Abstract
Purpose:
Developing effective deprescribing interventions relies on understanding attitudes, beliefs, and communication challenges of those involved in the deprescribing decision-making process, including the patient, the primary care clinician, and the pharmacist. The objective of this study was to assess patients’ beliefs and attitudes and identify facilitators of and barriers to deprescribing.
Methods:
As part of a larger study, we recruited patients ⩾18 years of age taking ⩾3 chronic medications. Participants were recruited from retail pharmacies associated with the University of Kentucky HealthCare system. They completed an electronic survey that included demographic information, questions about communication with their primary care clinician and pharmacists, and the revised Patients’ Attitudes Toward Deprescribing (rPATD) questionnaire.
Results:
Our analyses included 103 participants (n = 65 identified as female and n = 74 as White/Caucasian) with a mean age of 50.4 years [standard deviation (SD) = 15.5]. Participants reported taking an average of 8.4 daily medications (SD = 6.1). Most participants reported effective communication with clinicians and pharmacists (66.9%) and expressed willingness to stop one of their medications if their clinician said it was possible (83.5%). Predictors of willingness to accept deprescribing were older age [odds ratio (OR) = 2.99, 95% confidence interval (CI) = 1.45–6.2], college/graduate degree (OR = 55.25, 95% CI = 5.74–531.4), perceiving medications as less appropriate (OR = 8.99, 95% CI = 1.1–73.62), and perceived effectiveness of communication with the clinician or pharmacist (OR = 4.56, 95% CI = 0.85–24.35).
Conclusion:
Adults taking ⩾3 chronic medications expressed high willingness to accept deprescribing of medications when their doctor said it was possible. Targeted strategies to facilitate communication within the patient–primary care clinician–pharmacist triad that consider patient characteristics such as age and education level may be necessary ingredients for developing successful deprescribing interventions.
Plain Language Summary
Are patients willing to accept stopping medications?
Sometimes, medicines that a patient takes regularly become inappropriate. In other words, the risks of adverse effects might be greater than a medicine’s potential benefits. The decision to stop such medicines should involve the patient and consider their preferences. We surveyed a group of patients taking multiple medicines to see how they felt about having those medicines stopped. We also asked patients whether and how much they talk to their primary care clinician and pharmacists about their medicines. To qualify for this study, patients had to be at least 18 years old and to take three or more medicines daily; they also needed to speak English. Participants provided demographic information and answered questions about their medicines, their communication with primary care clinicians and pharmacists, and their feelings about having one or more of their medicines stopped. We recruited 107 people and were able to use responses from 103 of them. Their average age was 50 years; 65 of them identified as female, and 75 identified as White/Caucasian. Most of our participants mentioned having conversations with primary care clinicians and pharmacists and said they would be willing to stop a medication if their clinician said it was possible. Older participants, those with more years of education, those who thought their medications might lead to side effects, and those who communicated with their clinician or pharmacists were more willing to have one of their medicines stopped.
Our results indicate that patient characteristics and communication with clinicians and pharmacists are factors to consider when designing interventions to reduce the use of inappropriate medicines.
Keywords: communication, deprescribing, inappropriate medications, patient, polypharmacy
Introduction
The number of adults affected by polypharmacy, commonly defined as the use of five or more medications, is increasing, 1 with more adults experiencing polypharmacy in the United States than adults in other developed countries. 2 Although polypharmacy is not always inappropriate, 3 patients experiencing polypharmacy have a seven times higher risk for adverse effects due to inappropriate medication use (i.e. risks outweigh benefits). 4 High rates of comorbidities and over-prescribing in select clinical practices, along with the use of over-the-counter (OTC) medications, vitamins, and supplements, are important drivers of polypharmacy. 5 Regardless of the specific factors driving polypharmacy, measures to address it are important to consider.
