Abstract
Background and objectives
The administration of antifibrinolytics has been shown to be effective in reducing blood loss and the need for transfusions in surgeries. However, few studies have evaluated these drugs in cancer surgery. The objective was to review the efficacy and safety of the treatment with antifibrinolytics in patients who underwent oncologic surgeries.
Contents
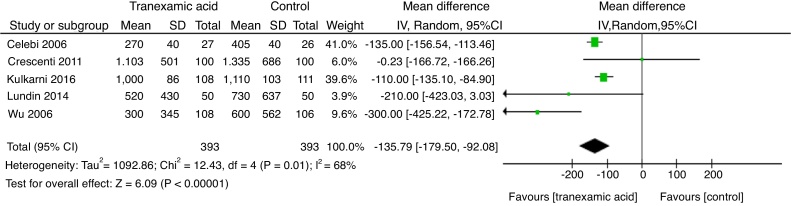
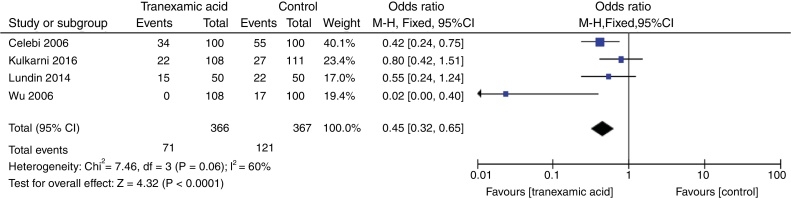
An electronic bibliographic research was conducted in PubMed, OVID, MEDLINE, EMBASE, EBSCO and in the Cochrane Library data basis in order to identify randomized clinical trials performed in any type of oncologic surgery. The data evaluated were blood loss, need for transfusion and incidence of arteriovenous thromboembolism. Five randomized controlled trials evaluating 838 patients met the inclusion requirements. In the analysis of the incidence of thromboembolic events in the five RCTs, there was no statistically significant difference between the administration of tranexamic acid when compared with the placebo (OR = 0.36, 95% IC: 0.11‒1.19, p = 0.09, I2 = 0%). However, when total estimated blood loss and need for blood transfusion are analyzed, the use of tranexamic acid was associated with a significant reduction over placebo (MD = −135.79, 95% CI: −179.50 to −92.08, p < 0.00001, I2 = 68%) and (OR = 0.45, 95% CI: 0.32‒0.65, p < 0.00001, I2 = 60%), respectively.
Conclusions
This meta-analysis found no evidence that the administration of antifibrinolytics increases the risk of thromboembolic complications in patients submitted to oncologic surgery, and has shown evidence that it is effective in reducing total perioperative blood loss and the need for blood transfusion.
Keywords: Antifibrinolytic agents, Cancer surgery, Thromboembolism, Blood loss
Resumo
Justificativa e objetivos
A administração de agentes antifibrinolíticos mostrou ser eficaz para reduzir a perda sanguínea e a necessidade de transfusões em cirurgias. No entanto, poucos estudos avaliaram esses agentes em cirurgias oncológicas. O objetivo foi revisar a eficácia e segurança do tratamento com antifibrinolíticos em pacientes submetidos a cirurgias oncológicas.
Conteúdo
Uma pesquisa bibliográfica foi conduzida nos bancos de dados eletrônicos PubMed, OVID, MEDLINE, EMBASE, EBSCO e na Biblioteca Cochrane para identificar ensaios clínicos randomizados feitos em qualquer tipo de cirurgia oncológica. Os dados analisados foram perda sanguínea, necessidade de transfusão e incidência de tromboembolismo arteriovenoso. Cinco ensaios clínicos randomizados que avaliaram 838 pacientes atenderam os critérios de inclusão. Na análise da incidência de eventos tromboembólicos em cinco ECR, não houve diferença estatisticamente significativa entre a administração do ácido tranexâmico, comparado ao placebo (OR = 0,36, IC 95%: 0,11; 1,19, p = 0,09; I2 = 0%). No entanto, quando a perda sanguínea total estimada e a necessidade de transfusão de sangue foram analisadas, o uso do ácido tranexâmico foi associado a uma redução significativa, comparado ao placebo. (DM: −135,79, IC 95%: −179,50, −92,08, p < 0,00001, I2 = 68%) e (OR = 0,45, IC 95%: 0,32, 0,65, p < 0,00001, I2 = 60%), respectivamente.
Conclusões
Esta metanálise não encontrou evidências de que a administração de antifibrinolíticos aumente o risco de complicações tromboembólicas em pacientes submetidos à cirurgia oncológica e apresentou evidências de que é eficaz para reduzir a perda sanguínea total no perioperatório e a necessidade de transfusão de sangue.
