Abstract
In the past decade, tuberculosis incidence has declined in much of the world, but has risen in central and South America. It is not yet clear what is driving this reversal of progress in tuberculosis control. Since 2000, the incarcerated population in central and South America has grown by 206%, the greatest increase in the world. Over the same period, notified tuberculosis cases among the incarcerated population (hereinafter termed persons deprived of their liberty [PDL], following the Inter-American Commission on Human Rights) have risen by 269%. In both central and South America, the rise of disease among PDL more than offsets tuberculosis control gains in the general population. Tuberculosis is increasingly concentrated among PDL; currently, 11% of all notified tuberculosis cases in central and South America occur among PDL who comprise less than 1% of the population. The extraordinarily high risk of acquiring tuberculosis within prisons creates a health and human rights crisis for PDL that also undermines wider tuberculosis control efforts. Controlling tuberculosis in this region will require countries to take urgent measures to prioritise the health of PDL.
Introduction
Tuberculosis kills more people than any other infectious disease, and in 2018 led to 1·2 million deaths and an additional 251 000 deaths among people living with HIV.1 Despite enhanced control efforts, substantial research advances, and increased funding,2 in recent years global tuberculosis incidence has declined only slowly, at a rate of 1–2% per year.1 Alarmingly, in central and South America, tuberculosis incidence has stagnated or risen.1 This reversal in progress against tuberculosis is not fully understood.
Since 2000, the incarcerated population (hereinafter termed persons deprived of their liberty [PDL], following the Inter-American Commission on Human Rights3) has grown by 24% globally.4 Much of this recent growth has occurred in the Americas,4 where 3·8 million people are currently incarcerated.4 In central and South America, the prison population has expanded by 206% because of increasing incarceration rates over this period (appendix p 1).4 Incarceration has serious social and public health consequences and puts people at heightened risk of mental illness, chronic diseases, and infectious diseases, including COVID-19, HIV, hepatitis C, and tuberculosis.5–9 Frequently, the epidemiological impact of incarceration extends to the families and communities of PDL.10
Prisons and other detention centres concentrate people into high-risk environments for transmission of infection, where access to health care is inadequate (panels 1, 2). The physical environment of prisons, including extended indoor confinement, poor ventilation, severe overcrowding, and limited sunlight exposure facilitate airborne transmission of pathogens.11 In a South African prison, overcrowding and poor case finding led to an annual tuberculosis infection risk of 90%.16 Although incarceration is a pronounced risk factor for tuberculosis,17 the effect of incarceration on national tuberculosis control efforts is largely unknown.
To reach regional and global targets of an 80% decrease in tuberculosis incidence by 2030 (compared with 2015 levels), we need to identify and address drivers of recent increases in tuberculosis incidence in central and South America. Here, we review data indicating that the recent substantial growth in imprisoned populations may be an important factor.
Assembling country-level tuberculosis case notifications in prisons and incarceration data
Although PDL are acknowledged by WHO as a high-risk population for tuberculosis,18 global data on tuberculosis cases among PDL are not routinely collected. We collaborated with the Pan American Health Organization (PAHO) and ministries of health to assemble case notification data for tuberculosis among PDL from 19 central and South American countries up to 2018. Notification data include total annual new and relapsed tuberculosis cases among incarcerated populations. The notification data were acquired through PAHO. Time series of case notifications among PDL differ across countries; to characterise regional trends over a consistent 6-year period, we extrapolated case notifications among PDL using cubic splines (appendix p 5).
To calculate the relative risk of tuberculosis among PDL compared with the general population in the same country and same year (appendix p 5), we included WHO country-level tuberculosis notifications, which include new and relapsed cases in addition to cases with unknown tuberculosis treatment history.1 We used incarceration data from the World Prison Brief and again extrapolated missing years (appendix p 5). We used the prisonbrief R package to access World Prison Brief data. Data and code to reproduce the manuscript figures are available online.
Increasing incarceration across central and South America
From 2000 to 2018, the prison population increased by 206% across central and South America, rising from 492 805 to 1 349 063 (appendix p 1).4 The greatest relative increases occurred in El Salvador, where the incarcerated population increased by 411%, and Ecuador, where the incarcerated population increased by 367%. The pronounced increase in PDL cannot be explained by the 22·9% growth in the total population from 2000 to 2018, but, instead, could be explained by rising incarceration rates across all countries in central and South America (appendix p 1). In 12 countries, incarceration rates more than doubled from 2000 to 2018.