Deprescribing is the thoughtful and systematic process of identifying problematic medications through a proper medication review conducted by a healthcare professional who reduces the dose of or completely withdraws inappropriate or unnecessary medications in a manner that is safe and effective, with the goal of maximizing patient health outcomes.6,7 Although clinician–pharmacist teams have been effective in previous deprescribing efforts,8–11 those efforts were mainly limited to older adults seen in settings with pharmacists available onsite or within research studies that were not sustained over time.12,13 The evidence from these studies underscores the importance of identifying factors for sustainable deprescribing interventions and expanding them to both younger populations and patients seen in a variety of health settings, including those that do not employ a staff pharmacist. 14
Past research indicates the value of patient-centeredness and shared decision-making focused on medication use; 15 however, there are communication barriers between members of the patient–clinician–pharmacist triad that challenge effective deprescribing interventions. 16 Consequently, understanding how to engage patients, clinicians, and pharmacists in communication concerning deprescribing in a unified and patient-centered manner is important for designing effective deprescribing interventions.
To understand the communication experiences and perceptions about deprescribing among members of the triad the research team conducted surveys with patients, clinicians, and community pharmacists in the Commonwealth of Kentucky. We recently published the results from the survey of clinicians and community pharmacists, the first study to compare primary care clinician and community pharmacist perceptions of deprescribing. 17 We identified important factors affecting the reported likelihood of deprescribing, including patient characteristics, time for counseling, communication, and trust within the clinician–patient–pharmacist triad. This article presents findings from the patient survey assessing beliefs and attitudes of patients taking multiple medications regarding deprescribing and their communication experiences with clinicians and pharmacists.
Methods
Study design and participants
As part of a larger study, 17 we conducted a cross-sectional survey of patients taking multiple medications. Participants were recruited in November 2019 by trained research assistants at retail pharmacies associated with the University of Kentucky HealthCare system, a tertiary healthcare system serving patients from across the Commonwealth of Kentucky. To qualify for the study, patients had to (1) be 18 years of age or older, (2) take at least three or more chronic medications (i.e. prescription medications, OTC medications, vitamins, and supplements), and (3) speak English. Given that our target population included a broader age range than typical deprescribing studies, we used a modified definition of polypharmacy, instead of the more commonly used definition of five or more medications for adults 65 years or older. The sample was one of convenience, based on the funding available to support the project and feasibility considerations. The target sample size of 100 participants meeting these eligibility criteria was determined a priori. There was no difference in the approach for recruitment based on age.
The survey was administered onsite at the retail pharmacies using iPads, and study data were collected using REDCap, a secure, HIPAA compliant, web-based software platform designed for electronic data capture.18,19 The survey took approximately 10 min to complete, and participants were compensated with a $10 gift card. To establish participant eligibility, the first survey question asked them to indicate the number of medications they take daily; all other questions were voluntary.
Measures
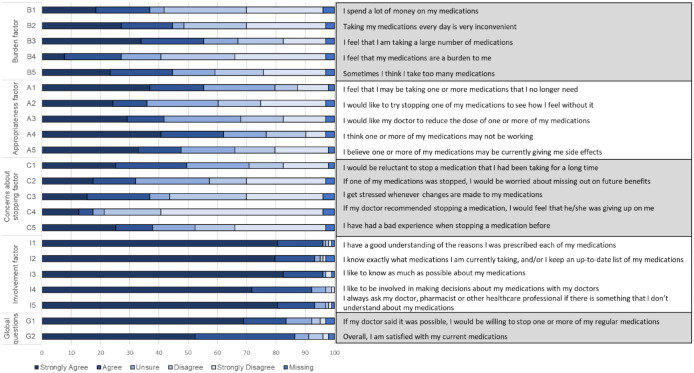
The survey was developed to assess patients’ beliefs, attitudes, and experiences with deprescribing and communication with healthcare providers. Participants provided demographic data and information about how often they visited the clinician who prescribes most of their medications, how often they communicated with this clinician and their pharmacist(s), and their perceived effectiveness of this communication. The revised Patients’ Attitudes Toward Deprescribing (rPATD) questionnaire comprised the remainder of the survey instrument. 20 The rPATD is a validated scale used to assess how patients feel about their medications and deprescribing. The rPATD contains 22 statements measured on a 5-point Likert-type scale (strongly agree to strongly disagree). The questionnaire includes two questions about overall satisfaction with medication use and willingness to accept deprescribing recommendations and 20 questions grouped into four validated factors: (1) perceived medication burden (Burden factor), (2) attitudes toward the appropriateness of medication prescribed (Appropriateness factor), (3) concerns about stopping medications (Concerns about stopping factor), and (4) how knowledgeable participants feel about their medication and how involved they feel in the medication decision-making process (Involvement factor). 20
