Abstract
Introduction and objectives
Quadratus Lumborum block was recently described and has already shown good results as an analgesic technique in abdominal surgeries, having the potential to significantly reduce opioids consumption and be a valid alternative to epidural catheter. We performed a type II Quadratus Lumborum block for analgesia in a septic patient having a sub-total gastrectomy.
Case report
An 80 year-old, ASA III, male patient, weighting 50 kg, with a history of arterial hypertension and hypercholesterolemia, diagnosed with sepsis due to purulent peritonitis was submitted to an open laparotomy. Bilateral ultrasound-guided type II Quadratus Lumborum block was performed before surgery, using 10 mL of levobupivacaine 0.25% and 5 mL of mepivacaine 1%, per side. Pain relief was achieved 5 minutes after injection and the patient referred no pain in the immediate postoperative period.
Discussion
Type II Quadratus Lumborum block may be considered a valid alternative for postoperative analgesia in a septic patient undergoing major abdominal surgery with some relative contraindications to epidural catheter placement. It allowed us to achieve excellent pain management avoiding opioids usage. However, more reports are still needed to properly access its usefulness.
Keywords: Peritonitis, Gastrectomy, Pain, Quadratus Lumborum, Ultrasound
Resumo
Introdução e objetivo
O bloqueio do quadrado lombar (QL) foi descrito recentemente e já mostrou bons resultados como técnica analgésica em cirurgias abdominais, com potencial para reduzir significativamente o consumo de opioides e ser uma alternativa válida ao cateter peridural. Realizamos um bloqueio do QL tipo II para analgesia em um paciente séptico para gastrectomia subtotal.
Relato de caso
Paciente do sexo masculino, 80 anos de idade, ASA III, 50 kg, com história de hipertensão arterial e hipercolesterolemia, diagnosticado com sepsis devido a peritonite purulenta foi submetido a uma laparotomia aberta. O bloqueio bilateral do QL tipo II guiado por ultrassom foi realizado antes da cirurgia com 10 mL de levobupivacaína a 0,25% e 5 mL de mepivacaína a 1%, por lado. O alívio da dor foi obtido em 5 minutos após a injeção, e o paciente não referiu dor no pós-operatório imediato.
Discussão
O bloqueio do quadrado lombar (QL) tipo II pode ser considerado uma alternativa válida para analgesia no pós-operatório em um paciente séptico submetido a cirurgia abdominal de grande porte, com algumas contraindicações relativas à colocação do cateter peridural. Permitiu-nos obter um excelente manejo da dor evitando o uso de opioides. Contudo, mais relatos ainda são necessários para avaliar corretamente a sua utilidade.
Palavras-chave: Peritonite, Gastrectomia, Dor, Quadrado lombar, Ultrassom
Introduction and objectives
Quadratus Lumborum block was initially described by R. Blanco with a postero-lateral abdominal injection of local anesthetic (LA) in the antero-lateral aspect of the QL muscle – type I QL block.1 Later, J. Børglum refined the QL block technique with the posterior transmuscular approach using the Erector Spinae (ES), QL, Psoas Major (PM) and transverse process of lumbar (L) 4 as references – Shamrock approach – and injecting the LA in the anterior aspect of the QL.2 More recently, R. Blanco described a QL block injecting the LA in the posterior aspect of the QL muscle, known as the type II QL block,3 which may be safer to perform because the LA is injected in a more superficial plane, therefore reducing the risk of lumbar plexus injuries and intra-abdominal complications.
Both types of QL block have been recently described for chronic pain following abdominal hernia repair4 and for postoperative analgesia following abdominal surgery. Visoiu M. et al. and Kadam V. R. refer complete pain relief in the distribution area from Thoracic (Th) 6 to L1 dermatomes.5, 6 Because of its similarities with transversus abdominis plane (TAP) block, in surgeries with peritoneal involvement it may reduce morphine consumption to less than 30%.7 It has been shown that the LA spreads between Th4 and L1 after a type I QL block, thus having the potential to cover the entire sensitive innervation of the abdominal wall and also block visceral afferent pathways to the medulla.8
Epidural catheters have been widely used for intra and postoperative analgesia in major abdominal surgeries but their placement may bring some major complications such as postdural puncture headache, direct neural injury, epidural hematomas, meningitis and epidural abcess.9 Many absolute and relative contraindications are well established and despite still being advocated for major abdominal surgeries, epidural catheters have been losing some pace due to great advances in peripheral nerve blocks.
