Abstract
Adolescent internalizing symptoms have increased since 2010, whereas adequate sleep has declined for several decades. It remains unclear how self-reported sleep attainment has affected internalizing-symptoms trends. Using 1991–2019 data from the Monitoring the Future Study (n ~ 390,000), we estimated age-period-cohort effects in adolescent internalizing symptoms (e.g., loneliness, self-esteem, self-derogation, depressive affect) and the association with yearly prevalence of a survey-assessed, self-reported measure of attaining ≥7 hours of sleep most nights. We focused our main analysis on loneliness and used median odds ratios to measure variance in loneliness associated with period differences. We observed limited signals for cohort effects and modeled only period effects. The feeling of loneliness increased by 0.83% per year; adolescents in 2019 had 0.68 (95% CI: 0.49, 0.87) increased log odds of loneliness compared with the mean, which was consistent by race/ethnicity and parental education. Girls experienced steeper increases in loneliness than boys (P < 0.0001). The period-effect median odds ratio for loneliness was 1.16 (variance = 0.09; 95% CI: 0.06, 0.17) before adjustment for self-reported frequency of getting ≥7 hours sleep versus 1.07 (variance = 0.02; 95% CI: 0.01, 0.03) after adjustment. Adolescents across cohorts are experiencing worsening internalizing symptoms. Self-reported frequency of <7 hours sleep partially explains increases in loneliness, indicating the need for feasibility trials to study the effect of increasing sleep attainment on internalizing symptoms.
Keywords: adequate sleep, adolescents, age-period-cohort effects, internalizing symptoms
Abbreviations
- APC
age-period-cohort
- CI
confidence interval
- HAPC
hierarchical age-period-cohort
- MOR
median odds ratio
- MTF
Monitoring the Future
Adolescent depression (1, 2), major depressive disorder (3), and suicide-related behavior (4–9) have increased in the United States since the 2000s. Core to depressive disorders and suicidal behavior is disruption of sense of self and self-worth, both of which are quintessential to internalizing symptoms (10)—thoughts, feelings, and behavior indicative of anxiety and depression, social withdrawal, and somatic complaints (11). Examples include loneliness, low self-esteem, high-self derogation, and depressive affect. Loneliness, described as disparity between desired and experienced social network quantity or quality (12), is associated with physical and mental health disorders (13) and substance use (14). Loneliness is common during adolescence (13) and has detrimental effects on social inclusion (15) and academic achievement (16).
Evaluating internalizing-symptoms trends is critical for establishing root causes and designing targeted interventions. Population distributions of mental health disorders can vary across 3 dimensions of time: age, period, and cohort. Data from 1991–2010 from US, Canadian, and UK age-period-cohort (APC) studies indicate that cohort and period effects explained variation in population mental health and psychological distress (17, 18). Yet the landscape of mental health has shifted in the past decade. Findings thus far indicate that incidence of adolescent depression and self-harm has increased since approximately 2010 (1, 3, 4, 19), suggesting that APC studies are needed to understand related adolescent mental health outcomes such as internalizing symptoms.
One potential risk factor that may influence internalizing-symptoms trends is adolescent sleep. Between 2009 and 2015, the percentage of adolescents reporting less than 7 hours of sleep most nights increased by 16%–17% (20). Inadequate sleep is associated with many adverse adolescent social and health outcomes, including increased body mass index (21), weaker academic performance (22), reckless behavior (23), poorer mental health (24), and substance use (25). Inadequate sleep is also associated with mood dysregulation through many pathways, including metabolic dysfunction and increased cortisol production (26). Internalizing symptoms, particularly loneliness, are associated with sleep disturbance (13, 27) and poorer sleep efficiency (28, 29). Moreover, sleep disruption is both a predictor (30–32) and result (30, 33) of poor mental health, suggesting that sleep is an important indicator across mental health outcomes, including loneliness.
In previous APC studies of mental health, researchers have also demonstrated that broad societal changes affect different demographic groups heterogeneously. For example, period effects on psychological distress in 1997–2011 generally affected individuals of low socioeconomic status more than other socioeconomic groups (18), and suicide risk in 1983–2012 increased in Black Americans at much younger ages than in White Americans (34). Increases in mental health disorders are greater in girls than boys (35), suggesting that APC effects observed may be more concentrated among girls. However, the extent to which recent mental health trends may affect certain adolescent groups disproportionately does not appear to have been systematically investigated.
To our knowledge, no study has directly examined APC effects of internalizing symptoms among US adolescents. Although sleep is an important indicator of mental health (13, 24, 27–29), its influence on internalizing symptoms has not been systematically evaluated. Thus, in the present study, we used data (1991–2019) from the Monitoring the Future (MTF) Study to estimate hierarchical APC (HAPC) effects to deconstruct population-level APC effects of adolescent internalizing symptoms. We focused our main analysis on loneliness, given its centrality to adolescent mental health, and examined consistency across additional outcomes of internalizing problems (namely, self-derogation, self-esteem, and depressive affect). We conducted subgroup analyses of APC effects of loneliness by sex, race/ethnicity, and parental education to compare with trends reported in other studies (17–19, 34–38). We then tested whether observed APC effects of loneliness are explained by trends in self-reported sleep attainment of at least 7 hours on most nights.
METHODS
Sample
MTF includes annually administered cross-sectional surveys of 8th, 10th, and 12th graders in the contiguous United States. Approximately 420 US public and private high schools are selected using a multistage random sampling design (n = 350 students per school maximum). Selected schools are invited to participate for 2 years, and those that decline are replaced. Self-administered questionnaires are given to students, typically in classroom settings with a teacher present. Teachers are instructed to avoid close proximity to the students during administration to ensure students can respond confidentially. For this study, we used cross-sectional data collected annually between 1991 and 2019. Student response rates within schools ranged from 79% (12th grade in 2008) to 91% (8th grade in 1996, 2002, 2006, 2007, 2011, and 2012), with most nonresponses due to absence (39, 40). Detailed descriptions of the MTF Study are provided elsewhere (39, 41). We used sample weights provided by MTF researchers in all calculations that reflect multistage sampling design and generate nationally representative estimates. Institutional review board approval was obtained for this study from the University of Michigan and Columbia University.
