Abstract
Purpose
In 2022, an inexpensive multi-radial infrared photoscreener, the AI Optic was released in a similar format as the 2012 PlusoptiX a-12 but utilizing artificial intelligence (AI) for online, central image interpretation. We studied them because no prior comparative validation concerning amblyopia risk factors and particularly refractive error has been done.
Patients and Methods
Children from a pediatric ophthalmology practice had AI Optic and PlusoptiX-a12 photoscreen concomitantly during comprehensive examination with precisely measured strabismus and refraction. Validation to AAPOS 2021 and 2013 guidelines was evaluated with receiver operating characteristic (ROC) curves while refractive estimates were compared by the ABCD ellipsoid univariable technique.
Results
In 200 ethnically diverse children aged 1–18, 148 were 4 years or older, 35% had developmental delays, and 2/3 had amblyopia risk factors (ARF). Area under the ROC curve (AUC) targeting AAPOS 2021 refractive plus strabismus for age ≥4 years was 0.58 for AI Optic and 0.74 for PlusoptiX while for children <4 years, AUC was 0.53 for AI Optic and 0.72 for PlusoptiX. For 134 comparable sphero-cylinder refractions, the ABCD Ellipsoid median (interquartile ranges) for AI Optic right eye 2.53 (1.54, 4.01) and left eye 3.05 (1.83, 5.00) did not approximate actual refraction as well as by PlusoptiX right eye 1.88 (1.12, 2.86) and left eye 2.10 (1.26, 3.04) Mann Whitney z=3.7 right and 4.2 left, p<0.001 each. AI Optic via central “AI” reading gave sphero-cylinder and referral estimates in all but 16 of 200 high risk children whereas Plusoptix had 25 inconclusives. On the other hand, with inconclusives scored as a refer, Plusoptix outperformed AI Optic in terms of ARF validation and refractive estimate.
Conclusion
Plusoptix provided more valid amblyopia and refractive screening than the cheaper AI Optic. Clinics must weigh cost versus performance, and central data sharing before selecting one of these vision-saving devices.
Keywords: photoscreening, amblyopia, sphero-cylinder refraction, amblyopia risk factor
Video Abstract

Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Photoscreening is a valid method for detection of amblyopia risk factors with a limited endorsement for children older than 3 years,1 but capable for toddlers and infants even younger than 1 year.2 Photoscreening is designed to identify the refractive amblyopia risk factors anisometropia, hyperopia, astigmatism and also myopia.3 In addition, photoscreeners can also target strabismus and deprivational amblyopia risk factors. The Vision Screening Committee of the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) has published confirmatory exam failure levels for amblyopia risk factors starting in 20033 and updated with three age ranges in 20134 with even further refinement in 2021.5
A given photoscreener manufacturer or vision screening clinic needs to select and set instrument referral criteria so the device can target AAPOS uniform guidelines risk factor levels with appropriate sensitivity and specificity. Some devices employ a single pre-selected instrument referral criteria (IRC) which, when selected to be sensitive for manufacturer liability often results in reduced specificity- and over-referral from the viewpoint of the receiving ophthalmologist. To help address the disparate screening program goals, Plusoptix (Nuremberg, Germany) has adopted a user-selectable group of published instrument referral criteria options targeting the 2013 AAPOS guidelines.
The Plusoptix family of photoscreeners (S04, s08, s09, s-12, s-16) has had extensive validation compared with eye chart visual acuity,6,7 digital flash cameras,7–9 the MTI photoscreener,9,10 the iScreen,9,11–13 Suresight,9,14–16 compared with SPOT,12,13,17–21 2WIN,17,21–26 GoCheck Kids,13 blinq,25,26 with Retinomax9,23,24,27,28 and table-top autorefractors,22,29 community screening30,31 and examination.28,32–44 The refractive accuracy has been compared.18,22,28,43,45 PlusoptiX is useful on special-needs children.46
Various alternative IRC have been compared.39 Evidence-based instrument referral guidelines with sensitive and specific alternatives for the three leading infrared photoscreeners PlusoptiX, SPOT (Welch-Allyn, Schenectady, New York) and the Adaptica 2WIN (Padova, Italy) targeting the 2021 revision in AAPOS guidelines5 have been published.21
Cost has been a barrier in the adoption of photoscreening for some pediatric clinics. In Spring 2022, a new infrared photoscreener with centralized, machine-learning-based interpretation was marketed called the AI-Optic Vision Screener (Beijing Fantasy Forest Intelligent Technology Company, Ltd, Beijing, China, www.ai-optic.com). The AI Optic photoscreener was priced below the cost of several existing photoscreening devices. The Alaska Blind Child Discovery (ABCD) promptly obtained a new device. The purpose of this paper is to describe the features of the new AI Optic device and to subject it to rigorous head-to-head validation compared to a conventional PlusoptiX a-12 in a pediatric ophthalmology practice. Practical use of the new device is described in detail. The AI Optic and the PlusoptiX a-12 are shown in Figure 1.
Figure 1.
The AI Optic (left) and the PlusoptiX a-12 photoscreeners.
Materials and Methods
The prospective evaluation of a screening test as a part of the Alaska Blind Child Discovery was approved by the institutional review of Providence Alaska Medical Center in compliance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Parents provided written informed consent and older children provided assent. De-identified data are provided: https://www.abcd-vision.org/references/AI%20Optics%20PlusoptiX%20de-ID%202022.pdf.
Released in 2022, the more recent device is called the AI Optic Vision Screener (version 0.8.3). AI Optics is a company since 2020 with address 145 Lexington Ave APT 10 New York, NY, 10016–8365 United States. From the product description, it is a multi-radial, Infrared (850 nm) photoscreener measuring at a distance of 100 ± 5 cm through pupils with diameter 4.0–9.0 mm, covering an interpupillary distance 50–70 mm over refractive range spherical power −8D to +8D and cylindrical power −3.50D to +1.0D. The intended age range is 3–50 years. The AI Optic offers no ability to select + or minus cylinder notation, but the output is mainly minus cylinder, but sometimes presents without the (-). Historical data stored in device can be individually or batch emailed but may, at times, not transmit with error message “Failed to login!”
