Abstract
Introduction
Workplace violence (WPV) is associated with adverse consequences for patients and health care workers (HCWs). The aim of this study was to assess the prevalence of WPV against HCWs in the hospital and pre-hospital settings.
Methods
Using PRISMA guidelines, data resources including Scopus, PubMed, Web of Science, and Google Scholar were used for the search. The searches were conducted without any time limit until the end of December 2021. The random-effects model was used for this meta-analysis. I2 index was used to examine heterogeneity and the Egger test was used to examine publication bias.
Results
Of the 255 studies identified, 14 studies entered the umbrella review. The overall prevalence was as follows: WPV (58.7%); physical violence (20.8%); verbal violence (66.8%); and sexual harassment (10.5%).
Conclusion
The prevalence of WPV and its types against HCWs is relatively high. WPV is associated with physical, psychological, and occupational consequences. Measures should be taken to reduce the consequences of WPV.
Keywords: workplace violence, health care workers, occupational risk, health care professionals, violence
Introduction
Workplace violence (WPV) is a situation in which a person is harassed, threatened, or attacked at work (1). According to the World Health Organization (WHO), WPV includes physical and psychological violence (2). WPV is a major issue in healthcare settings in both hospital and pre-hospital settings (3). Unfortunately, WPV is on the rise in all health care settings (4). Many factors such as night work, high stress, lack of resources, disproportionate gender representation, and inadequate workplace security can lead to WPV (5).
Health care workers (HCWs) are at high risk for exposure to WPV (6, 7). According to studies, 50–88% of HCWs have been exposed to WPV (3). Depending on the type and setting of the health care environments, the rates can be higher. For example, up to 90% of emergency medicine HCWs report some degree of WPV (4). Similarly, 83% of pre-hospital emergency medical technicians experience WPV at least once a year (8).
WPV for HCWs may be associated with negative consequences such as low job satisfaction, change of profession, and work absenteeism (9, 10). Additionally, the experience of WPV is associated with decreased self-esteem, increased anxiety, and stress (11–13). Furthermore, WPV toward HCWs can lead to reduced quality of patient care (14).
Numerous systematic review and meta-analysis studies of WPV against HCWs have been conducted, but a comprehensive evaluation summarizing the results is lacking. This umbrella review serves as a data reference for policymakers in the field of health care. The aim was to assess the prevalence of WPV against HCWs in hospital and pre-hospital settings.
Methods
This study was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (15). The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with code CRD42022296244.
Search strategy
Data resources including Scopus, PubMed, Web of Science, and Google Scholar were used to identify the studies. Related keywords, search fields and operators were used to formulate search strategies. Initially, a search strategy was developed for the PubMed database, and then other search strategies were designed in accordance with the PubMed database. The searches were conducted in English without any time limit until the end of December 2021. Search strategies for the types of databases are listed in Table 1.
Table 1.
Search strategies for types of databases.
| Database | Search strategy |
|---|---|
| Pubmed | ((“Workplace violence*”[tiab] OR aggression* OR “harassment*” OR bullying OR “workplace bullying” OR assault* OR abuse OR “physical abuse” OR violence OR “assaultive behavior”) AND (“health care provider*” OR “health personnel” OR “healthcare provider*” OR “health care worker*” OR “medical staff” OR “medical worker*” OR “healthcare professional*”) AND (“systematic review”[tiab]) AND (“meta-analysis”[tiab] OR “meta-analytic”)) |
| Scopus | ((TITLE - ABS (“workplace violence*”) OR ALL(aggression*) OR ALL(“harassment*”) OR ALL(bullying) OR ALL(“workplace bullying”) OR ALL(assault*) OR ALL(abuse) OR ALL(“physical abuse”) OR ALL (violence) OR ALL(“assaultive behavior”)) AND (ALL(“health care provider*”) OR ALL(“health personnel”) OR ALL(“healthcare provider*”) OR ALL(“health care worker*”) OR ALL(“medical staff”) OR ALL(“medical worker*”) OR ALL(“health care professional*”)) AND (TITLE-ABS (“systematic review”)) AND (TITLE-ABS(“meta-analysis”) OR ALL(“meta-analytic”))) |
| Web of Science | ((TS= (“workplace violence*”) OR TS= (aggression*) OR TS= (“harassment*”) OR TS= (bullying) OR TS= (“workplace bullying”) OR TS= (assault*) OR TS= (abuse) OR TS= (“physical abuse”) OR TS= (violence) OR TS= (“assaultive behavior”)) AND (TS= (“health care provider*”) OR TS= (“health personnel”) OR TS= (“health care provider*”) OR TS= (“healthcare worker*”) OR TS= (“medical staff”) OR TS= (“medical worker*”) OR TS= (“health care professional*”)) AND (TI= (“systematic review”)) AND (TI= (“meta-analysis”) OR TS= (“meta-analytic”))) |
Eligible criteria
All studies that reported the prevalence of WPV and its types in HCWs by meta-analysis were included. Exclusion criteria were the prevalence of WPV in home health workers and non-meta-analysis studies.
