Abstract
Introduction/Objectives:
Health-related social needs (HRSN) screening efforts have reported high rates of identified social needs. Little is known if efforts to conduct HRSN screening in resource-constrained federally-qualified health centers (FQHC) successfully captures a representative patient population.
Methods:
This cross-sectional study extracted EMR data from 2016 to 2020 for 4731 screened patients from 7 affiliated clinics of a FQHC. Unscreened patients were pulled as a random sample from the study period. A multivariable logistic regression was used to identify sociodemographic traits, chronic disease diagnoses and burden, and clinic visit type and frequency associated with being screened for HRSN.
Results:
BHC screened 4731 unique patients or <1% of the total clinic population. Screened patients had a median of 3.3 (±2.5) unmet HRSN. Medicaid patients had higher odds of being screened (aOR = 1.38, CI 1.19-1.61) relative to Medicare patients. The odds of being screened for social needs increased with more provider visits per year: compared to fewer than 1 visit per year, patients with 1 to 3 provider visits (aOR = 2.06, CI 1.73-2.32), 4 to 6 provider visits (aOR = 3.34, CI 2.89-3.87), and more than 6 provider visits (aOR = 5.16, CI 4.35-6.12) all had higher odds of social needs screening. Patients with a higher comorbid disease burden (>2 conditions, aOR = 2.80, CI 2.07-3.79) had higher odds of screening.
Conclusions:
Our findings demonstrate an increased likelihood to screen patients who visit outpatient services more often and have a higher comorbid disease burden. To meet state-level Medicaid requirements, resource-constrained FQHCs that implement clinic wide HRSN screening may be well served to identify a priori strategies to ensure representative and equitable screening across the patient population.
Keywords: social determinants of health, federally-qualified health centers, primary care, social needs screening, community health centers
Introduction
There is wide recognition unmet health-related social needs (HRSN) contribute to growing health disparities and are perpetuated by the social drivers of health (SDOH). Unmet HRSN are also associated with poor physical and mental health outcomes1 -3 and sub-optimal receipt of preventative care. 3 Identifying and addressing these needs is particularly relevant for federally qualified health centers (FQHCs) and community health centers (CHCs) because the movement to create FQHCs and CHCs was a direct response to combat SDOH and HRSN.4,5 FQHCs and CHCs have found high prevalence of HRSN, with most FQHC patients reporting 2 or more unmet HRSN.1,6
Spurred by the Medicaid Section 1115 Waiver, 7 which provides financial reimbursement for non-medical expenses, state Medicaid agencies have begun to require reporting of social needs screening as a means to improve health care quality. 8 Approximately one-half of all US state Medicaid agencies have mandates for reporting patient-level HRSN data, particularly for patients enrolled in Medicaid Managed Care Contracts (MCO). 9 FQHCs are directly impacted by these mandates because FQHCs contain a significant number of Medicaid enrolled patients. 10 11 FQHCs must therefore understand how to effectively implement HRSN screening to improve reach of HRSN screening and ensure sufficient data collection, development of appropriate referral programs, and partnerships with local community organizations. Despite the importance of screening for HRSN for their patients, FQHCs and CHCs face challenges to performing universal HRSN screening due to limited resources12 -14 and lack of standardized screening implementation strategies.6,15
To our knowledge, there is a dearth of peer-reviewed literature that examines implementation approaches for HRSN screening15 -17 in resource-constrained settings. Given these constraints, it is unknown if current outpatient HRSN screening processes capture a representative patient population, despite a push to universally screen.6,18-20 To address this gap, our study examines the reach of patients screened at the [blinded] Health Center (BHC), a FQHC based in MA with 7 satellite clinics, including a family medicine residency program. 21 Our aim was to: (1) examine patient characteristics, comorbid disease burden, health care utilization patterns, and unmet HRSN prevalence, for individuals screened for HRSN; (2) compare screened and unscreened patients to assess for possible sample biases in screening implementation strategies in our family medicine clinic; and (3) examine the current reach of screening approaches to inform future implementation strategies to increase screening.
Methods
Study Design
In this cross-sectional study, we extracted EMR data to evaluate patient demographics, chronic illness burden, and outpatient encounter type and encounter visit frequency. The study was approved by the (Blinded) Health Sciences Institutional Review Board.
