Abstract
Childhood maltreatment (CM) is linked to impairments in various domains of social functioning. Here, we argue that it is critical to identify factors that underlie impaired social functioning as well as processes that mediate the beneficial health effects of positive relationships in individuals exposed to CM. Key research recommendations are presented, focusing on: (1) identifying attachment-related alterations in specific inter- and intrapersonal processes (e.g., regulation of closeness and distance) that underlie problems in broader domains of social functioning (e.g., lack of perceived social support) in individuals affected by CM; (2) identifying internal (e.g., current emotional state) and external situational factors (e.g., cultural factors, presence of close others) that modulate alterations in specific social processes; and (3) identifying mechanisms that explain the positive health effects of intact social functioning. Methodological recommendations include: (1) assessing social processes through interactive and (close to) real-life assessments inside and outside the laboratory; (2) adopting an interdisciplinary, lifespan perspective to assess social processes, using multi-method assessments; (3) establishing global research collaborations to account for cultural influences on social processes and enable replications across laboratories and countries. The proposed line of research will contribute to globally develop and refine interventions that prevent CM and further positive relationships, which − likely through buffering the effects of chronic stress and corresponding allostatic load − foster resilience and improve mental and physical health, thereby reducing personal suffering and the societal and economic costs of CM and its consequences. Interventions targeting euthymia and psychological well-being are promising therapeutic concepts in this context.
Keywords: Child abuse, Social behavior, Social support, Interpersonal relations, Early interventions
Introduction
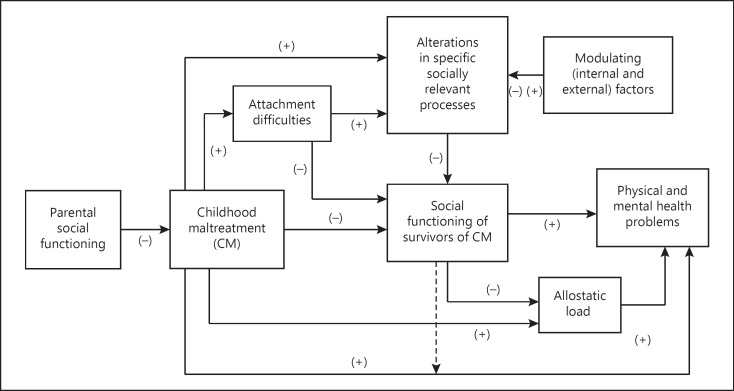
Childhood maltreatment (CM) includes all types of physical and/or emotional ill-treatment, sexual abuse, neglect, and exploitation, which result in actual or potential harm to the child's health, survival, development, or dignity in the context of a relationship of responsibility, trust, or power [1]. Prevalence rates depend on gender and vary across continents from 6 to 61% (emotional abuse), 22 to 60% (physical abuse), 6 to 27% (sexual abuse), and 17 to 65% (neglect) [2]. There is a well-documented link between CM and poor mental and physical health [3]. Moreover, there is a large body of evidence related to neurobiological changes stemming from CM, including genetic factors and epigenetic processes [4, 5]. Here, however, we argue that in addition to understanding, preventing, and treating the mental and physical consequences of CM, it is equally critical to understand and strengthen affected individuals' social functioning (i.e., their ability to interact with others and to fulfill social roles during daily work and leisure-related activities with family members, colleagues, friends, and partners). We provide an overview of the mental and physical health consequences of CM and summarize the detrimental effects of CM on a broad range of domains of social functioning as well as the protective, health-promoting effects of social relationships (see Fig. 1). We argue that to advance the field and develop effective interventions that strengthen social functioning in individuals with a history of CM, future research needs to focus on identifying factors that underlie impaired social functioning and on the processes that mediate the positive health effects of intact social functioning in individuals exposed to CM. We propose a conceptual framework of key factors and processes linking CM to mental health, physical health, and social functioning (Fig. 1), and specific recommendations (Table 1) and methodological considerations (Table 2) for future research. Finally, intervention approaches to improve social functioning in the context of CM are discussed.
Fig. 1.
Conceptual framework, illustrating the known associations between CM, mental health, physical health, and social functioning, and putative factors associated with CM, mental health, physical health, and social functioning. Positive associations are marked with (+); negative associations are marked with (−); dashed lines represent moderator effects.
Table 1.
Specific recommendations
| Overarching aims | Specific aims and research questions |
|---|---|
| 1. Identify key socially relevant processes in individuals affected by CM | Focus on processes that are likely affected by attachment difficulties arising from CM, including by taking a cross-cultural perspective and applying attachment-related concepts that reflect cultural variation |
| Assess whether alterations in specific social processes mediate the relationship between attachment difficulties and impaired social functioning |
|
| Identify specific intrapersonal processes (e.g., responses to social signals such as facial expressions and touch; regulation of closeness and distance; alterations in communicative processes and behaviors; non-verbal signals such as body posture, facial expressions, and expressions of emotions in the voice) |
|
| Explore whether specific interpersonal processes (e.g., interpersonal emotion regulation, shared social identities, group memberships, and social identity management) that have received increased attention in basic research are relevant for the field of traumatic stress, including CM | |
|
| |
| 2. Identify factors that enhance or buffer the degree to which alterations in specific socially relevant processes are present in a specific situation (Fig. 1) | Assess internal factors that can modulate social responding (e.g., an individual's current cognitive, emotional, and motivational state; personal resources in the form of compensatory mechanisms) |
| Assess external factors such as culture and social context (e.g., presence of trusted others) | |
|
| |
| 3. Assess whether specific socially relevant processes impact broader social problems | Explore if specific social processes known to be affected by CM are related to problems in broader domains of social functioning known to be affected by CM (e.g., quality of interactions and relationships, social support) |
| Replicate findings on the role of maladaptive internalized schemas, emotion regulation and recognition, and assess the role of social processes relevant to social functioning that have not been previously systematically studied in a CM context |
|
| Assess whether findings from non-clinical populations (e.g., effects of adequate perceptions of others' emotions on relationship satisfaction) apply to individuals affected by CM with mental disorders | |
|
| |
| 4. Identify factors that explain the positive health effects of intact social functioning | Assess whether the positive effect of social functioning on mental and physical health operates by buffering the effects of chronic stress (CM) on allostatic load |
| Focus on the biological pathways via which social support may benefit individuals exposed to CM | |
Table 2.
Methodological considerations
| Methodological aspects | Recommendations |
|---|---|
| Research setting | Balance the need for staying close to real-life conditions (enabling ecological validity and generalizability of findings) and the need for controlled, standardized conditions (in order to vary factors of interest systematically and to control for confounding variables) |
| Assess social processes outside and inside the laboratory |
|
| Develop and apply experimental stimuli and settings that are close to real-life (e.g., non-standardized or partially standardized interactive experimental paradigms; virtual reality environments) | |
|
| |
| Study designs | Complement cross-sectional study designs with longitudinal studies to map relational and affective domains to mental and physical health trajectories, and to assess how socio-emotional processes develop, interact, and predict social functioning over time |
|
| |
| Research methods | Use multi-method approaches (e.g., behavioral or psychophysiological assessments; ecological momentary assessment) to study socially relevant microprocesses, especially with different interaction partners |
|
| |
| Research teams | Establish interdisciplinary collaborations to assess the interplay of neuronal, peripheral physiological, hormonal, cultural, and genetic factors |
| Seek collaborations with basic science researchers to understand socially relevant and biological processes in the general population (before applying concepts to the field of CM) |
|
| Establish cross-national research collaborations that include researchers from currently underrepresented countries |
|
| Replicate findings across laboratories and countries to strengthen reliability and generalizability of findings | |
|
| |
| Cross-cultural research | Distinguish culture from ethnicity (diversity of cultures within broader categorizations of ethnicity) |
| Consider individual and intragroup differences in the internalization of cultural beliefs |
|
| Use standardized procedures for translation and back-translation and consider clinimetric selection criteria when translating existing self-report scales and developing new ones |
|
| Foster cross-cultural development of new psychometric assessment tools and experimental paradigms that are suitable for diverse cultural and ethnic groups | |
Effects of CM on Mental and Physical Health
CM is associated with a significantly increased risk of mental disorders during childhood, including posttraumatic stress disorder (PTSD), psychotic disorders, attention-deficit/hyperactivity disorder, anxiety, and depressive disorders [6, 7]. CM is also a significant risk factor for mental disorders in adolescence, and is associated with impaired mental health and dissociative symptoms in severe mental disorders such as schizophrenia, bipolar disorder, and personality disorders in adulthood [8].