MTF surveys comprise a core form given to all students and other randomly assigned forms; we focused on students who received forms that included questions regarding internalizing symptoms and self-reported sleep attainment of at least 7 hours on most nights. We highlighted the effects of loneliness in our main analysis because loneliness is a core facet of mental health, but we extended our analyses to include other internalizing symptoms to assess consistency. The maximum sample size for analyses of loneliness was 229,346 (n = 105,752 8th graders, 113,995 10th graders, and 9,599 12th graders). Sample sizes for subgroup analyses of loneliness (by sex, race/ethnicity, and parental education) ranged from 23,953 to 154,761, and sample sizes for other internalizing symptoms (namely, low self-esteem, high self-derogation, and depressive affect) ranged from 370,570 to 389,443. Nonresponse rates for covariates were low, with the highest missingness pertaining to the depressive affect measure (14.32%). Students with missing data were not included in the analysis. Those with missing data were slightly different than those with complete data on measured demographics, with the largest differences pertaining to age: 85.26% of students at least 18 years old were missing from the full-sample loneliness HAPC models (Web Table 1) (available at https://doi.org/10.1093/aje/kwac010).
Measures
Internalizing symptoms.
Students were asked how much they agree or disagree with statements related to each symptom. Three items measured loneliness: “A lot of times I feel lonely. I often feel left out of things. I often wish I had more good friends.” Four items measured self-esteem: “I take a positive attitude toward myself. I feel I am a person of worth, on an equal plane with others. I am able to do things as well as most other people. On the whole, I’m satisfied with myself.” Four items measured self-derogation: “I feel I do not have much to be proud of. Sometimes I think that I am no good at all. I feel that I can’t do anything right. I feel that my life is not very useful.” Four items measured depressive affect: “Life often seems meaningless. The future often seems hopeless. I enjoy life as much as anyone. It feels good to be alive.” Response options for each statement were on a Likert scale (disagree, mostly disagree, neither, mostly agree, agree), and items within each internalizing symptom category were averaged to create 1 item. Cronbach α value ranged from 0.68 (for loneliness in 1991) to 0.89 (for self-derogation in 2017), averaged across grades, and findings from previous studies suggest construct validity (42, 43).
Substance use.
We dichotomized past-year frequency of substance use into no use versus any use (≥1 occasion) in 3 separate variables measuring alcohol, cannabis, and other substance use. For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine in the “other substance use” category. For 8th and 10th graders, we did not include heroin, narcotics, or sedatives.
Self-reported attainment of at least 7 hours of sleep.
Students were asked, “During the last 12 months, how often do you…get at least seven hours of sleep? (never, seldom, sometimes, most days, nearly every day, every day).” For APC analysis, we calculated the percentage of students who slept at least 7 hours nearly every day of every day in each survey year and assigned this percentage to participants surveyed that year (period-level self-reported frequency of attaining ≥7 hours of sleep). We ran sensitivity analyses to explore what impact the categorization of frequency had on the study results; there was no evidence that a different categorization led to different results. For example, categorizing “most days” with “nearly every day/every day” led to similar findings (Web Figure 1). We did not include individual-level self-reported frequency of attaining at least 7 hours of sleep in the models, because it is in the pathway between period and cohort-level self-reported frequency of attaining at least 7 hours of sleep and internalizing symptoms trends.
Age, period, and birth cohort.
Age was measured in calendar years on the basis of self-reported birth year and month and was categorized as 2-year age groups up to age 18 years: 10–11, 12–13, 14–15, 16–17 years; the last age category included participants 18 years or older. Birth cohort was calculated as survey year (i.e., period) minus age.
Sociodemographics and other covariates.
Other self-reported measures included were sex (male vs. female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other race or ethnicity), grade point average (B– or less vs. B or higher), parental education (either parent had some college or less vs. completed college or more, reported by the adolescent). Tablet data collection was introduced for subsamples of students in 2019, and an analysis of paper implementation for data collection had higher odds of missingness of internalizing measures than did tablet implementation (e.g., for loneliness measure, odds ratio = 0.42; 95% confidence interval (CI): 0.34, 0.51). Thus, we included survey mode (paper vs. tablet) in our models.
Analysis
Descriptive analyses assessed means and frequencies by study year. We then conducted APC analysis, which historically has been difficult because of the fundamental correlation among cohort, period, and age (cohort = period – age) (44). HAPC models circumvent this identification problem by using random effects on periods and cohorts and fixed effects on individual-level covariates, such as age and other sociodemographic variables. The level-1 model is  , where the mean loneliness score for respondent i in period j and cohort k is a function of age and
, where the mean loneliness score for respondent i in period j and cohort k is a function of age and  that contains p other individual-level covariates;
that contains p other individual-level covariates;  is the mean loneliness score for the reference group surveyed in period j and belonging to cohort k;
is the mean loneliness score for the reference group surveyed in period j and belonging to cohort k;  is an error term following a normal distribution with mean 0 and variance
is an error term following a normal distribution with mean 0 and variance  (44–49). In the level-2 model,
(44–49). In the level-2 model,  ,
,  is the mean loneliness measure averaged across all periods and cohorts;
is the mean loneliness measure averaged across all periods and cohorts;  is the residual effect of period j averaged over all cohorts, which has a normal distribution with mean 0 and variance
is the residual effect of period j averaged over all cohorts, which has a normal distribution with mean 0 and variance  ;
;  is the residual effect of cohort k averaged over all periods and has a normal distribution with mean 0 and variance
is the residual effect of cohort k averaged over all periods and has a normal distribution with mean 0 and variance  (44–49). We used the HAPC formula as specified by Yang and Land (49). Although there are numerous potential models that allow for estimation of APC effects, HAPC models efficiently estimate unique parameters with a minimum of assumptions about the underlying processes, and more advanced HAPC models also enable assessment of covariates’ contributions in explaining observed age-period effects (44–49). Because of these and other advantages, HAPC models are increasingly commonly used in studies (50–56).
(44–49). We used the HAPC formula as specified by Yang and Land (49). Although there are numerous potential models that allow for estimation of APC effects, HAPC models efficiently estimate unique parameters with a minimum of assumptions about the underlying processes, and more advanced HAPC models also enable assessment of covariates’ contributions in explaining observed age-period effects (44–49). Because of these and other advantages, HAPC models are increasingly commonly used in studies (50–56).