AI Optic allows user selection of three instrument referral criteria (IRC): the pre-determined default is (1) “Arnold, (sensitivity 92% specificity 90% Indication of source: www.abcd-vision.org, Arnold is best at maximizing sensitivity and specificity for the latest AAPOS referral criteria.12 You can choose Arnold for routine check”. Other IRC are (234) and (332). The actual anisometropia/hyperopia/cylinder/myopia cut-offs for school-age for AI Optic IRC option (1) are 1.25/2.00/1.50/1.50, for option (2) are 1.00/3.50/1.25/3.00 and for IRC option (3) 1.25/1.00/1.25/1.00.
Inclusion criteria were children undergoing pediatric eye examination with favorable parental or legal guardian consent. Excluded were children either too young or not able to gaze at the photoscreeners. Each patient had an eye exam including best corrected visual acuity (for age), ocular motility including alternating prism cover test, stereopsis, anterior and posterior segment exams. Refraction was done with accommodation relaxed with cyclopentolate 1% 30 minutes before refraction in children under age 8 and with fogging at the phoropter for those older than 8. From the exam, refractive, strabismic and deprivational amblyopia risk factors meeting AAPOS criteria were identified.
SAMPLE SIZE CALCULATION: Prior experience with infrared photoscreener refraction comparison demonstrated the ABCD ellipsoid mean about 2.0 with standard deviation 2.0.21 Therefore, to detect a difference of 0.5, with beta 0.8 and alpha 0.05, a sample size of 126 would be needed. If 2/3 of the patients were predicted older than 4 years, then about 180 patients should be recruited expecting some to be inconclusive or out-of-range.
The ability of each device to screen for given risk factor targets for amblyopia are compared using receiver operating characteristic curves47 from which an area under the curve (AUC) was calculated.
From a range of individual subcomponent refractive and strabismic amblyopia instrument referral criteria that correlated between each device and the confirmatory eye examination, receiver operating characteristic curves were generated comparing the devices targeting 2013 and 2021 AAPOS Uniform guideline with failure criteria that recognize anisometropia, meridional hyperopia, astigmatism, myopia and strabismus. To a set of IRC called “regular”, “sensitive” and “specific” and extra level for “extra specific” was added to extend observed range on the ROC curves (Table 1).
Table 1.
Instrument Referral Criteria (IRC) for PlusoptiX a-12 and AI Optic Photoscreeners Targeting 2013 and 2021 AAPOS Uniform Guideline Refractive Amblyopia Risk Factors (ARF). Cut Off Ranges Include Anisometropia (A), Meridional Hyperopia (H), Myopia (M) and Astigmatism (C; cylinder)
| DEVICE | Age Range | Instrument Referral Criteria (IRC) | AAPOS Uniform Guideline | ||||
|---|---|---|---|---|---|---|---|
| Sensitive | Regular | Specific | Extra Specific | Year | Ages | ||
| PlusoptiX | School | 1.25A, 2.5H, −2M,2.25C | 1.75A,3H,-2.5M, 2.5C | 1.75A,3%H,-2.5M, 2.75C | 2A,4H,-3M,4C | 2013 | ≥4y |
| AI Optic | School | 1.25A,1.5H,-1.75M,1C | 1.5A,2H,-2.25M,1.5C | 2A,2.5H,-3M,2C | 2013 | ≥4y | |
| PlusoptiX | School | 1.25A, 2.5H, −2M,2.25C | 1.75A,3H,-2.5M, 2.5C | 1.75A,3%H,-2.5M, 2.75C | 2A,4H,-3M,4C | 2021 | ≥4y |
| AI Optic | School | 1.25A,1.5H,-1.75M,1C | 1.5A,2H,-2.25M,1.5C | 2A,2.5H,-3M,2C | 2021 | ≥4y | |
| PlusoptiX | Preschool | 1.5A, 2.5H, −3.25M, 3.25C | 1.75A, 3H, −3.5M, 3.5C | 1.75A,3.5H,-3.75M,3.75C | 2A,4H,-4M,4C | 2021 | <4y |
| AI Optic | Preschool | 1.25A,1.5H,-1.75M,1C | 1.5A,2H,-2.25M,1.5C | 2A,2.5H,-3M,2C | 2021 | <4y | |
The ability of each device to estimate age-based sphero-cylinder refractive error is compared using the ABCD ellipsoid method.24 The ABCD ellipsoid is derived as an oval-solid region on a 3 dimensional plot with J0 (x-axis), J45 (y-axis) and M spherical equivalent (z-axis) the displacement between two sphero-cylinder refractions leading to a single measure related to the degree of blur produced by the refractive difference.48
Results
PATIENTS: A total of 200 children aged 0.4 to 18 (mean 7.6 ±4.7 years) undergoing new or follow up pediatric ophthalmology examinations were concomitantly screened with the AI Optic and the PlusoptiX a12 devices (Table 2). 113 had age-based 2021 AAPOS refractive and/or strabismic amblyopia risk factors. The ethnic/racial/gender mix was 14 Asian, 18 Black, 24 Hispanic, 16 Alaska Native, 15 Pacific Islander and 113 White; 106 were male. Seventy-one had some form of neuro-developmental delay including 16 with autism, 11 premature, 7 with attention deficit (ADHD) and 6 with trisomy 21 and of whom cooperation was judged as poor in 9 and “fair” in 12. Sixteen were referred by community pediatric photoscreening and 15 had prior strabismus surgery.
Table 2.