In low- and high-income countries, women exposed to CM are at increased risk of developing postpartum depression [9], which in turn increases the risk of impaired maternal-child attachment [10] and depression in the child [11]. CM is also associated with increased risk of subclinical hypothyroidism in pregnancy [12]. Furthermore, potential associations between maternal exposure to CM, fetal brain development [13], brain anatomy [14], and obesity in the newborn [15] are well documented. Moreover, children exposed to CM are at risk for asthma, sleep disruptions, somatic complaints such as headache and nausea, and recurrent infectious diseases requiring hospitalization [16].
CM is also consistently related to poor long-term physical health (diabetes, chronic pain, obesity) and problematic health behaviors (physical inactivity, smoking, increased suicidal behavior, poor sexual health, risky sexual behaviors) [3, 17, 18, 19]. Furthermore, there is a well-documented risk for substance abuse and corresponding disorders in both children and adults exposed to CM [20]. Consistent with these findings, older adults who have experienced multiple types of CM have nearly twice the risk of premature mortality compared to unexposed older adults [21].
Figure 1 illustrates the effect of CM on mental and physical health. In line with the long-lasting effects of CM, differences in brain structures involved in the regulation of emotion and stress between CM and non-CM groups are well documented [22]. Differences in developmental timing (which refers to when CM occurs in relation to critical and sensitive periods of the nervous system and body development [23, 24]) have been linked to different brain structural volume [25], physiological and cognitive outcomes [26, 27]. CM experiences that span several developmental periods, including both early and later childhood stages, predict a cascade of internalizing and externalizing symptoms in childhood that eventuate in greater symptoms of anxiety, depression, substance use disorder, and antisocial personality disorder in emerging adulthood [28].
In this context, the concept of allostatic load [29] is important. Responding to stress requires activation of multiple neurobiological processes which, while adaptive, also contribute to allostatic load − the physical “wear and tear” that accumulates as a consequence of recurrent or chronic activation of neural and physiological regulatory systems. Increased allostatic load due to chronic stress is held to be a key etiological mechanism in the pathway from CM to disease [30], with longitudinal evidence showing that CM predicts allostatic load in adulthood [31], and emerging evidence that allostatic load mediates the influence of CM on adult depression [32] (see Fig. 1). In line with the many health-related consequences of CM, the overall economic consequences of CM are substantial. In the US, the average estimated lifetime cost is USD 830,928, while the estimated annual population lifetime burden of CM is USD 428 billion [33].
Positive Social Relationships as a Protective, Health-Promoting Factor
We propose that in the context of CM positive social relationships can prevent CM and contribute to mental and physical well-being in several ways. First, children of parents with a history of CM are more likely to be exposed to maltreatment [34]. However, between 12 and 93% of parents exposed to CM succeed in breaking this intergenerational cycle of maltreatment [35]. One factor that seems to have a preventive effect is intact social functioning; positive and supportive relationships between affected parents and other adults (e.g., romantic partners, co-parents) are linked to a lower risk for intergenerational continuity of CM [35]. That is, intact social functioning can prevent CM in the next generation (Fig. 1).
Second, positive social relationships can moderate the relationship between CM and health problems (see Fig. 1), protecting individuals exposed to CM from developing health problems. In support of this claim, for child and adult populations exposed to trauma including CM, perceived social support (i.e., warm and caring relationships with parents, other family members, peers, colleagues, friends, spouses, school personnel, or health providers) is one of the most consistently identified resilience factors, protecting against the development of trauma-related [36] and other mental disorders [37].
Third, intact social functioning can have a direct positive impact on mental and physical health. The more individuals feel positively connected to and supported by others, the lower their risk for mental and cardiovascular disorders, impaired cognitive functioning, dementia, obesity, mortality, alcohol abuse, and other risky health behaviors [38, 39] (Fig. 1). In sum, there is evidence that positive social relationships can serve as key protective factor for CM and associated adverse health outcomes.
CM Affects Broad Domains of Social Functioning
While positive social relationships may bring key benefits to CM survivors and subsequent generations, individuals exposed to CM may be less well equipped than others to access such support. Individuals with a history of CM show well-documented impairments in many domains of social functioning (Fig. 1). In children, CM has been linked to increased social isolation and withdrawal [40], perceived impairments in social competence and emotional intelligence [40, 41], and increased risk of bullying and victimization [42]. Furthermore, maltreated children were reported to be less well-liked and more likely to experience rejection by their peers than their non-maltreated counterparts [43]. The link between CM and social dysfunctioning seems to persist into adulthood. For example, adults with a documented history of CM report less positive perceptions of their romantic relationships, higher rates of separation, divorce, and problematic parenting behaviors, and a greater likelihood of involvement in intimate partner aggression and violence than matched controls (e.g., [44, 45, 46, 47]). While much of the research focuses on consequences of CM for intimate partner relationships, particularly amongst women exposed to child sexual abuse, prostitution, rape, and early marriage [48], social difficulties extend beyond intimate relationships, with CM being linked to increased family conflict [47], less adaptive social relationships [46], reduced perceptions of social support from family and friends [49], and increased perceptions of loneliness and social isolation [50]. Negative evaluations (low levels of perceived trustworthiness and likeability by unknown others) also seem to persist into adulthood [51].
Factors that might moderate the relationship between CM and social functioning are the type of CM and age at onset of CM. It has been proposed that early experiences of threat (e.g., physical exposure) and deprivation (e.g., neglect) impact different neural circuits [52] which, in turn, differentially impact cognitive functions [53], learning, and behavior [54, 55]. Such differential effects might affect not only mental and physical health, but also the development of social functioning. Furthermore, neglected children show more pronounced academic deficits and social withdrawal as well as lower peer acceptance than physically abused children, with exposure to neglect prior to kindergarten having a particularly pervasive influence on school achievement [56]. The setting in which CM is experienced may also affect social functioning. Yet, while emotional and sexual abuse in foster care settings are known to have negative effects on adult survivors' mental health [57], studies evaluating differences in social functioning in individuals with institutional versus intrafamilial CM or looking specifically at CM occurring in other non-familial settings, are lacking.
Understanding the Underlying Processes and Effects of Social Function and Dysfunction
Despite extensive evidence demonstrating significant social dysfunction in children and adults exposed to CM, there is limited knowledge on more specific processes and mechanisms that underlie broader social problems, and on factors that mediate the positive effects of intact social functioning on mental and physical health. This, in turn, limits the capacity to develop effective preventative and therapeutic interventions. We therefore propose that future research focuses on identifying the specific processes that contribute to broader social problems as well as on processes that mediate the relationship between intact social functioning and mental and physical health (Fig. 1). In the following sections, we outline specific aims (summarized in Table 1) and methods (summarized in Table 2) for such research.
Aims of Future Research
Identification of Key Interpersonal and Intrapersonal Socially Relevant Processes Affected by CM
The Role of Attachment
One key process already well known to be affected by CM is a child's ability to build secure and enduring relationships with their caregivers [58]. As proposed by attachment theory, a person's early interactions and relationships with their primary caregivers shape later attachment behavior [59]. A person's attachment style (i.e., behavioral tendencies and preferences that define the degree to which someone avoids or seeks attachment experiences) seems to be relatively stable across the lifespan [60] and affects the perceived quality of relationships with peers, romantic partners, and even children [61]. There is evidence for a strong relationship between CM and insecure attachment [62], and attachment difficulties, in turn, are linked to broad socio-interpersonal problems (in disclosure, social support, and acknowledgment) in adulthood. We propose that alterations in specific socially relevant processes mediate the relationship between attachment difficulties and impaired social functioning, including revictimization [48, 63], which should be tested in future research (Fig. 1).
In attempting to identify the specific processes that underlie the above-described broad problems in social functioning it thus seems promising to assess processes that are likely to be influenced by attachment difficulties (Fig. 1). However, claims of attachment theory, including the conceptualization of different attachment styles, are based on a Western child-rearing philosophy, which focuses on mother-infant attachment and emphasizes the development of personal autonomy. In its present form, attachment theory is thus not applicable to other cultures (e.g., [64]). When investigating effects of CM on attachment styles and how they impact specific social processes, it is thus necessary to apply (and, where necessary, first develop) attachment-related concepts that reflect cultural variation.