PALAVRAS-CHAVE: Agentes antifibrinolíticos, Cirurgia oncológica, Tromboembolismo, Perda sanguínea
Introduction
The presence of anemia secondary to bleeding, to the malignancy or to chemotherapy is often seen in cancer patients, and it may increase the need for transfusion of blood products during surgery, mainly due to changes in the coagulation and fibrinolytic system. However, to correct blood loss and hemorrhagic shock, these patients are routinely submitted to transfusion of blood products, which, as it was already well documented in the literature, are not exempt from complications such as the increase of the transmission rate of infectious diseases, increased and potentially life-threatening immune response, increased acute lung injury and postoperative infections.1, 2 In addition, some studies have reported an independent association between blood transfusion and increased risk of cancer recurrence.3, 4
Authors have argued that cancer cells act by increasing fibrinolytic activity with the expression on their cell surface of the tissue plasminogen activator, of the urokinase type plasminogen activator and inhibitor of plasminogen activator Type 1.5 In this regard, since bleeding during oncological surgeries may be severe, antifibrinolytics, especially tranexamic acid (TXA), administered in the perioperative period have been shown to be effective in reducing blood loss and the need for allogeneic blood transfusion in cardiac,6 urological7, 8, 9 and orthopedic10, 11 surgeries as well as in liver transplants.12 In a systematic review with more than 10,000 patients undergoing different types of surgeries, it was suggested that TXA administration was able to reduce the need for blood transfusion in 38%.13
The only commonly used antifibrinolytics are TXA and Epsilon-Aminocaproic Acid (EACA). Aprotinin has been used as a blood-sparing agent in surgeries, but due to evidence of an increased risk of cardiovascular complications and mortality, its use is currently quite restricted.14 TXA is a synthetic derivative of the lysine amino acid that exerts its antifibrinolytic effects through the reversible blockade of the lysine binding site in the plasminogen molecule, it is 6–10 times more powerful than EACA and has a longer half-life. EACA, however, combines itself with plasminogen and free plasmin, preventing the fibrinolytic enzymes from binding to the lysine residues present in the fibrinogen molecule. Some studies have shown that EACA also inhibits plasmin-induced activation of plasminogen pro-urokinase and prevents the degradation of glycoprotein Ib receptors, thereby preserving platelet function.5, 15
Some studies have reported that patients with malignant cancer are more likely to develop thrombosis due to risk factors such as the production of pro-coagulant cancer cells, tissue factor, anti-angiogenic therapies, increased pre-chemotherapy platelet counts, agents erythropoiesis stimulants, D-dimer increase, advanced stage of disease and the location of the tumor (pancreas, stomach, gynecological, bladder, brain, hematologic and lung).16, 17, 18, 19 Although surgical and oncological patients present a high risk for thromboembolic complications in the perioperative period, with an incidence of 5%‒10%,20, 21 the risk of thrombosis was not a significant clinical problem in this population.22, 23
People with cancer are likely to bleed due to various conditions specific to the disease itself. The angiogenesis and neovascularization may be pronounced particularly in tumors with widespread dissemination and bulky as in advanced ovarian cancer.24, 25 There may also be bleeding secondary to the loss of hemostatic factors in the extravascular space, to hypoproteinemia, to the reduction of coagulation factors, to platelet dysfunction or to increased fibrinolysis.26 Studies have reported associations between ovarian cancer and hyperfibrinolysis as a result of elevated levels of D-dimer and other fibrin degradation products and reduction of antithrombin III. These changes in coagulation appear to be more pronounced in people with an advanced stage of disease.27, 28
It is essential to document the safety of the antifibrinolytic agent because it blocks the breakage of fibrin by preventing the binding of the plasminogen-plasmin tissue activator complex, thus facilitating the formation of the clot.29 This mechanism raised concerns about the potential to increase thromboembolic events in a population that has procoagulant factors.
Although the efficacy of the administration of antifibrinolytics in the perioperative period of several surgeries is already well documented in the literature, there are few studies that have evaluated the use of these drugs in cancer surgery and the risk of complications such as thromboembolism. Thus, we set out to research in this systematic review the safety and benefit of antifibrinolytics in this population.
Methods
This systematic review and meta-analysis study was performed according to the methods listed on the Cochrane Handbook for Systematic Reviews of Interventions.30
Eligibility criteria
Randomized clinical trials evaluating the use of antifibrinolytics (TXA or EACA) in patients of both sexes and aged ≥18 years submitted to oncologic surgery, with the main criterion being the analysis of thromboembolic events. Oncologic surgery is defined as a surgical procedure in a patient with neoplasm in any organ that has surgery as a treatment, whether for healing or non-healing purposes.