Rapid increases in incarceration rates have led to severe prison overcrowding. Prisons in the region operate at an average of 167% occupancy. Overcrowding is particularly acute in some countries; in El Salvador, prisons operate at 348% capacity. Data on capacity are from World Prison Brief.
The growing burden of tuberculosis within prisons
From 2011 to 2017, tuberculosis case notifications among PDL quadrupled in central America (538 to 2489 cases) and more than doubled in South America (7798 to 17 285 cases; figure 1). Tuberculosis is also increasingly concentrated in prisons; in 2011, 8336 (5·0%) of 168 563 reported tuberculosis cases in central and South America occurred among PDL, compared with 19 774 (11·1%) of 177 622 in 2017 (figure 2). This increasing concentration of tuberculosis in prisons was most pronounced in Venezuela (113 [1·8%] of 6282 reported cases in 2011 compared with 1624 [15·3%] of 10 647 reported cases in 2017) and El Salvador (225 [11·9%] of 1896 reported cases in 2011 compared with 1889 [51·5%] of 3666 reported cases in 2017; figure 2).
Figure 1: Change in notified tuberculosis cases among PDL and the general population from 2011 to 2017.
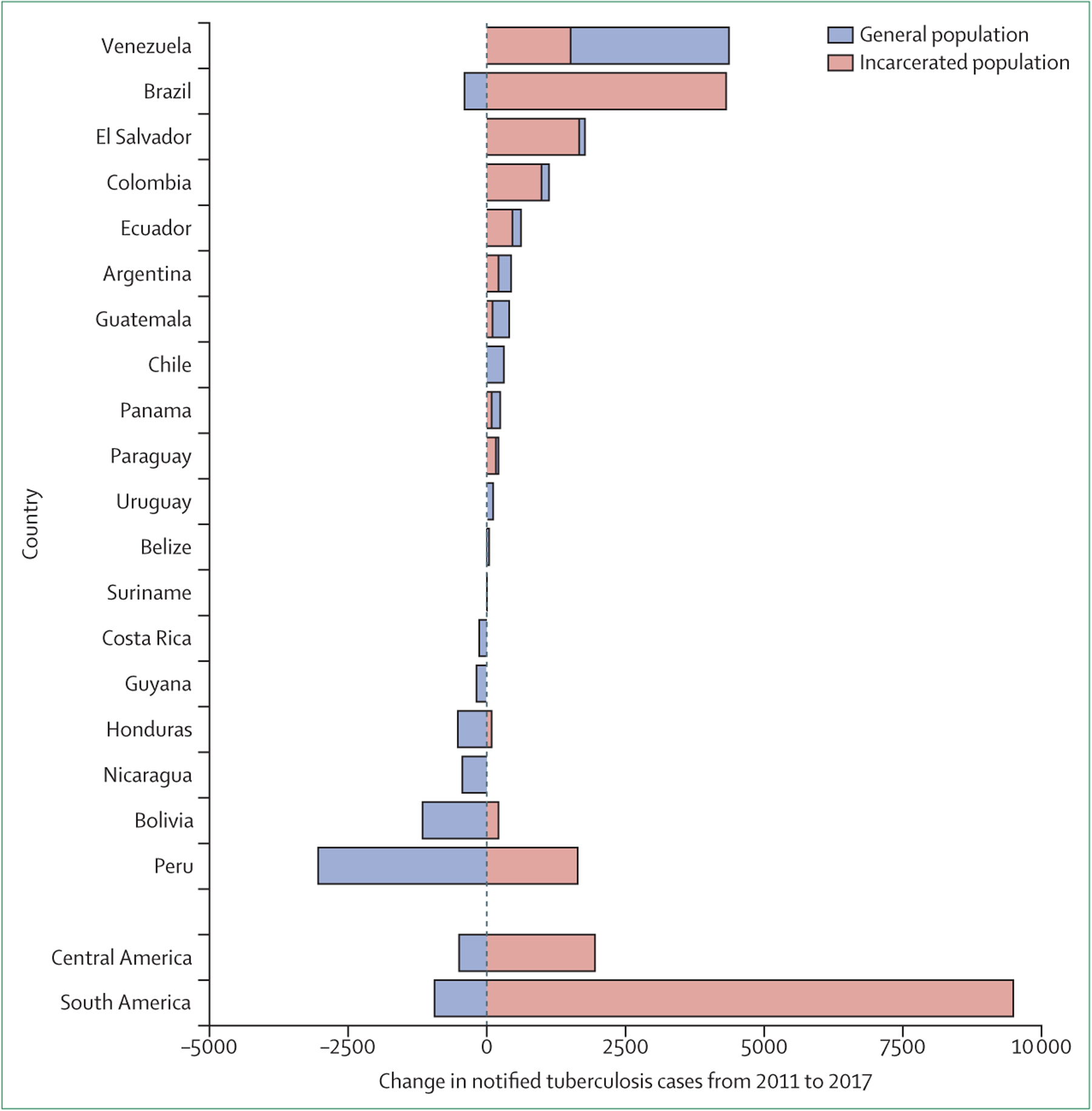
Change in notified tuberculosis cases for each country, ordered by cumulative change in tuberculosis burden over time, and change including all countries in both central and South America. Time series of case notifications among PDL differ across countries (appendix p 4); to characterise regional trends over a consistent time frame, we used cubic splines to extrapolate and interpolate missing years of case notifications among PDL for a 6-year period (2011–17) as described in the appendix (p 5). PDL=persons deprived of liberty.