Processes Known to Be Affected by CM
Some of the socially relevant processes known to be affected by CM (Fig. 1) have been documented. For instance, CM is linked to heightened emotional reactivity and problems in emotion regulation [65]. Furthermore, CM has been linked to alterations in the perception and interpretation of emotional [66, 67] and neutral facial expressions [68, 69, 70]. Children exposed to CM tend to perceive neutral expressions as more similar to negative emotional expressions [70]. Similarly, adults with (vs. without) histories of CM more frequently interpret neutral expressions as feelings of anger, sadness, fear, and contempt [68, 69]. This suggests that the negativity bias observed in children may persist throughout the life course. There is also less consistent evidence that children exposed to CM show diminished cognitive understanding of other individuals' mental states [71], with some of these effects persisting into adulthood [72] and impairments being more pronounced with exposure to CM across a greater number of time periods [73]. Furthermore, it has been reported that sexually abused children, especially those exposed to intrafamiliar sexual abuse, have greater difficulties in mentalizing [74]. Finally, revictimized women with a history of childhood sexual and physical abuse were found to perceive photographs of males with stronger implicit facial cues of aggressiveness as more attractive than revictimized women without such a history, identifying a social processing bias that could increase risk for future victimizing relationships [75].
Processes to Be Targeted by Future Research
Further research aimed at identifying processes that are likely affected by attachment difficulties (Fig. 1) should, i.a., focus on problems in the regulation of closeness and distance which might contribute to partnership conflict and reduced sexual and relationship satisfaction. It has recently been proposed that based on learning history, individuals exposed to CM show abnormal neural responses to social signals, such as facial expressions [76] or the perception of touch [77], which might result in discomfort in situations of physical proximity, and a preference for larger interpersonal distances [77, 78, 79]. In addition, future studies should try to identify alterations in communicative processes and behaviors that contribute to negative evaluation by others [51]. For example, non-verbal signals (e.g., body posture, facial expressions, and expressions of emotions in the voice) might induce cognitive, affective, and behavioral responses in interaction partners, affecting the quality of interactions and making it difficult to build and maintain social relationships [80]. Moreover, interpersonal processes such as (culture-dependent) interpersonal emotion regulation, shared social identities, group memberships, and social identity management have received increased attention in basic emotion science and social psychology research in recent years [81, 82] and might be of importance for the field of traumatic stress, including CM.
Identifying Modulating Factors
Various factors (e.g., social context, pre-existing mental disorders) may affect the degree to which alterations in specific social processes are present in a specific situation. That is, alterations in specific social processes might vary both within and between individuals affected by CM. It is therefore crucial to identify factors that determine whether and to what degree specific social processes are adversely affected by CM. In addition to socio-cultural factors, negative interpretations of non-verbal signals (e.g., facial expressions) might occur in some but not in other situations. For example, individuals affected by CM might display negative interpretations which activate negative schemas in interpersonal situations with strangers [83] but not in the real (or imagined) presence of trusted, close others [84]. Similarly, preferred interpersonal distances might vary within individuals. That is, a person who has experienced CM may alternate between preferring close proximity and larger distances, depending on their current cognitive, emotional, and motivational state, and on the person they interact with [78]. In addition, potential compensatory mechanisms should be explored. That is, potentially harmful alterations in specific social processes (e.g., in understanding non-verbal emotional signals) might be compensated by other skills (e.g., by the ability to interpret what another person says explicitly). In sum, research should explore internal (e.g., an individual's current emotional state, personal resources in the form of compensatory mechanisms) and external factors (e.g., social context, cultural factors) that enhance or buffer alterations in social processes (Fig. 1).
Examining the Relationship between Specific Social Processes and Broader Social Problems
It is essential to establish the extent to which alterations in specific socially relevant skills and processes in individuals who have experienced CM underpin broader problems in social functioning (Fig. 1). It seems likely that deficits in socio-emotional and socio-cognitive skills lead to problems in interpersonal interactions, which may, in turn, be related to a lower perceived quality of relationships (as one aspect of social functioning). For example, the ability to read others' emotions helps us to infer their current affective state, thoughts, and intentions. Based on this information, people can modulate their own behavior, and − through responsive, trust-building actions − bond with other individuals or groups [85]. In non-clinical populations, adequate perception of others' emotions has in fact been linked to relationship satisfaction [86, 87, 88]. However, the presence and direction of this link depends on the sex of relationship partners [86] and on the type of emotions [88].
The few studies that have assessed whether alterations in specific social processes are related to broader social problems in individuals affected by CM suggest that poor emotion regulation skills (including difficulties with emotional awareness [89]), maladaptive internalized schemas [90], and women's and their partner's accuracy in reading their partner's negative emotions [87] mediate the association between CM and relationship satisfaction. Research in this field needs to replicate these initial findings and explore whether other social processes known to be affected by CM, such as negative interpretations of facial expressions, larger preferred interpersonal distances, negative judgments by others, or the perception of aggressive photographed men as attractive [43, 51, 68, 69, 75, 77, 78, 79], have a negative impact on relationship satisfaction and other aspects of social functioning known to be affected by CM (Fig. 1). Moreover, whether these findings from non-clinical populations apply to individuals affected by CM with mental disorders is deserving of investigation. Relatedly, it is important to investigate whether effects are driven by CM or by associated psychopathology (e.g., PTSD and depression). Future research should thus use study designs as well as statistical methods that allow the dissociation of these effects [e.g., 69].
Positive Effects of Social Functioning: Identifying Mechanisms
The factors that mediate the effects of intact social functioning on mental and physical health are not well understood. There is evidence that the relationship between CM and allostatic load, as measured by indices of hypothalamic-pituitary-adrenal axis, neuroendocrine, immune, and sympathetic nervous system activation, is partially mediated by poor social support [91]. This suggests that supportive social relationships exert a positive effect on mental and physical well-being at least in part, by buffering the effects of chronic stress (CM) on allostatic load (see Fig. 1). However, evidence in this area is extremely limited and further research is urgently needed to elucidate the biological pathways via which social support may benefit individuals exposed to CM. Moreover, due to the lack of causal evidence in this field, it is hard to infer clear conclusions as to whether impaired social skills cause mental health and adverse outcomes, or whether mental disorders impair social functioning, or both.
Methodological Considerations
Assessing Social Processes Inside and Outside the Laboratory
Assessment of social processes requires laboratory studies conducted under controlled conditions, allowing for systematic variation of the factors of interest and control of confounding variables. Current research conducted in the laboratory frequently relies on experimental stimuli that differ strongly from social stimuli outside the laboratory [92]. For instance, pictures of facial expressions are used to assess emotion recognition [66] and computerized tasks are used to assess preferred interpersonal distance (e.g., [93]). These approaches allow one to standardize characteristics of social stimuli (e.g., the intensity of a facial expression or the exact interpersonal distance), yet they limit the conclusions that can be made regarding participants' behavior in real-life. While this is a general drawback of standardized experimental stimuli, it seems particularly important that socially relevant processes are also examined as they occur naturally. Next to observing relevant phenomena outside the laboratory, this can be achieved by developing and applying more non-standardized or partially standardized interactive experimental paradigms that allow for the assessment of social processes under real or close to real-life conditions. For example, couples or other interaction partners can be brought to the laboratory to discuss a topic (e.g., [94]) while being filmed (e.g., [95]), allowing for high ecological validity and generalizability and, at the same time, control of the environment and content of the interaction. Also, the use of virtual reality environments might help establish close to real-life settings under controlled conditions, for example when assessing whether preferred interpersonal distances are affected by the approaching person's facial expression [96].
Adopting Longitudinal and Multi-Method Assessments in an Interdisciplinary Context
Consistent with allostatic load incurred by chronic stress, CM produces “biological scars” [97] that have a bearing on premature aging in later adult years and that accelerate biological aging in adults with mood and anxiety disorders through processes such as epigenetic aging and telomere attrition [98]. In turn, increased satisfaction with social ties [99] and more positive and prosocial emotions in social situations [100] are linked to healthy aging (Fig. 1). Currently, there is a dearth of evidence on the impact of CM on relational-affective processes and social functioning in older adults. As relationship and affective domains are dynamic over the lifespan, repeated longitudinal measurements are needed to map these domains to mental and physical health trajectories [101] and to assess how both socially important impairments and skills develop, interact, and predict the quality of social relationships over time.
