Abstract
Objective
Build a microlaryngoscopy surgical simulator for endoscopic laryngeal surgery using standard microsurgical instruments and a CO2 laser.
Study design
Anatomical modeling, CAD design and 3D printed manufacturing.
Subjects and methods
We created a modular design for a microlaryngoscopy simulator in CAD software. Components include plastic and stainless‐steel models of a standard operating laryngoscope and a cassette system for mounting porcine or synthetic models of the vocal folds. All simulator parts, including the metallic laryngoscope model, were manufactured using 3D printing technology. Tumors were simulated in porcine tissue models by injecting a soy protein‐based tumor phantom. Residents and faculty in the Louisiana State University otolaryngology department evaluated the system. Each participant performed microlaryngoscopy with laser resection on a porcine larynx and cold instrument procedures on synthetic vocal folds. Participants scored the simulator using a 5‐point Likert scale.
Results
The microlaryngeal surgical simulator demonstrated in this project is realistic, economical, and easily assembled. We have included 3D printed parts files and detailed assembly instructions that will enable educators interested in surgical simulation to build the device.
Participants in the simulator evaluation session felt that the simulator faithfully represented the procedure to resect vocal fold lesions using a CO2 laser. The synthetic model allows the trainee to develop hand‐eye coordination while using standard laryngeal instruments.
Conclusions
The simulator described herein will enable surgeons to acquire the surgical skills necessary to perform operative microlaryngoscopy prior to operating on live patients.
Keywords: 3D printing, CO2 laser, microlaryngoscopy, surgical simulation
This article describes a microlaryngoscopy surgical simulator suitable for teaching trainees the basics of endoscopic laryngeal surgery. It includes the resources and detailed assembly instructions that readers can use to build the device.
1. INTRODUCTION
Microlaryngoscopy is one of the most difficult procedures that otolaryngology residents must master during their training. General tasks include learning to work though the microscope, safe application of the laser and developing proficiency in microlaryngoscopy instrument placement.
Advances in computer technology and the commercialization of three‐dimensional printing have enabled simulation for many surgical procedures. Published reports include applications in general surgery, otolaryngology, neurosurgery, gastroenterology, urology, and cardiovascular surgery. 1 , 2 , 3
Surgical simulators can be classified into four categories ‐ bench models, animal models, human cadavers, and virtual reality (VR). Live animals and human cadavers are useful for training courses and anatomical dissection, but they are difficult to acquire on a regular basis and are not reusable. Recently, most surgical simulation investigators have focused on VR systems. 4 , 5 , 6 The VR movement has been aided by advances in graphics processing unit (GPU) technology, computer graphics software and hardware including 3D visualization and haptic feedback devices. While VR is promising for some procedures, resemblance to corresponding in‐vivo procedures and validated effectiveness is lacking in many cases. 7 Bench models attempt to replicate the surgical field and simulate tissue interactions with the same instruments used for the corresponding in‐vivo procedure. Advances in affordable 3D printing have recently facilitated the development of these types of models. 8
We describe a combined animal‐bench model device engineered for the realistic simulation of microlaryngoscopy procedures including laryngeal tumor resection and endoscopic laryngeal suturing. Simulated procedures are performed using an operating microscope, a CO2 laser, and standard microlaryngoscopy instruments. Innovative features include a modular design that allows the use of porcine and synthetic larynges, an injectable tumor phantom to simulate early‐stage laryngeal carcinoma, and silicone vocal fold surrogates used for the synthetic larynges.
2. MATERIALS AND METHODS
The project was a joint effort of the Louisiana State University Health Sciences Center Department of Otolaryngology and the Biological Engineering Department of the Louisiana State University School of Engineering. Six undergraduate biological engineering students developed the simulator as part of a one‐year senior capstone design project. Engineering and otolaryngology faculty guided the project.
