nursing education and postings in their home towns to serve rural Muslim communities. 4) Healthcare Accreditation Institute (public organization) established by law, responsible for quality improvement. Brazil: 1) ProgeSUS: capacity building in health management. 2) UNA-SUS: distance learning program for SUS. 3) PRO-SAÚDE: bridging gaps between HRH and primary health care needs. 4) PET-Sauce: integration of education, services and communities. |
Lessons learned:
First, success in awarding adequate priority to HRH depends on political leadership and commitment. Second, strategies and actions in each of the AAAQ dimensions of HRH have brought about improvements in quality of care and effective coverage and these have resulted in better health outcomes. Third, the successes seen in the four countries examined in this paper reflect achievements made possible through partnerships in and outside the health sector. |
| Gerald Bloom (2016) (56) | Japan |
Finance Protection
Service Coverage |
Stewardship
Financing |
Three strategic decisions were made during the healthcare modernization in Japan.
It facilitated the development of primary healthcare services: it provided opportunities for established practitioners to integrate in the organized healthcare system during a gradual transition to Western medicine; it limited the supply of hospitals and gave them little public funding and it involved the Japan Medical Association, which was dominated by clinicbased physicians, in establishing a fee schedule that favored primary healthcare. |
3 lessons are learnt:
1-Integrate Existing Providers of Primary Healthcare Services into the Organized Health System. 2-Limit Government Commitment to Finance Hospital Services 3- Empower Providers of Primary Healthcare Services to Ensure That Their Livelihoods Reflect Their Importance to Health and Health Services |
| Abuya, T, et al. (2017) (57) | Kenya | Finance Protection | Financing |
-Moving from FMS (free maternity services) to NHIF (National Health Insurance Fund) using different programs during a long period of time:
1-10/20 program, a fee of 10 shillings at dispensaries and 20 shillings at health centers to register clients with a maternity card. 2-NHIF program (not achieved) 3-Selling vouchers, these vouchers were sold for $2 and specifically targeted poor women, as determined by a standardized poverty grading assessment administered to each potential user. (a successful program). 4-Working on HCF strategies with 4 pillars |
The transfer is a mechanism of achieving UHC, eliminating dependency on free services, and encouraging people to take responsibility of their health.
(According to the interviews the process is a meaningful way of achieving UHC). |
References
- 1.Chan WY, Fung IM, Chan E. Universal Health Coverage through Community Nursing Services: China vs. Hong Kong. Revista latino-americana de enfermagem doi: 10.1590/1518-8345.1664.2838. [DOI] [PMC free article] [PubMed]
- 2.Cheng SH, Chen CC, Tsai SL. The impacts of DRG-based payments on health care provider behaviors under a universal coverage system: a population-based study. Health Policy. 2012:202. doi: 10.1016/j.healthpol.2012.03.021. [DOI] [PubMed]
- 3.de Andrade, Pellegrini Filho, Solar O, Rigoli F, de Salazar, Serrate PC. et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. Lancet. 2015:1343. doi: 10.1016/S0140-6736(14)61494-X. [DOI] [PubMed]
- 4.Edward A, Branchini C, Aitken I, Roach M, Osei-Bonsu K, Arwal SH. Toward universal coverage in Afghanistan: A multi-stakeholder assessment of capacity investments in the community health worker system. Social science & medicine (1982) 2015 doi: 10.1016/j.socscimed.2015.06.011. [DOI] [PubMed]
- 5.Frenk J, Gomez-Dantes O. Health Systems in Latin America: The Search for Universal Health Coverage. Archives of medical research. 2018:79. doi: 10.1016/j.arcmed.2018.06.002. [DOI] [PubMed]
- 6.Frenk J, Gomez-Dantes O, Knaul FM. The democratization of health in Mexico: financial innovations for universal coverage. Bulletin of the World Health Organization. 2009:542. doi: 10.2471/BLT.08.053199. [DOI] [PMC free article] [PubMed]
- 7.Garchitorena A, Miller AC, Cordier LF, Ramananjato R, Rabeza VR, Murray M. et al. In Madagascar, Use Of Health Care Services Increased When Fees Were Removed: Lessons For Universal Health Coverage. Health affairs (Project Hope) 2017:1443. doi: 10.1377/hlthaff.2016.1419. [DOI] [PubMed]
- 8.Garg S. Universal health coverage in India: Newer innovations and the role of public health. Indian journal of public health. 2018:167. doi: 10.4103/ijph.IJPH_221_18. [DOI] [PubMed]
- 9.He AJ, Wu S. Towards Universal Health Coverage via Social Health Insurance in China: Systemic Fragmentation, Reform Imperatives, and Policy Alternatives. Applied health economics and health policy. 2017:707. doi: 10.1007/s40258-016-0254-1. [DOI] [PubMed]
- 10.Hongoro C, Rutebemberwa E, Twalo T, Mwendera C, Douglas M, Mukuru M. et al. Analysis of selected policies towards universal health coverage in Uganda: the policy implementation barometer protocol. Archives of public health = Archives belges de sante publique. 2018 doi: 10.1186/s13690-018-0258-4. [DOI] [PMC free article] [PubMed]
- 11.Hughes D, Leethongdee S. Universal coverage in the land of smiles: lessons from Thailand’s 30 Baht health reforms. Health Affairs. 2007:999. doi: 10.1377/hlthaff.26.4.999. [DOI] [PubMed]