Data analysis
Data analysis was performed using SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC, USA). 21 Descriptive statistics were used to characterize study participants and describe attitudes toward deprescribing. A logistic regression model with manual backward elimination was used to identify predictors associated with willingness to accept deprescribing, which was based on the global question ‘I would be willing to stop one or more of my medicines if my doctor said it was possible’. Models were constructed based on bivariable analysis with consideration for model fit [i.e. Akaike information criterion (AIC), r-squared] and number of variables. Responses were dichotomized to a binary outcome from the 5-point Likert-type scale. Specifically, we combined those who reported ‘strongly agree’ or ‘agree’ into the ‘agree’ category and those who reported ‘strongly disagree’, ‘disagree’, or ‘unsure’ into the ‘not agree’ category, as previously reported in the literature. 22 Demographic characteristics, perceived health status, perceived effective communication with clinician and pharmacist(s), number of medications, the use of a single pharmacy, and rPATD factor scores were considered as potential predictors and were evaluated for inclusion in the final logistic regression model. For the regression analysis, those with missing values on key characteristics were excluded.
Results
Participant demographics
Of the 107 patient participants who enrolled in the study, 103 were included in the analysis (three participants did not respond to any of the questions on the survey, and one reported <3 medications). Table 1 provides descriptive information on the study participants. Participants ranged in age from 19 to 86 years, with most participants identifying as female (n = 65) and White/Caucasian (n = 74). Participants reported taking an average of 8.4 total daily medications [standard deviation (SD) = 6.1, median = 7, interquartile range (IQR) = 4–10], with an average of 7.5 daily prescription medications (SD = 5.9, median = 6, IQR = 4–9.5). Most participants (n = 74) indicated that the prescription medications they were currently taking were prescribed by their primary care clinician, and almost half visited with their prescribing clinician every 3 months (n = 49). About half of the participants indicated that the pharmacy of choice for filling most of their prescriptions was associated with the hospital or clinic in which they received care (n = 56). When asked about their perceived health status (‘I believe I am a healthy individual’), more than half of the participants who responded (n = 100) somewhat agreed (n = 34) or strongly agreed (n = 21) with the statement, about a third somewhat disagreed (n = 13) or strongly disagreed (n = 16) with the statement, and the rest (n = 16) were unsure. Most of the study participants (n = 86) reported being willing to stop one of their medications if their clinician said it was possible. Responses to all the individual questions included in the rPATD questionnaire are presented in Figure 1, with summary information on factor scores and perception of communication with clinicians and pharmacists available in Table 2.
Table 1.
Characteristics of study participants (N = 103).
| Characteristic | ||
|---|---|---|
| Age | Mean (SD) | 50.4 (15.5) |
| Median (IQR) | 51.5 (39.5–62) | |
| Sex: n (%) | Female | 65 (63.1) |
| Male | 31 (30.1) | |
| Missing | 7 (6.8) | |
| Race a : n (%) | Black or African American | 17 (16.5) |
| White or Caucasian | 74 (71.8) | |
| More than one | 9 (8.7) | |
| Missing | 3 (2.9) | |
| Education: n (%) | High school or less | 32 (31.1) |
| Some college/college degree | 55 (53.4) | |
| Graduate level | 13 (12.6) | |
| Missing | 3 (2.9) | |
| Number of medications: n (%) | 3–4 | 29 (28.2) |
| 5–9 | 45 (43.7) | |
| >9 | 29 (28.2) | |
| Perceived health status b : n (%) | Excellent or very good | 29 (28.2) |
| Good | 42 (40.8) | |
| Fair or poor | 29 (28.2) | |
| Using single pharmacy: n (%) | Yes | 90 (87.38) |
| No | 12 (11.65) | |
| Missing | 1 (0.97) | |
IQR, interquartile range; SD, standard deviation.
Race categories included American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, Southeast Asian, White or Caucasian, and other. Participants could select more than one category.
