Abstract
The purpose of the review was to investigate the changes in mental health services during the COVID-19 pandemic. A systematic review of qualitative, quantitative and mixed-methods studies was conducted from February 2021 to March 2022 using four databases and five languages. 29 studies reporting on mental health services in 63 countries were included. Findings were organised according to nine major topics: (1) lack of preparedness vs. timely response and flexible solutions, (2) changes in access, referrals, and admission, (3) impacts on outpatient, community and psychosocial services, (4) inpatient: reorganisation of hospital psychiatric units/acute wards, (5) diagnostic and therapeutic adaptations, (6) effects on medication, (7) infection control measures, (8), changes in patients’ demands, engagement, and mental health, and (9) impacts on staff and team. Many services were closed intermittently or considerably reduced while telepsychiatric services were extensively expanded. Face-to-face services decreased, as did the work with therapeutic groups. Many inpatient units restructured their services to accommodate COVID-19 patients. While the digitalisation of services allowed for better access to services for some, restrictive measures hindered access for most. Staff experienced changes such as heightened impacts on their own mental health, burdens on patients and the pausing of professional training. Clearly, diverse findings of studies relate to different (national) contexts, type of service offered, but also to the time of the investigation, as studies noted several distinct phases of change during the pandemic. This review suggests directions for policy and service development, such as fostering community services and providing support services for particularly vulnerable populations.
Keywords: Community psychiatry, COVID-19, Coronavirus, Pandemic, Mental health services, Telepsychiatry, Systematic review
Introduction
The COVID-19 pandemic hit most parts of the world at the beginning of 2020 unpreparedly. When countries decided on measures to protect the population from the spread of the virus and healthcare systems from collapsing under the burden of too many patients in need of intensive care, many aspects of daily life changed. Public health crises are disproportionally associated with an increasing burden of psychological suffering and mental health (MH) problems in the population, especially among those with pre-existing psychological vulnerabilities (Roudini et al., 2017). Recent research is showing that the psychological effects of the COVID-19 pandemic and the restrictive measures are far reaching for the general population (Röhr et al., 2020), for healthcare professionals (Muller et al., 2020; Weibelzahl et al., 2021) and for people with pre-existing MH problems (Frank et al., 2020). In humanitarian crisis and public emergency situations, protocols, such as of the WHO (2005) or IASC (2015), recommend an increased focus on psychological support. However, in the COVID-19 pandemic the primary response across most countries seems to have been a segmented medical response – the focus was mostly on preventing the spread of the virus rather than a unified response of all healthcare sectors addressing the emergency situation in a way that included its potential psychological effects (Fasshauer et al., 2021a). According to Fasshauer et al. (2021a), people with pre-existing MH problems were not adequately considered in the laws which were introduced to protect the population and the interests of this group were rarely mentioned, at least in the German COVID-19 restriction policies. Yet, due to the pandemic situation, many professionals expect a surge in MH problems (Bäuerle et al., 2020).
Mental health services (MHS) encompass any intervention or therapy, including the assessment, diagnosis, treatment, or counselling, offered in inpatient, outpatient, private, or public settings for the maintenance or enhancement of MH or the treatment of psychological disorders (see APA, 2022). The organisation of MHS differ within and across countries, varying from community-based services to psychiatric hospital-based care (Thornicroft et al., 2016). More details on MHS globally can be found in the Mental Health Atlas, published by the WHO which provides up-to-date information on MHS, MH policy and MH systems worldwide since 2001 (WHO, 2021). Already before the COVID-19 pandemic, the WHO found a substantiated MH treatment gap between the number of people with psychological disorders and the number receiving treatment (Alonso et al., 2018; Evans-Lacko et al., 2018).
The challenges posed for healthcare systems by the COVID-19 pandemic are unprecedented (Byrne et al., 2021). However, research on other major crises, such as the Ebola virus disease, has shown that these emergency situations tend to result in impaired provision of healthcare (Heymann et al., 2015) and of mental healthcare in particular (Vivalya et al., 2022), while at the same time increasing the need for adequate responses of MHS (Roudini et al., 2017). At the same time, crises have often been regarded as catalyst to change holding the potential to transform public organisations (Brecher and Yehuda, 1985; Rochet et al., 2008).
Although being a respiratory disease, COVID-19 has affected the services caring for the needs of people with MH problems around the world (Bojdani et al., 2020; Thome et al., 2020). In Germany, for instance, psychiatric clinics reduced their inpatient treatment capacity by 40% relative to the time before the onset of the pandemic (Adorjan et al., 2021; Fasshauer et al., 2021b) and length of hospital stays as well as emergency hospital admissions decreased significantly in the first phase of the pandemic (Fasshauer et al., 2021c). At the same time, around the world, MHS tried to guarantee continuity of care by introducing telepsychiatry (Reay et al., 2020) which might represent a historical transformation emerging from the crisis. The term telepsychiatry (TP) is used here to refer to MHS (including psychosocial care and psychotherapy) that are provided via digital means (e.g., video call) or telephone.
While the move to TP seems to have been an overarching response of MHS globally, there is still little systematic knowledge about the positive and negative impacts of the pandemic on MHS provision. As more and more empirical studies are investigating the latter, it becomes of importance to integrate these results for a bigger picture. By conducting a systematic review of the primary literature, the current article aims to respond to the following question: Which changes did mental health services worldwide experience during and due to the COVID-19 pandemic?
2. Methods
The methods of this systematic review were specified in advance and documented in the International Prospective Register of Systematic Reviews (PROSPERO, registration number CRD42021297314).
2.1. Search strategy
The search strategy was extensive. We searched the databases Medline, Web of Science, PsycINFO and Redalyc using the direct database interfaces and furthermore Ovid, EBSCOhost and ProQuest. Keywords were “covid OR corona” AND “psychological OR psychiatric OR psychosocial OR mental health AND “services” Or “therapy” OR “care” in English, and the Spanish, Portuguese, French and German equivalents. Databases were searched on the 04.02.2021. Citation tracking and a google scholar alert were applied until the 31.03.2022.
2.2. Inclusion/exclusion criteria for studies
Primary studies had to be published from December 2019 until March 2022. We only included peer-reviewed empirical studies that applied qualitative, quantitative or mixed-methods. Studies had to focus on the changes of MHS during the COVID-19 pandemic. Studies that focused on other healthcare services, evaluations of TP, or changes in MH were excluded.
2.3. Screening methods and data extraction
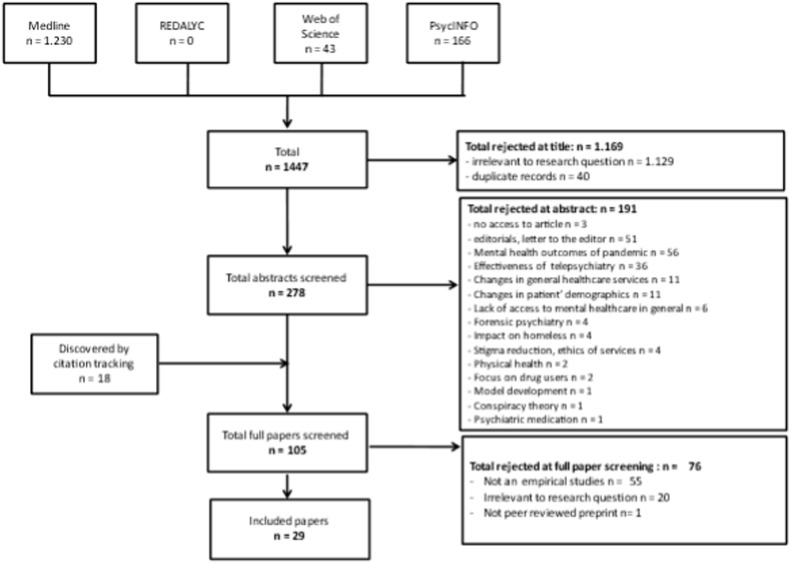
The screening of primary studies followed the guideline “preferred reporting items for systematic reviews and meta-analyses” (PRISMA; Moher et al., 2010; see Fig. 1 ). JabRef software was used to store and manage the data throughout the process. Title screening was conducted by a single team member. From the stage of abstract screening two independent reviewers evaluated the records and disagreement regarding inclusion/exclusion between the reviewers was resolved by discussions. Interrater reliability was high (percent agreement: 97.1%).
Fig. 1.
PRISMA flow chart.
Data extraction included study details such as study design, methods, participants’ characteristics, and primary results.
The quality of qualitative studies was assessed using the 10-item Critical Appraisal Skills Programme (CASP) checklist (CASP, 2018). For quantitative studies the 14-item “Checklist for assessing the quality of quantitative studies” was used (Kmet et al., 2004) with a reduced 10 item scoring manual. The quality of mixed methods studies was assessed with a 10-item combination of the CASP and the quantitative assessment tool, as well as elements of the Mixed Method Evaluation Rubric (MMER; Creamer; 2018). The items on each checklist were attributed a numerical value (No = 0, Can't Tell = 0.5, Yes = 1), resulting in a maximum total score of ten. The total score was used to categorise the methodological quality as either ‘high’ (>8–10), ‘moderate’ (6–8) or ‘low’ (≤5).
2.4. Synthesis method
Due to the recentness of the COVID-19 pandemic, we did not expect to identify large-scale longitudinal studies. Instead, we prepared for a heterogeneous range of study designs rendering formal comparison difficult. Therefore, we applied a combination of data-driven thematic synthesis (Thomas and Harden, 2008) and narrative synthesis (Popay et al., 2006) to identify key topics across studies. We described the findings of included studies and used tabulation to identify “patterns across studies” (Popay et al., 2006, p.17), referred to as “topics” here. The analysis was conducted by two team members who independently reviewed patterns to ensure that the synthesis reflects the studies’ findings and conclusions in relation to the review question. Note that the absence of a topic in a study does not necessarily mean the absence of that issue in practise, but rather might reflect the particular method of the study and the questions that were asked within the investigation.