Selection of studies
EndNote X7 software was used to manage search results. The initial identified studies were entered into this software. Duplicates were removed and exclusion/inclusion criteria were applied. The full text of the remaining studies were independently reviewed by two researchers (AS, MG) and the final studies were selected for quality evaluation.
Quality assessment and data extraction
Two researchers (AS, MG) independently used the AMSTAR-2 (A Measurement Tool to Assess Systematic Reviews, version 2) tool for qualitative evaluation of the selected studies (16). This tool has 16 items and the answer to each question is binary. The results were classified into four critical levels: Very low, low, medium, and high. For data extraction, the same two researchers, independently used a checklist designed in Word 2016 software to extract data including the first author of the study, place of study, number of reviewed studies, heterogeneity, publication bias, the prevalence of WPV and its variants from each study.
Statistical analysis
The random-effects model was used for the meta-analysis. Heterogeneity between studies was assessed by the I2 index. Heterogeneity <25%, 25–50%, 50–75, and more than 75%, respectively, indicated no, moderate, high, or very high heterogeneity (17, 18). Publication bias was assessed using the Egger test. The data was analyzed using STATA software (version 14).
Results
Search results
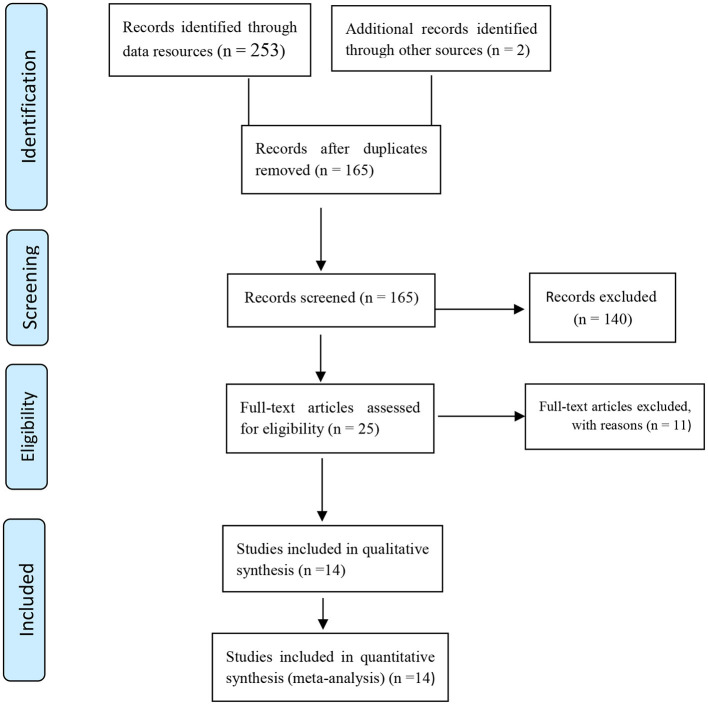
After the comprehensive search, 255 initial studies were identified and after removing duplicates, 165 studies were screened and finally, 14 studies were qualitatively evaluated and entered the meta-analysis phase. Figure 1 shows the selection stages of the studies.
Figure 1.
Flowchart of the selection of studies based on PRISMA.
Characteristics of studies
In the 14 final studies included in the meta-analysis, 674,266 health care workers were studied. Table 2 shows the characteristics and data of each study separately.
Table 2.