Participant was asked to respond to ‘In general, would you say that your health is . . .’.
Figure 1.
Attitudes toward deprescribing: rPATD individual questions.
Table 2.
Patient perceptions of medication-related communication and attitudes toward deprescribing.
| Effective communication about medications with clinician and pharmacist: n (%) | Strongly agree/agree | 69 (66.9) |
| Unsure | 23 (22.3) | |
| Disagree/strongly disagree | 7 (6.8) | |
| rPATD Appropriateness factor | Median (IQR) | 3.4 (2.6–4.2) |
| Mean (SD) | 3.4 (1.12) | |
| rPATD Burden factor | Median (IQR) | 3.0 (2.0–4.0) |
| Mean (SD) | 2.94 (1.18) | |
| rPATD Concerns about stopping factor | Median (IQR) | 2.6 (2.0–3.2) |
| Mean (SD) | 2.75 (1.05) | |
| rPATD Involvement factor | Median (IQR) | 5.0 (4.6–5.0) |
| Mean (SD) | 4.72 (0.59) | |
| rPATD Global question – Satisfaction with current medications | Median (IQR) | 5.0 (4.0–5.0) |
| Mean (SD) | 4.32 (0.93) | |
| rPATD Global question – Willingness to stop medication | Median (IQR) | 5.0 (4.0–5.0) |
| Mean (SD) | 4.5 (0.93) |
IQR, interquartile range; rPATD, revised Patients’ Attitudes Toward Deprescribing; SD, standard deviation.
Responses on the rPATD are measured on a 5-point Likert-type scale (5 = strongly agree to 1 = strongly disagree).
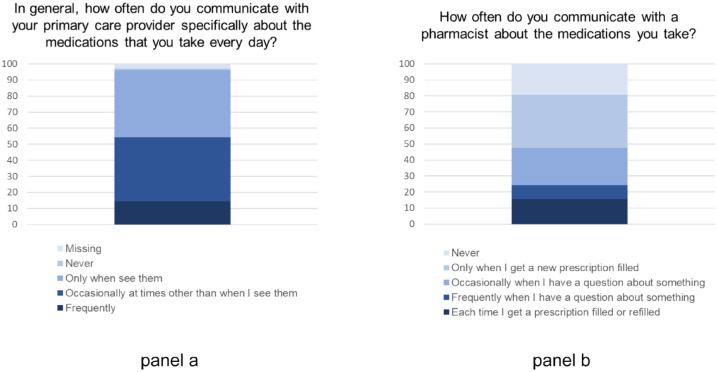
Regarding their communication with clinicians and pharmacists, almost all participants reported communicating with their primary care clinician (n = 99); however, one in five indicated never communicating with the pharmacist (n = 20) (Figure 2). When communication occurred, most participants agreed or strongly agreed that the communication about medications with their clinician or the pharmacist was effective (n = 69) (Table 2).
Figure 2.
Communication with primary care provider (panel a) and pharmacist (panel b).
Table 3 provides detailed information on the logistic regression analysis to identify predictors for willingness to accept deprescribing, including unadjusted odds ratios (ORs) with 95% confidence intervals (CIs) for every factor considered as a potential predictor, adjusted ORs and 95% CI based on the full model, and adjusted ORs and 95% CI based on the final model after backward selection. In the final model, factors predicting higher odds of willingness to accept deprescribing were age (OR = 2.99, 95% CI = 1.45–6.2 for every 10 years increase), college or graduate degree compared with high school or less (OR = 55.25, 95% CI = 5.74–531.4), perceiving medications as less appropriate (OR = 8.99, 95% CI = 1.1–73.62), and perceived effectiveness of communication with the clinician or pharmacist (OR = 4.56, 95% CI = 0.85–24.35). Those with higher levels of concern over stopping medications had lower odds of willingness to accept deprescribing (OR = 0.08, 95% CI = 0.01–0.66).
Table 3.