2.1. Laryngeal simulator construction
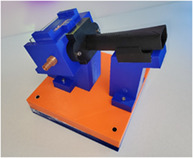
The completed simulator is shown in Figure 1. The design includes the laryngoscope, a cassette system to hold sections of the porcine larynx or synthetic focal folds, mounts for the laryngoscope and cassette carrier, and a weighted base. We modeled the laryngoscope after a standard adult operating scope. The cassette incorporates a smoke evacuation port and a plexiglass plate mounted behind the cassette to secure it in place and provide a barrier to CO2 laser light escape. The cassette design allows rapid exchange of the laryngeal sections. Users can preassemble and store cassettes prior to use. The main system components were 3D printed. The online supplement provides a detailed, illustrated description of the device assembly, a parts list with suppliers, and a set of stereolithography (.stl) part files for 3D printing.
FIGURE 1.
Microlaryngoscopy simulator with cassette inserted
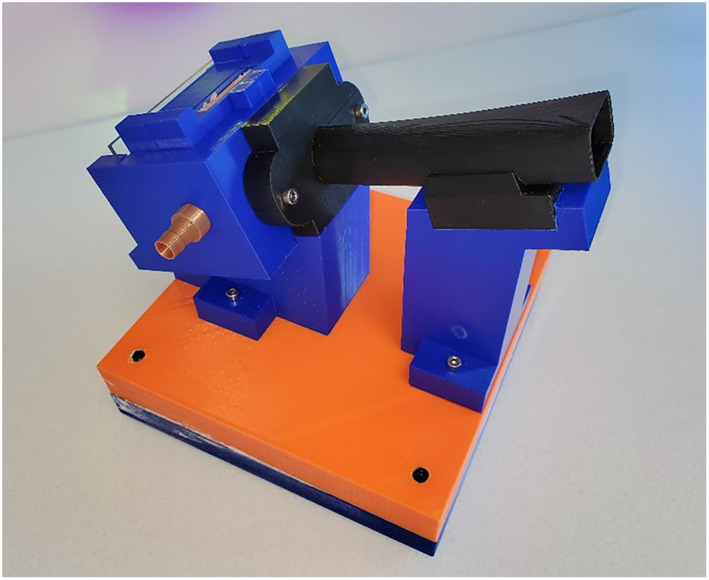
We injected porcine specimens with a soy protein‐gelatin based bio‐ink to simulate laryngeal carcinoma (Figure 2). Details are provided in the supplement.
FIGURE 2.
Porcine larynx injected with pigmented tumor phantom
For the synthetic vocal folds, a 3D model of a human laryngeal cross‐section containing the vocal folds was created from CT images. A nodular displacement on one of the vocal folds was added to simulate tumor. A negative mold of the computer model was 3D printed which was then injected with a mixture of curable silicone to create the synthetic laryngeal section (see supplement).
2.2. Tumor phantom bio‐ink preparation
We use a soy protein–gelatin–alginate preparation as bio‐ink for the tumor phantom. Soy protein isolate (SPI) powder was used without modification and forms the base component. It has low viscosity for injectability. Unmodified porcine gelatin, type A, was used to thicken and stabilize the preparation. Low‐viscosity sodium alginate was used in conjunction with the gelatin as a thickener. As an emulsifier, alginate improves ink consistency. After testing a series of formulations, we settled on a preparation of soy protein with 10% gelatin by weight (SG‐10) for the injectable tumor phantom (see supplement).
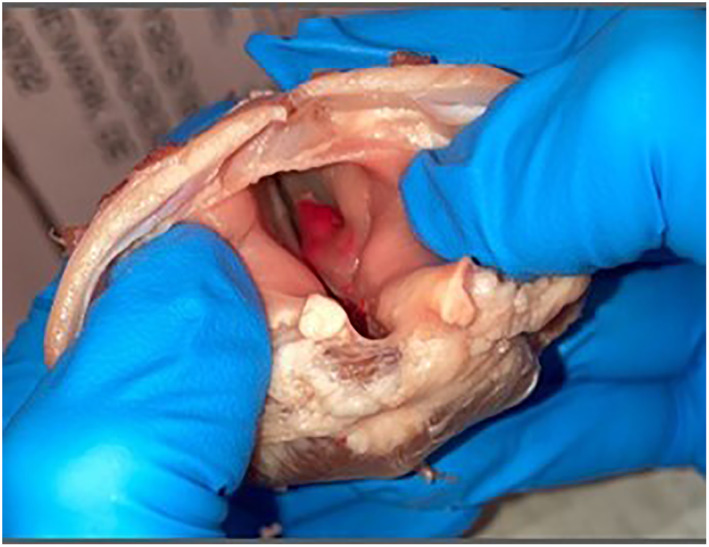
2.3. Porcine larynx preparation
Fresh frozen porcine larynges were obtained commercially. Each larynx was prepped and sectioned using the protocol described in the supplement. The sections were mounted between the upper and lower plates of the cassette and placed in the cassette carrier by sliding the cassette forward into the laryngoscope field (Figure 3). A plexiglass plate secures the cassette in place.
