Abstract
Objective
The purpose of this study was to explore perceived ease of use, usability, and the feasibility of using mobile health applications to manage hypertension self-care in rural Black older adults with hypertension.
Methods
A convergent parallel mixed method design was used to study a purposeful sample of 30 Black older adults (29 females, 1 male) from rural East Texas. Quantitative data included demographic characteristics and measured blood pressure, height, and weight, along with questionnaires: the Hill-Bone Compliance to High Blood Pressure Therapy Scale, the Krousel-Wood Medication Adherence Scale-4, and the Technology Acceptance Model Questionnaire (adapted). Qualitative data were obtained from five focus groups and analyzed using thematic analysis.
Results
Mean age was 66.3 ± 9.6 years. Less than half of the participants (46.7%) had a systolic and/or diastolic blood pressure >130/80. Greater participant adherence was noted with the Hill-Bone Compliance scale (63.3%) than the Krousel-Wood scale (23.3%). With the Technology Acceptance Model, perceived ease of use was significantly correlated with behavioral intention (r = 0.654, p < 0.000) and perceived usefulness (r = 0.585, p < 0.001), while behavioral intention was negatively associated with age r = −0.047 (p=0.009). Focus group data revealed five themes: 1) useful, 2) counterintuitive, 3) communication, 4) comfort with the status quo, and 5) educate/show me how.
Conclusion
Smartphone technology and other health-related computer technologies were not preferred by older adults in this study due to limited digital literacy. Simplicity and easy navigation in the design of mHealth apps are needed to improve treatment adherence and blood pressure control in rural older adults with hypertension.
Clinical Relevance
Mobile health applications have the potential to increase self-management of chronic hypertension if users are digitally literate. Health-care providers need to assess older patients for digital literacy and offer educational support and assistance.
Keywords: hypertension, African American, mobile health applications, smartphone, mixed methods
Video abstract

Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Exploring Feasibility of mHealth to Manage Hypertension in Rural Black Older Adults: A Convergent Parallel Mixed Method Study
For Blacks, the prevalence of hypertension (HTN) in the United States is among the highest in the world among males (56.6%) and females (55.3%).1 By 55 years of age, the cumulative incidence of HTN increases to 75% for Black men and women.2 As the leading cause of global disease burden, HTN contributes to a greater risk of cardiovascular-related diseases including heart disease, renal failure, and stroke. When compared to other racial/ethnic groups, Black adults are disproportionately affected by the overwhelming rates of HTN and HTN-related diseases.3
The reason for the high prevalence of HTN among Black adults is multifaceted and extends from the social determinates of health to societal-level disparities influenced by the effects of systemic and structural racism.4,5 In older adult rural populations, the social and systemic inequities that influence health disparities are accentuated by higher poverty rates, multiple chronic health conditions, limited access to health care, and less health promoting behaviors that are more pronounced in Black than White older adults.6 Likewise, the risk of HTN-related cardiovascular disease in rural populations is higher, especially among women who have additional cardiovascular risk factors because they are more likely to be older, poorer, uninsured, less educated, socially isolated, lack access to health services, and have higher rates of chronic disease.7
Effective methods to improve blood pressure (BP) control include adherence to antihypertensive medication along with lifestyle modifications (eg, increased physical activity, healthy diet, weight management, etc.).3,8 Modest changes in lifestyle modifications can lead to clinically significant reductions in BP.9 However, research supports that more intensive BP lowering with antihypertensive medication reduces major cardiovascular events by 11%, myocardial infarction by 13%, stroke by 24%, and end stage renal disease by 11%.10 Thus, BP control is paramount to prevent worsening of HTN-related diseases.
Research on antihypertensive medication adherence interventions was reported by Ruppar et al11 using a systematic review and meta-analyses of 37 studies with 45 interventions. Of note was one intervention that worked well with Black patients, and it included a medication packaging system (eg, blister packages, pillbox organizers, or specialized bottle labeling). The packaging enhanced adherence by allowing patients to organize their medications visually as a feedback mechanism. Interventions least effective for medication adherence were medication counseling, social support, computer-based intervention, interactive discussion, and provider training for skills to improve adherence.11 Therefore, research aimed at culturally responsive strategies to improve medication adherence in this population may be warranted.
Smartphones, Mobile Health Applications and Blood Pressure Control
Smartphone technology and mobile health applications (mHealth apps) have the potential to improve chronic conditions such as HTN by aiding disease self-management to promote health, increase quality of life, and reduce health-care costs.12,13 In a systematic review and meta-analyses of 23 studies, Li et al14 found that smartphone-based mHealth apps were effective in managing HTN and improving medication adherence. Results showed a greater reduction in both systolic and diastolic BP in the mHealth intervention groups compared to control groups. Similarly, another systematic review and meta-analyses of six studies15 using a smartphone intervention showed decreases in BP and increases in medication adherence in the intervention group. One study16 used a breathing awareness meditation via a smartphone app as a stress management strategy with significant systolic BP reductions. In contrast, another study using an automated text messaging system to improve medication adherence among Black adults with uncontrolled HTN and found nonsignificant yet clinically meaningful differences between groups for medication self-efficacy, BP, and adherence measures.8 An analysis of 107 mobile apps designed for smartphones and HTN management was conducted by Kumar et al.17 In this study, almost three-fourths of the apps facilitated health management tracking by recording and tracking BP, heart rate, caloric/sodium intake, and weight/BMI. It is evident that advances in mHealth app technology have the capacity to improve self-management of chronic diseases such as HTN.