Characteristics of Patients. Counts and Measured Variables are Quantified by Mean, Standard Deviation (S.D), Median, Minimum (min) and Maximum (max). There were 71 with Developmental Delay such as Autism, Trisomy 21, Marked Prematurity and Attention Deficit. Actual Refraction is Compared to Estimates by the PlusoptiX a-12 and AI Optic Photoscreeners Featuring Sphere Right and left (R and L) and Cylinder (Cyl)
| Characteristic | Quality | Count | Mean | S.D. | Median | Min | Max |
|---|---|---|---|---|---|---|---|
| AGE | 200 | 7.6 | 4.7 | 7.2 | 0.3 | 18 | |
| Gender | Female | 94 | |||||
| Delays | 71 | ||||||
| RACE/Ethnicity | |||||||
| Asian | 14 | ||||||
| Black | 18 | ||||||
| Caucasian | 113 | ||||||
| Hispanic | 24 | ||||||
| Alaska Native | 16 | ||||||
| Pacific Islander | 15 | ||||||
| STRABISMUS | Tropia > 8PD | 32 | |||||
| Media Opacity | 3 | ||||||
| Refraction | 200 | ||||||
| Sphere-R | −0.2 | 3.5 | 0 | −23.5 | 7.75 | ||
| Cyl-R | 1.2 | 1.3 | 0.8 | 0 | 9.5 | ||
| Sphere-L | 0.1 | 3.3 | 0.3 | −23.5 | 8 | ||
| Cyl-L | 1.1 | 1.3 | 0.8 | 0 | 8.5 | ||
| PlusoptiX | 175 | ||||||
| Sphere-R | −0.7 | 1.9 | −0.3 | −7 | 4.5 | ||
| Cyl-R | 1.5 | 1.5 | 1 | 0 | 7.75 | ||
| Sphere-L | −0.4 | 1.8 | 0 | −7.25 | 3.25 | ||
| Cyl-L | 1.4 | 1.4 | 1 | 0 | 8.25 | ||
| AI Optic | 184 | ||||||
| Sphere-R | −0.8 | 2.4 | −0.5 | −9.5 | 6.75 | ||
| Cyl-R | 0.7 | 0.7 | 0.5 | 0 | 2.75 | ||
| Sphere-L | 0.2 | 2.4 | 0.5 | −8.75 | 4.5 | ||
| Cyl-L | 0.7 | 0.7 | 0.5 | 0 | 3.25 | ||
PRACTICAL EXPERIENCE WITH THE DEVICES: The following are observations regarding advantages and disadvantages of each device when screening cooperative and developmentally delayed children. The AI Optic in 2022 US dollars costs less than $1000 while the other traditional infrared, multi-radial photoscreeners cost $6-8000.
The AI Optic requires WiFi for remote, automatic intelligence interpretation (takes 10–70 seconds) and charges in about 2 hours with USB-C affording 2 hours of cordless use for over 10–20 screenings. The AI Optic comes with a 13-page brief Product Instruction and an online training video which recommend fixing device to a tripod instead of hand holding. Presumably the tripod would be for adult and older-children refractions whereas actual pediatric photoscreening benefits from quick, creative camera focus and re-alignment. Therefore, for our validation in children, we used the device hand-held.
The display on this early release of AI Optics still has some English typos such as: “proceesing”, “enter your email to see you result” The instrument referral criteria we employed on the AI Optic matched one available on the PlusoptiX and was called “Arnold.”12
The PlusoptiX has extensive clinical experience with product and software updates.49 The replaceable AA batteries or rechargeable option are helpful. The user interface selecting patient age only affords quick screening and the internal computer interpretation is usually very fast (2–5 seconds image acquisition and 3 seconds interpretation). Focus is indicated by a green ring around the pupils. For children with complex refractions, blocked or non-round pupils, the PlusoptiX will not “guess” a quick interpretation but might take 30 seconds or more attempting to acquire reliable infrared pupil crescent information. If PlusoptiX interprets refractions out of range, instead of a presenting a sphero-cylinder refraction estimate, it will instead state “HYP” for excess hyperopia or hyperopic astigmatism and “MYO” for excess myopic refraction estimation. For age-dependent target conditions, Plusoptix uses a simple touch screen choice of years of age before enabling image acquisition.
The AI Optic has a brief user’s manual and a 13-minute online video so certain aspects of screening with this device were intuitive, but others required discovery with use. For instance, patient demographics name, gender and birthdate must be entered first, then image acquisition triggered by pressing a whirly-circle emblem on the touch screen; in a dim room the patient’s face and pupils were not visible until a second emblem- not specifically mentioned on the user manual, was activated initially. Focus is based on image clarity on the screen and then “Image proceesing” shows as the number of seconds for WiFi and internet transmission to the central reading center followed by return of a “refer” or “pass” color-coded interpretation with sphero-cylinder estimate mainly in minus cylinder form (however range of cylinder for the device listed as “from −3 to 1 diopter). Details about AI Optic proprietary central reading process, such as location, data storage and/or computer methods are not given in the accompanying printed product instructions or on the website. Almost always the left eye spherical equivalent is 0.75 to 1.0 diopters more hyperopic than the right eye. Stored screening results can be reviewed, selected individually or as a group and emailed however the device was able to email the initial 50 screenings, but gave an error when attempting to email as the group got larger. The ability to aim the camera and hold it steady on a stable, or a moving patient worked well hand-held by an experienced screener and the tripod was not needed.
The PlusoptiX A-12 (version 7.2.5.0, Nuremberg, Germany) originally designed in 2012 is an industry-standard, multi-radial infrared photorefractive screener with extensive validation. Plusoptix can work independently from internet with digital interpretation real-time through the device; Plusoptix does allow WiFi connectivity to electronic medical records, however. An S12 is for screening while the A-12 provides full sphero-cylinder refraction with similar red reflex analysis from the prior S04, S08 and S0946 models. These PlusoptiX devices use standard or rechargeable AA batteries. We employed IRC rating number 4 out of five options for specificity12 (anisometropia 1.25, hyperopia 2.00, cylinder 1.50 and myopia 1.50) when this device was employed hand-held in a dim exam room. A range of instrument referral criteria previously reported for PlusoptiX21 are employed and new regular, sensitive and specific and extra-specific alternatives are generated from adjusted ARF component contributions to preliminary AUC, particularly for the recently released AI Optics device are given in Table 1.
VALIDATION: The PlusoptiX was unable to give an interpretation in 25 cases usually due to strabismus and/or poor cooperation, in 9 excess hyperopia was noted in both eyes, in 3 excess myopia was noted and in 19 an excess of hyperopia was noted in one eye with sphero-cylinder estimate in the contralateral eye. For the AI Optic, 16 were unreadable yielding no refractive results of which two were patients with strabismus and two others had high hyperopia (5 diopters), but sphero-cylinder estimates were obtained for the remaining 184 whether strabismic or not. Of the 25 inconclusive interpretations with Plusoptix, 22 (88%) had 2021 AAPOS ARF while of the 16 inconclusive AI Optic, 10 (63%) had 2021 AAPOS ARF.