We present a case report involving a septic patient having a sub-total gastrectomy in whom we performed a type II QL block for analgesia.
Case report
We performed a bilateral ultrasound (US) guided type II QL block using the Shamrock approach (Fig. 1) in an 80 year-old, ASA III, male patient, weighting 50 kg, with a long known history of arterial hypertension and hypercholesterolemia, presenting with intense abdominal pain, anorexia and obstipation with 48 h of evolution, with tachycardia and hypotension and lactates 4.3 mmol.L−1. This patient was diagnosed with a purulent peritonitis due to a perforated gastric carcinoma after observation in the Emergency Department. Blood tests showed a platelet count of 86,000 × 103.uL−1, prolonged prothombin time (INR = 1.41) and an acute elevation of both blood urea nitrogen and serum creatinine (96 mg.dL−1 and 2.0 mg.dL−1, respectively); this septic scenario created additional risks for epidural catheterization. After accessing the risks and alternatives to the epidural catheter, we decided for the QL block as the primary analgesic technique.
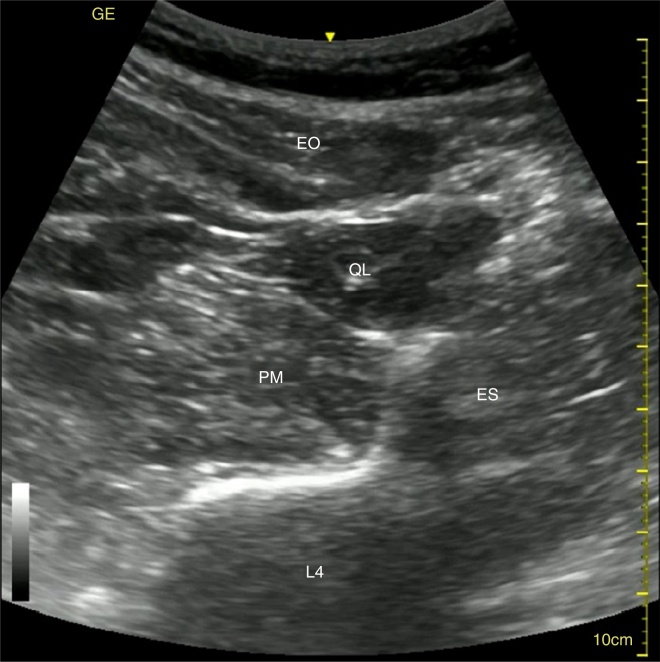
Figure 1.
Shamrock approach (EO - external oblique; ES - Erector Spinae; L4 - Lumbar 4; PM - Psoas Major; QL - Quadratus Lumborum).
The patient was monitored according to the American Society of Anesthesiology recommendations. Before the procedure, he received 0.05 mg of fentanil and 2 g of cefoxitine. The patient was placed in lateral decubitus with the side being blocked facing upwards. The bilateral US-guided QL block was performed with 10 mL of levobupivacaine 0.25% and 5 mL of mepivacaine 1%, per side, using a 21 G 50 mm needle (echoplex+, Vigon®), with a 2–5 MHz curved array transducer and the Vivid I GE ultrasound system, under aseptic technique. We visualized the injection spreading in the posterior surface of QL through a modified Shamrock approach, placing the needle in-plane in a parasagittal plane (Fig. 2). Pain relief was reported approximately 5 min after the injection took place. Induction of anesthesia and intubation was performed with fentanil 0.10 mg, propofol 50 mg and rocuronium 50 mg. Anesthesia was maintained with desflurane and a misture of O2 45%: air 55%. During surgery, the patient also received 0.625 mg of droperidol, approximately 3.5 L of crystalloids and an additional 20 mg of rocuronium. The surgery performed was a sub-total gastrectomy with a Bilroth II anastomosis, which took 1h30 to be completed. Skin incision ranged from Th6 to Th11. The patient remained hemodinamically stable with fluid therapy and did not receive any other analgesic measure.