The characteristic of studies included in the umbrella review and meta-analysis.
| References | Location | Sample size | Prevalence of overall WPV | Number of studies | Heterogeneity (I2) | Publication bias | Group studied |
|---|---|---|---|---|---|---|---|
| Azami et al. (19) | Iran | 10,858 | Verbal: 80.8% (95% CI:74.2–86.0) Physical: 24.8% (95% CI: 17.4–34) |
26 | Physical (I2 = 97%) Verbal (I2 =97.76%) | Begg and Egger's tests (no publication bias) | Nurses |
| Sahebi et al. (20) | Iran | 1,257 | Physical: 36.39% (95%CI: 27.29–45.50) Verbal: 73.13% (95% CI: 68.64–77.62) |
9 | Physical (I2 = 90.8%) Verbal (I2 = 62.7%) Cultural (I2 = 94.7%) | Begg's (p = 0.361) | Emergency Medical Personnel |
| Li et al. (21) | China | 61,800 | Physical: 19.33% (95% CI: 16.49–22.53%) |
65 | I2 = 98.8% | Begg's (P = 0.1012) | HCWs |
| Varghese et al. (22) | India | 42,222 | WPV: 58% (95% CI: 51–64) Verbal: 64% (95%CI: 59–70) Physical: 23% (CI: 14–34) Sexual harassment: 12% (95%CI: 7–17) |
38 | WPV (I2 = 99.26%) Verbal (I2 = 98.78%) Physical (I2 = 99.68%) | Egger's WPV (P = 0.18) Verbal (p = 0.81) Physical (p = 0.561) |
Nurses |
| Nowrouzi-Kia et al. (23) | Canada | 10,786 | WPV: 69% (95% CI: 58–78) |
6 | I2 = 0.974 | - | Physicians |
| Hossain et al. (24) | India | 2,849 | Verbal: 52% (95% CI: 45–60) Physical: 8% (95% CI: 5–11) WPV: 63% (95% CI: 54–72) |
15 | WPV (I2 =96.15%) Verbal (I2 = 93.90%) Physical (I2 = 93.70%) | - | HCWs |
| Dalvand et al. (25) | Iran | 5,639 | Verbal: 74% (95% CI: 66–83) Physical: 28% (95% CI: 21–35) |
22 | - | Egger's (P = 0.03) | Nurses |
| Liu et al. (26) | China | 331,544 | Physical: 24.4% (95% CI 22.4–26.4) Verbal: 57.6% (95% CI 51.8–63.4) Sexual harassment: 12.4% (95% CI: 10.6–14.2) WPV: 61.9% (95% CI 56.1–67.6) |
158 | - | - | HCWs |
| Liu et al. (27) | China | 22,968 | WPV: 71% (95% CI: 67–75) Verbal: 63% (95% CI: 58–67). Physical: 14% (95% CI: 11–18) Sexual harassment was 6% (95%CI: 4–9) |
38 | WPV (I2 = 98%) Physical (I2 = 98%) Verbal (I2 = 98%) |
Egger's (no publication bias) | Nurses |
| Lu et al. (28) | China | 78,026 | WPV: 62.4% (95% CI: 59.4–65.5) Physical: 13.7% (95% CI:12.2–15.1) Verbal: 61.2% (95% CI: 55.1–67.4) Sexual harassment: 6.3% (95% CI: 5.3–7.4) |
44 | Physical (I2 = 97.1) Verbal (I2 = 99%) Sexual harassment (I2 = 96.5%) |
WPV: Begg's (p = 0.229) |
HCWs |
| Shabanikiya et al. (29) | Iran | 8,694 | WPV: 66 % (95% CI: 20–111) Physical: 25% (95%CI: 16–34), Verbal: 58% (95%CI: 29–86) Sexual harassment: 16% (95%CI: 9–22) |
11 | WPV (I2 = 99.94%) Physical (I2 = 99.31%) | Egger's (P = 0.094) | Emergency Medical Personnel |
| Zeng et al. (30) | China | 39,486 | sexual harassment: 7.5% (95% CI: 5.5–10.1) |
37 | I2 = 97.79% | Egger's (P = 0.57) | Nurses |
| Lu et al. (31) | China | 52,345 | Sexual harassment in last 12 month: 13% (11–14) Sexual harassment in nursing career: 53.4% (95% CI: 23.1–83.7) |
34 | Sexual harassment in last 12 month (I2 = 98.6%) Sexual harassment in Nursing career (I2 = 99.7%) |
- | Nurses |
| Aljohani et al. (32) | USA | 5,792 | Verbal: 77 % (95% CI: 72–82) WPV: 24 % (95% CI: 18–31) |
22 | Verbal (I2 = 97%) WPV (I2 = 93%) |
- | HCWs |
HCWs, Healthcare Workers.
