Abstract
Background
Hand hygiene among healthcare workers is the leading measure to reduce healthcare-associated infections. However, hand hygiene behavior is complex and not readily understood. This study aimed to identify the determinants and the underlying mechanism of hand hygiene behavior based on the capability, opportunity, motivation-behavior model.
Methods
A self-constructed questionnaire survey was conducted among healthcare workers in Chongqing, China. Capability, opportunity, and motivation were designed as independent variables, and hand hygiene behavior was measured as a dependent variable. Internal consistency reliability analysis and confirmatory factor analysis were applied to examine the reliability and validity of the questionnaire. Structural equation modeling was performed to explore the relationships among capability, opportunity, motivation, and hand hygiene behavior.
Results
Four hundred and ninety-nine physicians and nurses were investigated. The Cronbach’s α coefficients were above 0.764. Confirmatory factor analysis was confirmed with good data fitness. The structural equation modeling had a good fit (root mean square error of approximation=0.070, comparative fit index=0.960, Tucker–Lewis index=0.956). Both opportunity (β=0.265, p<0.05) and motivation (β=0.333, p<0.05) directly affected hand hygiene behavior. Both capability (β=0.194, p<0.001) and opportunity (β=0.719, p<0.001) were indirectly linked to hand hygiene behavior through motivation.
Conclusion
To improve hand hygiene behavior, more efforts need to be focused on resource provision and motivation enhancement in the future compared to training.
Keywords: hand hygiene, behavior, COM-B model, healthcare workers
Introduction
Healthcare-associated infections (HAIs) represent the global challenge for patient safety, which increase the burden, prolong hospital stays, and threaten the lives of patients.1 It is estimated that 7 out of every 100 hospitalized patients in high-income countries and 10 out of every 100 hospitalized patients in low- and middle-income countries acquire one or more HAIs at any given time, according to the estimate by the World Health Organization (WHO) in 2019. Hand hygiene among healthcare workers (HCWs) is considered to be an important low-cost measure to reduce HAIs.2–4 However, hand hygiene compliance across the world is poor, at approximately 40%–60%.5–7
Poor compliance is attributed to the complexity of hand hygiene behavior,8–10 which includes multiple determinants covering knowledge, skills, attention, infrastructure, and motivation.11–15 Many interventions and strategies issued by WHO that were developed to improve hand hygiene compliance are proved to be a partial success.14,16–19 One of the reasons why the improvement of hand hygiene behavior is not ideal is that the interventions and strategies are usually not based on behavioral or psychological theory.13 Understanding the underlying mechanisms (the determinants of current and desired behavior) of hand hygiene behavior based on a theory can be effective to improve the hand hygiene compliance of HCWs.15 However, limited evidence is available in developing countries.16,20
The Capability, Opportunity, Motivation-Behavior (COM-B) model is regarded as a promising and systematic theoretical framework of behavior change21,22 and is cited as a key theoretical framework for understanding and supporting behavior change by the UK National Institute for Health and Care Excellence.23 It originates from a variety of health behavior models, so it can capture all factors that influence behavior change.23,24 It demonstrates that the change in human behavior results from one or more of the following: capability, opportunity, or motivation, which can guide the design of the most effective interventions for targeted behavior.21,23,24 Capability includes physical and psychological capacity about behavior. Motivation involves reflective and automatic processes that control behavior. Opportunity that is encompassed by external factors addresses all physical and social factors beyond one’s control.25
Previous studies have applied COM-B model to understand the barriers and facilitators of hand hygiene behavior and other infection control measures in HCWs to inform the design of intervention about behavior change.26,27 Recently more research has been performed with respect to the quantitative studies based on COM-B models. For example, Lydon et al mainly developed a valid questionnaire and found that capability and motivation make a significant contribution to hand hygiene behavior in Ireland.28 Tomsic et al reported that capability is associated with orthopedic physicians’ self‑reported compliance with surgical site infection prevention.29 However, how capability, opportunity and motivation together affect hand hygiene behaviors and what are the pathways between them are scarcely known. Besides, more studies should be performed in the different background to examine the generalization of COM-B model. Although Miller et al have explored the pathways among UK population,30 the evidence in HCWs is limited. The exploration of the pathway based on COM-B model among HCWs with respect to hand hygiene will help to understand the barriers and facilitators of infection control and improve hand hygiene. Therefore, this study aimed to identify the underlying mechanisms of hand hygiene behavior in HCWs in China based on the COM-B model.