- 12.Kingue S, Rosskam E, Bela AC, Adjidja A, Codjia L. Strengthening human resources for health through multisectoral approaches and leadership: the case of Cameroon. Bulletin of the World Health Organization. 2013:864. doi: 10.2471/BLT.13.127829. [DOI] [PMC free article] [PubMed]
- 13.Knaul FM, Frenk J. Health insurance in Mexico: Achieving universal coverage through structural reform - A 2003 reform is making good progress toward covering Mexico's eleven million uninsured families by 2010. Health Aff. 2005:1467. doi: 10.1377/hlthaff.24.6.1467. [DOI] [PubMed]
- 14.Knaul FM, Gonzalez-Pier E, Gomez-Dantes O, Garcia-Junco D, Arreola-Ornelas H, Barraza-Llorens M. et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012:1259. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed]
- 15.Limwattananon S, Neelsen S, O'Donnell O, Prakongsai P, Tangcharoensathien V, van Doorslaer. et al. Universal coverage with supply-side reform: The impact on medical expenditure risk and utilization in Thailand. J Public Econ. 2015
- 16.Long SK. On the road to universal coverage: impacts of reform in massachusetts at one year. Health affairs (Project Hope) 2008:w270. doi: 10.1377/hlthaff.27.4.w270. [DOI] [PubMed]
- 17.Lu C, Chin B, Lewandowski JL, Basinga P, Hirschhorn LR, Hill K. et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS ONE. 2012:e39282. doi: 10.1371/journal.pone.0039282. [DOI] [PMC free article] [PubMed]
- 18.Lu JFR, Chiang TL. Developing an adequate supply of health services: Taiwan's path to Universal Health Coverage. Soc Sci Med. 2018 doi: 10.1016/j.socscimed.2017.12.017. [DOI] [PubMed]
- 19.Maluka S, Chitama D, Dungumaro E, Masawe C, Rao K, Shroff Z. Contracting-out primary health care services in Tanzania towards UHC: how policy processes and context influence policy design and implementation. International journal for equity in health. 2018:118. doi: 10.1186/s12939-018-0835-8. [DOI] [PMC free article] [PubMed]
- 20.Meng Q, Xu L. Monitoring and Evaluating Progress towards Universal Health Coverage in China. PLoS Med. 2014 doi: 10.1371/journal.pmed.1001694. [DOI] [PMC free article] [PubMed]
- 21.Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S. et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012:126. doi: 10.1016/S0140-6736(12)60357-2. [DOI] [PubMed]
- 22.Nuñez PA, Fernández-Slezak D, Farall A, Szretter ME, Salomón OD, Valeggia CR. Impact of universal health coverage on child growth and nutrition in Argentina. Am J Public Health. 2016:720. doi: 10.2105/AJPH.2016.303056. [DOI] [PMC free article] [PubMed]
- 23.Obermann K, Jowett M, Kwon S. The role of national health insurance for achieving UHC in the Philippines: a mixed methods analysis. Global health action. 2018:1483638. doi: 10.1080/16549716.2018.1483638. [DOI] [PMC free article] [PubMed]
- 24.Okech TC, Lelegwe SL. Analysis of Universal Health Coverage and Equity on Health Care in Kenya. Global journal of health science. 2015:218. doi: 10.5539/gjhs.v8n7p218. [DOI] [PMC free article] [PubMed]
- 25.Pokharel R, Silwal PR. Social health insurance in Nepal: A health system departure toward the universal health coverage. The International journal of health planning and management. 2018 doi: 10.1002/hpm.2530. [DOI] [PubMed]
- 26.Tang S, Tao J, Bekedam H. Controlling cost escalation of healthcare: making universal health coverage sustainable in China. BMC public health. 2012 doi: 10.1186/1471-2458-12-S1-S8. [DOI] [PMC free article] [PubMed]
- 27.Vargas JR, Muiser J. Promoting universal financial protection: a policy analysis of universal health coverage in Costa Rica (1940-2000) Health Res Policy Syst. 2013 doi: 10.1186/1478-4505-11-28. [DOI] [PMC free article] [PubMed]
- 28.Zoidze A, Rukhazde N, Chkhatarashvili K, Gotsadze G. Promoting universal financial protection: Health insurance for the poor in Georgia - a case study. Health Research Policy and Systems. 2013 doi: 10.1186/1478-4505-11-45. [DOI] [PMC free article] [PubMed]
- 29.Soranz D, Pisco LAC. Primary health care reform in the cities of Lisbon and Rio de Janeiro: Context, strategies, results, learning and challenges. Cienc Saude Coletiva. 2017:679. doi: 10.1590/1413-81232017223.33722016. [DOI] [PubMed]
- 30.Somkotra T, Lagrada LP. Payments for health care and its effect on catastrophe and impoverishment: experience from the transition to Universal Coverage in Thailand. Social science & medicine (1982) 2008:2027. doi: 10.1016/j.socscimed.2008.09.047. [DOI] [PubMed]
- 31.Santos LMP, Oliveira A, Trindade JS, Barreto ICHC, Palmeira PA, Comes Y. et al. Implementation research: Towards universal health coverage with more doctors in Brazil. Bulletin of the World Health Organization. 2017:103. doi: 10.2471/BLT.16.178236. [DOI] [PMC free article] [PubMed]
- 32.Shibuya K, Hashimoto H, Ikegami N, Nishi A, Tanimoto T, Miyata H. et al. Future of Japan's system of good health at low cost with equity: beyond universal coverage. Lancet (London, England) 2011:1265. doi: 10.1016/S0140-6736(11)61098-2. [DOI] [PubMed]
- 33.Adhikari SR, Pandey AR, Ghimire M, Thapa AK, Lamsal DK. Universal Access to Essential Medicines: An Evaluation of Nepal's Free Health Care Scheme. Journal of Nepal Health Research Council. 2018:36. [PubMed]
- 34.Ayub A, Khan RS, Khan SA, Hussain H, Tabassum A, Shehzad JA. et al. Progress Of Khyber Pakhtunkhwa (Pakistan) Towards Universal Health Coverage. Journal of Ayub Medical College, Abbottabad : JAMC. 2018:482. [PubMed]
- 35.Aantjes C, Quinlan T, Bunders J. Towards universal health coverage in Zambia: impediments and opportunities. Dev Pract. 2016:298.