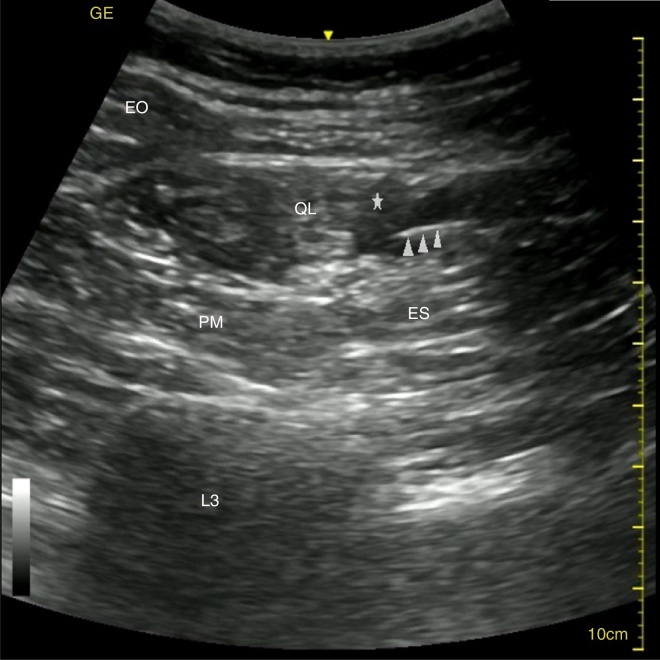
Figure 2.
US guided type II QL block (arrows’ head pointing the needle; star - local anesthetic; EO - external oblique; ES - Erector Spinae; L4 - Lumbar 4; PM - Psoas Major; QL - Quadratus Lumborum).
During his stay in the Post-Anesthesia Care Unit (PACU) the patient reported no pain, remained calm and cooperative and received an additional 1 L of crystalloids. He was discharged to the surgical ward 1 h after his arrival, having received a total of 4.5 L crystalloids in the perioperative period and registered a diuresis equivalent to 2 mL.Kg−1.h−1. Twelve hours after surgical procedure the patient started receiving an infusion of metamizol 6 g + tramadol 600 mg + metoclopramide 60 mg using an intravenous (iv) elastomeric pump at 3.1 mL.h−1 during 48 h. After that period the patient was discharged from our Acute Pain Unit with only mild pain during movement and no pain at rest (Visual Analog Scale 2 and 0, respectively). He received 1 g of acetaminophen and 100 mg of tramadol every 8 h, for the following 3 days after which he received 1 g of acetaminophen every 8 h. The patient was discharged from our hospital ten days after surgery and no rescue analgesia was needed during this period.
Discussion
Quadratus Lumborum block has only recently been described. There are some reports of its usefulness as an analgesic technique after abdominal surgery (duodenal tumor excision and after colostomy closure), achieving a good pain management in the postoperative period5, 6 and even to treat chronic pain following abdominal hernia repair.4 To our knowledge, we are the first to report the type II QL block use for a sub-total gastrectomy in a septic patient with peritonitis.
The QL originates from the lower border of the 12th rib and from the transverse processes of the upper 4 lumbar vertebrae and has its insertions on the inner lip of the iliac crest and in the iliolumbar ligament. The QL muscle is covered by the Transversalis Fascia (TF) and the Thoracolumbar Fascia, which share a common embryonic origin. The TF splits in two sheets at the diaphragmatic level, continuing as the inferior Diaphragmatic Fascia and Endothoracic Fascia.10
According to McDonnell JG et al., TAP block can significantly reduce opioids consumption in surgeries with peritoneal involvement.7 In addition, it seems that the closer to the spine we the LA is injected, the better will be the efficacy in TAP block, which may be related to the spreading of LA to the paravertebral space.11 In this case, we would need a subcostal TAP block to cover the dermatomes involved, which would have reduced probability of spreading to the paravertebral space. In QL block, LA is injected even closer to the spine with better longitudinal spreading as well as increased probability of reaching the paravertebral space and possibly blocking sympathetic ganglia. Therefore we believe that QL block will be at least as successful as TAP block for analgesia when there is peritoneal involvement.
Not only does avoiding opioid use during intra and postoperative period have benefits in preventing postoperative nausea and vomiting or paralytic ileum but, most importantly, it can limit immunosuppression which can influence both immediate recovery and tumor relapse or metastization.9 Either peripheral nerve blocks or epidural analgesia have great advantage over intravenous analgesia because both can significantly decrease opioids consumption and their related side effects.12 This propelled us to use an opioid sparing technique in this case.