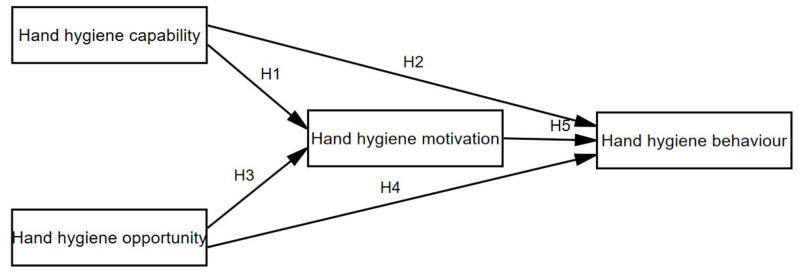
The theoretical framework was adapted from the COM-B model. The model holds that capability, opportunity, and motivation are determinants of behavior, and capability and opportunity influence motivation. Therefore, capability and opportunity affect behavior through direct and indirect paths.28 The following hypotheses were proposed in this study (Figure 1).
Figure 1.
Hypotheses of the COM-B model of hand hygiene behavior of HCWs.
H1: Capability affects motivation.
H2: Capability affects hand hygiene behavior.
H3: Opportunity affects motivation.
H4: Opportunity affects hand hygiene behavior.
H5: Motivation affects hand hygiene behavior.
H6: Motivation mediates the association between capability and hand hygiene behavior.
H7: Motivation mediates the association between opportunity and hand hygiene behavior.
Methods
Settings
Chongqing is located southwest of China and has a population of 31 million. The economic development of Chongqing is at the middle level in China, wherein the GDP was 2.16 trillion (yuan) in 2018, ranking 17 among 31 provinces. Tongnan District is located northwest of Chongqing, with a land area of 1583 km2 and a population of 1.03 million. The annual GDP of Tongnan reached 38.10 billion (yuan) in 2018, just above the average level of all counties in Chongqing. With its medium level of economic development in China, the Tongnan District in Chongqing Municipality was selected for this study because of its good representativeness. The survey was conducted in two secondary general hospitals in Tongnan District, which received 0.6 million patient visits per year.
Participants and Data Collection
All of the clinical physicians and nurses on duty during the period of the survey were invited to participate in the survey. Data were collected over the period from 22nd to 26th July 2019 by five trained investigators (recruited from postgraduate research students in social sciences and medicine). To guarantee the data quality, investigators explained the objective and procedure of the study to the participants. On average, the survey took about 10 min to complete. A token (roughly $1.65) was given to the respondent after completing the questionnaire.
Independent Measures
The questionnaire was derived based on previous studies and focus group discussion to guarantee content validity. Firstly, the questionnaire items from previous studies on hand hygiene were collected.8,10,16,21,31 Then, items with the same or similar meaning were merged, and 45 items were retained. Meanwhile, all of the items were translated from English into simplified Chinese by two translators. Then, a focus group discussion was held to confirm the necessity, appropriateness, understandability, and accuracy of each item, and five items were revised. The focus group comprised graduate students and teachers who worked on HAI prevention and control and were aware of the COM-B model. Finally, a 45-item questionnaire with four constructs was designed (Supplementary Table 1).
To guarantee the quality of formal investigation, we conducted a pilot survey in a general hospital. Sixteen physicians and nurses were face-to-face invited to fill in the questionnaire and provide suggestions. Participants reported that the items covered almost all factors related to hand hygiene.
The capability construct which comprised 10 items was developed to assess whether the respondent believed that he/she had the knowledge, skills, memory, attention, and decision processes to perform hand hygiene behavior. The opportunity construct which comprised 11 items was designed to assess whether the environmental context and resources were available to make hand hygiene behavior possible and whether the social environment influenced the personal hand hygiene behavior. The motivation construct which comprised 19 items aimed to assess whether the respondent had beliefs about consequences and capabilities and whether the social/professional role and identity, goals, and emotion supported personal hand hygiene behavior. Socio-demographic characteristics including gender, career type, age, working year and education degree were recorded.
Dependent Measures
Self-reported hand hygiene behavior was measured using the “Five moments of hand hygiene behavior” proposed by the WHO: (1) before patient contact, (2) before aseptic technique, (3) after body fluid exposure, (4) after patient contact, and (5) after patient surrounding contact. For each item, respondents indicated the frequencies with which they complied hand hygiene last year. Each item was scored from 1 “never” to 5 “always” by using a 5-point Likert scale.