- 36.Adams AM, Rabbani A, Ahmed S, Mahmood SS, Al-Sabir A, Rashid SF. et al. Bangladesh: Innovation for Universal Health Coverage 4: Explaining equity gains in child survival in Bangladesh: Scale, speed, and selectivity in health and development. The Lancet. 2013:2027. doi: 10.1016/S0140-6736(13)62060-7. [DOI] [PubMed]
- 37.Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Suparmi, Achadi EL. et al. Universal health coverage in Indonesia: concept, progress, and challenges. The Lancet. 2019:75. doi: 10.1016/S0140-6736(18)31647-7. [DOI] [PubMed]
- 38.Akashi H, Osanai Y, Akashi R. Human resources for health development: Toward realizing Universal Health Coverage in Japan. BioScience Trends. 2015:275. doi: 10.5582/bst.2015.01125. [DOI] [PubMed]
- 39.Akhnif E, Kiendrebeogo JA, Idrissi Azouzzi, Adam Z, Makoutode CP, Mayaka Manitu. et al. Are our 'UHC systems' learning systems. Piloting an assessment tool and process in six African countries. Health research policy and systems doi: 10.1186/s12961-018-0340-y. [DOI] [PMC free article] [PubMed]
- 40.Alkenbrack S, Jacobs B, Lindelow M. Achieving universal health coverage through voluntary insurance: What can we learn from the experience of Lao PDR. BMC health services research. 2013 doi: 10.1186/1472-6963-13-521. [DOI] [PMC free article] [PubMed]
- 41.Amaya JL, Ruiz F, Trujillo AJ, Buttorff C. Identifying barriers to move to better health coverage: Preferences for health insurance benefits among the rural poor population in La Guajira, Colombia. Int J Health Plann Manage. 2016:126. doi: 10.1002/hpm.2268. [DOI] [PubMed]
- 42.Andrade MV, Coelho AQ, Neto MX, De Carvalho, Atun R, Castro MC. Transition to universal primary health care coverage in Brazil: Analysis of uptake and expansion patterns of Brazil's Family Health Strategy (1998-2012) PLoS ONE. 2018 doi: 10.1371/journal.pone.0201723. [DOI] [PMC free article] [PubMed]
- 43.Asaria M, Ali S, Doran T, Ferguson B, Fleetcroft R, Goddard M. et al. How a universal health system reduces inequalities: Lessons from England. J Epidemiol Community Health. 2016:637. doi: 10.1136/jech-2015-206742. [DOI] [PMC free article] [PubMed]
- 44.Asfaw E, Dominis S, Palen JG, Wong W, Bekele A, Kebede A. et al. Patient satisfaction with task shifting of antiretroviral services in Ethiopia: implications for universal health coverage. Health policy and planning. 2014 doi: 10.1093/heapol/czu072. [DOI] [PMC free article] [PubMed]
- 45.Atun R, Aydin S, Chakraborty S, Sumer S, Aran M, Gurol I. et al. Universal health coverage in Turkey: enhancement of equity. Lancet. 2013:65. doi: 10.1016/S0140-6736(13)61051-X. [DOI] [PubMed]
- 46.Atun R, de Andrade, Almeida G, Cotlear D, Dmytraczenko T, Frenz P. et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015:1230. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed]
- 47.Aungkulanon S, Tangcharoensathien V, Shibuya K, Bundhamcharoen K, Chongsuvivatwong V. Post universal health coverage trend and geographical inequalities of mortality in Thailand. International journal for equity in health. 2016:190. doi: 10.1186/s12939-016-0479-5. [DOI] [PMC free article] [PubMed]
- 48.Baine SO, Kakama A, Mugume M. Development of the Kisiizi hospital health insurance scheme: lessons learned and implications for universal health coverage. BMC Health Serv Res. 2018:455. doi: 10.1186/s12913-018-3266-8. [DOI] [PMC free article] [PubMed]
- 49.Ballart X, Fuentes G. Gaining public control on health policy: the politics of scaling up to universal health coverage in Uruguay. Soc Theory Health. 2018
- 50.Barasa E, Nguhiu P, McIntyre D. Measuring progress towards Sustainable Development Goal 3. 8 on universal health coverage in Kenya. BMJ global health doi: 10.1136/bmjgh-2018-000904. [DOI] [PMC free article] [PubMed]
- 51.Barasa E, Rogo K, Mwaura N, Chuma J. Kenya National Hospital Insurance Fund Reforms: Implications and Lessons for Universal Health Coverage. Health systems and reform. 2018:1-16 doi: 10.1080/23288604.2018.1513267. [DOI] [PMC free article] [PubMed]
- 52.Barber SL, Huang B, Santoso B, Laing R, Paris V, Wu C. The reform of the essential medicines system in China: a comprehensive approach to universal coverage. J Glob Health. 2013:010303. doi: 10.7189/jogh.03.010303. [DOI] [PMC free article] [PubMed]
- 53.Bayarsaikhan D, Kwon S, Chimeddagva D. Social health insurance development in Mongolia: Opportunities and challenges in moving towards Universal Health Coverage. Int Soc Secur Rev. 2015:93.