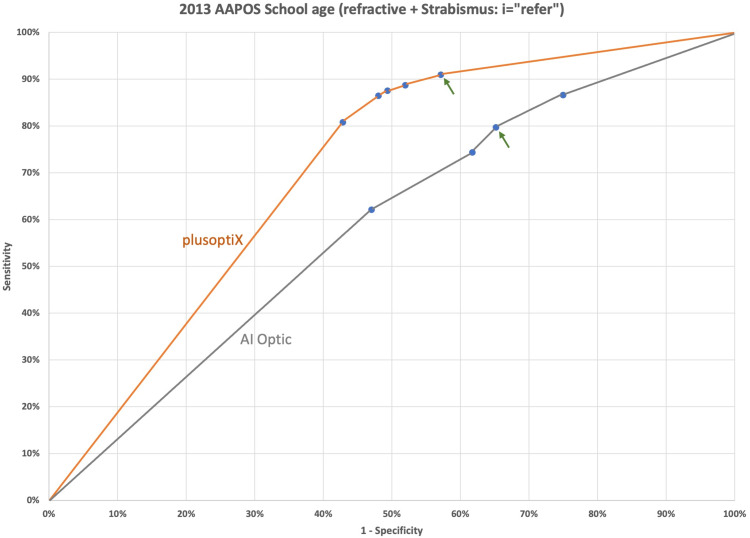
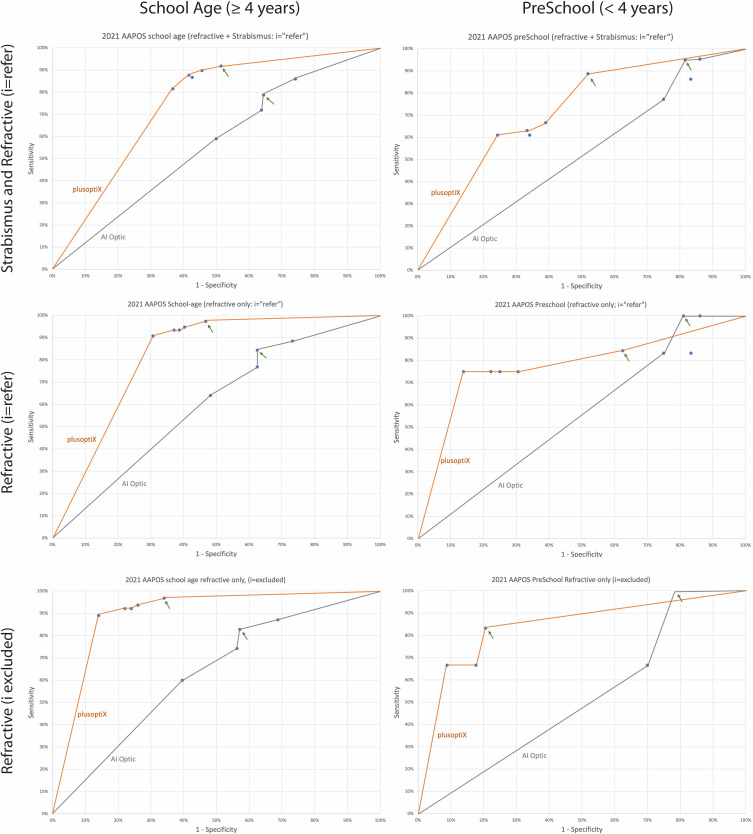
Receiver operating characteristic (ROC) curves demonstrate the predictive value targeting amblyopia risk factors comparing the two devices. AAPOS Uniform Guideline 2013 older age group (>47 months; Figure 2) and the more recent 2021 guidelines for preschool (<4 years) and also for children ≥ 4 years are presented (Figure 3). The actual “refer” or “pass” results from the PlusoptiX using device selected IRC option 4 of 5, and the Arnold default IRC for AI Optics are highlighted on each ROC curve with a green arrow (Figures 2 and 3). Estimates of the Area Under the Curve for ROC curves comparing devices in this high-prevalence cohort for school age 2013 and 2021 guidelines and for preschool 2021 are given in Table 3. For children over 4 years of age targeting 2021 refractive plus strabismic amblyopia risk factors, the AI Optics had AUC of 0.58 compared to 0.74 for PlusoptiX a-12. The corresponding instrument results between AI Optics and the PlusoptiX a-12 photoscreener influenced by developmental delay is shown in Table 4. For school age 2021 refractive plus strabismus, the Plusoptix “regular” IRC had sensitivity/specificity of 92%/82% for patients with developmental delay and 73%/81% for patients with normal development. For the same patients, targeting strabismus plus refractive 2021, AI Optic had sensitivity/specificity of 69%/28% for patients with developmental delay and 74%/48% for patients with normal neuro-development.
Figure 2.
The receiver operating characteristic (ROC) curves comparing AI Optic to the Plusoptix a-12 in children over 4 years of age targeting the 2013 AAPOS amblyopia risk factors for strabismus and refractive error with inconclusive results counted as a “refer” and Instrument referral criteria “Arnold, ABCD” chosen indicated by the green arrows.
Figure 3.
Receiver operating characteristic (ROC) curves targeting AAPOS 2021 refractive and strabismic amblyopia risk factors comparing school age (left column) with preschool (right column). Inconclusive results (i) are either counted as a “refer” (I = refer) or excluded from calculations of sensitivity and specificity. Instrument referral criteria “Arnold, ABCD” chosen indicated by the green arrows.
Table 3.