Studies that included another method in addition to intravenous antifibrinolytic therapy were eligible for screening if that other method was used in the active and control groups.
Studies that have evaluated the efficacy and/or safety of antifibrinolytic using the following parameters:
Venous thromboembolism recorded by an objective test (ultrasonography, fibrinogen absorption or venography for deep venous thrombosis, pulmonary ventilation perfusion scan, pulmonary angiography, or spiral computed tomography of pulmonary embolism), or arterial thrombosis (myocardial infarction, vascular or limb ischemia).
Estimated total volume of blood loss (mL).
Need for blood transfusion.
Types of result measures
Primary results
Incidence of arterial thromboembolic events (e.g. arterial thrombosis, myocardial infarction, stroke).
Incidence of venous thromboembolic events (e.g. venous thrombosis, pulmonary embolism).
Secondary results
Estimated blood loss.
Need for blood transfusion.
Search strategy
A research was conducted in PubMed, OVID, MEDLINE, EMBASE, EBSCO and in the Cochrane Central Register of Controlled Trial (CENTRAL).
The following keywords were used: “neoplasms” OR “surgical oncology” AND “antifibrinolytic agents” OR “antifibrinolytic agents” AND “clinical trial” OR “clinical trials as topic” OR “clinical trial” AND “humans” AND Clinical Trial. The research started from the first recoverable date of each database from August 2, 2017 until October 31, 2018. Articles written in all languages were searched.
Data collection and assessment
Selection of studies
Before examining the trials selected for possible inclusion, a data collection form was developed. All titles and abstracts retrieved by electronic search for a management database (EndNote) were downloaded and duplicated studies were removed. Three reviewers (A.M.S., G.M.N.G. and J.C.R.N.) separately examined the remaining references and assessed the eligibility of the selected publications. Researches that clearly did not meet the eligibility criteria were excluded. The risk of bias was assessed according to the Oxford Center for Evidence-Based Medicine. Full copies of potentially relevant texts were obtained. We assessed clinical trials, Meta-analyzes, case reports, cohort and reviews. Of these, clinical trials with a satisfactory level of evidence were selected. Any disagreement was solved through discussion or, when necessary, a fourth reviewer was consulted. We recorded the selection process with sufficient detail to design a flow chart and “Characteristics of excluded studies”.
Extraction and data management
Two reviewers (A.M.S. and J.C.R.N.) separately analyzed the characteristics, and the data results of the studies listed in a pre-piloted data collection form as well as the details of the experimental method, and the characteristics of both participants and interventions. Any disagreement was solved through discussion or, when necessary, a third party. The data was transferred to the Review Manager (RevMan) (Computer program; Version 5.3). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. The reviewers again analyzed whether the data were entered correctly by comparing the data presented in the systematic review with the study reports. A third reviewer (G.M.N.G.) verified the accuracy characteristics in the study following the test report. The authors of the selected trials were not contacted to confirm the accuracy of the extracted data and/or to provide any missing information or clarification. When more than one active treatment group was compared to a single control group (e.g. variable dose studies), the experimental groups were combined and then compared collectively with the control group.
Statistical analysis
The statistical of the collected data was performed using the program RevMan 5.3. The null hypothesis was discarded when the p-value was less than 0.05. For dichotomous results were calculated the Mantel–Haenzel Odds Ratios (OR) with 95% confidence intervals (CI). Continuous results data were expressed as the mean difference (MD).
The results for heterogeneity (I2) were tested and considered significant when I2 > 50% for a value of p < 0.05, according to the methods developed by DerSimonian and Laird.31 The fixed effects model was used when there was no evidence of heterogeneity among the studies; if there was any evidence of heterogeneity, the random effect model was used for meta-analysis. 95% OR and CI were calculated for each assay presented as forest plots. When possible, the assessment was done separately for each group by calculating 95% of OR and CI for each comparison. We evaluated the heterogeneity among the studies using the I2 statistic. Publication bias was assessed using the funnel plot.