- 54.Bredenkamp C, Evans T, Lagrada L, Langenbrunner J, Nachuk S, Palu T. Emerging challenges in implementing universal health coverage in Asia. Soc Sci Med. 2014 doi: 10.1016/j.socscimed.2015.07.025. [DOI] [PubMed]
- 55.Campbell J, Buchan J, Cometto G, David B, Dussault G, Fogstad H. et al. Human resources for health and universal health coverage: Fostering equity and effective coverage. Bulletin of the World Health Organization. 2013:853. doi: 10.2471/BLT.13.118729. [DOI] [PMC free article] [PubMed]
- 56.Bloom G. Universal Health Coverage and Primary Healthcare: Lessons From Japan Comment on "Achieving Universal Health Coverage by Focusing on Primary Care in Japan: Lessons for Low- and Middle-Income Countries". Int J Health Policy Manag. 2016:229. doi: 10.15171/ijhpm.2016.120. [DOI] [PMC free article] [PubMed]
- 57.Abuya T, Obare F, Matanda D, Dennis ML, Bellows B. Stakeholder perspectives regarding transfer of free maternity services to national health insurance fund in Kenya: Implications for universal health coverage. Int J Health Plann Manage. 2018:e648. doi: 10.1002/hpm.2515. [DOI] [PubMed]
Cite this article as : Koohpayehzadeh J, Azami-Aghdash S, Derakhshani N, Rezapour A, Alaei Kalajahi R, Sajjadi Khasraghi J, Nikoomanesh M, Sabetrohani H, Soleimanpour S. Best Practices in Achieving Universal Health Coverage: A Scoping Review. Med J Islam Repub Iran. 2021 (30 Dec);35:191. https://doi.org/10.47176/mjiri.35.191
References
- 1.Organization WH. The world health report 2000: health systems: improving performance: World Health Organization; 2000
- 2.Evans D, Saksena P, Elovainio R, Boerma T. Measuring progress towards universal coverage. Geneva: World Health Organization. 2012
- 3.Evans DB, Etienne C. Health systems financing and the path to universal coverage. SciELO Public Health; 2010. doi: 10.2471/BLT.10.078741. [DOI] [PMC free article] [PubMed]
- 4.Savedoff WD, de Ferranti, Smith AL, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. 2012:924. doi: 10.1016/S0140-6736(12)61083-6. [DOI] [PubMed]
- 5.Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012:933. doi: 10.1016/S0140-6736(12)61147-7. [DOI] [PubMed]
- 6.Organization WH. Tracking universal health coverage: first global monitoring report: World Health Organization; 2015
- 7.Pannarunothai S, Patmasiriwat D, Srithamrongsawat S. Universal health coverage in Thailand: ideas for reform and policy struggling. Health Policy. 2004:17. doi: 10.1016/S0168-8510(03)00024-1. [DOI] [PubMed]
- 8.Supachutikul A. Situation analysis on health insurance and future development: Thailand Health Research Institute; 1996
- 9.Maeda A, Araujo E, Cashin C, Harris J, Ikegami N, Reich MR. Universal health coverage for inclusive and sustainable development: a synthesis of 11 country case studies: The World Bank; 2014
- 10.Obare V, Brolan CE, Hill PS. Indicators for Universal Health Coverage: can Kenya comply with the proposed post-2015 monitoring recommendations. Int J Equity Health. 2014 doi: 10.1186/s12939-014-0123-1. [DOI] [PMC free article] [PubMed]
- 11.Xu Y, Huang C, Colón-Ramos U. Moving Toward Universal Health Coverage (UHC) to Achieve Inclusive and Sustainable Health Development: Three Essential Strategies Drawn From Asian Experience: Comment on" Improving the World’s Health Through the Post-2015 Development Agenda: Perspectives from Rwanda". Int J Health Policy Manag. 2015:869. doi: 10.15171/ijhpm.2015.156. [DOI] [PMC free article] [PubMed]
- 12.Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health. Lancet. 2012:917. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed]
- 13.Abdi Z, Yazdizadeh B, Ahmadnezhad E, Rahimi M, Majdzadeh R. Universal health coverage in Iran: What kind of knowledge is needed to achieve the goals. Med J Islam Repub Iran. 2019:393. doi: 10.34171/mjiri.33.65. [DOI] [PMC free article] [PubMed]
- 14.Garrett L, Chowdhury AMR, Pablos-Méndez A. All for universal health coverage. Lancet. 2009:1294. doi: 10.1016/S0140-6736(09)61503-8. [DOI] [PubMed]
- 15.Bredenkamp C, Evans T, Lagrada L, Langenbrunner J, Nachuk S, Palu T. Emerging challenges in implementing universal health coverage in Asia. Soc Sci Med. 2015 doi: 10.1016/j.socscimed.2015.07.025. [DOI] [PubMed]
- 16.Akashi H, Osanai Y, Akashi R. Human resources for health development: Toward realizing Universal Health Coverage in Japan. BioScience Trends. 2015:275. doi: 10.5582/bst.2015.01125. [DOI] [PubMed]
- 17.Maddison A. Contours of the world economy 1-2030 AD: Essays in macro-economic history: Oxford University Press; 2007
- 18.Naser Derakhshani, leila Doshmangir, Ayat Ahmadi, Ali Fakhri, Homayuon Sadeghi-Bazarghani, Gordeev VS. Monitoring process barriers and enables towards universal health coverage within the Sustainable Development Goals. BMC health services research. 21 January 2020 doi: 10.2147/CEOR.S254946. [DOI] [PMC free article] [PubMed]
- 19.Dolea C, Stormont L, Shaw D, Zurn P, Braichet J, editors. Increasing access to health workers in remote and rural areas through improved retention. Background paper for the first expert meeting to develop evidence-based recommendations to increase access to health workers in remote and rural areas through improved retention Geneva: World Health Organization; 2009
- 20.Mulupi S, Kirigia D, Chuma J. Community perceptions of health insurance and their preferred design features: implications for the design of universal health coverage reforms in Kenya. BMC Health Serv Res. 2013:474. doi: 10.1186/1472-6963-13-474. [DOI] [PMC free article] [PubMed]
- 21.Ehsani-Chimeh E, Sajadi HS, Majdzadeh R. Iran towards universal health coverage: The role of human resources for health. Med J Islam Repub Iran. 2018:578. doi: 10.14196/mjiri.32.100. [DOI] [PMC free article] [PubMed]
- 22. World Health Organization (WHO). Health systems financing: the path to universal coverage. The World Health Report. 2010. URL: http://www.who.int/whr/2010/en [ accessed 2014. oct 18 ]. [WebCite Cache ID 6TPqanY1w]. [DOI] [PMC free article] [PubMed]
- 23.Latko B, Temporão JG, Frenk J, Evans TG, Chen LC, Pablos-Mendez A. et al. The growing movement for universal health coverage. Lancet. 2011:2161. doi: 10.1016/S0140-6736(10)62006-5. [DOI] [PubMed]
- 24.Organization WH. Sustainable health financing, universal coverage and social health insurance. World Health Assembly Resolution. 2005
- 25.Campbell J, Buchan J, Cometto G, David B, Dussault G, Fogstad H. et al. Human resources for health and universal health coverage: fostering equity and effective coverage. Bull World Health Organ. 2013 doi: 10.2471/BLT.13.118729. [DOI] [PMC free article] [PubMed]
- 26.Ahmed S, Annear PL, Phonvisay B, Phommavong C, Cruz Vde, Hammerich A. et al. Institutional design and organizational practice for universal coverage in lesser-developed countries: challenges facing the Lao PDR. Soc Sci Med. 2013 doi: 10.1016/j.socscimed.2013.01.019. [DOI] [PubMed]
- 27.Marnani AB, Teymourzadeh E, Bahadori M, Ravangard R, Pour JS. Challenges of a large health insurance organization in Iran: A Qualitative Study. Int J Collab Res Intern Med Public. 2012:0.