Meta-analysis results
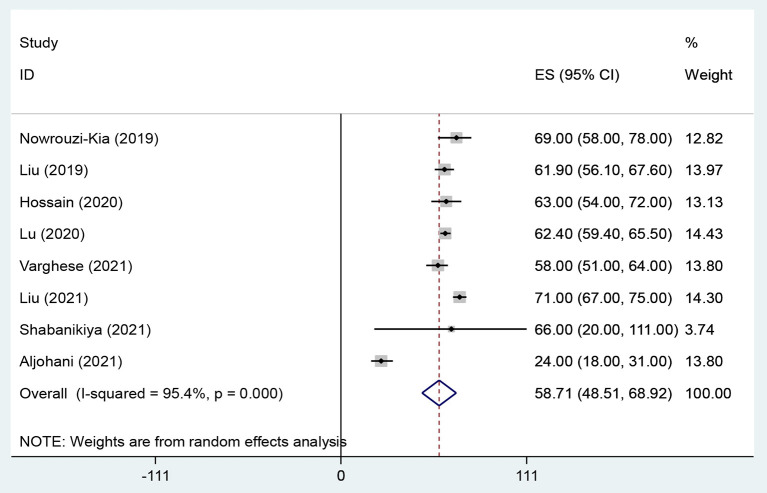
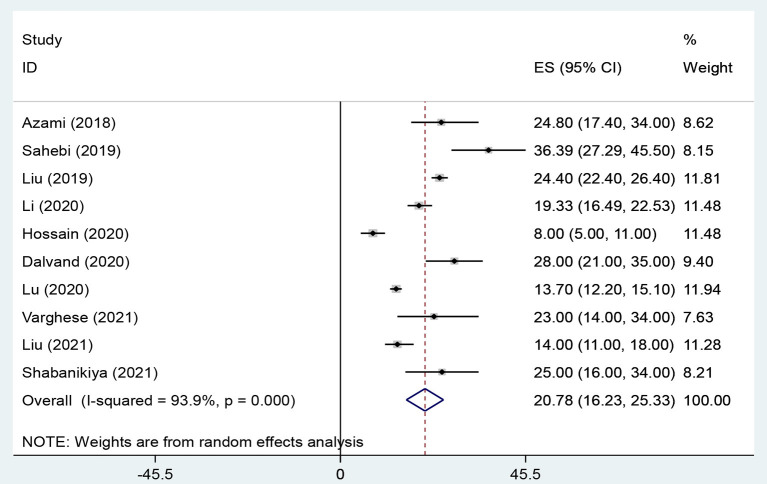
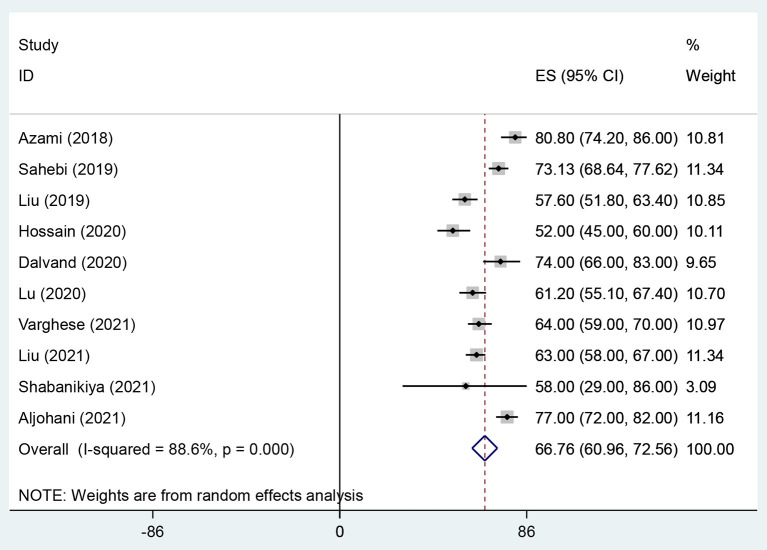
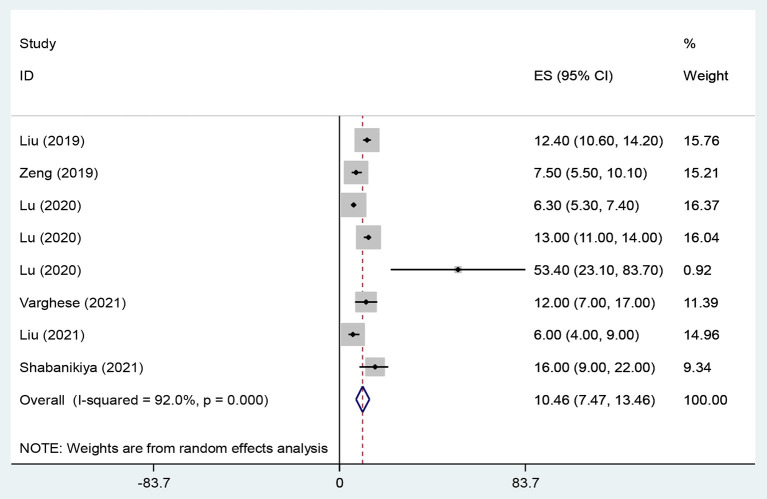
The overall prevalence of WPV, physical violence, verbal violence and sexual harassment in health care workers were 58.7% (95% CI: 48.51–68.92, I2 = 95.4%, p < 0.001) (Figure 2), 20.8% (95% CI: 16.23–25.33, I2 = 93.9%, p < 0.001) (Figure 3), 66.8% (95% CI: 60.96–72.56, I2 = 88.6%, p < 0.001) (Figure 4), and 10.5% (95% CI: 7.47–13.46, I2 = 92%, p < 0.001) (Figure 5) respectively. The I2 index showed that the heterogeneity between the studies is very high. Based on Egger's test, publication bias in overall of WPV (P = 0.629), physical violence (P = 0.256), verbal violence (P = 0.600), and sexual harassment (P = 0.263) was not significant.
Figure 2.
The Forest plot of overall and individual prevalence of WPV with 95% confidence interval.
Figure 3.
The Forest plot of overall and individual prevalence of physical violence with 95% confidence interval.
Figure 4.
The Forest plot of overall and individual prevalence of verbal violence with 95% confidence interval.
Figure 5.
The Forest plot of overall and individual prevalence of sexual harassment with 95% confidence interval.
Discussion
The prevalence of overall WPV, physical violence, verbal violence, and sexual harassment against HCWs are 58.7, 20.8, 66.8, and 10.5%, respectively. A 2020 meta-analysis study by Byon et al. showed that the prevalence of physical and non-physical violence against home health workers was 36.4 and 41.8%, respectively (33). Another meta-analysis