Results
Trials included
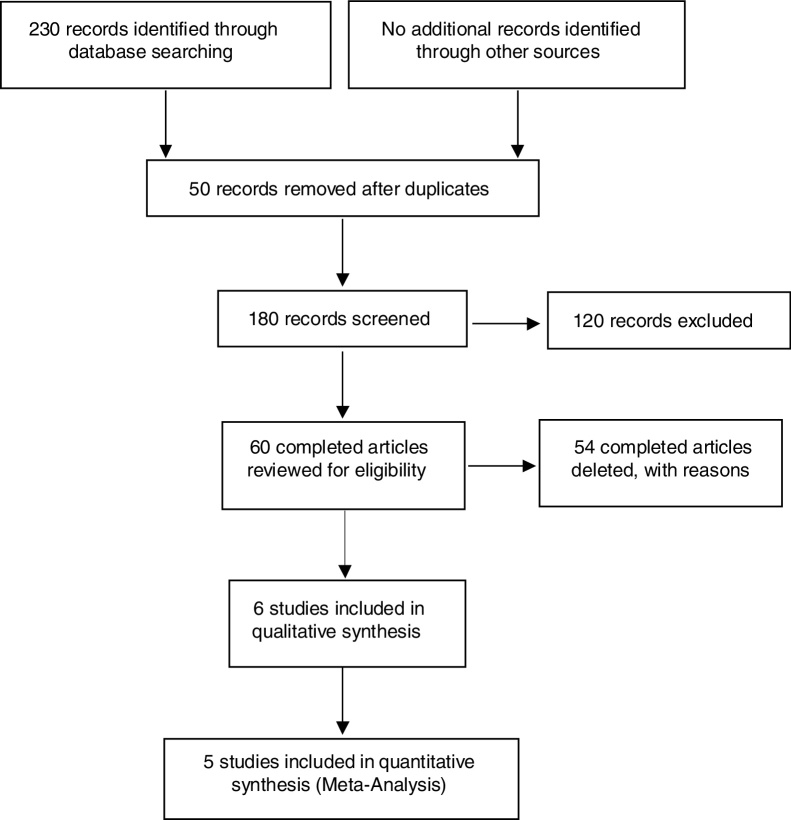
In the initial bibliographic survey, 230 publications were identified. After sorting the titles, abstracts and detailed evaluation, 5 randomized clinical trials (RCTs) where selected to be included in the quantitative synthesis, as detailed in the tracking algorithm (Fig. 1). The 5 trials included5, 9, 25, 32,33 in our study with 838 patients were published between 2006 and 2016 and all used a placebo as a comparator (Table 1).
Figure 1.
Flowchart of the search process, screening and exclusion of studies.
Table 1.
Characteristics of included studies.
| Studies | Sample size | Neoplasms | Dose | Intraoperative blood loss (mL) |
24 h blood loss (mL) |
Red blood cell transfusion unit/rate (%) |
Arterial and venous thromboembolism |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Ano) | (n) | Surgery | TXA | TXA | Placebo | TXA | Placebo | TXA | Placebo | TXA (n) | Placebo (n) |
| Crescenti (2011) | 200 | Prostate | 500 mg before surgery and 250 mg.h-1 until close the skin | 1103 ± 500.8 | 1335 ± 686.5 | 22/39 | 37/67 | 2 | 3 | ||
| Celebi (2006) | 105 | Uterine cervix | 10 mg.kg-1 before surgery | 270 ± 40 | 390 ± 35 | 0 | 0 | ||||
| Lundin (2014) | 100 | Ovary | 15 mg.kg−1 before surgery | 520 (−772 to 3351) | 730 (23–3855) | 0.76 ± 1.45/15 | 1.06 ± 1.49/22 | 2 | 5 | ||
| Kulkami (2016) | 219 | Head and neck | 10 mg.kg-1 before surgery | 750 (600‒1000) | 780 (150‒ 2600) | 1000 (735‒1250) | 1110 (850‒ 1467) | 22 | 27 | 0 | 0 |
| Wu (2006) | 214 | Liver | 500 mg before surgery and 250 mg 6/6 h for 3 days | 300 (30‒ 2100) | 600 (40‒ 3410) | 0 | 17 | 0 | 0 | ||
Quality evaluation
Five articles directly comparing intraoperative and postoperative period, thromboembolic events, blood loss and the need for blood transfusion with and without administration of TXA or EACA in patients undergoing oncologic surgeries were included in this meta-analysis. No articles with aprotinin were found. The sample size of these studies ranged from 100 to 219. TXA was present in all studies, but the EACA was only in one. The five trials reported both an adequate sequence generation and an allocation concealment. The amount of risk was assessed in relation to a number of factors, including random sequence generation, allocation concealment, blinding, selective reporting and other possible biases as well as to GRADE the quality of the evidence.34 See study Table 2.
Table 2.