- 28.Yazdizadeh B, Mohtasham F. Assessment of research systems in universal health coverage-related organizations. Med J Islam Repub Iran. 2018:83. doi: 10.18869/mjiri.32.15. [DOI] [PMC free article] [PubMed]
- 29.Shibuya K, Hashimoto H, Ikegami N, Nishi A, Tanimoto T, Miyata H. et al. Future of Japan's system of good health at low cost with equity: beyond universal coverage. Lancet. 2011:1265. doi: 10.1016/S0140-6736(11)61098-2. [DOI] [PubMed]
- 30.Van Minh, Pocock NS, Chaiyakunapruk N, Chhorvann C, Duc HA, Hanvoravongchai P. et al. Progress toward universal health coverage in ASEAN. Glob Health Action. 2014:25856. doi: 10.3402/gha.v7.25856. [DOI] [PMC free article] [PubMed]
- 31.Abiiro GA, De Allegri. Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates. BMC Int Health Hum Rights. 2015:17. doi: 10.1186/s12914-015-0056-9. [DOI] [PMC free article] [PubMed]
- 32.Tejativaddhana P, Briggs D, Fraser J, Minichiello V, Cruickshank M. Identifying challenges and barriers in the delivery of primary healthcare at the district level: a study in one Thai province. Int J Health Plann Manage. 2013:16. doi: 10.1002/hpm.2118. [DOI] [PubMed]
- 33.Damrongplasit K, Melnick G. Funding, coverage, and access under Thailand’s universal health insurance program: An update after ten years. Appl Health Econ Health Policy. 2015:157. doi: 10.1007/s40258-014-0148-z. [DOI] [PubMed]
- 34.Atun R, de Andrade, Almeida G, Cotlear D, Dmytraczenko T, Frenz P. et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015:1230. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed]
- 35.Tripathy RM. Public health challenges for universal health coverage. Indian J Public Health. 2014:156. doi: 10.4103/0019-557X.138619. [DOI] [PubMed]
- 36.Aguilera X, Castillo-Laborde C, Najera-De Ferrari, Delgado I, Ibañez C. Monitoring and evaluating progress towards universal health coverage in Chile. PLoS Med. 2014:e1001676. doi: 10.1371/journal.pmed.1001676. [DOI] [PMC free article] [PubMed]
- 37.Knaul FM, Bhadelia A, Atun R, Frenk J. Achieving effective universal health coverage and diagonal approaches to care for chronic illnesses. Health Aff. 2015:1514. doi: 10.1377/hlthaff.2015.0514. [DOI] [PubMed]
- 38.Mills A, Ally M, Goudge J, Gyapong J, Mtei G. Progress towards universal coverage: the health systems of Ghana, South Africa and Tanzania. Health Policy Plan. 2012:i4. doi: 10.1093/heapol/czs002. [DOI] [PubMed]
- 39.Rezapour A, Ebadifard Azar, Azami Aghdash, Tanoomand A, Hosseini Shokouh, Yousefzadeh N. et al. Measuring equity in household's health care payments (Tehran- Iran 2013): technical points for health policy decision makers. Med J Islam Repub Iran. 2015:685. [PMC free article] [PubMed]
- 40.McIntyre D, Ranson MK, Aulakh BK, Honda A. Promoting universal financial protection: evidence from seven low-and middle-income countries on factors facilitating or hindering progress. Health Res. Policy Syst doi: 10.1186/1478-4505-11-36. [DOI] [PMC free article] [PubMed]
- 41.Hajizadeh M, Nghiem HS. Out-of-pocket expenditures for hospital care in Iran: who is at risk of incurring catastrophic payments. Int J Health Care Finance Econ. 2011:267. doi: 10.1007/s10754-011-9099-1. [DOI] [PubMed]
- 42.Moghadam MN, Banshi M, Javar MA, Amiresmaili M, Ganjavi S. Iranian household financial protection against catastrophic health care expenditures. Iran J Public Health. 2012:62. [PMC free article] [PubMed]
- 43.Bennett S, Ozawa S, Rao KD. Which path to universal health coverage. Perspectives on the World Health Report 2010. PLoS Med doi: 10.1371/journal.pmed.1001001. [DOI] [PMC free article] [PubMed]
- 44.Fattore G, Tediosi F. The importance of values in shaping how health systems governance and management can support universal health coverage. Value Health. 2013:S19. doi: 10.1016/j.jval.2012.10.008. [DOI] [PubMed]