Figure 2: Increasing burden of tuberculosis among PDL in central and South America.
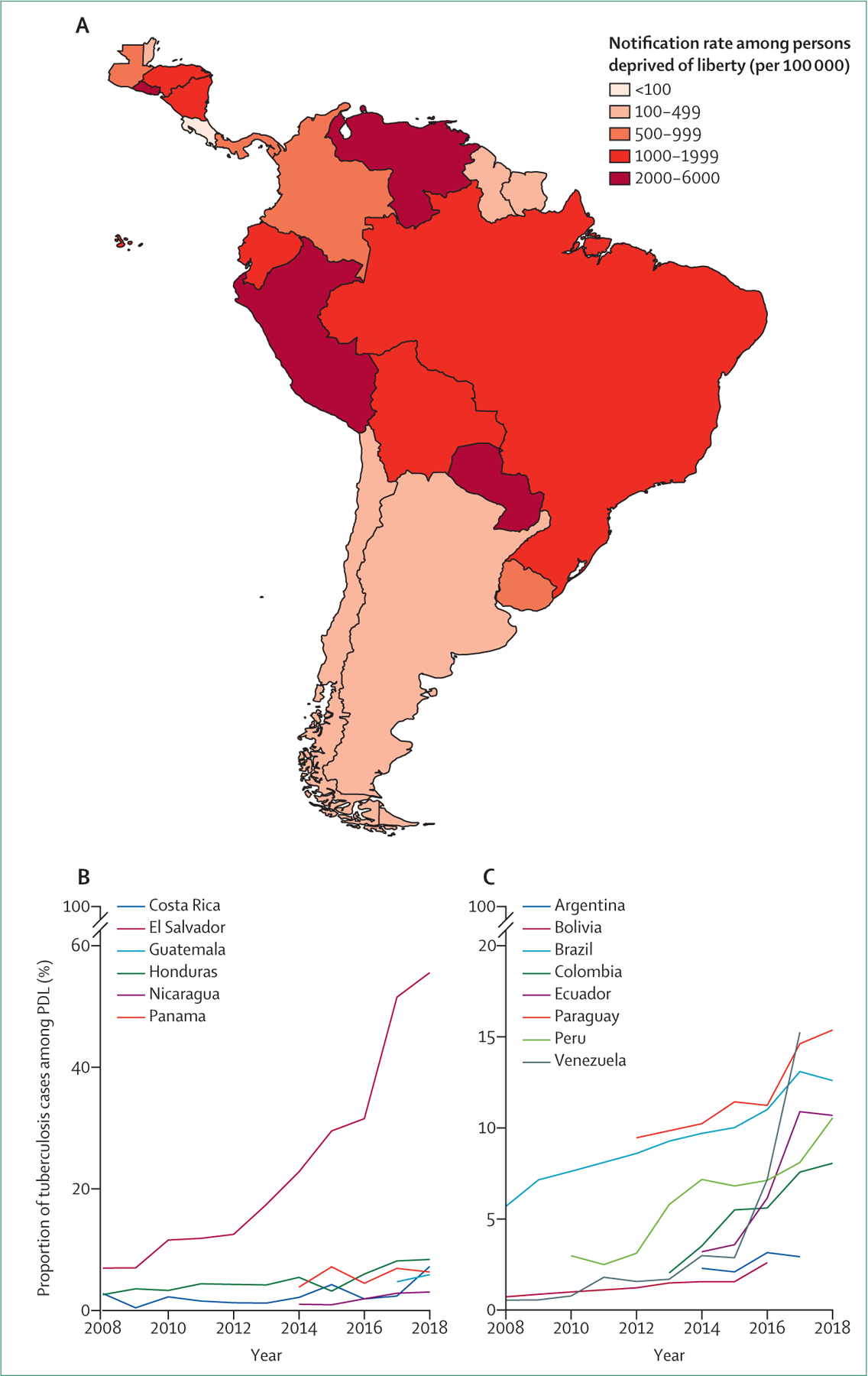
(A) Tuberculosis case notification rate among PDL in the most recent year of reported data (from 2014 [Belize] to 2018 [several countries]; appendix p 4). The percentage of tuberculosis notifications among PDL in central America (B) and South America (C) from 2008 to 2018. Countries with more than ten cases among PDL are included for central America and more than 100 cases among PDL for South America. Time series of case notifications among PDL differ across countries (appendix p 4). PDL=persons deprived of liberty.
In all central and South American countries, tuberculosis notification rates among PDL exceeded rates in the general population (appendix pp 2–3). In Venezuela, Paraguay, Ecuador, El Salvador, and Guatemala, case notification rates inside prisons were more than 40 times higher than notification rates outside prisons, in the most recent year of available data (ranged from 2014 [Belize] to 2018 [several countries]; appendix p 3). Although case notification rates were relatively stable in the general population, they increased in prisons throughout much of central and South America from 2011 to 2017 (appendix p 2).
The population attributable fraction (PAF) compares the observed tuberculosis burden with that expected if the risk created by incarceration were eliminated (appendix p 1). The extremely high and increasing relative risk of incarceration corresponds to an increase in the PAF of incarceration from 4·5% in 2011 to 9·7% in 2017. The PAF of incarceration exceeds global PAF estimates of diabetes (3·1%), smoking (7·6%), alcohol use (8·1%), and HIV (8·1%),1 and resulted in more than 16 000 