Furthermore, assessing social processes requires multi-method approaches. While retrospective self-report measures are prone to memory biases and show limited ecological validity, ecological momentary assessment (EMA; repeated real-time sampling of behaviors and experiences in their natural environment) overcomes these limitations and enables the study of socially relevant microprocesses with different interaction partners [102]. Nonetheless, effects of social desirability can distort self-report measures, including EMA. Thus, incorporation of behavioral or psychophysiological assessments can provide a crucial validation of findings based on self-report [103]. Even seemingly simple processes such as the perception of a facial expression comprise various cognitive and emotional processes that mutually impact one another and interplay with neuronal [104], peripheral physiological [105], hormonal [106], cultural [107], and genetic factors [5, 7].
Methodologically sound research, including multi-method measurements, thus requires professionals from different disciplines and with specific background knowledge and experience (ranging from animal research to developmental psychology and computer science). Many socially relevant skills and processes are not yet fully understood in normally developing individuals. For example, the role of automatic imitation of facial expressions in facial emotion recognition [108] and the biological (e.g., endocrinological) factors that determine how close we prefer to stand to someone [93, 96] still need to be understood in a comprehensive way. Equally, the concept of allostatic load provides a key biological framework through which the links between stress, mental health, and physical health can be understood. It is thus important to seek collaborations with basic science researchers to understand socially relevant processes in the general population, and to ensure that research in CM reflects the state of the art in the field with respect to methodological approaches (Table 2).
Taking Cultural Factors into Account and Fostering Global Collaborations
When assessing social processes and related concepts, it is essential to account for cultural factors which shape social perception and functioning [109]. For example, decades of research underscore the importance of cultural differences in the expression, perception, response to, and appraisal of emotion [e.g., 107]. Furthermore, collectivistic cultural groups (e.g., Asian cultures) engage more strongly in interpersonal emotion regulation strategies than individualistic cultural groups (e.g., North American cultures) [82], and higher interdependence predicts higher well-being in Japan while higher independence predicts higher levels of well-being and health in the USA [110]. Culture also affects which emotion regulation strategies are deemed beneficial, including in the aftermath of trauma [111]. Moreover, culture influences the effectiveness of close relationships and social support following exposure to life stressors [112]. Thus, cultural differences have applicability in the area of psychotraumatology [113] and need to be considered in research on CM and social functioning.
When focusing on the cultural milieu, it is important to recognize how beliefs and values may be internalized differently between distinct ethnic groups in a culture and different cultures within a single ethnic group, as well as the intragroup differences present in both cases [114]. To broaden our understanding of how cultural factors impact the relationship between CM and socially relevant processes, cross-national research collaborations [115], including researchers from currently underrepresented countries, are needed. This will allow for replication across countries and strengthen the reliability and generalizability of findings.
Although capturing cultural and ethnic variables and parsing them out from intragroup effects is a complex long-term undertaking, the development of sound psychometric assessment tools through standardized translation and back-translation procedures is an important basic step for cross-cultural collaboration. Collaborative groups should also consider joint development of new psychometric tools and experimental assessment paradigms that are suitable for diverse cultural and ethnic groups. When translating existing and developing new self-report scales, clinimetric selection criteria should be considered, next to applying traditional psychometric criteria [116]. The clinimetric approach focuses on the clinical utility of self-report measures, while disregarding other (traditional psychometric) criteria such as the unidimensionality of “to-be-assessed” constructs [116].
Targeting Social Functioning in Individuals Affected by CM: Intervention Approaches
Existing interventions that aim to diminish or prevent CM in at-risk families focus on parenting skills and social support (e.g., through home visitations, parent training, or multisystemic interventions) [117] as well as psychoeducational group interventions (e.g., [118]), training in emotionally supportive parent-child communication [119], and psychotherapeutic approaches that target social functioning in populations exposed to CM [120]. However, there is still a need for specific interventions that directly target social functioning in victims of CM [77, 121]. Training of social problem-solving skills has shown benefits for emotional problems, interpersonal communication, and assertiveness in traumatized youth in residential settings [122]. Furthermore, Skills Training in Affective and Interpersonal Regulation (STAIR), which encompasses strategies for changing relationship patterns and becoming closer to others, showed promising results in women with PTSD related to CM [123].
As major steps of socio-emotional development, including the development of attachment relationships, take place in early childhood [124], interventions to further social functioning should be applied as early as possible to reduce long-term risk for impaired social functioning, and consequently poor mental health [125]. Nonetheless, given the pervasive and chronic nature of CM [126], it seems unlikely that isolated interventions to improve social functioning will be sufficient to address the complex problems arising from CM. During later developmental stages and adulthood, when mental health problems may have become chronic, approaches that focus on symptoms of mental health problems could be beneficial. In this respect, interventions that target social functioning might also benefit interactions with health care providers, which is important considering the significance of the quality of the therapeutic relationship for therapy completion and outcome [127], and the barriers that difficulties in social skills could present to establishing a strong therapeutic partnership [128].
In summary, a range of interventions that include a focus on social relationships or processes have been tested, but we still have limited understanding of what elements of social functioning should be targeted through intervention to benefit well-being among those exposed to CM. A key question to be addressed is whether social processes related to social functioning should be worked on directly (e.g., in the form of emotion recognition training) and/or whether such processes can also be changed indirectly, for example through establishing a positive relationship with the therapist [129] or by working on maladaptive relational schemas [83].
The focus of interventions for CM to date has been on preventing or addressing negative outcomes, particularly a lack of significant symptoms. However, it has been argued that the presence of positive affect and psychological well-being should also be considered important therapeutic outcomes, in line with the concept of euthymia [130]. Euthymia is a transdiagnostic construct that shifts the focus away from specific disorder symptoms, which is potentially relevant to CM given its links to varied mental disorders. Well-being therapy [131] focuses explicitly on positive relationships, alongside other components of psychological well-being, in order to achieve a state of euthymia [132, 133]. Well-being therapy is typically combined with cognitive behavioral approaches and has yielded positive effects in patients with mood and anxiety disorders [134]. Other euthymia-oriented interventions such as mindfulness-based cognitive therapy [135] and acceptance and commitment therapy [136] have also shown positive effects, e.g., on rates of relapse and psychological well-being, in patients suffering from anxiety, depression, and chronic pain [137, 138]. Interventions pursuing social functioning but also euthymia more broadly might thus help individuals affected by CM to maintain well-being and to build healthy relationships and a sense of belonging, even when faced with recurrent and chronic health problems.
Conclusion
The lines of research proposed will expand the knowledge base needed to globally develop and implement preventive measures that counteract both the occurrence of CM and its adverse effects. Understanding the effects of CM on social functioning, and contributory cultural and ethnic influences, will advance the development (and assessment of effectiveness) of novel interventions and the refinement of existing interventions to strengthen social functioning. Given the major individual, societal, and economic costs of CM, improving social functioning in the context of CM is relevant not only for an individual's personal health and well-being, but also from public health (i.e., informing communities and raising awareness of CM) and economic perspectives.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The preparation of this manuscript was supported by two grants from the Swiss National Science Foundation (S-86403-02 and 10001C_185356) to Monique C. Pfaltz. Natalia E. Fares-Otero was supported by CIBERSAM: Biomedical Research Networking Center for Mental Health Network, Spain, and by a scholarship provided by the German Academic Exchange Service DAAD: Deutscher Akademischer Austauschdienst (91629413).
Author Contributions
All authors contributed to the conception of the work as part of regular discussion within the framework of the Global Collaboration on Traumatic Stress (www.global-psychotrauma.net), socio-emotional development across cultures subtheme (www.global-psychotrauma.net/socio-emotional-development). M.P., S.H., S.S., U.S., M.R.S., and S.H.N. wrote the first draft. All authors contributed substantially to the revision of the first draft. M.P., N.E.F.-O., S.H., S.S., U.S., S.H.N., and M.R.S. revised the manuscript. All authors approved the final version of the submitted manuscript.