Technology Challenges and Digital Literacy
Current data revealed that 90% or more Americans under the age of 34 have owned a smartphone since 2015, while the ownership rate among those aged 50 and older has risen from 53% to 67% over the same period.18 While most Americans own a smartphone, Black, Hispanic, and other non-White adults lag behind in terms of digital literacy.19 National estimates report that 16% of Americans do not have sufficient competence with technology to operate a computer and are classified as digitally illiterate. Although the United States is considered a world leader in advanced internet services and technology,20 the benefits of this technology are not easily accessible to all Americans, especially those in rural areas and this furthers the digital divide.19 Kontos et al21 described a second-level digital divide wherein availability of smartphones (computers, tablets, and other technology-enabled devices) has increased. In contrast, Powe’s22 study of health information seeking behaviors found internet usage has not increased among rural Caucasians, Hispanics, and Blacks with the lowest usage of 8% among older Black adults compared to 24% in both Caucasians and Hispanics.
Mobile health applications are increasing the ability of patients to self-manage chronic disease, promote wellness, and reduce the effects of chronic conditions.23 However, little is known about how mHealth apps may be used in rural settings to assist Black older adults with HTN who may be further challenged by limited digital literacy, ease of use, costs, and low socioeconomic status.24
No known studies have investigated the use of smartphones in rural older Black adults with HTN. Therefore, the purpose of this mixed method pilot study is twofold. First, the qualitative component explored the usability, acceptance, and feasibility of mHealth apps in rural Black older adults with HTN to better understand how participants viewed the use of mHealth apps for self-management of HTN and BP control. Secondly, the quantitative component addressed the relationship between behavioral intention to use mHealth apps, adherence, and BP control in rural older Black adults with HTN.
Theoretical Framework
Two (non-competing) frameworks guided this mixed method feasibility study. First, the Technology Acceptance model (TAM)25 was adapted for mHealth apps26 and is appropriate for the study purpose. This model’s major constructs are 1) perceived ease of use (PEU), the “degree to which a person believes that using a particular system would be free of effort”; and 2) perceived usefulness, “the degree to which a person believes that using a particular system would enhance their job performance.”25
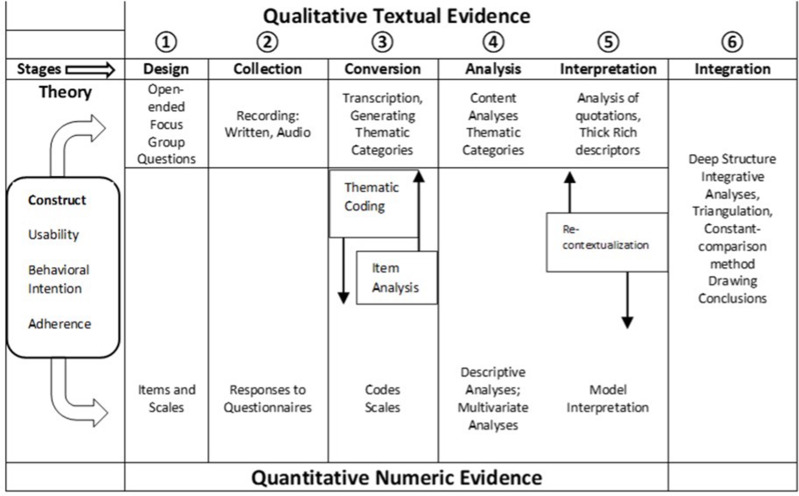
Secondly, the multistage paradigm for integrative mixed method approach27 was adapted to guide the underpinnings of this study (see Figure 1). This integrative process begins with conceptualizing the main constructs of usability, behavioral intention, and adherence as research evidence. Usability is defined as the quality or state of being usable.28 Behavioral intention (from Fishbein & Azjen’s Theory of Reasoned Action)29 is defined as, “the agent’s subjective probability that he/she will perform the behavior.” Adherence refers to the extent to which a person’s behavior corresponds with agreed recommendations from a health-care professional.30 Core constructs were explored under each of the six stages (listed in Figure 1) within a parallel process that facilitates data conversions, to encode thematic categories into thematic variables.
The greater the qualitative–quantitative parallelism in the study design and its’ implementation, the easier it is to compare and contrast textual and numeric forms of evidence in an integrative manner.27
Figure 1.
Adapted Integrative Mixed Method Paradigm.
We examined research evidence in both forms concurrently to obtain more definitive conclusions and for a more complete understanding of mobile health technology, usability, behavioral intention, adherence, along with the potential self-management of HTN in Black older adults with HTN. In addition, we used a full integrative perspective, to examine research evidence gathered using both data forms, to generate “deep structure” conclusions31 that offer enhanced explanatory power above and beyond the sole use of a qualitative or quantitative approach.
Methods
Research Design
A convergent parallel mixed method design was used to answer the research questions in this pilot study. Data for the quantitative strand of the study were collected first. The constructs of mobile technology’s perceived ease of use, overall usefulness, and behavioral intention to use were explored using the TAM questionnaire to determine if data revealed corroboration, convergence, or divergence with adherence scores, and mean BP readings (an indication of HTN control). The operational definition of adherence is the cumulative scores on the Krousel-Wood Medication Adherence scale (Krousel-Wood MAS-4)32 and Hill Bone Compliance to High Blood Pressure Therapy scale (CHBPT).33 Blood Pressure control is defined as BP ≤ 130/80 mmHg. The qualitative strand consisted of collecting data from focus group interviews.
A convergent parallel mixed methods approach provides a more complete understanding to answer the research questions than a single approach.34
Sample Description and Recruitment
A purposive sampling yielded 30 Black adults diagnosed with primary HTN. Eligible participants were women and men aged 50 years and older, self-identified as Black or African American, diagnosed with primary HTN, prescribed at least one antihypertensive medication, and living in rural counties of East Texas. Participants were recruited from Black churches and community centers, using church announcements, flyers, and word-of-mouth.
Ethical Considerations
The Institutional Review Board at The University of Texas at Tyler approved this study. Prior to signing the informed consent and receiving a copy, all study details including audio recordings, research procedures to maintain confidentiality of data, and anonymity with pseudonyms as participant names when reporting data were addressed with questions answered. Participants were assured they could withdraw from the study or refuse to answer any survey or focus group questions. At the completion of data collection, study participants received a $25 gift card as a thank-you for their time, effort, and travel expenses.