FIGURE 3.
Porcine laryngeal section in cassette and cassette carrier
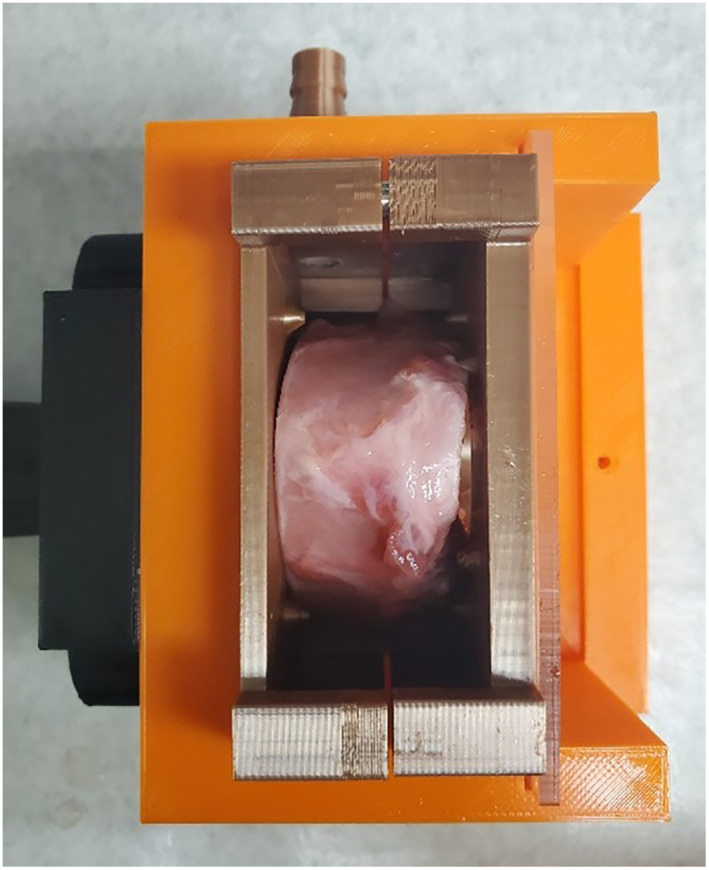
2.4. Synthetic laryngeal section preparations
Similarly, the synthetic laryngeal sections were mounted between cassette plates and placed in the cassette holder (Figure 4). The synthetic sections were 20 mm in thickness. Details are provided in the supplement.
FIGURE 4.
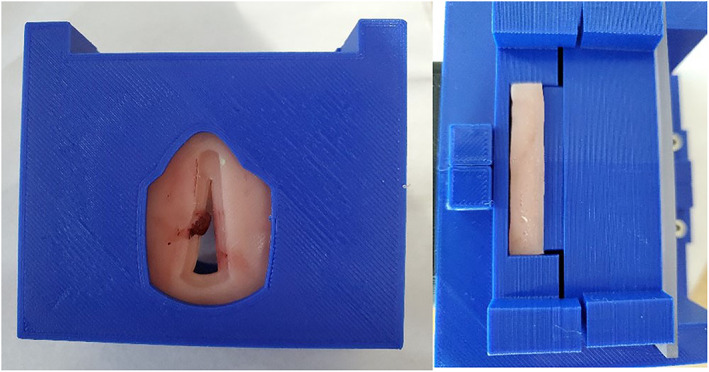
Synthetic vocal fold model and cassette
2.5. Simulator validation
The device was evaluated for face and content validity at the Louisiana State University Center for Advanced Practice Laboratory in New Orleans, LA. Eighteen participants performed microlaryngoscopy with laser resection on a porcine larynx and cold resection (microlaryngoscopy forceps and scissors) on a synthetic larynx. Following completion of the simulation tasks, each participant was asked to complete a survey assessing face validity of the simulator. The survey consisted of 17 questions, each rated on a Likert Scale of 1–5 (strongly disagree to strongly agree). Each participant was also given the opportunity to provide free text comments related to the simulator, equipment, and specimen. A total of 18 surveys were completed by 15 otolaryngology residents (post graduate years 1 through 5) and 3 attendings.
