Abstract
Introduction
Post covid-19 syndrome or Long Covid has been estimated to impact 1.3 million individuals in the UK. This study evaluates the outcomes of delivering a complementary Long Covid support service using psycho-educational and mind-body approaches within a community setting.
Methods
This study utilised quantitative methods to evaluate the outcomes of implementing a complementary approach to providing Long Covid support. The service offered a package of care including group sessions combining psychoeducation and mind-body complementary approaches and optional 1:2:1 sessions (physiotherapy and craniosacral therapy (CST)). Screening for the service and health information was obtained using the Covid-19-Yorkshire Rehabilitation Screening tool (C-19 YRS). The impact of the service was assessed using the patient reported outcome measure: Warwick Holistic Health Questionnaire (WHHQ-18), and a survey was designed for general evaluation and feedback about the service from participants.
Results
25 participants engaged with the service. The C-19YRS proved to be a useful tool to screen service users. The WHHQ-18 highlighted a positive group change (n = 16) in participants’ mental, physical, emotional, and spiritual wellbeing: mean group score at the start = 33.7 (SD=12.5), mean group score at the follow up = 39.5 (SD=10.8). In the feedback from the service evaluation, participants reported that the service was useful in supporting them with their health challenges resulting from Long Covid and was delivered to the standard expected.
Conclusion
In conclusion the psycho-educational and mind-body complementary approaches used within this service were well received and the measures used to evaluate were suitable for a service delivered within a community setting.
Keywords: Long covid, Psychoeducation, Complementary and integrative healthcare, Community setting, Service evaluation
1. Introduction
“According to the World Health Organisation “Long Covid or post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms and that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.
”.. At this time, it is unclear what triggers the development of Long Covid amongst those infected with SARS-CoV-2, the virus responsible for causing Coronavirus disease 2019 (COVID-19). It appears that the severity of the initial infection does not change upon the development of Long Covid. Over 200 symptoms have been reported, however, fatigue, shortness of breath and loss of smell are most prevalent [1]. Other commonly reported symptoms include chest pain, difficulty concentrating (‘brain fog’) headaches, muscle pains, gastrointestinal disturbance, rashes and depression [2]. Long Covid is an emerging phenomenon, it is not yet fully understood and as a result there are inconsistencies within data reporting and the literature.
The implications of Long Covid for individuals and society at large are slowly becoming clear [3]. According to the Office for National Statistics [1] 1.3 million people in the UK have self-reported persistent symptoms for more than 4 weeks and it is yet unclear how many of those continue to have symptoms beyond 12 weeks as defined by the WHO. Accessing services or support via usual means has become a challenge [4]. At the time of writing, there was no Long Covid support service available via the National Health Service (the publicly funded healthcare system in the UK) in the locality of this community setting. The delivery of this service was enabled and helped via voluntary sector funding.
This study reports on the evaluation of delivering a complementary and integrative Long Covid support group using psycho-educational and mind-body approaches within a community setting. Considerations were given on how to maximise engagement and accurately evaluate the impact of the interventions and the overall project outcomes are reported.
As this community project was started whilst the pandemic was unfolding, the delivery was done on an ad-hoc basis initially and guided to some extent by COVID-19 restrictions and protocols. Transport was made available to participants that could not access the project by any other means or were unable to concentrate long enough due to fatigue.
2. Study design
2.1. Methodology
2.1.1. Psychoeducation & mind-body interventions
World Health Organisation Road to Recovery guidance was used as a basis for the programme [3]. Participants were offered a package of care comprising of group sessions and optional 1:2:1 session of physiotherapy or Craniosacral Therapy (CST) [5].
2.1.2. Physiotherapy
Participants were offered 1:2:1 sessions of Physiotherapy to address strength, balance, endurance, and co-ordination, a combination of strength work to help restore muscle tone and joint support was combined with balance and coordination. All of which can be affected by fatigue and lethargy. Rehabilitation was therefore chosen to reflect this and was guided by recommendation from the Chartered Society of Physiotherapy [6]. Each session was up to 45 min in length. Each session consisted of advice on graded exercise and pacing alongside physical activity. Each session was adapted to the individual need.
2.1.3. Craniosacral therapy
Craniosacral Therapy (CST) is a hands-on mind-body modality that has its origin in Osteopathy [7] and has been reported to support positive outcomes in the areas of physical, mental, social relational and spiritual wellbeing [8]. CST has also been used with patients who have long term conditions such as chronic lower back pain [9] and fibromyalgia [9], [10], [11].
2.1.4. 4-week programme
The first programme was designed to run over a 4-week period and focused on four key areas of Long Covid symptoms (see table 1 ). The World Health Organisation document [3] named 12 areas of focus for supporting the recovery of those experiencing Long Covid symptoms. To develop a comprehensive Long Covid programme, and to meet the needs of such variable symptoms, the Support for Rehabilitation advice document was used as a template and transferred from theory into practice based on practitioner skill and service user need. The twelve recovery steps were grouped together into four larger topic areas for practical delivery to suit the timescale. The emergent themes of the document such as exercise, brain fog and memory, nutrition and mindfulness were used as the four core session titles. Each week, one core theme was addressed and presented using a mix of practical and educational group sessions. Group sizes were kept to no more than ten to aid discussion and to build rapport but to avoid feeling overwhelmed and inhibition. Facilitation of each session was led by experienced practitioners (NB & SA) and evolved in a fluid manner by participant need.
Table 1.