Setting and Participants
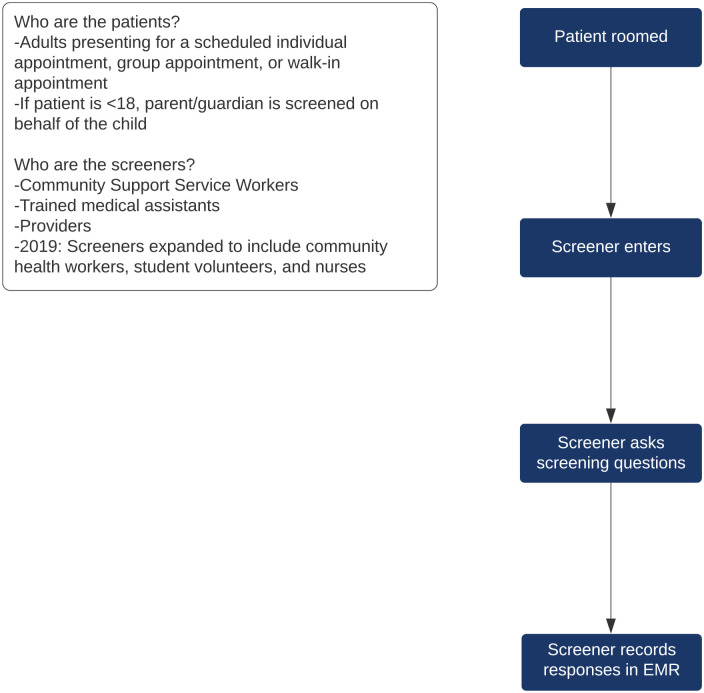
HRSN screening was performed by medical assistants, providers (attending and resident physicians or nurse practitioners), community health workers, student volunteers, and nurses at BHC family medicine clinic. The screener would ask the patient the 2-question Hunger Vital Signs 22 for food insecurity while awaiting the provider visit. Responses were recorded in the electronic medical record (EMR). All clinic visit types were eligible for screening. Where and when to ask screening questions during the patients’ visit was left to the discretion of the clinic staff, without specific workflows or designated staff to conduct screening (see Figure 1).
Figure 1.
Health-related social needs screening implementation workflow.
As a result of changes to state-led Medicaid requirements,9,23 the screening tool was further expanded in September 2019 and includes the following HRSN domains: housing quality and security, financial need, food insecurity, health literacy, immigration needs, transportation, utilities, domestic violence, and social isolation (see Supplement A for final HRSN screening instrument). Screening protocols included all 7 FQHC affiliated clinic sites. 21
Data Sources
EMR data were extracted for all clinic patients screened for unmet HRSN between January 2016 and December 2020. Between 2016 and 2020, BHC screened 4731 unique patients or <1% of the total clinic population. The unscreened comparison group was randomly identified from nearly 52 000 active FQHC patients who were not screened for HRSN during the study period. 24 Patients under the age of 18 and patients who had died during the study period were excluded.
We extracted HRSN screening responses, sociodemographic data including age, gender, self-identified race and ethnicity, preferred language, and insurance type; ICD-10 codes for 15 common chronic disease diagnoses; number of clinic visits during the study period (determined by reviewing the provider assigned to the clinic visit and checking their provider type, which includes physicians, nurse practitioners, physician assistants, family medicine residents, and nurses); and number of mental health (including both psychologist and psychiatric care) and social work visits during the study period. Identifying the type of provider helped to distinguish a clinical visit with any of the aforementioned providers with a non-clinical visit, such as vaccine or medication administration, or new medication teaching. HRSN screening was not implemented at non-clinical visits with pharmacists or registered nurses. Chronic disease diagnoses included: asthma, cancer, chronic ischemic heart disease, chronic kidney disease, chronic obstructive pulmonary disease, depression/anxiety, Type 1 and Type 2 diabetes mellitus, heart failure, hypertension, iron deficiency anemia, obesity, stroke/cerebral vascular disease, tobacco use disorder, and alcohol use disorder. A random subset of patients from each set were selected, and manually confirmed all visit and comorbidity data to ensure data reliability.
Statistical Analysis
A multivariable logistic regression was used to identify which factors (eg, sociodemographic status; chronic disease diagnoses and burden; and clinic visit type and frequency) are associated with being screened for HRSN. Covariates were imputed (10 cycles) for any variables for which more than 5% were missing. Missing data values were most present for race (16%), ethnicity (9%), and language (21%). There were no significant differences in results of multivariable analyses using imputed or non-imputed variables. A sensitivity analysis was run creating dummy variables to control for each of the 7 clinical sites affiliated with the FQHC. The results were unchanged. Odds ratios with a 95% confidence interval were reported for each variable. HRSN screening responses were categorized as either positive or negative. Statistical significance was determined at P = .05. All analyses were conducted in Stata 17.0 (StataCorp, College Station, Texas).