References
- 1.Child maltreatment [Internet] Geneva: WHO; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/child-maltreatment. [Google Scholar]
- 2.Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health. 2018 Dec;18((1)):1164. doi: 10.1186/s12889-018-6044-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017 Aug;2((8)):e356–66. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 4.Moreno-López L, Ioannidis K, Askelund AD, Smith AJ, Schueler K, van Harmelen AL. The resilient emotional brain: a scoping review of the medial prefrontal cortex and limbic structure and function in resilient adults with a history of childhood maltreatment. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020 Apr;5((4)):392–402. doi: 10.1016/j.bpsc.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Wang Q, Shelton RC, Dwivedi Y. Interaction between early-life stress and FKBP5 gene variants in major depressive disorder and post-traumatic stress disorder: a systematic review and meta-analysis. J Affect Disord. 2018 Jan;225:422–8. doi: 10.1016/j.jad.2017.08.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry. 2007 May;64((5)):577–84. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- 7.Warrier V, Kwong ASF, Luo M, Dalvie S, Croft J, Sallis HM, et al. Gene-environment correlations and causal effects of childhood maltreatment on physical and mental health: a genetically informed approach. Lancet Psychiatry. 2021 May;8((5)):373–86. doi: 10.1016/S2215-0366(20)30569-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rafiq S, Campodonico C, Varese F. The relationship between childhood adversities and dissociation in severe mental illness: a meta-analytic review. Acta Psychiatr Scand. 2018 Dec;138((6)):509–25. doi: 10.1111/acps.12969. [DOI] [PubMed] [Google Scholar]
- 9.Hutchens BF, Kearney J, Kennedy HP. Survivors of child maltreatment and postpartum depression: an integrative review. J Midwifery Womens Health. 2017 Nov;62((6)):706–22. doi: 10.1111/jmwh.12680. [DOI] [PubMed] [Google Scholar]
- 10.Lefkovics E, Baji I, Rigó J. Impact of maternal depression on pregnancies and on early attachment. Infant Ment Health J. 2014 Aug;35((4)):354–65. doi: 10.1002/imhj.21450. [DOI] [PubMed] [Google Scholar]
- 11.Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring up to 16 years of age. J Am Acad Child Adolesc Psychiatry. 2011 May;50((5)):460–70. doi: 10.1016/j.jaac.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Moog NK, Heim CM, Entringer S, Kathmann N, Wadhwa PD, Buss C. Childhood maltreatment is associated with increased risk of subclinical hypothyroidism in pregnancy. Psychoneuroendocrinology. 2017 Oct;84:190–6. doi: 10.1016/j.psyneuen.2017.07.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buss C, Entringer S, Moog NK, Toepfer P, Fair DA, Simhan HN, et al. Intergenerational transmission of maternal childhood maltreatment exposure: implications for fetal brain development. J Am Acad Child Adolesc Psychiatry. 2017;56((5)):373–82. doi: 10.1016/j.jaac.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moog NK, Entringer S, Rasmussen JM, Styner M, Gilmore JH, Kathmann N, et al. Intergenerational effect of maternal exposure to childhood maltreatment on newborn brain anatomy. Biol Psychiatry. 2018 Jan;83((2)):120–27. doi: 10.1016/j.biopsych.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindsay KL, Entringer S, Buss C, Wadhwa PD. Intergenerational transmission of the effects of maternal exposure to childhood maltreatment on offspring obesity risk: a fetal programming perspective. Psychoneuroendocrinology. 2020 Jun;116:104659. doi: 10.1016/j.psyneuen.2020.104659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh DL, Jerman P, Silvério Marques S, Koita K, Purewal Boparai SK, Burke Harris N, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018 Dec;18((1)):83. doi: 10.1186/s12887-018-1037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huffhines L, Jackson Y. Child maltreatment, chronic pain, and other chronic health conditions in youth in foster care. J Child Adolesc Trauma. 2019 Dec;12((4)):437–45. doi: 10.1007/s40653-019-0248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng QX, Yong BZJ, Ho CYX, Lim DY, Yeo WS. Early life sexual abuse is associated with increased suicide attempts: an update meta-analysis. J Psychiatr Res. 2018 Apr;99:129–41. doi: 10.1016/j.jpsychires.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Wang ZY, Hu M, Yu TL, Yang J. The relationship between childhood maltreatment and risky sexual behaviors: a meta-analysis. Int J Environ Res Public Health. 2019 Sept;16((19)):3666. doi: 10.3390/ijerph16193666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cicchetti D, Handley ED. Child maltreatment and the development of substance use and disorder. Neurobiol Stress. 2019 Feb;10:100144. doi: 10.1016/j.ynstr.2018.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health. 2015 Sept;37((3)):445–54. doi: 10.1093/pubmed/fdu065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paquola C, Bennett MR, Lagopoulos J. Understanding heterogeneity in grey matter research of adults with childhood maltreatment − a meta-analysis and review. Neurosci Biobehav Rev. 2016 Oct;69:299–312. doi: 10.1016/j.neubiorev.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 23.Juster R, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, et al. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Develop Psychopathol. 2011 Aug;23((3)):725–76. doi: 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- 24.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009 Jun;10:434–45. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 25.Herzog JI, Thome J, Demirakca T, Koppe G, Ende G, Lis S, et al. Influence of severity of type and timing of retrospectively reported childhood maltreatment on female amygdala and hippocampal volume. Sci Rep. 2020 Feb;10((1)):1–10. doi: 10.1038/s41598-020-57490-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raymond C, Marin MF, Wolosianski V, Journault AA, Longpré C, Lupien SJ. Adult women first exposed to early adversity after 8 years old show attentional bias to threat. Front Behav Neurosci. 2021 May;15:628099. doi: 10.3389/fnbeh.2021.628099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vogel SC, Perry RE, Brandes-Aitken A, Braren S, Blair C. Deprivation and threat as developmental mediators in the relation between early life socioeconomic status and executive functioning outcomes in early childhood. Dev Cogn Neurosci. 2021 Feb;47:100907. doi: 10.1016/j.dcn.2020.100907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russotti J, Warmingham JM, Duprey EB, Handley ED, Manly JT, Rogosch FA, et al. Child maltreatment and the development of psychopathology: the role of developmental timing and chronicity. Child Abuse Negl. 2021 Oct;120:105215. doi: 10.1016/j.chiabu.2021.105215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on health: a systematic review. Psychother Psychosom. 2021;90((1)):11–27. doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- 30.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010 Sept;35((1)):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Widom CS, Horan J, Brzustowicz L. Childhood maltreatment predicts allostatic load in adulthood. Child Abuse Negl. 2015 Sept;47:59–69. doi: 10.1016/j.chiabu.2015.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scheuer S, Wiggert N, Brückl TM, Awaloff Y, Uhr M, Lucae S, et al. Childhood abuse and depression in adulthood: the mediating role of allostatic load. Psychoneuroendocrinology. 2018 Aug;94:134–42. doi: 10.1016/j.psyneuen.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 33.Peterson C, Florence C, Klevens J. The economic burden of child maltreatment in the United States, 2015. Child Abuse Negl. 2018 Dec;86:178–83. doi: 10.1016/j.chiabu.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madigan S, Cyr C, Eirich R, Fearon RMP, Ly A, Rash C, et al. Testing the cycle of maltreatment hypothesis: meta-analytic evidence of the intergenerational transmission of child maltreatment. Dev Psychopathol. 2019 Feb;31((1)):23–51. doi: 10.1017/S0954579418001700. [DOI] [PubMed] [Google Scholar]