3. Results
3.1. Extracted records results
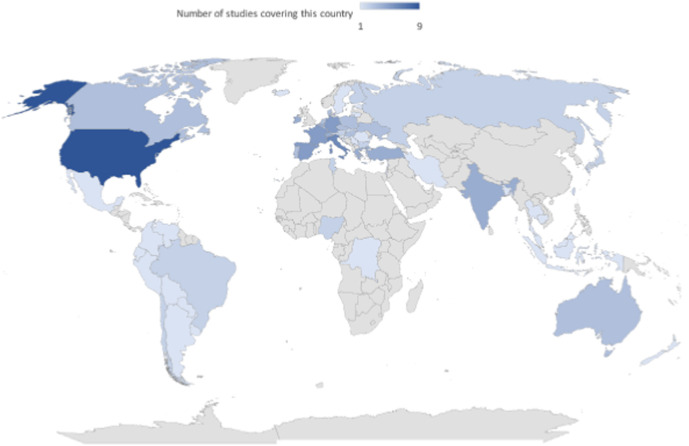
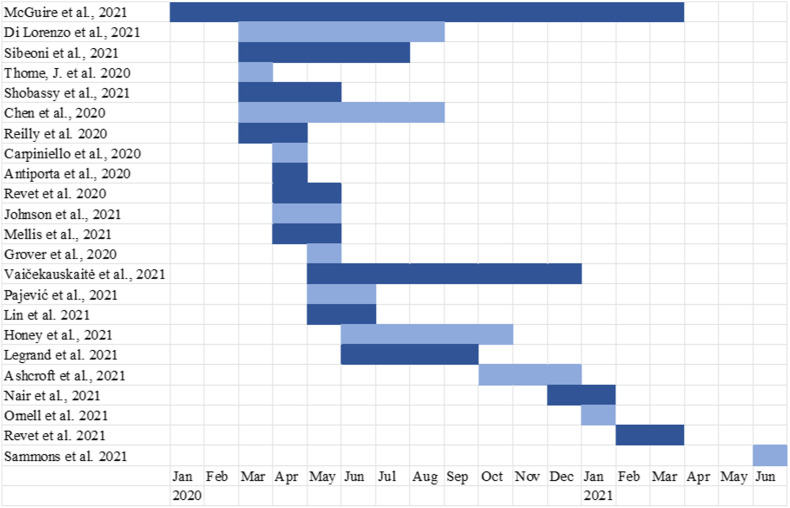
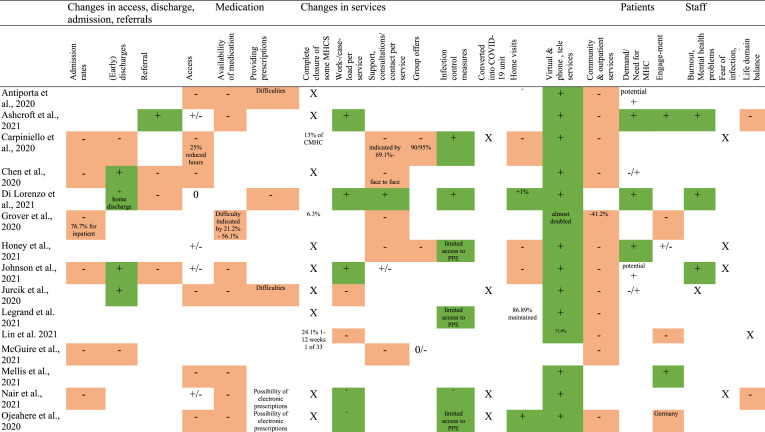
At the end of the selection process 29 articles were retained. Of the excluded empirical studies most reported on general MH outcomes for the population (n studies = 787), physical health (n = 83), the development of MH interventions against the effects of the pandemic (n = 79), intimate/domestic violence (n = 51), and evaluations of TP (n = 36). General characteristics of the included studies are represented in Table 1 . They were published in 2020 (n = 11) and 2021 (n = 18) with studies having been carried out at various time points (see Fig. 2 ). 22 studies were single country studies, and seven studies were carried out in several countries (see Fig. 3 ). Ten studies used qualitative, 16 quantitative and three mixed methods approaches.
Table 1.
Included articles (n = 29).
| Reference | Country and Region of Study | Data collection period | Aim | Methods | Participants & Setting/Data sources | Main Findings | Quality |
|---|---|---|---|---|---|---|---|
| Antiporta DA, Bruni A. Emerging mental health challenges, strategies, and opportunities in the context of the COVID-19 pandemic: Perspectives from South American decision-makers. Rev Panam Salud Publica;44:e154. | Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Paraguay, Peru, Uruguay, Venezuela | Mid April 2020 | Identify emerging MH problems, strategies to address them, & opportunities to reform MH systems during the COVID-19 pandemic in South America | Online semi-structured questionnaire Thematic & summative content analysis |
9 South American ministries of health |
|
moderate |
| Ashcroft, R., Donnelly, C., Dancey, M., Gill, S., Lam, S., Kourgiantakis, T., … & Brown, J. B. (2021). Primary care teams' experiences of delivering mental health care during the COVID-19 pandemic: a qualitative study. BMC family practice, 22(1), 1–12. | Canada (Ontario) | October–December 2020 | Impact of COVID-19 on primary care teams' delivery of MHS | Descriptive qualitative design: Focus Groups using online virtual video platform Thematic Analysis |
11 focus groups with 10 primary care teams - total of 48 participants | Three key themes:
|
high |
| Carpiniello B, Tusconi M, Zanalda E, Di Sciascio G, Di Giannantonio M; (2020). Executive Committee of The Italian Society of Psychiatry. Psychiatry during the Covid-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatry 20(1):593. | Italy (Northern Italy; Central Italy; Southern Italy, including the Islands) | 01.04.2020–11.04.2020 | Impact of the current emergency on the activities of services & the way in which MHS are addressing the current pandemics | Survey | 71 mental health departments 107 Psychiatric Wards in General Hospitals |
|
high |
| Chen, S.; Jones, P. B.; Underwood, B. R.; Moore, A.; Bullmore, E. T.; Banerjee, S.; Osimo, E. F.; Deakin, J. B.; Hatfield, C. F.; Thompson, F. J. (2020). The early impact of COVID-19 on mental health and community physical health services and their patients' mortality in Cambridgeshire and Peterborough, UK. Journal of psychiatric research, 2(131), 244-254 | United Kingdom (Cambridgeshire and Peterborough) | 23.3.2020 (lockdown, week 13) - May/August 2020 (depending on record system & obtained data) | Changes in presentations & referrals to the primary provider of MHS & community health services, plus service activity and deaths | Interrupted time series analyses | Data obtained from four clinical records systems (RiO, SystmOne, PCMIS & Epic) Analysis of: referrals, calls to MH emergency, presenting problems, admissions, discharges, detention, documentation, types & numbers of contacts, & deaths per day |
|
high |
| Di Lorenzo, R., Fiore, G., Bruno, A., Pinelli, M., Bertani, D., Falcone, P., … & Ferri, P. (2021). Urgent psychiatric consultations at mental health center during COVID-19 pandemic: retrospective observational study. Psychiatric Quarterly, 1–19. | Italy (Modena) | 1.3.2019–31.8.2019 and 1.3.2020–31.8.2020 | Investigate changes which occurred in the urgent psychiatric consultations (UPC) at outpatient MHS in Modena |
Retrospective observational study - demographic & clinical data on patients who required UPC - referral to UPC - setting of UPC - clinical motivations - therapeutic prescriptions - UPC outcomes |
2019: 656 urgent psychiatric consultations requested by 425 patients 2020: 811 UPC requested by 488 patients |
|
high |
| Grover, S.; Mehra, A.; Sahoo, S.; Avasthi, A.; Tripathi, A.; D'Souza, A.; Saha, G.; Jagadhisha, A.; Gowda, M.; Vaishnav, M. (2020). Impact of COVID-19 pandemic and lockdown on the state of mental health services in the private sector in India. Indian Journal of Psychiatry, 62, 488 | India (no region specified) | 01.05.2020–15.05.2020 | impact of lockdown & COVID-19 pandemic on private MHS in India | Online survey | 396 members of the Indian Psychiatric Society: 40.7% single-chamber outpatient clinic, 19.7% working in corporate hospitals, 17.4% hospital with inpatient facility, 13.6% hospital with the only outpatient facility, 8.6% other set-up |
|
moderate |
| Honey, A., Waks, S., Hines, M., Glover, H., Hancock, N., Hamilton, D., & Smith-Merry, J. (2021). COVID-19 and Psychosocial Support Services: Experiences of People Living with Enduring Mental Health Conditions. Community mental health journal, 57(7), 1255–1266. | Australia (no region specified) | June–October 2020 | How did the COVID-19 pandemic shape people's engagement in & experiences with psychosocial support services in Australia? | Qualitative secondary analysis Data from written questionnaires & in-depth interviews |
total of 121 people with enduring mental illness discussed COVID-19: 59 in the questionnaire only, 55 in the interview, & 7 in both questionnaire & interview |
|
high |
| Johnson S, Dalton-Locke C, Vera San Juan N, Foye U, Oram S, Papamichail A, Landau S, Rowan Olive R, Jeynes T, Shah P, Sheridan Rains L, Lloyd-Evans B, Carr S, Killaspy H, Gillard S, Simpson A (2021). COVID-19 Mental Health Policy Research Unit Group. Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol. 56(1):25–37. | United Kingdom (no region specified) | 22.04.2020–12.05.2020 | staff reports regarding impact of the COVID-19 pandemic in early weeks on MHC & MHS users in the UK | mixed methods survey | 2180 staff from a range of sectors, professions & specialties: 1,935, (88.9%) worked in the NHS - nurses (664, 30.6%), 347 psychologists (16.0%), 254 psychiatrists (11.7%), 97 social workers (4.5%), 80 as peer support workers (3.7%). 826, (38.0%) identified as a manager/lead clinician in their service |
|
high |
| Jurcik, T.; Jarvis, G. E.; Zeleskov Doric, J.; Krasavtseva, Y.; Yaltonskaya, A.; Ogiwara, K.; Sasaki, J.; Dubois, S. & Grigoryan, K. (2020). Adapting mental health services to the COVID-19 pandemic: Reflections from professionals in four countries. Counselling Psychology Quarterly, 1-27 | Australia, Canada, Japan, Russia | not indicated | Experience of MHP working in Covid-19 | Collaborative autoethnographic method | 8 clinicians |
|
high |
| Legrand, G., Boisgard, C., Canac, B., Cardinaud, Z., Gorla, M. G., Gregoire, E., … & Vaury, P. (2021). Organisation and timeline of measures in French psychiatric establishments during the first wave of the COVID-19 epidemic: EvOlu’Psy study. BMC psychiatry, 21(1), 1–17. | France (metropolitan France, no region specified) | June–September 2020 (survey) | assess the organisation by psychiatric facilities in France of their response to COVID-19 during the first wave (5.3.2020 - 6.6.2020) |
Structured audit grid & Review & Phone survey |
94 hospitals in metropolitan France with capacity for fulltime, inpatient psychiatric hospitalisation of adults |
|
high |
| Lin, T., Stone, S. J., & Anderson, T. (2021). Treating from Afar: Mental Health Providers' Challenges and Concerns During the COVID-19 Pandemic. Behavioral Medicine, 1–4. | USA (no region specified) | 28.05.2020–30.06.2020 | identify how therapists have been responding to the public health crisis and the rapid transition to telepsychology |
Survey | 502 MHP |
|
moderate |
| McGuire, A.B.; Flanagan, M.E.; Kukla, M.; Rollins, A.L.; Myers, L.J.; Bass, E.; Garabrant, J.M.; Salyers, M.P. (2021). Inpatient Mental Healthcare before and during the COVID-19 Pandemic. Healthcare, 9, 1613. |
USA (every region of the continental USA) | 01.09.2019–15.03.2021 | 1) describe changes to inpatient MHS: admissions, length of stay, and therapeutic services, before and after the COVID-19 pandemic onset 2) examine relationship between inpatient MHCS provision & relapse rates |
Data from the Veterans Affairs Corporate Data Warehouse: medical records | cohort of 33 Veterans Health Affairs (VHA) acute inpatient mental health units |
|
high |
| Mellis AM, Potenza MN, Hulsey JN. (2021). COVID-19-related treatment service disruptions among people with single- and polysubstance use concerns. J Subst Abuse Treat.,121:108,180 | USA (no region specified) | 27.04.2020–13.05.2020 | Determine if specific groups with substance use were more likely to experience unmet service needs | Survey of patients & family networks | 1148 participants who use substances and their relatives |
|
high |
| Nair, S., Kannan, P., Mehta, K., Raju, A., Mathew, J., & Ramachandran, P. (2021). The COVID-19 pandemic and its impact on mental health services: the provider perspective. Journal of Public Health, 43(Supplement_2), ii51-ii56. | India (Chennai, Tamil Nadu) | December 2020–January 2021 | the impact on services and adaptations during the COVID 19 pandemic | In-depth interviews and a focus group discussion | 10 service providers from an NGO: managers of clinical services, administrative staff, psychiatrists, social workers, psychologist, and researcher staff employed in community research projects |
|
high |