Results
Between 2016 and 2020, BHC screened 4731 unique patients or <1% of the total clinic population.
Table 1 presents sociodemographic characteristics for the screened group. The mean age of the screened group was 48, identified as Hispanic/Latinx (87%), and spoke Spanish (74%) as their primary language. The sample also had a higher percentage of female (69%) and Medicaid insured (67%) patients.
Table 1.
Sample Characteristics of Screened Patients (n = 4731) and Unscreened Patients (n = 4731).
| Screened N (%) | Unscreened N (%) | |
|---|---|---|
| Age—mean (SD) | 48 (16) | 46 (16) |
| Age categories in years—n (%) | ||
| 18-29 | 698 (15) | 795 (17) |
| 30-39 | 866 (18) | 1144 (24) |
| 40-49 | 888 (19) | 960 (20) |
| 50-59 | 1011 (21) | 835 (18) |
| ≥60 | 1268 (27) | 995 (21) |
| Language—n (%) | ||
| Spanish | 3515 (74) | 2748 (58) |
| English | 848 (18) | 881 (19) |
| Other | 73 (2) | 78 (2) |
| Missing | 295 (6) | 1022 (21) |
| Gender—n (%) | ||
| Female | 3258 (69) | 2621 (55) |
| Race—n (%) | ||
| White | 3164 (67) | 2875 (61) |
| Black/African American | 1293 (27) | 1049 (22) |
| Asian | 35 (<1) | 65 (1) |
| Other | 5 (<1) | 6 (<1) |
| Missing | 234 (5) | 734 (16) |
| Ethnicity—n (%) | ||
| Not Hispanic or Latino | 510 (11) | 587 (12) |
| Hispanic or Latino | 4129 (87) | 3731 (79) |
| Missing | 92 (2) | 411 (9) |
| Insurance—n (%) | ||
| Medicaid | 3189 (67) | 2859 (60) |
| Medicare | 835 (18) | 617 (13) |
| Private | 274 (6) | 603 (13) |
| Uninsured | 433 (9) | 650 (14) |
Table 2 presents the prevalence of each HRSN for the screened population. Table 3 presents the mean number of HRSNs in the population who received the multi-domain screener (n = 2497). Of those who received the multi-domain screener, 80% of patients screened positive for at least 1 HRSN, 67% of patients screened positive for at least 2 HRSN, with a mean of 3.3 HRSN.
Table 2.
Social Needs Prevalence by Screening Domain in Screened Patients (n = 4731).
| Positive screen N (%) | Negative screen N (%) | Total screened | |
|---|---|---|---|
| Social needs N (%) | |||
| Housing | 549 (23) | 1885 (77) | 2434 |
| Material/financial hardship | 1331 (55) | 1101 (45) | 2432 |
| Food insecurity | 3126 (66) | 1580 (34) | 4706 |
| Literacy concerns | 761 (32) | 1646 (68) | 2407 |
| Immigration concerns | 221 (9) | 2174 (91) | 2395 |
| Transportation | 425 (18) | 1970 (82) | 2395 |
| Utilities | 252 (12) | 1814 (88) | 2066 |
| Physical abuse | 57 (3) | 2002 (97) | 2059 |
| Social isolation | 825 (43) | 1081 (57) | 1906 |
Table 3.
Social Needs Prevalence in Individuals Who Were Screened for All Domains (n = 2497).