Factors predicting willingness to accept deprescribing.
| Characteristic | Crude OR (95% CI) | Adjusted OR (95% CI) full model | Adjusted OR (95% CI) reduced model* |
|---|---|---|---|
| Age (for 10 years increase) | 1.51 (1.02–2.23) | 11.47 (1.44–91.61) | 2.99 (1.45–6.2) |
| Sex (reference: male) | 0.65 (0.16–2.61) | 0.05 (0.002–1.49) | – |
| Race (reference: white) | |||
| Black or African American | 3.15 (0.38–26.02) | 1.75 (0.01–228.51) | – |
| Other | 1.57 (0.18–13.77) | 0.005 (<0.001–3.44) | – |
| Education (reference: high school or less) | 11.18 (2.84–43.91) | >999.99 (10.67–>999.99) | 55.25 (5.74–531.39) |
| Number of medications (per one medication increase) | 1.18 (0.98–1.43) | 1.11 (0.74–1.68) | – |
| Polypharmacy (reference: <5 medications/day): | |||
| 5–9 medications/day | 1.34 (0.4–4.49) | – | – |
| 10 or more medications/day | 7.04 (0.79–62.86) | – | – |
| rPATD: Appropriateness factor (reference: ⩾median) | 1.88 (0.55–6.5) | 267.52 (0.93–>999.99) | 8.99 (1.1–73.62) |
| rPATD: Burden factor (reference: <median) | 3.16 (0.92–10.86) | 0.75 (0.03–17.93) | – |
| rPATD: Concern about stopping factor (reference: <median) | 0.42 (0.12–1.44) | <0.001 (<0.001–0.47) | 0.08 (0.01–0.66) |
| Using single pharmacy | 1.25 (0.24–6.42) | 52.58 (0.14–>999.99) | – |
| Effective communication (reference: disagree or unsure) | 3.34 (1.01–11.02) | 43.16 (0.95–>999.99) | 4.56 (0.85–24.35) |
| Perceived health status (reference: excellent or very good) | |||
| Good | 0.8 (0.21–3.03) | 0.004 (<0.001–0.48) | – |
| Fair or poor | 1.33 (0.27–6.58) | 0.05 (<0.001–5.11) | – |
CI, confidence intervals; OR, odds ratio; rPATD, revised Patients’ Attitudes Toward Deprescribing.
c-statistic = 0.93, Hosmer–Lemeshow’s test (p = 0.98).
Discussion
This article reports on the findings from a survey of adult patients taking three or more medications on a regular basis. The survey was conducted as part of a larger study that also recruited primary care clinicians and pharmacists to investigate attitudes toward deprescribing, as well as barriers and facilitators to deprescribing. The results of this study align with other studies evaluating attitudes toward deprescribing, which found that 70–93% of participants were willing to have a medication stopped.22–28 In our sample of adult patients, we found that most participants (83.5%) were willing to have one of their medications discontinued if their doctor said it was possible.
The patient survey identified effective communication between patient and clinician and pharmacist as a predictor of willingness to have a medication stopped. Similarly, our survey of primary care clinicians and pharmacists identified communication, as well as trust within the clinician–patient–pharmacist triad, as important to the deprescribing process. 17 Although we did not specifically include questions related to trust within the clinician–patient–pharmacist triad in the patient survey, the survey did investigate patients’ perceptions of communication with primary care clinicians and pharmacists in further detail. We learned that, whereas most of our participants reported some level of communication with their primary care clinicians, one in five reported never communicating with a pharmacist about the medications they were taking. Considering that most participants reported using only one pharmacy to fill their prescriptions and that existing communication with primary care clinicians and pharmacists was perceived as effective, this study indicates a window of opportunity in (1) educating patients about the importance of engaging in discussions not only with their physicians but also with pharmacists and (2) finding ways to create and optimize channels of communication among the members of the patient–primary care clinician–pharmacist triad. 16
The importance of facilitating conversations is also supported by our finding that patients who reported effective communication with primary care clinicians and pharmacists had greater willingness to accept deprescribing if their clinicians said it was possible, whereas patients reporting higher concerns about stopping their medications had lower willingness to accept deprescribing. Because communication plays such a central role in our quest to identify effective ways to address the problem of polypharmacy and inappropriate prescribing, our previous finding that physicians and pharmacists perceive lack of time as an important barrier to deprescribing 17 becomes essential to address. Although healthcare systems might not easily adapt to allow more time for primary care clinicians to engage patients in conversations about deprescribing, possible solutions include educational interventions targeting the patient, as well as models of care that (1) streamline the deprescribing process using structured protocols, (2) recognize the role pharmacists can play in driving deprescribing and treatment optimization efforts in the community setting, (3) allow for a wider implementation of designated deprescribing clinics, and (4) recognize the importance of actively integrating pharmacists in primary care settings. Given the questions included in our survey and the use of a convenience sample for this study, this study cannot provide insights on the value of these strategies. Additional research is needed to evaluate the strategies in addressing perceived barriers and implementing effective deprescribing interventions involving patients, providers, and pharmacists in primary care settings.