Data Collection and Measures
Quantitative data were collected first beginning with demographics (e.g., age, education, income, etc.), and followed by BP, height, and weight measurements. Using an Omron digital BP device, a resting BP was taken three times with the mean of the second and third readings. Weight and height were measured on a HealthOMeter® professional physician beam scale. The body mass index was calculated using weight in kilograms divided by height in meters squared35 (see Table 1 for measurement tools). Next, three standardized instruments were used to collect data on technology acceptance and adherence to the treatment regimen, and to measure mediating, moderating, and dependent variables.
Table 1.
Established Reliability and Validity of Study Tools
| Measure/Construct | Instrument/Method | Reliability/Validity/Accuracy/Precision |
|---|---|---|
| Technology Acceptance Model (TAM) Questionnaire -modified smartphone use | TAM questionnaire | High Convergent validity.25 Cronbach alphas: 0.812 and 0.803.26 Cronbach’s alpha was 0.870 in this study. |
| Adherence (±1) | Krousel-Wood MAS-4 | C statistic of 0.704, [95% confidence interval (CI) 0.683–0.714]; sensitivity and specificity of 67.4 and 67.8%.32 Cronbach alpha was 0.61 in this study. |
| Adherence (>80%) | HBCHBPT scale | Cronbach alphas: 0.74 and 0.84. Content validity (100% agreement).33 Cronbach alpha was 0.741 in this study. |
| Body Mass Index (BMI) | Formula: weight (kg)/[height (m)]2 | CDC guidelines.35 |
| BP control BP<130/80 | Omron digital BP device model HEM-780-N3 Intellisense | Calibration before study initiation mean BP of 2nd and 3rd readings obtained |
| Height/weight | HealthO-Meter® Professional physician beam scale designed to measure height and weight | Calibration before study initiation (Model 402KL) (Pelstar LLC, McCook, IL). |
| mHealth app Usefulness | Focus group | Credibility: Prolonged engagement, persistent observation, peer debriefing, triangulation, member checking. Transferability: Purposive sampling, thick description, and robust data Dependability: Use of overlap methods (triangulation) Confirmability: Audit trail, reflexive journaling.38,39 |
| Ease of Use | Focus group | Olympus digital voice recorder Mp3 digital files transcribed word-for-word with audit trail using MaxQDA.40 |
The Technology Acceptance Model (TAM) questionnaire (adapted)25 is a 10-item instrument that measures 3 constructs, perceived ease of use, behavioral intention, and perceived usefulness. This instrument has a 5-item Likert scale ranging from “strongly agree” to “strongly disagree”. The TAM model was validated by several researchers across disciplines26,36,37 and has influenced the health information research that assesses technology usability. In this study, the TAM was used to predict usage of mHealth apps on the smartphone. This study adapted the original item (computer) with the word “smartphone” to determine the correlation between perceived usefulness, ease of use, and behavioral intention.
The Krousel-Wood Medication Adherence scale (Krousel-Wood MAS-4) captures four domains of adherence behavior: 1) medication-taking self-efficacy, 2) physical function quality of life, 3) intentional non-adherence, and 4) forgetfulness.32 This brief 4-item hybrid instrument has a Likert scale from 0 (none of the time) to 4 (all of the time) with higher scores indicating worse adherence. Thus, scores ≥1 indicate low adherence and <1 indicates high adherence.
The Hill-Bone Compliance to High Blood Pressure Therapy (Hill Bone CHBPT)33 scale is comprised of 14 items in three subscales: 1) reduced sodium intake; 2) appointment keeping; and 3) medication taking. This scale has a four-point Likert type scale from 1 (strongly agree) to 5 (strongly disagree) with scores ranging from 14 to 56. Lower scores indicate perfect adherence. See Table 1 for the established reliability and validity for each of the study tools.
Lastly, for the qualitative component, semi-structured, open-ended interview questions (see Table 2) were used to collect data in a community setting using focus groups that consisted of 5–10 participants. Focus groups met for 60–90 minutes in a closed, private room at various locations agreeable to the participants in a rural setting. Using participant pseudonyms, data were recorded with an Olympus™ digital voice recorder (Model VN-702PC). Field notes were taken and compared to participant transcriptions and main themes. Member checks were conducted with a subset of focus group participants after interviews. An audit trail was done using MaxQDA memo feature. The framework created by Lincoln and Guba38 was used to establish trustworthiness and rigor (credibility, dependability, confirmability, and transferability) (see Table 1).
Table 2.