| Mean number of social needs, SD | 3.3 (2.5) |
| Overall social needs in population, N (%) | 2004 (80) |
| Number of social needs (N) % | |
| 0 | 493 (20) |
| 1 | 315 (13) |
| 2 or more | 1689 (67) |
Table 4 presents the results of the multivariate logistic regression. The outcome of interest was odds of being screened in clinic. Female sex (aOR = 1.44, CI 1.3-1.59), identifying as Black (aOR = 1.13, CI 1.09-1.26), and preferring Spanish (aOR = 1.43, CI 1.22-1.68) were independently associated with higher odds of being screened for social needs. With Medicare being the reference group, having Medicaid was associated with higher odds of being screened (aOR = 1.38, CI 1.19-1.61), while having private insurance was associated with lower odds of being screened (aOR = 0.72, CI 0.58-0.89). Heart failure (aOR = 0.48, CI 0.34-0.69) and cancer diagnosis (aOR = 0.70, CI 0.52-0.88) were associated with reduced odds of being screened. Patients with 3 or more chronic illnesses had higher odds of being screened relative to patients without any illnesses (aOR = 2.80, CI 2.07-3.79). Patients had a higher odd of being screened if they had any behavioral health (aOR = 1.03, CI 1.01-1.05) or social work visit (aOR = 1.13, CI 1.08-1.17) during the study period. The odds of being screened for social needs increased with more provider visits per year: with less than 1 visit per year as the reference group, patients with 1 to 3 provider visits (aOR = 2.06, CI 1.8-2.37), 4 to 6 provider visits (aOR = 3.34, CI 2.89-3.87), and more than 6 provider visits (aOR = 5.16, CI 4.35-6.12) all had higher odds of social needs screening.
Table 4.
Multivariate Regression to Identify Odds of Being Screened.
| Adjusted odds ratios of screening | P-value | ||
|---|---|---|---|
| aOR | 95% CI | ||
| Age | 1.00 | 1.00-1.03 | .83 |
| Female | 1.44 | 1.30-1.59 | <.05 |
| Race | |||
| White | Reference | ||
| Black | 1.13 | 1.09-1.26 | <.05 |
| Ethnicity | |||
| Non hisp | Reference | ||
| Hisp or Latino | 0.96 | 0.79-1.18 | .72 |
| Preferred language | |||
| English | Reference | ||
| Spanish | 1.43 | 1.22-1.68 | <.05 |
| Insurance | |||
| Medicare | Reference | ||
| Medicaid | 1.38 | 1.19-1.61 | <.05 |
| Private | 0.72 | 0.58-0.89 | <.05 |
| Uninsured | 1.03 | 0.85-1.25 | .73 |
| Co-morbidities | |||
| Cancer | 0.70 | 0.52-0.88 | <.05 |
| Anemia | 0.95 | 0.83-1.08 | .42 |
| Diabetes | 0.96 | 0.81-1.12 | .59 |
| Hyperlipidemia | 1.09 | 0.97-1.22 | .17 |
| Substance use disorder | 1.12 | 0.95-1.32 | .17 |
| Depression/anxiety | 1.08 | 0.97-1.19 | .15 |
| Hypertension | 1.07 | 0.95-1.21 | .24 |
| Cardiovascular disease | 1.07 | 0.81-1.4 | .64 |
| Heart failure | 0.48 | 0.34-0.69 | <.05 |
| Obesity | 1.07 | 0.97-1.18 | .16 |
| Peripheral arterial disease | 1.05 | 0.55-2.03 | .88 |
| Chronic obstructive pulmonary disease | 1.06 | 0.80-1.39 | .70 |
| Asthma | 0.91 | 0.76-1.09 | .30 |
| Chronic kidney disease | 1.18 | 0.91-1.54 | .22 |
| Chronic disease, count | |||
| None | Reference | ||
| Mild (1) | 1.09 | 0.94-1.26 | .26 |
| Moderate (2) | 1.24 | 0.95-1.61 | .11 |
| Severe (>2) | 2.80 | 2.07-3.79 | <.05 |
| Behavioral health visits | 1.03 | 1.01-1.05 | <.05 |
| Social work visits | 1.13 | 1.08-1.17 | <.05 |
| Provider visits, categoriesa | |||
| <1 visit per year | Reference | ||
| 1-3 visits per year | 2.06 | 1.80-2.37 | <.05 |
| 4-6 visits per year | 3.34 | 2.89-3.87 | <.05 |
| >6 visits per year | 5.16 | 4.35-6.12 | <.05 |
Boldface indicates statistical significance (P < .05). Screened patients (n = 4731), unscreened patients (n = 4731).
Annualized (number of visits in study period over years in study sample).
Discussion
This study presents patient characteristics and utilization patterns of those screened for HRSN in an FQHC and then compares patient characteristics, health care utilization patterns, and comorbid disease burden between screened and unscreened patients at an FQHC. We have found high comorbidity burden and frequent clinic visits among our population, with high prevalence of unmet social needs. Unlike prior work,2,16,25 this study highlights patients with frequent visits are more likely to be screened, and these patients are significantly different from unscreened patients.