- 45.Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, De Paepe, da Silva, Unger JP. et al. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med doi: 10.1016/j.socscimed.2014.01.054. [DOI] [PubMed]
- 46.Govender V, Chersich MF, Harris B, Alaba O, Ataguba JE, Nxumalo N. et al. Moving towards universal coverage in South Africa. Lessons from a voluntary government insurance scheme. Glob Health Action doi: 10.3402/gha.v6i0.19253. [DOI] [PMC free article] [PubMed]
- 47.Ibrahimipour H, Maleki M-R, Brown R, Gohari M, Karimi I, Dehnavieh R. A qualitative study of the difficulties in reaching sustainable universal health insurance coverage in Iran. Health Policy Plan. 2011:485. doi: 10.1093/heapol/czq084. [DOI] [PubMed]
- 48.Rezapour A, Ebadifard Azar, Azami Aghdash, Tanoomand A, Ahmadzadeh N, Sarabi Asiabar. Inequity in household's capacity to pay and health payments in Tehran-Iran-2013. Med J Islam Repub Iran. 2015:674. [PMC free article] [PubMed]
- 49.Mirabedini SA, Fazl Hashemi, Sarabi Asiabar, Rezapour A, Azami-Aghdash S, Hosseini Amnab. Out-of-pocket and informal payments in Iran's health care system: A systematic review and meta-analysis. Med J Islam Repub Iran. 2017:401. doi: 10.14196/mjiri.31.70. [DOI] [PMC free article] [PubMed]
- 50.Saleh SS, Alameddine MS, Natafgi NM, Mataria A, Sabri B, Nasher J. et al. The path towards universal health coverage in the Arab uprising countries Tunisia, Egypt, Libya, and Yemen. Lancet. 2014:368. doi: 10.1016/S0140-6736(13)62339-9. [DOI] [PubMed]
- 51.Patel V, Parikh R, Nandraj S, Balasubramaniam P, Narayan K, Paul VK. et al. Assuring health coverage for all in India. Lancet. 2015:2422. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed]
- 52.Organization WH. The world health report: health systems financing: the path to universal coverage: executive summary. World Health Organization; 2010. doi: 10.2471/BLT.10.078741. [DOI] [PMC free article] [PubMed]
- 53.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff. 2007:972. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed]
- 54.Alebachew A, Hatt L, Kukla M. Monitoring and evaluating progress towards Universal Health Coverage in Ethiopia. PLoS Med. 2014 doi: 10.1371/journal.pmed.1001696. [DOI] [PMC free article] [PubMed]
- 55.Blanchet K, Gordon I, Gilbert CE, Wormald R, Awan H. How to achieve universal coverage of cataract surgical services in developing countries: lessons from systematic reviews of other services. Ophthalmic Epidemiol. 2012:329. doi: 10.3109/09286586.2012.717674. [DOI] [PubMed]
- 56.Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S. et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012:126. doi: 10.1016/S0140-6736(12)60357-2. [DOI] [PubMed]
- 57.Marten R, McIntyre D, Travassos C, Shishkin S, Longde W, Reddy S. et al. An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS) Lancet. 2014:2164. doi: 10.1016/S0140-6736(14)60075-1. [DOI] [PMC free article] [PubMed]
- 58.Khan K, Kunz R, Kleijnen J, Antes G. Systematic reviews to support evidence-based medicine: Crc Press; 2011
- 59.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005:19.
- 60.Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 [PMC free article] [PubMed]
- 61.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed]
- 62.Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. J Administ Gov. 2009:72.
- 63.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013:1. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed]
- 64.World Bank,
- 65.Organization WH. Global tuberculosis control: surveillance, planning, financing: WHO report 2008: World Health Organization; 2008
- 66.Organization WH. Global strategy on human resources for health: workforce 2030. 2016
- 67. United nations high-level meeting on universal health coverage in 2019, key targets, commitments & actions. Available from: [https://wwwuhc2030org/fileadmin/uploads/uhc2030/Documents/UN_HLM/UHC_key_targets_actions_commitments_15_Nov_2019__1_pdf]. 2019 .