Summary of results.
| Outcome | Quality of the evidence |
Effect Estimate (95% CI) | Quality (GRADE) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Study design | No of participants (studies) | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication Bias | |||
| Thromboembolic events | RCT | 838 (5 studies) | Serious risk of bias, downgrade one level | Low heterogeneity | Not appear to be an issue | Some imprecision exists: Few events | Observed asymmetry in funnel plot | OR: 0.36 (0.11‒1.19) | ⊕⊕OO Low |
| Estimated total blood loss | RCT | 838 (5 studies) | Serious risk of bias, downgrade one level. | Substantial heterogeneity | Not appear to be an issue | Some imprecision exists: Few events and wide confidence intervals | Observed asymmetry in funnel plot | MD:-135.79 ( -179.50 to -92.08) | ⊕⊕OO Low |
| Need for blood transfusion | RCT | 838 (5 studies) | Serious risk of bias, downgrade one level. | Substantial heterogeneity | Not appear to be an issue | Some imprecision exists: Few events | Observed asymmetry in funnel plot | OR = 0.45 (0.32‒0.65) | ⊕⊕OO Low |
RCT, randomized clinical trials; CI, confidence interval; MD, mean difference; OR, odds ratios.
GRADE of evidence: high quality, the true effect lies close to that of the estimate of the effect; moderate quality: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; low quality: the true effect may be substantially different from the estimate of the effect; very low quality: the true effect is likely to be substantially different from the estimate of effect.
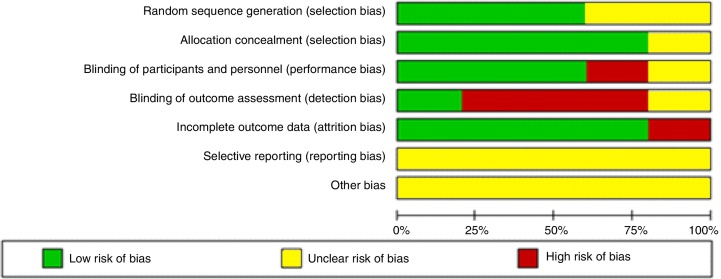
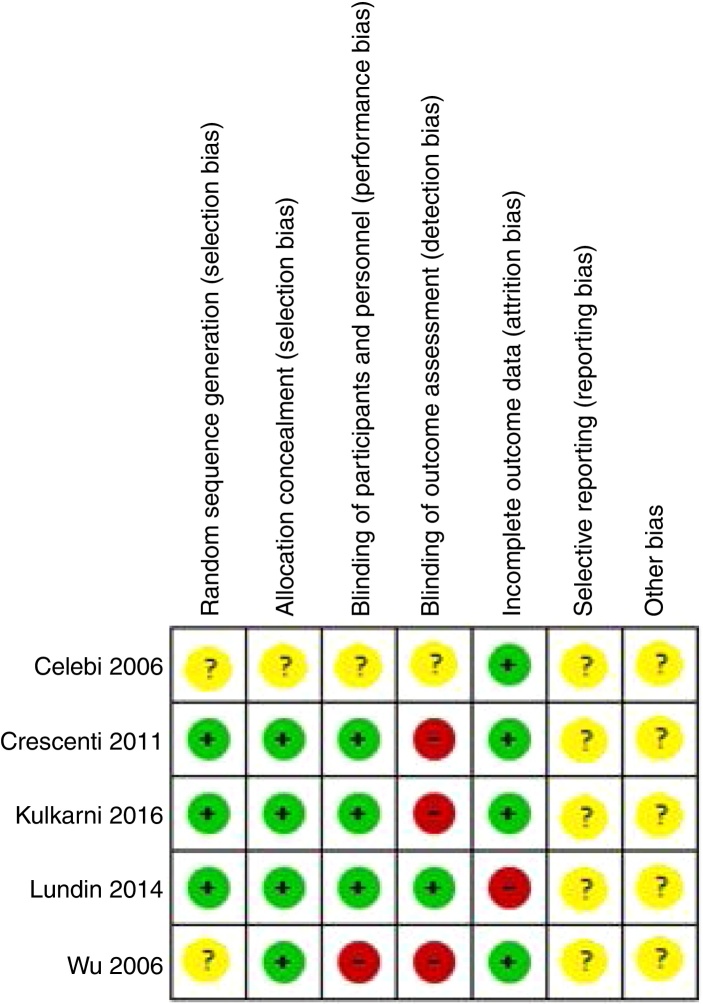
The results for the publication bias were evaluated and shown in Figure 2, Figure 3. The study by Amar et al.35 was excluded because the researchers did not investigate thromboembolic complications between the groups, according to the characteristics of the excluded studies.
Figure 2.
Risk of bias summary: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.