Content of each weekly session in the Long Covid ‘Road to Recovery’ 4-week programme.
| Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|
| Group discussion - experiences of Covid-19 & Long Covid | Memory | Qigong & Nutrition: Eating for immunity | Meditation, Mindfulness, Aromatherapy. Reflection and evaluation |
2.1.5. 6-week programme
The longer 6-week programme was developed (see table 2 ) in response to participant feedback from the 4-week group as reported on in the results section of this article. Sessions were designed so that they could easily be adapted to suit individual need, all participants were closely monitored throughout. The same format was used for this longer programme, facilitators took the lead and all participants engaged in both practical and educational discussion, reflecting on how Covid impacted their lives. The other 2 weeks enabled increased rapport, engagement, and reflection throughout.
Table 2.
Content of each weekly session in the Long Covid ‘Road to recovery’ 6-week programme.
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
|---|---|---|---|---|---|
| Group discussion - experiences of Covid-19 & Long Covid | Strength & Conditioning | Memory | Chair yoga | Nutrition: Eating for immunity | Meditation, Mindfulness, Aromatherapy. Reflection and evaluation |
Group participants were given a booklet which included information on the skills covered by the course, so that they could continue to implement skills at home in-between sessions and at the end of the course.
2.1.6. Aftercare
Participants who attended the final course sessions were given a resource pack, which included a scented candle, aromatherapy roll-on, mindfulness colouring book, inspirational cards, herbal tea bags and information leaflets about local services that could support their wellbeing.
Quantitative methods were used to evaluate the project outcomes of a complementary approach to Long Covid rehabilitation.
3. Methods
3.1. Ethics
As this was a service evaluation to evaluate the outcomes of this project ethical approval was not required or sought.
3.2. Recruitment
Recruitment into the project was carried out through posts on social media platforms (Torus Wellbeing Facebook and Linked-In pages), distribution of posters via social prescribing networks (also known as community referral networks, which enabling health professionals to refer people to a range of local, non-clinical services [12]), professional networks including consultants at Royal Stoke University Hospital Respiratory Department, National Health Service Community Physiotherapy Services, private physiotherapy practices and word of mouth.
3.3. Inclusion criteria
Inclusion was partly determined by the funding remit. To participate, each participant met the criteria stated:
-
•
Minimum of 15 years old with no upper age limit.
-
•
Participants were invited to join the project if they lived within the County of Staffordshire.
-
•
To have had COVID-19 and be struggling with after-effects
4. Exclusion criteria
-
•
Individuals with organ damage, or other related conditions.
-
•
Those awaiting a diagnosis of COVID-19.
-
•
Individuals under care of the CRISIS team (NHS UK CRISIS teams support people who might otherwise need to go to hospital), acute psychiatric services or are having regular psychiatric input for acute or escalating mental health concerns.
5. Delivery
Due to the timing of the project delivery various levels of support were available as the project started. In the first instance whilst lock down was in place, screening calls were made to assess the immediacy and discuss possible need. Clinical judgement and patient-need determined if four one-to-one sessions (of either physiotherapy with a registered Physiotherapist (SA) or craniosacral therapy (CST) sessions with registered practitioner (NB), CST is a hands-on mind-body complementary and integrative medicine approach [13] were given. Participants were also offered the opportunity to take part in the Long Covid support group: a programme of either four or six weekly sessions.
6. Data collection
Data was collected from participants depending on the level of engagement they had with the project. Name, address, contact details (telephone and or an email) were required as a minimum referral.
Five measures were used to gather data on this project.
-
•
An adapted version of COVID-19 Yorkshire Rehabilitation Screening (C19-YRS), developed by the Leeds, Airedale and Hull NHS Trusts, was used to assess and record symptoms and guide the Long Covid support provision for the participants [14]. Participants were asked to rate their functionality (both before and after having COVID-19) including breathlessness, throat & airways, ability to engage in everyday activities, fatigue, cognitive functioning, distress, anxiety, and depression. A screening call and completion of the adapted C-19-YRS followed by a first face-to-face assessment for some participants.
-
•
The Warwick Holistic Health Questionnaire (WHHQ-18) [15], a patient reported outcome measure that evaluates changes in physical, mental, emotional, spiritual and social wellbeing was implemented at the start of the first and last session of the 4-or 6-week versions of the programmes.
-
•
Blood pressure and 4) oxygen saturation was measured at the start of each session to monitor participants ability to take part in the movement sessions and to observe changes across the weekly sessions.
-
•
An evaluation form was developed to capture participants feedback using a combination of multiple choice and free text response options on the elements of the course and to help inform the team on the activities that best suited those with Long Covid (Appendix A). This was administered in the last session of the 4- and 6- week programmes.
7. Consent
All participants who took part in the project provided signed consent for photography, voice recording (for transcription, anonymization, and analysis), and the publication of anonymous outcomes and service evaluation data.
8. Data analysis
Demographic and categorical data from the C-19 YRS and the evaluation form were analysed, and descriptive statistics are presented as an arithmetic mean.
Comparative statistics were generated from the baseline WHHQ compared to the follow up WHHQ. The WHHQ is assessed based upon the change in score at an individual level - whether their score improved, remained the same, or declined.
Blood pressure and oxygen saturation assessment was analysed in situ by facilitators (SA & NB) to ensure that participants were fit to exercise. The data captured on the service evaluation form was scored and reviewed by the facilitators.