Patient characteristics such as older age, which has been linked previously11,29,30 to increasing comorbidity and medication burden, and higher education were shown in our multivariable regression analysis to increase the odds of willingness to accept medications being stopped when their doctor said it was possible to do so. Whereas most previous research focused on older adults with polypharmacy and multiple chronic conditions, a population for whom polypharmacy and inappropriate prescribing might be perceived of higher importance,1,11,31 it is important to note that this study included younger adults who may not meet the more commonly used definition of polypharmacy (i.e. five medications or more). Including younger adults allowed this study to reveal that, like the older adults in our sample, they were also willing to accept deprescribing if their doctor said it was possible. This was also shown by an earlier study of women living in Appalachia Kentucky reporting that younger adults are open to deprescribing. 28 Another important finding from our survey was that willingness to accept deprescribing was not influenced by the number of medications or whether the participant met the formal definition of polypharmacy. This indicates the opportunity for primary prevention of polypharmacy by engaging younger patients and those taking less than five or more medications in conversations about deprescribing. This study also identified education as a predictor of willingness to accept deprescribing. Although education is a non-modifiable factor, it still can be considered when developing interventions to address medication-related problems by targeting intervention materials to account for education level. Future studies could evaluate the effectiveness of such tailored materials and targeted communication strategies on deprescribing acceptance.
Limitations
This study had several limitations that should be considered when interpreting our findings and attempting to generalize them. This study was conducted using a small convenience sample of people who were picking up prescriptions at retail pharmacies associated with a tertiary healthcare system in the Commonwealth of Kentucky. Although these pharmacies serve patients from across of the Commonwealth, they are likely not representative of the entire population living in Kentucky. Comparing our results with the results of the recent Kentucky census, we found that our sample included more Black or African American participants (17.8%) than the general population (8.5%); participants in our sample also were more educated (66% reported some college or higher education) than the general population (51.3%).32,33
Another important limitation of this study is that we used a hypothetical situation to evaluate participants’ willingness to accept stopping a chronic medication when faced with a deprescribing proposition. In addition, the scenarios presented to participants did not specify medications; therefore, it is unclear whether deprescribing acceptance differs by the indication or type of medication (e.g. a multivitamin versus an opioid). To our knowledge, no study to date has investigated whether willingness to accept deprescribing translates into acceptance of deprescribing in a real setting. Because our team was not directly involved in the care of the participants responding to our survey and because the questionnaire was self-administered, anonymous, and allowed participants to skip any question they did not want to answer, we believe the potential for desirability bias (i.e. over-reporting of willingness to accept deprescribing) was reduced, however.
Finally, the confidence intervals for the OR estimates from the multivariable logistic regression analysis are wide, possibly because of the small sample size, the fact that we used a convenience sample, or our inability to collect information on other predictors of deprescribing, notably specific medications and indications. As a result, the value of the point estimates should be considered with caution.
Conclusion
Participants in this study were willing to accept deprescribing of medications when their doctor said it was possible. This study revealed important factors to consider when developing interventions to reduce inappropriate medication use, including age, level of education, perceived medication appropriateness, patients’ concern with stopping medications, and perceived effectiveness of communication with the clinician or pharmacist. Targeted strategies to facilitate communication within the patient–primary care clinician–pharmacist triad may help deprescribing interventions succeed.