In addition, our patient had a septic condition and arrived in a hypovolemic state with Acute Kidney Injury (AKI). In both scenarios, epidural catheter placement may be disadvantageous. First, it is long known that a patient with sepsis has greater risk for meningitis after an epidural catheter placement. Secondly, a thoracic epidural catheter would certainly produce hypotension due to increased splanchnic venous pooling and decreased venous return to the heart. In a patient with AKI (probably due to hypovolemia and consequent kidney hypoperfusion) we could enter in a tricky situation with hypotension due to decreased cardiac output and to extra hypoperfusion, requiring fluids and drugs for hemodynamic support. Also, the patient had two minor coagulation disturbances, increasing the risks for epidural catheterization.
It has been proved that LA can spread from Th4 until L1 after type I QL block as well as around the paravertebral space, having the potential to block visceral and abdominal wall pain.8 This would be important because sympathetic ganglia block reduces catecholamines in circulation, reducing the risk for cardiovascular events or respiratory compromise and improving the outcome of the anastomosis.9 No studies with type II QL block have been conducted yet and we also lack other reports for comparison, but we were able to main hemodynamic stability in a major upper abdominal surgery with relatively few analgesic measures – the patient did not report significant pain for a 12 h period. Therefore we think we also managed to achieve some visceral pain blockade.
Nonetheless, some questions remain unanswered. First, QL block is performed through an injection at lumbar level. However, LA spreads cephalically blocking thoracic roots while reaching only the first lumbar roots. Second, the ideal injection point for QL block remains elusive. Whether injecting LA in a more cephalic or caudal level will influence the success of the block remains to be determined. Also, it would be important to compare type I and type II QL block. There may be important differences in LA spread if we inject anteriorly or posteriorly to QL muscle that may affect the quality, onset and success of the block. Third, the volume of LA needed for a successful block has yet to be determined. From our own experience, it seems the greater the volume is injected, the sooner we achieve a satisfactory block with more longitudinal dermatomes involved but there are no consistent results.
In conclusion, QL block type II may constitute a valid alternative to epidural catheter both in patients with major contraindications or when the risks associated with catheter placement are elevated. Peripheral nerve blocks have less reported complications than neural axis approaches and QL block has theoretically minimal risk of intra-abdominal complications or lumbar plexus injuries, as well as having the potential to provide some degree of visceral blockade. Nevertheless, more studies are still needed to properly access the role of QL block in major surgeries.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Blanco R. TAP block under ultrasound guidance: the description of a ‘nonpopstechnique’. Reg Anaesth Pain Med. 2007;32:130. [Google Scholar]
- 2.Børglum J, Jensen K, Moriggl B, et al. Ultrasound guided transmuscular quadratum lumborum blockade. http://www.bja.oxfordjournals.org.
- 3.Blanco R. Optimal point of injection: the quadratum lumborum type I and II blocks. Anaesthesia. 2014 [Google Scholar]
- 4.Carvalho R., Segura E., Loureiro M.C., Assunção J.P. Bloqueio do quadrado lombar em dor crônica pós-hernioplastia abdominal: relato de caso. Rev Bras Anestesiol. 2014 doi: 10.1016/j.bjan.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Vivoiu M., Yakovleva N. Continuous postoperative analgesia via quadratum lumborum block – an alternative to transversus abdominins plane block. Paediatr Anaesth. 2013;23:959–961. doi: 10.1111/pan.12240. [DOI] [PubMed] [Google Scholar]
- 6.Kadam V.R. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesthesiol Clin Pharmacol. 2013;29:550–552. doi: 10.4103/0970-9185.119148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDonnell J.G., O’Donnell B., Curley G., et al. The analgesic efficacy of transverses abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 8.Carney J., Finnerty O., Rauf J., et al. Studies on the spread of local anaesthetic solution in transverses abdominis plane blocks. Anaesthesia. 2011;66:1023–1030. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 9.Nimmo S., Harrington L.S. What is the role of epidural analgesia in abdominal surgery? Cont Educ Anaesth Crit Care and Pain. 2014;14:224–229. [Google Scholar]
- 10.Standring S. 39th ed. Elsevier Churchill Livingstone; London: 2005. Gray's anatomy the anatomical basis of clinical practice; pp. 1113–1116. [Google Scholar]
- 11.Abdallah F.W., Laffey J.G., Halpern S.H., et al. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111:721–735. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 12.Wu Y., Liu F., Tang H., et al. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth Analg. 2013;111:507–513. doi: 10.1213/ANE.0b013e318297fcee. [DOI] [PubMed] [Google Scholar]