excess tuberculosis cases attributable to incarceration in 2017. Mass incarceration is recent and incarceration rates are not fixed, but they have increased markedly since 2000 (appendix p 1). The substantial PAF of incarceration underscores that reducing exposure to incarceration—by reducing incarceration rates—could markedly reduce the population-level burden of tuberculosis.
The effect of incarceration on the general tuberculosis epidemic
The increasing tuberculosis burden among PDL in central and South America may explain recent stalled progress in tuberculosis control. In central America, total annual tuberculosis notifications increased from 13 082 in 2011 to 14 534 in 2017. Even though overall annual notifications outside prisons decreased, this was more than offset by the increase of 1951 cases among PDL (figure 1).
Similarly, total annual tuberculosis notifications in South America increased from 155 481 in 2011 to 164 024 in 2017. Declines outside prisons were more than offset by the increase of 9487 cases among PDL (figure 1). These trends reflect the combined effect of growth in the incarcerated population and moderate increases in tuberculosis incidence among PDL, in contrast with the comparatively stable incidence in the general population (appendix p 2).
Although tuberculosis is increasingly concentrated among PDL across the region, the trajectories of individual countries vary (figure 1). The stark increase in tuberculosis among PDL in central America is largely driven by the increase of 1664 cases in El Salvador from 2011 to 2017, while the observed decline in cases outside of prisons can be largely attributed to declines in Honduras (with a decline of 435 cases) and Nicaragua (with a decline of 438 cases).