| Ojeahere MI, de Filippis R, Ransing R, Karaliuniene R, Ullah I, Bytyçi DG, Abbass Z, Kilic O, Nahidi M, Hayatudeen N, Nagendrappa S, Shoib S, Jatchavala C, Larnaout A, Maiti T, Ogunnubi OP, El Hayek S, Bizri M, Schuh Teixeira AL, Pereira-Sanchez V, Pinto da Costa M. (2020). Management of psychiatric conditions and delirium during the COVID-19 pandemic across continents: lessons learned and recommendations. Brain Behav Immun Health., 100,147. |
Bangladesh Brazil, Germany, India, Italy, Iran, Kosovo, Lebanon, Nigeria, Pakistan, Portugal, Turkey, Thailand, Tunisia, UK, USA |
not indicated | Challenges and good practices faced in the management of psychiatric conditions manifesting in patients with Covid-19 | Group discussion | 21 early careers psychiatrists from 16 countries |
|
moderate |
| Ornell, F., Borelli, W. V., Benzano, D., Schuch, J. B., Moura, H. F., Sordi, A. O., Paim Kessler, F.H, Nichterwitz Scherer, J. & von Diemen, L. (2021). The next pandemic: impact of COVID-19 in mental healthcare assistance in a nationwide epidemiological study. The Lancet Regional Health-Americas, 100,061. | Brazil (no region specified) | January 2021 | - analyse temporal trends & prediction of appointments held in Brazil's public health system - compare observed & expected number of MHC appointments during COVID-19 pandemic |
Ecological time-series study | Brazilian governmental database (period January 2016–August 2020) |
|
high |
| Pajević I, Hasanović M, Avdibegović E, Džubur-Kulenović A, Burgić- Radmanović M, Babić D, Mehić-Basara N, Zivlak-Radulović N & Račetović G. (2020). Organisation of mental healthcare in Bosnia and Herzegovina during coronavirus disease 2019 pandemic. Indian J Psychiatry, 62, S479–S491. | Bosnia and Herzegovina (no region specified) | 11.05.2020–10.06.2020 | explore organisation of psychiatric services in Bosnia and Herzegovina to meet MH needs during particular restrictive measures in COVID-19 pandemic | Online survey with open and closed questions | 38 MHS: 3 departments of psychiatry (University Clinical Centres), 2 psychiatric hospitals, 4 psychiatric wards in general hospitals, 27 Community MH Centres, 2 institutes for alcoholism & addiction disorders |
|
low |
| Patel, R., Irving, J., Brinn, A., Broadbent, M., Shetty, H., Pritchard, M., … & McGuire, P. (2021). Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ open, 11(3), e046365. | UK (South London) | not indicated | pandemic impact on use of remote consultation & prescribing of psychiatric medications |
Clinical Record Interactive Search tool - deidentified electronic health records of people receiving MHC (7.1.2019–20.9.2020) |
Patients receiving MHC from South London and Maudsley NHS Foundation Trust → secondary MHC data |
|
high |
| Reilly SE, Zane KL, McCuddy WT, Soulliard ZA, Scarisbrick DM, Miller LE, Mahoney Iii JJ. (2020). Mental Health Practitioners' Immediate Practical Response During the COVID-19 Pandemic: Observational Questionnaire Study. JMIR Ment Health, 1;7(9):e21237. | USA (Midwest, Northeast, South, West) |
30.3.2020–10.4.2020 | characterize how MHP have changed their practices during the pandemic | Online survey (Qualtrics) | 903 MHP:
|
|
high |
| Revet A, Hebebrand J, Anagnostopoulos D, Kehoe LA (2021). COVID-19 Child and Adolescent Psychiatry Consortium, Klauser P. ESCAP CovCAP survey of heads of academic departments to assess the perceived initial (April/May 2020) impact of the COVID-19 pandemic on child and adolescent psychiatry services. Eur Child Adolesc Psychiatry 20; 1–10. | Austria, Belgium, Czech Republic, Denmark, France, Germany, Greece, Hungary, Ireland, Italy, Poland, Slovenia, Spain, Switzerland, Turkey, The Netherlands, Estonia, Bulgaria, Serbia, Slovakia | 16.04.2020–19.05.2020 | - evaluate (early) impact of COVID-19-pandemic on child & adolescent psychiatry (CAP) services in Europe - assess abilities to meet the new challenges | Online Survey | 82 participants (56 complete responses): heads of academic CAP services in 20 European countries |
|
high |
| Revet, A., Hebebrand, J., Anagnostopoulos, D., Kehoe, L. A., Gradl-Dietsch, G., & Klauser, P. (2021). Perceived impact of the COVID-19 pandemic on child and adolescent psychiatric services after 1 year (February/March 2021): ESCAP CovCAP survey. European Child & Adolescent Psychiatry, 1–8. | Austria Belgium Bulgaria Croatia Czech Republic Denmark France Germany Greece Hungary Italy Ireland Netherlands Poland Portugal Slovakia Slovenia Spain Switzerland Turkey UK Ukraine |
19.02.2021–25.03.2021 | - estimate impact of COVID-19 on CAP services in Europe - assess abilities to meet the new challenges |
Online Survey | 72 heads of CAP university services in 22 countries |
|
moderate |
| Roncero C, García-Ullán L, de la Iglesia-Larrad JI, Martín C, Andrés P, Ojeda A, González-Parra D, Pérez J, Fombellida C, Álvarez-Navares A, Benito JA, Dutil V, Lorenzo C, Montejo ÁL. (2020). The response of the mental health network of the Salamanca area to the COVID-19 pandemic: The role of the telemedicine. Psychiatry Res.;291; 113,252. |
Spain (Salamanca) | not indicated | - investigate response of the MH Network of Salamanca Area (Spain) to COVID-19 pandemic & reorganisation of resources within the first 8 weeks after declaration of state of alarm (14.03.2020) | Observational study, comparing the organisation and medical activities with the same period of 2019 (March to April) |
|
moderate | |
| Rosenberg S, Mendoza J, Tabatabaei-Jafari H (2020). Pandemic-Mental Health International Network (Pan-MHIN), Salvador-Carulla L. International experiences of the active period of COVID-19 - Mental health care. Health Policy Technol.;9(4):503–509. | Australia, Denmark, Italy, Spain, Taiwan, UK, USA | not indicated | understand changes in MH systems | Rapid Synthesis and Translation Process (RSTP) Synthesis, Interviews, expert panel, digital conferencing |
8 webinars, 15 interviews - 16 locations, 500 participants |
|
moderate |
| Sammons, M. T., Elchert, D. M., & Martin, J. N. (2021). Mental health service provision during COVID-19: results of the third survey of licensed psychologists. Journal of Health Service Psychology, 47(3), 119–127. | USA (no region specified) | 01.06.2021–21.06.2021 | report on psychologists' changing perceptions of practice in a post-pandemic era | Survey | 2807 psychologists With professional liability insurance from The Trust/holders of the National Register's Health Service Psychologist credential |
|
high |
| Shaw H, Robertson S, Ranceva N. What was the impact of a global pandemic (COVID-19) lockdown period on experiences within an eating disorder service? A service evaluation of the views of patients, parents/carers and staff. J Eat Disord. 9(1):14 | UK (Liverpool) | not indicated | service evaluation: how did the pandemic change service provision in a young person's eating disorder service | audit online survey open ended answers open ended focus groups |
42 participants: 12 patients, 19 parents/carers 12 staff members |
|
high |
| Shobassy, A., Nordsletten, A. E., Ali, A., Bozada, K. A., Malas, N. M., & Hong, V. (2021). Effects of the COVID-19 pandemic in a psychiatric emergency service: Utilization patterns and patient perceptions. The American Journal of Emergency Medicine, 52, 241–243. | USA (Midwestern academic medical center) | 16.03.2020–17.05.2020 | -understand early impacts of the COVID-19 pandemic on youth & adults in Psychiatric Emergency Services (PES) - examine patterns of PES service utilization & assess various ramifications per patient report |
1) retrospective analysis of visits to PES during study period 2) questionnaire addressing patients' experiences in pandemic |
1.) Retrospective visit analysis 2.) n = 271 patients filling in survey |
|
moderate |
| Sibeoni, J., Manolios, E., Costa-Drolon, E., Meunier, J. P., Verneuil, L., & Revah-Levy, A. (2021). Clinical practice during the COVID-19 pandemic: a qualitative study among child and adolescent psychiatrists across the world. Child and adolescent psychiatry and mental health, 15(1), 1–15. | Tunisia, India, Ireland, Chile, Bangladesh, Canada, Taiwan, Indonesia, Finland, Switzerland, Greece, France, Malaysia, Belgium Mexico, Ukraine, Nigeria, Cambogia, Hungry, New Zealand Congo-Kinshasa, USA, Japan, Germany, UK, Portugal | March–July 2020 | explore lived experience of clinical practice during the pandemic among Child & adolescent psychiatrists across the globe | structure of lived experience (IPSE) approach |
39 Child and adolescent psychiatrists from 26 countries (age range 32–70 years; 23 women). |
|
high |
| Thome, J.; Deloyer, J.; Coogan, A. N.; Bailey-Rodriguez, D.; da Cruz E Silva, O. A.; Faltraco, F.; Grima, C.; Gudjonsson, S. O.; Hanon, C.; Holly, M. (2020). The impact of the early phase of the COVID-19 pandemic on mental-health services in Europe.The World Journal of Biological Psychiatry, 1-10 | Belgium, Czech Republic, Finland, France, Germany, Greece, Iceland, Ireland, Israel, Italy, Luxembourg, Malta, The Netherlands, Poland, Portugal, Romania, Russia, Spain, Sweden, Switzerland, Turkey, Ukraine, UK | late March 2020- 2nd week of April 2020 | pan-European snapshot of MHS during the early phase of the European COVID-19 epidemic | Ad-hoc survey | 23 participants: 10 psychiatrists, 4 specialists in psychiatric nursing, 6 psychologists, 2 allied health professionals working in MH |
|
high |
| Vaičekauskaitė, R., Babarskienė, J., & Grubliauskienė, J. (2021). Mental health services during the pandemic: the experiences of Lithuanian psychologists. Sabiedrība. Integrācija. Izglītība: starptautiskās zinātniskās konferences materiāli: gada 28.-29. maijs, 7, 217–229. | Lithuania (no region specified) | May–December 2020 | experiences of Lithuanian psychologists providing mental health services during the pandemic | semi-structured interview; some responded in written form, qualitative content analysis (Graneheim, 2017) | 10 participants, 9 females and one male (average age of 30 years) from Lithuania - all psychologists |
|
moderate |
Fig. 2.