- 68.Adhikari SR, Pandey AR, Ghimire M, Thapa AK, Lamsal DK. Universal Access to Essential Medicines: An Evaluation of Nepal's Free Health Care Scheme. J Nepal Health Res Counc. 2018:36. [PubMed]
- 69.Pokharel R, Silwal PR. Social health insurance in Nepal: A health system departure toward the universal health coverage. Int J Health Plann Manage. 2018 doi: 10.1002/hpm.2530. [DOI] [PubMed]
- 70.Baine SO, Kakama A, Mugume M. Development of the Kisiizi hospital health insurance scheme: lessons learned and implications for universal health coverage. BMC Health Serv Res. 2018:455. doi: 10.1186/s12913-018-3266-8. [DOI] [PMC free article] [PubMed]
- 71.Hongoro C, Rutebemberwa E, Twalo T, Mwendera C, Douglas M, Mukuru M. et al. Analysis of selected policies towards universal health coverage in Uganda: the policy implementation barometer protocol. Arch Public Health. 2018:12. doi: 10.1186/s13690-018-0258-4. [DOI] [PMC free article] [PubMed]
- 72.Lu C, Chin B, Lewandowski JL, Basinga P, Hirschhorn LR, Hill K. et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One. 2012:e39282. doi: 10.1371/journal.pone.0039282. [DOI] [PMC free article] [PubMed]
- 73.Maluka S, Chitama D, Dungumaro E, Masawe C, Rao K, Shroff Z. Contracting-out primary health care services in Tanzania towards UHC: how policy processes and context influence policy design and implementation. Int J Equity Health. 2018:118. doi: 10.1186/s12939-018-0835-8. [DOI] [PMC free article] [PubMed]
- 74.Asfaw E, Dominis S, Palen JG, Wong W, Bekele A, Kebede A. et al. Patient satisfaction with task shifting of antiretroviral services in Ethiopia: implications for universal health coverage. Health Policy Plan. 2014:ii50. doi: 10.1093/heapol/czu072. [DOI] [PMC free article] [PubMed]
- 75.Edward A, Branchini C, Aitken I, Roach M, Osei-Bonsu K, Arwal SH. Toward universal coverage in Afghanistan: A multi-stakeholder assessment of capacity investments in the community health worker system. Soc Sci Med. 2015 doi: 10.1016/j.socscimed.2015.06.011. [DOI] [PubMed]
- 76.Garchitorena A, Miller AC, Cordier LF, Ramananjato R, Rabeza VR, Murray M. et al. In Madagascar, Use Of Health Care Services Increased When Fees Were Removed: Lessons For Universal Health Coverage. Health Aff (Project Hope) 2017:1443. doi: 10.1377/hlthaff.2016.1419. [DOI] [PubMed]
- 77.He AJ, Wu S. Towards Universal Health Coverage via Social Health Insurance in China: Systemic Fragmentation, Reform Imperatives, and Policy Alternatives. Appl Health Econ Health Policy. 2017:707. doi: 10.1007/s40258-016-0254-1. [DOI] [PubMed]
- 78.Meng Q, Xu L. Monitoring and Evaluating Progress towards Universal Health Coverage in China. PLoS Med. 2014 doi: 10.1371/journal.pmed.1001694. [DOI] [PMC free article] [PubMed]
- 79.Obermann K, Jowett M, Kwon S. The role of national health insurance for achieving UHC in the Philippines: a mixed methods analysis. Glob Health Action. 2018:1483638. doi: 10.1080/16549716.2018.1483638. [DOI] [PMC free article] [PubMed]
- 80.Okech TC, Lelegwe SL. Analysis of Universal Health Coverage and Equity on Health Care in Kenya. Glob J Health Sci. 2015:218. doi: 10.5539/gjhs.v8n7p218. [DOI] [PMC free article] [PubMed]
- 81.Vargas JR, Muiser J. Promoting universal financial protection: a policy analysis of universal health coverage in Costa Rica (1940–2000) Health Res Policy Syst. 2013:28. doi: 10.1186/1478-4505-11-28. [DOI] [PMC free article] [PubMed]
- 82.Cheng SH, Chen CC, Tsai SL. The impacts of DRG-based payments on health care provider behaviors under a universal coverage system: a population-based study. Health Policy. 2012:202. doi: 10.1016/j.healthpol.2012.03.021. [DOI] [PubMed]
- 83.Tang S, Tao J, Bekedam H, editors. Controlling cost escalation of healthcare: making universal health coverage sustainable in China. BMC Public Health. 2012 doi: 10.1186/1471-2458-12-S1-S8. [DOI] [PMC free article] [PubMed]
- 84.Asaria M, Ali S, Doran T, Ferguson B, Fleetcroft R, Goddard M. et al. How a universal health system reduces inequalities: Lessons from England. J Epidemiol Community Health. 2016:637. doi: 10.1136/jech-2015-206742. [DOI] [PMC free article] [PubMed]
- 85.Borgonovi E, Compagni A. Sustaining universal health coverage: the interaction of social, political, and economic sustainability. Value Health. 2013:S34. doi: 10.1016/j.jval.2012.10.006. [DOI] [PubMed]
- 86.Tangcharoensathien V, Limwattananon S, Suphanchaimat R, Patcharanarumol W, Sawaengdee K, Putthasri W. Health workforce contributions to health system development: a platform for universal health coverage. Bull World Health Organ. 2013 doi: 10.2471/BLT.13.120774. [DOI] [PMC free article] [PubMed]
- 87.McIntyre D, Ranson MK, Aulakh BK, Honda A. Promoting universal financial protection: evidence from seven low- and middle-income countries on factors facilitating or hindering progress. Health Res Policy Syst. 2013 doi: 10.1186/1478-4505-11-36. [DOI] [PMC free article] [PubMed]
- 88.Nyandekwe M, Nzayirambaho M, Baptiste Kakoma. Universal health coverage in Rwanda: dream or reality. Pan Afr Med J. 2014 doi: 10.11604/pamj.2014.17.232.3471. [DOI] [PMC free article] [PubMed]
- 89.Hatanaka T, Eguchi N, Deguchi M, Yazawa M, Ishii M. Study of global health strategy based on international trends: Promoting universal health coverage globally and ensuring the sustainability of japan’s universal coverage of health insurance system: Problems and proposals. Japan Med Assoc J. 2015:78. [PMC free article] [PubMed]
- 90.Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009:63. doi: 10.1093/heapol/czn037. [DOI] [PubMed]
- 91.Saadati M, Rezapour R, Derakhshani N, Naghshi M. Comparative Study of Fair Financing in the Health Insurance. J Healthc Manag. 2017:65.