Risk of bias summary: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
Effects of intervention
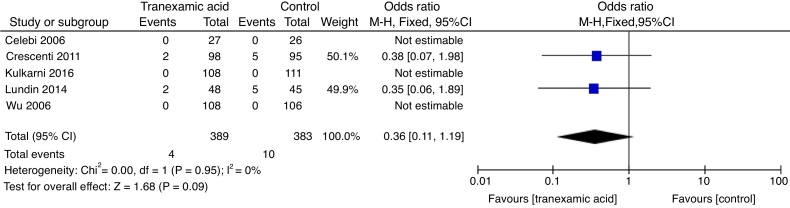
Thromboembolic events
There was no evidence of difference in relation the incidence of thromboembolic events with tranexamic acid administration when compared to placebo (OR = 0.36, 95% CI: 0.11‒1.19, p = 0.09, I2 = 0%) (Fig. 4).
Figure 4.
Forest plot of comparison: 1 analysis of the comparison of tranexamic acid versus placebo in thromboembolic complications.
Estimated total blood loss
Tranexamic acid vs. placebo
The use of tranexamic acid was associated to a significant reduction in total perioperative blood loss when compared to placebo (MD = −135.79, 95% CI: −179.50 to −92.08, p < 0.00001). The heterogeneity of (I2 = 68%) was statistically significant (p = 0.01) (Fig. 5).
Figure 5.
Forest plot of comparison: 2 analysis of the comparison of tranexamic acid versus placebo in the estimated total blood loss.
Need for blood transfusion
Tranexamic acid vs. placebo
The use of tranexamic acid was associated with significant reduction of the need for blood transfusion when compared to placebo (OR = 0.45, 95% IC: 0.32‒0.65, p < 0.00001, I2 = 60%) (Fig. 6).
Figure 6.
Forest plot of comparison: 3 analysis of the comparison of tranexamic acid versus placebo in the need for blood transfusion.
Discussion
This study investigated the administration of antifibrinolytics in oncologic surgeries in five RCTs, with 838 patients, and the association of these drugs in the reduction of blood loss, blood transfusion and thromboembolic events. However, there was a need for a meta-analysis to provide scientific evidence related to this type of surgery. There is a study in which the authors approached only gynecologic oncological surgeries, reinforcing the need for further studies on this topic.36
This meta-analysis did not find statistical significance in the incidence of thromboembolic events (OR = 0.36, 95% CI: 0.11‒1.19), when TXA was compared with the placebo in the 5 RCTs. Similarly, Zaid et al.7 did not show an increased risk of thromboembolic complications in a cohort of 200 patients who underwent radical prostatectomy using TXA and a 6 month follow-up. Gupta et al.37 also did not find an increased risk of thromboembolic complications with the prophylactic administration of intraoperative TXA in radical surgery.
In this review, there was significant reduction in blood loss (MD: −135.79, 95% CI: −179.50 to −92.08) and in the need for blood transfusion (OR = 0.45, 95% IC: 0.32‒0.65), in patients who received TXA when compared to those receiving placebo. In accordance with our results, Wu et al.32 reported in a randomized clinical trial with 214 patients that in resections of liver tumors, perioperative blood loss as well as need for blood transfusion were significantly reduced in the TXA group when compared with placebo.
In a recent meta-analysis, similarly to our findings, the authors argued that the administration of antifibrinolytics was not associated with increased risk of venous thromboembolism, and that they were effective in reducing blood loss and the need for transfusion.38
Kietpeerakool et al.16 corroborating with this review, evidenced in the meta-analysis, evaluating patients with advanced ovarian cancer submitted to cytoreductive surgery, that the TXA was associated with a significant reduction of blood loss. But, on the other hand, disagreeing this study, these authors evidenced no significant difference in the need for blood transfusion between the groups. Additionally, in a randomized controlled trial, the authors did not observe a significant difference in blood loss during orthopedic surgeries in cancer patients receiving antifibrinolytics.35
Despite the inclusion of only randomized clinical trials to increase the quality of this analysis, there are some limitations such as the small number of samples, significant amount of heterogeneity among several of the results, variations in the population under study, type of surgery performed, methodology and different doses among the different studies may explain the heterogeneity. Moreover, the analysis of bleeding and thromboembolic events varied in the researches, which may interfere with the result. In addition, thromboembolism was only investigated if there had been any clinical evidence, and which may have underestimated the frequency of this complication. Thus, the data need to be evaluated with caution, since these parameters usually require larger studies. More randomized clinical trials are needed to further confirm the results of this meta-analysis.