- 35.Langevin R, Marshall C, Kingsland E. Intergenerational cycles of maltreatment: a scoping review of psychosocial risk and protective factors. Trauma Violence Abuse. 2021 Oct;22((4)):672–88. doi: 10.1177/1524838019870917. [DOI] [PubMed] [Google Scholar]
- 36.Wang Y, Chung MC, Wang N, Yu X, Kenardy J. Social support and posttraumatic stress disorder: a meta-analysis of longitudinal studies. Clin Psychol Rev. 2021 Apr;85:101998. doi: 10.1016/j.cpr.2021.101998. [DOI] [PubMed] [Google Scholar]
- 37.Yule K, Houston J, Grych J. Resilience in children exposed to violence: a meta-analysis of protective factors across ecological contexts. Clin Child Fam Psychol Rev. 2019 Sept;22((3)):406–31. doi: 10.1007/s10567-019-00293-1. [DOI] [PubMed] [Google Scholar]
- 38.Holz NE, Tost H, Meyer-Lindenberg A. Resilience and the brain: a key role for regulatory circuits linked to social stress and support. Mol Psychiatry. 2020 Feb;25((2)):379–96. doi: 10.1038/s41380-019-0551-9. [DOI] [PubMed] [Google Scholar]
- 39.Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017 Nov;152:157–71. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 40.Kinard EM. Perceived social skills and social competence in maltreated children. Am J Orthopsychiatry. 1999;69((4)):465–81. doi: 10.1037/h0080395. [DOI] [PubMed] [Google Scholar]
- 41.Mattar JW. The difference in emotional intelligence in relation to levels of maltreatment of Jordanian secondary school students. Int J Adolesc Youth. 2018 Jan;23((1)):61–9. [Google Scholar]
- 42.Xiao Y, Jiang L, Yang R, Ran H, Wang T, He X, et al. Childhood maltreatment with school bullying behaviors in Chinese adolescents: a cross-sectional study. J Affect Disord. 2021 Feb;281:941–8. doi: 10.1016/j.jad.2020.11.022. [DOI] [PubMed] [Google Scholar]
- 43.Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology: pathways linking maltreatment, emotion regulation, and psychopathology. J Child Psychol Psychiatry. 2009 Dec;51((6)):706–16. doi: 10.1111/j.1469-7610.2009.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zamir O. Childhood maltreatment and relationship quality: a review of type of abuse and mediating and protective factors. Trauma Violence Abuse. 2021 Mar; doi: 10.1177/1524838021998319. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 45.Savage LÉ, Tarabulsy GM, Pearson J, Collin-Vézina D, Gagné LM. Maternal history of childhood maltreatment and later parenting behavior: a meta-analysis. Dev Psychopathol. 2019 Feb;31((1)):9–21. doi: 10.1017/S0954579418001542. [DOI] [PubMed] [Google Scholar]
- 46.White HR, Widom CS. Intimate partner violence among abused and neglected children in young adulthood: the mediating effects of early aggression, antisocial personality, hostility and alcohol problems. Aggr Behav. 2003 Aug;29((4)):332–45. [Google Scholar]
- 47.Labella MH, Johnson WF, Martin J, Ruiz SK, Shankman JL, Englund MM, et al. Multiple dimensions of childhood abuse and neglect prospectively predict poorer adult romantic functioning. Pers Soc Psychol Bull. 2018 Feb;44((2)):238–51. doi: 10.1177/0146167217736049. [DOI] [PubMed] [Google Scholar]
- 48.Walker HE, Freud JS, Ellis RA, Fraine SM, Wilson LC. The prevalence of sexual revictimization: a meta-analytic review. Trauma Violence Abuse. 2019 Jan;20((1)):67–80. doi: 10.1177/1524838017692364. [DOI] [PubMed] [Google Scholar]
- 49.Evans SE, Steel AL, DiLillo D. Child maltreatment severity and adult trauma symptoms: does perceived social support play a buffering role? Child Abuse Negl. 2013 Nov;37((11)):934–43. doi: 10.1016/j.chiabu.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shevlin M, McElroy E, Murphy J. Loneliness mediates the relationship between childhood trauma and adult psychopathology: evidence from the adult psychiatric morbidity survey. Soc Psychiatry Psychiatr Epidemiol. 2015 Apr;50((4)):591–601. doi: 10.1007/s00127-014-0951-8. [DOI] [PubMed] [Google Scholar]
- 51.Hepp J, Störkel LM, Kieslich PJ, Schmahl C, Niedtfeld I. Negative evaluation of individuals with borderline personality disorder at zero acquaintance. Behav Res Ther. 2018 Dec;111:84–91. doi: 10.1016/j.brat.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 52.McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014 Nov;47:578–91. doi: 10.1016/j.neubiorev.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson D, Policelli J, Li M, Dharamsi A, Hu Q, Sheridan MA, et al. Associations of early-life threat and deprivation with executive functioning in childhood and adolescence: a systematic review and meta-analysis. JAMA Pediatr. 2021 Nov;175((11)):e212511. doi: 10.1001/jamapediatrics.2021.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sheridan MA, McLaughlin KA. Neurodevelopmental mechanisms linking ACEs with psychopathology. In: Asmundson GJG, Afifi TO, editors. Adverse childhood experiences: using evidence to advance research, practice, policy, and prevention. London: Academic Press; 2020. pp. 265–85. [Google Scholar]
- 55.Sheridan MA, Shi F, Miller AB, Salhi C, McLaughlin KA. Network structure reveals clusters of associations between childhood adversities and development outcomes. Dev Sci. 2020 Sep;23:e12934. doi: 10.1111/desc.12934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hildyard KL, Wolfe DA. Child neglect: developmental issues and outcomes. Child Abuse Negl. 2002 Jun;26((67)):679–95. doi: 10.1016/s0145-2134(02)00341-1. [DOI] [PubMed] [Google Scholar]
- 57.Lueger-Schuster B, Knefel M, Glück TM, Jagsch R, Kantor V, Weindl D. Child abuse and neglect in institutional settings, cumulative lifetime traumatization, and psychopathological long-term correlates in adult survivors: the Vienna Institutional Abuse Study. Child Abuse Negl. 2018 Feb;76:488–501. doi: 10.1016/j.chiabu.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 58.Nowalis S, Godleski SA, Schenkel LS. Attachment as a moderator in the relation between child maltreatment and symptoms of depression. J Interpers Violence. 2022;37((3–4)):NP1516–43. doi: 10.1177/0886260520933050. [DOI] [PubMed] [Google Scholar]
- 59.Bowlby J. A secure base: parent-child attachment and healthy human development. London: Routledge; 1988. [Google Scholar]
- 60.Fraley RC, Vicary AM, Brumbaugh CC, Roisman GI. Patterns of stability in adult attachment: an empirical test of two models of continuity and change. J Pers Soc Psychol. 2011 Nov;101((5)):974–92. doi: 10.1037/a0024150. [DOI] [PubMed] [Google Scholar]
- 61.Lo CKM, Chan KL, Ip P. Insecure adult attachment and child maltreatment: a meta-analysis. Trauma Violence Abuse. 2019 Dec;20((5)):706–19. doi: 10.1177/1524838017730579. [DOI] [PubMed] [Google Scholar]
- 62.Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Attachment security and disorganization in maltreating and high-risk families: a series of meta-analyses. Dev Psychopathol. 2010 Feb;22((1)):87–108. doi: 10.1017/S0954579409990289. [DOI] [PubMed] [Google Scholar]
- 63.Liem JH, Boudewyn AC. Contextualizing the effects of childhood sexual abuse on adult self- and social functioning: an attachment theory perspective. Child Abuse Negl. 1999 Nov;23((11)):1141–57. doi: 10.1016/s0145-2134(99)00081-2. [DOI] [PubMed] [Google Scholar]
- 64.Keller H. Attachment and culture. J Cross Cult Psychol. 2013;44((2)):175–94. [Google Scholar]
- 65.Lavi I, Katz LF, Ozer EJ, Gross JJ. Emotion reactivity and regulation in maltreated children: a meta‐analysis. Child Dev. 2019 Sep;90((5)):1503–24. doi: 10.1111/cdev.13272. [DOI] [PubMed] [Google Scholar]
- 66.Doretto V, Scivoletto S. Effects of early neglect experience on recognition and processing of facial expressions: a systematic review. Brain Sci. 2018 Jan;8((1)):10. doi: 10.3390/brainsci8010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.da Silva Ferreira GC, de Sousa Crippa JA, de Lima Osório F. Facial emotion processing and recognition among maltreated children: a systematic literature review. Front Psychol. 2014 Dec;5:1460. doi: 10.3389/fpsyg.2014.01460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Catalan A, Díaz A, Angosto V, Zamalloa I, Martínez N, Guede D, et al. Influye el trauma infantil en el reconocimiento de las emociones faciales independientemente del diagnóstico de trastorno mental grave? Rev Psiquiatr Salud Ment. 2020 Jul;13((3)):140–9. doi: 10.1016/j.rpsm.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 69.Pfaltz MC, Passardi S, Auschra B, Fares-Otero NE, Schnyder U, Peyk P. Are you angry at me? Negative interpretations of neutral facial expressions are linked to child maltreatment but not to posttraumatic stress disorder. Eur J Psychotraumatol. 2019 Dec;10((1)):1682929. doi: 10.1080/20008198.2019.1682929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pollak SD, Cicchetti D, Hornung K, Reed A. Recognizing emotion in faces: developmental effects of child abuse and neglect. Dev Psychol. 2000 Sep;36((5)):679–88. doi: 10.1037/0012-1649.36.5.679. [DOI] [PubMed] [Google Scholar]