3. RESULTS
The simulator can be assembled from 3D printed parts costing around 400 $US for the plastic laryngoscope model suitable for synthetic focal fold inserts and standard microlaryngoscopy instruments. The stainless‐steel version for the porcine inserts and CO2 laser surgical simulation costs approximately 1200 $US. The overall dimensions of the device are 20 × 19 × 19 cm. Once the 3D printed parts are completed, assembly takes about 2 h.
Representative simulator use is shown in Figure 5. Endo‐laryngeal views are illustrated in Figure 6. Overall, participants felt that this simulator was a valuable training exercise. The porcine and synthetic larynges closely mimic actual laryngeal anatomy with the porcine larynges more closely resembling the consistency of human tissue. The basic skills employed during the simulator exercises correlated well with those required for microlaryngeal surgery, including hand eye coordination, bimanual use of endoscopic laryngeal instruments, and basic CO2 laser skills. Of the three participating attendings, all would be interested in using this model to train residents and felt that it would increase resident competency when used prior to their first transoral laser microsurgical procedure.
FIGURE 5.
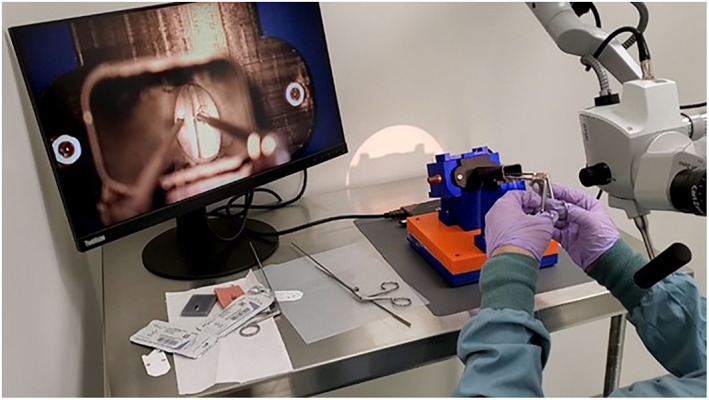
Microlaryngoscopy simulator in use
FIGURE 6.
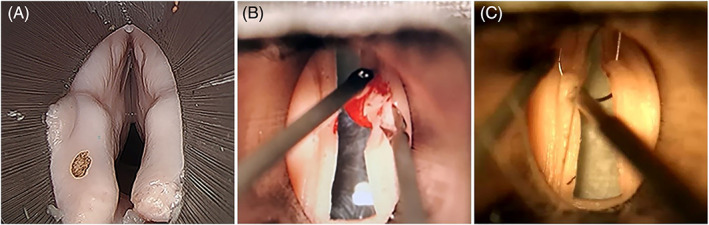
Endo‐laryngeal views during simulator use (A, porcine laryngeal section, B, synthetic vocal folds, tumor resection, and C, synthetic vocal folds, suture technique)
Skills specific to tumor resection including mobilizing a glottic tumor for excision and removing the lesion en bloc were rated favorably. However, participants found that the technical skills for evaluating tumor depth within the vocal folds and evaluating tumor margins were not as realistic. The survey results are shown in Table 1.
TABLE 1.