This meta-analysis found no evidence that the administration of antifibrinolytics in patients undergoing oncologic surgery increases the risk of thromboembolic complications but suggests that it is effective in reducing total perioperative blood loss and the need for blood transfusion.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Alter H.J., Klein H.G. The hazards of blood transfusion in historical perspective. Blood. 2008;112:2617–2626. doi: 10.1182/blood-2008-07-077370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amer K., Rehman S., Amer K., et al. Efficacy and safety of tranexamic acid in orthopedic fracture surgery: a meta-analysis and systematic literature review. J Orthop Trauma. 2017;31:520–525. doi: 10.1097/BOT.0000000000000919. [DOI] [PubMed] [Google Scholar]
- 3.De Oliveira G.S., Jr., Schink J.C., Buoy C., et al. The association between allogeneic perioperative blood transfusion on tumour recurrence and survival in patients with advanced ovarian cancer. Transfus Med. 2012;22:97–103. doi: 10.1111/j.1365-3148.2011.01122.x. [DOI] [PubMed] [Google Scholar]
- 4.Schiergens T.S., Rentsch M., Kasparek M.S., Frenes K., Jauch K.W., Thasler W.E. Impact of perioperative allogeneic red blood cell transfusion on recurrence and overall survival after resection of colorectal liver metastases. Dis Colon Rectum. 2015;58:74–82. doi: 10.1097/DCR.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni A.P., Chaukar D.A., Patil V.P., et al. Does tranexamic acid reduce blood loss during head and neck cancer surgery. Indian J Anaesth. 2016;60:19–24. doi: 10.4103/0019-5049.174798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andreasen J.J. Pharmacologic methods to reduce postoperative bleeding in adult cardiac surgery. A mini-review. Curr Pharm Des. 2013;19:3992–3995. doi: 10.2174/1381612811319220007. [DOI] [PubMed] [Google Scholar]
- 7.Zaid H.B., Yang D.Y., Tollefson M.K., et al. Efficacy and safety of intraoperative tranexamic acid infusion for reducing blood transfusion during open radical cystectomy. Urology. 2016;92:57–62. doi: 10.1016/j.urology.2016.02.044. [DOI] [PubMed] [Google Scholar]
- 8.Rannikko A., Pétas A., Taari K. Tranexamic acid in control of primary hemorrhage during transurethral prostatectomy. Urology. 2004;64:955–958. doi: 10.1016/j.urology.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Crescenti A., Borghi G., Bignami E., et al. Intraoperative use of tranexamic acid to reduce transfusion rate in patients undergoing radical retropubic prostatectomy: double blind, randomised, placebo controlled trial. BMJ. 2011;343 doi: 10.1136/bmj.d5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim C., Park S.S.-H., Davey J.R. Tranexamic acid for the prevention and management of orthopedic surgical hemorrhage: current evidence. J Blood Med. 2015;6:239–244. doi: 10.2147/JBM.S61915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alshryda S., Sarda P., Sukeik M., et al. Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Br. 2011;93:1577–1585. doi: 10.1302/0301-620X.93B12.26989. [DOI] [PubMed] [Google Scholar]
- 12.Badenoch A., Sharma A., Gower S., et al. The effectiveness and safety of tranexamic acid in orthotopic liver transplantation clinical practice: a propensity score matched cohort study. Transplantation. 2017;101:1658–1665. doi: 10.1097/TP.0000000000001682. [DOI] [PubMed] [Google Scholar]
- 13.Ker K., Edwards P., Perel P., et al. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054. doi: 10.1136/bmj.e3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henry D.A., Carless P.A., Moxey A.J., et al. Antifibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2011 [Google Scholar]
- 15.Mannucci P.M., Levi M. Prevention and treatment of major blood loss. N Engl J Med. 2007;356:2301–2311. doi: 10.1056/NEJMra067742. [DOI] [PubMed] [Google Scholar]
- 16.Modrau I.I., Iversen L.L., Thorlacius-Ussing O.O. Hemostatic alterations in patients with benign and malignant colorectal disease during major abdominal surgery. Thromb Res. 2001;104:309–315. doi: 10.1016/s0049-3848(01)00373-5. [DOI] [PubMed] [Google Scholar]
- 17.Sud R., Khorana A.A. Cancer-associated trombosis: risk factors, candidate biomarkers and a risk model. Thromb Res. 2009;123:S18–21. doi: 10.1016/S0049-3848(09)70137-9. [DOI] [PubMed] [Google Scholar]
- 18.Blom J.W., Doggen C.J., Osanto S., et al. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293:715–722. doi: 10.1001/jama.293.6.715. [DOI] [PubMed] [Google Scholar]
- 19.Prandoni P., Falanga A., Piccioli A. Cancer and venous thromboembolism. Lancet Oncol. 2005;6:401–410. doi: 10.1016/S1470-2045(05)70207-2. [DOI] [PubMed] [Google Scholar]