9. Results
Between May 2021 and December 2021, N = 46 participants self-referred into the project from four referral pathways (n = 30 hospital; n = 11 self-referrals; n = 1 GP; n = 4 NHS physiotherapy service). The clinical team tried to contact all participants referred into the project either via telephone or email. Of those who were contacted n = 25 engaged in some level of support see table 3 .
Table 3.
Attendance and level of support received.
| Attendance and Level of Support Received n = 25 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Participant ID | Initial Assessment | 1:2:1 Physio | 1:2:1 CST | 4-week programme Week 1 | 4-week programme Week 4 | 6-week programme Week 1 | 6-week programme Week 6 | |
| JP06 | * | |||||||
| TM02 | * | * | * | |||||
| KW05 | * | * | * | |||||
| JC03 | * | * | * | * | ||||
| AK43 | DNA | |||||||
| GG14 | * | * | ||||||
| MN25 | * | * | ||||||
| SB31 | * | |||||||
| AW26 | DNA | |||||||
| MS22 | * | * | ||||||
| LP27 | * | * | ||||||
| DP38 | * | * | ||||||
| SM28 | * | * | ||||||
| EH44 | * | * | ||||||
| LK45 | * | * | ||||||
| ET41 | * | * | ||||||
| BB42 | * | DNA | ||||||
| AG46 | * | DNA | ||||||
| GW21 | * | * | ||||||
| SH20 | DNA | DNA | ||||||
| AC23 | * | DNA | ||||||
| MW35 | * | * | ||||||
| SN13 | * | * | ||||||
| CG18 | * | DNA | ||||||
| MH04 | ⁎⁎ | |||||||
Key.
Attended.
Discharged as recovered. DNA (Registered for session but did not attend).
10. Participant characteristics
Of the n = 25, 7 were male, 15 were female and three did not disclose their gender. The group were predominantly white British n = 18, n = 1 Asian and white, n = 2 other white background, n = 1 Chinese and n = 3 was undisclosed ethnicity. The age range of participants was between 15 and 92 years. Table 4 shows a breakdown of participants ages.
Table 4.
Age range of participants.
| Age range | N = 25 |
|---|---|
| 15–24 years | n = 1 |
| 25–34 years | n = 5 |
| 35–54 years | n = 8 |
| 55–64 years | n = 7 |
| 65 years plus | n = 4 |
Transport was arranged (booked and paid for by the project) on behalf of n = 6 participants who attended weekly group sessions. N = 3 participants did not engage beyond the initial telephone conversation.
10.1. C-19 yrs screening tool data
The C-19 YRS screening tool data provided a health profile of the participants. Of N = 22 participants some had existing health conditions. These conditions included: Hypertension, Hypotension, Diabetes, Joint and Bone conditions (Osteoporosis, Arthritis), Chronic Obstructive Pulmonary Disease (COPD), Lung cancer, Asthma, Spinocerebellar ataxia (SCA), Recent surgery, Fibromyalgia, Multiple Sclerosis, Myalgic encephalomyelitis (ME), and Chronic pain.
N = 12 reported that they were admitted to hospital with COVID-19. Of those twelve participants admitted to hospital, an average of 7 days was spent in hospital, with a collective 92 days in hospital.
Participants self-rated the impact COVID-19 had on sixteen areas of their lives. Response options included yes/no and impact range: with 0 being no impact and 10 being extremely impactful (See tables 5 and 6 ).
Table 5.
C-19 YRS data: Average impact on 7 functions, before and after COVID-19 on a 0–10 scale.
| Function | Group average impact rating at time of completion | Group average impact rating pre-covid | Group average change |
|---|---|---|---|
| 1. Breathlessness | 4.33 | 1.67 | 1.67 |
| 2. Mobility | 5.00 | 1.00 | 3.00 |
| 3. Fatigue | 7.00 | 2.00 | 5.00 |
| 4. Usual activities | 6.00 | 1.00 | 4.00 |
| 5. Pain/discomfort | 5.00 | 2.00 | 3.00 |
| 6. Anxiety | 5.00 | 2.00 | 2.00 |
| 7. Depression | 4.00 | 2.00 | 1.00 |
Table 6.
C19 YRS data. The change of 5 functions after having COVID-19, and the impact this change has had on their lives.
| Function | Number of Yes responses: Have these functions changed since having covid? | Impact of the change +/- |
|---|---|---|
| 8.Laryngeal & airway complications | 11 | +3.00 |
| 9. Voice | 11 | +3.00 |
| 10.Swallowing | 8 | +2.00 |
| 11.Nutrition | 8 | +3.00 |
| 12. Personal Care | 11 | +3.00 |
Table 5: C-19 YRS data: Average impact on seven functions, before and after covid on a 0–10 scale.
Since contracting COVID-19 all participants (n = 22) reported that they had been impacted in the areas of 1) breathlessness, 2) mobility, 3) fatigue, 4) usual activities, 5) pain/discomfort, 6) anxiety, 7) depression.
10.2. Cognition
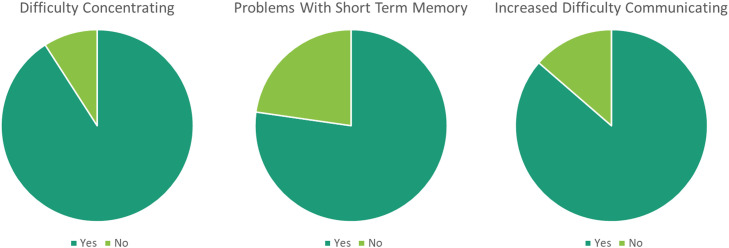
N = 22, participants were asked if they struggled with cognition and response options included Yes or No. If participants responded yes, more details were sought. a) n = 20 stated that they had difficulty concentrating, b) n = 17 stated that they had experienced new or worsened difficulty with their short-term memory, c) n = 19 participants stated that they had increased difficulty with communication (See Fig. 1 a.,1b.,1c.).