Area Under the Curve (AUC) for Receiver Operating Characteristic (ROC) Curves Validating the PlusoptiX a-12 and the AI Optic Photoscreeners Targeting American Association of Pediatric Ophthalmology and Strabismus (AAPOS) Refractive Alone and Refractive Plus Strabismic Amblyopia Risk Factors (ARF). The total Number of Children for Each Age Range (n) and The Prevalence of Those Above the Examination Failure Levels are Given. Validation Sensitivity (sens) and Specificity (spec) from the ABCD Criteria (Arnold) for School age Targeting Refractive ± Strabismic Amblyopia Risk Factors are Given. Inconclusive Device Results (i) are Reported as if They Were a “Refer (i = r), and also as if They Are Not Included in the Calculations (Exclude i)
| AAPOS Uniform Guideline | Amblyopia Risk Factor (ARF) | Refractive only | Strabismus + Refractive | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exam Failure Levels | i=r | Exclude i | ARF | i=r | ||||||||||
| DEVICE | Year | Age | Aniso | Hyper | Myop | Cyl | Prevalence | AUC | AUC | Sens/spec | n | Strabismus | AUC | Sens/spec |
| PlusoptiX | 2013 | ≥4y | >1.5D | >3.5D | <-3D | >1.5D | 65% | 0.76 | 0.83 | 97%/66% | 148 | Manifest | 0.71 | 81%/65% |
| AI Optic | 2013 | ≥4y | >1.5D | >3.5D | <-3D | >1.5D | 65% | 0.63 | 0.65 | 77%/41% | 148 | Manifest | 0.59 | 77%/41% |
| PlusoptiX | 2021 | ≥4y | >1.25D | >4.0D | <-2D | >1.75D | 65% | 0.82 | 0.90 | 92%/76% | 148 | >9 PD | 0.74 | 85%/78% |
| AI Optic | 2021 | ≥4y | >1.25D | >4.0D | <-2D | >1.75D | 65% | 0.61 | 0.63 | 74%/44% | 148 | >9 PD | 0.58 | 69%/44% |
| PlusoptiX | 2021 | <4y | >1.25D | >4.0D | <-3D | >3D | 33% | 0.78 | 0.84 | 67%/79% | 52 | >9 PD | 0.72 | 86%/63% |
| AI Optic | 2021 | <4y | >1.25D | >4.0D | <-3D | >3D | 33% | 0.53 | 0.52 | 87%/31% | 52 | >9 PD | 0.53 | 93%/22% |
Table 4.
Corresponding Results Between AI Optic and PlusoptiX a-12 Photoscreening Accounting for the Number (in Parentheses) with Developmental Delays
| n (Delay) | AI Optic | ||||
|---|---|---|---|---|---|
| Refer | Pass | Inconclusive | |||
| PlusoptiX | Refer | 72 (21) | 21(7) | 9(3) | |
| Pass | 44(18) | 27(7) | 2(2) | ||
| Inconclusive | 18(8) | 2(1) | 5(4) | ||
| 200(71) | |||||
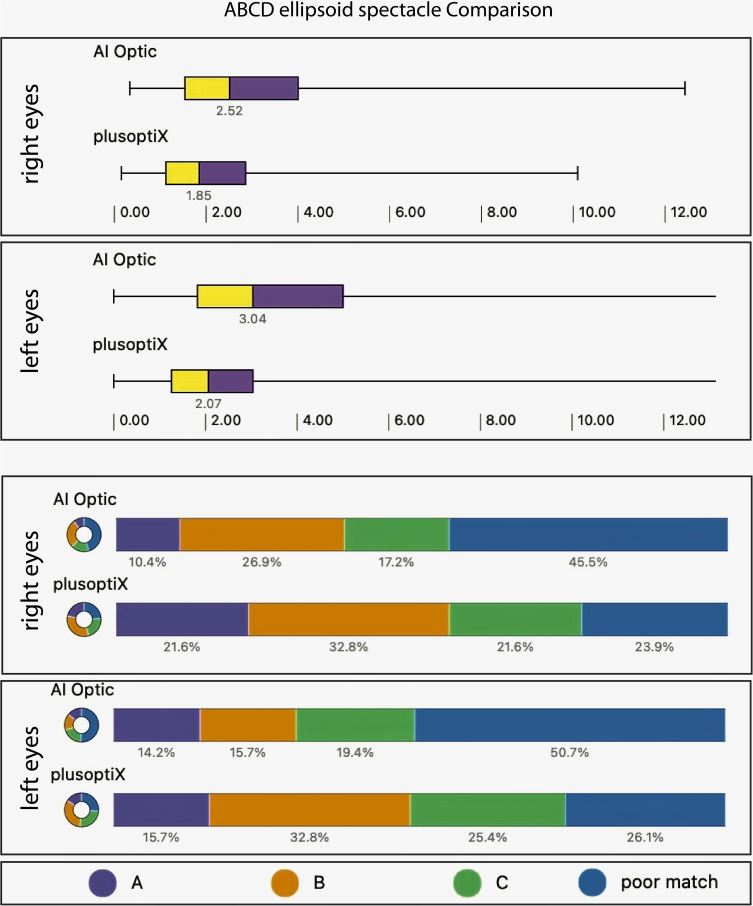
REFRACTIVE COMPARISON: The accuracy of each device’s photoscreen estimation of refraction was compared to actual refraction using the ABCD ellipsoid method.24 Of the 200 patients, 134 had sphero-cylinder estimates in both AI Optics and PlusoptiX for comparison. ABCD ellipsoid mean (±S.D) for PlusoptiX right eye 2.20±1.5 and left eye 2.34±1.6 differed from AI Optics right eye (3.15±2.3) and left eye (3.63±2.6) using Student’s t-test with right eye (t(266) = 4.0 and left eye t(266) = 4.9 both being significant (p<0.001). However, the Shapiro–Wilk test for normal distribution for ABCD ellipse right eye (z=6.0) and ellipse left eye (z=6.8) PlusoptiX and for IA Optics right eye (z=6.3) and left eye (z=4.9) all were not normally distributed (p<0.001). Therefore, the ABCD ellipsoid median with inter-quartiles (Q1,Q3) for PlusoptiX right eye 1.88 (1.12,2.86) and left eye 2.10 (1.26,3.04) differed from AI Optics right eye 2.53 (1.54,4.01) and left eye 3.05 (1.83,5.00) demonstrated by Mann–Whitney z=3.7 right eye and z=4.2 left eye (Figure 4; p<0.001 each).
Figure 4.
The ABCD ellipsoid compares spherical cylindrical refractions from Plusoptix and AI Optic with actual (cycloplegic) refraction. Top metric box plots with interquartile ranges (yellow and purple) highlights values of 1 correspond to one line visual acuity blur (grade A) while value of 2 implies 3 logMAR lines blur (grade B) and value of 3 6 logMAR lines blur (grade C). Bottom metric shows proportion with each grade (colors purple, Orange and green) blur and those that are a poorer spectacle match than grade C (teal color) (more than 6 lines visual acuity blur).