- 71.Benarous X, Guilé JM, Consoli A, Cohen D. A systematic review of the evidence for impaired cognitive theory of mind in maltreated children. Front Psychiatry. 2015 Jul;6:108. doi: 10.3389/fpsyt.2015.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Germine L, Dunn EC, McLaughlin KA, Smoller JW. Childhood adversity is associated with adult theory of mind and social affiliation, but not face processing. PLoS One. 2015 Jun;10((6)):e0129612. doi: 10.1371/journal.pone.0129612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crawford KM, Choi K, Davis KA, Zhu Y, Soare TW, Smith AD, et al. Exposure to early childhood maltreatment and its effect over time on social cognition. Dev Psychopathol. 2022;34((1)):409–19. doi: 10.1017/S095457942000139X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ensink K, Normandin L, Target M, Fonagy P, Sabourin S, Berthelot N. Mentalization in children and mothers in the context of trauma: an initial study of the validity of the Child Reflective Functioning Scale. Br J Dev Psychol. 2015 Jun;33((2)):203–17. doi: 10.1111/bjdp.12074. [DOI] [PubMed] [Google Scholar]
- 75.Lieberz KA, Müller-Engelmann M, Bornefeld-Ettmann P, Priebe K, Weidmann A, Fydrich T, et al. Detecting implicit cues of aggressiveness in male faces in revictimized female PTSD patients and healthy controls. Psychiatry Res. 2018 Sep;267:429–37. doi: 10.1016/j.psychres.2018.05.061. [DOI] [PubMed] [Google Scholar]
- 76.McCrory EJ, De Brito SA, Kelly PA, Bird G, Sebastian CL, Mechelli A, et al. Amygdala activation in maltreated children during pre-attentive emotional processing. Br J Psychiatry. 2013 Apr;202((4)):269–76. doi: 10.1192/bjp.bp.112.116624. [DOI] [PubMed] [Google Scholar]
- 77.Maier A, Gieling C, Heinen-Ludwig L, Stefan V, Schultz J, Güntürkün O, et al. Association of childhood maltreatment with interpersonal distance and social touch preferences in adulthood. Am J Psychiatry. 2020 Jan;177((1)):37–46. doi: 10.1176/appi.ajp.2019.19020212. [DOI] [PubMed] [Google Scholar]
- 78.Vranic A. Personal space in physically abused children. Environ Behav. 2003 Jul;35((4)):550–65. [Google Scholar]
- 79.Lüönd AM, Wolfensberger L, Wingenbach T, Schnyder U, Weilenmann S, Pfaltz MC. Don't get too close to me: child maltreatment with and without depressive symptoms is linked to larger comfortable interpersonal distance towards strangers. Submitted. [DOI] [PMC free article] [PubMed]
- 80.van den Berg LJM, Tollenaar MS, Compier-de Block LHCG, Bakermans-Kranenburg MJ, Elzinga BM. An intergenerational family study on the impact of experienced and perpetrated child maltreatment on neural face processing. Psychoneuroendocrinology. 2019 May;103:266–75. doi: 10.1016/j.psyneuen.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 81.Muldoon OT, Haslam SA, Haslam C, Cruwys T, Kearns M, Jetten J. The social psychology of responses to trauma: social identity pathways associated with divergent traumatic responses. Eur Rev Soc Psychol. 2019 Jan;30((1)):311–48. [Google Scholar]
- 82.Liddell BJ, Williams EN. Cultural differences in interpersonal emotion regulation. Front Psychol. 2019 May;10:999. doi: 10.3389/fpsyg.2019.00999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pilkington PD, Bishop A, Younan R. Adverse childhood experiences and early maladaptive schemas in adulthood: a systematic review and meta‐analysis. Clin Psychol Psychother. 2021 May;28((3)):569–84. doi: 10.1002/cpp.2533. [DOI] [PubMed] [Google Scholar]
- 84.Mikulincer M, Shaver PR. Attachment theory and intergroup bias: evidence that priming the secure base schema attenuates negative reactions to out-groups. J Pers Soc Psychol. 2001 Jul;81((1)):97–115. [PubMed] [Google Scholar]
- 85.Fischer AH, Manstead ASR. Social functions of emotion. In: Lewis M, Haviland-Jones JM, Barrett LF, editors. Handbook of emotions. New York: Guilford Press; 2008. pp. 456–68. [Google Scholar]
- 86.Cohen S, Schulz MS, Weiss E, Waldinger RJ. Eye of the beholder: the individual and dyadic contributions of empathic accuracy and perceived empathic effort to relationship satisfaction. J Fam Psychol. 2012;26((2)):236–45. doi: 10.1037/a0027488. [DOI] [PubMed] [Google Scholar]
- 87.Maneta EK, Cohen S, Schulz MS, Waldinger RJ. Linkages between childhood emotional abuse and marital satisfaction: the mediating role of empathic accuracy for hostile emotions. Child Abuse Negl. 2015 Jun;44:8–17. doi: 10.1016/j.chiabu.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Simpson JA, Orina MM, Ickes W. When accuracy hurts, and when it helps: a test of the empathic accuracy model in marital interactions. J Pers Soc Psychol. 2003 Nov;85((5)):881–93. doi: 10.1037/0022-3514.85.5.881. [DOI] [PubMed] [Google Scholar]
- 89.Bradbury LL, Shaffer A. Emotion dysregulation mediates the link between childhood emotional maltreatment and young adult romantic relationship satisfaction. J Aggress Maltreat Trauma. 2012 Jul;21((5)):497–515. [Google Scholar]
- 90.Messman-Moore TL, Coates AA. The impact of childhood psychological abuse on adult interpersonal conflict: the role of early maladaptive schemas and patterns of interpersonal behavior. J Emot Abuse. 2007 Dec;7((2)):75–92. [Google Scholar]
- 91.Horan JM, Widom CS. From childhood maltreatment to allostatic load in adulthood: the role of social support. Child Maltreat. 2015 Nov;20((4)):229–39. doi: 10.1177/1077559515597063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Abel DB, Minor KS. Social functioning in schizophrenia: comparing laboratory-based assessment with real-world measures. J Psychiatr Res. 2021 Jun;138:500–6. doi: 10.1016/j.jpsychires.2021.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Perry A, Nichiporuk N, Knight RT. Where does one stand: a biological account of preferred interpersonal distance. Soc Cogn Affect Neurosci. 2016 Feb;11((2)):317–26. doi: 10.1093/scan/nsv115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Weilenmann S, Luckner A, Huber C, Aron A, Schnyder U, Pfaltz MC. Experimental induction of emotional and sexual intimacy: self-reported and physiological responses to an extension of the German fast friends procedure in individuals with and without child maltreatment. Arch Sex Behav. 2022;51((3)):1703–19. doi: 10.1007/s10508-021-02081-x. [DOI] [PubMed] [Google Scholar]
- 95.Bélanger C, Sabourin S, El-Baalbaki G. Behavioral correlates of coping strategies in close relationships. Eur J Psychol. 2012;8((3)):449–60. [Google Scholar]
- 96.Riem MME, Kunst LE, Steenbakkers FDF, Kir M, Sluijtman A, Karreman A, et al. Oxytocin reduces interpersonal distance: examining moderating effects of childrearing experiences and interpersonal context in virtual reality. Psychoneuroendocrinology. 2019 Oct;108:102–9. doi: 10.1016/j.psyneuen.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 97.Teicher MH. Scars that won't heal: the neurobiology of child abuse. Sci Am. 2002 Mar;286((3)):68–75. doi: 10.1038/scientificamerican0302-68. [DOI] [PubMed] [Google Scholar]
- 98.Kuzminskaite E, Penninx BWJH, van Harmelen AL, Elzinga BM, Hovens JGFM, Vinkers CH. Childhood trauma in adult depressive and anxiety disorders: an integrated review on psychological and biological mechanisms in the NESDA Cohort. J Affect Disord. 2021 Mar;283:179–91. doi: 10.1016/j.jad.2021.01.054. [DOI] [PubMed] [Google Scholar]
- 99.Rook KS, Charles ST. Close social ties and health in later life: strengths and vulnerabilities. Am Psychol. 2017 Sep;72((6)):567–77. doi: 10.1037/amp0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lwi SJ, Haase CM, Shiota MN, Newton SL, Levenson RW. Responding to the emotions of others: age differences in facial expressions and age-specific associations with relational connectedness. Emotion. 2019 Dec;19((8)):1437–49. doi: 10.1037/emo0000534. [DOI] [PubMed] [Google Scholar]