Timeline of the study periods
Note. There was no information on study periods available for Jurcik et al. (2020); Ojeahere et al. (2020); Patel et al., (2021); Roncero et al., (2020); Rosenberg et al. (2020); Shaw et al. (2021)..
Fig. 3.
World map of countries investigated by primary studies.
During the process of synthesising primary studies, we developed a data-driven framework with nine topics.
3.1.1. Lack of preparedness and closure vs. timely response and flexible solutions
All MHS were affected by the COVID-19 pandemic to some extent. The level and type of impact differed depending on the location, and on the diverse phases of the pandemic. Rosenberg et al. (2020) established a COVID-19 MH international network whose members engaged in eight webinars and 15 interviews. The authors described three different phases of change during the COVID-19 pandemic: the preparatory, active and recovery phase. Particularly the early phase of the pandemic was characterised by anxiety and uncertainty (Sibeoni et al., 2021; Thome et al., 2020; Vaičekauskaitė et al., 2021). Revet et al. (2020, 2021) administered two online surveys to heads of child and adolescent psychiatry services (CAPS) across Europe – one in April-Mai 2020), the other one in February–March 2021. In 2020, 80% of the participants reported that COVID-19 had a major or extreme impact on service provision, whereas in 2021 the majority reported only a minor impact.
Apparent in most studies was a description of a lack of preparedness of MHS. Many studies noted staff as poorly trained to respond to the pandemic, particularly concerning the delivery of TP (Antiporta and Bruni, 2020; Rosenberg et al., 2020; Thome et al., 2020). In some places, scarce resources had affected the MHS already before the pandemic and were now hindering the transition to TP or caused job loss and pay cuts (Antiporta and Bruni, 2020; Nair et al., 2021; Ojeahere et al., 2020). Some services closed completely for a certain amount of time (n studies = 20, see Table 2 ). Ojeahere et al. (2020) conducted group discussions with psychiatrists from 16 countries and found that services were suspended in Indian private psychiatric outpatient departments, in Nigerian inpatient clinics, and in Thailand in general hospitals. Grover et al. (2020) administered an online survey to members of the Indian Psychiatric Society and found a total shut down for 6.3% of all MHS during lockdown. Legrand et al. (2021) used a structured audit grid and a phone survey of hospitals with inpatient psychiatric units in metropolitan France. The researchers found that while 94.7% of services maintained fulltime inpatient hospitalisation, 96.4% of services closed or only partially maintained day hospitalisation under the first COVID-19 wave. In a survey of MH departments and psychiatric wards (PW) in Italy, Carpiniello et al. (2020) observed that since the first lockdown 13.1% of the PW had been closed, and only small residential facilities (RFs) remained functioning. In the USA, a survey of MH professionals (MHP, Lin et al., 2021) showed that 24.1% had to suspend clinical work for a period of one to 12 weeks. In analysing data from the US Veterans Affairs, McGuire et al. (2021), found a high variability in disruption of MHS across acute inpatient units with drops from 3% to 100% in April 2020. In Europe, 68% of heads of CAPS indicated a closure of day-care and 32% of inpatient units in 2020, while in 2021, 14.3% reported closure of day-care, 10.7% of inpatient and 8.9% of outpatient units (Revet et al., 2020, 2021).
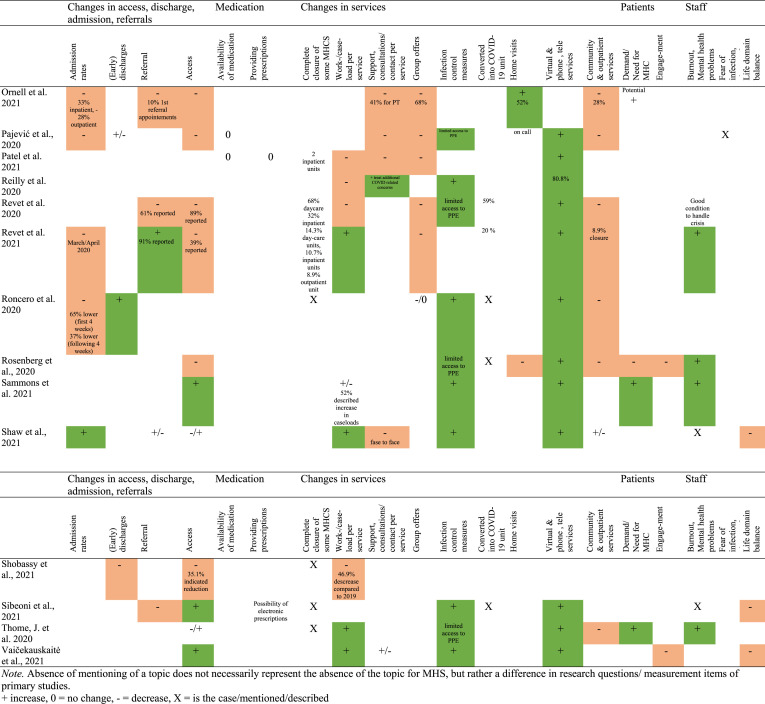
Table 2.
Changes in mental healthcare services as represented by the studies..
At the same time, some articles stressed the timely response of MHS to the challenges posed by the pandemic. Jurcik et al. (2020) conducted a collaborative autoethnography with clinicians from Australia, Canada, Japan and Russia and perceived particularly the services in Australia to adapt quickly to the new situation. Rosenberg et al. (2020) stressed that especially in Taiwan well established pandemic plans supported a quick adaptation. In an online survey and focus groups-based evaluation of an eating disorder service in the UK, patients appreciated the continuous availability of supportive teams and the integrity of services during the pandemic (Shaw et al., 2021). Sometimes flexible solutions to new challenges were found, for instance in Thailand, where health volunteers in villages helped to distribute psychotropic medication (Ojeahere et al., 2020). Sibeoni et al. (2021) found professionals to work “outside the box”, such as by encountering patients in outside spaces, taking walks, or playing games online with them. The study was an exploration of the clinical practice experience during the pandemic among child and adolescent psychiatrists from 26 countries. Johnson et al. (2021) carried out a mixed methods survey in the UK with MH staff. The authors identified shifts towards reduced bureaucracy, more flexibility, and agile and responsive ways of working. In many places, helplines and new crisis services were rapidly established as alternatives to emergency departments, and some community MHS changed the type of help offered, such as starting to provide resource packs for patients (Johnson et al., 2021; Legrand et al., 2021; Nair et al., 2021).
3.1.2. Changes in access, admission, and referrals
Due to concerns of spreading COVID-19 access to services was considerably impaired (studies = 18, see Table 2). In Italy, 25% of community MHS decreased their hours of access (Carpiniello et al., 2020). Nair et al. (2021) used interviews and a focus group discussion with Indian NGO service providers in Chennai, Tamil Nadu, and found that patients could not physically access MHS or were restricted in their movement. Often waitlists became longer as demand for MHS increased (Ashcroft et al., 2021; Sammons et al., 2021). 35.1% of patients responding to a questionnaire in the USA indicated decreased access to MHS (Shobassy et al., 2021). Of this group 42.7% stated that this limited access had contributed to their need to seek psychiatric emergency services (PES), and 22.1% indicated having delayed care seeking due to fears of infection. However, studies also reported increased access due to the shift to remote services (n studies = 9), as overall attrition decreased, and some patients felt less threatened by teleconsultations.
In many places admission rates decreased (n studies = 10) at some point in the pandemic. In India, the number of patients admitted to inpatient services dropped by 76.6% (Grover et al., 2020). In Italy, 84.5% of community MHS indicated a reduction in hospital admission, 87.8% of PWs reported decreased admission and 77.4% of MHS suspended new admissions to RFs (Carpiniello et al., 2020). McGuire et al. (2021) observed a noticeable drop in admissions in the analysed acute inpatient MH units in April, November and December 2020, which the authors link to the peaks in COVID-19 rates in the USA. Ornell et al. (2021) conducted an ecological time-series study using Brazilian governmental data from January 2016 to August 2020. The researchers compared observed and expected numbers of MHS appointments and found a 33% decrease in hospital admissions for inpatient care during the pandemic. Roncero et al. (2020) compared the activities of the Salamanca MH network during the first eight pandemic weeks with the same period in 2019. The study identified a decrease of 65% in hospital admissions during the first four weeks of the pandemic, and of 37% during the following four weeks.
A pattern emerged across studies in relation to referral rates. The fact that many services closed or did not provide care for new patients lead to decreased referral rates at the beginning of the pandemic (n studies = 6). All focus groups of UK primary care teams in the study by Ashcroft et al. (2021) reported increased referrals, but less referrals during the first lockdown. Via an interrupted time series analyses of clinical UK records, Chen et al. (2020) identified a sharp reduction in MHS referrals at lockdown (particularly for those without a recorded severe mental illness, SMI) followed by an increase towards normal levels. In line with this pattern, 61% of participants in the study by Revet et al. (2020) reported a decrease in referrals at the beginning of the pandemic, while 91% reported an increase in 2021 (Revet et al., 2021).
3.1.3. Impacts on outpatient, community, and psychosocial services
Social, community, and rehabilitation services were considerably reduced or ceased (n studies = 19), so that discharged patients were less likely to receive outpatient care in a timely manner. The closure of these services was often related to them being deemed non-essential in public health policy (Jurcik et al., 2020). In the US study conducted by Lin et al. (2021), participants listed as primary reasons for the suspension of services: technological issues and preparation for remote work, one's own health and government restrictions and clinic policies. In an online survey of MHP in the USA (Reilly et al., 2020), 48.2% rescheduled appointments, 26.6% cancelled them, and 17.2% restricted appointments. In Revet et al. (2020), 89% of child and adolescent psychiatrists indicated restricted access to outpatient care. 57.5% of staff in UK inpatient services experienced difficulties with discharging patients, as community MHS were less available (Johnson et al., 2021). In Brazil, an average of 28% fewer appointments for outpatient care than predicted were reported during the first six months of the pandemic (Ornell et al., 2021). Grover et al. (2020) found that during lockdown only 58.8% of the Indian professionals reported providing outpatient services and 16.7% psychotherapy services, compared to 100% and 61.6% before lockdown, respectively. In Italy operational day centres that focus on rehabilitation and psychosocial activities saw a reduction of 85% (Carpiniello et al., 2020).