- 20.Wang J.K., Boorjian S.A., Frank I., et al. Non-O blood type is associated with an increased risk of venous thromboembolism after radical cystectomy. Urology. 2014;83:140–145. doi: 10.1016/j.urology.2013.08.046. [DOI] [PubMed] [Google Scholar]
- 21.Sun A.J., Djaladat H., Schuckman A., et al. Venous thromboembolism following radical cystectomy: significant predictors, comparison of different anticoagulants and timing of events. J Urol. 2015;193:565–569. doi: 10.1016/j.juro.2014.08.085. [DOI] [PubMed] [Google Scholar]
- 22.Molenaar I.Q., Warnaar N., Groen H., et al. Efficacy and safety of antifibrinolytic drugs in liver transplantation: a systematic review and meta-analysis. Am J Transplant. 2007;7:185–194. doi: 10.1111/j.1600-6143.2006.01591.x. [DOI] [PubMed] [Google Scholar]
- 23.Levy J.H., Koster A., Quinones Q.J., et al. Antifibrinolytic therapy and perioperative considerations. Anesthesiology. 2018;128:657–670. doi: 10.1097/ALN.0000000000001997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Obaji S., Alikhan R., Rayment R., et al. Unclassified bleeding disorders: outcome of haemostatic challenges following tranexamic acid and/or desmopressin. Haemophilia. 2016;22:285–291. doi: 10.1111/hae.12811. [DOI] [PubMed] [Google Scholar]
- 25.Lundin E.S., Johansson T., Zachrisson H., et al. Single-dose tranexamic acid in advanced ovarian cancer surgery reduces blood loss and transfusions: double-blind placebo-controlled randomized multicenter study. Acta Obstet Gynecol Scand. 2014;93:335–344. doi: 10.1111/aogs.12333. [DOI] [PubMed] [Google Scholar]
- 26.Kvolik S., Jukic M., Matijevic M., et al. An overview of coagulation disorders in cancer patients. Surgical Oncol. 2010;19:e33–46. doi: 10.1016/j.suronc.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 27.Gadducci A., Baicchi U., Marrai R., et al. Pretreatment plasma levels of fibrinopeptide-A (FPA), D-dimer (DD), and von Willebrand factor (vWF) in patients with ovarian carcinoma. Gynecol Oncol. 1994;53:352–356. doi: 10.1006/gyno.1994.1146. [DOI] [PubMed] [Google Scholar]
- 28.Koh S.C., Khalil R., Lim F.K., Ilancheran A., Choolani M. The association between fibrinogen, vonWillebrand Factor, antithrombin III, and D-dimer levels and survival outcome by 36 months from ovarian cancer. Clin Appl Thromb Hemostat. 2006;12:3–8. doi: 10.1177/107602960601200102. [DOI] [PubMed] [Google Scholar]
- 29.Sitalakshmi S., Rameshkumar K., Damodar P. Significance of haemostatic markers in ovarian carcinoma. Indian J Med Paediatr Oncol. 2008;29:6–10. [Google Scholar]
- 30.Higgins J.P.T., Green S. The Cochrane Collaboration; 2011. Cochrane handbook for systematic reviewsof interventions. Version 333 5.1.0 The Cochrane Collaboration;2011. https://training.cochrane.org/handbook Available from.
- 31.DerSimonian R., Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Wu C.C., Ho W.M., Cheng S.B., et al. Perioperative parenteral tranexamic acid in liver tumor resection: a prospective randomized trial toward a "blood transfusion"-free hepatectomy. Ann Surg. 2006;243:173–180. doi: 10.1097/01.sla.0000197561.70972.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Celebi N., Celebioglu B., Selcuk M., et al. The role of antifibrinolytic agents in gynecologic cancer surgery. Saudi Med J. 2006;27:637–641. [PubMed] [Google Scholar]
- 34.Ryan R., Hill S. Cochrane Consumers and Communication Group; 2016. How to GRADE the quality of the evidence. http://cccrg.cochrane.org/author-resources Version 3.0 December 2016. Available at.
- 35.Amar D., Grant F.M., Zhang H., et al. Antifibrinolytic therapy and perioperative blood loss in cancer patients undergoing major orthopedic surgery. Anesthesiology. 2003;98:337–342. doi: 10.1097/00000542-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Kietpeerakool C., Supoken A., Laopaiboon M., et al. Effectiveness of tranexamic acid in reducing blood loss during cytoreductive surgery for advanced ovarian cancer. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD011732.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gupta K., Rastogi B., Krishan A., et al. The prophylactic role of tranexamic acid to reduce loss blood during radical surgery: a prospective study. Anesth Essays Res. 2012;6:70–73. doi: 10.4103/0259-1162.103378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Montroy J., Fergusson N.A., Hutton B., et al. The safety and efficacy of lysine analogues in cancer patients: a systematic review and meta-analysis. Transfus Med Rev. 2017;31:141–148. doi: 10.1016/j.tmrv.2017.03.002. [DOI] [PubMed] [Google Scholar]