Statistical Analysis
Descriptive statistics were used to describe the demographic and clinical characteristics of the sample. Internal consistency reliability and confirmatory factor analyses (CFA) were applied to examine the reliability and validity of the questionnaire. Because the responses were ordinal variables (5-Likert scale), factor analysis with the means and variance-adjusted weighted least squares extraction (WLSMV) estimation were used in CFA and structural equation modeling (SEM).32
CFA was applied to validate whether the hypothesized latent variables could represent item load on constructs. Firstly, the CFA for capacity, opportunity, and motivation constructs was conducted separately. Items with a standardized coefficient above 0.6 on measured latent variables were considered effective measure items for targeted latent variables and were retained. Secondly, the CFA for capacity and opportunity, capacity and motivation, and opportunity and motivation was conducted. There was no cross loading when goodness-of-fit indices were up to standard. Thirdly, the CFA for capacity, opportunity, and motivation was conducted to examine whether the construct was acceptable. Furthermore, the reliability was determined by calculating Cronbach’s α. After the measurement was validated, SEM was conducted to construct the COM-B model of hand hygiene behavior. If some modification indexes were very high, then modifications were made.33
Goodness-of-fit indices were used to evaluate the fitness of the CFA and SEM model:34 root mean square error of approximation (RMSEA; <0.08 acceptable, <0.05 excellent), comparative fit index (CFI; >0.90 acceptable, >0.95 excellent), and Tucker–Lewis index (TLI; >0.90 acceptable, >0.95 excellent).35
The Statistical Package for Social Sciences for Windows (version 24.0, SPSS Inc., Chicago, IL, USA) and MPLUS (version 7.0, Muthén & Muthén, Los Angeles, CA, USA) were used to conduct analyses. The significance level was set at 0.05.
Results
Characteristics of Respondents
A total of 585 HCWs were willing to fill the questionnaires. Among the 585 HCWs, 499 (85.3%) were valid respondents. A number of 86 questionnaires were excluded to analyze for incomplete information and low quality. Most of the respondents were female (75.3%) and nurses (61.0%). The average age and working years were 32.5±8.7 and 10.2±8.9 years, respectively. About 69.5% of respondents obtained a bachelor’s degree or above (Table 1).
Table 1.
Demographics and Clinical Characteristics of Respondents
| Characteristics | Mean±SD†/N (%) |
|---|---|
| Age (years) | 32.5±8.7 |
| Gender | |
| Male | 123 (24.7) |
| Female | 375 (75.3) |
| Profession | |
| Physician | 194 (39.0) |
| Nurse | 304 (61.0) |
| Department | |
| Internal medicine | 184 (36.9) |
| Surgery | 107 (21.4) |
| Obstetrics and gynecology | 32 (6.4) |
| Pediatrics | 42 (8.4) |
| ICU | 42 (8.4) |
| Acupuncture/massage/rehabilitation | 34 (6.8) |
| Ophthalmology/otolaryngology/dermatology | 19 (3.8) |
| Emergency | 16 (3.2) |
| Anesthesiology | 23 (4.6) |
| Educational background | |
| Associate degree | 152 (30.5) |
| Bachelor’s degree | 333 (66.9) |
| Master’s degree | 12 (2.4) |
| Doctoral degree | 1 (0.2) |
| Technical title | |
| To be appraised | 53 (10.7) |
| Junior | 271 (54.9) |
| Middle | 105 (21.3) |
| Senior | 63 (12.8) |
| Working years (years) | 10.2±8.9 |
Abbreviation: †SD, standard deviation.
Reliability and Validity of Measures
According to the CFA results, three items from the capability construct, three items from the opportunity construct and eight items from the motivation construct were removed. The three-factor model with 26 items was confirmed with good data fitness: RMSEA=0.078, CFI=0.964, and TLI=0.960.
The Cronbach’s α coefficient values were acceptable for all constructs. The specific reliability values for the constructs were as follows (Table 2): (1) capability (0.850), (2) opportunity (0.764), (3) motivation (0.877), and (4) hand hygiene behavior (0.808).
Table 2.
Constructs for Capability, Opportunity, Motivation and Behavior
| Constructs | Items | β | p-value | Mean | SD† | Cronbach’s α |
|---|---|---|---|---|---|---|
| Capability | C1 | 0.825 | <0.001 | 4.45 | 0.425 | 0.850 |
| C2 | 0.886 | <0.001 | ||||
| C3 | 0.783 | <0.001 | ||||
| C4 | 0.749 | <0.001 | ||||
| C5 | 0.780 | <0.001 | ||||
| C6 | 0.735 | <0.001 | ||||
| C7 | 0.770 | <0.001 | ||||
| Opportunity | O1 | 0.661 | <0.001 | 4.155 | 0.472 | 0.764 |
| O2 | 0.681 | <0.001 | ||||
| O3 | 0.417 | <0.001 | ||||
| O4 | 0.390 | <0.001 | ||||
| O6 | 0.658 | <0.001 | ||||
| O8 | 0.849 | <0.001 | ||||
| O9 | 0.873 | <0.001 | ||||
| O10 | 0.713 | <0.001 | ||||
| Motivation | M1 | 0.822 | <0.001 | 4.329 | 0.407 | 0.877 |
| M2 | 0.739 | <0.001 | ||||
| M5 | 0.763 | <0.001 | ||||
| M6 | 0.713 | <0.001 | ||||
| M7 | 0.670 | <0.001 | ||||
| M9 | 0.746 | <0.001 | ||||
| M11 | 0.850 | <0.001 | ||||
| M13 | 0.634 | <0.001 | ||||
| M14 | 0.808 | <0.001 | ||||
| M15 | 0.769 | <0.001 | ||||
| M18 | 0.808 | <0.001 | ||||
| Behavior | B1 | 0.738 | <0.001 | 4.524 | 0.474 | 0.808 |
| B2 | 0.762 | <0.001 | ||||
| B3 | 0.802 | <0.001 | ||||
| B4 | 0.920 | <0.001 |
Abbreviation: †SD, standard deviation.