Home care and visits were maintained by 86.9% of the responding institutions in France (Legrand et al., 2021), but were continued only when absolutely necessary in the UK (Johnson et al., 2021). Honey et al.’s (2021) qualitative secondary analysis of data from people living with enduring MH condition showed that home visits were rarely continued during the pandemic in Australia. On the other hand, in the USA, home-based treatment for patients with mild to moderate symptoms was adapted as an alternative to inpatient hospitalisation (Ojeahere et al., 2020). Similarly, in Brazil, home appointments were about 52% higher than predicted (Ornell et al., 2021).
3.1.4. Inpatient: reorganisation of hospital psychiatric units/acute wards
The closure of inpatient services was related to infection control, but moreover to the transformation of units to emergency COVID-19 units (n studies = 9, see Table 2). Further changes to inpatient services included reducing available beds, as well as restricting patients from leaving the hospital or from receiving visitors. Many inpatient services focused increasingly only on emergency cases and some reported early discharges (n studies = 6). Pajević et al. (2020) conducted an online survey of MHS in Bosnia and Herzegovina and explained that whilst patients without SMI were discharged for home treatment after the beginning of the pandemic, more severe patients were kept in the inpatient units. Activities within units were reduced so that admitted patients were less likely to receive treatment. For instance, 69.1% of participants indicated a decrease of consultations in PWs in Italy (Carpiniello et al., 2020) and in Brazil, daily psychiatric treatment was reduced by 66% (Ornell et al., 2021).
Especially the management of the comorbidity of SMI and COVID-19 was a topic of concern. For instance, 60% of PWs in Italy indicated admission to general COVID-19 units of positive and symptomatic COVID patients with non-SMI, whilst SMI patients with COVID were transferred to newly created COVID-19 PWs or to isolated parts of the wards (Carpiniello et al., 2020).
3.1.5. Diagnostic & therapeutic adaptations
Often, assessment and therapeutic activities were discontinued, reduced or adapted in diverse ways, such as by limiting the numbers of participants, excluding family members, establishing “zero” physical contact and particularly by shifting to a virtual format.
Especially group activities were cancelled or reduced in number of participants (n studies = 9). Carpiniello et al. (2020) reported that group psychotherapies and psychosocial interventions were reduced by approximately 90–95%. Ornell et al. (2021) found a decrease of 68% in group appointments, and 70% of participants in the survey by Revet et al. (2021) were majorly concerned about not being able to maintain treatment groups.
Professionals started using therapy apps (Johnson et al., 2021), social media (Jurcik et al., 2020; Reilly et al., 2020), and messengers to reach out to patients (Honey et al., 2021; Shaw et al., 2021), or the general public, patients or families or they established helplines (Jurcik et al., 2020; Legrand et al., 2021; Nair et al., 2021; Ojeahere et al., 2020; Reilly et al., 2020; Revet et al., 2020; Pajević et al., 2020).
Most studies reported that services rapidly implemented or extended TP (n studies = 26), while at the same time decreasing face-to-face contacts. This was the case across countries and services. Analysing electronic health records in South London (UK) from before and after the pandemic onset, Patel et al. (2021) noted a considerable decrease in number of weekly in-person contacts with MHP, while remote contacts increased. Revet et al. (2020) found 95% of MHP substituting face-to-face contacts by TP despite only 20% using TP before the pandemic. In the study by Lin et al. (2021), 96% of participating MHP provided TP at the time of the investigation. Reilly et al. (2020) found that 80.2% of MHP shifted to TP, and whilst in December 2019 80.4% had not been using TP, by early April 2020 this number had dropped to 22.1%. Sammons et al. (2021) conducted a US survey with psychologists and observed that with the pandemic a hybrid model of care evolved. In September 2020, 68% of MHP conducted all or almost all services using TP. In June 2021, TP was still predominated, but with declined numbers of respondents relying completely on this modality. Jurcik et al. (2020) found that particularly in Australia, the charging for TP was facilitated. However, in many places TP was not administratively regulated, and the covering of costs remained difficult (Pajević et al., 2020).
3.1.6. Infection control measures
The introduction of infection control procedures in MHS was described in most studies (n studies = 16). This included the use of personal protective equipment (PPE), screening for signs of infections or COVID-19 testing before entrance and physical distancing. For instance, 82% of survey institutions in France systematically checked for clinical signs of COVID-19 at admission, 84% had introduced training for staff about hospital hygiene for COVID-19, and 78.7% in taking nasopharyngeal samples (Legrand et al., 2021). Further measures included family members no longer accompanying patients, reduced time spent at services, and the use of outside spaces (Honey et al., 2021; Legrand et al., 2021).
Some MHP found infection control measures difficult to follow. Sometimes, guidelines were lacking (Ojeahere et al., 2020), MHP were not familiar with them (Rosenberg et al., 2020), the measures kept changing or were perceived as conflicting, too complex, impractical, or inappropriate (Johnson et al., 2021; Jurcik et al., 2020). For instance, 50.5% professionals in UK inpatient and residential care reported that they could not follow the rules consistently (Johnson et al., 2021). Several studies described limited availability of PPE in MHS (n studies = 7). Furthermore, there were concerns about impacts of PPE on therapeutic relationships. Child and adolescent psychiatrists, for example, reported difficulties in interacting with patients when they only saw half of the face (Sibeoni et al., 2021). Lack of space and space layouts were hurdles to follow physical distancing or to store PPE. For instance, 51.6% of staff in RF identified a difficulty of maintaining infection control as people could not be segregated from one another (Johnson et al., 2021).
3.1.7. Effects on prescriptions and access to medication
Studies found difficulties in access to prescriptions (n studies = 3). As services transferred to remote consultations, online prescriptions became of particular importance. These were facilitated in some places, such as India, where prescriptions were signed in official prescription pads and shared as a picture with patients over messenger services (Nair et al., 2021). Mostly however online prescriptions remained legally difficult (Jurcik et al., 2020). This may explain why Di Lorenzo et al. (2021) noted in their retrospective observational study that the increase in TP led to a significant decrease in drug prescription during the pandemic compared to 2019. Patel et al. (2021) could not find any substantial changes in prescriptions, except for an increase in aripiprazole depot, and a decrease in mentions of antipsychotics for adolescents and children, which the authors explain by the closure of inpatient units.
The pandemic caused a lack of availability of certain medications (n studies = 8), which was especially described in India, Nigeria, and South America (Antiporta and Bruni, 2020; Grover et al., 2020; Nair et al., 2021; Ojeahere et al., 2020). For instance, Nair et al. (2021) observed how not all local Indian pharmacies stocked MH medication, and Grover et al. (2020) reported patients having difficulties purchasing benzodiazepines (56.1%), antipsychotics (43.9%) and antidepressants (36.9%), among others. Antiporta and Bruni (2020) administered an online questionnaire to South American ministries of health and observed a disruption in the availability of psychotropic medications. In an US survey of participants who use substances, Mellis et al. (2021) found that polysubstance-involved participants were more likely than those with single substance use to experience inability to access naloxone and needle exchange services.
3.1.8. Changes in patients’ demands, engagement, MH and future expectations
Variation was reported regarding the engagement of services users (Honey et al., 2021). Five articles discussed a decrease in patients’ attendance and engagement, but two others observed increased engagement, such as less no-shows. Some patients dropped out of MHS due to financial issues or were reluctant to visit services due to fear of infection (Jurcik et al., 2020; Thome et al., 2020; Vaičekauskaitė et al., 2021).
Studies found drops (n studies = 3) and increases (n studies = 7) in demand for MHS during the pandemic. For instance, Di Lorenzo et al. (2021) found a significantly higher demand for urgent psychiatric consultations in 2020 compared to 2019. Similarly, Shobassy et al. (2021) reported that a significantly higher proportion of patients of PES were requiring psychiatric admission (50.7%) in 2020, relative to 2019 (37.9%). On the other hand, Jurcik et al. (2020) found that in many countries, professionals perceived a decreasing demand, and Chen et al. (2020) registered a drop in telephone calls to the crisis MHS and in self-presentations across the MHS system.
Some studies identified a surge in MH problems (n studies = 11), a deterioration of pre-existing conditions or expected future increases in MH issues. For instance, 46.3% of staff (Johnson et al., 2021) rated “relapse and deterioration in MH triggered by COVID-19 stresses” as relevant. In contrast to this, 32% of respondents in Revet et al. (2020) reported no change in psychopathology (but only 1% in Revet et al., 2021). Similarly, McGuire et al. (2021) did not find significant differences in a pre-COVID-19, and a COVID-19 period sample concerning relapse rates. Such differences might be due to patients' reluctance to seek help during the pandemic, the decreased access to services, and different pandemic periods of the studies (see Fig. 2).
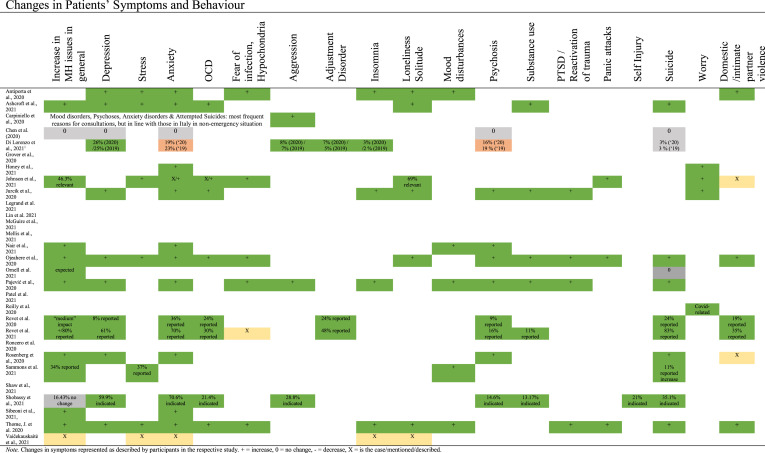
To varying degrees increases were reported in anxiety (n studies = 12, see Table 3 ) and worry about the future (n = 4), hypochondria, obsessions, or fear about contamination (n = 4). For instance, 70.6% of respondents in Shobassy et al. (2021) indicated experiencing more anxiety due to the pandemic. Increases were also reported for depression (n = 10), suicidality (n = 9), OCD (n = 8), psychosis, paranoia and delusional beliefs (n = 8), isolation, or loneliness (n = 7), substance use (n = 6), general stress (n = 6), and sleep disturbances (n = 5). Furthermore, surges were reported for aggressivity (n = 4), reactivation of trauma or PTS symptoms (n = 4), adjustment disorder (n = 3), and panic attacks (n = 3). Furthermore, several studies reported elevated levels of domestic violence (n = 5). At the same time, some articles reported on patients being resilient and stoic (Jurcik et al., 2020; Sibeoni et al., 2021), showing great responsibility for themselves and others (Pajević et al., 2020) and experiencing less stress, for instance due to restrictions on social interaction (Jurcik et al., 2020).