showed that the prevalence of sexual violence among home health workers is 6% (34). We surmise that critical medical conditions, delirium, personality disorders, and lack of long-term relationships in hospital and pre-hospital settings lead to this higher prevalence of violence against HCWs than home health workers. Negative factors such as lack of information, inadequate personnel, and equipment increase the risk of WPV in health care services (35). Furthermore, in health care settings, factors such as work stress, poor co-worker relationships, and poor social support can lead to WPV (36).
The prevalence of violence, especially verbal violence against HCWs in hospital and pre-hospital settings is high. Sun et al. showed that the prevalence of verbal WPV against doctors in China was 76.2% (37). Magnavita et al. showed that WPV has a direct relationship with sleep problems (38). Other review studies have shown that WPV reduces the quality of work, increases mental health problems, and can lead to HCWs quitting their jobs (39). Additionally, workplace violence is directly related to burnout, lower job satisfaction, less patient safety, and an increase in medical mistakes (40–42). Therefore, health care policymakers should constantly screen for WPV and establish regulations and enact programs to minimize its occurrence.
Conclusion
The prevalence of WPV against HCWs is high. WPV has negative physical, psychological, and occupational consequences for HCWs and their patients. Therefore, the health system managers should screen HCWs for the occurrence and impacts of WPV and establish regulations to minimize them.