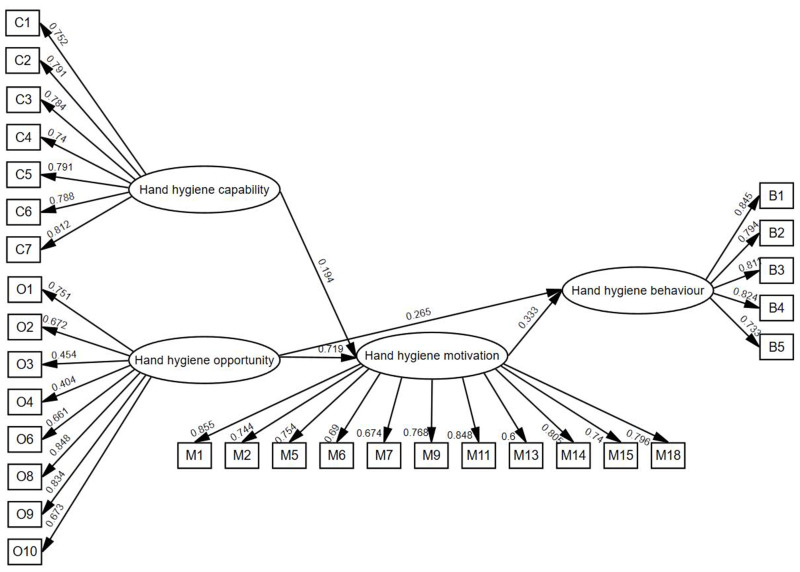
A total of 499 respondents were included for SEM analysis. Figure 2 reports the results of standardized path coefficients with statistical significance (p<0.05). Only one hypothesized path (H2) was insignificant. After three modifications, the final SEM model had good data fitness: chi-square=1450.809, chi-square/DF=3.414, RMESA=0.070, CFI=0.960, TLI=0.956, and SRMR=0.059.
Figure 2.
Final SEM model of hand hygiene behavior of HCWs.
As initially hypothesized, capability (β=0.194, p<0.001) and opportunity (β=0.719, p<0.001) had direct effects on motivation (R2=0.773), and opportunity (β=0.265, p<0.05) and motivation (β=0.333, p<0.05) directly affected hand hygiene behavior (R2=0.328). Capability (β=0.065, 95% CI=0.052–0.102) and opportunity (β=0.239, 95% CI=0.170–0.314) had indirect effects on hand hygiene behavior. To sum up, hypotheses H1, H3, H4, H5, H6 and H7 were accepted, while hypothesis H2 was rejected.
Discussion
This study confirmed how capacity, opportunity and motivation affect hand hygiene behavior among HCWs. Opportunity and motivation directly affect hand hygiene behavior. Capability is not a significant predictor of hand hygiene behavior, while it has an indirect effect on hand hygiene behavior through motivation. Opportunity has a direct and indirect impact on hand hygiene behaviors.