Table 3.
Changes in patients’ symptoms and Behaviour.
3.1.9. Impacts on staff and team
The pandemic also impacted the MH of staff in MHS. Many professionals were worried for their patients, themselves and their families, reported loneliness and sadness about the pandemic's consequences (Shaw et al., 2021; Sibeoni et al., 2021). The potential of burnout or mental health problems was described in several studies (n studies = 7). On the other hand, Revet et al. (2020) reported a good MH condition of staff and the implementation of strategies to reduce staff stress, such as home office. By May/June 2020, 61.8% of MHP in the USA surveyed by Lin et al. (2021) worked only from home. Home office was cited as a main reason for a disrupted work-life balance, as it blurred the boundaries between private and professional life (Vaičekauskaitė et al., 2021). Some reported difficulties of working without the presence of their team and feeling isolated in their clinical work (Sibeoni et al., 2021). Furthermore, remote clinical work was described as more emotionally tiring and intense (Vaičekauskaitė et al., 2021).
In some places, a shortage of staff was reported already before the pandemic (Ojeahere et al., 2020), which was now worsened as professionals got infected, were quarantined, or transferred to other parts of the health system (Rosenberg et al., 2020; Thome et al., 2020). For instance, Carpiniello et al. (2020) found that 66.2% of community MHS indicated staff members in quarantine, and 52% reported COVID cases for staff and patients. 55.6% of participants in RFs described that they were not able to have as much contact as usual with residents due to staff shortages (Johnson et al., 2021). Even when staff infection rates remained low, COVID-19 had effects on professionals, for instance with 52% reporting infections and 9% deaths of family, colleagues or friends (Sammons et al., 2021). Not surprisingly, some professionals were suffering from a fear of contracting COVID-19 (n = 5) with 91.5% of MHP in Italy having concerns about their personal safety (Carpiniello et al., 2020).
Poor finances, that had impacted MHS before the pandemic already, were now jeopardizing even more (Antiporta and Bruni, 2020; Nair et al., 2021; Ojeahere et al., 2020; Thome et al., 2020). In India, the reduction of monthly income of psychiatrists was 69.8%, while, at the same time one-third of MHP provided services free of charge (Grover et al., 2020). Sibeoni et al. (2021) also found that some MHP stopped charging their patients as they felt their work were no real consultations anymore.
Related to the variation in demands for MHS, reports on changing work- and caseloads per service varied (see Table 2). Johnson et al. (2021) identified a particularly high reported stress and workload for managers and lead clinicians and Vaičekauskaitė et al. (2021) found that in Lithuania the number of (irregular) working hours augmented. Some studies reported lower caseloads (n studies = 7). For instance, Reilly et al. (2020) found that MHP had significantly fewer patients weekly in late March/early April 2020 compared to before the pandemic. In Revet et al. (2020), 88% of child and adolescent psychiatrists saw a substantial drop in the daily number of occupied inpatient beds (≈1/3 reduction) and of outpatients (≈2/3 reduction). On the other hand, there were reports on increases of caseloads (n studies = 10). For instance, a survey with European MH experts (Thome et al., 2020) identified that these were treating an increased number of patients and additionally providing psychological support for healthcare workers. Similar to the pattern in demand, a tendency became apparent across studies showing a decrease in caseload at the beginning of the pandemic, followed by an increasing caseload. For instance, whilst in September 2020, 35% of US respondents had reported a decreased caseload, in June 2021, 52% described an increased caseload (Sammons et al., 2021).
The pandemic made constant adjustments by professionals necessary (Grover et al., 2020; Johnson et al., 2021; Nair et al., 2021; Sibeoni et al., 20021). An often-mentioned issue were the uncertainty and the rapid changes in guidelines which turned planning difficult. In some MHS, the number of meetings increased to handle the crisis, which led to concerns about not having time to provide adequate clinical work (Revet et al., 2020). MHP also assumed new tasks, such as addressing myths about the pandemic, providing resources, crisis care or nonclinical support groups (Grover et al., 2020; Nair et al., 2021; Reilly et al., 2020). Positive team and staff changes included new creative “research collaborations” and “waves of solidarity”, among colleagues and between professionals and patients (Sibeoni et al., 2021), teams showing flexibility and adaptability (Revet et al., 2021) and MHP learning new skills (Jurcik et al., 2020; Shaw et al., 2021), such as developing TP competences.
4. Discussion
This review aimed at synthesising the impacts of the COVID-19 pandemic on MHS worldwide. In 29 primary studies, major effects of the pandemic were described. The findings show that globally MHS have been compromised at a time when they were likely required the most. Societal measures, introduced to protect populations from the spread of the virus, caused confusion, uncertainty and disruptions in a sector which normally forms a pillar for some of the most vulnerable members of our society.
As stated before, the level and type of impact of the pandemic on MHS may have differed due to various factors. The various phases of the pandemic and times in which the studies were conducted (see Fig. 2) must be taken into consideration: For instance, Sammons et al. (2021) describe the transition to a hybrid model of care, echoing a crisis as opportunity finding (Brecher and Yehuda, 1985). This might reflect that the study was conducted in June 2021 – a later phase of the pandemic in which MHS had over a year to adjust already. In comparison, Thome et al. (2020) conducted their study in April 2020, at the beginning of the pandemic, and their results demonstrate a chaotic emergency situation characterised by anxiety and uncertainty.
Similarly, the COVID-19 rates at the time of investigation and at the geographic location (see Fig. 3) of the study may have been a decisive factor for the results. It is likely that in moments and locations of higher COVID-19 rates and, thus, more pressure on the healthcare systems, changes such as the transformation of units to emergency COVID-19 units happened. At the same, during the times with highest rates and most restrictive measure, patients’ service demands, and use are likely to have gone down (Tromans et al., 2020). For instance, regarding demand for MHS, access, referral and admission rates and caseloads, the findings of this review seem contradictory at first, but can be understood considering the different phases of the pandemic. A pattern emerged in which all types of numbers (demand, access, referral, admission, caseload) seem to have dropped at the beginning of the pandemic and then risen to normal levels and above. The first drop can be explained by the partial closure of services, inpatient services emptying their units, MHS restricting admission and introducing access protocols, such as COVID-testing and waitlists (Tromans et al., 2020). The numbers are also influenced by changes in patient behaviour (e.g., worry about infection at services), and the transition to TP. However, when COVID-19 case rates dropped in a specific country, MHS adopted and lessened their restrictions, which led to caseloads rising to again. However, as the primary studies often included various time periods and various locations and did not report on COVID-19 rates, the direct effects cannot be disentangled here. Future research will need to assess and compare the numbers retrospectively taking into consideration specific settings and pandemic phases.
Furthermore, a substantial factor relates to the various healthcare systems in place across countries which vary in scope and availability of MHS and in their form of organisation from community-based services to psychiatric hospital-based care (Thornicroft et al., 2016). While community services were among those MHS most affected by the pandemic, the findings of this review point to benefits that a more community-oriented MH system (Antiporta and Bruni, 2020; Ojeahere et al., 2020) might entail in times of crisis. These services have been shown to be able to react more adaptably and flexible to new situations and can better guarantee low-threshold access (Duden et al., 2022; Xiang et al., 2020). The risk of infection with COVID-19 was considered lower across many community and outpatient services compared to residential and accommodation settings (Rosenberg et al., 2020). Similarly, care at home provides a good alternative when psychiatric hospital spaces decrease as they become transformed into units to care for COVID-19 patients. Globally, community care is still not a priority in MHS with the majority of countries allocating no more than 20% to these services (WHO, 2021). Indeed, the present review, as well as the WHO report found outpatient and community services to be particularly highly affected by the pandemic (WHO, 2021), which led to a situation where discharged patients could not be referred to any outpatient MHS. This points to the urgent need to expand community services and care at home in order to decrease existing MH gaps.
The lack of preparedness of the MH systems found in this review and evident in closures and disruptions of MHS particularly in the early phases of the pandemic was confirmed recently by the WHO report which found that in just 7% of investigated countries all services were fully operational, while 93% of countries reported some disruption to their MHS (WHO, 2021).This report provides the first global data showing the detrimental effects of COVID-19 on access to MHS and highlights the need to increase funding and support of this sector (WHO, 2021). The present review further indicates that MHS had difficulties to put regulations and guidelines into practise, due to missing resources, safety equipment, lack of space and staff or funding issues, but also caused by confusing and ever-changing protocols. Even though unprecedented in its global dimension and the extent of its impact, there have been other crises around the world before with major effects for healthcare systems. For instance, the Ebola virus disease resulted in impaired provision of healthcare (Heymann et al., 2015) and particularly of mental healthcare (Vivalya et al., 2022), while at the same time increasing the need for adequate responses of MHS. Emergency situations such as Ebola and COVID-19 cause an exacerbated burden on MHS staff, increased work-related pressures and psychological strain on healthcare workers. This may have lasting negative consequences for individuals and national healthcare: acute conditions developed in response to stress can become chronic and entail physiological comorbidities (Duric et al., 2016). Rising sickness absence rates and resigning staff may be a consequence that would further aggravate staff shortage and worsen working conditions for the remaining staff. Taken together with the increased exhaustion among MHS staff this may lead to a decreasing quality of patient care (Phillips, 2020; Weibelzahl et al., 2021).
Apart from MHS disruptions, the present review identified a global transition to telepsychiatry as most reported change to MHS (Reay et al., 2020). Organisational studies show that innovation and change does not emerge from applying prescriptive knowledge, but rather from the acquisition of new organisational capabilities (Rochet et al., 2008) – the COVID-19 pandemic might represent the catalyst transforming the MH sector in a historical manner by stimulating a large-scale extension of telepsychiatry. Even though the earliest documentation of TP dates to 1956 (Stevens et al., 1999), since then there have been only minor developments in its use within psychological and psychiatric consultations (Chakrabarti, 2015). The exponential increase of TP since the start of the pandemic represents a historical marker of an eminent change in care in the development of mental health services. Even though not the primary focus of this review, most included studies discussed to some extent the benefits and disadvantages of TP. As the pandemic starts to appease, many services are keeping some of their digital offers, transitioning, as described by Sammons et al. (2021) to a hybrid model of care. Future research will need to investigate the possibilities and difficulties of this model of care. For instance, establishing therapeutic rapport at the beginning of a therapy might require at least some sort of face-to-face interaction, and TP might be particularly suited for people with less complex needs (Johnson et al., 2021; Shaw et al., 2021). One of the upcoming challenges will concern the establishment of regulations regarding virtual prescriptions to guarantee access to medication in times where face-to-face visits at doctors’ offices and hospitals become difficult or even dangerous. The pandemic has brought these issues forward to quite some extent. For instance, various regulations around the provision of telehealth have been waived in many countries, such as the US (Torous et al., 2020).