Having a HRSN screening tool is necessary, but insufficient for FQHCs to achieve a higher saturation with social needs screening. One potential explanation for why staff screened patients who visited the clinic more frequently is staff may be more familiar with these patients’ needs as a result of these patients’ high visit rates. Staff may perceive HRSN screening as challenging, as prior work suggests time constraints,12 -14,16,20 insufficient training,12,14,20 concern about lack of resources to address positive screening results,13,14,20,26 and recognition that patients are being asked to provide sensitive information that was not previously required all may lead to lower implementation rates of HRSN screening.12,18,27 In the setting of these challenges, staff may find it easier to pre-select patients with whom staff have a rapport and have a need staff are already familiar with, which may be evidenced by screening patients with high visit rates.
Another potential explanation for higher screening rates among patients who visit more frequently is that these patients may be screened more due to random chance. Each encounter in the clinic represents an opportunity to be screened and showing up more frequently may increase the probability an opportunity to be screened presents itself. This may be relevant for patients with higher comorbid disease burden who are scheduled for more frequent visits to monitor their health.
When patients who utilized more outpatient services have higher screening rates this misses opportunities to screen patients who visit clinic less often, yet may also have unmet social needs. We suspect that our clinic population, including unscreened individuals, has a high prevalence of social needs because 84% of our population lives under the federal poverty line 24 and 46% of residents in towns served by our FQHC report food insecurity. 28 Broader implementation of social needs screening will allow FQHCs to better meet the needs of their patient population by capturing patients who are at risk of worsening health status but are often ignored by current health care risk stratification models.
Second, HRSN screening implementation may result in a stronger patient-provider relationship and therapeutic alliance. Patients are interested in being screened for HRSN; patients recognize HRSN impact their health and feel screening strengthens their relationship with their provider.29 -31 Patients who are screened reported higher patient satisfaction scores after screening30,32 and greater likelihood of using CHCs as their usual source of care compared to the ED. 32
These 2 issues, missing patients with potential HRSN and foregoing opportunities to grow the patient-provider relationship, suggest the need for FQHCs to refine HRSN screening implementation. Investigators must identify implementation strategies that support wider adoption and reach of HRSN screening among diverse clinical settings. Focus on implementation strategies to address gaps in reach and adoption is needed.15 -17,33,34 Implementation science offers investigators frameworks through which the necessary implementation strategies and measures can be systematically identified to impact both screening uptake and patient capture.15,35,36
Studies that used the RE-AIM framework to examine HRSN screening implementation found screening was limited in its reach15,16 and insured patients were more likely to undergo screening. 16 Our study found similar results. Implementation science frameworks that focus on assessing reach and adoption should be prioritized,16,25,37 but other frameworks anchored in equity could hold value in this space including: the Health Equity Implementation Framework,17,33 the Active Implementation Framework, 38 and the Exploration, Preparation, Implementation, and Sustainment framework. 39
In addition to more frequent clinic visits, our study found that screened patients had a higher number of comorbid conditions compared to unscreened patients. It is unknown if this comorbidity represents uncontrolled or well-controlled chronic disease burden, and therefore difficult to ascertain if patients were coming in frequently due too poorly controlled disease requiring frequent clinic visits, or if providers a priori identified social needs in their patients, and brought those in with multiple comorbidities in for more frequent visits and closer monitoring. Literature to date has demonstrated that patients who a have a higher number of comorbid conditions tend to report more than one social need.1 -3,40 This is the first study to our knowledge to suggest ad hoc HRSN screening processes may preferentially screen patients with more comorbidity.