Opportunity is found to be the important predictor of hand hygiene behavior in this study, which is inconsistent with the results of a similar study conducted in an intensive care unit in Ireland.28 In Lydon et al’s study, opportunity was not found to be a significant predictor in the Irish sample, but they speculated that opportunity may be the predictive factor of behavior in less-resourced healthcare systems with inadequate and inconvenient hand hygiene facilities and may not be relevant in better-resourced healthcare systems.28 The allocation of resources about HAIs was limited and the lack of fund was the barrier to many hospitals, which contributed to inadequate and inconvenient hand hygiene facilities and other limited infrastructure.36,37 This study confirms Lydon et al’s hypothesis. Previous recommendations also have pointed out that limited hand hygiene infrastructure was a key factor in developing and low-income countries.5,28,38–40 Several studies have explored approaches to increase opportunity to improve hand hygiene behavior. For example, a systematic review indicated that increased accessibility of hand sanitizers and placement of dispensers in more visible places can increase hand hygiene compliance.41 Moreover, a heavy workload is a barrier to hand hygiene. In some situations, hand hygiene is not being performed because staff are too busy or called away to a more urgent task.19,40–42 Heavy workload on the working nurses makes them distracted and gives priority to clinical and nursing procedures more than hand hygiene.43,44 Furthermore, better opportunity can indirectly promote hand hygiene behavior through motivation, which is consistent with other studies. For example, Smiddy et al reviewed 11 qualitative research studies, and the results indicated that opportunity (eg, social influences, use of cues) was a factor in hand hygiene motivation.45 In summary, greater efforts need to be made to provide more adequate resources and staff in the future.20 For example, pediatric-friendly reminder posters, pamphlets and increased accessibility of hand sanitizers were proved to improve HCW hand hygiene compliance.41,46
In our study, capability was not directly linked to hand hygiene behavior but indirectly linked to hand hygiene behavior through motivation, which is an interesting finding. Many studies have revealed that inadequate capability (eg, knowledge and skills) was one of the key reasons for low hand hygiene compliance.28,47,48 Thus, “training and education” is one of the most frequent components of multimodal intervention strategies for hand hygiene.11,14,19,20,49 Contrary to these studies, De Wandel et al identified that good theoretical knowledge was not a significant predictor of hand hygiene practice,50 and there was a disconnect between hand hygiene knowledge and behavior.20 Moreover, a previous study showed that educational intervention would not lead to higher compliance if knowledge was lacking.11 Furthermore, although capability alone does not contribute to changes in practice,1,21 this study revealed that capability may indirectly increase hand hygiene compliance by increasing hand hygiene motivation. However, various studies have found that the majority of HCWs had good hand hygiene knowledge.41,49,51–53 Whether education and training will be the priority of multimodal intervention strategies for hand hygiene requires further study.
According to the SEM results, motivation was a significant predictor of hand hygiene behavior, which is consistent with previous results.28 Many social cognition theories reveal that effective behavioral changes are primarily caused by motivated individuals.54 Salamati et al showed that composite hand hygiene scores increased after a motivational interviewing intervention.55 Motivation not only can directly affect hand hygiene behaviors, but also can mediate the relationship between capacity and hand hygiene behaviors as well as opportunity and hand hygiene behaviors. Interestingly, Miller found the same pathways among UK population.30 These findings suggest that policymakers or hospital administrators should focus on improving HCWs’ motivation (eg, by setting a goal, modeling, or incentivizing) to increase hand hygiene compliance. With respect to the items in the questionnaire compared to previous study, the items in our study were characterized by the thought of HCWs30 and hold broad meanings about motivation like the concern for others and fear about transmission.28
This study has some limitations. First, this study was conducted in one province of China. Thus, we should remain cautious in our attempts to generalize the findings of this study. Second, we measured self-report hand hygiene behavior instead of practices, which may result in an overestimation of hand hygiene compliance.21,56 Aside from this, self-reports remain an important source of information about hand hygiene behavior.21 Third, as SEM was constructed using cross-sectional data, which was difficult to make causal inferences and results would differ if another time frame had been chosen, longitudinal analyses should be used to assess relationships across time. Fourthly, because this study was conducted based on COM-B model, the main variables are confined to capability, opportunity, motivation and behavior. Thus, the empirical evidence of the effect of workload and level of training or beliefs was not supported.
Conclusion
This study confirmed the pathway in which capacity, opportunity and motivation affect hand hygiene behavior among HCWs. The results show that opportunity and motivation are significant predictors of hand hygiene behavior. Capability plays an important role in motivating HCWs to perform hand hygiene. Although capability is not a significant predictor of hand hygiene behavior, it has an indirect effect on hand hygiene behavior through hand hygiene motivation. Opportunity has an impact on hand hygiene behaviors through both direct and indirect channels. To improve hand hygiene behavior, more efforts should focus on resource provision and hand hygiene motivation enhancement. Practically, reminder posters, pamphlets, increased accessibility of hand sanitizers and incentivizing can be conducted in hospital. Future study can be conducted in a different context to examine the generalization and robustness of the model and the potential factors that may moderate the pathway in COM-B model.
Acknowledgments
The authors would like to acknowledge the following individuals who helped collect data: Du Yaling, Geng Yarui, Fan Lili.
Funding Statement
This research was funded by the National Natural Science Foundation of China, grant number 71473098 and 2021 Wuhan Medical Research Project, grant number WG21D05.