Web Figures 2–5 depict period and cohort effects of adolescent internalizing symptoms analyzed in this study. Interpretation of period and cohort effects are as follows: the period effect denotes the overall change across survey years averaged across cohorts, controlling for age and other covariates in X, and the cohort effect denotes the change across cohorts averaged across survey years, controlling for age and other covariates in X, which contains p other individual-level covariates (57). When model building in HAPC analysis, one typically evaluates the inclusion of APC effects by examining change in model fit given inclusion of each component (57–59). In the models in the present study, there was no meaningful contribution of birth cohort to trends in internalizing symptoms. Therefore, the final HAPC models included age and period effects only. Although there may be cohort effects of high self-derogation (Web Figure 3), the variations between cohorts are relatively small compared with period effects.
We estimated hierarchical age and period models of loneliness, low self-esteem, high self-derogation, and depressive affect, adjusting for age, sex, race/ethnicity, parental education, grade point average, past-year alcohol/cannabis/other substance use, and survey mode. Adjusting for grade instead of age did not change our results. We also conducted stratified analyses for loneliness by sex, race/ethnicity, and parental education, adjusting for all other aforementioned sociodemographic variables. Next, we added period-level self-reported frequency of attaining at least 7 hours of sleep as another predictor to understand if period-level trends in self-reported frequency of that much sleep explained age-period effects of loneliness. Analyses were conducted in SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina) (60), and graphs were created in ggplot2 (61) in R (R Foundation for Statistical Computing, Vienna, Austria).
Moreover, we calculated median odds ratios (MORs) to quantify the variation between periods (62). MOR is interpreted as the odds ratio of loneliness between 2 individuals who have the same individual-level covariates but are in different periods; the MOR is always at least 1 (62, 63). Therefore, a MOR > 1 indicates that 2 individuals from different periods are more likely to be have different loneliness measures; increasing MOR suggests more variation between periods. We used the variance parameter estimate from the hierarchical age and period models and the following formula: MOR =  (62).
(62).
To test the robustness of our main HAPC results for loneliness, we conducted a sensitivity analysis using the intrinsic estimator approach for estimating APC effects (44, 64), which has been implemented in other studies (18, 44, 65). Using this method, we estimated coefficients for APC effects that represent the mean change in loneliness for specific APC groups relative to the overall mean for all APC groups combined (44, 64). We excluded students younger than 12 and older than 20 years of age, because of small cell sizes. Modeling was conducted using the “apc_ie” command in the “apc” Stata package (StataCorp LP, College Station, Texas) (64, 66).
RESULTS
Between 1991 and 2019, we observed a 20.0% increase in adolescents reporting they mostly agree/agree with survey items measuring loneliness (18.5% in 1991 vs. 22.2% in 2019), with the lowest rates of loneliness in 2008 (13.6%) (Figure 1). Self-reported adequate sleep attainment simultaneously decreased: 33.5% of adolescents reported sleeping at least 7 hours in 2019, a 40.6% decrease from 56.4% in 1991 (Figure 1).
Figure 1.
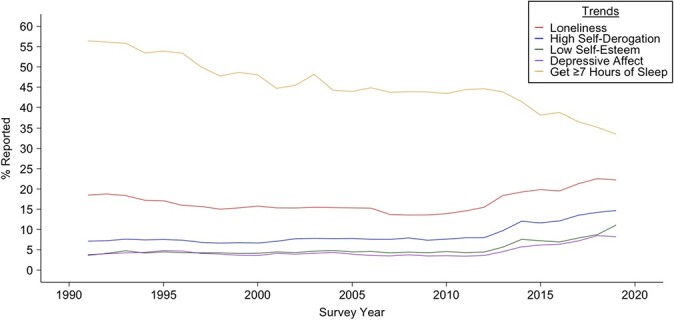
Trends in loneliness, high self-derogation, low self-esteem, depressive affect, and self-reported frequency of attaining ≥7 hours of sleep nearly every day or every among 8th, 10th, and 12th graders in the Monitoring the Future Study (1991–2019). Trends in internalizing symptoms represent the prevalence of students who mostly agreed or agreed with measures composing each scale, respectively. Trends in sleeping ≥7 hours nearly every day or every day are based on responses for the entire sample of students who answered the question (for loneliness, n = 231,867; for high self-derogation, n = 391,655; for low self-esteem, n = 393,301; for depressive affect, n = 374,249; for sleep, n = 385,557). Weighted responses were used for all trends.
Figure 2 provides estimates of the period effect on loneliness. We observed a U-shaped curve after adjusting for sex, race/ethnicity, parental education, grade point average, past-year cannabis/alcohol/other drug use, and survey mode. The log odds of loneliness were 0.68 (95% CI: 0.49, 0.87) higher for adolescents in 2019 compared with the overall mean, but adolescents in 1991 had 0.45 (95% CI: 0.32, 0.58) higher log odds compared with the overall mean, with the lowest log odds observed in 2010 (–0.43, 95% CI: –0.57, –0.28). Subgroup analyses by sex, race/ethnicity, and parental education also generally exhibited a U-shaped period effect (Web Figures 6–8). However, girls experienced steeper increases in loneliness than did boys from 2013 onward (P < 0.0001) (Web Figure 6, Web Table 2).
Figure 2.
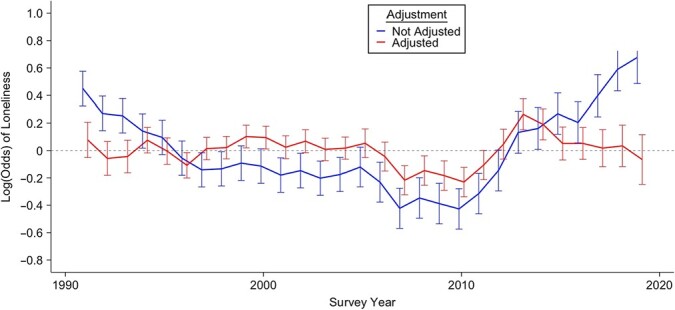
Hierarchical age-period estimates of period effects of loneliness among 8th, 10th, and 12th graders in the Monitoring the Future Study (1991–2019), with and without adjustment for self-reported frequency of attaining ≥7 hours of sleep nearly every day or every day. Models were also adjusted for sex (male vs. female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other races or ethnicities), parental education (either parent had some college or less vs. completed college or more, as reported by the adolescent), grade point average (B– or less vs. B or higher), survey implementation technique (paper vs. tablet), and past-year cannabis/alcohol/other drug use. Drugs in the “other substance use” category varied by grade: For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine. We did not include heroin, narcotics, or sedatives for 8th and 10th graders (n = 229,346).