With the largest population in the region (209 million in 2018), regional trends in South America are driven by Brazil, which reported the largest growth in absolute number of notified tuberculosis cases in prisons (4314 cases). While tuberculosis notifications in this country declined in the general population, the growth of cases in prisons was more than the declines from 2011 to 2017, leading to a net growth of tuberculosis cases. Brazil accounted for 4314 (45%) of the increase in tuberculosis cases among PDL and for 402 (43%) of the decrease in cases in the general population in South America from 2011 to 2017. Tuberculosis cases increased in both the prisons and the general population in several countries, while in Peru, Bolivia, and Honduras, overall cases declined despite substantial increases in prisons (figure 1). Cumulatively, central and South America both reported declines in tuberculosis cases in the population outside prisons, but 11 countries reported increases in tuberculosis cases outside prisons from 2011 to 2017, most notably in Venezuela. No country documented decreases in tuberculosis notifications among PDL.
An under-recognised burden and data limitations
Tuberculosis case notifications reflect underlying incidence as well as case detection rates, which depend on health-care and surveillance infrastructure and can vary across countries. Although it is difficult to distinguish improvements in case detection from underlying growth in an epidemic, notification data are likely to underestimate the true burden of tuberculosis attributable to incarceration. First, the lack of health-care infrastructure in most prisons suggests that under-reporting is likely. Second, prisons often act as institutional amplifiers of tuberculosis,13 perpetuating the epidemic through spillover of disease from high-transmission prison environments into the population outside. However, notification data do not include infections that occur in prison, but are diagnosed only following release. Third, prison workers,19 visitors, and family members are all put at high risk of infection by entering prisons and contribute to a hidden tuberculosis burden attributable to prisons.
Recent investments in case finding and diagnostic capacity in prisons by many countries in central and South America may contribute to the observed increases in tuberculosis notifications among PDL. For example, after a case finding programme was introduced in El Salvador prisons in 2011, tuberculosis notification rates among PDL increased.20 Cases notified among PDL may reflect infection in the community before incarceration. However, our observational and modelling study in Brazil13 found that at the time of incarceration, individuals had low prevalence of latent tuberculosis. Rates of tuberculosis rose during incarceration and, after release, declined to that of the general population over a period of seven years. These results suggest that the prison environment, rather than host risk factors, drives tuberculosis risk (panels 1, 2). Concurrent rises in inequality, economic recession, and cuts in funding for health and social programmes in the region are likely to also contribute to increases in population-wide tuberculosis incidence (appendix p 2). Finally, estimates of incarcerated population size may also have low accuracy.
An escalating health and human rights crisis
Across central and South America, rapid increases in incarceration have put PDL at extremely high risk of tuberculosis, contributing to a disproportionate and growing burden of tuberculosis. Although notification rates outside prisons have declined modestly, they have increased slightly within prisons. The growing epidemic within prisons constitutes a health and human rights crisis for incarcerated populations and subverts gains in tuberculosis control elsewhere. Consequently, addressing the escalating tuberculosis burden within and outside of prisons requires urgent action that extends far beyond biomedical interventions.
The detention of people in environments with extraordinarily high risk of tuberculosis infection, without access to adequate preventive measures or health care, constitutes systematic violation of national and international human rights law, including the Nelson Mandela Rules and the Principles and Best Practices on the Protection of PDL in the Americas.3,7,21 As stated by the Institute for Criminal Policy Research, “A sentence of imprisonment is a sentence of deprivation of liberty, not of damage to health”.22 Human rights law has been—and should continue to be—invoked to hold states responsible for protecting the right to health and humane living environments of incarcerated people. For example, the Rio de Janeiro State public defender sued the state for failing to prevent high tuberculosis mortality within state prisons.23 In another case, the Inter-American Court of Human Rights ordered Brazil to implement an emergency health-care plan in Curado Prison in Pernambuco State to reduce rampant overcrowding and improve tuberculosis diagnosis and treatment.24