Ethical Considerations
The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG: IORG0003571). Written informed consent was obtained from the respondents, and any information that could identify participants was guaranteed confidentiality.
Disclosure
The authors declare that there is no conflict of interests.
References
- 1.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356(9238):1307–1312. doi: 10.1016/s0140-6736(00)02814-2 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Patient Safety: Global Action on Patient Safety: Report by the Director-General. Geneva: World Health Organization; 2019. [Google Scholar]
- 3.Schreiber PW, Sax H, Wolfensberger A, Clack L, Kuster SP. The preventable proportion of healthcare-associated infections 2005-2016: systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2018;39(11):1277–1295. doi: 10.1017/ice.2018.183 [DOI] [PubMed] [Google Scholar]
- 4.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the Proportion of Healthcare-Associated Infections That Are Reasonably Preventable and the Related Mortality and Costs. Infect Control Hospital Epidemiol. 2011;32(2):101–114. doi: 10.1086/657912 [DOI] [PubMed] [Google Scholar]
- 5.Borg MA, Benbachir M, Cookson BD, et al. Health care worker perceptions of hand hygiene practices and obstacles in a developing region. Am J Infect Control. 2009;37(10):855–857. doi: 10.1016/j.ajic.2009.06.003 [DOI] [PubMed] [Google Scholar]
- 6.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31(3):283–294. doi: 10.1086/650451 [DOI] [PubMed] [Google Scholar]
- 7.Jeanes A, Coen PG, Gould DJ, Drey NS. Validity of hand hygiene compliance measurement by observation: a systematic review. Am J Infect Control. 2019;47(3):313–322. doi: 10.1016/j.ajic.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 8.Dyson J, Lawton R, Jackson C, Cheater F. Development of a theory-based instrument to identify barriers and levers to best hand hygiene practice among healthcare practitioners. Implement Sci. 2013;8:111. doi: 10.1186/1748-5908-8-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand Hygiene among Physicians: performance, Beliefs, and Perceptions. Ann Intern Med. 2004;141(1):1–8. doi: 10.7326/0003-4819-141-1-200407060-00008 [DOI] [PubMed] [Google Scholar]
- 10.Squires JE, Linklater S, Grimshaw JM, et al. Understanding Practice: factors That Influence Physician Hand Hygiene Compliance. Infect Control Hospital Epidemiol. 2014;35(12):1511–1520. doi: 10.1086/678597 [DOI] [PubMed] [Google Scholar]
- 11.Huis A, van Achterberg T, de Bruin M, Grol R, Schoonhoven L, Hulscher M. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci. 2012;7:92. doi: 10.1186/1748-5908-7-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McLaws M-L, Maharlouei N, Yousefi F, Askarian M. Predicting hand hygiene among Iranian health care workers using the theory of planned behavior. Am J Infect Control. 2012;40(4):336–339. doi: 10.1016/j.ajic.2011.04.004 [DOI] [PubMed] [Google Scholar]
- 13.Srigley JA, Corace K, Hargadon DP, et al. Applying psychological frameworks of behaviour change to improve healthcare worker hand hygiene: a systematic review. J Hosp Infect. 2015;91(3):202–210. doi: 10.1016/j.jhin.2015.06.019 [DOI] [PubMed] [Google Scholar]
- 14.Valim MD, Rocha I, Souza TPM, et al. Efficacy of the multimodal strategy for Hand Hygiene compliance: an integrative review %J Revista Brasileira de Enfermagem. Revista Brasileira de Enfermagem. 2019;72:552–565. [DOI] [PubMed] [Google Scholar]
- 15.Lambe K, Lydon S, Madden C, et al. Understanding hand hygiene behaviour in the intensive care unit to inform interventions: an interview study. BMC Health Serv Res. 2020;20(1):353. doi: 10.1186/s12913-020-05215-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fuller C, Besser S, Savage J, McAteer J, Stone S, Michie S. Application of a theoretical framework for behavior change to hospital workers’ real-time explanations for noncompliance with hand hygiene guidelines. Am J Infect Control. 2014;42(2):106–110. doi: 10.1016/j.ajic.2013.07.019 [DOI] [PubMed] [Google Scholar]
- 17.Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2010;1(9):CD005186. doi: 10.1002/14651858.CD005186.pub3 [DOI] [PubMed] [Google Scholar]
- 18.Schweizer ML, Reisinger HS, Ohl M, et al. Searching for an optimal hand hygiene bundle: a meta-analysis. Clin Infect Dis. 2014;58(2):248–259. doi: 10.1093/cid/cit670 [DOI] [PubMed] [Google Scholar]