Screening patients with more clinic visits and higher comorbid disease burden could be an attempt by clinics to prioritize screening patients who are perceived to have more risk factors for social needs. However, the relationship between outpatient health care utilization, chronic disease burden, and risk for social needs remains unclear. Current literature demonstrates that patients with advanced age1,41 and who receive Medicaid benefits 41 report more social needs, while female and male patients report different clusters of social needs. 42 Clinics that use limited resources to perform screening only for perceived high-risk patients may unintentionally reinforce prejudice and stigma through screening 18 and miss capturing a significant percentage of patients who experience unmet social needs. 19
Limitations
There are several limitations to this study. First, our study was a single-site study and may not be generalizable to other settings. Second, visit type (eg, follow-up vs same-day visit vs new physical) and staff screener type were not included in the data, and therefore we cannot discern if the higher visit frequency was due to uncontrolled disease, which may have been a trigger for provider HRSN screening, or well-controlled multiple chronic illnesses. The data extracted only total number of behavioral health or social work visits and not when they occurred, and therefore we are unable to tell the timing of these visits relative to when HRSN screening was performed. We also cannot discern how staff screener type impacts which patients are screened. Third, our study’s population primarily identified as Latinx, spoke Spanish, and were insured through Medicaid. This may limit generalizability to other primary care settings. Fourth, we do not know the prevalence of social needs in the unscreened group and could not assess whether need was similar between the screened and unscreened groups. Future research should study optimal implementation strategies to improve adoption and reach in other patient populations to determine if similar implementation problems exist. Fifth, food insecurity was the most commonly reported unmet social need; while current literature suggests that food insecurity is common in other settings,1,40,41 our results may overstate food insecurity prevalence because food insecurity was the only social need domain screened for in the first half of the study period. Finally, our social needs screening pilot captured less than 1% of all clinic patients, of which 78% were screened once, and therefore makes it difficult to ascertain how rates vary over time. The low overall uptake makes it difficult to understand how changes in screening for a single domain to more than 1 domain may have impacted overall rates of screening, although the number of patients screened per year remained constant throughout the study period, suggesting the impact was minimal. Future research on screening implementation should identify an acceptable number of screenings over time, as current literature suggests that repeat screening might be unacceptable to patients. 43
Conclusions
Our study demonstrated that social needs screening implementation in a high needs primary care population preferentially screened patients with a higher burden of chronic illness and more frequent clinic visits. Our study highlights that how HRSN screening is implemented matters. In our resource-constrained clinic, we were unable to reach most of the patient population, screening <1% of the total clinic population. Medicaid agencies are incentivizing screening for all enrollees so that care teams can identify HRSN and provide resources that improve health and reduce cost. This may be difficult to do without a priori implementation strategies to ensure adequate reach. Our work suggests that without careful attention to social needs screening implementation in resource-constrained FQHCs, screening practices may miss patients who do not present to the clinic as often. Screening practices that prioritize including all patients may offer benefits for both the patient and provider. It could strengthen the patient-provider therapeutic relationship and improve patient satisfaction. Future work should include implementation considerations to identify strategies that improve widespread adoption and reach in FQHCs.
Supplemental Material
Supplemental material, sj-docx-1-jpc-10.1177_21501319221118809 for Implementing Health Related Social Needs Screening in an Outpatient Clinic by Raman Nohria, Nan Xiao, Rubeen Guardado, Mari-Lynn Drainoni, Cara Smith, Keith Nokes and Elena Byhoff in Journal of Primary Care & Community Health
Acknowledgments
We would like to thank Jonathan Lichkus and Nan Xiao for their help with the study’s design, data collection, and implementation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Publication of this article was supported by the National Institute on Minority Health and Health Disparities (K23MD015267). The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institute on Minority Health and Health Disparities.
Financial Disclosures: No financial disclosures were reported by the authors of this paper.