Supplemental Material
Supplemental material, sj-docx-1-taw-10.1177_20420986221116465 for Patients’ attitudes toward deprescribing and their experiences communicating with clinicians and pharmacists by Kaylee M. Lukacena, James W. Keck, Patricia R. Freeman, Nancy Grant Harrington, Mark J. Huffmyer and Daniela C. Moga in Therapeutic Advances in Drug Safety
Acknowledgments
The authors thank Drs Amelia L. Bradshaw, Sara L. Hamilton, Melissa L. Jackson, Megan J. Ma, Brittany N. McHolan, Bao-Han N. Nguyen, Mary Sau, Ana Vo, and Morgan Vogel for helping with data collection for this study. The authors also thank Mrs Teri Timmons and Mrs Hannah Keeler for providing administrative support for the study.
Footnotes
ORCID iD: Daniela C. Moga  https://orcid.org/0000-0002-3648-8197
https://orcid.org/0000-0002-3648-8197
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Kaylee M. Lukacena, Center for Social and Behavioral Science, Office of the Vice Chancellor for Research and Innovation, University of Illinois Urbana-Champaign, Urbana, IL, USA
James W. Keck, Department of Family and Community Medicine, College of Medicine, University of Kentucky, Lexington, KY, USA
Patricia R. Freeman, Department of Pharmacy Practice and Science, College of Pharmacy, University of Kentucky, Lexington, KY, USA
Nancy Grant Harrington, Department of Communication, College of Communication and Information, University of Kentucky, Lexington, KY, USA.
Mark J. Huffmyer, Department of Pharmacy Practice and Science, College of Pharmacy, University of Kentucky, Lexington, KY, USA
Daniela C. Moga, Department of Pharmacy Practice and Science, College of Pharmacy, University of Kentucky, Lexington, KY, USA. Department of Epidemiology, College of Public Health, University of Kentucky, Lexington, KY, USA; Sanders-Brown Center on Aging, University of Kentucky, 789 South Limestone Street, Lexington, KY 40536, USA.
Declarations
Ethics approval and consent to participate: The study was approved by the University of Kentucky Institutional Review Board (IRB# 53162); informed consent was implied as participants read a cover letter providing a brief description of the study, along with risks and potential benefits, before starting the survey.
Consent for publication: Not Applicable.
Author contributions: Kaylee M. Lukacena: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Writing – original draft; Writing – review & editing.
James W. Keck: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Writing – review & editing.
Patricia R. Freeman: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Writing – review & editing.
Nancy Grant Harrington: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Writing – review & editing.
Mark J. Huffmyer: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Writing – review & editing.
Daniela C. Moga: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The project was supported by the pilot funding from the Igniting Research Collaborations Grant (University of Kentucky), the NIH National Center for Advancing Translational Sciences through grant no. UL1TR001998, and the National Institute of Aging (R01AG054130). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or NIA.
Competing interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Data are available upon reasonable request.
References
- 1. Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017; 17: 230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Quinn KJ, Shah NH. A dataset quantifying polypharmacy in the United States. Sci Data 2017; 4: 170167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cadogan CA, Ryan C, Hughes CM. Appropriate polypharmacy and medicine safety: when many is not too many. Drug Saf 2016; 39: 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moriarty F, Hardy C, Bennett K, et al. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 2015; 5: e008656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kessler C, Ward MJ, McNaughton CD. Reducing adverse drug events: the need to rethink outpatient prescribing. JAMA 2016; 316: 2092–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reeve E, Thompson W, Farrell B. Deprescribing: a narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. Eur J Intern Med 2017; 38: 3–11. [DOI] [PubMed] [Google Scholar]
- 7. Reeve E, Gnjidic D, Long J, et al. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol 2015; 80: 1254–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kaur S, Mitchell G, Vitetta L, et al. Interventions that can reduce inappropriate prescribing in the elderly: a systematic review. Drugs Aging 2009; 26: 1013–1028. [DOI] [PubMed] [Google Scholar]