- 19.Martos-Cabrera MB, Mota-Romero E, Martos-García R, et al. Hand Hygiene Teaching Strategies among Nursing Staff: a Systematic Review. Int J Environ Res Public Health. 2019;16(17):3039. doi: 10.3390/ijerph16173039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chatfield SL, DeBois K, Nolan R, Crawford H, Hallam JS. Hand hygiene among healthcare workers: a qualitative meta summary using the GRADE-CERQual process. J Infection Prevent. 2017;18(3):104–120. doi: 10.1177/1757177416680443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boscart VM, Fernie GR, Lee JH, Jaglal SB. Using psychological theory to inform methods to optimize the implementation of a hand hygiene intervention. Implementation Science. 2012;7(1):77. doi: 10.1186/1748-5908-7-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorencatto F, Charani E, Sevdalis N, Tarrant C, Davey P. Driving sustainable change in antimicrobial prescribing practice: how can social and behavioural sciences help? J Antimicrobial Chemotherapy. 2018;73(10):2613–2624. doi: 10.1093/jac/dky222 [DOI] [PubMed] [Google Scholar]
- 23.Keyworth C, Epton T, Goldthorpe J, Calam R, Armitage CJ. Acceptability, reliability, and validity of a brief measure of capabilities, opportunities, and motivations (“COM-B”). Br J Health Psychol. 2020. doi: 10.1111/bjhp.12417 [DOI] [PubMed] [Google Scholar]
- 24.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science. 2011;6(1):42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sc. 2011;6:42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herbeć A, Chimhini G, Rosenberg-Pacareu J, et al. Barriers and facilitators to infection prevention and control in a neonatal unit in Zimbabwe a theory-driven qualitative study to inform design of a behaviour change intervention. J Hosp Infect. 2020;106(4):804–811. doi: 10.1016/j.jhin.2020.09.020 [DOI] [PubMed] [Google Scholar]
- 27.Castro-Sánchez E, Alexander CM, Atchison C, et al. Evaluation of a personal protective equipment support programme for staff during the COVID-19 pandemic in London. J Hosp Infect. 2021;109:68–77. doi: 10.1016/j.jhin.2020.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lydon S, Greally C, Tujjar O, et al. Psychometric evaluation of a measure of factors influencing hand hygiene behaviour to inform intervention. J Hospital Infection. 2019;102(4):407–412. doi: 10.1016/j.jhin.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 29.Tomsic I, Ebadi E, Gossé F, et al. Determinants of orthopedic physicians’ self-reported compliance with surgical site infection prevention: results of the WACH-trial’s pilot survey on COM-B factors in a German University hospital. Antimicrob Resist Infect Control. 2021;10(1):67. doi: 10.1186/s13756-021-00932-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson Miller J, Hartman TK, Levita L, et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br J Health Psychol. 2020;25(4):856–864. doi: 10.1111/bjhp.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith JD, Corace KM, MacDonald TK, et al. Application of the Theoretical Domains Framework to identify factors that influence hand hygiene compliance in long-term care. J Hospital Infection. 2019;101(4):393–398. doi: 10.1016/j.jhin.2018.12.014 [DOI] [PubMed] [Google Scholar]
- 32.Li CH. Confirmatory factor analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48(3):936–949. doi: 10.3758/s13428-015-0619-7 [DOI] [PubMed] [Google Scholar]
- 33.Whittaker TA. Using the Modification Index and Standardized Expected Parameter Change for Model Modification. J Exp Educ. 2012;80(1):26–44. [Google Scholar]
- 34.Schreiber JB. Core reporting practices in structural equation modeling. Res Social Adm Pharm. 2008;4(2):83–97. doi: 10.1016/j.sapharm.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 35.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 36.Lai X, Wang X, Yang Q, et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Control. 2020;9(1):83. doi: 10.1186/s13756-020-00746-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qiao F, Huang W, Zong Z, Yin W. Infection prevention and control in outpatient settings in China-structure, resources, and basic practices. Am J Infect Control. 2018;46(7):802–807. doi: 10.1016/j.ajic.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 38.Jumaa PA. Hand hygiene: simple and complex. Int J Infect Dis. 2005;9(1):3–14. doi: 10.1016/j.ijid.2004.05.005 [DOI] [PubMed] [Google Scholar]