Focus Group Semi-Structured Question Examples
| Primary Questions | Themes |
|---|---|
| 1.Do you own/use a smartphone? Why or why not? 2.Tell me how you use your smartphone. |
Useful |
| 3.Tell me your opinion about how easy a cell phone/smartphone is to use. 4.Tell me how you feel about using mobile applications on your phone. |
Counterintuitive |
| 5.Tell me what barriers you have with using a smartphone. | Comfortable with status quo |
| 6.Tell me how you feel about health apps for smartphones. | Show me how |
| 7.How do you feel about sharing your health information with your doctor? 8.What app would you like to see on your smartphone to assist you with your health? |
Communication |
Data Analysis
Quantitative data were analyzed using descriptive statistics, simple linear regression, correlation, and reliability. IBM SPSS Statistics (Version 24) was used to analyze data. A priori level of significance was 0.05. Initial tests for normality were analyzed with Kolmogorov–Smirnov and Shapiro–Wilk tests. Five qualitative focus group interviews were transcribed verbatim and thematic content analysis was conducted using constant-comparison method with MAXQDA 2020.40 Braun and Clark41 thematic analysis process was used and included the following steps: 1) Familiarize with the data. 2) Generate initial codes, 3) Search for themes, 4) Review themes, 5) Define and name themes, and 6) Produce the report. Data integration/deep structure analyses were conducted using triangulation, constant comparison, and qualitative descriptive techniques.42 Analyses included confirmation and disconfirmation of qualitative and quantitative results to reveal “deep structure”.31 Deep structure analyses include exploring study findings in the context of Black participants’ core values, beliefs, norms, and worldviews to provide context and give saliency to the research questions and findings.43
Results
Quantitative
Thirty Black older adults including 29 females and 1 male, ranging in age from 50 to 87 years (mean 66.3, SD±9.6) participated in the study. Age was normally distributed in this sample with a median age of 66.5 years and an interquartile range was 14.50. All but one participant (96.7%) reported having a family history of HBP and 56.7% (n = 17) reported being diagnosed with HBP for 10 years or longer (see Table 3). Almost all participants (96.7%, n = 29) had a BMI over 25 with a mean of 34.48 (SD ±6.46) and were taking one to three anti-hypertensive medications (83.3%, n = 25). Four participants (13.2%) reported taking folk remedies such as vinegar, lemon juice, and mustard to treat HBP (see Table 4).
Table 3.
Sociodemographic Characteristics (N = 30)
| Variable | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Sex | |||
| Male | 1 (3.3) | ||
| Female | 29 (96.7) | ||
| Age (years) | 66.3(9.6) | 37 (50-87) | |
| Education | |||
| High school and less | 15 (50.0) | ||
| Post-high school | 15 (50.0) | ||
| Income (annual) | |||
| 29, 999 or less | 21 (70.0) | ||
| 30,000 or above | 9 (30.0) | ||
| Marital status | |||
| Married | 6 (20.0) | ||
| Separated/Divorced | 10 (33.3) | ||
| Widow | 11 (36.7) | ||
| Close Friends (Support) | 10(10) | 49 (1-50) | |
| Length of HBP | |||
| 10 years or more | 17 (56.7) | ||
| Family History | |||
| Yes | 29 (96.7) | ||
| Insurance | |||
| Yes | 28 (93.3) | ||
| Insurance to buy medication | |||
| Yes | 27 (90.0) |
Abbreviation: SD, standard deviation.
Table 4.
Physiological, Adherence Scales, and Blood Pressure-Related Participant Characteristics (N = 30)
| Variables | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Blood Pressure Constructs | |||
| Body Mass Index (kg/m2) | 34.48 (6.46) | 22.5 (24.4-46.9) | |
| Under 25 | 1 (3.3) | ||
| Overweight (25-29.9) | 9 (30.0) | ||
| Obese (30 or greater) | 20 (66.7) | ||
| Number of HBP Medication(s) | |||
| One | 10 (33.33) | ||
| Two to Three | 15 (50) | ||
| Five to Seven | 5 (16.67) | ||
| Blood Pressure | |||
| Systolic | 129 (18.7) | 70 (90-160) | |
| Diastolic | 73 (13.2) | 48 (50-98) | |
| Uncontrolled Blood Pressure | |||
| Systolic > 130 mmHg | 14 (46.7) | ||
| Diastolic > 80 mmHg | 9 (30.0) | ||
| Both Systolic/Diastolic BP <130/80 | 14 (46.7) | ||
| Those Taking Folk Remedies | 4 (13.3) | ||
| Adherence Constructs | |||
| HBCHBPT Scale (Score Range: 14-56) | 21 (4.98) | 21 (15-36) | |
| Low adherers < 22 | 19 (63.3) | ||
| High adherers ≥ 22 | 11 (36.7) | ||
| K-Wood-MAS-4 (Score Range: 0-4) | 1 (1) | 4 (0-4) | |
| Low adherers ≥ 1 | 7 (23.0) | ||
| High adherers < 1 | 23 (76.0) |
Abbreviations: SD, standard deviation; HBP, High blood pressure; HBCHBPT, Hill-Bone Compliance to High Blood Pressure Therapy; K-Wood-MAS-4, Krousel-Wood Medication Adherence Scale-4.
High BP Characteristics
The mean systolic BP was 129 (± 18.7) mm Hg and diastolic BP was 73 (± 13.2) mm Hg. However, 46.7% of the sample had a systolic >130 mm Hg and 30% had a diastolic >80 mmHg indicating poor BP control. Only 46.7% (n = 14) had both systolic and diastolic BP controlled (see Table 4).
Adherence
Results of the Hill Bone CHBPT scale resulted in a mean scale score of 21.7 (± 4.98). A cut score of 22 or below indicates greater adherence (80% or more), thus 63.3% (n = 19) of participants were below 22 and 36.7% (n = 11) were above 22 indicating poorer adherence scores. Results of the Krousel-Wood MAS-4 questionnaire showed a mean score 1.63 (±1.35) with 23.3% (n = 7) of participants with good adherence and 76.7 (n = 23) with poorer adherence (See Table 4).
Smartphone Use, Acceptance, and Behavioral Intention
Of the study participants, 76.3% (n = 23) reported owning a smartphone, were familiar with its use, and were able to text message (see Table 5). Whereas, slightly over half (53.3%, n = 16) of the participants reported the ability to use a personal computer along with email use (60%, n = 18). When asked if they needed help to use technology, 36.7% (n = 11) replied yes. After stratified by age, data revealed younger participants aged 50–66 years used technology to the fullest. However, older participants (67–87 years) did not use technology, had no intention to use technology (email, text messaging, or a computer), and replied “no” when asked if they needed help using technology. Perceived Ease of Use was significantly correlated with Behavioral Intention (r = 0.654, p < 0.000) and Perceived Usefulness (r = 0.585, p < 0.001), indicating a moderate positive relationship between the variables. Behavioral Intention was negatively associated with age r = −0.047 (p=0.009, 1-tailed).
Table 5.