However, we cannot rely on the courts alone to reverse increases in imprisonment. To minimise the population put at increased risk of tuberculosis, governments will need to reduce incarcerated populations and find alternatives to criminal justice policies that rely on detention.25 The early prison releases begun by many countries in response to the COVID-19 pandemic show that such reductions in prison populations are politically feasible. Incarceration should be considered a last resort and alternatives such as restorative justice approaches should be made available in its place.22 Reducing the population of pre-trial detainees—who make up more than 36% of the incarcerated population across the Americas26—is one of many ways to reduce the population put at increased risk of tuberculosis and other infectious diseases.25 The recent growth in the length of prison sentences also contributes to overcrowding and ageing of the incarcerated population.22 Finally, the criminalisation of drugs is a major driver of increased incarceration across the Americas, and reforms of drug laws would reduce crowding and thereby diminish the infection risk associated with prisons.14 In Brazil, for example, the number of people incarcerated because of drugs increased by 345% from 2005 to 2013.27 The recent rise in incarceration rates of women across many countries in central and South America largely reflects the criminalisation of drugs; in many countries, most women in prison are incarcerated for drug crimes.27 Drug laws are applied selectively, resulting in disproportionate incarceration of racial minorities and poor people.27–29
Immediate action is also needed to reduce health risks for people currently incarcerated across central and South America. Although several countries in the region have recently expanded tuberculosis diagnosis in detention facilities,20 diagnostic infrastructure and overall health care within prisons remain inadequate. Systematic active screening for tuberculosis at prison entry and exit, improvements in ventilation, isoniazid preventive therapy, and other infection control measures are likely to improve case finding and reduce transmission within prisons and spillover outside prisons.11,13,30 Success of tuberculosis treatment is dependent on the continuity of medical care, and improving treatment outcomes will require expanding access to housing, food, and other essential services during and after incarceration.7 The urgency of this health crisis will require further collaboration between national tuberculosis programmes, ministries of justice, and correctional system authorities that could be facilitated by PAHO and other agencies, to ensure that health care is not differentiated by incarceration status.
An effective response to the crisis of tuberculosis in PDL requires consistent and centralised reporting and close monitoring of the epidemic in prisons. WHO should collect and report case notifications among PDL, as PAHO has begun to do, and monitor the PAF of incarceration, as it does for several other risk factors for tuberculosis.1 Although central and South America have not yet been affected by extraordinarily high rates of drug-resistant tuberculosis in prisons, as seen in many eastern European countries,31 the current trajectory suggests that drug resistance should also be closely monitored.32,33
In central and South America, the tuberculosis epidemic continues to impose a substantial health burden and is increasingly concentrated in PDL. The social and environmental conditions that drive tuberculosis transmission within prisons also drive transmission of many other infectious diseases, including COVID-19. Incarceration rates continue to rise in many countries, and the burden of disease attributable to prisons is growing. These effects transcend prison walls and may be undermining regional tuberculosis control efforts. The health and human rights crisis of tuberculosis among PDL and their communities demand urgent action and sustained attention from ministries of health and justice and the global medical community.
Supplementary Material
Panel 1: Environmental tuberculosis risk factors potentially affected by incarceration.
Incarceration has severe and lasting physical and mental health consequences.6
Overcrowding
Prisons are frequently over capacity; many people are forced to live in close proximity,4 where the rate of potentially infectious tuberculosis contacts is high.11
Access to health care
Prisons often have inadequate health-care capacity and insufficient health-care personnel; underlying medical conditions may go undiagnosed and untreated; tuberculosis may be undiagnosed, diagnosed late, or untreated.7,8
Access to nutrition
Prisons frequently do not provide sufficient, nutritious food, increasing susceptibility to tuberculosis.7
Poor ventilation
Low air exchange rate within prison cells increases the risk of airborne tuberculosis transmission.7,11
Indoor and unsanitary confinement
Indoor confinement in overcrowded cells increases transmission risk;11 indoor confinement reduces the potential for the sun’s ultraviolet radiation to inactivate Mycobacterium tuberculosis and is associated with low concentrations of vitamin D among incarcerated people, which is linked to increased risk of active tuberculosis disease.12
Disruption of social and support networks
The removal of people from their families and communities is associated with deterioration in overall physical and mental health and can increase susceptibility to many infections.6
Movement by the carceral system
Frequent movement within and between prisons increases the size of contact networks and can amplify tuberculosis epidemics;13 movement can also disrupt treatment regimens.
Panel 2: Host tuberculosis risk factors potentially affected by incarceration.
Host risk factors reflect the impact of incarceration and previous incarceration on individuals, including the disproportionate incarceration of poor people and minority groups who may have been marginalised by health-care systems before incarceration.
HIV status
Prisons are also high-risk transmission environments for HIV, hepatitis C, and other infections;14 co-infection with HIV increases susceptibility to tuberculosis.