The ABCD ellipsoid for PlusoptiX did not correlate with AI Optics for right eye (Pearson Product-Moment Correlation r(132) = 0.107, p=0.22) or for left eye (Pearson Correlation r(132) = 0.07, p=0.42).
Discussion
The 2022 released, less-expensive AI Optic was compared to the similar shaped and configured 2012 released PlusoptiX a-12 photoscreener on 200 children from a pediatric eye practice. Since the 2021 guidelines have only recently been published, each device still utilized Instrument Referral Criteria that target 2013 AAPOS guidelines.4 Approximately 1/3 of the younger children less than 4 years old and about 2/3 of the older children had amblyopia risk factors defined by the 2021 AAPOS guidelines.5 For the 2013 and 2021 Guidelines, the extensively utilized PlusoptiX a-12 outperformed the newer AI Optic in terms of amblyopia risk factor screening and refractive estimation.
A strength of this study is a sufficient number of ethnically-diverse, older children with high prevalence of amblyopia risk factors. On the other hand, subgroup analysis of the younger group less than 4 years of age was limited by sample size of just 52. Developmentally delayed children were not excluded. Uniform guideline recent target amblyopia risk factors were analyzed in addition to the former 2013 exam failure levels for which each device has software to target. Refractive comparison utilized validated, single metric ABCD ellipsoid values and grades with sufficient sample size.
PlusoptiX had more inconclusive results than AI Optic. A refractive estimate was delivered in 175 of the PlusoptiX screenings and 184 of the AI Optic screenings in this high risk cohort with 32 patients with a tropia of greater than 8 prism diopters. Due to variations in pupillary red reflex crescent during ocular misalignment, the Plusoptix with real-time, in-device interpretation is programmed to not give a refractive estimate when substantial strabismus is suspected. On the other hand, AI Optic with remotely AI-interpreted images produced refractive estimates sometimes in the presence of constant strabismus. Eighteen inconclusive Plusoptix interpretations were regarded as a refer by AI Optic while 5 patients were inconclusive on both devices (Table 4).
A weakness of the study is that it is not performed in community cohort with typical risk factor prevalence then combined with uniform exam definition of refractive error, strabismus, media opacity and age-appropriate visual acuity from which amblyopia itself can be diagnosed. Instead of highly experienced screener as in this study, the experience level of the screener could have been more typical such as studying a lay screener or pediatric technician or nurse. A thorough cost-benefit analysis was not done to compare the devices; instead price range and validation data are presented.
Plusoptix had been the only photoscreener to offer a user a choice of five instrument referral criteria39 but now AI Optics has been designed to offer three of these also.
With further clinical experience and validation, the accuracy of this new AI Optics with artificial intelligent interpretation might have the potential to get even better.
Conclusion
The inexpensive AI Optic resembles the Plusoptix in form and configuration including user-selected instrument referral guidelines, however it does not yet achieve Plusoptix’s high level of performance targeting uniform amblyopia risk factor guidelines or estimates of sphero-cylinder refractive error. With further validation and AI, the performance of the new AI Optic might be increased.
Funding Statement
There is no funding to report.
Abbreviations
AAPOS, American Association for Pediatric Ophthalmology and Strabismus; ABCD, Alaska Blind Child Discovery; AI, artificial intelligence, AUC, area under the curve; D, diopter; GoCheck Kids, brand of photoscreener based on smartphone; I.R.C., instrument referral criteria; PD, prism diopter; ROC, receiver operating characteristic; s04, s08, s09, s12, s16 are successive model numbers of Plusoptix photoscreener developed in than year since 2000 A.D.; SPOT, brand of photoscreener; USB, universal serial bus; WiFi, wireless fidelity network protocol; 2WIN, brand of photoscreener.
Data Sharing Statement
De-identified data https://www.abcd-vision.org/references/AI%20Optics%20PlusoptiX%20de-ID%202022.pdf.
Disclosure
Dr. Arnold coordinates the Alaska Blind Child Discovery which has received discounted vision screen technology from several vendors. He is board member of PDI Check which makes a vision screening game for autostereoscopic devices and also of Glacier Medical software which markets the cloud-based ROP screening software ROP Check. Also he is Protocol developer and Investigator for PEDIG. In addition, Dr Arnold reports unpaid advisory board member for GoCheck Kids, iScreen, Adaptica and PlusoptiX. The author reports no other conflicts of interest in this work.