Validation survey results
| Likert Scale Survey Results (1 = strongly disagree, 5 = strongly agree) | ||
|---|---|---|
| Average ± SD | % agreement (Likert ≥4) | |
| Portions of this model simulated an actual case start to finish | 4.11 ± 0.94 | 83.3% |
| The model is high fidelity and closely mimics actual laryngeal anatomy | 4.17 ± 0.76 | 88.9% |
| This model helps to develop skills needed for laryngeal exposure | 4.19 ± 0.95 | 70.6% |
| This model helps to develop hand eye coordination needed for endoscopic laryngeal surgery | 4.83 ± 0.37 | 100% |
| This model helps develop bimanual dexterity in endoscopic laryngeal surgery | 5.0 ± 0 | 100% |
| The model correlates with essential skills needed for laryngeal surgery | 4.88 ± 0.32 | 100% |
| This model helps to develop basic instrumentation skills for endoscopic laser surgery | 4.83 ± 0.14 | 100% |
| This model helps to develop basic use of CO2 laser for excising lesions | 4.89 ± 0.31 | 100% |
| The transoral laser microsurgery simulator is a valuable training exercise | 4.83 ± 0.14 | 100% |
| This model helps develops basic use of the endoscopic instruments to mobilize a glottic tumor for excision | 4.61 ± 0.59 | 94.5% |
| This model helps develop basic knowledge of evaluating tumor depth within the vocal folds | 3.59 ± 0.97 | 47.1% |
| This model helps to develop basic skills for removing a lesion en‐bloc | 4.56 ± 0.60 | 94.5% |
| This model helps to develop skills for evaluating margins of a glottic cancer | 3.41 ± 0.97 | 41.2% |
| This model allows for appropriate depth perception | 3.88 ± 1.17 | 68.8% |
| Use of this model will increase resident competency when used to train residents prior to their first transoral laser microsurgery | 4.94 ± 0.23 | 100% |
| The model is an adequate training model for future surgeons | 4.78 ± 0.42 | 100% |
| I would be interested in using the model to train residents | 4.83 ± 0.50 | 100% |
4. DISCUSSION
The past 20 years have seen a trend towards more conservative, larynx sparing surgery for stage I, II, and selected stage III laryngeal carcinoma performed through a trans‐oral, endoscopic approach. Achieving adequate resection margins can be challenging, especially for inexperienced surgeons. In 2019, a retrospective review of the National Cancer Database found that 22.3% of patients undergoing transoral laser microsurgery for T1S–T3 laryngeal carcinoma had positive oncologic margins. 9 Positive margins are associated with high rates of recurrence, revision surgery and the need for adjuvant radiation therapy and chemotherapy.
Peroral laryngeal surgery is one of the more technically challenging procedures performed by otolaryngologists. Difficulties in training include the need for a single operator, reduced visualization in a narrow cylindrical field, long fulcrum instrumentation and the need to master surgery using an operating microscope. This study documents the potential for meaningful simulation of microlaryngeal surgery with and without the laser. The modular design and incorporation of real tissue and synthetic models promotes efficient implementation of the device.
With advances in computer graphics and 3D print manufacturing, surgical simulation has become a more pervasive form of training for advanced surgical skills. Simulation is playing an expanding role in resident education and procedural skills demonstration. Realistic simulation requires the same visual and haptic perceptions as the actual surgical procedure. Much of the current research in surgical simulation involves VR devices. 10 While VR has achieved highly realistic visual simulations of surgical anatomy, touch perception and instrument simulation are often lacking. Bench model simulators allow trainees to use the same instruments deployed in the operating room but often lack the perception of real tissue. 1
Here we chose to develop a hybrid bench model for laryngeal simulation using porcine laryngeal tissue supplemented with a soy protein isolate tumor phantom. In aqueous solution, SPI crosslinks to form a semisolid material hydrogel. The properties of the crosslinked compound can be controlled with the addition of thickeners and emulsifiers. The mechanical properties of the target tissue, laryngeal tumor in this case, can be predicted from rheological measures of elasticity and stress–strain relationships. The bovine laryngeal sections require manual pre‐processing but are suitable for the injectable tumor phantom and CO2 laser surgical simulations.
The synthetic laryngeal sections provide simple, yet highly realistic, models useful for learning basic microlaryngoscopy instrument skills. Study participants rated the synthetic sections nearly as realistic as the porcine models for tumor resection. The synthetic models are also useful for practicing endoscopic laryngeal suturing.
Face validity is a subjective assessment of the simulator's realism. It reflects the model's anatomical accuracy and the fidelity of the simulated tissue types. Content validity assesses the simulated procedure relative to live surgery (i.e., are the instruments the same, is the positioning of the patient the same, etc.). 11 In this study we used a simple postsimulation Likert scale questionnaire to assess validity. With additional refinements to the simulator, we plan to perform a more comprehensive evaluation including construct (ability to differentiate trained from untrained subjects) and predictive (performance measures in human patients) validation.