Fig. 1.
a: Difficulty concentrating
Fig. 1b: Difficulty with short term memory
Fig. 1c: Increased difficulty communicating.
Participants responded Yes or No to indicate if their function in five additional areas had changed since their COVID-19 diagnosis, shown in Table 6
Half (n = 11) of the participants reported changes that had a detrimental impact on the function of their 8) laryngeal & airway, 9) voice and ability to do their own 12) personal care. Thirty-six percent (n = 8) reported changes of detrimental impact in 10) swallowing and 11) nutrition.
10.3. Continence
18% of participants (n = 22), (n = 4) stated that they had new problems with bowel incontinence and 14% of participants (n = 3) stated that they had new issues with urinary incontinence, since developing covid-19 it was unclear whether this was due to stress incontinence secondary to respiratory symptoms or of other cause - this was beyond the remit of this study.
10.4. PTSD screen
n = 8 individuals stated that they had unwanted memories of COVID-19 or their hospital admission and rated their distress between mild and severe (n = 4 mild, n = 3 moderate, n = 1 severe). Secondly, n = 7 participants experienced unpleasant dreams about their illness or hospital admission and rated their distress between mild and severe (n = 4 mild, n = 2 moderate, n = 1 severe). Participants were asked about avoidance of thoughts and feelings related to COVID-19 and their hospital admission. n = 8 participants had tried to avoid these thoughts and feelings and rated their effort between mild and extreme (n = 1 mild, n = 5 moderate, n = 1 severe, n = 1 extreme).
10.5. Global health status
Participants were asked to self-report their health status when they registered. Response options included: very good, good, fair and poor. Sixty-four percent (n = 14) of participants self-reported that their health was fair at the start of the project. Nine percent (n = 2) reported that their health was poor. Fourteen percent (n = 3) reported their health to be good and the remaining fourteen percent (n = 3) that their health was very good.
10.5.1. Sessions
10.5.1.1. Physiotherapy
Two participants chose to attend the face-to-face physiotherapy sessions (n = 1 male, n = 1 female) each both had two sessions before attending the group. Sessions included simple functional activity such as sit to stand and step work for stair practice. It also included some balance work and coordination for core stability. In some individuals that had returned to a higher level of activity prior to attending the project, we introduced some light resistance work for the upper and lower limb. Heart rate and oxygen saturation were taken at the start and the finish of each session, each session was low intensity and plenty of breaks were taken between exercises. Participants were asked to monitor any aggravation of symptoms as it was important for us to avoid symptom exacerbation.
10.5.1.2. Craniosacral therapy
The individuals that were given CST were treated using a pragmatic approach depending on their needs. N = 6 participants were offered 4 × 1:2:1 sessions of CST, a potential 24 1-hour sessions. 16 1-hour sessions were delivered. Gender (n = 2 male, n = 4 female). n = 2 participants attended all the sessions available to them. n = 1 attended two out of four but did not attend the remainder, due to illness and not feeling well enough. n = 1 did not continue beyond initial session, as they did not feel the sessions were of benefit despite being pain free for the first time in years whilst on the table. n = 1 attended three out of four sessions but did not attend the final session. n = 1 attended 2 sessions and then chose to have physiotherapy as part of this service.
10.5.1.3. 4-week programme
N = 10 participants registered and n = 8 attended the initial and final week of the 4-week programme.
10.5.2. Blood pressure (BP) assessment
A normal blood pressure level is estimated between 90/60 and 120/80 mmHg (Whelton et al., 2017). BP readings for those participants that attended the weekly groups were recorded on arrival and can be seen in Table 7 .
Table 7.
Weekly blood pressure readings of participants attending the 4-week programme.
| Participant | Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|---|
| JC03 | 132/82* | 125/73* | 125/71* | 140/73⁎⁎ |
| MN25 | 108/76 | 105/77 | 115/77 | 117/76 |
| SB31 | 113/67 | 104/50 | 101/63 | 110/60 |
| LP27 | 133/86 | 118/80 | 129/76* | 137/88* |
| SM28 | Absent | 141/90⁎⁎ | 130/83* | 125/84* |
| GW21 | 180/90⁎⁎ | 167/72⁎⁎ | 143/75⁎⁎ | 135/61* |
| MP22 | 168/90⁎⁎ | 147/82⁎⁎ | 149/67⁎⁎ | 158/83⁎⁎ |
Key.
pre-high BP.
high BP.
10.5.3. Oxygen saturation (SATS) assessment
SATS were taken and recorded for all participants that attended weekly sessions and can be seen in Table 8 . A normal oxygen saturation is anywhere between 95 and 100% (Teo, 2020).
Table 8.
Weekly oxygen saturation readings of participants attending the 4-week programme.
| Participant | Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|---|
| JC03 | 99 | 98 | 97 | 99 |
| MN25 | 98 | – | 99 | 98 |
| SB31 | 97 | 97 | 99 | 99 |
| LP27 | 98 | 98 | 99 | 98 |
| SM28 | – | 98 | 88** | 95* |
| GW21 | 91* | 98 | – | 88⁎⁎ |
| MP22 | 95 | 95 | 98 | 98 |
Key.