Characteristics of Smartphone/Technology Use and Technology Acceptance Model (TAM) Questionnaire in Rural Older African Americans (N = 30)
| Items | N (%) | Mean (SD) | Range |
|---|---|---|---|
| Use/own a smartphone | |||
| Yes | 23 (76.3 | ||
| Use text messaging? | |||
| Yes | 23 (76.3) | ||
| Use a personal computer | |||
| Yes | 16 (53.3) | ||
| Use email | |||
| Yes | 18 (60) | ||
| Need help to use technology | |||
| No | 19 (63.3) | ||
| TAM questionnaire (10 items) | |||
| Perceived Ease of Use 1 | 3.53 (1.54) | ||
| Perceived Ease of Use 2 | 2.23 (1.38) | ||
| Perceived Ease of Use 3 | 3.23 (1.61) | ||
| Total Perceived Ease of Use Subscale | 9 (2.88) | 12 (3-15) | |
| Behavioral Intention 4 | 3.16 (1.46) | ||
| Behavioral Intention 5 | 3.30 (1.36) | ||
| Behavioral Intention 6 | 2.50 (1.16) | ||
| Total Behavioral Intention Subscale | 8.96 (3.36) | 11 (3-14) | |
| Perceived Usefulness 7 | 2.73 (1.52) | ||
| Perceived Usefulness 8 | 3.13 (1.16) | ||
| Perceived Usefulness 9 | 2.93 (1.36) | ||
| Perceived Usefulness 10 | 2.90 (1.24) | ||
| Total Perceived Usefulness Subscale | 11.7 (4.42) | 16 (4-20) |
Abbreviation: TAM, Technology Acceptance Model.
After testing for assumptions, we calculated a simple linear regression to predict behavioral intention based on age. A significant regression equation (F (1, 28) = 6.23, p < 0.019) with an R2 of 0.182 found that as age increased, behavioral intention to use mHealth apps decreased.
We also sought to determine if there was a relationship between intent to use mHealth apps, adherence scores, and BP control in older Black adults with HTN. Study variables were constructed to answer this research question. The variables were: Krousel-Wood MAS-4 -adherers (high [n = 7] and low [n = 23]), BP control (yes [n = 14] or no, [n = 16]), and the dependent variable Behavioral Intention (yes [n = 13] or no [n = 17]). Bivariate correlational analyses showed non-significant low correlations between these variables. The correlation between BP control and Behavioral Intention was r = 0.261 (p.=.164). Inverse relationships were found between BP control and Krousel-Wood MAS-4 adherers r = −0.274 (p = 0.143), and Behavioral Intention and Krousel-Wood MAS-4 adherers, r = - 0.154 (p = 0.417).
Qualitative Results
During the focus group interviews, participants were asked semi-structured questions (see Table 2). Five themes were identified from data analyses: 1) Useful, 2) Counterintuitive, 3) Communication, 4) Comfortable with the Status Quo, and 5) Educate/Show Me How. Exemplars of participant interviews were used to establish authenticity39 (See Table 6).
Table 6.
Integration of Quantitative and Qualitative Findings (Constructs-Usability, Behavioral Intention, and Adherence)
| Theme | Qualitative Exemplars | Quantitative Results | (Integration, Corroboration, Convergence-Divergence of Results) |
|---|---|---|---|
| 1. Useful | “Yes, I have a smartphone and I use it every day” Susie-Yes, I own a smartphone and I use it for personal reasons and business reasons. |
TAM questionnaire Perceived Usefulness |
Corroboration |
| 2. Counterintuitive | “If it’s just making calls, then it’s pretty easy. But when I get into messages and apps and all, … now sometimes it gets complicated. Yeah, hard as hell.” -“It’s easy to me. I’m not familiar with pulling up apps and doing a lots of things. Sometimes I make a mistake and turn my camera on, and it’ll be taking pictures of things around me. I’ve taken pictures of my feet.” |
Perceived Ease of Use Behavioral Intention |
Divergence |
| 3. Communication | “all I use it for is calling” “it gives me updated information continuously” “I want to talk to her face-to-face. You know, I don’t want to communicate what issue is going on with my body over no phone.” |
Survey of smartphone use:
|
Corroboration |
| 4. Comfortable with the Status Quo | “ … I guess it’s just all new. I spent most of my life without having to use all this electronic stuff, so it’s just hard getting used to.” “I have a computer phone and it’s giving me the blues. I’m 85 years old. I like the old methods; I can’t write and stuff like that.” “My pastor says he doesn’t even know why I have a cell phone because I never answer it. But, I’m not married to it, you know, like some people.” |
|
|
| 5. Educate/Show me How | Yes, my grandchild helps me out with mine, with everything from my medication to his homework, to everything. If we get lost, … we use it.” Well they are easy to use (health apps) if somebody show me how to pull them up. I do not know how to pull them up. |
|
Corroboration |
Useful
Participants described their mobiles phone as useful for communication, text messaging, telephone communication and using other mobile applications such as the alarm clock, calendar, games for entertainment, and various activities such as browsing the Internet, using Google, looking up medications, and social networking sites such as Facebook.
Counterintuitive
Most participants described their smartphones as being “easy to use” but further discussions elicited that navigating, understanding, and using a smartphone device was counterintuitive. Redundant textual descriptions described how participants own a smartphone but struggle with trying to figure out how to best use the device. When asked, “How easy is a smartphone to use?”
“Charles stated: “If it’s just making calls, then it’s pretty easy. But when I get into messages and apps and all, that kind of thing, now sometimes it gets complicated. Yeah, hard as h*ll.”
Rosie stated, “It’s easy to me, yes. I’m not familiar with pulling up apps and doing a lots of things [sic]. Sometimes I make a mistake and turn my camera on, and it’ll be taking pictures of things around me. I’ve taken pictures of my feet” … “I have a lot. Some of the things, the problems I have is answering my phone. When it say [sic], people say tap it up and I lose my call because I’m not familiar with doing, rubbing it up. The swiping, you got it.”