- 39.Shen L, Wang X, An J, et al. Implementation of WHO multimodal strategy for improvement of hand hygiene: a quasi-experimental study in a Traditional Chinese Medicine hospital in Xi’an, China. Antimicrob Resist Infect Control. 2017;6:98. doi: 10.1186/s13756-017-0254-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ataiyero Y, Dyson J, Graham M. Barriers to hand hygiene practices among health care workers in sub-Saharan African countries: a narrative review. Am J Infect Control. 2019;47(5):565–573. doi: 10.1016/j.ajic.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 41.Andriani Y, Nadjib M. The Importance of Implementation of Hand Hygiene Practice in Reducing Healthcare-associated Infections: a Systematic Review. KnE Life Sciences. 2018;4:135. doi: 10.18502/kls.v4i9.3565 [DOI] [Google Scholar]
- 42.Zhang S, Kong X, Lamb K, Wu Y. High nursing workload is a main associated factor of poor hand hygiene adherence in Beijing, China: an observational study: poor hand hygiene adherence and high workload. Int J Nurs Pract. 2019;25:e12720. doi: 10.1111/ijn.12720 [DOI] [PubMed] [Google Scholar]
- 43.El-Soussi AH, Asfour HI. A return to the basics; nurses’ practices and knowledge about interventional patient hygiene in critical care units. Intensive Crit Care Nurs. 2017;40:11–17. doi: 10.1016/j.iccn.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 44.Smith JD, Corace KM, MacDonald TK, et al. Application of the Theoretical Domains Framework to identify factors that influence hand hygiene compliance in long-term care. J Hosp Infect. 2019;101(4):393–398. doi: 10.1016/j.jhin.2018.12.014 [DOI] [PubMed] [Google Scholar]
- 45.Smiddy MP, O’ Connell R, Creedon SA. Systematic qualitative literature review of health care workers’ compliance with hand hygiene guidelines. Am J Infect Control. 2015;43(3):269–274. doi: 10.1016/j.ajic.2014.11.007 [DOI] [PubMed] [Google Scholar]
- 46.Wong MWH, Xu YZ, Bone J, Srigley JA. Impact of patient and visitor hand hygiene interventions at a pediatric hospital: a stepped wedge cluster randomized controlled trial. Am J Infect Control. 2020;48(5):511–516. doi: 10.1016/j.ajic.2019.09.026 [DOI] [PubMed] [Google Scholar]
- 47.Jeanes A, Coen PG, Drey NS, Gould DJ. The development of hand hygiene compliance imperatives in an emergency department. Am J Infect Control. 2018;46(4):441–447. doi: 10.1016/j.ajic.2017.10.014 [DOI] [PubMed] [Google Scholar]
- 48.Pittet D. Improving adherence to hand hygiene practice: a multidisciplinary approach. Emerg Infect Dis. 2001;7(2):234–240. doi: 10.3201/eid0702.010217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Price L, MacDonald J, Gozdzielewska L, et al. Interventions to improve healthcare workers’ hand hygiene compliance: a systematic review of systematic reviews. Infect Control Hospital Epidemiol. 2018;39(12):1449–1456. doi: 10.1017/ice.2018.262 [DOI] [PubMed] [Google Scholar]
- 50.De Wandel D, Maes L, Labeau S, Vereecken C, Blot S. Behavioral determinants of hand hygiene compliance in intensive care units. Am J Crit Care. 2010;19(3):230–239. doi: 10.4037/ajcc2010892 [DOI] [PubMed] [Google Scholar]
- 51.Lee K. Student and infection prevention and control nurses’ hand hygiene decision making in simulated clinical scenarios: a qualitative research study of hand washing, gel and glove use choices. J Infect Prev. 2013;14(3):96–103. doi: 10.1177/1757177413484784 [DOI] [Google Scholar]
- 52.Doronina O, Jones D, Martello M, Biron A, Lavoie-Tremblay M, Systematic A. Review on the Effectiveness of Interventions to Improve Hand Hygiene Compliance of Nurses in the Hospital Setting. J Nurs Scholarsh. 2017;49(2):143–152. doi: 10.1111/jnu.12274 [DOI] [PubMed] [Google Scholar]
- 53.Taneja J, Mishra B. Promotion of Successful Hand Hygiene practices in the Intensive Care Units of a Tertiary Care Hospital. J Patient Safety Infection Control. 2015;3(3):130–133. doi: 10.1016/j.jpsic.2015.11.004 [DOI] [Google Scholar]
- 54.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychologist. 2000;55(1):68–78. doi: 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 55.Salamati P, Poursharifi H, Rahbarimanesh AA, Koochak HE, Najafi Z. Effectiveness of motivational interviewing in promoting hand hygiene of nursing personnel. Int J Prev Med. 2013;4(4):441–447. [PMC free article] [PubMed] [Google Scholar]
- 56.Grol R. Successes and Failures in the Implementation of Evidence-Based Guidelines for Clinical Practice. Med Care. 2001;39:II46–54. doi: 10.1097/00005650-200108002-00003 [DOI] [PubMed] [Google Scholar]