ORCID iDs: Raman Nohria  https://orcid.org/0000-0003-3313-4833
https://orcid.org/0000-0003-3313-4833
Elena Byhoff  https://orcid.org/0000-0003-3438-2695
https://orcid.org/0000-0003-3438-2695
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Kreuter MW, Garg R, Li L, et al. How do social needs cluster among low-income individuals? Popul Health Manag. 2021;24(3):322-332. doi: 10.1089/pop.2020.0107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cole MB, Nguyen KH. Unmet social needs among low-income adults in the United States: associations with health care access and quality. Health Serv Res. 2020;55 Suppl 2(S2):873-882. doi: 10.1111/1475-6773.13555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164-172. doi: 10.1136/bmjqs-2015-004521 [DOI] [PubMed] [Google Scholar]
- 4. Shin P, Alvarez C, Sharac J, et al. A profile of community health center patients: implications for policy. KFF. Published December 23, 2013. Accessed August 10, 2021. https://www.kff.org/medicaid/issue-brief/a-profile-of-community-health-center-patients-implications-for-policy/
- 5. Geiger HJ. The first community health center in Mississippi: communities empowering themselves. Am J Public Health. 2016;106(10):1738-1740. doi: 10.2105/AJPH.2016.303421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kreuter MW, Thompson T, McQueen A, Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annu Rev Public Health. 2021;42(1):329-344. doi: 10.1146/annurev-publhealth-090419-102204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Medicaid. About section 1115. demonstrations. Accessed April 25, 2022. https://www.medicaid.gov/medicaid/section-1115-demonstrations/about-section-1115-demonstrations/index.html
- 8. Bailit Health. Developing a social risk factor screening measure. Published October 2020. https://www.shvs.org/wp-content/uploads/2020/10/Developing-a-SRF-Screening-Measure_Issue-Brief.pdf
- 9. KFF. States reporting social determinant of health related policies required in Medicaid Managed Care Contracts. Published October 27, 2021. Accessed April 25, 2022. https://www.kff.org/other/state-indicator/states-reporting-social-determinant-of-health-related-policies-required-in-medicaid-managed-care-contracts/
- 10. Hoag SD, Norton SA, Rajan S. Federally qualified health centers: surviving Medicaid managed care, but not thriving. Health Care Financ Rev. 2000;22(2):103-117. [PMC free article] [PubMed] [Google Scholar]
- 11. Degenfelder C. The FQHC alternative payment methodology toolkit: fundamentals of developing a capitated FQHC APM. Published online July 2017: 38. [Google Scholar]
- 12. Butler ED, Morgan AU, Kangovi S. Screening for unmet social needs: patient engagement or alienation? Published online 2020: 10. [Google Scholar]
- 13. Browne J, Mccurley JL, Fung V, Levy DE, Clark CR, Thorndike AN. Addressing social determinants of health identified by systematic screening in a Medicaid Accountable Care Organization: a qualitative study. J Prim Care Community Health. 2021;12:2150132721993651. doi: 10.1177/2150132721993651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Quiñones-Rivera A, Wing HE, Barr-Walker J, Yee M, Harrison JM, Gottlieb LM. Provider impacts of socioeconomic risk screening and referral programs: a scoping review. J Am Board Fam Med. 2021;34(4):820-831. doi: 10.3122/jabfm.2021.04.210039 [DOI] [PubMed] [Google Scholar]
- 15. Fiori KP, Heller CG, Flattau A, et al. Scaling-up social needs screening in practice: a retrospective, cross-sectional analysis of data from electronic health records from Bronx county, New York, USA. BMJ Open. 2021;11(9):e053633. doi: 10.1136/bmjopen-2021-053633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wallace AS, Luther BL, Sisler SM, Wong B, Guo JW. Integrating social determinants of health screening and referral during routine emergency department care: evaluation of reach and implementation challenges. Implement Sci Commun. 2021;2(1):114. doi: 10.1186/s43058-021-00212-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Drake C, Batchelder H, Lian T, et al. Implementation of social needs screening in primary care: a qualitative study using the health equity implementation framework. BMC Health Serv Res. 2021;21(1):975. doi: 10.1186/s12913-021-06991-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316(8):813-814. doi: 10.1001/jama.2016.9282 [DOI] [PubMed] [Google Scholar]
- 19. Cottrell EK, Hendricks M, Dambrun K, et al. Comparison of community-level and patient-level social risk data in a network of community health centers. JAMA Netw Open. 2020;3(10):e2016852. doi: 10.1001/jamanetworkopen.2020.16852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kostelanetz S, Pettapiece-Phillips M, Weems J, et al. Health care professionals’ perspectives on universal screening of social determinants of health: a mixed-methods study. Popul Health Manag. 2022;25:367-374. doi: 10.1089/pop.2021.0176 [DOI] [PubMed] [Google Scholar]
- 21. About—Greater Lawrence Family Health Center. Accessed August 10, 2021. https://glfhc.org/about/
- 22. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26-e32. doi: 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 23. Mass.gov. Mass health risk adjustment methodology. Accessed April 25, 2022. https://www.mass.gov/lists/masshealth-risk-adjustment-methodology