Smoking
Higher rates of smoking among some incarcerated populations is associated with increased risk of tuberculosis infection10 and may increase infectiousness (risk of onward transmission).15
Drug use
The criminalisation of drug use and subsequent higher rates of drug use among incarcerated populations is associated with increased tuberculosis risk.14
Access to health care before incarceration
The disproportionate incarceration of poor people and minority groups perpetuates disparities in access to health care that may exist before incarceration.7
Acknowledgments
LM was supported by a National Institutes of Health (NIH) award T32 AI 052073. JRA and KSW were supported by NIH award R01 AI130058. The funding source had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. We would like to thank the national tuberculosis programmes across countries in central and South America who provided the data discussed in this manuscript: Argentina, Belize, Bolivia, Brazil, Chile, Colombia, Costa Rica, Ecuador, El Salvador, Guatemala, Guyana, Honduras, Nicaragua, Panama, Paraguay, Peru, Suriname, Uruguay, and Venezuela. We would also like to acknowledge the contributions of Pedro Avedillo, Ernesto Montoro, Oscar Bernal, and Keisha Westby, members of the PAHO Regional Tuberculosis Team who reviewed the manuscript and provided comments.
Footnotes
For the World Prison Brief see https://www.prisonstudies.org/
For the prisonbrief R package see https://danilofreire.github.io/prisonbrief/
For the data and code used to reproduce manuscript figures see https://github.com/ksw9/tb-prisons-americas
Declaration of interests
RAL-O serves as Tuberculosis Prevention, Control and Elimination Advisor at the HIV, Hepatitis, Tuberculosis and Sexually Transmitted Infections Unit of the PAHO. MAE is Director of the Department of Communicable Diseases and Environmental Determinants of Health at the PAHO. All other authors declare no competing interests.
References
- 1.WHO. Global tuberculosis report 2019. Geneva: World Health Organization, 2019. [Google Scholar]
- 2.Su Y, Garcia Baena I, Harle AC, et al. Tracking total spending on tuberculosis by source and function in 135 low-income and middle-income countries, 2000–17: a financial modelling study. Lancet Infect Dis 2020; 20: 929–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inter-American Commission on Human Rights. Report on the human rights of persons deprived of liberty in the Americas. Washington, DC: Dec 31, 2011. http://www.oas.org/en/iachr/pdl/docs/pdf/PPL2011eng.pdf (accessed Aug 9, 2020). [Google Scholar]
- 4.Walmsley R World prison population list, 12th edn. London: Institute for Criminal Policy Research, 2018. [Google Scholar]
- 5.Fazel S, Hayes AJ, Bartellas K, Clerici M, Trestman R. Mental health of prisoners: prevalence, adverse outcomes, and interventions. Lancet Psychiatry 2016; 3: 871–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fazel S, Baillargeon J. The health of prisoners. Lancet 2011; 377: 956–65. [DOI] [PubMed] [Google Scholar]
- 7.Rubenstein LS, Amon JJ, McLemore M, et al. HIV, prisoners, and human rights. Lancet 2016; 388: 1202–14. [DOI] [PubMed] [Google Scholar]
- 8.Cords O, Martinez L, Warren J, et al. Incidence and prevalence of tuberculosis in incarcerated populations: a systematic review and meta-analysis. Lancet Public Health (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akiyama MJ, Spaulding AC, Rich JD. Flattening the curve for incarcerated populations - COVID-19 in jails and prisons. N Engl J Med 2020; published online April 2. 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacchi FPC, Praça RM, Tatara MB, et al. Prisons as reservoir for community transmission of tuberculosis, Brazil. Emerg Infect Dis 2015; 21: 452–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Urrego J, Ko AI, da Silva Santos Carbone A, et al. The impact of ventilation and early diagnosis on tuberculosis transmission in Brazilian prisons. Am J Trop Med Hyg 2015; 93: 739–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maceda EB, Gonçalves CCM, Andrews JR, Ko AI, Yeckel CW, Croda J. Serum vitamin D levels and risk of prevalent tuberculosis, incident tuberculosis and tuberculin skin test conversion among prisoners. Sci Rep 2018; 8: 997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mabud TS, de Lourdes Delgado Alves M, Ko AI, et al. Evaluating strategies for control of tuberculosis in prisons and prevention of spillover into communities: an observational and modeling study from Brazil. PLoS Med 2019; 16: e1002737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet 2016; 388: 1089–102. [DOI] [PubMed] [Google Scholar]