Web Figures 9–11 graph period effects of high self-derogation, low self-esteem, and depressive affect (after adjustment for the aforementioned covariates). Adolescents in 2019 had higher log odds of these internalizing symptoms than did adolescents in 1991. For example, adolescents in 2019 had a 1.27 (95% CI: 1.08, 1.45) increase in log odds of depressive affect compared with the overall mean, but adolescents in 1991 had a –0.15 (95% CI: –0.32, 0.02) increase in log odds compared with the overall mean (Web Figure 11), with similar values observed for high self-derogation and low self-esteem (Web Figure 9–10).
Table 1 provides the MORs for the period effect on loneliness, overall and by subgroup. The period-effect MOR for feelings of loneliness was 1.16 (variance = 0.09; 95% CI: 0.06, 0.17), denoting that 2 individuals with the same level of covariates are 1.16 times as likely to have different levels of loneliness if they were from different periods (i.e., birth cohorts) (Table 1). Subgroup analyses by race/ethnicity and parental education yielded similar MORs. However, by sex, MOR was 1.22 among girls and 1.13 among boys.
Table 1.
Median Odds Ratio for the Hierarchical Age-Period Estimates of Period Effects of Loneliness Among 8th, 10th, and 12th Graders in the Monitoring the Future Study, 1991–2019a
| Not Adjusting for Self-Reported Frequency of Attaining ≥7 Hours of Sleep Nearly Every Day or Every Day | Adjusting for Self-Reported Frequency of Attaining ≥7 Hours of Sleep NearlyEvery Day or Every Day | |||||
|---|---|---|---|---|---|---|
| Subgroup | Variance Parameter Estimate | 95% CI | MOR | Variance Parameter Estimate | 95% CI | MOR |
| Overall | 0.091 | 0.057, 0.171 | 1.157 | 0.015 | 0.009, 0.032 | 1.066 |
| Sex | ||||||
| Girls | 0.175 | 0.109, 0.328 | 1.223 | 0.044 | 0.026, 0.092 | 1.114 |
| Boys | 0.058 | 0.035, 0.113 | 1.126 | 0.014 | 0.008, 0.031 | 1.065 |
| Race/ethnicity | ||||||
| Black | 0.062 | 0.035, 0.138 | 1.142 | 0.013 | 0.006, 0.059 | 1.082 |
| White | 0.094 | 0.058, 0.178 | 1.161 | 0.019 | 0.011, 0.042 | 1.076 |
| Hispanic | 0.119 | 0.070, 0.248 | 1.194 | 0.028 | 0.013, 0.092 | 1.110 |
| Other race or ethnicity | 0.096 | 0.056, 0.207 | 1.176 | 0.003 | 0.001, 36.648 | 1.068 |
| Parental education | ||||||
| Less than college | 0.122 | 0.074, 0.235 | 1.187 | 0.02 | 0.011, 0.048 | 1.081 |
| College or more | 0.076 | 0.047, 0.146 | 1.144 | 0.016 | 0.009, 0.037 | 1.071 |
Abbreviations: CI, confidence interval; MOR, median odds ratio.
a MORs were interpreted as the odds ratio of the internalizing symptoms between 2 individuals who have the same individual-level covariates but in different periods or cohorts. Therefore, a larger period (cohort) MOR indicates that 2 individuals with different loneliness measures are more likely to be from different periods (i.e., birth cohorts), suggesting stronger period (cohort) effects. Models also were adjusted for sex (male vs. female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other race or ethnicity), parental education (either parent had some college or less vs. completed college or more, as reported by the adolescent), grade point average (B– or less vs. B or higher), survey implementation technique (paper vs. tablet), and past-year cannabis/alcohol/other drug use. Drugs in the “other substance use” category varied by grade: For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine. For 8th and 10th graders, we did not include heroin, narcotics, or sedatives.
We then examined whether period-specific trends in self-reported frequency of attaining at least 7 hours of sleep explained period effects of loneliness in adolescents. After controlling for period-level self-reported frequency of sleeping at least 7 hours, we found that period effects produced a more attenuated signal (Figure 2), which was fairly consistent by race/ethnicity and parental education (Figures 3–5). However, the extent to which self-reported frequency of attaining at least 7 hours of sleep explained period effects varied by sex: Loneliness increased in girls in the early 2010s and peaked in 2013, whereas the period effect in boys remained stagnant (Figure 3).
Figure 3.
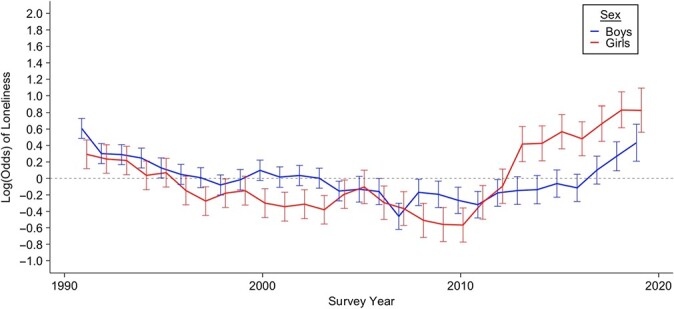
Hierarchical age-period estimates, by sex, of period effects of loneliness among 8th, 10th, and 12th graders in the Monitoring the Future Study (1991–2019), adjusted for self-reported frequency of attaining ≥7 hours of sleep nearly every day or every day. The model also was adjusted for race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other races or ethnicities), parental education (either parent had some college or less vs. completed college or more, as reported by the adolescent), grade point average (B– or less vs. B or higher), survey implementation technique (paper vs. tablet), and past-year cannabis/alcohol/other drug use. Drugs in the “other substance use” category varied by grade: For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine. We did not include heroin, narcotics, or sedatives for 8th and 10th graders (girls: n = 120,420; boys: n = 108,926).
Figure 5.