Denotes those with SATS lower than normal range.
referral to specialist required.
10.5.4. Service evaluation 4-week programme
N = 7 participants gave feedback about the 4-week programme.
Participants in the 4-week programme scored the programme as an 12/16 or a percentage of 74%, based on factors such as content of sessions, session length, number of sessions, as well as if the programme met their expectations. Based on feedback it was identified that the Qigong session was the most enjoyed (n = 5) and that the memory session was the least enjoyed session (n = 2). Participants reported that the most favoured number of sessions for the programme was six. As a result of this feedback the team decided to extend the programme by 2 weeks to offer more opportunity for them to practice some of the movement interventions such as strengthening and toning which had been perceived as useful for their rehabilitation. Overall participants really enjoyed the programme and rated it highly, as is highlighted in the comments below:
In response to Q1: “What new skills have you learnt?”
“It has been useful to learn new techniques and be reminded of previous knowledge, bringing it to the forefront to be applied. It has also been helpful to learn about things that have helped others in the group.” - PPT6
In response to Q4: ‘What have you enjoyed most about the programme?’
“I have enjoyed all sessions, as they have allowed me time to focus on my own wellbeing. The Qi Gong was something new for me, and was useful, as it gave me hope about doing exercise to improve fitness.” - PPT6
“Qi-gong meditation activities and being with others in a similar situation.” - PPT1
10.5.5. 6-week programme
N = 10 registered and n = 8 participants attended the 6-week programme, of which n = 5 completed the programme.
BP was taken and recorded for all participants on the 6-week programme and can be seen in Table 9 .
Table 9.
Weekly blood pressure readings of participants attending the 6-week programme.
| Participant | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
|---|---|---|---|---|---|---|
| DP38 | Absent | 154/98⁎⁎ | 139/90* | 139/96* | 155/102⁎⁎ | 121/81* |
| EH44 | 142/109⁎⁎ | 149/105⁎⁎ | 145/99⁎⁎ | absent | 148/96⁎⁎ | 148/110⁎⁎ |
| LK41 | 113/74 | 105/73 | 120/79 | absent | 121/83 | 122/89 |
| MB45 | Reading not taken | absent | 137/77* | absent | absent | absent |
| AG46 | 142/83* | 137/91* | 120/68 | absent | Absent | absent |
| MW35 | 136/77* | 131/90* | – | 129/75* | 115/71 | 154/103* |
| CG18 | Reading not taken | absent | absent | absent | absent | absent |
| ET43 | 112/78 | 100/75 | 139/75* | 110/72 | 115/74 | 106/76 |
Key.
pre-high BP.
high BP.
10.5.6. Oxygen saturation (SATS) assessment
SATS were recorded at the start of weekly sessions for participants on the 6-week programme see Table 10 .
Table 10.
Weekly oxygen saturation readings of participants attending the 6-week programme.
| Participant | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
|---|---|---|---|---|---|---|
| DP38 | absent | 93* | 95* | 97 | 96 | 94* |
| EH44 | 99 | 99 | 99 | absent | 99 | 99 |
| LK41 | 99 | 98 | 99 | absent | 98 | 99 |
| MB45 | Reading not taken | absent | 90* | absent | absent | absent |
| AG46 | 99 | 99 | 98 | Absent | absent | absent |
| MW35 | 99 | 98 | 93* | 97 | 92* | 96 |
| CG18 | Reading not taken | absent | absent | absent | absent | absent |
| ET43 | 99 | 98 | 97 | 98 | 97 | 98 |
Key.
Denotes those whose SATS were below the normal range.
10.5.7. Service evaluation 6-week programme
N = 5 Participants gave feedback about the 6-week programme. Participants that attended the 6-week programme scored the delivery as 11/16 with an overall percentage score of 69%, slightly lower than the first group delivery. Once again, the feedback we received was that participants wished to have more sessions in which to implement the techniques and skills they had learnt within the sessions and to continue receive the social benefits of being around others with a similar experience:
“If possible, it would be great to continue the service over a longer period of time. Along with the benefits of the content of the sessions, the social benefits have been invaluable. Being in a room of people who understand without judgement has helped greatly. Thank you.” - EH44
In the second cohort, the sessions enjoyed the most included exercise sessions such as seated yoga & strength and conditioning (n = 3), Breathing techniques & mindfulness (n = 2):
“Exercises - chair to build up - good to build up strength and also to boost wellbeing as made me smile.” - ET43
“Any of the sessions that touched on mindfulness and calming techniques, as this is something I struggle with.” - EH44
However, these sessions were also rated as the least enjoyable by others: Physical exercise sessions (n = 2), breathing and mindfulness (n = 2):
“Breathing/mindfulness - breathing exercises make me anxious.” - LK41
“Exercises, felt it was difficult due to [my existing] health conditions” - MW35
Overall, the programme was highly rated by the participants within the second cohort that attended the 6-week version:
“Loved the sessions. It is good that you know that it isn't just you [struggling with Long Covid] …Fab, fab course with lovely people. Lots of understanding and empathy. Thank - you. X” - ET43
10.5.8. WHHQ-18 data
As table 11 demonstrates, of those individuals that completed both the first and second WHHQ-18 forms, n = 12 showed an improved score, n = 1 showed a decline and n = 3 did not complete.
Table 11.