Moreover, staff needs to receive adequate training to attend virtually. However, this review, as well as others (e.g. Duden et al., 2022) showed that many professionals felt unprepared to shift to a virtual model of care – while at the same time experiencing major distributions in vocational training. Other studies have also found that the pandemic significantly impacted mental health education and training in general as well as clinical research (Byrne et al., 2021; Sparasci,et a., 2022). In the future vocational training should aim at bettering professionals’ preparedness to attend virtually. Furthermore, and particularly in future crises, it will be necessary to look at vocational training not as a bonus or add-on that can be omitted if the situation tightens, but as an essential module to maintain the overall service quality as well as the mental health of professionals.
Finally, the review indicates that the pandemic is leading to a higher MH burden on both – patients and professionals. Studies reported increases in symptoms in patients or expected surges in MH problems in the future. The constraints and consequences of the pandemic including social isolation and lack of routines, job losses, death of loved ones, school closure and parental distress, are likely to have major impacts on people already vulnerable to MH issues, particularly when combined with periods of no or limited access to MHS. There is an emerging body of evidence, pointing to the adverse impacts on the MH of the general population (Hossain et al., 2020; Rajkumar, 2020; Röhr et al., 2020), and of specific groups, such as people with pre-existing MH problems (Frank et al., 2020; Newby et al., 2020), or healthcare workers (Muller et al., 2020; Weibelzahl et al., 2021). The infection control measures leading to adaptations in MHS may have had detrimental effects on patients whose therapies were cancelled or reduced, or who were confined in inpatient facilities with reduced treatment offers and visitor restrictions (Moreno et al., 2020).
4.1. Methodological considerations
The findings of this review are limited by some aspects. The findings of the primary studies may have been very context-dependent and varied greatly in relation to the service(s) under investigation, the country of origin and its restrictive measures, the phase of pandemic and numbers of COVID-19 cases, as well as on the specific measurements used in the studies. For instance, the absence of a finding such as difficulties in access to prescriptions in a study, might not reflect the absence of the issue in practise, but rather be the result of the questions asked in the primary study. However, this review aimed to generalise across the increasing number of individual studies that are being carried out across the world, in order to help researchers and practitioners to see where we are at right now – two years after the start of the pandemic – in terms of mental health care. As of now, the literature on the topic is still sparse and large scale and comparable studies are missing, so that our aggregation and generalisation across contexts seemed appropriate to obtain a bigger picture. Future studies will need to take the specific geographical context and pandemic phase into consideration. Thereby, it will be important to allocate resources to the investigation of whether terminologies in different contexts reflect the implementation and real nature of MHS as there may exist a nomenclature confusion across countries (Thornicroft et al., 2016). Secondly, critiques may relate to the review's exclusion of grey literature and inclusion of only peer-reviewed, published research. We can thus not rule out the possibility that the findings of the review are affected by publication bias. Finally, the selected studies are methodologically diverse, including qualitative, quantitative and mixed-methods studies and focus on diverse MHS. This makes the broad interpretations of the results only tentative. Combining descriptive statistics of such heterogeneous studies may be judged as not meaningful. Future studies will need to provide more comparable results (e.g., caseload rates, time-series analysis) and might quantitatively test the validity of the qualitatively obtained findings of the present review.
5. Conclusion
As of April 2022, there are still many ongoing investigations on the effects of the COVID-19 pandemic on people, systems, and services. The current review found that most studies in the field of MH focus on changes to MH conditions in the general population, as well as on evaluations of telepsychiatry. The studies that are being undertaken to look at the impacts of the pandemic on MHS show a diverse picture, marked by large disruptions, shortages of staff, equipment and of guidance, transitions to a virtual or hybrid model of care, as well as expected or already occurring increases in caseloads due to intensification of MH problems. In the near future, efforts will be necessary to help the helpers, i.e., to assist staff working in MHS for instance by increased guidance from managers, supervision and spaces to unwind in order to lessen staff burden and prevent burnout. MHS need to find specific attention in pandemic regulations as their role in helping some of the most vulnerable groups to endure such a time of crisis cannot be underestimated.
Grant support
This research was funded by MPR.00.00019.20/Fördernetzwerk Interdisziplinäre Sozialpolitikforschung (Bundeministerium für Arbeit und Soziales).
Declaration of competing interest
The authors declare that they have no known conflict interest and no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Articles included in the systematic review.
- Adorjan K., Pogarell O., Pröbstl L., Rüb M., Wiegand H.F., Tüscher O., et al. Auswirkungen der COVID-19-Pandemie auf die Versorgungssituation in psychiatrischen Kliniken in Deutschland. Nervenarzt. 2021;1–8 doi: 10.1007/s00115-021-01129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso J., Liu Z., Evans‐Lacko S., Sadikova E., Sampson N., Chatterji S., et al. Treatment gap for anxiety disorders is global: results of the World Mental Health Surveys in 21 countries. Depress. Anxiety. 2018;35(3):195–208. doi: 10.1002/da.22711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antiporta D.A., Bruni A. vol. 44. Revista Panamericana De Salud Pública; 2020. (Emerging Mental Health Challenges, Strategies, and Opportunities in the Context of the COVID-19 Pandemic: Perspectives from South American Decision-Makers). ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association APA dictionary of psychology. 2022. https://dictionary.apa.org/mental-health-services Available at.
- Ashcroft R., Donnelly C., Dancey M., Gill S., Lam S., Kourgiantakis T., Adamson K., Verrilli D., Dolovich L., Kirvan A., others Primary care teams' experiences of delivering mental health care during the COVID-19 pandemic: a qualitative study. BMC Fam. Pract. 2021;22:1–12. doi: 10.1186/s12875-021-01496-8. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A., Steinbach J., Schweda A., Beckord J., Hetkamp M., Weismüller B., et al. Mental health burden of the CoViD-19 outbreak in Germany: predictors of mental health impairment. Journal Primary Care & Community Health. 2020;11:1–8. doi: 10.1177/2150132720953682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojdani E., Rajagopalan A., Chen A., Gearin P., Olcott W., Shankar V., et al. COVID-19 pandemic: impact on psychiatric care in the United States, a review. Psychiatr. Res. 2020;289 doi: 10.1016/j.psychres.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brecher M., Yehuda H.B. System and crisis in international politics. Rev. Int. Stud. 1985;11(1):17–36. [Google Scholar]
- Byrne A., Barber R., Lim C.H. Impact of the COVID‐19 pandemic–a mental health service perspective. Prog. Neurol. Psychiatr. 2021;25(2):27–33b. [Google Scholar]
- Carpiniello B., Tusconi M., Zanalda E., Di Sciascio G., Di Giannantonio M. Psychiatry during the Covid-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatr. 2020;20:1–12. doi: 10.1186/s12888-020-02997-z. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J. Psychiatr. 2015;5(3):286. doi: 10.5498/wjp.v5.i3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Jones P.B., Underwood B.R., Moore A., Bullmore E.T., Banerjee S., Osimo E.F., Deakin J.B., Hatfield C.F., Thompson F.J., others The early impact of COVID-19 on mental health and community physical health services and their patients' mortality in Cambridgeshire and Peterborough. UK. J. Psych. Res. 2020;131:244–254. doi: 10.1016/j.jpsychires.2020.09.020. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer E.G. Sage; Thousand Oaks, CA: 2018. An Introduction to Fully Integrated Mixed Methods Research. [Google Scholar]
- Di Lorenzo R., Fiore G., Bruno A., Pinelli M., Bertani D., Falcone P., Marrama D., Starace F., Ferri P. Urgent psychiatric consultations at mental health center during COVID-19 pandemic: retrospective observational study. Psychiatr. Q. 2021:1–19. doi: 10.1007/s11126-021-09907-w. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duden G.S., Gersdorf S., Trautmann K., Steinhart I., Riedel-Heller S., Stengler K. LeiP#netz 2.0: mapping COVID-19-related changes in mental healthcare services in the German city of Leipzig. Soc. Psychiatr. Psychiatr. Epidemiol. 2022 doi: 10.1007/s00127-022-02274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duric V., Clayton S., Leong M.L., Yuan L.L. 2016. Comorbidity Factors and Brain Mechanisms Linking Chronic Stress and Systemic Illness. (Neural plasticity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Lacko S., Aguilar-Gaxiola S., Al-Hamzawi A., Alonso J., Benjet C., Bruffaerts R., et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol. Med. 2018;48(9):1560–1571. doi: 10.1017/S0033291717003336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasshauer J.M., Bollmann A., Hohenstein S., Mouratis K., Hindricks G., Meier-Hellmann A., et al. Impact of COVID-19 pandemic on involuntary and urgent inpatient admissions for psychiatric disorders in a German-wide hospital network. J. Psychiatr. Res. 2021;142:140–143. doi: 10.1016/j.jpsychires.2021.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasshauer J.M., Bollmann A., Hohenstein S., Hindricks G., Meier-Hellmann A., Kuhlen R., et al. Emergency hospital admissions for psychiatric disorders in a German-wide hospital network during the COVID-19 outbreak. Soc. Psychiatr. Psychiatr. Epidemiol. 2021;56:1469–1475. doi: 10.1007/s00127-021-02091-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasshauer J.M., Schomerus G., Stengler K. COVID-19-Pandemie und Versorgung schwer psychisch erkrankter Menschen – inwieweit wurden die Interessen psychisch erkrankter Menschen in den Schutzverordnungen des Bundes und der Länder berücksichtigt? Psychiatr. Prax. 2021;48:1–7. doi: 10.1055/a-1353-1774. [DOI] [PubMed] [Google Scholar]
- Frank A., Hörmann S., Krombach J., et al. Psychisch krank in Krisenzeiten: subjektive Belastungen durch COVID-19. Psychiatr. Prax. 2020;47:267–272. doi: 10.1055/a-1179-4230. [DOI] [PubMed] [Google Scholar]
- Grover S., Mehra A., Sahoo S., Avasthi A., Tripathi A., D'Souza A., Saha G., Jagadhisha A., Gowda M., Vaishnav M., others Impact of COVID-19 pandemic and lockdown on the state of mental health services in the private sector in India. Indian J. Psychiatr. 2020;62:488. doi: 10.4103/psychiatry.IndianJPsychiatry_568_20. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann D.L., Chen L., Takemi K., Fidler D.P., Tappero J.W., Thomas M.J., et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet. 2015;385(9980):1884–1901. doi: 10.1016/S0140-6736(15)60858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honey A., Waks S., Hines M., Glover H., Hancock N., Hamilton D., Smith-Merry J. COVID-19 and psychosocial support services: experiences of people living with enduring mental health conditions. Community Ment. Health J. 2021;57:1255–1266. doi: 10.1007/s10597-021-00871-0. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L., et al. Epidemiology of mental health problems in COVID-19: a review. F1000Research. 2020:9. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter-Agency Standing Committee IASC . Mental Health and Psychosocial Support in Ebola Virus Disease Outbreaks: A Guide for Public Health Programme Planners. IASC; Geneva: 2015. Reference group on mental health and psychosocial support in emergency settings. [Google Scholar]