- 9. Patterson SM, Hughes C, Kerse N, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 2012; 5: CD008165. [DOI] [PubMed] [Google Scholar]
- 10. Page AT, Clifford RM, Potter K, et al. The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol 2016; 82: 583–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Steinman MA. Polypharmacy-time to get beyond numbers. JAMA Intern Med 2016; 176: 482–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moga DC, Abner EL, Rigsby DN, et al. Optimizing medication appropriateness in older adults: a randomized clinical interventional trial to decrease anticholinergic burden. Alzheimers Res Ther 2017; 9: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Martinez AI, Abner EL, Jicha GA, et al. One-year evaluation of a targeted medication therapy management intervention for older adults. J Manag Care Spec Pharm 2020; 26: 520–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Elbeddini A, Sawhney M, Tayefehchamani Y, et al. Deprescribing for all: a narrative review identifying inappropriate polypharmacy for all ages in hospital settings. BMJ Open Qual 2021; 10: e001509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reeve E, Denig P, Hilmer SN, et al. The ethics of deprescribing in older adults. J Bioeth Inq 2016; 13: 581–590. [DOI] [PubMed] [Google Scholar]
- 16. Foley RA, Hurard LL, Cateau D, et al. Physicians’, nurses’ and pharmacists’ perceptions of determinants to deprescribing in nursing homes considering three levels of action: a qualitative study. Pharmacy 2020; 8: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Huffmyer MJ, Keck JW, Harrington NG, et al. Primary care clinician and community pharmacist perceptions of deprescribing. J Am Geriatr Soc 2021; 69: 1686–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95: 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reeve E, Low LF, Shakib S, et al. Development and validation of the revised patients’ attitudes towards deprescribing (rPATD) questionnaire: versions for older adults and caregivers. Drugs Aging 2016; 33: 913–928. [DOI] [PubMed] [Google Scholar]
- 21. SAS v9.4 . Cary, NC: SAS Institute Inc., 2013. [Google Scholar]
- 22. Reeve E, Low LF, Hilmer SN. Attitudes of older adults and caregivers in Australia toward deprescribing. J Am Geriatr Soc 2019; 67: 1204–1210. [DOI] [PubMed] [Google Scholar]
- 23. Galazzi A, Lusignani M, Chiarelli MT, et al. Attitudes towards polypharmacy and medication withdrawal among older inpatients in Italy. Int J Clin Pharm 2016; 38: 454–461. [DOI] [PubMed] [Google Scholar]
- 24. Kalogianis MJ, Wimmer BC, Turner JP, et al. Are residents of aged care facilities willing to have their medications deprescribed? Res Social Adm Pharm 2016; 12: 784–788. [DOI] [PubMed] [Google Scholar]
- 25. Ng WL, Tan MZW, Koh EYL, et al. Deprescribing: what are the views and factors influencing this concept among patients with chronic diseases in a developed Asian community? Proc Singap Healthc 2017; 26: 172–179. [Google Scholar]
- 26. Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Social Adm Pharm 2017; 13: 864–870. [DOI] [PubMed] [Google Scholar]
- 27. Reeve E, Wiese MD, Hendrix I, et al. People’s attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc 2013; 61: 1508–1514. [DOI] [PubMed] [Google Scholar]
- 28. Martinez A, Spencer J, Moloney M, et al. Attitudes toward deprescribing in a middle-aged health disparities population. Res Social Adm Pharm 2020; 16: 1502–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Steinman MA. Polypharmacy and the balance of medication benefits and risks. Am J Geriatr Pharmacother 2007; 5: 314–316. [DOI] [PubMed] [Google Scholar]
- 30. Jyrkka J, Enlund H, Korhonen MJ, et al. Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging 2009; 26: 1039–1048. [DOI] [PubMed] [Google Scholar]
- 31. Steinman MA, Hanlon JT. Managing medications in clinically complex elders: ‘there’s got to be a happy medium’. JAMA 2010; 304: 1592–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.https://www.census.gov/quickfacts/KY (accessed 16 September 2021).
- 33.https://statisticalatlas.com/state/Kentucky/Educational-Attainment (accessed 16 September 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-taw-10.1177_20420986221116465 for Patients’ attitudes toward deprescribing and their experiences communicating with clinicians and pharmacists by Kaylee M. Lukacena, James W. Keck, Patricia R. Freeman, Nancy Grant Harrington, Mark J. Huffmyer and Daniela C. Moga in Therapeutic Advances in Drug Safety