- 92.McIntyre D, Garshong B, Mtei G, Meheus F, Thiede M, Akazili J. et al. Beyond fragmentation and towards universal coverage: insights from Ghana, South Africa and the United Republic of Tanzania. Bull World Health Organ. 2008:871. doi: 10.2471/BLT.08.053413. [DOI] [PMC free article] [PubMed]
- 93.Okoroh JS, Chia V, Oliver EA, Dharmawardene M, Riviello R. Strengthening health systems of developing countries: inclusion of surgery in universal health coverage. World J Surg. 2015:1867. doi: 10.1007/s00268-015-3031-7. [DOI] [PubMed]
- 94.Ataguba JE, Day C, McIntyre D. Monitoring and evaluating progress towards universal health coverage in South Africa. PLoS Med. 2014 doi: 10.1371/journal.pmed.1001686. [DOI] [PMC free article] [PubMed]
- 95.Cheng SH, Chen CC, Chang WL. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy. 2009:158. doi: 10.1016/j.healthpol.2009.03.008. [DOI] [PubMed]
- 96.Ballart X, Fuentes G. Gaining public control on health policy: the politics of scaling up to universal health coverage in Uruguay. Soc Theory Health. 2019:348.
- 97.Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014 doi: 10.1371/journal.pmed.1001701. [DOI] [PMC free article] [PubMed]
- 98.Kwon S. Health care financing in Asia: key issues and challenges. Asia Pac J Public Health. 2011:651. doi: 10.1177/1010539511422940. [DOI] [PubMed]
- 99.Tang S, Brixi H, Bekedam H. Advancing universal coverage of healthcare in China: translating political will into policy and practice. Int J Health Plann Manage. 2014:160. doi: 10.1002/hpm.2207. [DOI] [PubMed]
- 100.Officer RW. Measuring Universal Health Coverage to Ensure Continuing Care for Older People: A Scoping Review with Specific Implications for the Iranian Context. 2020. doi: 10.26719/emhj.21.040. [DOI] [PubMed]
- 101.Frenk J, Gomez-Dantes O. Health Systems in Latin America: The Search for Universal Health Coverage. Arch Med Res. 2018:79. doi: 10.1016/j.arcmed.2018.06.002. [DOI] [PubMed]
- 102.Nuñez PA, Fernández-Slezak D, Farall A, Szretter ME, Salomón OD, Valeggia CR. Impact of universal health coverage on child growth and nutrition in Argentina. Am J Public Health. 2016:720. doi: 10.2105/AJPH.2016.303056. [DOI] [PMC free article] [PubMed]
- 103.Chan WY, Fung IM, Chan E. Universal Health Coverage through Community Nursing Services: China vs. Hong Kong. Rev Lat Am Enfermagem doi: 10.1590/1518-8345.1664.2838. [DOI] [PMC free article] [PubMed]
- 104.Knaul FM, Frenk J. Health insurance in Mexico: Achieving universal coverage through structural reform - A 2003 reform is making good progress toward covering Mexico's eleven million uninsured families by 2010. Health Aff. 2005:1467. doi: 10.1377/hlthaff.24.6.1467. [DOI] [PubMed]
- 105.Adams AM, Ahmed T, El Arifeen, Evan s, Huda T, Reichenbach L. Innovation for universal health coverage in Bangladesh: a call to action. Lancet. 2013:2104. doi: 10.1016/S0140-6736(13)62150-9. [DOI] [PubMed]
- 106.Aantjes C, Quinlan T, Bunders J. Towards universal health coverage in Zambia: impediments and opportunities. Dev Pract. 2016:298.
- 107.Barasa E, Rogo K, Mwaura N, Chuma J. Kenya National Hospital Insurance Fund Reforms: Implications and Lessons for Universal Health Coverage. Health Syst Reform. 2018:346. doi: 10.1080/23288604.2018.1513267. [DOI] [PMC free article] [PubMed]
- 108.Barasa E, Nguhiu P, McIntyre D. Measuring progress towards sustainable development goal 3. 8 on universal health coverage in Kenya. BMJ Glob Health doi: 10.1136/bmjgh-2018-000904. [DOI] [PMC free article] [PubMed]
- 109.Hughes D, Leethongdee S. Universal coverage in the land of smiles: Lessons from Thailand's 30 Baht health reforms. Health Aff. 2007:999. doi: 10.1377/hlthaff.26.4.999. [DOI] [PubMed]
- 110.Alkenbrack S, Jacobs B, Lindelow M. Achieving universal health coverage through voluntary insurance: What can we learn from the experience of Lao PDR. BMC Health Serv Res. 2013 doi: 10.1186/1472-6963-13-521. [DOI] [PMC free article] [PubMed]
- 111.Adebayo EF, Uthman OA, Wiysonge CS, Stern EA, Lamont KT, Ataguba JE. A systematic review of factors that affect uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res. 2015:543. doi: 10.1186/s12913-015-1179-3. [DOI] [PMC free article] [PubMed]
- 112.Amaya JL, Ruiz F, Trujillo AJ, Buttorff C. Identifying barriers to move to better health coverage: Preferences for health insurance benefits among the rural poor population in La Guajira, Colombia. Int J Health Plann Manage. 2016:126. doi: 10.1002/hpm.2268. [DOI] [PubMed]
- 113.Garg S. Universal health coverage in India: Newer innovations and the role of public health. Indian J Public Health. 2018:167. doi: 10.4103/ijph.IJPH_221_18. [DOI] [PubMed]
- 114.Lu JFR, Chiang TL. Developing an adequate supply of health services: Taiwan's path to Universal Health Coverage. Soc Sci Med. 2018 doi: 10.1016/j.socscimed.2017.12.017. [DOI] [PubMed]
- 115.Atun R, Aydin S, Chakraborty S, Sumer S, Aran M, Gurol I. et al. Universal health coverage in Turkey: enhancement of equity. Lancet. 2013:65. doi: 10.1016/S0140-6736(13)61051-X. [DOI] [PubMed]
- 116.Barber SL, Huang B, Santoso B, Laing R, Paris V, Wu C. The reform of the essential medicines system in China: a comprehensive approach to universal coverage. J Glob Health. 2013 doi: 10.7189/jogh.03.010303. [DOI] [PMC free article] [PubMed]