Limitations
In most of the included studies, the prevalence of WPV in men and women was not reported separately, so it was not possible to report the prevalence of WPV by gender. Another limitation of this study was the high degree of heterogeneity between the studies. Finally, the studies selected were in the English language and primarily from Asian continent sources. Thus, the results may not be generalizable to worldwide communities.
Implication of this research
The authors used a systematic review and meta-analysis approach in this study for two reasons. First, an umbrella review of meta-analyses provides a higher level of evidence than other studies that review and evaluate original studies. Second, this is the first study in this field with this title. Numerous systematic reviews and meta-analyses have been conducted on the mental health outcomes, among health care workers (HCWs). Still, no single study has combined these results to identify overarching trends or conclusions. Therefore, the present umbrella review of meta-analyses aims to serve as the first and most comprehensive study in this regard. This umbrella review assesses all meta-analyses conducted on the prevalence of workplace violence against health care workers in hospital and pre-hospital settings among HCWs worldwide to estimate the prevalence of workplace violence against in this population. This study's results can serve as a resource for policy-makers or health managers to implement appropriate plans to improve the mental health of HCWs around the world.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
This article was approved by the Ethical Committee of Karmen University of Medical Sciences with Reg. No. 401000012. The Ethic Approval Code is IR.KMU.REC.1401.074.
Author contributions
AS, MG, SM, MT, and HS designed the review, developed the inclusion criteria, screened titles and abstracts, appraised the quality of included papers, and drafted the manuscript, reviewed the study protocol and inclusion criteria and provided substantial input to the manuscript, and reviewed the study protocol. AS and MG read and screened articles for inclusion. All authors critically reviewed drafts and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Sheikhbardsiri H, Afshar PJ, Baniasadi H, Farokhzadian J. Workplace violence against prehospital paramedic personnel (city and road) and factors related to this type of violence in Iran. J Interpers Violence. (2022) 37:NP11683–98. 10.1177/0886260520967127 [DOI] [PubMed] [Google Scholar]
- 2.Duan X, Ni X, Shi L, Zhang L, Ye Y, Mu H, et al. The impact of workplace violence on job satisfaction, job burnout, and turnover intention: the mediating role of social support. Health Qual Life Outcomes. (2019) 17:93. 10.1186/s12955-019-1164-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xing K, Jiao M, Ma H, Qiao H, Hao Y, Li Y, et al. Physical violence against general practitioners and nurses in Chinese township hospitals: a cross-sectional survey. PLoS ONE. (2015) 10:e0142954. 10.1371/journal.pone.0142954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta S, Grant K, Atlin C, Ackery A. Mitigating staff risk in the workplace: the use of RFID technology during a COVID-19 pandemic and beyond. BMJ Health Care Inform. (2020) 27:e100230. 10.1136/bmjhci-2020-100230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teymourzadeh E, Rashidian A, Arab M, Akbari-Sari A, Hakimzadeh SM. Nurses exposure to workplace violence in a large teaching hospital in Iran. Int J Health Policy Manag. (2014) 3:301–5. 10.15171/ijhpm.2014.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yousefi K, Sahebi A. Workplace violence against nurses and its reduction strategies in Iran. Int J High Risk Behav Addict. (2019) 8:e96582. 10.5812/ijhrba.96582 [DOI] [Google Scholar]
- 7.Pouryaghoub G, Mehrdad R, Alirezaei P. Workplace violence in medical specialty training settings in Iran: a cross-sectional study. Int J Occup Hyg. (2017) 9:15–20. [Google Scholar]