WHHQ-18 data (n = 16), demonstrating the individual score changes of WHHQ-18 baseline compared to the follow up.
| Mean Score Before Attending Programme | Mean Score After Attending Programme | +/- Individual Change Score |
|---|---|---|
| 45 | 47 | +2 |
| 57 | 52 | −5 |
| 16 | 23 | +7 |
| 43 | 48 | +5 |
| 30 | 38 | +8 |
| 32 | 45 | +13 |
| 37 | 52 | +15 |
| 29 | 41 | +12 |
| 25 | 27 | +2 |
| 48 | Incomplete | Incomplete |
| 27 | Incomplete | Incomplete |
| 42 | 47 | +5 |
| 5 | 17 | +12 |
| 40 | 43 | +3 |
| 37 | Incomplete | Incomplete |
| 26 | 33 | +7 |
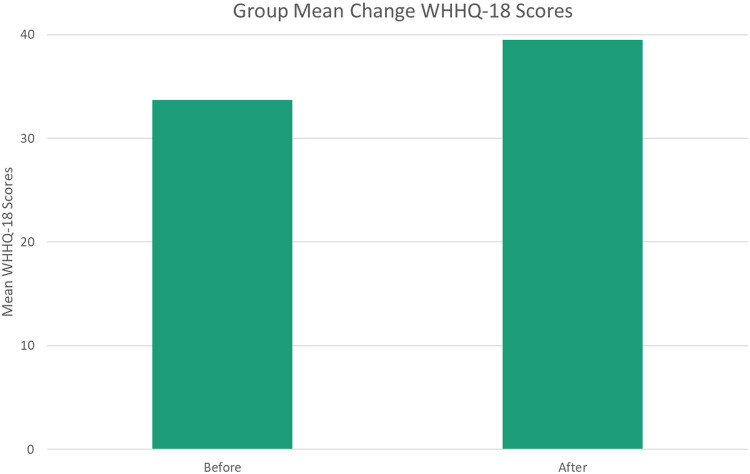
The WHHQ-18 data seen in Fig. 2 , showed a positive change in wellbeing of the group (n = 16), with a mean score of 33.7 (SD=12.5) at the start of the programme and a mean score of 39.5 (SD=10.8) at the follow-up.
Fig. 2.
Group mean change WHHQ-18 scores.
11. Discussion
The paper aimed to report on the evaluation of the outcomes from delivering and assessing a complementary and integrative approach for those struggling with the effects of Long Covid within a community setting. A quantitative approach and exploratory study design were employed. To our knowledge this is one of the first studies to be published about Long Covid combining psychoeducation and mind-body complementary approaches within a community setting.
11.1. Challenges to implementation
Recruitment into the project was initially slow as the team found it difficult to get the information to GP networks and beyond a few social prescribers. An introduction was made to the Respiratory Department of Royal Stoke Hospital to make them aware of the Long Covid project, and as a result, consultants shared the information to their patients’ who self-referred to the project. As this project was delivered during the pandemic and local public healthcare providers were in crisis, there was no opportunity to target specific clinicians or to take time to speak to other voluntary sector groups in person who could sign-post the community members that they support. Social media as a main mode of recruiting relies heavily on others liking and sharing, information and a strong campaign is required. Identifying or having access to clinicians in the relevant area is important to ensure that the project serves those for who it is intended.
Beyond this the challenges faced were COVID-19 restrictions initially, the uncertainty as to whether face to face delivery was possible and therefore the team had to take a slow and steady approach. Public venues such as community centres, were under restrictions so identifying a suitable venue which accommodated the needs of participants and the project delivery was important, a local private physiotherapy centre was used to host the groups. Under normal circumstances a project supporting those with Long Covid may be best hosted in a community room within a GP practice or a local fire-station (free to use for community groups, accessible, free parking, on transport routes and be a resource for social prescribers to draw on).
The county of Staffordshire is in the Midlands of West Central England and is approximately 1000 miles square and the team decided to see where referrals were coming from before determining where to base the project. The option to fund and provide transport for participants that may not be able to access the project was made to minimise barriers to access as much as possible. Based on the geographical distance and the level of fatigue a participant was experiencing determined if transport was arranged by the project. Attempts to use local voluntary car schemes were thwarted as they were impacted by the lack of volunteer drivers shielding during the pandemic and as a result taxis were arranged and paid on behalf of participants. All participants that used this aspect of the project, acknowledged that without it they would not have been able to attend the weekly groups.
The very nature of Long Covid symptoms can limit participation as some people do not feel well enough on the day to attend. This influenced attendance and retention rates throughout the project.
11.2. Covid-19 yorkshire rehabilitation scale screening tool
For this service, the Covid-19 Yorkshire Rehabilitation Scale (C-19 YRS) screening tool was adapted for use online. Some participants willingness or ability to complete an online registration form was limited. Literacy can be a barrier to accessing healthcare or support for many [16]. This was mitigated through offers of support and a practitioner sitting with the participant and going through the questions. Having participants complete the C-19 YRS screening tool online meant that the data was easily accessible in an excel spreadsheet for the purpose of analysis. Three participants asked for the form to be printed so that they could use a paper version, and all received support with completing it. Yet the C-19 YRS tool proved useful to determine the needs of the participants in the groups and enabled the facilitators to use clinical reasoning to make decisions about the suitability of the activities delivered within the groups, and to identify those participants that had pre-existing health complications. Fatigue, pain, breathlessness, anxiety, and cognitive impairment are the most cited symptoms in Long Covid, this was consistent with our findings. Some participants had pre-existing difficulties with these complaints and their reporting of symptoms showed this had been exacerbated with Covid. For others, Covid was the primary source of these problems. Unlike the more specific questionnaires for generalised anxiety or physical difficulty, the C-19 YRS attempts to encompass the wider ranging effects of Long Covid. This was essential to capture the greater impact of COVID-19 on everyday life. Recent research has shown the C-19 YRS to be clinically useful with good internal validity [17].