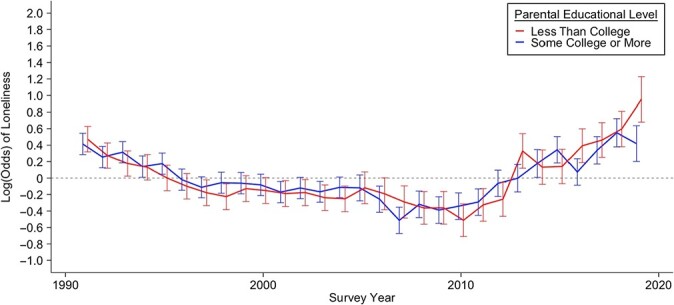
Hierarchical age-period estimates, by parental education, of period effects of loneliness among 8th, 10th, and 12th graders in the Monitoring the Future Study (1991–2019), adjusted for self-reported frequency of attaining ≥7 hours of sleep nearly every day or every day. The models also were adjusted for sex (male vs. female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other races or ethnicities), grade point average (B– or less vs. B or higher), survey implementation technique (paper vs. tablet), and past-year cannabis/alcohol/other drug use. Drugs in the “other substance use” category varied by grade: For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine. We did not include heroin, narcotics, or sedatives for 8th and 10th graders (parental education is less than college, n = 102,629; for parental education is college or more, n = 126,717).
Figure 4.
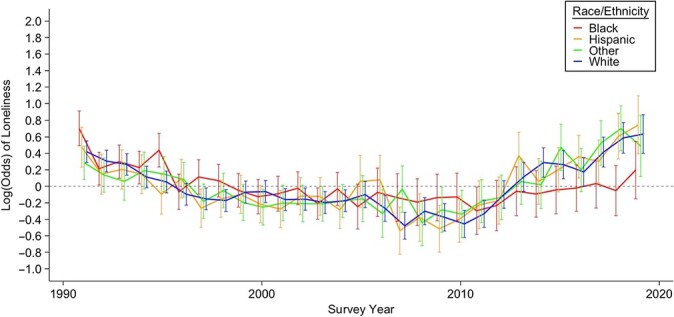
Hierarchical age-period estimates, by race/ethnicity, of period effects of loneliness among 8th, 10th, and 12th graders in the Monitoring the Future Study (1991–2019), adjusted for self-reported frequency of attaining ≥7 hours of sleep nearly every day or every day. The model also was adjusted for sex (male vs. female), parental education (either parent had some college or less vs. completed college or more, as reported by the adolescent), grade point average (B– or less vs. B or higher), survey implementation technique (paper vs. tablet), and past-year cannabis/alcohol/other drug use. Drugs in the “other substance use” category varied by grade: For 12th graders, we included lysergic acid diethylamide, other hallucinogens, cocaine, amphetamines, sedatives, tranquilizers, heroin, narcotics, crack, and other forms of cocaine. We did not include heroin, narcotics, or sedatives for 8th and 10th graders (Black students, n = 23,953; White students, n = 154,761; Hispanic students, n = 24,029; students of other races or ethnicities, n = 26,603).
The MOR adjusted for self-reported frequency of attaining at least 7 hours of sleep can be compared with the MOR before adjustment to assess how much variation in loneliness is explained by period-specific self-reported frequency of sleeping at least 7 hours (Table 1). The period-effect MOR for feelings of loneliness decreased from 1.16 before adjustment to 1.07 after adjustment (variance = 0.02; 95% CI: 0.01, 0.03), suggesting again that period-specific self-reported frequency of getting at least 7 hours of sleep is explaining a substantial proportion of the period-specific trends in loneliness (Table 1). Similarly, subgroup analyses race/ethnicity and parental education yielded lower period-effect MORs across all groups. However, slight differences in MOR were still observed by sex even after adjusting for self-reported frequency of attaining at least 7 hours of sleep: MOR was still higher among girls (MOR = 1.1; variance = 0.04; 95% CI: 0.03, 0.09) than boys (MOR = 1.07; variance = 0.01; 95% CI: 0.01, 0.03).
Sensitivity analysis.
The sensitivity analysis using the intrinsic estimator approach revealed a U-shaped period effect of loneliness (Web Figure 12) consistent with the observed period effects from the HAPC models. However, compared with results from the HAPC model of loneliness (Web Figure 2), the intrinsic estimator revealed a slight decreasing cohort effect among recent birth cohorts. Differences between the HAPC and intrinsic estimator approach are likely the result of excluding students younger than 12 and older than 20 years, because of small cell sizes; we have presented both for the reader to note that these models are sensitive to model assumptions.
DISCUSSION
We used nationally representative data of US adolescents in this study and documented that increases in internalizing symptoms after 2010 are driven by period effects. Thus, adolescents are experiencing worsening internalizing symptoms across cohorts, which form crucial building blocks for adolescent mental health (12, 67–69).
Period effects in loneliness are partially explained by self-reported frequency of attaining at least 7 hours of sleep, consistent with the hypothesis that inadequate self-reported sleep attainment may be associated with increasing loneliness among adolescents. Specifically, trends in internalizing symptoms could result from sleep being an indicator of mood disturbances (30), which may contribute to greater social isolation and feelings of loneliness. In prior studies, researchers found similar links between sleep quality and loneliness (13, 27, 70). Although we did not measure sleep quality in this study, in future studies, researchers may incorporate more nuanced measures of sleep to inform our understanding of adolescent mental health trends. Observed APC effects in self-reported frequency of attaining at least 7 hours of sleep may intersect with other trends. For instance, in a study in Hong Kong, researchers found that older age at menarche, an important indicator of female puberty, is associated with longer sleep duration (≥9 hours) (71). As this research moves forward, examining the intersection of pubertal timing, sleep, and societal changes therein will be critical to understanding trends in adolescent mental health.
Self-reported frequency of obtaining at least 7 hours of sleep is an incomplete indicator of true sleep prevalence, but it has been used in many other studies of adolescent health (20, 55, 72–74). Given the centrality of sleep to adolescent health, assessing trends in adolescent self-reported sleep measures may be an accessible early warning sign of internalizing symptoms that should prompt additional and more in-depth assessments. Furthermore, evidence from prior studies suggests that adolescents’ subjective experience of various dimensions of sleep quality, including sleep attainment, can provide valuable insights for understanding adolescent internalizing symptoms (75) and other markers of poor mental health (76).