- 8.Hosseinikia SH, Zarei S, Najafi Kalyani M, Tahamtan S. A cross-sectional multicenter study of workplace violence against prehospital emergency medical technicians. Emerg Med Int. (2018) 2018:7835676. 10.1155/2018/7835676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heponiemi T, Kouvonen A, Virtanen M, Vänskä J, Elovainio M. The prospective effects of workplace violence on physicians' job satisfaction and turnover intentions: the buffering effect of job control. BMC Health Serv Res. (2014) 14:19. 10.1186/1472-6963-14-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Najafi F, Fallahi-Khoshknab M, Ahmadi F, Dalvandi A, Rahgozar M. Antecedents and consequences of workplace violence against nurses: a qualitative study. J Clin Nurs. (2018) 27:e116–28. 10.1111/jocn.13884 [DOI] [PubMed] [Google Scholar]
- 11.Afkhamzadeh A, Azadi N-A, Farahmandian Z, Mohamadi-Bolbanabad A. Prevalence of workplace violence of emergency medical staff and relevant factors in Sanandaj, Iran in 2016. Sci J Nurs Midwifery Paramed Fac. (2018) 4:71–80. Available online at: http://sjnmp.muk.ac.ir/article-1-158-en.html [Google Scholar]
- 12.Jodaki K, Mousavi M-S, Mokhtari R, Asayesh H, Vandali V, Golitaleb M. Effect of rosa damascene aromatherapy on anxiety and sleep quality in cardiac patients: a randomized controlled trial. Complement Ther Clin Pract. (2021) 42:101299. 10.1016/j.ctcp.2020.101299 [DOI] [PubMed] [Google Scholar]
- 13.Harorani M, Noruzi Zamenjani M, Golitaleb M, Davodabady F, Zahedi S, Jadidi A, et al. Effects of relaxation on self-esteem of patients with cancer: a randomized clinical trial. Support Care Cancer. (2020) 28:405–11. 10.1007/s00520-019-05025-3 [DOI] [PubMed] [Google Scholar]
- 14.Hedayati Emam G, Alimohammadi H, Zolfaghari Sadrabad A, Hatamabadi H. Workplace violence against residents in emergency department and reasons for not reporting them; a cross sectional study. Emergency. (2018) 6:e7. [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahebi A, Abdi K, Moayedi S, Torres M, Golitaleb M. The prevalence of insomnia among health care workers amid the COVID-19 pandemic: an umbrella review of meta-analyses. J Psychosom Res. (2021) 149:110597. 10.1016/j.jpsychores.2021.110597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adibi A, Yousefi K, Jamshidbeigi Y. The prevalence of generalized anxiety disorder among health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:658846. 10.3389/fpsyt.2021.658846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Azami M, Moslemirad M, YektaKooshali MH, Rahmati S, Soleymani A, Bigdeli Shamloo MB, et al. Workplace violence against iranian nurses: a systematic review and meta-analysis. Int J Environ Res Public Health. (2018) 33:1148–75. 10.1891/0886-6708.33.6.1148 [DOI] [PubMed] [Google Scholar]
- 20.Sahebi A, Jahangiri K, Sohrabizadeh S, Golitaleb M. Prevalence of workplace violence types against personnel of emergency medical services in Iran: a systematic review and meta-analysis. Iran J Psychiatry. (2019) 14:325–34. 10.18502/ijps.v14i4.1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y-L, Li R-Q, Qiu D, Xiao S-Y. Prevalence of workplace physical violence against health care professionals by patients and visitors: a systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:299. 10.3390/ijerph17010299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varghese A, Joseph J, Vijay V, Khakha DC, Dhandapani M, Gigini G, et al. Prevalence and determinants of workplace violence among nurses in the South-East Asian and Western Pacific Regions: a systematic review and meta-analysis. J Clin Nurs. (2021) 31:798–819. 10.1111/jocn.15987 [DOI] [PubMed] [Google Scholar]
- 23.Nowrouzi-Kia B, Chai E, Usuba K, Nowrouzi-Kia B, Casole J. Prevalence of type II and type III workplace violence against physicians: a systematic review and meta-analysis. Int J Occup Environ Med. (2019) 10:99–110. 10.15171/ijoem.2019.1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hossain MM, Sharma R, Tasnim S, Al Kibria GM, Sultana A, Saxena T. Prevalence, characteristics, and associated factors of workplace violence against healthcare professionals in India: a systematic review and meta-analysis. medRxiv. (2020) 10.1101/2020.01.01.20016295 [DOI] [Google Scholar]
- 25.Dalvand S, Ghanei Gheshlagh R, Najafi F, Zahednezhad H, Sayehmiri K. The prevalence of workplace violence against iranian nurses: a systematic review and meta-analysis. Shiraz E-Med J. (2018) 19:e65923. 10.5812/semj.6592330573555 [DOI] [Google Scholar]