References
- 1.Grossman DC, Curry SJ, Owens DK, et al. Vision screening in children aged 6 months to 5 years: US preventive services task force recommendation statement. JAMA. 2017;318(9):836–844. doi: 10.1001/jama.2017.11260 [DOI] [PubMed] [Google Scholar]
- 2.Longmuir SQ, Boese EA, Pfeifer W, Zimmerman B, Short L, Scott WE. Practical community photoscreening in very young children. Pediatrics. 2013;131(3):e764–e769. doi: 10.1542/peds.2012-1638 [DOI] [PubMed] [Google Scholar]
- 3.Donahue S, Arnold R, Ruben JB. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results from studies of preschool vision screening. J AAPOS. 2003;7(5):314–316. doi: 10.1016/S1091-8531(03)00182-4 [DOI] [PubMed] [Google Scholar]
- 4.Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17(1):4–8. doi: 10.1016/j.jaapos.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 5.Arnold RW, Donahue SP, Silbert DI, et al. Uniform guidelines for pediatric vision screen validation 2021. J AAPOS. 2022;26(1):p1.e-.e6. doi: 10.1016/j.jaapos.2021.09.009 [DOI] [PubMed] [Google Scholar]
- 6.Vaughan J, Dale T, Herrera D. Comparison of photoscreening to chart methodology for vision screening. J Sch Nurs. 2020;38(3):306–310. doi: 10.1177/1059840520940370 [DOI] [PubMed] [Google Scholar]
- 7.Leman RE, Clausen MM, Bates J, Stark L, Arnold KK, Arnold RW. A comparison of patched HOTV visual acuity and photoscreening. J Sch Nurs. 2006;22(4):237–243. doi: 10.1177/10598405050220040901 [DOI] [PubMed] [Google Scholar]
- 8.Clausen MM, Arnold RW. Pediatric eye/vision screening. Referral criteria for the pediavision plusoptix s 04 photoscreener compared to visual acuity and digital photoscreening. Kindergarten computer photoscreening. Binocul Vis Strabismus Q. 2007;22(2):83–89. [PubMed] [Google Scholar]
- 9.Arnold RW, Davis B, Arnold LE, Rowe KS, Davis JM. Calibration and validation of 9 objective vision screeners with contact-lens induced anisometropia. J Pediatr Ophthalmol Strabismus. 2013;50(3):184–190. doi: 10.3928/01913913-20130402-02 [DOI] [PubMed] [Google Scholar]
- 10.Matta NS, Arnold RW, Singman EL, Silbert DI. Comparison between the plusoptiX and MTI Photoscreeners. Arch Ophthalmol. 2009;127(12):1591–1595. doi: 10.1001/archophthalmol.2009.294 [DOI] [PubMed] [Google Scholar]
- 11.Wang J, Suh D. Comparison between the plusoptix and iScreen photoscreeners in detecting amblyopic risk factors in children (meeting abstract). J AAPOS. 2012;16(1):105. doi: 10.1016/j.jaapos.2011.12.113 [DOI] [Google Scholar]
- 12.Arnold RW, Arnold AW, Armitage MD, Shen JM, Hepler TE, Woodard TL. Pediatric photoscreeners in high risk patients 2012: a comparison study of Plusoptix, iScreen and SPOT. Binoc Vis and Strabismus Quart. 2013;28(1):20–28. [PubMed] [Google Scholar]
- 13.D’Souza H, Kun A, Martinson S, Bejarano L, McCole S. The positive predictive value of photoscreening devices for amblyogenic conditions. J AAPOS. 2021;25(6):P342.E1–342.E4. doi: 10.1016/j.jaapos.2021.06.008 [DOI] [PubMed] [Google Scholar]
- 14.Silbert D, Matta N, Tian J, Singman E. Comparing the SureSight autorefractor and the plusoptiX photoscreener for pediatric vision screening. Strabismus. 2014;22(2):64–67. doi: 10.3109/09273972.2014.904896 [DOI] [PubMed] [Google Scholar]
- 15.Silbert DI, Matta NS, Ely AL. Comparison of SureSight autorefractor and plusoptiX A09 photoscreener for vision screening in rural Honduras. J AAPOS. 2014;18(1):42–44. doi: 10.1016/j.jaapos.2013.09.006 [DOI] [PubMed] [Google Scholar]
- 16.Lang D, Leman R, Arnold AW, Arnold RW. Validated portable pediatric vision screening in the Alaska Bush. A VIPS-like study in the Koyukon. Alaska Med. 2007;49(1):2–15. [PubMed] [Google Scholar]
- 17.Kirk S, Armitage MD, Dunn S, Arnold RW. Calibration and validation of the 2WIN photoscreener compared to the PlusoptiX S12 and the SPOT. J Pediatr Ophthalmol Strabismus. 2014;51(5):1–4. doi: 10.3928/01913913-20140701-01 [DOI] [PubMed] [Google Scholar]
- 18.Crescioni M, Miller JM, Harvey EM. Accuracy of the spot and plusoptix photoscreeners for detection of astigmatism. J AAPOS. 2015;19(5):435–440. doi: 10.1016/j.jaapos.2015.07.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trivedi RH, Wilson ME, Peterseim MM, Papa C, Husain M. Prospective evaluation of photoscreeners in the pseudophakic eyes of children. J Pediatr Ophthalmol Strabismus. 2016;53(3):146–149. doi: 10.3928/01913913-20160405-08 [DOI] [PubMed] [Google Scholar]
- 20.Zhang X, Wang J, Li Y, Jiang B. Diagnostic test accuracy of Spot and Plusoptix photoscreeners in detecting amblyogenic risk factors in children: a systemic review and meta-analysis. Ophthalmic Physiol Opt. 2019;39(4):260–271. doi: 10.1111/opo.12628 [DOI] [PubMed] [Google Scholar]
- 21.Arnold RW, Silbert DI, Modjesky H. Instrument referral criteria for Plusoptix, SPOT and 2WIN targeting 2021 AAPOS guidelines. Clin Ophthalmol. 2022;16:489–505. doi: 10.2147/OPTH.S342666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yalcin E, Sultan P, Yilmaz S, Pallikaris IG. A comparison of refraction defects in childhood measured using Plusoptix S09, 2WIN photorefractometer, benchtop autorefractometer, and cycloplegic retinoscopy. Semin Ophthalmol. 2017;32(4):422–427. doi: 10.3109/08820538.2015.1118135 [DOI] [PubMed] [Google Scholar]
- 23.Racano E, Alessi S, Pertile R. Comparison of 2Win and plusoptiX A12R refractometers with Retinomax handheld autorefractor keratometer. J AAPOS. 2019;23(5):276e1–276 e5. doi: 10.1016/j.jaapos.2019.05.017 [DOI] [PubMed] [Google Scholar]