Other results of our study also support findings from existing literature. In multiple studies, researchers have shown that recent increases in poor mental health occurred across all adolescent age groups (1–5, 19), an observation that is indicative of a period effect, although formal tests for period versus cohort effects have been conducted in few studies. We expanded on this prior work (1–5, 19) to demonstrate that period effects are also apparent across different internalizing symptoms, are consistent across race/ethnicity and parental education, and are stronger among girls than boys. Findings from prior studies support our findings that girls are largely driving the increase in mental health problems among adolescents in recent years (35). Taken together, the literature demonstrates that adolescents are exhibiting increases in internalizing symptoms, that girls are experiencing a greater increase, and that these increases are consistent across many demographics, indicative of a growing potential mental health crisis.
Limitations to this study should be considered. We used a series of cross-sectional surveys to analyze trends over time, and this design does not disaggregate the direction of associations. Data are self-reported and may be susceptible to recall and reporting biases, particularly constructs related to risk-taking behavior such as substance use and the self-reported sleep-attainment measure. Specifically, our measure of the percentage of adolescents who frequently get at least 7 hours of sleep has a large recall period of 12 months, which can lead to recall bias. Miller et al. (77) documented that a similar self-reported measure of adult sleep attainment was imprecise and only agreed with diary estimates within a range of 2.5–3 hours.
Results from this study should be also considered in light of the differences between objective and self-reported sleep attainment. We note that the self-reported sleep-attainment measure used in our study has not been validated, and we asked specifically about frequency of getting at least 7 hours of sleep rather than allowing for open-ended responses of average sleep. Moreover, we asked participants to report how often they attained at least 7 hours of sleep in the past year, which may have measurement error. The impact of these measurement issues on the results of the present study are difficult to untangle; for example, previous work indicates that self-reports are more likely to be overestimates of sleep than underestimates, although existing data largely are from adults and thus potentially not generalizable to adolescents (78–82). Research that incorporates validated measures of sleep is warranted to expand on these results.
Self-reporting of internalizing symptoms may also be affected by changes in the acceptability of disclosing mental health. Although we do not have clinical assessments of mental health, the measures we used are similar to those used in other studies in which related constructs were examined (42, 43). Data do not include information on region or school. However, sampling weights assigned to each respondent incorporate these variables. The MTF survey instrument underwent slight wording changes over time, which potentially could lead to measurement variation. In addition, our results indicate that self-reported frequency of attaining at least 7 hours of sleep was declining among US adolescent before the increase in internalizing symptoms began to occur, suggesting that the self-reported frequency of sleeping at least 7 hours most nights may not completely explain internalizing symptom increases and that the drivers of self-reported sleep attainment and internalizing symptom increases may have unique antecedents. We also did not directly assess individual-level self-reported frequency of attaining at least 7 hours of sleep or quality of sleep and, therefore, cannot draw conclusions about associations between loneliness and individual sleep patterns. Researchers should consider how sociostructural factors such as school and home environments confound observed trends as well as the potential for reverse causality, because the relationship between self-reported frequency of attaining at least 7 hours of sleep and internalizing symptoms is bidirectional (30–33).
We caution about overinterpretation of the results of this study, because of their sensitivity to model assumptions and techniques, as well as the limitations of our self-reported measure of sleeping at least 7 hours most nights. Results presented in this study might not be relevant for US adolescents who do not attend school or for adolescents globally. Furthermore, a higher percentage of students aged 18 years or older were excluded from the sample because of data missingness; thus, the results are generalizable to students aged 17 years and younger who attend school.
This study provides evidence of increases in internalizing symptoms over the past decade among adolescents of all ages, and the association with self-reported frequency of attaining at least 7 hours of sleep may be a potential contributing factor. Adolescent mental health is a growing public health issue, with sequalae of internalizing symptoms such as depression and suicide increasing concomitant to the trends we observed in the present analysis. Thus, those engaged in public health efforts to reduce adolescent internalizing symptoms may want to consider conducting feasibility trials to study the effect of increasing adolescent sleep attainment on internalizing symptoms.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York, United States (Navdep Kaur, Ava D. Hamilton, Deborah Hasin, Silvia S. Martins, Katherine M. Keyes); Department of Biostatistics, Mailman School of Public Health, Columbia University, New York, New York, United States (Qixuan Chen); Division of Translational Epidemiology, New York State Psychiatric Institute, New York, New York, United States (Deborah Hasin); and Department of Population Health, New York University School of Medicine, New York, New York, United States (Magdalena Cerda).
This work was supported by the Centers for Disease Control and Prevention (grant R49CE003094), the National Institute of Mental Health (grant 5 T32 MH 13043-49), and the National Institute on Drug Abuse (grant R01-DA048853).
Data from this study are not available for public use.
This work was reported in a recorded oral presentation at SERdigital, online, November 3, 2020; and in a poster presentation at the 2021 American Psychopathological Association annual meeting, virtual, March 5, 2021.
Conflict of interest: none declared.
REFERENCES
- 1. Keyes KM, Gary D, O’Malley PM, et al. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol. 2019;54(8):987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu W. Adolescent depression: national trends, risk factors, and healthcare disparities. Am J Health Behav. 2019;43(1):181–194. [DOI] [PubMed] [Google Scholar]
- 3. Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention . Trends in the Prevalence of Suicide-Related Behaviors National YRBS: 1991–2017. 2018. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2017_suicide_trend_yrbs.pdf. Accessed August 1, 2020.