The team decided to not have participants complete the C-19 YRS tool for a second time at the end of the 4- or 6-week programmes, as it was deemed as too burdensome for participants.
11.3. Interventions
The initial sessions of the 4-and 6-week programmes where participant experiences of Long Covid were shared and explored were recorded and are being reported separately. The team observed that participants valued being with others who were experiencing similar symptoms and liked that they could share and compare things that helped them cope with the impact of Long Covid and things that didn't.
The recording of blood pressure and SATS indicated to the facilitators whether the participant was well enough to undertake exercise that day. The clinical experience of the facilitators proved important as some participants had high blood pressure at the time of monitoring, after discussion the facilitators had deemed them OK to undertake the gentle exercise on that day, ongoing monitoring of each participant was carried out.
11.4. Service evaluation
Participants were asked to explain what skills they had learnt from the activities that were delivered and how they had applied them. They were asked to say what they most and least enjoyed and why? They were asked for feedback on the logistics of the project (session days, times, duration). They were also asked to make suggestions for improvements for future projects. Most of the feedback from participants who took part in the project was positive. The changes implemented between the first cohort and second cohort to increase the number of group sessions from 4 to 6 so that more time could be spent practising and implementing the gentle exercises learnt. On the 4-week programme the memory session was the least preferred, this may have been to do with the fact that this session involved listening and concentration which can be difficult for those with fatigue. On the 6-week programme, one participant found the breathing exercise a challenge due to anxiety and a second participant had physical disabilities which made the movement sessions more challenging. From a facilitation perspective having participants do only what felt comfortable and within their own abilities mitigated potential problems. The booklet provided which covered all the programme contents was deemed useful reading as a reminder of what was delivered during each session. From a facilitation perspective combining psychoeducation and mind-body complementary approaches worked well in the community setting.
11.5. WHHQ-18 evaluation
Evaluating the wellbeing of the participants who attended the weekly group sessions was an important factor to monitor. Wellbeing is feeling good and functioning well [18] and as most of the participants had not been feeling good or functioning well prior to attending the sessions, having their symptoms and challenges acknowledged and heard by professionals and to share experiences with others who were having similar experiences improved their sense of wellbeing.
Of the n = 18 participants that started on the programme only n = 13 completed both baseline and follow up WHHQ's. Although the number of participants who used the service was small, positive changes to wellbeing were recorded on the WHHQ-18 by participants of one of the individuals undertaking 1:2:1 CST sessions and all participants except one who took part in 4-week and 6-week programmes. This sample size is not deemed large enough to measure change from a statistical significance perspective.
11.6. Limitations of this study
All data was self-reported by the participants. The numbers of participants who attended the groups from start to finish were small and therefore the results of the WHHQ-18 cannot be generalised. The heterogenous nature of Long Covid would require that if these methods were to be replicated a large sample size would be needed. The lack of ethnic diversity within our cohorts could reflect the overall lack of diversity in some of the more rural areas of Staffordshire and us not accessing inner city GP networks whilst promoting the service.
11.7. Strengths of this study
This project was delivered as the UK was emerging from lock-down and the phenomenon and understanding of Long Covid was evolving. We aimed to support as many people as possible with diverse issues due to the heterogenous nature of those with Long Covid and the multiple systems that this phenomenon has been shown to affect. Having a broad inclusion criterion was a strength, as if the inclusion criteria had been too narrow, it may have been difficult to extrapolate the data to inform practice of the wider issues of Long Covid. This was a novel approach with a range of activities that could be easily adapted to suit the needs of individuals. The feedback from participants was positive about the format and content of the weekly groups. There were positive clinical changes reported using the WHHQ-18 in individuals between baseline and follow up, indicating that the activities offered to the group were improving the wellbeing of those that attended.
11.8. Recommendations and implications
Whilst this project was funded and delivered as a voluntary sector project for the local community (non-National Health Service), it is recommended that future UK based Long Covid support services be promoted through National Health Service and GP networks and social prescribing networks to ensure the number of participant referrals is sufficient to deliver a programme combining psycho-education and mind-body complementary interventions such as those delivered in the ‘Torus Road to Recovery Long Covid Project.’ At the time of writng there are was no National Health Service provision within Staffordshire for Long Covid. a project such as this could be a useful resource for any individual struggling with the after-effects of COVID-19.
Barriers to attendance including location and distance to travel, all have bearing when delivering within community settings. The Long Covid symptoms such as fatigue, can not only affect people's willingness to travel, but their ability to engage and drive home safely at the end of a session. Having registered participants, helps to know who will be ‘turning up’ on the day and help with planning, delivering to fewer participants is good for them, but the costs still are the same. Maximising full attendance where possible is better from an organisational perspective and a better use of clinical resources.
12. Conclusion
Support combining psycho-educational and mind-body approaches for those struggling with the effects of Long Covid in the community was well received. The methods of evaluation used appear to be an acceptable way to evaluate a service of this kind within a community setting. The sample size in this project was small, yet positive changes in wellbeing were reported by participants, and interventions such as those delivered in this project may be worth replicating in a population of those with Long Covid.