Alexandra: Another statement, “Yeah, I guess, I’m just not used to it, you know. Um-hum. Or like the next steps, where to go from here? Yeah, yeah, it’s kinda confusing.”
Communication
A majority of participants expressed using their smartphones for means of communication either via telephone calls, or text messaging for those who are able to text. Only seven participants (ages 50–63, M = 57) stated they used their smartphones to communicate with health-care providers whereas all others preferred face-to-face interaction.
Comfortable with the Status Quo
From this theme, repeated excerpts showed participants being comfortable with the way things have always been with respect to telecommuting.
Charles stated, “It’s just, I guess it’s just all new. I spent most of my life without having all this electronic stuff, so it’s just hard getting used to.”
Sam stated, “It’s very easy. But I have found that it’s harder for probably older people to use it. Younger people, maybe it’s because the young people, their mind is fresher and the older people are kinda, do not like change, maybe. I think it’s easier for the younger people to get in there and go different places than it is for the older people.”
Educate/Show Me How
Participants expressed different levels of smartphone use and voiced their feelings and anxieties about their device. A recurrent theme that participants mentioned was needing someone to “show them how”. Whether it was a child or grandchild, this theme was identified from several participants.
Rosie described her experience with smartphones as, “But when it come to the smartphone, it’s a lot that I would love to learn, and I probably could learn more about my health on the phone. But mainly information, getting information, but I am dumb when it come to that. I have children and they haven't attempt [sic] to help me.”
Tutti stated: “I never had no one to show me how.”
Sally stated, “Yes, my grandchild helps me out with mine, with everything from my medication to his homework, to everything. If we get lost, you know, we use it.”
Data Integration
The quantitative and qualitative data were compared and contrasted for evidence of convergence, corroboration, and divergence. Table 6 is a “joint display”34 that shows evidence of the integration, corroboration, and the convergence-divergence of results and draws out new insights beyond the information from separate quantitative and qualitative results.44 We believe the results indicate Perceived Usefulness was confirmed by the qualitative evidence, however, Perceived Ease of Use was both confirmed by younger participants and disconfirmed by older participants. Behavioral Intention was present in younger participants and absent in older participants, thus data divergence was apparent when stratifying results by age (50–66 and 67–87). Through triangulation, integration of the construct adherence both converges and diverges with qualitative results that revealed new knowledge. Further exploration of these results is interpreted as a mean HBCHBPT scale score of 21 which is below the 22-cut score indicating at least 80% adherence with their HTN treatment regimen. However, the data diverges when participants were asked what app they would you like to see on their smartphone to assist them with their health. Only seven participants (23%) responded affirmatively, whereas most participants (76%) did not prefer to use an app to assist with their healthcare management. Adherence scores for these seven participants were between 15 and 22 (mean 18.7). The qualitative theme “comfortable with the status quo” aligns with adherence.
Discussion
The convergent parallel mixed method research design increases our knowledge of smartphone usage in rural older Black adults with HTN. In this pilot study, we sought to determine the feasibility of using mobile health application technology to manage high BP in rural Black older adults with HTN. During recruitment efforts, only one older Black male was recruited for the study. The primary reason for the underrepresentation of Black men was due to the heavy populace of Black women in the churches and community centers of this rural setting.
From the quantitative measures it is evident adherence to HTN treatment regimen and maintaining BP within normal limits is difficult. Almost half of participants had BP higher than the recommended BP of less than 130/80 mm Hg despite taking between one and five medications. Additionally, we believe the high BMI for 96.7% of participants contributes to sustained HTN. From the adherence measures the mean score of 21 for the HBCHBPT scale indicates the average number of participants are one point below the cut score of 22 indicating 80% compliance. However, this score has a SD of 4.98 with participants are above and below the 80% threshold within 5 points. From the K-Wood-MAS-4 the results showed only seven participants (23%) are highly adherent while 23 (76%) of participants are low adherers. Further research is needed to determine the accuracy of adherence in these two scales.
The five qualitative themes identified in this study were useful, counterintuitive, communication, comfortable with the status quo, and educate/show me how. While research studies of Blacks and technology-related research are lacking,45 our results are consistent with the results of Harmon Still et al46 in terms of nonacceptance of technology and using smartphones for social interactions such as communication and connecting with family and friends. Moreover, similar findings were found in the study by Harmon Still et al46 in being comfortable with the status quo. While there is a paucity of research with rural African Americans with hypertension and smartphone use, Senteio47 study of Community-Based Health Education Program to Promote African American Elders’ Use of Technology Designed to Support Chronic Disease Self-Management demonstrated commonalities with this study regarding younger adults assisting elders to use technology that parallels our study finding (theme) of educate/show me how. What is evident is the reality that older participants were used to analog technology in the digital age.
In terms of managing health, a smartphone is utilized by younger participants who can navigate the technology but rejected in older participants for a variety of reasons (limited knowledge, poor digital literacy and numeracy, concerns regarding lack of privacy and mistrust). Heiney et al48 successfully developed a smartphone app for managing heart failure in older African Americans. Thus, self-management of chronic conditions is possible if participants are willing and digitally literate.
Additional concerns were the loss of privacy/confidentiality. This is a known barrier to adoption of information technology for older adults.49 However, the use of a smartphone device is particularly important as declining mobility with age makes communication more important.49 Other benefits include game-based interventions that are known to improve cognitive abilities and preliminary evidence indicates that digital gameplay is associated with increased well-being in older adults.49,50
Implications
The findings of this pilot study revealed that in order for mobile app developers to create mobile apps that will aid in the management of chronic illness such as HTN for rural Black older adults with limited digital literacy, the user interface must be developed with simplicity. Rural older Black participants will require extensive education and training to be able to use smartphone technology unaided. Because cultural values and practices necessitate having eye contact with their health-care provider, developers may need to incorporate video chat features into mHealth apps. Importantly, while smartphones’ use is ubiquitous there are still persons who cannot use these devices with mastery and health-care providers need to assess for this knowledge deficit.