- 101.Smith TW, Weihs K. Emotion, social relationships, and physical health: concepts, methods, and evidence for an integrative perspective. Psychosom Med. 2019 Oct;81((8)):681–93. doi: 10.1097/PSY.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 102.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 103.Mauss IB, Robinson MD. Measures of emotion: a review. Cogn Emot. 2009 Feb;23((2)):209–37. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Del Casale A, Kotzalidis GD, Rapinesi C, Janiri D, Aragona M, Puzella A, et al. Neural functional correlates of empathic face processing. Neurosci Lett. 2017 Aug;655:68–75. doi: 10.1016/j.neulet.2017.06.058. [DOI] [PubMed] [Google Scholar]
- 105.Tsikandilakis M, Bali P, Derrfuss J, Chapman P. Anger and hostility: are they different? An analytical exploration of facial-expressive differences, and physiological and facial-emotional responses. Cogn Emot. 2020 Apr;34((3)):581–95. doi: 10.1080/02699931.2019.1664415. [DOI] [PubMed] [Google Scholar]
- 106.Osório FL, de Paula Cassis JM, Machado de Sousa JP, Poli-Neto O, Martín-Santos R. Sex hormones and processing of facial expressions of emotion: a systematic literature review. Front Psychol. 2018 Apr;9:529. doi: 10.3389/fpsyg.2018.00529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Matsumoto D, Sung Hwang H. Judging faces in context: faces in context. Soc Personal Psychol Compass. 2010 Jun;4((6)):393–402. [Google Scholar]
- 108.Holland AC, O'Connell G, Dziobek I. Facial mimicry, empathy, and emotion recognition: a meta-analysis of correlations. Cogn Emot. 2021 Jan;35((1)):150–68. doi: 10.1080/02699931.2020.1815655. [DOI] [PubMed] [Google Scholar]
- 109.Freeman JB, Rule NO, Ambady N. Progress in brain research [Internet] Amsterdam: Elsevier; 2009. The cultural neuroscience of person perception; pp. 191–201. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0079612309178135. [DOI] [PubMed] [Google Scholar]
- 110.Kitayama S, Karasawa M, Curhan KB, Ryff CD, Markus HR. Independence and interdependence predict health and wellbeing: divergent patterns in the United States and Japan. Front Psychol. 2010 Dec;1:163. doi: 10.3389/fpsyg.2010.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nagulendran A, Jobson L. Exploring cultural differences in the use of emotion regulation strategies in posttraumatic stress disorder. Eur J Psychotraumatol. 2020 Dec;11((1)):1729033. doi: 10.1080/20008198.2020.1729033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Campos B, Kim HS. Incorporating the cultural diversity of family and close relationships into the study of health. Am Psychol. 2017 Sep;72((6)):543–54. doi: 10.1037/amp0000122. [DOI] [PubMed] [Google Scholar]
- 113.Hansford M, Jobson L. Sociocultural context and the posttraumatic psychological response: considering culture, social support, and posttraumatic stress disorder. Psychol Trauma. 2021 Jan 28; doi: 10.1037/tra0001009. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 114.Oyserman D. Self-concept and identity. In: Tesser A, Schwarz N, editors. The Blackwell handbook of social psychology. Malden: Blackwell; 2001. pp. 499–517. [Google Scholar]
- 115.Olff M, Bakker A, Frewen P, Aakvaag H, Ajdukovic D, Brewer D, et al. Screening for consequences of trauma: an update on the global collaboration on traumatic stress. Eur J Psychotraumatology. 2020 Dec;11((1)):1752504. doi: 10.1080/20008198.2020.1752504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Carrozzino D, Patierno C, Guidi J, Berrocal Montiel C, Cao J, Charlson ME, et al. Clinimetric criteria for patient-reported outcome measures. Psychother Psychosom. 2021;90((4)):222–32. doi: 10.1159/000516599. [DOI] [PubMed] [Google Scholar]
- 117.Van der Put CE, Assink M, Gubbels J, van Solinge NFB. Identifying effective components of child maltreatment interventions: a meta-analysis. Clin Child Fam Psychol Rev. 2018 Jun;21((2)):171–202. doi: 10.1007/s10567-017-0250-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hébert M, Tourigny M. Effects of a psychoeducational group intervention for children victims of sexual abuse. J Child Adolescent Trauma. 2010;3:143–60. [Google Scholar]
- 119.Valentino K, Cummings EM, Borkowski J, Hibel LC, Lefever J, Lawson M. Efficacy of a reminiscing and emotion training intervention on maltreating families with preschool-aged children. Dev Psychol. 2019;55((11)):2365–78. doi: 10.1037/dev0000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cloitre M, Cohen LR, Ortigo KM, Jackson C, Koenen KC. Treating survivors of childhood abuse and interpersonal trauma: STAIR narrative therapy. New York: Guilford Press; 2020. [Google Scholar]
- 121.Finch M, Featherston R, Chakraborty S, Bjørndal L, Mildon R, Albers B, et al. Interventions that address institutional child maltreatment: an evidence and gap map. Campbell Syst Rev. 2021;17((1)):e1139. doi: 10.1002/cl2.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tyler PM, Aitken AA, Ringle JL, Stephenson JM, Mason WA. Evaluating social skills training for youth with trauma symptoms in residential programs. Psychol Trauma. 2021 Jan;13((1)):104–13. doi: 10.1037/tra0000589. [DOI] [PubMed] [Google Scholar]
- 123.Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, et al. Treatment for PTSD related to childhood abuse: a randomized controlled trial. Am J Psychiatry. 2010;167((8)):915–24. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- 124.Malik F, Marwaha R. Developmental stages of social emotional development in children. Treasure Island: StatPearls Publishing; 2018. [PubMed] [Google Scholar]
- 125.Afifi TO, MacMillan HL. Resilience following child maltreatment: a review of protective factors. Can J Psychiatry. 2011 May;56((5)):266–72. doi: 10.1177/070674371105600505. [DOI] [PubMed] [Google Scholar]
- 126.Kim H, Drake B. Cumulative prevalence of onset and recurrence of child maltreatment reports. J Am Acad Child Adolesc Psychiatry. 2019;58((12)):1175–83. doi: 10.1016/j.jaac.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 127.Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol. 2000 Jun;68((3)):438–50. [PubMed] [Google Scholar]
- 128.Hudson AR, De Coster L, Spoormans H, Verbeke S, Van der Jeught K, Brass M, et al. Childhood abuse and adult sociocognitive skills: distinguishing between self and other following early trauma. J Interpers Violence. 2021;36((23–24)):NP13254–74. doi: 10.1177/0886260520906190. [DOI] [PubMed] [Google Scholar]
- 129.Slade A, Holmes J. Attachment and psychotherapy. Curr Opin Psychol. 2019;25:152–6. doi: 10.1016/j.copsyc.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 130.Fava GA, Guidi J. The pursuit of euthymia. World Psychiatry. 2020;19((1)):40–50. doi: 10.1002/wps.20698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fava GA, Ruini C. Development and characteristics of a well-being enhancing psychotherapeutic strategy: well-being therapy. J Behav Ther Exp Psychiatry. 2003 Mar;34((1)):45–63. doi: 10.1016/s0005-7916(03)00019-3. [DOI] [PubMed] [Google Scholar]
- 132.Guidi J, Fava GA. The emerging role of euthymia in psychotherapy research and practice. Clin Psychol Rev. 2020 Dec;82:101941. doi: 10.1016/j.cpr.2020.101941. [DOI] [PubMed] [Google Scholar]
- 133.Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83((1)):10–28. doi: 10.1159/000353263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fava GA, Cosci F, Guidi J, Tomba E. Well‐being therapy in depression: new insights into the role of psychological well‐being in the clinical process. Depress Anxiety. 2017 Sep;34((9)):801–8. doi: 10.1002/da.22629. [DOI] [PubMed] [Google Scholar]
- 135.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- 136.Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. 2nd ed. New York: Guilford Press; 2012. [Google Scholar]
- 137.Fava GA, Bech P. The concept of euthymia. Psychother Psychosom. 2016;85((1)):1–5. doi: 10.1159/000441244. [DOI] [PubMed] [Google Scholar]
- 138.Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45((1)):5–31. doi: 10.1080/16506073.2015.1098724. [DOI] [PubMed] [Google Scholar]