Financial support
This project was funded by the National Lottery Community Fund, Project ID: 20153533. NB & SA were paid to deliver this project . The funders were not involved in the journal article.
CRediT authorship contribution statement
Nicola Brough: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Supervision, Writing – original draft, Writing – review & editing. Sally Abel: Conceptualization, Investigation, Methodology, Writing – review & editing. Lucy Priddle: Data curation, Formal analysis, Writing – review & editing.
Declaration of Competing Interests
NB & SA are practitioners of CST & Physiotherapy and may gain an increase in clients because of publishing this manuscript.
Acknowledgments
Acknowledgements
The authors would like to thank Janine Proctor for supporting the funding acquisition. Carys Roberts of Swan Health & Physiotherapy for the use of their facilities. Lucy Priddle Intern on the Keele University Student Skills Exchange programme for her presence at the weekly support groups. Catherine Jaroszek for facilitating the Qi-gong session, Deborah Jackson for facilitating the seated yoga sessions. Esther Donoff, Nutritional Therapist for her contribution to the nutritional section, ‘eating for immunity’ in the Long Covid support service booklet. Finally, to the participants for their contributions in both engagement and feedback.
Data Availability
The dataset(s) supporting the conclusions of this article is (are) available from Mendeley.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eujim.2022.102182.
Appendix. Supplementary materials
References
- 1.(ONS), O.F.N.S., Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK 2022: London. p. 1.
- 2.W.H.O. World Health Organisation; 2021. A Clinical Case Definition of Post COVID-19 Condition By a Delphi consensus; p. 20. vi. [Google Scholar]
- 3.W.H.O. World Health Organisation: Europe; 2021. Support For rehabilitation: Self-Management After COVID-19-related Illness. [Google Scholar]
- 4.Moynihan R., et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. British Med. J. Open. 2021;11 doi: 10.1136/bmjopen-2020-045343. e0453435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brough N., et al. Perspectives on the effects and mechanisms of craniosacral therapy: a qualitative study of users' views. Eur. J. Integr. Med. 2015;7(2):172–183. [Google Scholar]
- 6.CSP. and C.S.o . The Chartered Society of Physiotherapists; London, UK: 2021. Physiotherapist, Safety First Approach to Long Covid Assessment, in Frontline. [Google Scholar]
- 7.Green C., et al. A systematic review of craniosacral therapy: biological plausibility, assessment reliability and clinical effectiveness. Complement Ther. Med. 1999;7(4):201–207. doi: 10.1016/s0965-2299(99)80002-8. [DOI] [PubMed] [Google Scholar]
- 8.Brough N., et al. Perspectives on the effect and mechanisms of craniosacral therapy: a qualitative study of users' views. Eur. J. Integr. Med. 2015;7:172–183. [Google Scholar]
- 9.Castro-Sanchez A.M., et al. Benefits of craniosacral therapy in patients with chronic low back pain: a randomized controlled trial. J. Altern. Compl. Med. 2016;22(8):650–657. doi: 10.1089/acm.2016.0068. [DOI] [PubMed] [Google Scholar]
- 10.Mataran-Penarrocha G.A., et al. Influence of craniosacral therapy on anxiety, depression and quality of life in patients with fibromyalgia. Evidence-based Compl. Altern. Med. 2011 doi: 10.1093/ecam/nep125. 2011 (no pagination)(178769) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castro-Sanchez A.M., et al. A randomized controlled trial investigating the effects of craniosacral therapy on pain and heart rate variability in fibromyalgia patients. Clin. Rehabil. 2011;25(1):25–35. doi: 10.1177/0269215510375909. [DOI] [PubMed] [Google Scholar]
- 12.Fund, T.K. What is social prescribing? 2017 [cited 2022 12 August 2022]; Available from: https://www.kingsfund.org.uk/publications/social-prescribing?gclid=CjwKCAjw9NeXBhAMEiwAbaY4lp9S2_ZyFB5Mwmzs1MyenQM6DYgMunwU9QQJJYtb9L9YI12fxsnJghoCpXYQAvD_BwE#what-is-it.
- 13.Biggs A., et al. A Survey of craniosacral therapy (CST) practitioners. Profiling practice and informing organisational strategy. Eur. J. Integr. Med. 2015:684. [Google Scholar]
- 14.Sivan M., Halpin S., Gee J. Assessing long-term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool) Adv. Clin. Neurosci. Rehabil. 2020;19(4):14–17. [Google Scholar]
- 15.Brough N., et al. Development and validation of a PROM to capture holistic outcomes in traditional, complementary and integrative medicine - the warwick holistic health questionnaire (WHHQ-18) Eur. J. Integr. Med. 2021;47 [Google Scholar]
- 16.England P.H. Public Health England; London: 2015. Local Action on Health Inequalities: Improving Health Literacy to Improve Health Inequalities. [Google Scholar]
- 17.O'Connor R.J., et al. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): application and psychometric analysis in a post-COVID-19 syndrome cohort. J. Med. Virol. 2022;94(3):1027–1034. doi: 10.1002/jmv.27415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huppert F.A., So T.T. Flourishing across Europe: application of a new conceptual framework for defining well-being. Soc. Indic. Res. 2013;110(3):837–861. doi: 10.1007/s11205-011-9966-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset(s) supporting the conclusions of this article is (are) available from Mendeley.