Additionally, these results provide data that will inform researchers of the potential use of mHealth apps to foster patient-provider communication, and self-management of HTN in older Black adults. Increasing the use of technology to foster self-management of chronic disease has implications for healthcare cost savings, improved patient engagement in health and well-being, and positive health outcomes.
As a major strength, this study underscores the need to simplify smartphone technology for older adults with limited digital literacy and numeracy. Limitations include the small sample size, geographical location, and inability to generalize to older adults in other settings. In addition, there was no comparison group to determine if findings were specific to age or rural location. Also, the overrepresentation of older women revealed self-selection bias of men who did not choose to participate in the study. Thus, the sample is not representative of all rural adults who may use smartphone technology to manage their HTN. Further research is needed to explore mHealth apps and smartphone technology in diverse older adult populations and settings.
Conclusion
Smartphone technology and other health-related computer technologies were not preferred by older adults in this study due to limited digital literacy. The steep learning curve associated with smartphone apps was difficult for older adults to master. Simplicity and easy navigation in the design of mHealth apps for smartphones are needed to improve treatment adherence and BP control in rural older adults with HTN.
Acknowledgments
This study was funded by a grant from The Office of Research and Scholarship at The University of Texas at Tyler. The authors wish to thank the participants of this study.
Disclosure
The authors declare they have no conflict of interest.
References
- 1.Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update. Circulation. 2021;143(8):e254–e743. doi: 10.1161/cir.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 2.Thomas SJ, Booth JN, Dai C, et al. Cumulative incidence of hypertension by 55 years of age in Blacks and Whites: the Cardia study. J Am Heart Assoc. 2018;7(14). doi: 10.1161/jaha.117.007988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/apha/ash/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6). doi: 10.1161/hyp.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 4.Muntner P, Anstey DE. Social determinants of health: past, current, and future threats to hypertension and blood pressure control. Am J Hypertens. 2021;34(7):680–682. doi: 10.1093/ajh/hpab023 [DOI] [PubMed] [Google Scholar]
- 5.Commodore-Mensah Y, Turkson-Ocran R-A, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens. 2021;34(7):707–717. doi: 10.1093/ajh/hpab011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carter B, Dean O. Rural–urban health disparities among US adults ages 50 and older. Washington, DC: AARP Public Policy Institute; 2021. doi: 10.26419/ppi.00151.001 [DOI] [Google Scholar]
- 7.Coke LA, Hayman LL. Rural health. J Cardiovasc Nurs. 2020;35(5):E11–E14. doi: 10.1097/jcn.0000000000000730 [DOI] [PubMed] [Google Scholar]
- 8.Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR Mhealth Uhealth. 2017;5(2):e9. doi: 10.2196/mhealth.6630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS. Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis. Curr Hypertens Rep. 2015;17(12):94. doi: 10.1007/s11906-015-0606-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lv J, Neal B, Ehteshami P, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS Med. 2012;9(8):e1001293. doi: 10.1371/journal.pmed.1001293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruppar TM, Dunbar-Jacob JM, Mehr DR, Lewis L, Conn VS. Medication adherence interventions among hypertensive Black adults: a systematic review and meta-analysis. J Hypertens. 2017;35(6):1145–1154. doi: 10.1097/HJH.0000000000001260 [DOI] [PubMed] [Google Scholar]
- 12.Alessa T, Abdi S, Hawley MS, de Witte L. Mobile apps to support the self-management of hypertension: systematic review of effectiveness, usability, and user satisfaction. JMIR Mhealth Uhealth. 2018;6(7):e10723. doi: 10.2196/10723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jamaladin H, van de Belt TH, Luijpers LC, et al. Mobile apps for blood pressure monitoring: systematic search in app stores and content analysis. JMIR Mhealth Uhealth. 2018;6(11):e187. doi: 10.2196/mhealth.9888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li R, Liang N, Bu F, Hesketh T. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020;8(3):e17776. doi: 10.2196/17776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu H, Long H. The effect of smartphone app-based interventions for patients with hypertension: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020;8(10):e21759. doi: 10.2196/21759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams ZW, Sieverdes JC, Brunner-Jackson B, et al. Meditation smartphone application effects on prehypertensive adults’ blood pressure: dose-response feasibility trial. Health Psychol. 2018;37(9):850–860. doi: 10.1037/hea0000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar N, Khunger M, Gupta A, Garg N. A content analysis of smartphone-based applications for hypertension management. J Am Soc Hypertens. 2015;9(2):130–136. doi: 10.1016/j.jash.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 18.Pew Research Center. Smartphone ownership is growing rapidly around the world, but not always equally. Available from: http://www.pewglobal.org/2019/02/05/smartphone-ownership-is-growing-rapidly-around-The-world-but-not-always-equally/. Accessed February 1, 2022..