- 15.Huang CC, Tchetgen ET, Becerra MC, et al. Cigarette smoking among tuberculosis patients increases risk of transmission to child contacts. Int J Tuberc Lung Dis 2014; 18: 1285–91. [DOI] [PubMed] [Google Scholar]
- 16.Johnstone-Robertson S, Lawn SD, Welte A, Bekker LG, Wood R. Tuberculosis in a South African prison – a transmission modelling analysis. S Afr Med J 2011; 101: 809–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Pan American Health Organization. Tuberculosis in the Americas 2018. Washington, DC: Pan American Health Organization, 2018. [Google Scholar]
- 18.WHO. Status paper on prisons and tuberculosis. Copenhagen: World Health Organization, 2007. [Google Scholar]
- 19.Nogueira PA, Abrahão RMCM, Galesi VMN. Infecção tuberculosa latente em profissionais contatos e não contatos de detentos de duas penitenciárias do estado de São Paulo, Brasil, 2008. Rev Bras Epidemiol 2011; 14: 486–94. [DOI] [PubMed] [Google Scholar]
- 20.Ayala G, Garay J, Aragon M, Decroo T, Zachariah R. Trends in tuberculosis notification and treatment outcomes in prisons: a country-wide assessment in El Salvador from 2009–2014. Rev Panam Salud Publica 2016; 39: 38–43. [PubMed] [Google Scholar]
- 21.UN Office on Drugs and Crime. The United Nations standard minimum rules for the treatment of prisoners (the Nelson Mandela Rules). Vienna: United Nations Office on Drugs and Crime, 2016. [Google Scholar]
- 22.Heard C Towards a health-informed approach to penal reform? Evidence from ten countries. London: Institute for Crime & Justice Policy Research, 2019. [Google Scholar]
- 23.Larouzé B, Ventura M, Sánchez AR, Diuana V. Tuberculose nos presídios brasileiros: entre a responsabilização estatal e a dupla penalização dos detentos. Cad Saude Publica 2015; 31: 1127–30. [DOI] [PubMed] [Google Scholar]
- 24.Sidhu N, Clark M, Barba M, et al. Tuberculosis, human rights and the law: a compendium of case law, 1st edn. Chicago, IL: International Human Rights Clinic, University of Chicago Law School, 2017. [Google Scholar]
- 25.Heard C, Fair H. Pre-trial detention and its over-use: evidence from ten countries. London: Institute for Crime & Justice Policy Research, 2019. [Google Scholar]
- 26.Walmsley R World pre-trial/remand imprisonment list, 3rd edn. London: Institute for Criminal Policy Research, 2016. [Google Scholar]
- 27.Boiteux L The incarceration of women for drug offenses. The Research Consortium on Drugs and the Law (CEDD), 2015. http://fileserver.idpc.net/library/CEDD-women-2015.pdf (accessed July 1, 2020).
- 28.Campos MS. Pela metade: a lei de drogas do Brasil. São Paulo: Annablume, 2019. [Google Scholar]
- 29.Campos MS. Growingly empty, growingly full: drug policy reform in Brazil. Norman, OK: University of Oklahoma, Center for Brazil Studies, 2020. [Google Scholar]
- 30.Santos AdS, de Oliveira RD, Lemos EF, et al. Yield, efficiency and costs of mass screening algorithms for tuberculosis in Brazilian prisons. Clin Infect Dis 2020; published online Feb 17. 10.1093/cid/ciaa135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zumla A, Grange JM. Multidrug-resistant tuberculosis—can the tide be turned? Lancet Infect Dis 2001; 1: 199–202. [DOI] [PubMed] [Google Scholar]
- 32.Warren JL, Grandjean L, Moore DAJ, et al. Investigating spillover of multidrug-resistant tuberculosis from a prison: a spatial and molecular epidemiological analysis. BMC Med 2018; 16: 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ritacco V, López B, Ambroggi M, et al. HIV infection and geographically bound transmission of drug-resistant tuberculosis, Argentina. Emerg Infect Dis 2012; 18: 1802–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