- 26.Liu J, Gan Y, Jiang H, Li L, Dwyer R, Lu K, et al. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. (2019) 76:927–37. 10.1136/oemed-2019-105849 [DOI] [PubMed] [Google Scholar]
- 27.Liu X, Yang H, Hu Y, Zhou Y, Wang J, Dong L, et al. Incidence of workplace violence against nurses among Chinese hospitals: a meta-analysis. J Nurs Manag. (2021). 10.1111/jonm.13427 [DOI] [PubMed] [Google Scholar]
- 28.Lu L, Dong M, Wang S-B, Zhang L, Ng CH, Ungvari GS, et al. Prevalence of workplace violence against health-care professionals in China: a comprehensive meta-analysis of observational surveys. Trauma Violence Abuse. (2020) 21:498–509. 10.1177/1524838018774429 [DOI] [PubMed] [Google Scholar]
- 29.Shabanikiya H, Kokabisaghi F, Mojtabaeian M, Sahebi T, Varmaghani M. Global prevalence of workplace violence against paramedics: a systematic review and meta-analysis. Health Emerg Disasters. (2021) 6:205–16. 10.32598/hdq.6.4.259.3 [DOI] [Google Scholar]
- 30.Zeng L-N, Zong Q-Q, Zhang J-W, Lu L, An F-R, Ng CH, et al. Prevalence of sexual harassment of nurses and nursing students in China: a meta-analysis of observational studies. Int J Biol Sci. (2019) 15:749–56. 10.7150/ijbs.28144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu L, Dong M, Lok GK, Feng Y, Wang G, Ng CH, et al. Worldwide prevalence of sexual harassment towards nurses: a comprehensive meta-analysis of observational studies. J Adv Nurs. (2020) 76:980–90. 10.1111/jan.14296 [DOI] [PubMed] [Google Scholar]
- 32.Aljohani B, Burkholder J, Tran Q, Chen C, Beisenova K, Pourmand A. Workplace violence in the emergency department: a systematic review and meta-analysis. Public health. (2021) 196:186–97. 10.1016/j.puhe.2021.02.009 [DOI] [PubMed] [Google Scholar]
- 33.Byon HD, Lee M, Choi M, Sagherian K, Crandall M, Lipscomb J. Prevalence of type II workplace violence among home healthcare workers: a meta-analysis. Am J Ind Med. (2020) 63:442–55. 10.1002/ajim.23095 [DOI] [PubMed] [Google Scholar]
- 34.Clari M, Conti A, Scacchi A, Scattaglia M, Dimonte V, Gianino MM. Prevalence of workplace sexual violence against healthcare workers providing home care: a systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:8807. 10.3390/ijerph17238807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mento C, Silvestri MC, Bruno A, Muscatello MRA, Cedro C, Pandolfo G, et al. Workplace violence against healthcare professionals: a systematic review. Aggression Violent Behav. (2020) 51:101381. 10.1016/j.avb.2020.101381 [DOI] [Google Scholar]
- 36.Arnetz J, Hamblin LE, Sudan S, Arnetz B. Organizational determinants of workplace violence against hospital workers. J Occup Environ Med. (2018) 60:693–9. 10.1097/JOM.0000000000001345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun T, Gao L, Li F, Shi Y, Xie F, Wang J, et al. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open. (2017) 7:e017182. 10.1136/bmjopen-2017-017182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Magnavita N, Di Stasio E, Capitanelli I, Lops EA, Chirico F, Garbarino S. Sleep problems and workplace violence: a systematic review and meta-analysis. Front Neurosci. (2019) 13:997. 10.3389/fnins.2019.00997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Binmadi NO, Alblowi JA. Prevalence and policy of occupational violence against oral healthcare workers: Systematic review and meta-analysis. BMC oral health. (2019) 19:279. 10.1186/s12903-019-0974-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu J, Zheng J, Liu K, Liu X, Wu Y, Wang J, et al. Workplace violence against nurses, job satisfaction, burnout, and patient safety in Chinese hospitals. Nurs Outlook. (2019) 67:558–66. 10.1016/j.outlook.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 41.Ariza-Montes A, Muniz NM, Montero-Simó MJ, Araque-Padilla RA. Workplace bullying among healthcare workers. Int J Environ Res Public Health. (2013) 10:3121–39. 10.3390/ijerph10083121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Navajas-Romero V, Ariza-Montes A, Hernández-Perlines F. Analyzing the job demands-control-support model in work-life balance: a study among nurses in the European context. Int J Environ Res Public Health. (2020) 17:2847. 10.3390/ijerph17082847 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.