- Johnson S., Dalton-Locke C., San Juan N.V., Foye U., Oram S., Papamichail A., Landau S., Olive R.R., Jeynes T., Shah P., others Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff. Soc. Psychiatr. Psychiatr. Epidemiol. 2021;56:25–37. doi: 10.1007/s00127-020-01927-4. (*) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurcik T., Jarvis G.E., Zeleskov Doric J., Krasavtseva Y., Yaltonskaya A., Ogiwara K., Sasaki J., Dubois S., Grigoryan K. Adapting mental health services to the COVID-19 pandemic: reflections from professionals in four countries. Counsell. Psychol. Q. 2020:1–27. ∗. [Google Scholar]
- Kmet L.M., Cook L.S., Lee R.C. Alberta Heritage Foundation for Medical Research; 2004. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. [Google Scholar]
- Legrand G., Boisgard C., Canac B., Cardinaud Z., Gorla M.G., Gregoire E., Jamon C., Oussal T., Vaury P. Organisation and timeline of measures in French psychiatric establishments during the first wave of the COVID-19 epidemic. EvOlu’Psy study. BMC Psychiatry. 2021;21:1–17. doi: 10.1186/s12888-021-03293-0. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin T., Stone S.J., Anderson T. Treating from Afar: mental health providers' challenges and concerns during the COVID-19 pandemic. Behav. Med. 2021;1:4. doi: 10.1080/08964289.2021.1908217. ∗. [DOI] [PubMed] [Google Scholar]
- McGuire A.B., Flanagan M.E., Kukla M., Rollins A.L., Myers L.J., Bass E., Garabrant J.M., Salyers M.P. Inpatient mental healthcare before and during the COVID-19 pandemic. Healthcare. 2021;9:1613. doi: 10.3390/healthcare9121613. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellis A.M., Potenza M.N., Hulsey J.N. COVID-19-related treatment service disruptions among people with single-and polysubstance use concerns. J. Subst. Abuse Treat. 2021:121. doi: 10.1016/j.jsat.2020.108180. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatr. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatr. Res. 2020 Nov;293 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair S., Kannan P., Mehta K., Raju A., Mathew J., Ramachandran P. The COVID-19 pandemic and its impact on mental health services: the provider perspective. J. Publ. Health. 2021;43:ii51–ii56. doi: 10.1093/pubmed/fdab163. ∗. [DOI] [PubMed] [Google Scholar]
- Newby J.M., O'Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One. 2020;15 doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojeahere M.I., de Filippis R., Ransing R., Karaliuniene R., Ullah I., Bytyçi D.G., Abbass Z., Kilic O., Nahidi M., Hayatudeen N., others Management of psychiatric conditions and delirium during the COVID-19 pandemic across continents: lessons learned and recommendations. Brain, Behavior, & Immunity-Health. 2020;9 doi: 10.1016/j.bbih.2020.100147. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Borelli W.V., Benzano D., Schuch J.B., Moura H.F., Sordi A.O., Kessler F.H.P., Scherer J.N., von Diemen L. The Lancet Regional Health-Americas; 2021. The Next Pandemic: Impact of COVID-19 in Mental Healthcare Assistance in a Nationwide Epidemiological Study. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajević I., Hasanović M., Avdibegović E., Džubur-Kulenović A., Burgić-Radmanović M., Babić D., Mehić-Basara N., Zivlak-Radulović N., Račetović G. Organization of mental healthcare in Bosnia and Herzegovina during coronavirus disease 2019 pandemic. Indian J. Psychiatr. 2020;62:S479. doi: 10.4103/psychiatry.IndianJPsychiatry_1044_20. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel R., Irving J., Brinn A., Broadbent M., Shetty H., Pritchard M., Downs J., Stewart R., Harland R., McGuire P. Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-046365. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips C. Relationships between workload perception, burnout, and intent to leave among medical–surgical nurses. JBI Evidence Implementation. 2020;18(2):265–273. doi: 10.1097/XEB.0000000000000220. [DOI] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N., Roen K., Duffy S., others Guidance on the conduct of narrative synthesis in systematic reviews. A Product from the ESRC Methods Programme Version. 2006;1:b92. [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psych. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly S.E., Zane K.L., McCuddy W.T., Soulliard Z.A., Scarisbrick D.M., Miller L.E., Mahoney J.J., Iii Mental health practitioners' immediate practical response during the COVID-19 pandemic: observational questionnaire study. JMIR Mental Health. 2020;7 doi: 10.2196/21237. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reay R.E., Looi J.C., Keightley P. Telehealth mental health services during COVID-19: summary of evidence and clinical practice. Australas. Psychiatr. 2020;28:514–516. doi: 10.1177/1039856220943032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revet A., Hebebrand J., Anagnostopoulos D., Kehoe L.A., Gradl-Dietsch G., Klauser P. Perceived impact of the COVID-19 pandemic on child and adolescent psychiatric services after 1 year (February/March 2021): ESCAP CovCAP survey. Eur. Child Adolesc. Psychiatr. 2021:1–8. doi: 10.1007/s00787-021-01851-1. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revet A., Hebebrand J., Anagnostopoulos D., Kehoe L.A., Klauser P. ESCAP CovCAP survey of heads of academic departments to assess the perceived initial (April/May 2020) impact of the COVID-19 pandemic on child and adolescent psychiatry services. Eur. Child Adolesc. Psychiatr. 2020:1–10. doi: 10.1007/s00787-020-01699-x. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochet C., Keramidas O., Bout L. Crisis as change strategy in public organizations. Int. Rev. Adm. Sci. 2008;74(1):65–77. [Google Scholar]
- Röhr S., Müller F., Jung F., et al. Psychosoziale Folgen von Quarantänemaßnahmen bei schwerwiegenden Coronavirus-Ausbrüchen: ein Rapid Review. Psychiatr. Prax. 2020;47:179–189. doi: 10.1055/a-1159-5562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncero C., García-Ullán L., Javier I., Martín C., Andrés P., Ojeda A., González-Parra D., Pérez J., Fombellida C., Álvarez-Navares A., others The response of the mental health network of the Salamanca area to the COVID-19 pandemic: the role of the telemedicine. Psychiatr. Res. 2020;291 doi: 10.1016/j.psychres.2020.113252. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg S., Mendoza J., Tabatabaei-Jafari H., Network T.P.-M.H.I., Salvador-Carulla L. International experiences of the active period of COVID-19-Mental health care. Heal. Pol. Technol. 2020;9:503–509. doi: 10.1016/j.hlpt.2020.08.016. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roudini J., Khankeh H.R., Witruk E. Disaster mental health preparedness in the community: a systematic review study. Health psychology open. 2017;4(1) doi: 10.1177/2055102917711307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sammons M.T., Elchert D.M., Martin J.N. Mental health service provision during COVID-19: results of the third survey of licensed psychologists. J. Health Soc. Pol. 2021;47:119–127. doi: 10.1007/s42843-021-00044-3. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw H., Robertson S., Ranceva N. What was the impact of a global pandemic (COVID-19) lockdown period on experiences within an eating disorder service? A service evaluation of the views of patients, parents/carers and staff. Journal of Eating Disorders. 2021;9:1–11. doi: 10.1186/s40337-021-00368-x. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shobassy A., Nordsletten A., Ali A., Bozada K., Malas N., Hong V. Effects of the COVID-19 pandemic in a psychiatric emergency service: utilization patterns and patient perceptions. Am. J. Emerg. Med. 2021;52:241–243. doi: 10.1016/j.ajem.2021.03.082. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibeoni J., Manolios E., Costa-Drolon E., Meunier J.-P., Verneuil L., Revah-Levy A. Clinical practice during the COVID-19 pandemic: a qualitative study among child and adolescent psychiatrists across the world. Child Adolesc. Psychiatr. Ment. Health. 2021;15:1–15. doi: 10.1186/s13034-021-00417-y. ∗. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparasci O., Bhui K., Biswas A., Chamberlain S., Dubicka B., Dudas R., et al. Impact of COVID-19 on mental health research: is this the breaking point? Br. J. Psychiatr. 2022;220(5):254–256. doi: 10.1192/bjp.2022.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens A., Doidge N., Goldbloom D., Voore P., Farewell J. Pilot study of televideo psychiatric assessments in an underserviced community. Am. J. Psychiatr. 1999;156:783–785. doi: 10.1176/ajp.156.5.783. [DOI] [PubMed] [Google Scholar]
- Thome J., Coogan A.N., Fischer M., Tucha O., Faltraco F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatr. Clin. Neurosci. 2020;74:406–415. doi: 10.1111/pcn.13019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thome J., Deloyer J., Coogan A.N., Bailey-Rodriguez D., da Cruz E Silva O.A., Faltraco F., Grima C., Gudjonsson S.O., Hanon C., Hollỳ M. The impact of the early phase of the COVID-19 pandemic on mental-health services in Europe. World J. Biol. Psychiatr. 2020:1–10. doi: 10.1080/15622975.2020.1844290. ∗. [DOI] [PubMed] [Google Scholar]
- Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G., Deb T., Henderson C. Community mental health care worldwide: current status and further developments. World Psychiatr. 2016;15(3):276–286. doi: 10.1002/wps.20349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Myrick K.J., Rauseo-Ricupero N., Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment. Heal. 2020;7(3) doi: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromans S., Chester V., Harrison H., Pankhania P., Booth H., Chakraborty N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych open. 2020;6(6) doi: 10.1192/bjo.2020.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaičekauskaitė R., Babarskienė J., Grubliauskienė J. Mental health services during the pandemic: the experiences of Lithuanian psychologists. Sabiedrı̄ba. Integrācija. Izglı̄tı̄ba: starptautiskās Zinātniskās Konferences Materiāli: 2021. Gada 28.-29. Maijs. 2021;7:217–229. ∗. [Google Scholar]
- Vivalya B.M.N., Vagheni M.M., Kitoko G.M.B., Vutegha J.M., Kalume A.K., Piripiri A.L., et al. Developing mental health services during and in the aftermath of the Ebola virus disease outbreak in armed conflict settings: a scoping review. Glob. Health. 2022;18(1):1–6. doi: 10.1186/s12992-022-00862-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weibelzahl S., Reiter J., Duden G.S. Depression and anxiety in healthcare professionals during the COVID-19 pandemic. Epidemiol. Infect. 2021;149 doi: 10.1017/S0950268821000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2005. WHO Global Influenza Preparedness Plan: the Role of WHO and Recommendations for National Measures before and during Pandemics.https://apps.who.int/iris/handle/10665/68998 [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2021. Mental Health Atlas 2020. [Google Scholar]
- Xiang Y.-T., Zhao Y.-J., Liu Z.-H., Li X.-H., Zhao N., Cheung T., Ng C.H. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int. J. Biol. Sci. 2020;16:1741. doi: 10.7150/ijbs.45072. [DOI] [PMC free article] [PubMed] [Google Scholar]