- 24.Arnold R, Martin SJ, Beveridge JR, et al. Ellipsoid spectacle comparison of PlusoptiX, retinomax and 2WIN autorefractors. Clin Ophthalmol. 2021;15:3637–3648. doi: 10.2147/OPTH.S326680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keffalos MA, Martin SJ, Arnold RW. Drive-by photoscreening: plusoptiX, 2WIN and blinq amblyopia detection during the COVID-19 pandemic. Clin Ophthalmol. 2021;15:775–782. doi: 10.2147/OPTH.S300871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnold R, Angi M. Multifaceted amblyopia screening with blinq, 2WIN and PDI Check. Clin Ophthalmol. 2022;16:411–421. doi: 10.2147/OPTH.S349638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinori M, Molina I, Hernandez EO, et al. The PlusoptiX photoscreener and the retinomax autorefractor as community-based screening devices for preschool children. Curr Eye Res. 2018;43:1–5. [DOI] [PubMed] [Google Scholar]
- 28.Payerols A, Eliaou C, Trezeguet V, Villain M, Daien V. Accuracy of PlusOptix A09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmol. 2016;16:72. doi: 10.1186/s12886-016-0247-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Won JY, Shin HY, Kim SY, Lee YC. A comparison of the Plusoptix S09 with an autorefractometer of noncycloplegics and cycloplegics in children. Medicine. 2016;95(35):e4596. doi: 10.1097/MD.0000000000004596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kiatos E, Armstrong JJ, Makar I. Successes and shortfalls of community Plusoptix photoscreening: results from the iSee study in Southwestern Ontario. Can J Ophthalmol. 2021;56(1):49–56. doi: 10.1016/j.jcjo.2020.07.022 [DOI] [PubMed] [Google Scholar]
- 31.Al-Haddad C, El Moussawi Z, Hoyeck S, et al. Amblyopia risk factors among pediatric patients in a hospital-based setting using photoscreening. PLoS One. 2021;16(7):e0254831. doi: 10.1371/journal.pone.0254831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arthur BW, Riyaz R, Rodriguez S, Wong J. Field testing of the plusoptiX S04 photoscreener. J AAPOS. 2009;13(1):51–57. doi: 10.1016/j.jaapos.2008.08.016 [DOI] [PubMed] [Google Scholar]
- 33.Matta NS, Singman EL, McCarus C, Matta E, Silbert DI. Screening for amblyogenic risk factors using the PlusoptiX S04 photoscreener on the indigent population of Honduras. Ophthalmology. 2010;117(9):1848–1850. doi: 10.1016/j.ophtha.2010.01.038 [DOI] [PubMed] [Google Scholar]
- 34.Matta NS, Singman EL, Silbert DI. Performance of the plusoptiX S04 photoscreener for the detection of amblyopia risk factors in children aged 3 to 5. J AAPOS. 2010;14(2):147–149. doi: 10.1016/j.jaapos.2010.01.006 [DOI] [PubMed] [Google Scholar]
- 35.Bloomberg J, Suh D. Performance of the plusoptix A08 photoscreener for the detection of amblyopia risk factors in children 0–5 in central Iowa (Meeting abstract). J AAPOS. 2012;16(1):105. doi: 10.1016/j.jaapos.2011.12.044 [DOI] [Google Scholar]
- 36.Saber Moghadam A, Alizadeh R, Zarei-Ghanavati M. Plusoptix S08 sensitivity in detecting strabismus as amblyogenic risk factor. Strabismus. 2013;21(4):230–234. doi: 10.3109/09273972.2013.851259 [DOI] [PubMed] [Google Scholar]
- 37.Silbert DI, Matta NS, Andersen K. Plusoptix photoscreening may replace cycloplegic examination in select pediatric ophthalmology patients. J AAPOS. 2013;17(2):163–165. doi: 10.1016/j.jaapos.2012.11.008 [DOI] [PubMed] [Google Scholar]
- 38.Silbert J, Matta N, Tian J, Singman E, Silbert DI. Pupil size and anisocoria in children measured by the plusoptiX photoscreener. J AAPOS. 2013;17(6):609–611. doi: 10.1016/j.jaapos.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 39.Singman E, Matta N, Tian J, Silbert D. A comparison of referral criteria used by the plusoptiX photoscreener. Strabismus. 2013;21(3):190–194. doi: 10.3109/09273972.2013.811606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singman E, Matta N, Tian J, Silbert D. The accuracy of the plusoptiX for measuring pupillary distance. Strabismus. 2014;22(1):21–25. doi: 10.3109/09273972.2013.877941 [DOI] [PubMed] [Google Scholar]
- 41.Lowry EA, Wang W, Nyong’o O. Objective vision screening in 3-year-old children at a multispecialty practice. J AAPOS. 2015;19(1):16–20. doi: 10.1016/j.jaapos.2014.09.008 [DOI] [PubMed] [Google Scholar]
- 42.Yan XR, Jiao WZ, Li ZW, Xu WW, Li FJ, Wang LH. Performance of the Plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PLoS One. 2015;10(6):e0126052. doi: 10.1371/journal.pone.0126052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fogel-Levin M, Doron R, Wygnanski-Jaffe T, Ancri O, Ben Zion I. A comparison of plusoptiX A12 measurements with cycloplegic refraction. J AAPOS. 2016;20(4):310–314. doi: 10.1016/j.jaapos.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 44.Huang D, Chen X, Zhang X, et al. Pediatric vision screening using the plusoptiX A12C photoscreener in Chinese preschool children aged 3 to 4 years. Sci Rep. 2017;7(1):2041. doi: 10.1038/s41598-017-02246-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li R, Huang D, Zhu H, et al. 双目屈光筛查仪在4~5岁学龄前儿童视力筛查中的应用研究. [The performance of visual photoscreening for Chinese preschool children aged 4 to 5 years]. Zhonghua Yan Ke Za Zhi. 2020;56(3):189–196. Chinese. doi: 10.3760/cma.j.issn.0412-4081.2020.03.006 [DOI] [PubMed] [Google Scholar]
- 46.Singman E, Matta N, Fairward A, Silbert D. Evaluation of plusoptiX photoscreening during examinations of children with autism. Strabismus. 2013;21(2):103–105. doi: 10.3109/09273972.2013.786736 [DOI] [PubMed] [Google Scholar]
- 47.Miller JM. Designing a rational screening program. Am Orthopt J. 2006;56(1):30–34. doi: 10.3368/aoj.56.1.30 [DOI] [Google Scholar]
- 48.Arnold RW, Beveridge JS, Martin SJ, Beveridge NR, Metzger EJ, Smith KA. Grading sphero-cylinder spectacle similarity. Clin Optom. 2021;13:23–32. doi: 10.2147/OPTO.S289770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaur K, Kannusamy V, Mouttapa F, Gurnani B, Venkatesh R, Khadia A. To assess the accuracy of Plusoptix S12-C photoscreener in detecting amblyogenic risk factors in children aged 6 months to 6 years in remote areas of South India. Indian J Ophthalmol. 2020;68(10):2186–2189. doi: 10.4103/ijo.IJO_2046_19 [DOI] [PMC free article] [PubMed] [Google Scholar]