5. CONCLUSIONS
This microlaryngoscopy surgical simulator will allow surgeons in training to develop skills to resect laryngeal tumors and perform endolaryngeal suturing. It is unique in its modular design and the incorporation of real tissue with phantom tumor simulation as well as easily created synthetic models. Advantages over existing simulators include the use of standard operating instrumentation with a microscope and realistic tumor simulation. It can also be used for surgical laser training.
FUNDING INFORMATION
Louisiana State University Health Sciences Center–resident research grant.
CONFLICT OF INTEREST
The author declares there is no potential conflicts of interest.
Supporting information
Supplementary Materials. Stereolithography files for 3D printed parts ‐ laryngeal_simulator_parts.zip.
Microlaryngoscopy simulator assembly instructions–laryngeal_assembly.docx.
ACKNOWLEDGMENTS
Lumenis Ltd.–provided laser for microlaryngoscopy simulation.
Zeiss Optical–provided microscope for microlaryngoscopy simulation.
Bressler SE, Adkins LK, Dunham ME, et al. A modular surgical simulator for microlaryngoscopy using standard instruments and the carbon dioxide laser. Laryngoscope Investigative Otolaryngology. 2022;7(4):1065‐1070. doi: 10.1002/lio2.854
Level of evidence: NA.
Funding information Louisiana State University
REFERENCES
- 1. Sutherland LM, Middleton PF, Anthony A, et al. Surgical simulation: a systematic review. Ann Surg. 2006;243(3):291‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schout BM, Hendrikx AJ, Scheele F, et al. Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc. 2010;24:536‐546. doi: 10.1007/s00464-009-0634-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moglia A, Vincenzo F, Morelli L, et al. A systematic review of virtual reality simulators for robot‐assisted surgery. Eur Urol. 2016;69(6):1065‐1080. [DOI] [PubMed] [Google Scholar]
- 4. McCloy R, Stone R. Science, medicine, and the future. Virtual Reality Surg BMJ. 2001;323(7318):912‐915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barsom EZ, Graafland M, Schijven MP. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016;30:4174‐4183. doi: 10.1007/s00464-016-4800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brewin J, Nedas T, Challacombe B, Elhage O, Keisu J, Dasgupta P. Face, content and construct validation of the first virtual reality laparoscopic nephrectomy simulator. BJU Int. 2010;106:850‐854. [DOI] [PubMed] [Google Scholar]
- 7. Huang C, Agrawal SK, Ladak HM. Virtual reality simulator for training in myringotomy with tube placement. J Med Biol Eng. 2016;36:214‐225. doi: 10.1007/s40846-016-0124-1 [DOI] [Google Scholar]
- 8. Malik HH, Darwood RJ, Shaunak S, et al. Three‐dimensional printing in surgery: a review of current surgical applications. J Surg Res. 2015;199(2):512‐522. doi: 10.1016/j.jss.2015.06.051 [DOI] [PubMed] [Google Scholar]
- 9. Hanna J, Brauer PR, Morse E, Mehra S. Margins in laryngeal squamous cell carcinoma treated with Transoral laser microsurgery: a National Database Study. Otolaryngol–Head Neck Surg. 2019;161(6):986‐992. [DOI] [PubMed] [Google Scholar]
- 10. Kuppersmith RB, Johnston R, Jones SB, Jenkins HA. Virtual reality surgical simulation and otolaryngology. Arch Otolaryngol Head Neck Surg. 1996;122(12):1297‐1298. [DOI] [PubMed] [Google Scholar]
- 11. Huang C, Cheng H, Bureau Y, Agrawal SK, Ladak HM. Face and content validity of a virtual‐reality simulator for myringotomy with tube placement. J Otolaryngol Head Neck Surg. 2015;44:40. doi: 10.1186/s40463-015-0094-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Materials. Stereolithography files for 3D printed parts ‐ laryngeal_simulator_parts.zip.
Microlaryngoscopy simulator assembly instructions–laryngeal_assembly.docx.