- 5. Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141(6):e20172426. [DOI] [PubMed] [Google Scholar]
- 6. Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. 2019;173(6):598–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999–2014. No. 241. 2016. http://www.cdc.gov/nchs/data/databriefs/db241.pdf. [PubMed]
- 8. Kalb LG, Stapp EK, Ballard ED, et al. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miron O, Yu K-H, Wilf-Miron R, et al. Suicide rates among adolescents and young adults in the United States, 2000–2017. JAMA. 2019;321(23):2362–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liu J, Chen X, Lewis G. Childhood internalizing behaviour: analysis and implications. J Psychiatr Ment Health Nurs. 2011;18(10):884–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- 12. Perlman D, Peplau LA. Loneliness. Encycl Ment Heal. 1998;1:571–581. [Google Scholar]
- 13. Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin Psychol Rev. 2006;26(6):695–718. [DOI] [PubMed] [Google Scholar]
- 14. Stickley A, Koyanagi A, Koposov R, et al. Loneliness and health risk behaviours among Russian and US adolescents: a cross-sectional study. 2014;14:366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vanhalst J, Luyckx K, Van Petegem S, et al. The detrimental effects of adolescents’ chronic loneliness on motivation and emotion regulation in social situations. J Youth Adolesc. 2018;47(1):162–176. [DOI] [PubMed] [Google Scholar]
- 16. Benner AD. Latino adolescents’ loneliness, academic performance, and the buffering nature of friendships. J Youth Adolesc. 2011;40(5):556–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bell A. Life-course and cohort trajectories of mental health in the UK, 1991-2008 – a multilevel age-period-cohort analysis. Soc Sci Med. 2014;120:21–30. [DOI] [PubMed] [Google Scholar]
- 18. Keyes KM, Nicholson R, Kinley J, et al. Age, period, and cohort effects in psychological distress in the United States and Canada. Am J Epidemiol. 2014;179(10):1216–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Twenge JM, Cooper AB, Joiner TE, et al. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. 2019;128(3):185–199. [DOI] [PubMed] [Google Scholar]
- 20. Twenge JM, Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009–2015 and association with new media screen time. Sleep Med. 2017;39:47–53. [DOI] [PubMed] [Google Scholar]
- 21. O’Dea JA, Dibley MJ, Rankin NM. Low sleep and low socioeconomic status predict high body mass index: a 4-year longitudinal study of Australian schoolchildren. Pediatr Obes. 2012;7(4):295–303. [DOI] [PubMed] [Google Scholar]
- 22. Wolfson AR, Carskadon MA. Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506. [DOI] [PubMed] [Google Scholar]
- 23. Meldrum RC, Restivo E. The behavioral and health consequences of sleep deprivation among U.S. high school students: relative deprivation matters. Prev Med (Baltim). 2014;63:24–28. [DOI] [PubMed] [Google Scholar]
- 24. Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics. 2007;119(suppl 1):S29–S37. [DOI] [PubMed] [Google Scholar]
- 25. Terry-McElrath YM, Maslowsky J, O’Malley PM, et al. Sleep and substance use among US adolescents, 1991-2014. Am J Health Behav. 2016;40(1):77–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: from physiological to pathological conditions. Sleep Sci. 2015;8(3):143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris RA, Qualter P, Robinson SJ. Loneliness trajectories from middle childhood to pre-adolescence: impact on perceived health and sleep disturbance. J Adolesc. 2013;36(6):1295–1304. [DOI] [PubMed] [Google Scholar]
- 28. Mahon NE. Loneliness and sleep during adolescence. Percept Mot Skills. 1994;78(1):227–231. [DOI] [PubMed] [Google Scholar]
- 29. Cacioppo JT, Hawkley LC, Berntson GG, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol Sci. 2002;13(4):384–387. [DOI] [PubMed] [Google Scholar]
- 30. Shanahan L, Copeland WE, Angold A, et al. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(5):550–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Littlewood DL, Kyle SD, Carter LA, et al. Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychol Med. 2019;49(3):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Biddle DJ, Hermens DF, Lallukka T, et al. Insomnia symptoms and short sleep duration predict trajectory of mental health symptoms. Sleep Med. 2019;54:53–61. [DOI] [PubMed] [Google Scholar]
- 33. Kenney SR, Lac A, Labrie JW, et al. Mental health, sleep quality, drinking motives, and alcohol-related consequences: a path-analytic model. J Stud Alcohol Drugs. 2013;74(6):841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang Z, Yu C, Wang J, et al. Age-period-cohort analysis of suicide mortality by gender among white and black Americans, 1983–2012. Int J Equity Health. 2016;15(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Twenge JM. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc Indic Res. 2015;121(2):437–454. [Google Scholar]
- 36. Wickramaratne PJ, Weissman MM, Leaf PJ, et al. Age, period and cohort effects on the risk of major depression: results from five United States communities. J Clin Epidemiol. 1989;42(4):333–343. [DOI] [PubMed] [Google Scholar]
- 37. Kasen S, Cohen P, Chen H, et al. Depression in adult women: age changes and cohort effects. Am J Public Health. 2003;93(12):2061–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Todd M, Teitler J. Darker days? Recent trends in depression disparities among U.S. Adults. 2019;89(6):727–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Miech RA, Johnston LD, O’Malley PM, et al. Monitoring the Future National Survey Results on Drug Use, 1975–2018: Volume I, Secondary School Students. 2019. https://deepblue.lib.umich.edu/handle/2027.42/150622. Accessed August 15, 2020.
- 40. Miech R, Johnston L, O’Malley PM, et al. Trends in adolescent vaping, 2017–2019. N Engl J Med. 2019;381(15):1490–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bachman JG, Johnston LD, O’Malley PM, et al. The Monitoring the Future Project After Four Decades: Design and Procedures. Monitoring the Future Occasional Paper No. 82. 2015. Ann Arbor, MI: Institute for Social Research, University of Michigan; 93 pp. https://deepblue.lib.umich.edu/bitstream/2027.42/137908/1/mtf-occ82.pdf. Accessed August 15, 2020.