- 24. Health Center Program Uniform Data System (UDS) data overview. Accessed May 23, 2022. https://data.hrsa.gov/tools/data-reporting/program-data?grantNum=H80CS00314
- 25. Fiori KP, Heller CG, Rehm CD, et al. Unmet social needs and no-show visits in primary care in a US Northeastern Urban Health System, 2018–2019. Am J Public Health. 2020;110(Suppl 2):S242-S250. doi: 10.2105/AJPH.2020.305717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tong ST, Liaw WR, Kashiri PL, et al. Clinician experiences with screening for social needs in primary care. J Am Board Fam Med. 2018;31(3):351-363. doi: 10.3122/jabfm.2018.03.170419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schleifer D. It’s about trust: low-income parents’ perspectives on how pediatricians can screen for social determinants of health. Health Serv Res. 2020;55(Suppl 1):134-135. doi: 10.1111/1475-6773.13524 [DOI] [Google Scholar]
- 28. eagletribune.com. Poll measures food insecurity levels. Merrimack Valley. Accessed May 23, 2022. https://www.eagletribune.com/news/merrimack_valley/poll-measures-food-insecurity-levels/article_28533da6-31a1-57f2-8cc2-51961827b5fb.html
- 29. Byhoff E, De Marchis EH, Hessler D, et al. Part II: a qualitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med. 2019;57(6 Suppl 1):S38-S46. doi: 10.1016/j.amepre.2019.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hsu C, Cruz S, Placzek H, et al. Patient perspectives on addressing social needs in primary care using a screening and resource referral intervention. J Gen Intern Med. 2020;35(2):481-489. doi: 10.1007/s11606-019-05397-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rogers AJ, Hamity C, Sharp AL, Jackson AH, Schickedanz AB. Patients’ attitudes and perceptions regarding social needs screening and navigation: multi-site survey in a large integrated health system. J Gen Intern Med. 2020;35(5):1389-1395. doi: 10.1007/s11606-019-05588-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nguyen KH, Trivedi AN, Cole MB. Receipt of social needs assistance and health center patient experience of care. Am J Prev Med. 2021;60(3):e139-e147. doi: 10.1016/j.amepre.2020.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Woodward EN, Singh RS, Ndebele-Ngwenya P, Melgar Castillo A, Dickson KS, Kirchner JE. A more practical guide to incorporating health equity domains in implementation determinant frameworks. Implement Sci Commun. 2021;2(1):61. doi: 10.1186/s43058-021-00146-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gottlieb L, Cottrell EK, Park B, Clark KD, Gold R, Fichtenberg C. Advancing social prescribing with implementation science. J Am Board Fam Med. 2018;31(3):315-321. doi: 10.3122/jabfm.2018.03.170249 [DOI] [PubMed] [Google Scholar]
- 35. Moullin JC, Dickson KS, Stadnick NA, et al. Ten recommendations for using implementation frameworks in research and practice. Implement Sci Commun. 2020;1(1):42. doi: 10.1186/s43058-020-00023-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Curran GM. Implementation science made too simple: a teaching tool. Implement Sci Commun. 2020;1(1):27. doi: 10.1186/s43058-020-00001-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322-1327. doi: 10.2105/ajph.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Velonis AJ, O’Campo P, Rodrigues JJ, Buhariwala P. Using implementation science to build intimate partner violence screening and referral capacity in a fracture clinic. J Eval Clin Pract. 2019;25(3):381-389. doi: 10.1111/jep.13128 [DOI] [PubMed] [Google Scholar]
- 39. Smith JD, Polaha J. Using implementation science to guide the integration of evidence-based family interventions into primary care. Fam Syst Health J Collab Fam Healthc. 2017;35(2):125-135. doi: 10.1037/fsh0000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chambers EC, McAuliff KE, Heller CG, Fiori K, Hollingsworth N. Toward understanding social needs among primary care patients with uncontrolled diabetes. J Prim Care Community Health. 2021;12:2150132720985044. doi: 10.1177/2150132720985044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Heller CG, Parsons AS, Chambers EC, Fiori KP, Rehm CD. Social risks among primary care patients in a large urban health system. Am J Prev Med. 2020;58(4):514-525. doi: 10.1016/j.amepre.2019.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Byhoff E, Tripodis Y, Freund KM, Garg A. Gender differences in social and behavioral determinants of health in aging adults. J Gen Intern Med. 2019;34(11):2310-2312. doi: 10.1007/s11606-019-05225-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. De Marchis EH, Hessler D, Fichtenberg C, et al. Part I: a quantitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med. 2019;57(6 Suppl 1):S25-S37. doi: 10.1016/j.amepre.2019.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpc-10.1177_21501319221118809 for Implementing Health Related Social Needs Screening in an Outpatient Clinic by Raman Nohria, Nan Xiao, Rubeen Guardado, Mari-Lynn Drainoni, Cara Smith, Keith Nokes and Elena Byhoff in Journal of Primary Care & Community Health