- 19.Mamedova S, Pawlowski E. U. S. Department of Education, American Institutes for Research. A description of U. S. adults who are not digitally literate. Stats in Brief, NCES-2018-161; 2018. Available from: https://nces.ed.gov/pubs2018/2018161.pdf. Accessed August 9, 2022. [Google Scholar]
- 20.Council of Economic Advisers. Mapping the Digital Divide. Washington, DC: Executive Office of the President of the United States; 2015. [Google Scholar]
- 21.Kontos EZ, Emmons KM, Puleo E, Viswanath K. Communication inequalities and public health implications of adult social networking site use in the United States. J Health Commun. 2010;15(Suppl3):216–235. doi: 10.1080/10810730.2010.522689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Powe BD. Health information seeking among rural African Americans, Caucasians, and Hispanics: it is built, did they come? Nurs Clin North Am. 2015;50(3):531–543. doi: 10.1016/j.cnur.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 23.Robbins R, Krebs P, Jagannathan R, Jean-Louis G, Duncan DT. Health app use among US mobile phone users: analysis of trends by chronic disease status. JMIR Mhealth Uhealth. 2017;5(12):e197. doi: 10.2196/mhealth.7832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferdinand KC, Yadav K, Nasser SA, et al. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J Clin Hypertens. 2017;19(10):1015–1024. doi: 10.1111/jch.13089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quart. 1989;13(3):319–340. doi: 10.2307/249008 [DOI] [Google Scholar]
- 26.Mohamed AH, Tawfik H, Al-Jumeily D, Norton L. MoHTAM: a technology acceptance model for mobile health applications. In: Developments in E-Systems Engineering (DESE). Dubai, United Arab Emirates; 2011:13–18. doi: 10.1109/DeSE.2011.79 [DOI] [Google Scholar]
- 27.Castro FG, Coe K. Traditions and alcohol use: a mixed-methods analysis. Cultur Divers Ethnic Minor Psychol. 2007;13(4):269–284. doi: 10.1037/1099-9809.13.4.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Merriam-Webster. Merriam-Webster.com dictionary. Available from: https://www.merriam-webster.com. Accessed March 1, 2021.
- 29.Fishbein M, Ajzen I. Belief, Attitude, Intention and Behavior: An Introduction to Theory and Research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- 30.World Health Organization. Adherence to long-term therapies: evidence for action/[edited by Eduardo Sabaté]. World Health Organization; 1970. Available from: https://apps.who.int/iris/handle/10665/42682. Accessed February 1, 2022. [Google Scholar]
- 31.Castro FG, Nieri T. Culturally-Sensitive Research: Emerging Approaches in Theory, Measurement and Methods for Effective Research on Acculturation, Ethnic Identity and Gender. Washington, DC: Meeting of the Society for Social Work Research; 2008. [Google Scholar]
- 32.Krousel-Wood M, Peacock E, Joyce C, et al. A hybrid 4-item Krousel-Wood Medication Adherence Scale predicts cardiovascular events in older hypertensive adults. J Hypertens. 2019;37(4):851–859. doi: 10.1097/hjh.0000000000001955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy scale. Prog Cardiovasc Nurs. 2000;15(3):90–96. doi: 10.1111/j.1751-7117.2000.tb00211.x [DOI] [PubMed] [Google Scholar]
- 34.Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 5th ed. Sage Publications; 2018. [Google Scholar]
- 35.About adult BMI. Centers for Disease Control and Prevention; 2021. Available from: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/. Accessed February 1, 2022.
- 36.Hendrickson AR, Massey PD, Cronan TP. On the test-retest reliability of perceived usefulness and perceived ease of use scales”. MIS Quart. 1993;17(2):227–230. doi: 10.2307/249803 [DOI] [Google Scholar]
- 37.Yoon H-Y. User acceptance of mobile library applications in academic libraries: an application of the technology acceptance model. J of Acad Librar. 2016;42(6):687–693. doi: 10.1016/j.acalib.2016.08.003 [DOI] [Google Scholar]
- 38.Lincoln YS, Guba EG. Naturalistic Inquiry. Sage Publications; 1985. [Google Scholar]
- 39.Guba EG, Lincoln YS. Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. 2nd ed. Sage Publications; 1994:105–117. [Google Scholar]
- 40.VERBI Software. MAXQDA 2020 [computer software]. Berlin, Germany: VERBI Software; 2019. Available from https://www.maxqda.com. Accessed August 9, 2022. [Google Scholar]
- 41.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res in Psych. 2006;3:77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 42.Thorne S. Interpretive Description. Left Coast Press, Inc; 2008. [Google Scholar]
- 43.Wang-Schweig M, Kviz FJ, Altfeld SJ, Miller AM, Miller BA. Building a conceptual framework to culturally adapt health promotion and prevention programs at the deep structural level. Health Promot Pract. 2014;15(4):575–584. doi: 10.1177/1524839913518176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guetterman TC, Fetters MD, Creswell JW. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann Fam Med. 2015;13(6):554–561. doi: 10.1370/afm.1865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.James DC, Harville C 2nd, Sears C, Efunbumi O, Bondoc I. Participation of African Americans in e-health and m-health studies: a systematic review. Telemed J E Health. 2017;23(5):351–364. doi: 10.1089/tmj.2016.0067 [DOI] [PubMed] [Google Scholar]
- 46.Harmon Still C, Jones LM, Moss KO, Variath M, Wright KD. African American older adults’ perceived use of technology for hypertension self-management. Res Gerontol Nurs. 2018;11(5):249–256. doi: 10.3928/19404921-20180809-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Senteio CR. Investigating the enduring impact of a community-based health education program to promote African American elders’ use of technology designed to support chronic disease self-management. Geriatrics. 2018;3(4):70. doi: 10.3390/geriatrics3040070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heiney SP, Donevant SB, Arp Adams S, Parker PD, Chen H, Levkoff S. A smartphone app for self-management of heart failure in older African Americans: feasibility and usability study. JMIR Aging. 2020;3(1):e17142. doi: 10.2196/17142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Charness N, Boot WR. Chapter 20 - Technology, gaming, and social networking. In: Schaie KW, Willis SL, editors. Handbook of the Psychology of Aging. 8th ed. Academic Press/Elsevier; 2016:389–407. [Google Scholar]
- 50.Allaire JC, McLaughlin AC, Trujillo A, Whitlock LA, LaPorte L, Gandy M. Successful aging through digital games: socioemotional differences between older adult gamers and non-gamers. Comput Human Behav. 2013;29(4):1302–1306. doi: 10.1016/j.chb.2013.01.014 [DOI] [Google Scholar]