- 42. Clark DMT, Loxton NJ, Tobin SJ. Declining loneliness over time: evidence from American colleges and high schools. Pers Soc Psychol Bull. 2015;41(1):78–89. [DOI] [PubMed] [Google Scholar]
- 43. Trzesniewski KH, Donnellan MB. Rethinking “Generation Me”: a study of cohort effects from 1976-2006. Perspect Psychol Sci. 2010;5(1):58–75. [DOI] [PubMed] [Google Scholar]
- 44. Yang Y, Fu WJ, Land KC. A methodological comparison of age-period-cohort models: the intrinsic estimator and conventional generalized linear models. Sociol Methodol. 2004;34(1):75–110. [Google Scholar]
- 45. Yang Y. Bayesian inference for hierarchical age-period-cohort models of repeated cross-section survey data. Sociol Methodol. 2006;36(1):39–74. [Google Scholar]
- 46. Yang Y, Land KC. A mixed models approach to the age-period-cohort analysis of repeated cross-section surveys, with an application to data on trends in verbal test scores. Sociol Methodol. 2006;36(1):75–97. [Google Scholar]
- 47. Yang Y, Land KC. Age–period–cohort analysis of repeated cross-section surveys fixed or random effects? Sociol Methods Res. 2008;36(3):297–326. [Google Scholar]
- 48. Yang Y, Land KC. Mixed effects models: hierarchical APC–cross-classified random effects models (HAPC-CCREM), part I: the basics. In: Keiding N, Morgan BJT, Wikle CK, Heijden P, eds. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. London, UK: Chapman and Hall/CRC; 2013:191–230. [Google Scholar]
- 49. Yang Y, Land KC. Mixed effects models: hierarchical APC–cross-classified random effects models (HAPC-CCREM), part II: advanced analyses. In: Keiding N, Morgan BJT, Wikle CK, Heijden P, eds. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. London, UK: Chapman and Hall/CRCChapman and Hall/CRC; 2013:231–284. [Google Scholar]
- 50. Kaur N, Keyes KM, Hamilton AD, et al. Trends in cannabis use and attitudes toward legalization and use among Australians from 2001–2016: an age-period-cohort analysis. Addiction Published online October. 2020;7(5):1152–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hamilton AD, Jang JB, Patrick ME, et al. Age, period and cohort effects in frequent cannabis use among US students: 1991–2018. Addiction. 2019;114(10):1763–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ananth CV, Friedman AM, Keyes KM, et al. Primary and repeat cesarean deliveries. Epidemiology. 2017;28(4):567–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jang JB, Patrick ME, Keyes KM, et al. Frequent binge drinking among US adolescents, 1991 to 2015. Pediatrics. 2017;139(6):e20164023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Keyes KM, Ananth CV. Age, period, and cohort effects in perinatal epidemiology: implications and considerations. Paediatr Perinat Epidemiol. 2014;28(4):277–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Keyes KM, Maslowsky J, Hamilton A, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics. 2015;135(3):460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Keyes KM, Rutherford C, Hamilton A, et al. Age, period, and cohort effects in synthetic cannabinoid use among US adolescents, 2011–2015. Drug Alcohol Depend. 2016;166:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Keyes KM, Utz RL, Robinson W, et al. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971–2006. Soc Sci Med. 2010;70(7):1100–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Carstensen B. Age–period–cohort models for the Lexis diagram. Stat Med. 2007;26(15):3018–3045. [DOI] [PubMed] [Google Scholar]
- 59. Clayton D, Schifflers E. Models for temporal variation in cancer rates. II: Age–period–cohort models. Stat Med. 1987;6(4):469–481. [DOI] [PubMed] [Google Scholar]
- 60. SAS Institute Inc . SAS. Cary, NC: SAS Institute Inc; 2014. [Google Scholar]
- 61. Wickham H, Navarro D, Pedersen TL. Ggplot2: Elegant Graphics for Data Analysis. 2nd ed. Basel, Switzerland: Springer; 2016. [Google Scholar]
- 62. Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161(1):81–88. [DOI] [PubMed] [Google Scholar]
- 64. Yang Y, Schulhofer-Wohl S, Fu WJ, et al. The intrinsic estimator for age-period-cohort analysis: what it is and how to use it. Am J Sociol. 2008;113(6):1697–1736. [Google Scholar]
- 65. Masters RK, Hummer RA, Powers DA, et al. Long-term trends in adult mortality for U.S. blacks and whites: an examination of period- and cohort-based changes. Demography. 2014;51(6):2047–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Stata Corporation . Stata Statistical Software, Release 16. College Station, TX: StataCorp; 2019. [Google Scholar]
- 67. Carpenito-Moyet LJ. Nursing Diagnosis: Application to Clinical Practice. 14th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 68. Kaplan HB, Martin SS, Robbins C. Application of a general theory of deviant behavior: self-derogation and adolescent drug use. J Health Soc Behav. 1982;23(4):274–294. [PubMed] [Google Scholar]
- 69. Dorpat TL. Depressive affect. Psychoanal Study Child. 1977;32(1):3–27. [DOI] [PubMed] [Google Scholar]
- 70. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wang J, Kwok MK, Au Yeung SL, et al. Age of puberty and sleep duration: observational and Mendelian randomization study. Sci Rep. 2020;10(1):3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Jackson DB, Vaughn MG. Adolescent health lifestyles and educational risk: findings from the monitoring the future study, 2010–2016. Am J Prev Med. 2019;57(4):470–477. [DOI] [PubMed] [Google Scholar]
- 73. Shimoga SV, Erlyana E, Rebello V. Associations of social media use with physical activity and sleep adequacy among adolescents: cross-sectional survey. J Med Internet Res. 2019;21(6):e14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Jackson DB, Boccio CM, Leal WE. Do youth who vape exhibit risky health lifestyles? Monitoring the Future, 2017. Prev Med (Baltim). 2020;136:106101. [DOI] [PubMed] [Google Scholar]
- 75. Rubens SL, Evans SC, Becker SP, et al. Self-reported time in bed and sleep quality in association with internalizing and externalizing symptoms in school-age youth. Child Psychiatry Hum Dev. 2017;48(3):455–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Becker SP. External validity of children’s self-reported sleep functioning: associations with academic, social, and behavioral adjustment. Sleep Med. 2014;15(9):1094–1100. [DOI] [PubMed] [Google Scholar]
- 77. Miller CB, Gordon CJ, Toubia L, et al. Agreement between simple questions about sleep duration and sleep diaries in a large online survey. Sleep Heal. 2015;1(2):133–137. [DOI] [PubMed] [Google Scholar]
- 78. Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration. Epidemiology. 2008;19(6):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Girschik J, Fritschi L, Heyworth J, et al. Validation of self-reported sleep against actigraphy. J Epidemiol. 2012;22(5):462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jackson CL, Patel SR, Jackson WB, et al. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(6):zsy057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Jackson CL, Ward JB, Johnson DA, et al. Concordance between self-reported and actigraphy-assessed sleep duration among African-American adults: findings from the Jackson Heart Sleep Study. Sleep. 2020;43(3):462zsz246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Muzni K, Groeger JA, Dijk D, et al. Self-reported sleep quality is more closely associated with mental and physical health than chronotype and sleep duration in young adults: a multi-instrument analysis. J Sleep Res. 2021;30(1):e13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


